#Medical Disorders
Explore tagged Tumblr posts
Text
so before now ive only kinda half understood when people are like "i found out the name of this medical condition i have and cried" bc like yeah, that does sound really affirming and a relief but i hadnt ever empathised with it until right now
was rotting my brain on tiktok and came across this girl who was talking about this rare medical condition and the symptoms sounded so much like things i experience and so i did a google deep dive and yeah now im crying because im not insane im not crazy i didnt make it up 😭
im crying again now because its genuinely such a strong emotional feeling to be hit with knowing that this thing you thought wasnt real is actually a proper medical condition that youve not been making up in your head
this thing that has affected you all your life, that has had a huge impact on so much of every day life and interactions with people and the way i have to go about certain things, is real. i have never felt such intense feelings as right now 😭
5 notes
·
View notes
Text
my chronically ill best friend just said "I feel like the side effects part of a medication commercial" SO FUCKING TRUE BABE
#we have the same medical condition#pots#potsie#pots syndrome#chronic nausea#chronic joint pain#chronically ill#chronic fatigue syndrome#chronic illness#chronic pain#chronic fatigue#spoonie#invisible disability#disabled#actually disabled#gastroparesis#hypermobile ehlers danlos#ehlers danlos syndrome#hypermobility spectrum disorder#hypermobile eds#hypermobility#wheelchair#wheelchair user#mobility aid#cripple punk#cripplepunk
2K notes
·
View notes
Text
Metabolic syndrome is a complex and potentially life-threatening condition that can significantly impact an individual’s health. Therefore, it is crucial for patients of family practice in Linwood NJ to understand its risks and take proactive measures to manage and prevent it.
0 notes
Text
Medical cannabis can only be administered if the patient has a current written certification from a board-registered practitioner. Medical marijuana certifications in Virginia are only valid for one year. Thus, if your certificate is set to expire, you must submit for cannabis certificate renewal in Virginia. Is this, however, necessary? Yes! But why is this so?
1 note
·
View note
Text
Here's a reminder to fight the internalized sanism/ableism in your head.
If you have executive dysfunction, don't compare your productivity to people who don't.
If you have anhedonia, don't compare your struggling to keep up with hobbies to someone who doesn't.
If you have paranoia, don't think of your fears as any less valid than the fears of someone who doesn't.
If your meds make you tired constantly, don't compare your energy levels to someone who doesn't take those meds.
If you have issues with concentration, then you won't be able to pay attention as well as someone who doesn't.
If you're in the deep end of a pool, then you can't compare how well you keep your head above water to someone who is standing in a kiddie pool.
Please try to think of these things when you feel "lazy" or "childish" or "a failure" compared to other people that don't struggle with the same symptoms as you. If you have a mental illness that will affect how you act in everyday situations, then it will in fact affect you in everyday situations. It's not an excuse, it's just a reality. We need to try to be kinder to ourselves.
#mental illness#mental health awarness#mental health reminders#neurodivergent community#neurodivergent#neurodivergency#schizophrenic#schizophrenia#schizoaffective disorder#executive dysfunction#anhedonia#paranoia#tw medication side effects#concentration issues
3K notes
·
View notes
Text
PURE BITTER ALMOND OIL
Almond oil absorbs fast into our skin, making it a potent and efficient moisturizer. It is a light oil that does not leave a greasy aftertaste. It is high in Vitamin E, a potent antioxidant that promotes healthy skin and collagen synthesis. It also included a natural SPF of 5, which is said to be healthful and helps protect the skin and scalp from sun damage. Organic Bitter almond oil is extensively used in the components of hair products because it helps to strengthen the hair and improves its shine of the hair, therefore almond oil is commonly used as a hair conditioner or hair tonic. It has antispasmodic qualities and is used to treat medical disorders such as spasms, discomfort, and cramping.

0 notes
Text
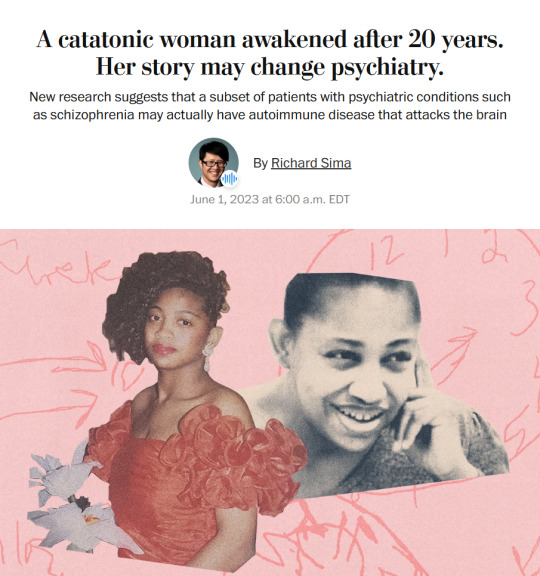
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes
Text
My lifesaving medication should not be $4000 per dose.
