#such a widely varying disorder and the symptoms one can have from it can be genuinely terrifying and severe
Explore tagged Tumblr posts
Note
wait, are the health claims from bone broth bogus? (genuine/good faith question). i’ve always heard that it’s high in collagen, which supposedly is good for you and better if you get it ‘naturally’ like from bone broth. is that another thing that’s not actually true, or wildly exaggerated?
Bone broth has been eaten for centuries in various cultures because it is easy to digest and believed to have healing properties. Chicken broth is highly valued by some as a remedy for the flu. In more recent years it has been promoted to help symptoms from psychiatric and neurodevelopmental disorders including autism and attention-deficit hyperactivity. [7] Claims that it detoxifies the liver, improves digestion, reverses wrinkles, builds bones, and relieves join pain have led some marketing analysts to predict that the bone broth market will approach $3 billion by 2024. [8] In reality, bone broth contains only small amounts of minerals naturally found in bone including calcium, magnesium, potassium, iron, phosphorus, sodium, and copper. The amount of protein, obtained from the gelatin, varies from 5-10 grams per cup. There is some concern that bone broth contains toxic metals like lead. One small study found that bone broth made from chicken bones contained three times the lead as chicken broth made with the meat only. [7] However the amount of lead in the bone broth per serving was still less than half the amount permitted by the Environmental Protection Agency in drinking water. A different study found that bone broth, both homemade and commercially produced, contained low levels (<5% RDA) of calcium and magnesium as well as heavy metals like lead and cadmium. [9] The study noted that various factors can affect the amount of protein and minerals extracted in bone broth: the amount of acidity, cooking time, cooking temperature, and type of animal bone used. Therefore it is likely that the nutritional value of bone broths will vary widely.
(Source: https://nutritionsource.hsph.harvard.edu/collagen/)
Your body makes collagen; eating collagen will put the things that make collagen into your body to make collagen with, but so will eating things that go into making collagen (amino acids, basically).
There's not good evidence that eating a ton of collagen or supplementing collagen improves your body's collagen production, and studies on collagen supplementation tend to be done by companies that make collagen supplements or produce expensive bone broth.
Basically if you're eating the 9 essential amino acids by consuming complete proteins (which can be done on any kind of diet, vegan or vegetarian or including meat - this is NOT one of those things your body relies on animal products to produce) your body is going to make collagen and it's going to have the amino acids handy to make collagen; consuming more collagen may mean that your body has more of those collagen-forming amino acids on hand, but it doesn't mean that your body is going to be any more efficient at producing collagen (and your body is going to become less efficient at producing collagen as you age).
But yeah bone broth health claims are primarily bogus. If you want more collagen in your diet for whatever reason, it's probably about as effective to eat jello as it is to eat bone broth but also more collagen in your diet likely isn't doing anything special.
1K notes
·
View notes
Note
Heey, hope this finds you well! Can you make writing notes about psychoses? I'm really interested about writing about my OC's mental state, thanks!
Writing Notes: Psychosis
Defining "Psychosis"
Psychosis - a collection of symptoms that affect the mind, where there has been some loss of contact with reality. During an episode of psychosis, a person’s thoughts and perceptions are disrupted and they may have difficulty recognizing what is real and what is not.
The 3 Main Symptoms of psychosis are:
hallucinations – where a person hears, sees and, in some cases, feels, smells or tastes things that do not exist outside their mind but can feel very real to the person affected by them; a common hallucination is hearing voices
delusions – where a person has strong beliefs that are not shared by others; a common delusion is someone believing there's a conspiracy to harm them
disordered thinking and speaking - a person's thoughts and ideas come very quickly, which can make their speech fast and confusing
The combination of hallucinations and delusional thinking can cause severe distress and a change in behaviour.
Experiencing the symptoms of psychosis is often referred to as having a psychotic episode.
Psychosis occurs when a person loses contact with reality. The person may:
Have false beliefs about what is taking place, or who one is (delusions)
See or hear things that are not there (hallucinations)
It is an abnormal mental state involving significant problems with reality testing.
Characterized by serious impairments or disruptions in the most fundamental higher brain functions:
perception,
cognition and cognitive processing, and
emotions or affect
as manifested in behavioral phenomena, such as:
delusions,
hallucinations, and
significantly disorganized speech
Psychosis is most likely to occur in young adults and is quite common.
Around 3 out of every 100 young people will experience a psychotic episode.
Most make a full recovery from the experience.
Psychosis can happen to anyone.
An episode of psychosis is treatable, and it is possible to recover.
It is widely accepted that the earlier people get help the better the outcome.
25% of people who develop psychosis will never have another episode, another 50% may have more than one episode but will be able to live normal lives.
Some people who develop psychosis may need ongoing support and treatment throughout their lives.
Historically: psychosis referred to any severe mental disorder that significantly interferes with functioning and ability to perform activities essential to daily living.
First Episode Psychosis
Refers to the first time someone experiences psychotic symptoms or a psychotic episode.
People experiencing a first episode may not understand what is happening.
The symptoms can be highly disturbing and unfamiliar, leaving the person confused and distressed.
Unfortunately, negative myths and stereotypes about mental illness and psychosis in particular are still common in the community.
A psychotic episode occurs in 3 phases. The length of each phase varies from person to person:
Phase 1: Prodome (psychosis syndrome)
The early signs may be vague and hardly noticeable. There may be changes in the way some people describe their feelings, thoughts and perceptions, which may become more difficult over time. Each person’s experience will differ and not everyone will experience all of the following "common signs":
Reduced concentration
Decreased motivation
Depressed mood
Sleep disturbance
Anxiety
Social withdrawal
Suspiciousness
Deterioration in functioning
Withdrawal from family and friends
Odd beliefs/magical thinking
[Magical thinking - the belief that events or the behavior of others can be influenced by one’s thoughts, wishes, or rituals. Magical thinking is typical of children up to 4 or 5 years of age, after which reality thinking begins to predominate.]
