#is this the medication or just my personality and the way i’ve developed with condition? who can say
Explore tagged Tumblr posts
Text
i have the type of adhd that makes me try aggressively harder until it consumes me when it’s extremely difficult to acquire medication, instead of giving up because phone calls scary
#an hour and a half of my work day has been dedicated to this#honestly at this point it’s out of spite i take like 10mg twice a day#some insane part of me is like ‘oh there’s a shortage? this bullshit is def making other ppl with adhd give up but i am the alpha’#‘and i will persist and acquire the limited resource’#is this the medication or just my personality and the way i’ve developed with condition? who can say#but i’m not going to be beaten here#i will choose to go off of it but only if i genuinely think it’s the right call#and not bc i’m unwilling to do what i need to do to get it#only allowed to refill the day i run out every single month? i’ve got it hand me the phone and calendar#insurance changing coverage guidelines? doctor’s appointment made to get prior authorization or otherwise change dosage#widespread shortage? i will call every pharmacy in the area to figure out who has it this month#and call my doctor’s office as many times asking them to send it there#until they get it right after two inevitable failures#all in the same 7 hour period bc i’m legally only allowed to fill it when i’m literally about to be out of it#all while i have FUCKING ADHD
5 notes
·
View notes
Text
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
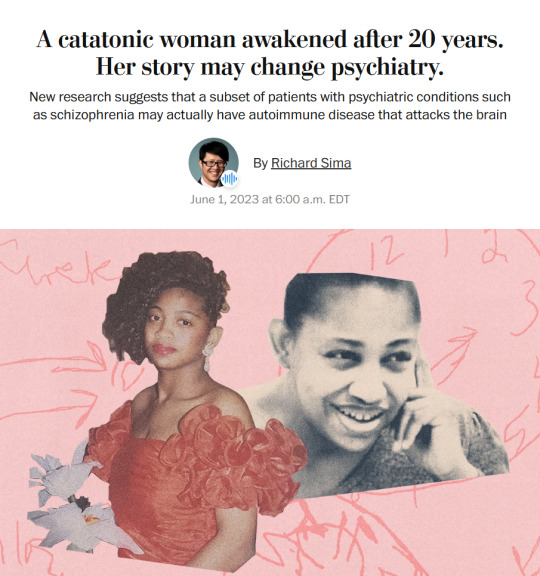
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes
Note
Begging you to stop assuming that trans people are just gay people who can't admit to being gay. I'm bi regardless of whether I'm the woman the body I was born into is supposed to make me or the man that I feel like I was supposed to be. I won't say that no one has ever transitioned to avoid homophobia, but there are better ways to address that than to stop genuinely transsexual people from transitioning.
I've been in therapy for 27 years. Since puberty sunk its teeth in me. NOTHING is going to make me feel like being a woman is the right fit for me and trying to force myself to fit into that box has made me suicidal for decades. Convincing myself I could just be a masculine woman barely soothed any of that. I'm sorry that transition wasn't the right fit for you, and you deserve all of the support you need for that, but it's no more fair to force me to be a woman just because of the body that I was born into than it would be to force you to keep identifying as a man and taking hormones.
I don’t know you and it’s none of my business how you live your life.
My opposition to transition is primarily due to the medical risks of testosterone therapy on women.
Testosterone causes our reproductive organs to atrophy, potentially irreversibly. I’ve heard stories of people who develop chronic pain, persisting even after stopping T. People whose ovaries no longer work correctly after only a few years on T, causing various problems from low hormone production. People with urinary incontinence and pelvic floor issues caused by T essentially putting them into early menopause. PCOS worsening. Ovaries twisting. People who have had unnecessary gynecological surgeries due to the effects of T. People with chronic chest pain after top surgery. People who developed arthritis in their joints, or autoimmune conditions while on T. People who had mental health crises triggered by being on testosterone. People with chronic debilitating vocal pain or clitoral pain due to the effect on those areas. People who developed cholesterol or blood pressure problems only after being on T, causing them to be at higher risk for heart health issues.
That’s just off the top of my head, and that’s just things I’ve personally witnessed in myself and friends, both trans and detrans.
Live your life, do what makes you happy. I’m not going to stop talking about this health crisis that’s currently affecting young women, many of whom are just gay or tomboys, and would eventually become fine with themselves if they were able to grow up with masculine female role models and actual feminist education.
Even if there was a small minority of “true transsexuals”, even if you are one of them, that doesn’t make what I’m saying wrong or unimportant. You can’t deny that women are getting harmed by transition.
38 notes
·
View notes
Text
Entry #012
Hypermobility
A problem many autistic fellows of mine, including me, are suffering from is hypermobility. It's a underdiagnosed, underrecognized part of autism.
I personally deal with Ehlers-Danlos Syndrome (EDS), which runs in my family. My great-grandmother, grandmother, and mother all have it, and so do I. It comes with a host of symptoms: atrophic scars, mitral valve insufficiency, postural / orthostatic tachycardia syndrome, gastric motility disorder, pelvic and bladder dysfunction, extremely soft and stretchy skin, and, of course, extreme hypermobility. I can bend my joints in ways that I only learned in medical school was abnormal, and I’ve often felt like a bit of a freak during skills practices. I remember asking an orthopaedic surgeon during training why people couldn’t do 90 degrees flexion and extension with their forefeet, only to be met with confusion. When I demonstrated what I meant, the look on his face was one of pure astonishment. This highlights how different our experiences can be and how misunderstood they often are.
One of the most frustrating parts is not being taken seriously by some doctors. I’m lucky to have a medical degree and trusted colleagues I can consult, but many autistic individuals don’t have this luxury. Too often, our symptoms are dismissed or attributed to our mental health, leading us to delay seeking help until things get really bad. Please, don’t wait. The longer you put off seeing a doctor, the harder it becomes to treat your symptoms. Find a physician who listens and takes you seriously. Hypermobility doesn't necessarily mean you have EDS, but hypermobile or not, moving and living isn’t easy. Chronic exhaustion is real and debilitating. I touched on managing energy levels in entry #003 with routines based on my modified spoon theory, which I call the cutlery theory. I’ll dive deeper into this in a future post.