My other lifesaving medication should not be $1200 per dose.
My other lifesaving medication should not be $200 per bottle.
The medication that I need to live should not cost more than my rent.
#medication#health care#united healthcare#health insurance#blue cross blue shield#chronic illness#disabled#chronic disability#chronically ill#chronic disease#chronicpain#other chronic illness bs#disability#disablity#undiagnosed chronic illness#chronic disorder#chronic pain#chronic fatigue#nerve pain#joint pain#disabilities#actually disabled#invisible disability#physically disabled#cpunk#angry cripple#cripple life#cripple problems#cripple punk#cripplepunk
345 notes
·
View notes
Text
I hope you heal so much that taking care of yourself is one of your favorite things to do and I hope you can forgive yourself for everything you did before you got there
#trauma recovery#complex trauma#ed recovery#ana recovery#csa survivor#cptsd healing#cptsd vent#trauma disorders#traumagenic#adverse childhood experiences#childhood trauma#medical trauma#autistic trauma#neurodiversity#did osdd#complex post traumatic stress disorder#post traumatic growth#self care#trauma healing#trauma brain#childhood neglect#childhood abuse#substance abuse#abuse recovery#late diagnosed autistic#childhood emotional neglect#bpd thoughts#autistic borderline#borderline personality disorder#adhd autistic
1K notes
·
View notes
Text
LAP Bands should be illegal
This post is going to deal with medical fatphobia, weight loss surgery, coercion, emetophobia, food issues, disordered eating, and just all around bad shit. But it’s important.
Shortly after I reached adulthood, I was coerced into weight loss surgery. I weighed about 250 pounds and was considered morbidly obese.
The Lap Band is a disgrace to the medical profession and is just another example of how the medical profession does not care about the lives of fat people.
To preface this: the surgery works. I lost 70 pounds and people treated me differently and I hated them all for it.
The Lap Band made my life miserable. When it was filled, I could not eat until noon without getting stuck. Even then, getting stuck was always a risk. There was a strict diet to follow and you were supposed to be safe from that if you followed it. On top of that, there were rules for how you ate. One standard I saw was not to eat in bites larger than your fingernail. Can you see yourself doing that for a week, let alone years and years?
Getting stuck is a horror you can't imagine. The food lodges in the top of your stomach, blocking off your system. You continue to produce saliva and swallow it down. Slowly, the mucous in your saliva builds up. It feels like you're drowning. Eventually, you have to essentially throw it all up. A disgusting experience (and a mortifying one if you're in public.) The saliva is thick and ropy. This experience is often called "sliming" on the forums.
I became frightened of eating in public. In a way, I became frightened of food altogether. I knew something had to give the day I reacted to someone biting a hamburger in a tv show the way a regular person would react to a killer jumping out in a horror movie. I developed the disgusting and unhealthy habit of chewing and spitting out food. I completely lost my enjoyment of many foods I had previously enjoyed because of how problematic they were (I can no longer enjoy a chicken thigh for example.) I stopped eating meals and began grazing. I developed eating habits worse than the ones that "made me fat"
After 3 years, I had the band emptied of fluid, which significantly decreased, but did not stop, these problems. I regained the weight, and found it didn't bother me. (Along the way I discovered that my discomfort with my body had never been weight related)
I had my band removed after 6.5 years earlier this year. I am in a support group on facebook for victims of this malpractice. There are 5.6 thousand members, each with their own horror stories. Some of them cannot get the band removed because insurance will not cover the procedure, though they happily covered the band's placement. Some have tried to go through with removal but have had surgeons try to coerce them into getting a different weight-loss surgery instead of just removing it. Many have long-term damage from the band eroding the walls of their stomach or esophagus, or from the band adhering to multiple organs. Many of them had the band for 12-14 years, before removal because none of our doctors told us it needs to be removed within 10.
Many practices no longer perform Lap Band surgery and now believe it is unethical. The surgeon who removed my band still performs this surgery regularly.
A study performed in 2011 with 151 lap band patients, found that 22% of patients experienced minor complications and 39% experienced major complications. The person who coerced me into surgery actually experienced major complications and needed an emergency removal.
I experienced no serious complications. Everything I described above is considered normal. And It still drastically lowered my quality of life.