Phase 2: Acute
The acute phase is when the symptoms of psychosis begin to emerge.
It is also known as the "critical period."
Clear psychotic symptoms are experienced, such as hallucinations, delusions or confused thinking.
During this phase, the person experiencing psychosis can become extremely distressed by what is happening to them or behave in a manner that is so out of character that family members can become extremely concerned and may start to seek help. Before this stage the individual may have been experiencing a more gradual decline.
Phase 3: Recovery
With effective treatment most people will recover from their first episode of psychosis and may never have another episode.
It is important to remember that psychosis is a treatable condition and if help is sought early, an individual may never suffer another episode.
Initially, some of the symptoms that are apparent in the acute phase may linger in the recovery phase but with appropriate treatment most people successfully recover and return to their normal, everyday lives.
Some Symptoms of Psychosis
A person with psychosis may have any of the following:
Disorganized thought and speech
False beliefs that are not based on reality (delusions), especially unfounded fear or suspicion
Hearing, seeing, or feeling things that are not there (hallucinations)
Thoughts that "jump" between unrelated topics (disordered thinking)
What does psychosis look like? Responding to things, losing track of thoughts, appearing frightened or being very sure of things which don’t seem to be true, some people are more withdrawn, or their personality seems different. Big changes in behaviour and ability to do their usual activities.
Each person who experiences psychosis will have a unique experience and combination of symptoms, which may include:
Hearing, seeing, smelling, feeling or tasting things that other people don’t (sometimes called hallucinations)
Feeling unsafe and that people are working against you, or trying to harm you
Believing that you have special powers or abilities
Noticing patterns or feeling that things have a special significance for you (such as believing a famous song has been written about you or an event in the news has been caused by you)
Finding it hard to follow conversations, getting muddled in your thoughts or when speaking
Feeling that your thoughts have been removed or tampered with, or that someone else is in control of your body
Some people also become quite withdrawn and experience loss of motivation and emotions
When experiencing psychosis, people often struggle with their relationships, daily activities, school or work.
Some people, when told they have psychosis, worry that they might have a long-term mental illness like schizophrenia.
It’s important to know that psychosis can happen for all sorts of different reasons and having an episode doesn’t necessarily mean that you will have another or that you will have a long-term problem.
Psychotic symptoms typically include changes in thinking, mood and behavior. Symptoms vary from person to person and may change over time. Some of the more characteristic symptoms can be grouped into 5 categories:
Confused Thinking: Thoughts become muddled or confused. The person may not make sense when speaking. The person may have difficulty concentrating, following a conversation or remembering things. His or her mind may race or appear to be processing information in slow motion.
False Beliefs: False beliefs, known as delusions, are common. The person can be so convinced of the reality of their delusion that no amount of logical argument can dissuade them. For example, they may believe the police are watching them, or they might think they are receiving special messages from the television, radio or newspaper.
Hallucinations: In psychosis, the person sees, hears, feels, smells or tastes something that is not actually there. For example, they may hear voices which no one else can hear, or see things which aren’t there. Things may taste or smell as if they are bad or even poisoned.
Changed feelings: How someone feels may change for no apparent reason. They may feel strange and cut off from the world. Mood swings are common and they may feel unusually excited or depressed. A person’s emotions feel dampened and they may show less emotion to those around them.
Changed behavior: People with psychosis may behave differently from the way they usually do. They may be extremely active or lethargic. They may laugh inappropriately or become angry or upset without apparent cause. Often, changes in behavior are associated with the symptoms already described above. For example, a person believing they are in danger may call the police. Someone who believes he is Jesus Christ may spend the day preaching in the streets. A person may stop eating because they are concerned that the food is poisoned, or have trouble sleeping because they are scared.
The symptoms of psychosis are often categorized as either “positive” or “negative.”
Positive symptoms are those that add to or distort the person’s normal functioning. They include:
delusions (false beliefs that are firmly held and are out of keeping with the person’s culture)
hallucinations (hearing, seeing, tasting, smelling or feeling something that is not actually there)
disorganized speech, thoughts or behaviour (e.g., switching rapidly between subjects in speaking; finding it hard to concentrate or follow a conversation; being unable to complete everyday tasks).
Negative symptoms involve normal functioning becoming lost or reduced. They may include:
restricted emotional and facial expression
restricted speech and verbal fluency
difficulty with generating ideas or thoughts
reduced ability to begin tasks
reduced socialization and motivation.
Other symptoms may include:
cognitive symptoms, such as difficulties with attention, concentration and memory
mood changes
suicidal thoughts or behaviours
substance abuse
sleep disturbances.
Possible Causes of Psychosis
Medical problems that can cause psychosis include:
Alcohol and certain illegal drugs, both during use and during withdrawal
Brain diseases, such as Parkinson disease and Huntington disease
Brain tumors or cysts
Dementia (including Alzheimer disease)
HIV and other infections that affect the brain
Some prescription drugs, such as steroids and stimulants
Some types of epilepsy
Stroke
Psychosis may also be found in:
Most people with schizophrenia
Some people with bipolar disorder (manic-depressive) or severe depression
Some personality disorders
Assessment
Psychiatric evaluation and testing are used to diagnose the cause of the psychosis. Laboratory testing and brain scans may not be needed, but sometimes can help pinpoint the diagnosis. Tests may include:
Blood tests for abnormal electrolyte and hormone levels
Blood tests for syphilis and other infections
Drug screens
MRI of the brain
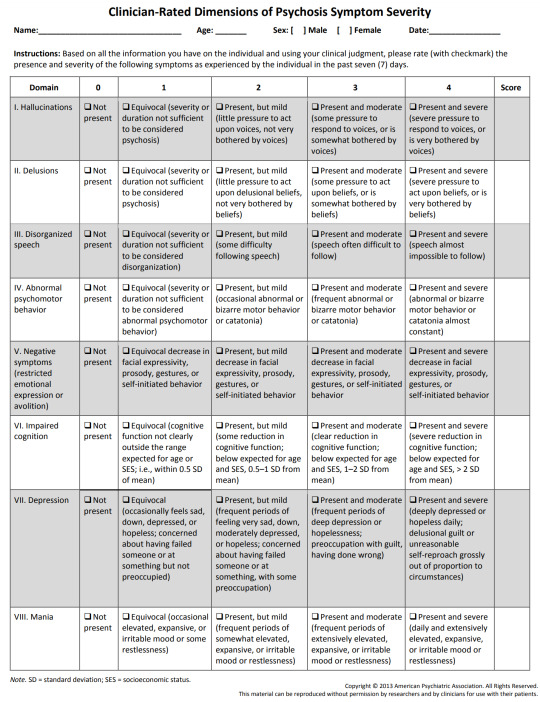
Clinician-Rated Dimensions of Psychosis Symptom Severity. The American Psychiatric Association is offering a number of “emerging measures” for further research and clinical evaluation.