Living with hypermobility means constant joint pain, frequent dislocations, and early arthritis. I’ve never known a pain-free day, and overdoing it physically just makes things worse. Recovery takes time, and I’m still figuring out if physical and mental fatigue recover together or separately. Overstraining definitely not only impacts physical, but also my mental state. Not everyone can access rehabilitation programs, but there are steps you can take on your own to make it a little easier or better. Start by tracking your symptoms to identify patterns. This can help you find ways to support yourself. Working with a physiotherapist or occupational therapist is ideal, but you can also use trial and error to find what works for you. I’m always here to brainstorm and offer support.
I’m a big believer in creative therapy. One exercise is to color in a body image to show where you feel comfortable, uncomfortable, or in pain. This helps you and your healthcare providers understand your condition better and develop a personalised treatment plan.
Also, braces can be a lifesaver for dislocated or overstretched joints, even though I hate wearing them. They help prevent further injury and aid in recovery. Despite the awkward looks and comments, they’re definitely worth it.
In conclusion, hypermobility is often a comorbidity of autism. It can cause mental fatigue and chronic pain, among other symptoms. Don’t suffer in silence, but find ways to accommodate yourself and make life easier. Medication and surgery aren’t always the answers, although they can help. Awareness and lifestyle adjustments can make a big difference too. Talk to your physician, physiotherapist, occupational therapist, and fellow patients to find what works for you.
#autism#autistic#high functioning autism#autistic spectrum#autism spectrum disorder#autistic adult#autistic community#actually autistic#autistic things#being autistic#autistic experiences#unmasking autism#high masking autism#hypermobility#hypermobile ehlers danlos#hypermobile eds#hypermobile spectrum disorder#chronic fatigue#mental fatigue#chronically fatigued
16 notes
·
View notes
Text

Hi I do education stuff including public facing sliding scale online workshops and classes n shit. More deets below cut
This workshop covers a variety of holistic pain management strategies for individuals and practitioners, primarily focusing on chronic pain.
Upcoming class date: Sunday March 3rd, 4:00PM-5:30PM EST
Registration: Send an email to mildewamyx(at)protonmail(dot)com and specify the email or phone # you would like me to send the class link & recording to. You don't have to attend live to recieve the recording but you do have to register.
Requirements: This is an intermediate-level workshop that assumes familiarity with western herbal terminology and herbal medicine making. (pssst! All background knowledge required is covered in An Anarchist Free Herbal)
Suggested donation: $15-$45; No one turned away for lack of funds
Recording policy: Registration is required to receive the recording. There will be an UNRECORDED q&a portion at the end of the class.
Background
I’ve been in pain every day for over half my life, from a varying combination of joint instability, neurological problems, and repetitive injuries. Like many chronically ill and disabled people, my experience of pain is not just a sense of urgency or a signal to stop doing something: It’s brain fog, immobility, dissociation, low empathy, a short temper, mood swings, both an ever-present sensation and something I have to actively remember to address. Naturally, I’ve spent a lot of my life thinking about and discussing extreme pain. Many friends and accomplices and I have been dissatisfied with pain management options available via western medicine; especially when we’ve been presented with potentially-dangerous long-term NSAID prescriptions or non-indicated medications with unpleasant side effects. Herbalism can offer a wider range of potential management strategies that can be compatible with western medical treatment for underlying conditions or offer relief to those of us who have chosen not to pursue or continue medical treatment for any number of personal reasons.
Course Description
Over the years, I’ve developed a set of specific indications centering around different experiences of pain, which I will now share with you! We’ll talk about ways of conceptualizing and communicating about pain and explore a wide variety of pain management options—Not just analgesic herbs (although don’t get me wrong, there’s plenty!) but strategies and practices for living with chronic and long-term pain like sensory redirection, ritual, nervous system support and more. This workshop intends to develop a rich, multifaceted and adaptable toolkit that focuses on increasing quality of life in difficult situations with strategically-targeted, doable steps.
14 notes
·
View notes
Text
A while ago I did an interview with stats Canada (basically the organization responsible for census and demographics data in canada) about potentially developing a census question about being intersex, and the person doing the interview was super nice and receptive, but one of the things I tried to convey especially is that with intersex people, if you’re surveying our prevalence or whatever in a population based off of self-reported answers like a census, the number you come up with is probably going to be less than the actual number of us out there to the point where it’s almost certain that there’s a higher percentage of intersex people out there than a census number suggests. This isn’t to say that it’s not important to have data that’s as accurate as can be about us on a national scale, because that’s one of the reasons I did the interview because it is important to help work on policy etc, but being intersex isn’t necessarily like other demographic information in that there’s a few ways that can and will interfere with someone’s reporting of their intersex status, and so there will be a gap between how many people say they are intersex on a survey and the higher number of how many people actually are intersex.
For one, an intersex person may simply be undiagnosed. There are quite a few intersex variations which may not be very apparent externally unless you know what to look for, and many that can’t be confirmed without a karyotype. If you had asked me or my parents if I was intersex before I was 15, we would’ve said no- not because I wasn’t always intersex, but simply because no one knew, my diagnostic process hadn’t even started yet. The other big reason is intersex erasure. What used to be considered the ‘standard of care’ for people with my variation, CAIS, up until very relatively recently, was to just lie to us and tell us that we had ovarian cancer as an excuse to remove our gonads- really internal testes- and then not tell us the truth under the assumption that we’d commit suicide if we found out we ‘weren’t real women’. This is something that the majority of older people with CAIS that I’ve spoken to have gone through, only finding out the truth later. But some of us have likely never discovered the truth, and may still not know they have it, meaning that if they put that they weren’t intersex on a census, this would be unknowingly wrong. This is just one example with one variation, but having people attempt to erase our intersex-ness is pretty common among intersex people of all variations.
This brings me to my final factor to consider: the language used for questions like these and intersex-ness in general. The medical establishment, in order to perpetuate our erasure, is incredibly resistant to the word intersex. Whether it be refusing to accept that conditions accepted by the community as intersex are intersex, or refusing to use the word at all, instead opting to erase us through the term DSD, even people who are told about our conditions may have to discover that we indeed fall under the intersex umbrella on our own. And so while in general I very much don’t like the term DSD and don’t want it to be used anywhere near me, I do think that for the purposes of collecting data, it is a term that should be included in explanations for what intersex means in these demographics questions. I won’t hate it any less, but it’s the unfortunate reality that many people won’t know themselves as intersex except through that term, because of the general erasure of the term intersex and the pushing of DSD language despite it being rejected by the general intersex community. I don’t think it’s right and I don’t think it’s a term that should have to be mentioned, but especially in a population where we have all these barriers to accurate data, we end up having to include these euphemisms because unfortunately there’s been such a successful push of these terms in the medical community that they’re what people know their intersex-ness as.
