#autoimmine disease
Explore tagged Tumblr posts
Text
how does one get tested for celiac disease?
i have a multitude of autoimmune diseases already, it wouldn’t surprise me if i had something. (whether it be celiac disease, or something else tummy related.)
For your future information, here are medical innovations younger than both the basics of HRT for trans ppl & the first gender-reassignment/gender-confirmation surgery. I put together this incomplete list earlier today bc I was bored:
all organ transplants
most modern vaccines, including the polio vaccine
the gluten-free diet as a treatment for celiac disease
synthetic insulin
oral contraceptives
MRIs
the concept of a "blood bank"
pacemakers
hydrocortisone
ibuprofen
diazepam
artificial hearts
sumatriptan
naproxen (Aleve)
tramodol
dialysis
ECT
ondansetron (Zofran)
chemotherapy
IVF
CPR
CT scans
transdermal patches
liposuction
intravascular stents
penicillin
In case you run into someone talking about how 'experimental' HRT is.
#idk if i have celiac disease#but gods i know how this feels#never been tested but wouldnt surprise me#chronic illness#autoimmune#autoimmine disease
5K notes
·
View notes
Text
Some people don’t want to hear this but sometimes accessibility is not sustainable or eco-friendly. Disabled people sometimes need straws, or pre-made meals in plastic containers, or single-use items. Just because you can work with your foods in their least processed and packaged form doesn’t mean everyone else can.
#chronic fatigue#chronic illness#chronic pain#chronically ill#disability#disabled#fibromyalgia#lupus#autoimmine disease#pots#pots syndrome#invisible illness#invisible disability#accessibility#cripple punk
39K notes
·
View notes
Text
I don't think my body realizes how healthy my labs say I am
#chronic life#chronic disease#chronic illness#autoimmune#chronicillness#chronicillnesshumor#spoonie#spoonie humor#autoimmine disease
7K notes
·
View notes
Text

This is a threat
#disability pride#disability#autoimmine disease#chronic pain#chronic illness#chronically ill#mobility aid#queer#sapphic#achillean#bisexual#asexual#lesbian#gay#homosexual#pride month#lgbt#aromantic#nonbinary#transgender#transfem#transmasc#mental disability#pansexual#actually neurodivergent#neurodivergent#neurological disability#neurodiversity#actually neurodiverse#my art
21K notes
·
View notes
Text
Why is it always up to disabled people to look after other disabled people. Why do able-bodied people feel no obligation to assist? Why do they throw the additional responsibility on disabled individuals. Why is their whole system built on isolating groups??
#spoonie#chronic illness#chronic fatigue#chronic pain#disabled#actually disabled#disabled community#spoonie life#spoonie problems#autoimmine disease
2K notes
·
View notes
Text
When you have a chronic ailment, you hear all the time “I could never.”
Oh, you cut out dairy/gluten/ect? I could never. Oh, you do self injections? I could never.
I could never deal with that much pain. I couldn’t live with all those doctor appointments. I could never stay in bed all day, I’d just get so bored! I couldn’t do it, I couldn’t live like that, can’t couldn’t wouldn’t…
Please stop implying to people with something chronic that you’d rather die than go through what they’re going through, and take a minute to understand that their treatment isn’t a hobby. It’s survival.
Yes, people with chronic ailments ARE incredibly strong. They ARE doing things you think you couldn’t ever do.
But they’re the same things that they likely thought they couldn’t ever do until they had no other option.
Yes. Often, someone with a chronic issue sees a notable decline in their quality of life.
That doesn’t make it less worth living.
You could do it if you had to.
“I could never” is not the empathetic response you think it is.
#disabled#disability#chronic illness#chronic pain#arthritis#autoimmine disease#rheumatoid arthritis#pots#chronic migraine#advocacy
3K notes
·
View notes
Text
When a disabled person says that they can’t do something, we don’t mean that we just don’t want to. We also don’t mean maybe. We mean that we physically cannot do it or that we could, but it could really harm us. We have to pay consequences. You don’t.