These patient assessment measures were developed to be administered at the initial patient interview and to monitor treatment progress.
They should be used in research and evaluation as potentially useful tools to enhance clinical decision-making and not as the sole basis for making a clinical diagnosis.
Treatment
Depends on the cause of the psychosis.
Care in a hospital is often needed to ensure the person's safety.
Antipsychotic drugs, which reduce hallucinations and delusions and improve thinking and behavior, are helpful.
Psychosis can prevent people from functioning normally and caring for themselves.
Left untreated, people can sometimes harm themselves or others.
Prevention depends on the cause. For example, avoiding alcohol prevents psychosis caused by alcohol use.
Coordinated specialty care consists of multiple components:
Individual or group psychotherapy is tailored to a person’s recovery goals. Cognitive and behavioral therapies focus on developing the knowledge and skills necessary to build resilience and cope with aspects of psychosis while maintaining and achieving personal goals.
Family support and education programs teach family members about psychosis as well as coping, communication, and problem-solving skills. Family members who are informed and involved are more prepared to help loved ones through the recovery process.
Medication management (also called pharmacotherapy) means tailoring medication to a person’s specific needs by selecting the appropriate type and dose of medication to help reduce psychosis symptoms. Like all medications, antipsychotic medications have risks and benefits. People should talk with a health care provider about side effects, medication costs, and dosage preferences (daily pill or monthly injection).
Supported employment and education services focus on return to work or school, using the support of a coach to help people achieve their goals.
Case management provides opportunities for people with psychosis to work with a case manager to address practical problems and improve access to needed support services.
How well a person does depends on the cause of the psychosis.
If the cause can be corrected, the outlook is often good. In this case, treatment with antipsychotic medicine may be brief.
Some chronic conditions, such as schizophrenia, may need lifelong treatment with antipsychotic drugs to control symptoms.
Early Intervention
Research has found that early intervention is beneficial for patients and loved ones for the following reasons:
Less treatment resistance and lower risk of relapse
Reduced risk for suicide
Reduced disruptions to work or school attendance
Retention of social skills and support
Decreased need for hospitalization
More rapid recovery and better prognosis
Reduced family disruption and distress
A person will often show changes in their behavior before psychosis develops. Behavioral warning signs for psychosis include:
Suspiciousness, paranoid ideas, or uneasiness with others
Trouble thinking clearly and logically
Withdrawing socially and spending a lot more time alone
Unusual or overly intense ideas, strange feelings, or a lack of feelings
Decline in self-care or personal hygiene
Disruption of sleep, including difficulty falling asleep and reduced sleep time
Difficulty telling reality from fantasy
Confused speech or trouble communicating
Sudden drop in grades or job performance
Alongside these symptoms, a person with psychosis may also experience more general changes in behavior that include:
Emotional disruption
Anxiety
Lack of motivation
Difficulty functioning overall
In some cases, a person experiencing a psychotic episode may behave in confusing and unpredictable ways and may harm themselves or become threatening or violent toward others. The risk of violence and suicide decreases with treatment for psychosis, so it is important to seek help. If you find that you are experiencing these changes in behavior or notice them in a friend or family member and they begin to intensify or do not go away, reach out to a health care provider.
IN TEENS OR YOUNG ADULTS. Before having clear symptoms of psychosis, a teen or young adult often experiences distressing changes in thoughts and emotions. They might:
believe something odd is going on with them, or feel confused about what is real or imaginary
feel singled out, watched, or not fully in control of their thoughts
report changes in perception, such as their eyes or ears playing tricks, hearing jumbled, incomprehensible voices, or seeing shadows or figures in the corners of their eyes
ask for help in trying to make sense of unsettling experiences like these.
Programs specializing in psychosis risk aim to reach out to these individuals.
Recognizing the early signs of psychoses are important in order to get appropriate treatment as early as possible. Early symptoms of psychosis may include, but are not limited to:
odd or bizarre behavior
changes in thinking or speech
decrease in personal hygiene
social withdrawal
preoccupation with a particular topic
marked changes in emotion
Other, more obvious symptoms may include:
extreme suspicion of others,
paranoia,
auditory or visual hallucinations,
delusions and odd, irrational beliefs.
Psychosis is often stigmatized and misunderstood, which can get in the way of getting help. But research has shown that three-quarters of people who do get effective help early can experience relief from their symptoms.
For people who show signs of a possible psychosis, sometimes called "attenuated psychosis syndrome," only about one-third go on to develop a full-blown psychosis. However, they usually have symptoms of depression and anxiety, which can benefit from treatment.
Psychosis as a Symptom
A number of mental illnesses can include psychosis as a symptom, including:
Schizophrenia: A person has some psychotic symptoms for at least 6 months, with a significant decline in the ability to function.
Schizophreniform disorder: A person has some psychotic symptoms for more than one month and less than 6 months.
Bipolar disorder: With this type of illness, the symptoms of psychosis relate more to mood disturbance than to thought disturbance.
Schizoaffective disorder: A person will have symptoms of schizophrenia and, at some point in the course of illness, concurrent symptoms of a mood disturbance.