I don't know why I'm sharing this or who I'm sharing it for, but here I am. If you know anyone considering the lap band surgery, don't let them go through with it without knowing the truth. And please be kinder to your body than the medical profession wants you to be.
3K notes
·
View notes
Text
i remember being ten years old and wishing to die rather than experience the pain i was in yet still my parents and my doctors didn’t believe me. sometimes it just hits me. that wasn’t a normal experience for a ten year old, was it?
#chronic illness#chronically ill#chronic pain#cripple posting#cripple punk#cripplepunk#crip punk#cripple shit#queer cripple#crippunk#angry cripple#cripple life#cripple problems#functional neurological disorder#fibro problems#fibromyalgia#the chronicles of illness#stomach issues#gi disability#gi issues#medical neglect#medical trauma#physically disabled#physical disability#disabled#disability#disabilties#cripple punk community#c punk#pain posting
587 notes
·
View notes
Text
Sometimes I feel like celiac disease doesn't actually count as a disability since it's so easy and stress free compared to deadly allergies, but then I remember that I have to meticulously plan every trip I go to and play 4D chess with uni campus restaurant menus and for a brief moment there was genuine consideration if I should be put on growth hormones because I was so small from not getting enough nutrients
#...but then again its so easy. its no deadly nut allergy or diabetes#but then again i cant go to some countries?????#but then again i dont even have to take like medication and im not in pain constantly#but then again i was so pale and small before they found my celiac. there was no growth in my body and i shouldve been taller#but i wont DIE if i ingest gluten#but i would have a landslide's amount of other symptoms if i did ingest gluten regularly to this day#but its really just a stomach ache its nothing#but the food is more expensive and that really adds up in the long run when theres no welfare for celiac from the government#but its so accessible nowadays its like theres no issue at all#but... i have been told people feel sorry for me#but its so easy! it doesnt really count.#not fish#complicated thoughts about a lifelong autoimmune disorder is all
276 notes
·
View notes
Text

SUBJECT FASCINATION DISORDER
(SFD)
A Medically Unrecognized Disorder characterized by the unadulterated need to investigate and or study people in the likes of a test subject.
People with this disorder oftentimes struggle with their identity due to confusion of interests and self. They may also have a difficult time forming relationships, as infatuation is confused with genuine bonds.
#radqueer#rq#rq 🌈🍓#transid#transid coining#rq community#rq please interact#transdid#medically unrecognized disorder
296 notes
·
View notes
Text
#flashback#living with cptsd#cptsd recovery#cptsd problems#cpstd#psychiatrist#psychiatry#psychology#complex post traumatic stress disorder#medical ptsd#ptsd recovery#complex ptsd#ptsd#childhood trauma
302 notes
·
View notes
Text



fictional reliance disorder (FRD)
> when one is heavily impacted by or heavily reliant on works of fiction. this includes;
holding views or beliefs that are mainly present in fiction/mainly based in fiction.
having unrealistic expectations of certain experiences.
relying heavily on works of fiction to function or prefering to interact with fiction over reality.
experiencing confusion or upsetness when something turns out different from the media they consume.
maladaptive daydreaming, if not daydreaming is still prevelant.
have an interest in creative arts such as drawing or writing.


#radqweer ♡ ིྀ ܀#cwoins ♡ ིྀ ܀#fictional reliance disorder#medically unrecognized disorder#mud coining#radq safe#pro transid#pro radq#radqueer#rq safe#rq 🌈🍓#rq 🍓🌈#rqc🌈🍓#rq community#pro rq 🌈🍓#radqueer 🍓🌈#radq please interact#radq interact
72 notes
·
View notes
Text
Please take kids seriously they are actually people. sentient intelligent beings believe it or not. they know when they’re being blatantly lied to.
They might not understand it, but they know when grownups are being shady.
They know.
Please stop acting like it’s inconsequential if you lie to them or ignore them or dismiss their thoughts and feelings. It’s not. It stays with them forever.
Please take kids seriously.
#i will die on this hill#fucking take kids seriosuly#child advocacy#kids are people too#childhood trauma#childhood emotional neglect#childhood neglect#childhood emotional abuse#child neglect#child abuse#complex trauma#parental trauma#medical trauma#family trauma#autistic trauma#adhd trauma#adhd autistic#audhd problems#borderline stuff#trauma disorders#did osdd#traumagenic#trauma brain#cptsd healing#trauma recovery#late diagnosed autistic#late diagnosed adhd#childhood depression#child care#childhood abuse
466 notes
·
View notes