#chronically ill#chronic illness#epilepsy#mecfs#myalgic encephalomyelitis#pots#pots syndrome#postural orthostatic tachycardia syndrome#dysautonomia#autoimmine disease#hashimotos#disabled#disability
1K notes
·
View notes
Text
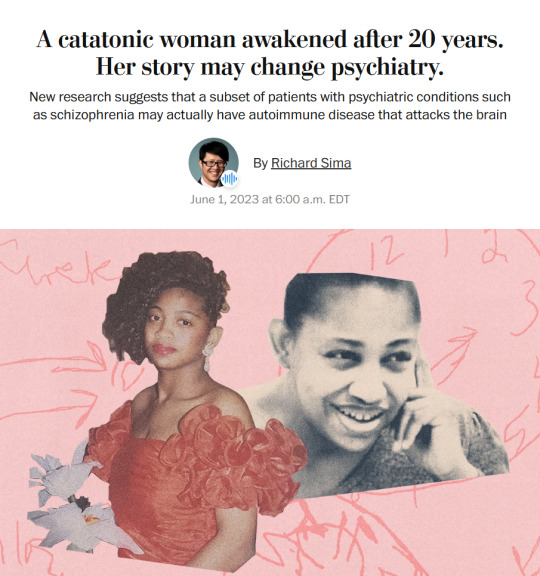
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
7K notes
·
View notes
Text
Chronically ill people will literally be like bro can you break my forearm real quick. Can you bash my head in the doorway a few times. Can you dislocate my kneecap. Ohhh my god thanks dude that's so much better. Yeah just a really bad flare today.
#chronically ill#chronic pain#chronic illness#pots syndrome#autoimmine disease#dysautonomia#relatable
1K notes
·
View notes
Text
The 5-year Anniversary of the most egregious Crimes Against Humanity…
“We have people walking around with no immune system…no ability to make an immune system…they were injected with 81 strands of foreign bacteria…and 8 strands of foreign HIV" 🤔
#pay attention#educate yourselves#educate yourself#reeducate yourselves#knowledge is power#reeducate yourself#think about it#think for yourselves#think for yourself#do your homework#do some research#do your research#do your own research#ask yourself questions#question everything#truth be told#evil lives here#lies exposed#government secrets#government lies#government corruption#medical corruption#crimes against humanity#save humanity#save the children#autoimmine disease#hidden history#hidden secrets#history lesson#history
353 notes
·
View notes
Text



#chronic illness#chronic pain#disability#autoimmine disease#comic#lupus#it’s funny to draw with your finger
336 notes
·
View notes
Text
Say it with me! Wheelchairs aren’t sad! Mobility aids aren’t sad! Mobility aids are instruments of freedom!
#chronically ill#chronic illness#chronic pain#disability#disabled#chronic fatigue#autoimmine disease#mobility aid#cripple punk
36K notes
·
View notes
Text
Sometimes u just need to sob and scream and cry and bitch about ur disability
I think a lot of people feel like they need to be at completely at peace with their disability
And you don’t!
Be mad be sad be pissed off!
#disabled#disabled problems#disability#ehlers danlos syndrome#immunocompromised#rheumarthritis#chronic illness#autoimmine disease#angry cripple#this post is about physically disabled people#autoimmune#rheumatoid arthritis#cripple punk
4K notes
·
View notes
Text
Just a reminder:
If a mobility aid helps you live life, then use one. Seriously, i mean it. If that cane or walker or whatever helps you live more and manage your symptoms and flare-ups, then do it.
You are not too young
You are not "not sick enough"
You are not faking
You are valid, and your disability is real whether or not it's visible or diagnosed
Mobility aids are for anyone and if you think you need one then you probably do babe✨️
#pots syndrome#potsie#pots#fibromyalgia#chronically ill#chronic illness#chronic pain#chronic fatigue#chronic fаtiguе ѕуndrоmе#autoimmune#autoimmine disease
213 notes
·
View notes
Text
One thing able-bodied people don’t get is that sometimes your condition is in its best possible state. My chronic illnesses are incurable. They are progressive and that’s it. With that will come symptoms no matter what. And im very lucky with mine considering the progression of my condition. Frankly I think my mental health has been far harder than my physical.
There is this idea that fighting a doctor or racing through treatment after treatment may fix something. And sometimes it can. But sometimes the body and state one is in is the best it can be. No doctor is going to be able to change it.
A condition has symptoms. Very rarely does it not. And if the condition cannot disappear then neither can all of the symptoms. Improvement is possible - perfection is not. And for me right now; my body is as good as she’s going to be. And I need people around me to accept that so I can live my life free from their judgment and their shame.
It’s a hard fact to explain. And it’s a hard one to accept. But it’s the reality. 🌸
#chronic illness#spoonie#chronic fatigue#chronic pain#disabled#actually disabled#disabled community#autoimmine disease#spoonie life#spoonie problems
496 notes
·
View notes