Depression with psychotic features: A person has severe depression and symptoms of psychosis without the mania associated with bipolar disorder.
Drug-induced psychosis: The use of drugs such as cannabis, cocaine, ecstasy, ketamine, LSD, amphetamines and alcohol can sometimes cause psychotic symptoms.
Organic psychosis: Sometimes, symptoms of psychosis may appear as a result of a physical illness or a head injury.
Brief psychotic disorder: This type of psychosis usually lasts less than a month. It is sometimes triggered by a major stress in the person's life, such as a death in the family.
Delusional disorder: This type of psychosis consists of very strong, fixed beliefs in things that are not true, without the presence of hallucinations.
Psychotic Disorder - any of a number of severe mental disorders, regardless of etiology, characterized by gross impairment in reality testing. The accuracy of perceptions and thoughts is incorrectly evaluated, and incorrect inferences are made about external reality, even in the face of contrary evidence. Specific symptoms indicative of psychotic disorders are delusions, hallucinations, and markedly disorganized speech, thought, or behavior; individuals may have little or no insight into their symptoms. Some examples of psychotic disorders are schizophrenia, schizophreniform disorder, schizoaffective disorder, delusional disorder, brief psychotic disorder, and psychotic disorders due to a substance (see substance-induced psychotic disorder) or to a medical condition.
How to help someone else experiencing symptoms of psychosis:
Often, family and friends help identify someone who is struggling with psychosis, and suffering from their symptoms, so they're important to getting them in touch with professionals who can help.
Stressful life events, such as going off to college or breaking up with a significant other, can trigger psychosis. Further research is needed into why this is, but a low underlying "stress tolerance" level is often seen.
It's all right to mention to someone that you're worried about them, and open the door to discussing it at that point or later. You can find out if there's an early-psychosis clinic near you, and provide information or offer to contact them.
If you notice signs that they're harming themselves, that's the time to seek immediate help, often by starting with contacting suicide hotline or nearby psychiatric emergency room for advice. People with psychosis have 10 to 15 times the risk of suicidal thoughts or behaviors than others.
Treatment, support and how to help find answers for people struggling with psychosis:
Treatments for people showing potential signs of psychosis mostly focus on talk therapy, also called cognitive behavioral therapy. Family and group therapy are also important, and can be done virtually.
For people who show clear breaks with reality, antipsychotic medication can help greatly. The vast majority of people who receive these medicines experience improvement in their symptoms, but they may also experience side effects, so it's important to work with a trained professional to find the best fit.
Women who experienced postpartum psychosis after having a baby are at high risk of experiencing it again if they have another pregnancy, and should receive special attention during and after pregnancy.
A very small number of people with psychosis may be driven by their paranoia or hallucinations to act strangely in public or try to harm others. If you find yourself having to call the police because of such behaviors, make sure they understand and acknowledge that the person you're calling about has a mental health condition and needs help getting to appropriate care.
Just like many infectious diseases can cause a fever, psychosis is part of many mental health conditions – but what exactly causes it isn't well understood. That's why researchers needs people with psychosis to consider taking part in the studies they're running.
"Psychosis strikes in the years when people are just starting to be truly independent in life, work and school, which can make it especially devastating to the person and the family. The process of brain maturation depends on a lot of things going right inside our brains and if they don't, things can go askew. The longer they go untreated, the higher the chance they may experience damage to the brain and be worse off even when they get treatment." Stephan Taylor M.D., who leads a team at Michigan Medicine that specializes in early care for psychosis
Sources: 1 2 3 4 5 6 7 8 9 10 11 12 13 ⚜ More: Notes ⚜ Resources PDFs
Writing about Mental Health Conditions
Hi, here are some references. Choose which ones are most appropriate to incorporate in your story. If possible, it would also be valuable if you know person/s who experience psychosis & speaking with them about it (or if you have personal experiences you could draw from). There's a wide range, so narrowing your depiction down to model one specific life story (or borrowing from just a few) could make your writing more realistic. Do go through the sources linked above as well for more details I wasn't able to include here. Hope this helps with your writing!
#writing notes#character development#writeblr#literature#writers on tumblr#dark academia#writing reference#spilled ink#writing prompt#creative writing#writing tips#writing advice#light academia#writing inspiration#writing ideas#character building#writing resources
150 notes
·
View notes
Text
"If you really had DID, you wouldn't know!"
Says who?!
The idea that people with dissociative identity disorder (DID) can't be aware of their symptoms until they're diagnosed... This is a huge myth about DID and similar experiences; one that has been debunked again and again by experts. Yet it remains! Here are a few examples of this misconception being spread around online: source.
People with DID can be, and often are, aware of their DID symptoms before ever speaking to a clinician.
Where is the proof? Khan (2024) states that, while it's normal for dissociative people to not realize the full extent of their symptoms, trauma, or alters, they can still become aware of any of these things at any point. Source. Dell (2006) actually considers the awareness of alters before diagnosis to be a "common occurrence in DID" which has been widely documented in studies. Multiple diagnostic screening tools inquire about awareness of alters for this reason. Source.
Additionally, alters can have varying degrees of awareness of each other and their symptoms. To quote Howell (2011) from her book, on pages 3-4: Source.
"Different dissociative parts may or may not have knowledge of the affects, behaviors, histories, motives, and thoughts of other parts. How coconscious patients are also varies—that is, the extent to which they have knowledge of and are privy to the thoughts, history, and affairs of the other parts varies. Often, the part of the self that is in executive control is unaware of the thoughts and activities of other parts (often called one-way amnesia). However, this is a tricky topic to try to make clear. For example, coconsciousness may be minimal before beginning psychotherapy for DID but tends to increase considerably in the course of appropriate psychotherapeutic work. Although parts other than the part who is most often in executive control (often called the “host”) are more likely to know of each other and of the host, this is not always the case and is not always the same for different parts of the same patient. Some parts may be unknown by many of the others. The dissociative structure of each patient is different."