2 notes
·
View notes
Text
fatness and health
Being fat means that people call me unhealthy even though I’ve been to all possible blood tests and I’ve been described as ”healthy” by all the health professionals I’ve met… And there’s no reason they would believe otherwise besides my weight.
And so what if I will become sick in the future? I probably will: my family already has all sorts of conditions that me, and my skinny siblings alike, will most likely develop in the future. You too, will become sick at some point, regardless of how good you think your health is. You might also get into an accident and die any day.
You see, if fatness was as unhealthy as you think, fatphobia would have started as an actual medical concern, and not as eugenicist propaganda. I’m not saying that fatness and certain conditions have no correlation: we know that they do. However, this doesn’t mean that fatness causes those conditions: researchers and doctors have kind of just assumed that it does, and further research is still ongoing.
We also have research stating that ”obesity paradox” exists. And there is research claiming that slightly overweight people (BMI under 30) live even longer than skinny people.
And whether that or any research is true or not, it doesn’t change the fact that fat people don’t need to change their bodies. Heavy smokers can die even 12-13 years earlier than non-smokers, but heavy smokers still do not owe you smoking cessation. We fat people also don’t owe you weight-loss, just because some research states that people with a BMI higher than 30 die about 4-6 years earlier than people with a ”normal” BMI (BMI is not accurate, but it is also what most weight-related research uses).
(…Even just an every-day (non-heavy) smoker can lose 8 years of their lifetime: if you cared about our health and lives so much, then you’d also go harass skinny cigarette users about their health (I’m not advocating for it, but I recognize that there is a clear difference in how much shit we fat people get for our health vs skinny smokers). And for stuff like vapes, we don’t even know what they do to our bodies in a long term, yet! But I digress.)
Whether you think that we are ”glorifying obesity” or whatever, it doesn’t change the fact that we are human. We are not a type of subhumans you can bully or joke about. If we say we deserve respect, you should realize that that is a basic ass human right, and not a reason to whine about ”glorifying obesity”.
Especially if you are a part of another marginalized group, then it’s about time you educate yourself on fat experiences. I for sure want the queer community to accept my body the way it is.
We just don’t owe you weight-loss, we don’t owe you our health history, we shouldn’t have to listen to any bullshit on how we are a burden on society. The point of society is to take care of the people who need care!!
If you ask me, I believe a massive part of why we fat people die faster isn’t our fatness: it’s medical mistreatment, unemployment, homelessness, and poverty, all of which are more prevelent among fat people.
I know of too many fat people who have died because of medical professionals not taking them or their health seriously: my ”obese” grandpa actually died in surgery in which not all safety protocols were followed. This isn’t necessarily proof of medical mistreatment because of fatness, but he was a 70 year old ”obese” man with type 2 diabetes, BED, and sleep apnea. This make him at least an example of a fat person who died not because of his fatness, or other conditions that are correlated with fatness. My other, skinny, grandpa died 7 years earlier than my fat grandpa with diabetes and sleep apnea.
And I know that some troll will likely reblog this as well: someone even reblogged my book recommendation on a book that debunks parts of fatphobia. You guys are literally broken records that dedicate their entire accounts on reblogging fat people’s content as a way to get back at them… Kinda pathetic and useless: you guys think you can say anything more hurtful about my weight than my own literal mom said to me at 9? You’re most likely grown ass adults: go do something else instead of scrolling tags related to fatness and reblogging every single post with the same talking points.
2 notes
·
View notes
Text
I’m in a very Modeling sort of mood right now, so have a framework for life based on the levels of organization in biology:
Biosphere—The actual world we’re living in, and the knowledge and experiences we have of it that provide a reason to keep living, independent of values and goals—the existence which precedes essence, so to speak.
Ecosystem—The values you hold, the things that matter to you and that you want to support in some capacity.
Community—The system and environment you’re directly a part of, which impacts both the conditions of your day-to-day existence and the means by which you learn to support your values.
Population—Your obligations and responsibilities to the people around you, which emerge as a result of your own personal values and the needs and values of your community.
Organism—A long-term plan for your own life. It doesn’t need to be anything fancy or certain, but it should hopefully give you a starting point for how you could fulfill the different levels of organization. Right now I think my plan is to major in environmental science and try to get involved in restoration work at my school, and see what emerges as a result of that.
Organ systems—The practical goals you set to work towards fulfilling your plan and engaging with your community in a functional, enjoyable, and sustainable way. I’ve been taking a break from school to figure out exactly what these are for me.
Organs—The specific obligations and responsibilities that come about as a result of the goals you set for yourself and the things that people need from you—the work you have to do, the things you need to schedule, the ways you can support the people you care about, including yourself.
Tissues—The short-term means by which you fulfill your obligations—the strategies you use to stay organized, motivated, and happy in the life you’re trying to live.
Cells—The physiological and psychological mechanisms by which these strategies work—which you don’t necessarily have to know, but I’d say the more you can work towards figuring out why and how something works for you, the better equipped you’ll be to apply it appropriately.
Organelles/molecules/atoms—The physical basis for everything that you do and are. Every level of biological organization actualized—your evolutionary history, your genetic makeup, your environmental influences, your individual development, the physiological and molecular mechanisms by which you are able to maintain homeostasis and interface with the world around you. The essence which precedes existence, and which is never going to be truly and completely understood, no matter how thoroughly we work to tease it apart. And for so long I’ve been living in this mindset of wanting to Know Everything and Unify Everything, and thinking about molecular biology always gets me in that emotional space, only now that I don’t feel like I actually Have To Keep Learning About Molecular Biology, it’s honestly just exhausting. I hope it’ll be less exhausting once I’m off my medication, and I can engage with molecular biology and immunology as I want to engage with all of biology—with empathy and curiosity and appreciation, and the occasional research rabbit hole.
