#Mental Illness and Psychology
Explore tagged Tumblr posts
Text

#Michel Foucault#philosophy#Mental Illness and Psychology#Revision#1962#Translation#1976#Hubert Dreyfus
1 note
·
View note
Text
I talk to many people who say things like "oh I have trauma but I don't have PTSD", but then when I talk to them a little more I realize that they most likely do, they just can't recognize it as such due to how lacking PTSD awareness is, even beyond the whole "it's not just a veteran's disorder" thing.
The main reason they think they don't have PTSD usually has to do with flashbacks and nightmares, either they have one but not the other or have neither. But here's the thing, those are only two symptoms out of the 23-odd recognized symptoms. Flashbacks and nightmares are two of the five symptoms under Criterion B (Intrusion), which you only need one of for a diagnosis. The other three symptoms are unwanted upsetting memories, emotional distress after being reminded of trauma and physical reactivity after being reminded of trauma (i.e. shaking, sweating, heart racing, feeling sick, nauseous or faint, etc). Therefore you can have both flashbacks and nightmares, one but not the other, or neither and still have PTSD.
In fact, a lot of the reasons people give me for why they don't think they have PTSD are literally a part of the diagnostic criteria.
"Oh, I can barely remember most parts of my trauma anyway." Criterion D (Negative Alterations in Cognition and Mood) includes inability to recall key features of the trauma.
"Oh but I don't get upset about my trauma that often because I avoid thinking of it or being around things that remind me of it most of the time." Criterion C (Avoidance) includes avoiding trauma-related thoughts or feelings and avoiding trauma-related external reminders, and you literally cannot get diagnosed if you don't have at least one of those two symptoms.
"Oh I just have trouble getting to sleep or staying asleep, but I don't have nightmares." Criterion E (Alterations in Arousal and Reactivity) includes difficulting sleeping outside of nightmares.
"But I didn't have many/any trauma symptoms until a long time after the trauma happened." There's literally an entire specification for that.
Really it just shows how despite being one of the most well-known mental illnesses, people really don't know much about PTSD. If you have trauma, I ask you to at least look at the criteria before you decide you don't have PTSD. Hell, even if you don't have trauma, look at the criteria anyway because there are so many symptoms in there that just are not talked about.
PTSD awareness is not just about flashbacks and nightmares.
#ptsd#post traumatic stress disorder#cptsd#complex post traumatic stress disorder#complex ptsd#trauma#actually ptsd#actually cptsd#mental illness#mental health#mental health awareness#ptsd awareness#cptsd awareness#neurodivergent#ptsd thoughts#awareness#important#mentally ill#actually mentally ill#psychology
49K notes
·
View notes
Text