Even in the case someone has no memory of their symptoms, they can be made aware through external evidence such as finding purchases or notes that other alters made, police reports confirming traumatic events, someone pointing out their dissociation, etc.
Now let’s talk about something that I feel goes frequently unrecognized: becoming aware of symptoms is often a positive thing! For many people, recognizing their own symptoms is the first step to seeking help for them. As mental health awareness and access to useful information increases, we will likely see an uptick in people with DID developing more awareness of their symptoms and getting help sooner. That’s incredibly positive!
Finally, a small note about diagnosis... Diagnosis is its own loaded topic for a different day. However, I want to point out that people diagnosed with DID still had the DID before their diagnosis. The symptoms were still there, whether they were aware of it or not.
Furthermore, not everyone with DID can obtain a diagnosis or even wants one. There are a myriad of potential reasons for that and I encourage you to do your own research on it. These articles can be a good starting point: source, source, source.
Thanks for reading!
#actuallydid#actually did#dissociative identity disorder#mental health awareness#mental health#did awareness#did misinfo#did information#did osdd#dissociative system#mental illness#mental disorder#dissociative misinfo#dissociative disorder
102 notes
·
View notes
Text
❤️🩹 my take on a PMDD (premenstrual dysphoric disorder) flag 🧠

clipart .png credit
i had been waiting from months to a year to see someone design a flag for PMDD since i'm not very confident in my own ability, so i decided to go ahead and bite the bullet with an attempt. this is currently planned to just be a draft and may be subject to change with new updated versions in the future.
TW FOR MEDICAL TRAUMA/ABUSE: although this topic is not very widely discussed, or at least doesn't seem to be commonly present, online among the disabled community, my personal experiences with PMDD have made acknowledging its existence as well as its consequences quite necessary to me. as of the time of writing this, i am 19 years old, and when i was 15 exactly this time of year (as well as the first similar incident a couple months prior), i had an intense hyper-emotional episode the week before my period that was so bad i ended up getting institutionalized at a psych ward against my will and have never been the same since. for years now, i've been on a birth control pill that suppresses my cyclical hormones and prevents my period from occurring most of the time.
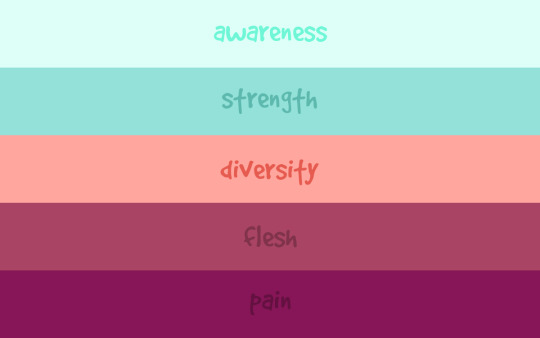
before getting into the stripes' meanings, there are two factors to explain behind my thought process:
dark teal is considered to be the awareness color for this disorder, although i went with a light aqua color because i think it looks better with the pink, and it's in the same family so i believe it still works.
pink is meant not to represent femininity necessarily since uterus-owners can come in many different gender expressions, but rather fit with the vibe of internal organs, especially since pink is closely related to red which is how warm blood appears (and is a key element of uterine cycles).
as for the stripe meanings, here is my proposal for each single word:
awareness ─ suffering from premenstrual dysphoric disorder is a very real thing that happens to müllerian individuals everywhere. according to the cleaveland clinic, which i am an active visiting patient of, about 10% of people with our reproductive body types who are at least of minimum pubescent age may be affected by it. although it does not tend to be a risk toward physical health, it is often a deadly threat to our mental state and well-being, which can lead to suicidal ideation.
strength ─ i consider this to be an invisible disability, with most of the symptoms taking place within our internal worlds and fighting a constant battle with negative thoughts + emotions. in addition to this, physical symptoms also arise and can cause severe discomfort before menstruation even begins. all of this happens within the confines of our own homes, and we tend to suffer through it alone. people who do not have PMDD probably fail to realize how strong we have to be in order to get through this difficult time repeatedly & endlessly, despite their well-intended efforts.
diversity ─ this is intended to have multiple meanings, and to include anything i may not have come up with so far. for one thing, there are plenty of different experiences to be had with this disorder, such as varying levels of cramping + sickness or depression + anxiety. on another note, not only do our bodies each work differently (some may also have endometriosis and/or PCOS, which are also intersex conditions, as a double-whammy), but many of us do not conform to societal ideas of gender despite all having these parts in common. there are infinite possibilities to mix & match with presentation & identity, which is not limited by biology.
flesh ─ although many factors are involved in this process, including hormones, PMDD centers around the uterus, which is an internal organ. the flesh represents the physical aspects of this experience, and how we must take great care of our bodies in order to ease how we feel.
pain ─ there is so much physical + mental pain that builds around this disorder, which deserves to be recognized, sympathized with, and treated. the deep pink (to me) somewhat resembles what ibuprofen & benadryl pills look like; painkillers & antihistamines respectively (i'm not sure if anyone else needs the latter, but my skin's condition gets really reactive when i go through my cycle).
anyone is free to reblog/use accordingly, although you may have to be mindful of permission/credit with the uterus imagery from the source!
tagging for reach (it may not fit your gimmick exactly, so feel free to ignore if you're uninterested, or reblog somewhere else!): @idwl @satyrradio @spaghettimakesflags @obnebulant-mogai @caeliangel @intervex @arco-pluris @beyond-mogai-pride-flags @radiomogai @themogaidragon @neopronouns @mad-pride @disabilitypride
#disability#actual disability#disabled#actually disabled#pmdd#pmdd awareness#premenstrual dysphoric disorder#reproductive disability#invisible disability#mullerian#müllerian#intersex#pcos#polycystic ovarian syndrome#endometriosis#cleveland clinic#medical mistreatment#anti psych#medipunk
67 notes
·
View notes
Text
My analysis on Midoriya and why I think he has undiagnosed BPD
Throughout Izuku's childhood, he was always seen as weird, off-putting, an outsider to social norms. Being left out, being seen as "different" is very common amongst people, especially kids, with undiagnosed disorders. So let's jump straight into it. What is BPD and how does it develop? (Contains manga spoilers)
Here are a few summaries amongst many that I have found (also, I'm not a psychologist or a healthcare professional, these are all just based on my own observations):
BPD, short for Borderline Personality Disorder, is a severe mental health condition characterized by a pervasive and challenging pattern of symptoms including emotional dysregulation, unstable self-identity, fear of abandonment, intense and unstable interpersonal relationships, impulsivity, and self-harming behaviors.