#modeling#biology#metaphorical frameworks#homeostasister’s neuroexistential crisis#I think I kinda get what Kierkegaard was on about tbh
2 notes
·
View notes
Text
Pop culture has conditioned us to say "I forgive you" when someone apologizes, but you're not obliged to follow the social ritual, so I didn't.
I’m so glad someone added this!
No one is owed your forgiveness; for absolution from their actions they still performed and continued at an age they knew it was wrong and after being told it was wrong.
No one is owed absolution for taking away your childhood! For making you live in fear, and see what should be a safe place and one of learning (preferably also fun) as a DANGER. They don’t deserve to have that weight lifted off their shoulders—if they even felt a weight to begin with.
If one of mine came to me, I’d tell them I was impressed they were able to get over themselves enough to even come close to unpacking what the fuck their issues were back then and why they took it out on another child. I’d probably ask them what the bug was that they’d had up their ass for years on end because my largest vice is needing to know.
If they had a child(ren), I’d tell them that I hope better than either of us had for their kid(s) and for them to be a decent parent, but that no matter how good of a parent they are or person they’ve become, nothing would undo or override what they did to me. The years of fear, the buckets of tears and the insane levels of stress. The literal ptsd. (Literally, somehow, getting adults to join them!) All of which will impact me for the rest of my life.
But is it really being healed to demand catharsis and then revert when you’re told you don’t deserve it?
But my views on forgiveness are different than a lot of peoples’, and a lot of that is because of what I went through. There’s no right or wrong way to view “forgive and forget” in whatever light is best for you. Hence, I’ve added another view to this post.
Part of me wishes they would. I’m a believer is retributive karma: experiencing what you gave out. I want them to understand in the realest posisble terms what they put me through. But I also know the closest way is by proxy, and that my child self will never have catharsis. Her window for going to school without fear of a prosecutor is long past; even high school having been tainted. Her and all those other children she knew. We won’t get what we deserve.
Now I’m crying and forgot where exactly I wanted to go with this. I think just to show the severity of “child antics.” Those were formative years. Those were years designed to impact the rest of our lives. No matter what development and realizations or “healing” those bullies go through, it will never, ever excuse their behavior, nor will being better for their kids or nieces unwrite the deeply ingrained trauma patterns in our brains. Again, trying to “redeem” themselves by being better parental figures is good, but it’s not magic.
So I won’t be saying “I take the responsibility of your own actions off you.” But I will say “I curse you to hold more of the responsibility of what you chose to do to me, and you being a better adult (or parent figure) is the LEAST you owe everyone.”
Y’all can disagree with me, but I won’t be arguing with you. And yes, I’m healing. I’m in therapy. Still, that doesn’t mean I’m obliged to them, especially not to say “it’s okay you hurt me so deeply and so long because I’m in medical debt over therapy and spent years trying to overcome my own trauma.”
Life really does align in weird ways.
My bully from 5th grade who snapped my glasses in front of his friends just found me on social media a few weeks ago.
He wrote me a long apology saying how he was now a father to a 3 year old little girl and was taking her to get her first pair of little glasses in the next few days—and it brought back what he did. He said couldn’t ever handle the idea of someone doing that to her.
My first instinct was to tell him to get lost, but I realized I was getting what I always prayed for. I just wanted the people who were mean to me to eventually understand it—even if it took a personal experience to relate to and 14 years to open their eyes.
A piece of me healed in that moment as I gave him glasses advice for his daughter because I was the same age when I got my first pair.
Kids are really ruthless, but it takes a healed adult to reach out to apologize. And there is always time to change; it’s never too late.
49K notes
·
View notes
Text
Resolving Things
This time of year is as good as any at resolving things, and it's just not me who thinks this way. Four thousand years ago the Babylonians, while celebrating their festival of Akitu, thought it might be a good idea to make resolutions to their gods. Their reasoning being, if they could keep their resolute promises throughout the year, the gods in turn then would treat them favorably.
So, New Year's resolutions started out having little to do with one’s own personal improvement, but more of a bargain; if I do this, then you’ll grant me that.
I wonder how much luck played into the Babylonian’s success at being granted the favor they craved? Today, one might resolve to earn or win a million dollars this year and, by using the Babylonian method, you could make a New Year’s resolution to buy a lottery ticket each day as your promise of being diligent. However, I’m not convinced that the “statistical gods” are going to reward you for keeping your promise. While I don’t like your odds, conversely, you have to be in to win. Therefore, I’m resolving things. I haven’t done this in a long time; been too busy. My take is this: you’re better off at least having a road map of where you want to go, right?
I’m not sure, though, that 2025 is simply a matter of where I want to go. Must admit, I’ve never felt discernment like this before. I’ve not been known necessarily as a look-before-you-leap kind of guy, but 2025 just feels different. It’s not a feeling of fear, but more of caution and extreme uncertainty. I normally charge into a new year, but I feel like I’m tiptoeing into 2025. As an example, think how one feels when entering a supposedly vacant house. You quietly make your way down the hall, checking each room in hope of verifying that nothing or nobody is there to alarm you, however, acknowledging your concern for what’s around the next corner.
So, I can map out my new year in any way that I want, but something tells me I better use chalk. Here’s my list:
My extended family are expecting new additions in 2025, a girl and a boy. No added pressure, but he will be the family’s first grandson. My role is to be the supportive “Poppa”, and I can get better at this. However, being made over with eye glitter is where my wife, “Mimi” excels and I have no desire to compete with her in this respect.
Here I’m repeating a mantra I posted earlier from an Akron, Ohio lady, “time will always be your most valuable asset.” I want to get better in 2025 at calibrating my usage of time so that I’m never too busy for family and friends and this especially includes caring to my mother in her continued rehabilitation.
It’s a delicate balance actually, reserving time for yourself as well as for others. That’s why I’m resolving to take more time to smell the roses, just not spray, prune and fertilize them this year. Besides, I have a glasshouse that needs erecting so that I can nurture seedlings into plants for our garden. This should reduce the number of trips to Lowes!
Similarly, I resolve to avoid the upcoming Trump tariff tax wherever I can. I’m already seeing the price of things increase by 30% and 40% in advance of the 2025 tax hike. My plan is to simply make my own or do without, and this could be a difficult promise to uphold. It might mean going without my beloved homemade guacamole for quite some time.