#positive mental attitude#mental health#mental illness#actually mentally ill#stress#psychology#mentally fucked#meme#funny#funny memes#humor#haha#lol#memes#funny shit#weird memes#funny post#overwhelmed
2K notes
·
View notes
Text
#spoonie#chronic illness#chronically ill#chronic disease#invisible disability#disabled#disabled people#disability#mentally disabled#actually disabled#disabled artist#disabled girl#disabilties#disabled pride#disabled representation#disabled community#disabled life#disabled rights#disabledcreator#physical disability#physically disabled#disabledandcute#psychology
1K notes
·
View notes
Text
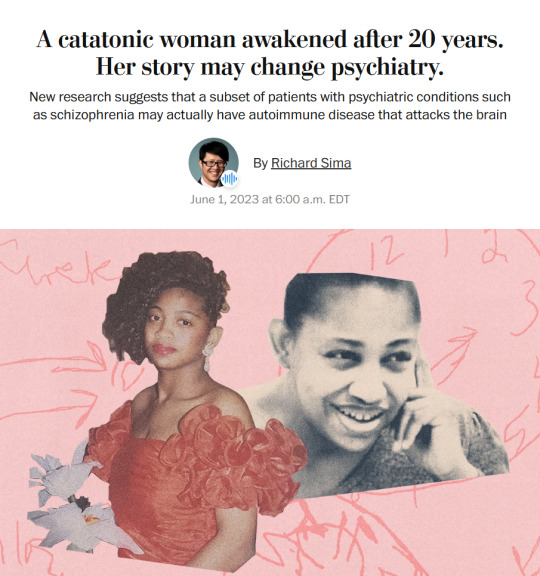
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes
Text
Does anyone else feel lonesome?
Not lonely. Not alone. Just... lonesome. Like you don't feel connected to anyone. Like you never feel that you will find anyone that understands you, that will see you truly, let alone someone who will even like you. You see friends everywhere, but you don't see yourself in their place, like that is not for you, like you're not made for that and that's not made for you. You see people having fun and laughing and dancing and getting drunk and falling in love and you just... don't feel that for yourself. Like you're not supposed to have that, like you can't because it's not for you and you're not for it.
Like you're supposed to be seeing all these beautiful things in the world but not experience them yourself. Like you want to experience so much, experience everything, but be overwhelmed by it so you don't do any of it.
Like you want to be everywhere and do everything, but you don't belong anywhere and can't do anything. Like you're not supposed to be here. Not in a self-deprecating way but in an incongruous way. You want to live you want to be alive, but you feel you're not supposed to be. Not here at least, not like this. Just a presence in the world, not an active member of it. Even your body doesn't feel like home, your face isn't a face you recognise, like you're not supposed to have either. Like you're just supposed to be.
Like you're supposed to observe, but not experience.
#life#deep thoughts#deep feelings#how do I tag this?#mental illness#?#autism#is this the autism?#audhd#adhd#neurodivergence#neurodivergent#psychology#alone#lonesome#lonely#loneliness#ace#asexual#aro#aromantic#aroace
4K notes
·
View notes
Text
Reblog/interact if your blog is a safe space for all people struggling with their Cluster A, B, and C personality disorder regardless of whether they are high or low-functioning in their disorder.
#cluster b safe#cluster a#cluster b#cluster c#cluster a safe#cluster c safe#alex talks#psychology#mental health#mental disability#mental disorders#mental illness#ppd#ppd safe#ScPD#scpd safe#stpd#stpd safe#aspd#bpd#npd#hpd#aspd safe#bpd safe#npd safe#hpd safe#avpd#dpd#ocpd#dpd safe
663 notes
·
View notes
Text
i really can not stand the “fandom is so fun we’re all just projecting and making shit up” thing. because no i actually deeply admire the canon of my favorite media and all the intention and care and craft put into it. we are not the same.
#ur supposed to do that when the source material sucks#when theres huge gaps worth filling whether its in representation or just bad writing or SOMETHING fundamentally unexplored#when the source material is good and smart and has like 2 decades worth of really well developed characters with psychological complexity#stories about queerness and mental illness and neurodivergence and shit. all right there in canon. ripe to pick and dig ur teeth in#WHY BOTHER MAKING SHIT UP it just. dumbs down everything.#not to be like a rick and morty redditor going umm ackshully u need a high iq to understand this show ☝️🤓#but like. it’s true maybe? media literacy is kicking half this fandom’s ass#im not talking about anyone in particular just a general trend im seeing getting worse
874 notes
·
View notes
Text
Hey just to ruin your day I want you guys to remember that before Drake in the second book Andrew had been making genuine steps towards recovery even if we didn’t get to see it very closely
Andrew being on his meds for the first and second book make it hard to see, especially since we didn’t meet him before he was on his meds but it can be inferred that he was making real progress on reclaiming his autonomy
He went to therapy regularly in which he actually talked to and got along with his therapist. He was able to have an ongoing relationship with Roland, and even though he insisted on using handcuffs that’s actually a healthy coping mechanism (he was able to recognise a problem which caused him distress aka people touching him without permission and applied a non-harmful solution which allowed him to continue without running away that’s the definition of learning to cope), he was not actively self-harming which we know by the fact that he has scars, not wounds, scratches or anything else, just healed scars. He was also able to accept and embrace his sexuality despite his history. He still has suicidal ideation but he is no longer practicing suicidal tendencies, which is genuinely huge progress
His biggest issues during the book are his meds (which seem to make it harder for him to regulate his emotions and his reactions and therefore causes him to the extreme measures which are familiar to him aka violence) and his relationship with Aaron/Kevin caused by an unhealthy desire to protect people. He was making an actual recovery, albeit a slow one, which just makes what happens to him all the more horrible
During the second book it had been seven years since he experienced that kind of abuse, seven years in which he clearly was slowly getting better only to be retraumatised again
Just
I think about this all the time I need to inflict this onto someone else
#all for the game#aftg#putting the psychology knowledge to use with this one#psychoanalysing my faves#don’t get me wrong he was still very mentally ill in the first books#like he had issues to work through fr#but he was getting better#andrew minyard#neil josten#he’s not mentioned here but they’re a matched set#aaron minyard#kevin day
564 notes
·
View notes
Text
Needs to be said, probably controversial, but "bad" people deserve support for their mental health issues as well. "Bad" people should not be dehumanized and berated for their mental health issues. I dont care what they've done
#mental health#mental illness#actually mentally ill#mental health awareness#npd#aspd#cluster b#psychology#actually aspd#antisocial personality disorder#cluster b pds#personality disorder#aspd positivity
725 notes
·
View notes
Text