People with borderline personality disorder (BPD) experience extreme emotions. Once a powerful emotion is triggered, it is very hard for them to calm down. Because of this, they often have unstable relationships. They also engage in self-destructive behavior.
Researchers think that BPD is caused by a combination of factors, including:
Stressful or traumatic life events (for example, emotional abuse, neglect, often having felt afraid, upset, unsupported or invalidated),
And genetic factors.
Symptoms may include:
A strong fear of abandonment. This includes going to extreme measures so you're not separated or rejected, even if these fears are made up.
A pattern of unstable, intense relationships, such as believing someone is perfect one moment and then suddenly believing the person doesn't care enough or is cruel.
Quick changes in how you see yourself. This includes shifting goals and values, as well as seeing yourself as bad or as if you don't exist.
Periods of stress-related paranoia and loss of contact with reality.
Self-injury
Wide mood swings that last from a few hours to a few days. These mood swings can include periods of being very happy, irritable or anxious, or feeling shame.
Ongoing feelings of emptiness.
Inappropriate, strong anger, such as losing your temper often, being sarcastic or bitter, or physically fighting.
Now, let's get into it.
BPD, like all disorders, isn't the same for every person. Symptoms and the intensity of these symptoms can vary. It can make some people's life and relationships really difficult, but others can go on for years undiagnosed living a completely happy life without even knowing there's anything wrong. Midoriya's case, in my opinion, is the latter. These symptoms don't surface that obviously in him, but I believe, in different circumstances (queue those Villain Deku and traumatized Deku fics) these symptoms and behaviours could actually turn into much bigger problems and affect his life in a much more impactful way. But, in any case, let's analyze these symptoms and how they may have surfaced in him throughout the manga.
Of course, I decided to turn to TikTok as well and watch some actual explanations and experiences from people who actually have been diagnosed with this disorder in order to understand BPD on a more subjective level, not just objective. And what I have found turned out to be very interesting.
People with BPD often develop a very emotionally attached connection with one specific person in their life, which is their "Favorite person". This person can be anything including a friend, family, therapist, partner, etc. This is a person that someone with BPD can become dependent on. They often view them as a person who's perfect and can do nothing wrong. They might overshare, and expect availability from that person at all times. The dependence on this person goes beyond just adoration, because they are idolizing them to the point where it's all consuming. A person with BPD can switch from absolute adoration one moment to absolute hate the next. They might have trouble with boundaries, sometimes even having zero boundaries when it comes to that person. Their life constantly revolves around that person and the favorite person's identity becomes their own, and they can feel literal physical pain when losing that person. You see where I'm getting at?
I believe Midoriya has developed this dependency and attachment towards one particular person, can you guess who?
Yep, Bakugo Katsuki
Midoriya views Kacchan as perfect, as the embodiment of the image of victory. It's like he blindly ignores Katsuki's bad traits and the things he has done to him, and he idealizes him to the point that Katsuki became his symbol of victory. So much so that he himself has absorbed this identity that he built around Katsuki, for example during battles, which we see during the moments he clearly imitates Bakugo and mirrors him. Izuku "ILoveKacchan'sPersonalSpace" Midoriya basically has zero boundaries when it comes to Katsuki, I mean y'all let's not forget he basically stalked him and even knows what body part Katsuki washes first in the shower. Not to mention he gives zero fucks about boundaries when he butts into Bakugo's emotions even though Bakugo has clearly tried setting boundaries for almost their whole time knowing each other. Deku has also overshared with Katsuki(and only Katsuki), when he told him about OFA even though it was literally meant to be the one secret that he should have kept to himself. His life has always revolved around Bakugo to the point he cannot keep himself away from him.
And talk about experiencing physical pain when losing the favorite person...remember when Bakugo was kidnapped? Yeah, remember that kinda cringe and second hand embarrassing, absolutely animalistic scream that Midoriya let out? Yeah, well..... And then when he actually lost Katsuki, when he saw his dead body. Izuku lost control of his quirks in the middle of a freaking battle, LITERALLY started choking on Blackwhip and screaming in pain, and Blackwhip turned into a heart pierced by three swords that symbolizes intense and extreme physical and emotional pain. Need I say more? No.
And if you think Midoriya isn't capable of extreme hate too, ahhahaha, you're wrong. He can fr switch from absolutely adoring his Kacchan to planning how he's gonna rip off his legs in his diary. Yeah, I haven't forgotten about that one, Izuku.
So, it's very clear that Bakugo is Midoriya's FP and that he has developed this unhealthy, borderline toxic dependency towards him. But let's break down his character even further.
People with BPD tend to engage in self-harming and dangerous activities impulsively, diving in without thinking, in order to feel something. Well, we can tick that one too. Problem child number 1 is known to do and jump into things impulsively without thinking, even if it causes self-injury. In fact, he sometimes engages these self-destructive behaviours on purpose, like all those times when he broke his own bones over and over again. All this just so he can make Todoroki use his right side. Seriously, Deku. Yes, they are training to be heroes, but noone in the class is as reckless and impulsive as Izuku.