I’m also resolving to turn off the news channels. Yes, I’m volunteering to personally disconnect from all of the chaos that’s about to descend upon Washington D.C. Let those within the inner belt duke it out, just don’t mess with my family being able to sit around our fire pit undisturbed. And yes, I’m admitting that I’m removing myself from the reality of it all.
No, I don’t feel a need to apologize to the world for what is about to happen. Others understand and are already pitying us here in the U.S.
Here’s a recent development: to continue my active surveillance of my medical condition and utilize the opinions of the professionals, and my own common sense, to begin medical intervention when it is necessary.
I’m resolving to continue to seek solace in my seven thousand Spotify songs so that I can fall back to sleep at 2 am.
Ok, I’ve left the most challenging resolution until now. I resolve to send to my publisher the manuscript of my sequel by years’ end. I might need someone like my niece again, to hold me to this pledge.
And finally, here’s one to either make you smile or grimace. I resolve to continue posting my musings and random thoughts in this monthly blog, and as always, welcome your input.
These aren’t the 10 Commandments nor the 10 Suggestions, but more akin to the yardstick that gets taped to the kitchen wall to see how you measure up at the end of the year.
Wishing health, prosperity and glad tidings to all this year.
0 notes
Text
youtube
Living with bipolar schizoaffective disorder is a complex and often challenging experience. It's a condition that combines symptoms of both bipolar disorder and schizophrenia, which can create a unique and difficult journey. Understanding what it feels like to live with this condition requires a deep dive into its emotional, psychological, and social aspects.
The Daily Reality
Each day can be unpredictable. Some moments, I feel elated, bursting with creativity and energy, while others plunge me into deep despair. These mood swings can be intense and significantly affect my daily life. During a manic phase, I might stay up all night, fueled by ideas and plans, feeling invincible and capable of anything. However, this high is often followed by a crash into depression, where even getting out of bed feels like an insurmountable task.
In addition to mood fluctuations, the schizoaffective aspect brings its own set of challenges. I might experience hallucinations or delusions that distort my perception of reality. For example, I may hear voices that aren't there or feel as though I'm being watched. These experiences can be terrifying and isolating, making it hard to connect with others or feel safe in my surroundings.
Coping Mechanisms
To navigate the complexities of living with bipolar schizoaffective disorder, I've developed various coping strategies. Therapy plays a crucial role in my management plan. Having a therapist to talk to helps me process my feelings and experiences, and provides me with tools to handle my symptoms. Cognitive Behavioral Therapy (CBT) has been particularly effective for me, as it helps challenge and reframe negative thoughts.
Medication is another cornerstone of my treatment. Finding the right combination of medications has been a journey in itself. Some days, I feel like a lab rat, trying different pills and dosages, but when I find something that works, it can make a significant difference. It's important to recognize that medication is not a cure, but rather a way to manage symptoms and provide stability.
Social Interactions and Relationships
Building and maintaining relationships can be difficult. Friends and family often don’t fully understand what I’m experiencing. I’ve had to learn how to communicate my needs and symptoms effectively. There are times when I withdraw from social situations, fearing that my mood swings or hallucinations will alienate those I care about. This isolation can lead to loneliness, reinforcing the cycle of depression.
However, I have also found incredible support from others who understand what it’s like to live with a mental health condition. Joining support groups, both in-person and online, has helped me connect with people who share similar struggles. These connections remind me that I am not alone in my journey.
The Importance of Advocacy
Understanding and raising awareness about bipolar schizoaffective disorder is important for both those who live with it and the general public. Stigma can create barriers to treatment and understanding. By sharing my story, I hope to shed light on the realities of this condition, encouraging empathy and support from others.
Conclusion
Living with bipolar schizoaffective disorder is not just about managing symptoms; it's about navigating a complex emotional landscape. It's a journey filled with ups and downs, requiring strength, resilience, and understanding. By sharing my experiences, I hope to foster a greater understanding of this condition, helping others to see the person behind the diagnosis.
Ultimately, while this journey can be daunting, it is also filled with moments of hope and connection. I strive to take each day as it comes, celebrating the small victories and learning from the challenges. Understanding my condition is a continuous process, and I welcome the journey ahead.
#Youtube#schizophrenia#schizophrenic disorder#bipolar schizoaffective#actually schizophrenic#schizoaffective#schizoposting#schizophrenic spectrum#paranoid schizophrenic#bipolar disorder#true story#personal story#true life#real story#this is my life#spread awareness#schizophrenia awareness#schizophrenia advocate#mental health#mental health advocate#mental health awareness#difficult disability#disability advocacy#invisible illness#invisible disability#invisible disease#not all disabilities are visible#understanding#bipolar schizophrenic#bipolar schizophrenia
1 note
·
View note
Text

Page 305 of Harriet Jacobs's Incidents in the Life of a Slave Girl, published in 1861. Edited by L. Maria Child for its author, Jacobs, who uses the pseudonym Linda Brent.
This is an ongoing blog. The James Norcom Family Papers are extensive, including over 900 documents, and I've barely scratched the surface. There are several documents from 1847, for instance, about Norcom's politics that I have yet to delve into. Naturally, continuing to look through these is, of course, the first next...
...step. As the development of my project from last semester to this one has shown, there are always new things to find and new clarifications to be made.
This semester, I’ve become particularly intrigued by Norcom’s connections with prominent Penn faculty members—beyond Rush and Wistar, for whom he named his sons—such as Frederick Beasley, Benjamin Smith Barton, and James Woodhouse. I would love to explore this in more depth. Additionally, the materials Norcom instructed his son to retrieve from Philadelphia may offer valuable insights into his medical ideology. Either of these would be worthy of a full-semester project.
I have also found intriguing Norcom's connections to those close to Jacobs. For instance, he was the business partner of M.E. Sawyer, the father of Samuel Tredwell Sawyer, who fathered Jacobs’ children. Additionally, Norcom served as an officer in the Society Auxiliary to the ACS alongside James Iredell Jr., the brother-in-law of James Iredell Tredwell, with whom Jacobs’ daughter stayed in New York. Norcom's pursuit of and vendetta against Jacobs may have been more personal than previously realized, and I would love to further explore these "it's-a-small-world" connections.
Norcom’s role as an advisor—and later, son-in-law—of Elizabeth Horniblow and her family is ripe with potential for exploration. Specifically, it suggests how he may have leveraged his medical degree to access enslaved individuals, acting as both executor and beneficiary of several Horniblow family wills. Reconstructing what Norcom received from this family would give insight into how and why he was able to access Jacobs and others he would later enslave.