Hi there! My name is Bri Pastro and I’m a queer doctoral candidate in Clinical Psychology at Fordham University. I’m a part of a research team collaborating with University of Maine to investigate mental health in rural vs. urban teenagers!
Our study is regarding risk & resilience related to mental health in adolescents. We’re particularly interested in online and interpersonal interactions and how these factor into mental health. Participating includes completing a 25 minute online survey.
In order to participate in this study participants must: Be 15-18 years old, be comfortable reading and speaking English, and live in a rural community OR an urban community in the United States.
If you are interested in participating in the study, please click on the link below. Participants who complete the study will be entered into a raffle to win one of 20, $25 Amazon gift cards.
If you know someone who may be interested, please send them this link!
Thank you for helping me with my doctoral research! Participation is completely voluntary, and participants may end the study at any time. All data is confidential. This study was approved by the Fordham University and University of Maine Institutional Review Boards.
We hope that this research helps us better understand experiences for adolescents across the United States. Please reach out to us at [email protected] with any questions. We are closing recruitment at the end of the month and are putting one last push to get more participants! Please repost as you can :)
#mental health#research#rural#gay#lgbt#lesbian#lgbt+#lgbtqia#psychology#psych#mental health awareness month#mental illness#mental wellness#mental heath support#mental wellbeing#stress#therapy#burnout
204 notes
·
View notes
Text










Images (Robert Altman, 1972)
#Films watched in 2024#Images#Robert Altman#1972#Susannah York#Cathryn Harrison#René Auberjonois#Rene Auberjonois#horror#seis#hands#drama#intrigue#psychological thriller#puzzle#murder#mental illness#reflections#knife#house
154 notes
·
View notes
Text
I just want kill myself but i’m scared. I guess i’m just coward…

#sad thoughts#depressing shit#depressing life#lonelly#loneliest#im so tired#tired#lost#lost in thought#i'm sad#in pain#writing#writeblr#writers on tumblr#mental health#mental illness#mentally fucked#actually mentally ill#mentally exhausted#mentally tired#mental heath support#psychology#sorry for being depressing#never enough#negative#i hate my body#i hate everything#hate myself#i want to cry#i want die
310 notes
·
View notes
Text
This is so terrible I'm going to kill... (remembers that suicide jokes help normalize having those types of thoughts and make it easier being open about self harm and suicide without stigma) myself.
#196#tw s3lf harm#tw sui ideation#tw self destruction#tw scuicide#tw scuicidal thoughts#scuicide#mental health#mental illness#actually mentally ill#mentally fucked#anti psychiatry#anti psychology#madpunk#mad pride#neurodivergent#neurodiversity#neuropunk
175 notes
·
View notes
Text

This is your "oh shit it's getting hot again" reminder that SSRIs / antidepressants cause sun sensitivity and make you more prone to dehydration. Stay hydrated babes.
#spoonie#chronic illness#chronically ill#chronic disease#invisible disability#mental illness#disabled life#disabled community#disability#mental heath support#ssri#mental health support#mental health#mental health awareness#mentalheathawareness#mental heath awareness#psychology#little psa#psa#this has been a psa#good to know#good to reblog#spread the word
883 notes
·
View notes