Which actually brings me to my next point, which is people with BPD objectifying themselves for validation, going insane lengths just to prove their own self-worth, never having a clear sense of self and seeing themselves as bad or as if they don't exist. I have talked about this in a previous theory of mine too, which you can read here. Midoriya Izuku does not have a clear sense of self. He mirrors others around him, behaving according to the mood and expectations of others. He has no sense of self, because he has built his identity around wanting to be a hero. To him, he is only worth something if he reaches that goal, that dream. Meaning he has no self worth or identity unless he does as he is expected to do, aka be a hero and put everyone else before himself, sacrificing his own needs, and in worse cases his own well-being. He basically objectifies his own self and turns himself into a simple puppet, a Deku, an empty vessel that can hold OFA and his dream of being a hero. To himself, he is nothing more than an object that's meant to be sacrificed if it's needed.
Now, let's continue with: emotional dysregulation, extreme mood swings, and inappropriate, strong anger, such as losing your temper often, being sarcastic or bitter, or physically fighting.
Well, first let's talk about something that's called "splitting". BPD is a disorder that causes extreme mood swings, making the person go one second from feeling happy and fine, to the next second feeling complete, pure rage. There is a fine line between these two moods, and it's very easy to fall over the edge. For some people, it can happen multiple times a day and could last from minutes to hours to even days, and for others, it can happen very rarely, it depends on how severe the symptoms are for each person. One thing in common though, is that splitting occurs when a specific memory, trauma or emotion gets triggered.
There are different types of splits, one of them being Rage split. Rage splits usually come with sudden outbursts of anger that seemingly come out of nowhere. When it occurs, the person might feel a tightness in their chest, their vision might narrow. They might experience a burning sensation in their chest as if their heart is trying to escape. This overwhelming emotion of anger can cause them to become infuriated with someone or something for no apparent reason. These episodes can cause impulsive actions, inappropriate speech and violent behaviour. It's almost like a cathartic release of emotion, and oftentimes the person doesn't remember the event fully, or only remembers it as a blur.
Now let's compare Midoriya's rage and outbursts and how they could be considered as splitting.
Scenario One: Izuku screaming his ass off saying GIVE ME MY KACCHAN BACK, charging at the obviously overpowered villains with two broken arms. Now, we can all agree that this was pretty out of character for him, and everyone was like Okay wtf. So the threat of losing Katsuki(which also directly correlates to his fear of abandonment) triggered him and made him impulsively and recklessly run towards the villains, even though he was completely defenseless.
Scenario Two: "Monoma, you b*tch". Midoriya literally unlocking a NEW QUIRK cause Monoma was talking shit about his FP, causing violent behaviour from him, getting tunnel vision, being completely OUT of it to the point they had to use Shinso's quirk to make him snap out of the episode. And now, this wasn't just about some rando insulting Bakugo. In my theory I explained how Monoma insulting Bakugo was essentially Monoma insulting Izuku's own values and identity. Because he has absorbed Bakugo's ideals, his values, his desire to win. Monoma talking shit about him felt like he just insulted who Izuku was as a person, as if he jabbed at the very essence of Izuku's dream, of his ideals. THAT was why it triggered him so bad.
Scenario Three: Midoriya vs Shigaraki 1. FP got stabbed, Midoriya immediately saw red and ran straight into the villain's hand without thinking about the consequences. He almost rage quit y'all. He raged so hard he bit the goddamn tendril like a freaking dog. He disassociated so hard he got tunnel vision and his eyes actually lit ablaze. Bruh.
Scenario There'stoomuchtokeepcount: Midoriya vs Shigaraki 2. Aka Deku AFK-ing in the middle of a freaking war and being like I'm out, y'all on your own now, after seeing FP's dead body. Tightness in his chest, unable to breathe, vision narrowed, in fact, completely blocked because of Smokescreen. A burning sensation in his chest as if his heart wanted to escape = Three of Swords. A cathartic release of emotion as his quirks released and gotten out of control. His biggest rage split moment right there.
But, rage isn't the only type of splitting that can occur. Another type is Isolation split.
Isolation splits usually stem from a deep-seated fear of abandonment. You may find yourself feeling unwelcome and unwanted, even in familiar environments such as school. You might have an urge to push people away, and often cut yourself off from others. For some, this means aggressively cutting people out of their lives for no apparent reason, for others, it might be a more subtle withdrawal from social groups and conversations. All the while hoping that someone will notice and ask them how they are doing. It might also include suppressing anger into anxiety, guilt, or self-hatred, identity dysmorphia, self-sabotaging relationships to be in control, stress-related paranoia, loss of contact with reality, and on-going feelings of emptiness.
Reminds me of a certain Vigilante Arc.
Isolation splits usually stem from fear of abandonment. In Izuku's case, why did he leave UA? Well, on the surface level, it was to protect his classmates from harm. But on a deeper level..
During his Vigilante Arc, he felt like he had to carry the burden of OFA all by himself. He felt like this responsibility that he carried made him a burden for others, including Katsuki, his friends, his family, and All Might. He feared that they would also realize this and feel like he's a burden, so he pushed them away, cut himself off, and left before they could leave him behind. Of course, this is not the truth, but this is what he believed. His feelings of anxiety towards the possibility of losing them in the war, his guilt of being a burden, his self-sabotaging is what made him believe that he is unwanted, unwelcome. During splits, the person views everything as either black or white, no in-between. Either all good, or all bad. He wanted to feel in control by leaving them behind for "their sake", almost maniacally insistent on being alone, like in the scene where All Might wanted to check on him and give him some food, but Deku ultimately ended up pushing him away and leaving him on the ground too.
During these episodes, people with BPD cannot logically think the situation through, they don't understand that their intense paranoia and belief that everyone hates them is just the reflection of their own feelings. During this episode, this Vigilante Arc(the episode didn't last for the entire arc, but there were probably higher and lower moments instead) he lost contact with reality and lived in a state of constant paranoia and a feeling of emptiness. He believed it was for the "better", but deep inside, that child inside of him just wanted someone to save him, to pull him back and not let go. Deep down he was just a child who just wanted some reassurance and to be validated. Like in his letter to Katsuki. Although we didn't see the whole letter, there were snippets of "Help me", and "thanks for everything" in it, reflecting Izuku's own feelings of "Please love me" and how even though he said he wanted to be alone, deep down he just wanted Katsuki to save him, to be there by his side.