Letter dated December 2, 1809, addressed to “Mrs. Horniblow.” Letter 14 of the James Norcom Family Papers. This letter is briefly discussed here, with further explanation of Norcom's relationship with the Horniblows provided here.
And those are just some of the many ways this semester has opened up new avenues for exploration.
To reiterate from last semester, although Rush and Wistar have been studied extensively, I believe their lecture materials, manuscripts, notes, and other documents—particularly those from 1795 to 1800, when Norcom was a student—warrant deeper exploration to reconstruct Norcom’s time at Penn. I would say the same about the materials of Barton and Woodhouse, who were professors at the time Norcom attended. While this project has focused on material from after Norcom graduated, it would be immensely valuable to re-create the conditions of his time at Penn Medical School. This would help determine the influence Penn had on Norcom’s life, especially through his education under Rush, with whom he remained close throughout his life.
Additionally, Norcom’s sons, John, Benjamin R., Caspar W., William A.B., and Henderson S., attended the University of Pennsylvania after their father. How the curriculum at Penn Medical School influenced Norcom’s sons, Benjamin R., Caspar W., and Henderson S., who also attended and graduated from the program, and how the University of Pennsylvania shaped the intellect and politics of his son John, who graduated from the collegiate department, at the time they each attended is a fruitful question for further research. As a student with limited time, I haven’t been able to fully explore the intergenerational legacy of the Norcom family at Penn. However, this long-standing connection to the University offers a fascinating opportunity to study how Penn influenced the Norcom family across generations, both academically and ideologically.
In the future, I would like to write a more in-depth comparison of Norcom’s self-portrayal—through his correspondence, actions, medical writings, and other records—with his depiction in Harriet Jacobs’s autobiography, drawing on specific passages from her work. Additionally, I hope to investigate any evidence of how the Norcom family may have reacted to Incidents in the Life of a Slave Girl upon its release, or how they grappled with that legacy after historian Jean Fagan Yellin revealed Jacobs to be its author.
I am also interested in further exploring the connections between Penn, Freemasonry, and slavery, as well as the relationship between Penn, Whig politics, and slavery—topics I have only begun to examine in my paper and on this blog.
All-in-all, the work on this project has only just begun. For now, I would like to extend my gratitude to anyone who has made it this far and take a moment to acknowledge the following for their invaluable help this semester and last:
Kathleen Brown
Scott Wilds
John Pollack of Kislak Center for Special Collections
Jim Duffin of the University Archives
Paul Wolff Mitchell
Historical Society of Pennsylvania
Library Company of Philadelphia
State Archives of North Carolina
James Pensabene
Ann Farnsworth-Alvear
Finally, I would like to provide, in a more traditional format, the sources I have used throughout this project here.
#Harriet Jacobs#Incidents in the Life of a Slave Girl#Dr. Flint#James Norcom#Benjamin Rush#Caspar Wistar#Frederick Beasley#Benjamin Smith Barton#James Woodhouse#Elizabeth Horniblow
0 notes
Text
Understanding Diabetes: What You Need to Know
Diabetes is a chronic condition that affects how your body processes glucose (sugar). There are three main types of diabetes:
Type 1 Diabetes: This occurs when the immune system attacks the insulin-producing cells in the pancreas. It typically develops in childhood or adolescence.
Type 2 Diabetes: In this type, your body either becomes resistant to insulin or doesn't produce enough. It is often related to lifestyle factors and usually occurs in adults.
Gestational Diabetes: This develops during pregnancy but usually goes away after childbirth. However, it increases the risk of developing Type 2 diabetes later in life.
Recognizing symptoms early, such as frequent urination, excessive thirst, blurred vision, and unexplained weight loss, is key to getting proper treatment. If you experience any of these symptoms, consult a healthcare provider.
Diabetes-Friendly Meals: What to Eat
Managing diabetes through diet is essential for controlling blood sugar levels. Here are some tips for making your meals diabetes-friendly:
Choose whole grains: Brown rice, quinoa, and whole-wheat pasta are better options than refined carbs.
Focus on lean proteins: Chicken, turkey, and plant-based proteins like tofu and legumes are excellent choices.
Fill your plate with vegetables: Non-starchy vegetables like spinach, kale, broccoli, and cucumbers are packed with nutrients and fiber.
Incorporate healthy fats: Avocados, nuts, seeds, and olive oil can help keep you full and are great for heart health.
By carefully planning your meals, you can maintain better control of your blood sugar. It’s always best to consult a dietitian to personalize your eating plan.
How Exercise Helps Manage Diabetes
Regular physical activity plays a major role in managing diabetes. Exercise helps improve insulin sensitivity, which means your body can use insulin more effectively. Here's how it benefits those with diabetes:
Regulates blood sugar: Exercise helps muscles use glucose for energy, lowering blood sugar levels.
Supports heart health: Diabetes increases the risk of cardiovascular diseases, and exercise can reduce this risk.
Improves mood: Physical activity can reduce stress and help manage diabetes-related emotional struggles.
Try to aim for at least 30 minutes of moderate activity most days of the week. Walking, cycling, swimming, or even yoga can be great ways to keep moving!
My Journey with Type 2 Diabetes
Living with Type 2 diabetes can be challenging, but it’s also a journey of learning and adaptation. When I was first diagnosed, I felt overwhelmed and unsure of what the future would hold. But over time, I’ve learned to take control of my health. With the right combination of diet, exercise, and medication, I’ve been able to manage my blood sugar levels.
There are days when it feels tough, but I remind myself that small steps lead to big changes. And the support of my community—whether friends, family, or online groups—has been crucial in my journey. If you’re newly diagnosed or struggling, remember: you’re not alone. Progress is key, not perfection.
How to Manage Diabetes Burnout
Managing diabetes can sometimes feel like a full-time job. The constant checking of blood sugar, insulin doses, and meal planning can lead to “diabetes burnout.” Here’s how you can handle it:
Take breaks: It’s important to rest and not let the demands of managing diabetes overwhelm you. Mental health matters.
Connect with others: Whether it’s a support group or a close friend, talking to others going through the same thing can help you feel less isolated.
Simplify your routine: Consider planning your meals for the week or setting reminders to check your blood sugar at specific times.
Remember, it’s okay to have challenging days. Taking care of your mental and emotional health is just as important as managing your diabetes.
Busting Common Diabetes Myths
There are many misconceptions about diabetes, and it's essential to clear them up. Here are some common myths debunked:
Myth: Only older people get diabetes.
Fact: Type 2 diabetes can develop at any age, especially with risk factors like obesity and inactivity. Type 1 is typically diagnosed in children or young adults.
Myth: People with diabetes can’t eat sugar.
Fact: People with diabetes can eat sugar in moderation. The focus should be on balanced meals and portion control.
Myth: Insulin is a cure for diabetes.
Fact: Insulin is a tool to help manage blood sugar, but it doesn’t cure diabetes. It’s just part of the treatment plan for many.
Understanding the truth behind diabetes is key to managing it effectively. Don’t let myths stop you from seeking the right care and information.
Diabetes and Mental Health: Why It Matters
Living with diabetes can take a toll on your mental health. The constant management of blood sugar levels, medication, and potential complications can lead to stress, anxiety, and depression. Here’s why mental health should be a priority:
Stress affects blood sugar: Chronic stress can make it harder to control blood sugar levels, leading to more fluctuations.
Diabetes-related anxiety: The fear of complications or dealing with daily management can cause emotional strain.
Depression and motivation: Feeling down can affect your ability to take care of yourself, making it harder to manage your condition.
If you feel overwhelmed, talk to a professional who can help. There are also support groups for people living with diabetes, where you can connect with others who understand.
0 notes
Text
Understanding the Role of Occupational Therapy in Mental Health Recovery
When we talk about mental health recovery, most people immediately think of therapy or medication, and I have to admit, I was one of those people. I had to sit down and ask myself the other day when I was preparing to go on my psych block for the first time since last year that what is going to be my role exactly here? Well, now I know the answer but I didn’t know before, OT focuses on helping people find meaning in their daily activities, which can play a huge role in their mental health. Research shows that engaging in these meaningful activities can improve mental health by adding structure, purpose, and better ways to handle stress (Crisp, 2022).
As an OT student, I’ve often wondered how our work fits into mental health, especially with clients who don’t have obvious physical problems. This was exactly my experience a few days ago when I was preparing my write-up and trying to decide on an activity for my client. I found myself thinking, “What activity should I choose?” My previous physical block seemed more straightforward—patients had clear physical limitations, so it was easy to identify activities to do with a patient like bathing or dressing. But now, faced with a client who has bipolar disorder and substance use disorder, I was confused. This person could bathe and dress themselves—so what was my role here as an OT?
My confusion made me question the unique role of OT in mental health settings. What do we offer that psychologists, social workers, or psychiatrists don’t? As a third-year student, this felt like a question I should already know the answer to, especially since I’d had a psychosocial block before and I also know that OT is just way more than bathing or dressing. According to Homewood Health Centre (2024), OTs help individuals with mental health challenges engage in meaningful activities and improve their overall well-being. This made sense to me—but what if the patient already knows how to do those activities? They have no physical limitations, so for example with my patient, how does bipolar disorder affect their ability to function?
It was only after I thought deep and read through my observations and deductions that I wrote down before when I saw the light. As I thought more about it, I remembered that OT isn’t just about physical ability. For example, someone with bipolar disorder—especially during a manic phase—might struggle with attention, concentration, and task completion (Stan Clark, 2021). These challenges can make it difficult for them to perform activities like cooking, grooming, or leisure tasks that require sustained focus. This realization was a breakthrough for me. Even though my client might not have physical impairments, their mental health condition impacts their ability to complete activities that require cognitive skills, attention, and emotional regulation.
We always hear the word holistic in class and that’s what OT is- HOLISTIC, that’s what’s makes us unique. We look at the whole person—not just their physical abilities, but also their cognitive, emotional, and social needs. In the case of my client with bipolar disorder, I could focus on helping them improve their task completion skills through structured activities. These activities could also be used to teach mindfulness, develop effective coping mechanisms, and set healthy boundaries—areas where OTs can make a big difference (Courtney Gardener, 2024). It’s different from the work of psychologists or psychiatrists because we focus on practical, everyday tasks that help clients integrate therapeutic strategies into their daily lives.
Reflecting on this experience, I realized how i was so stuck in the mindset of my previous block. I was so focused on physical limitations that I wasn’t thinking “outside the box” as an OT should. This experience taught me that being an OT, especially in mental health, requires flexibility, creativity, and a holistic view of the person. It’s not just about what the client can or can’t do physically; it’s about how their mental health impacts their overall functioning and quality of life. It’s about helping people find meaning in their everyday lives, even when they seem capable on the surface
So, why are OTs in mental health? Because we bring a unique, holistic perspective that considers the person’s ability to engage in meaningful activities, their cognitive and emotional challenges, and their environment (HPCSA, 2022). We help clients navigate the complexities of their mental health conditions in a way that’s practical and grounded in everyday life. That’s what makes our role so essential—and it’s why I’m proud to be on this journey, even when it feels overwhelming.
In future practice, I will be definitely considering the fact that every client, regardless of their condition, has the potential to engage in activities that enhance their well-being. Our job as occupational therapists is to guide them toward those opportunities, empowering them to lead fulfilling lives.
REFERENCES
hw_admin. (2023, November 9). The Role of Occupational Therapy in Mental Health Treatment. Homewood Health Centre. https://homewoodhealthcentre.com/articles/the-role-of-occupational-therapy-in-mental-health-treatment/
Does Bipolar Disorder Affect Someone’s Ability to Learn? - International Bipolar Foundation. (2021, April 14). Ibpf.org. https://ibpf.org/articles/does-bipolar-disorder-affect-someones-ability-to-learn/#:~:text=Driven%20to%20Distraction%20by%20Mood
HPCSA. (2022, November 10). The occupational therapist’s role in promoting mental health -. Hpcsa-Blogs.co.za. https://www.hpcsa-blogs.co.za/the-occupational-therapists-role-in-promoting-mental-health/#:~:text=Occupational%20therapists%20use%20standardised%20assessments
Occupational Therapists and Mental Health Interventions - Moving With Hope. (n.d.). https://www.movingwithhope.org/posts/occupational-therapists-and-mental-health-interventions/#:~:text=Occupational%20therapists%20use%20activities%20of
0 notes
Text
**From a Bipolar Mind: What It’s Like to Not Be Able to Do Anything But Sleep**
Living with bipolar disorder can be an emotional rollercoaster, characterized by extreme highs and devastating lows. One of the most challenging aspects for me is the periods of debilitating fatigue where it feels like the only thing I can do is sleep. It’s not just feeling tired; it’s an overwhelming sense of exhaustion that seeps into every part of my being, making even the simplest tasks feel insurmountable.
### The Overwhelming Fatigue
When I’m in a depressive phase, my energy levels plummet to the point where getting out of bed feels impossible. This isn't your average tiredness after a long day; it’s a bone-deep exhaustion that blankets my entire existence. The mental fog is so thick that concentrating on anything feels futile. My body feels heavy, and my mind is clouded with a sense of hopelessness. Sleeping becomes a refuge, a way to escape the relentless grip of depression.
### The Guilt and Shame
As I succumb to the need to sleep, guilt and shame often follow. Society values productivity, and there’s immense pressure to be constantly active and engaged. When I’m unable to meet these expectations, I feel like I’m failing. The guilt is compounded by the awareness that others might perceive my need for rest as laziness. But the truth is, bipolar disorder is a medical condition, and these episodes of extreme fatigue are a symptom, not a choice.
### The Isolation
During these times, isolation becomes a significant issue. The world keeps moving while I’m stuck in a cycle of sleep and inactivity. It’s hard to reach out to friends or family when I’m in this state, partly because I don’t have the energy, and partly because I fear judgment. This isolation only deepens the depression, creating a vicious cycle that’s hard to break.
### Self-Care and Understanding
Managing bipolar disorder is a constant balancing act, and self-care becomes crucial during these episodes. I’ve learned to be kinder to myself and to recognize that rest is a legitimate need. This means creating a supportive environment where I can sleep without feeling guilty and where I can slowly regain my energy. Understanding and compassion from loved ones also make a significant difference. Knowing that I have a support system that acknowledges my struggle helps alleviate some of the emotional burden.
### Seeking Help
If there’s one piece of advice I can give to others in a similar situation, it’s to seek professional help. Therapy and medication can play vital roles in managing bipolar disorder. Talking to a therapist provides a safe space to express feelings and develop coping strategies. Medication can help stabilize mood swings and reduce the severity of depressive episodes, making it easier to manage daily life.
### Conclusion
Living with bipolar disorder means navigating a complex landscape of emotions and experiences. The periods of extreme fatigue and the need to sleep are just one aspect of this condition. It’s essential to recognize these symptoms for what they are—a part of the illness—and not a reflection of personal failure. With the right support and self-care, it’s possible to manage these episodes and find a way back to a more balanced and fulfilling life.
#encouragement#self care#self help#motivation#self improvement#humor#bipolar 2#bipolar#actually mentally ill
0 notes
Text
Hello everyone, Lucas here. I’m a 26 year old learning to live with multiple mental health diagnoses including; BPD, CPTSD and MDD with psychotic tendencies. This journal is my attempt at externalizing my feelings about my journey of healing and hoping that it might help some people who don’t have a voice about their own problems to know they aren’t alone.
My Discovery:
You know that inner voice? The one that’s like a personal GPS, guiding you through life’s decisions, like reminding you to look both ways before crossing or nudging you towards that lemon ice tea you can’t get enough of. It’s a mix of a coach and a critic, especially when you’re beating yourself up over a mistake. But here’s the kicker: I recently discovered that what I thought was just me… isn’t just me. I’ve been hosting an uninvited guest in my head, let’s call him “Jeremy.” This guy, Jeremy, isn’t the cheerleading type. He’s been with me since I was a kid, whispering sweet nothings of the not-so-sweet variety, convincing me I’m less than, leading me down paths best left untrodden.
This revelation hit me like a freight train during a group therapy session focused on the not-so-gentle art of self-talk. We were peeling back the layers of self-criticism when suddenly, my internal dialogue split right down the middle. For the first time, I could hear “Jeremy” as someone separate from me. The realization that I wasn’t alone in my head was terrifying. I mean, hearing voices is one thing I never wanted to check off my list, and here I was, thinking I had just unlocked a new level of “not okay.”
The aftermath of this discovery had me floored — literally. I was a mess, tears and tremors, caught in the grip of fear. It felt like my mind had turned against me. But, salvation came in the form of my psychiatrist’s timely intervention. He explained that “Jeremy’s” presence wasn’t as outlandish as it felt. For someone juggling BPD, CPTSD, and MDD, hearing a voice like Jeremy could be part of the complex tapestry of my mental health. It seems my brain’s eclectic mix of conditions created the perfect stage for Jeremy to perform his unsettling monologues.
A New Chapter:
Switching meds isn’t always smooth sailing, but in my case, the timing couldn’t have been better. I was already in the process of tapering off my old antidepressants when “Jeremy” decided to crash the party. Given the new developments with my diagnoses, my psychiatrist thought it was time to introduce anti-psychotics into the mix. It’s been 2.5 days since I started the new medication, and the difference is night and day. My mood has lifted in a way I hadn’t dared to hope for. “Jeremy” has been unusually quiet, and there’s a newfound sense of joy threading through my days.
While I’m savoring this peaceful phase, I’m conscious that the immediate uplift might be due to the novelty of the new medication. There’s a chance its effects could diminish over time. That’s where my therapy plays a crucial role. Thankfully, my diagnoses respond well to Dialectical Behavior Therapy (DBT), which equips me with skills to maintain this level of mental peace alongside the medication. I won’t lie — it feels daunting. The path to managing my mental health seems like a steep climb, and part of me questions if the effort is worth the reward. However, the thought of the people who care for me, who support me unconditionally, reignites my will to push forward. I owe it to them, and to myself, not to give up.
#ptsd#post traumatic stress disorder#cptsd#complex post traumatic stress disorder#complex ptsd#trauma#actually ptsd#actually cptsd#mental illness#mental health#mental health awareness#ptsd awareness#cptsd awareness#neurodivergent#ptsd thoughts#awareness#important#mentally ill#actually mentally ill#psychology#bpd#borderline personality disorder#self h@rm
1 note
·
View note