Lastly, another symptom of BPD that can occur, albeit rarely, is the idolization, devaluation and ghosting of certain people, specifically the Favorite Person. This might just, technically, explain the ending of the manga and Chapter 431. Midoriya subconsciously idolized Katsuki his whole life seeing him as perfect. But as we all know, nobody is perfect. Midoriya had always viewed Kacchan as his image of victory, as someone who cannot lose. Yet, he has. The very person who he believed could never ever lose died on the battlefield. The person who believed was the strongest broke down crying in front of him saying he wants to be on his heels for the rest of his life. And what was Izuku's reaction?
Stop crying, this isn't like you.
Midoriya progressively went through the devaluation of Bakugo Katsuki's character, of his Favorite Person. Now, this is just a theory, because devaluation doesn't necessarily mean anything bad. It just means that he had stopped blindly idolizing Katsuki and realized that he is just a human too.
But in some cases of BPD, devaluation also comes with losing interest. Of finding a new favorite person who they see as their new "idol". Or to put it simply, Uraraka. Now, I don't want to go into more details because I am still very much hurt from Chapter 431, but we have seen an obvious ignorance, almost ghosting from Izuku's side towards Katsuki, something that is completely the opposite of how he would have acted before the war. Instead, he is looking at Ochaco as if she was his hero, and he sees her as a person that he wants to get to know more, to get closer to. Leaving Bakugo behind.
I spy an untreated BPD right there. But how could this disorder have developed in Midoriya? Well, it can be due to either genetics, or a series of traumatic events during childhood, for example emotional abuse, neglect, and going through feelings like being afraid, upset, unsupported or unvalidated.
Well emotional abuse came from the bullying. Neglect came from his father leaving. Being afraid was also because of the bullying and Bakugo. He felt unsupported by his own mother when it came to his dream of becoming a hero after being diagnosed quirkless. And he felt unvalidated his whole life simply because he didn't have a quirk. So yeah. I'm pretty sure these were all reasons that he has developed BPD, although not a severe case. If he actually turned into a villain and never got into UA, I imagine these symptoms could have worsened, making him extremely irritable, prone to snapping and having emotional outbursts and having an even more toxic codependency in his relationships.
I'm not saying that BPD is anything bad, I also have a friend who has BPD and it doesn't make you a bad person, people with BPD just simply experience emotions more intensely than others.
So yeah, I hope you guys enjoyed this analysis, and of course, let me know what you guys think!
#mha#bnha#my hero academia#boku no hero academia#bkdk#bakugou katsuki#midoriya izuku#bakugo#deku#mha analysis#bnha analysis#bpd
49 notes
·
View notes
Note
Hi. I have OCD (and various other mental illnesses) and have a character who has OCD. However, this character lives in a setting with aliens who are basically psychic with extra steps (they communicate via electromagnetic fields and can identify and interact with humans brain's electrical impulses.) What I'm wondering is should I make it so these aliens can like, easily distinguish some types of neurodiversity. i.e. they can easily recognize OCD character because his thought/brain patterns are more "repetitive?"
Personally I'm very torn on this. On one hand it feels validating because like a sort of "proof" that the difference is there and to ignore it is foolish. But at the same time it feels reductive to be, even indirectly, identified primarily by disability.
Possibly relevant, I don't think all neurodiversity should be easily identifiable by this species. Like I don't think autism could be identified (too much variation) but maybe something like DID could (parts of the brain field are somewhat "segregated")
Thank you for your ask! I think if the aliens have had contact with humans (or similar alien species) before, they might have some knowledge on what conditions are associated with certain thought patterns. If the aliens haven’t specifically spoken to humans on the matter they might make their own classifications which would probably look a lot different than ours (especially with how wide symptoms vary in one condition and how many symptoms overlap in so many conditions).
Your character doesn’t have to be only identified by their OCD, that may be what stands out at first to the aliens but if your character is well rounded they can be identified by their other traits. For example, when you first meet someone you might think of them as ‘the person with the interesting fashion sense,’ but as time goes on and you learn more about them you associate them with more traits.
Have a nice day!
Mod Rot
Hey!
I think that it's an interesting idea. I feel that it would make sense for an alien psychic creature to recognize that there are some "thinking patterns" that some humans sometimes have. As an example, I can see how they would pick up that certain people have a very specific Pure O pattern just from psychic-ing various people.
Depending on if/how the topic of mental health/neurodiversity exists in the alien society, they might not even necessarily consider it as such. If they don't recognize the pattern as a disorder, they might just think of it as a type of thinking that humans just have, like how they can perceive that some humans have brown hair while others are redheads (while readers would probably pick up on what is implied if they know anything about OCD). The alien aspect gives you a lot of possibilities.
As someone with OCD, I don't see it as "reducing" at all. It's true that his thoughts happen in a different manner than most peoples', but there's still content in them, right? His OCD is just affecting them, which is just how that works. The only exception here is that his OCD process itself is a part of the story - unless you decided to put his entire character's focus on how Weird and Exotic that is, you should be perfectly fine. I think it's an interesting part of worldbuilding to add.
If you are really worried about him being "identifiable" by his OCD, you can always make it so that different OCD types are seen as distinct (or, from an alien's perspective, perhaps even unrelated). For example, someone who's thought process is occupied with visual intrusive thoughts, versus one who is mainly having a specific compulsion-obsession pattern over and over, etc. - this will show OCD as the wide range that it is, and definitely not as "a label" that someone could just be instantly identified with. You can also make sure to show that every person's thought patterns are different to some degree (even if they're as neurotypical as it's humanly possible), and perhaps those with OCD's patterns are just hyperspecific enough to be recognized as more different; a "genre" of thought patterns of sorts. Because at the end of the day, there will also be people who don't have OCD who might share a few of these "OCD patterns" (and who don't fully get read as having it, maybe as adjacent at best), as well as two people who do have it and whose brain patterns don't match at any point, who still do get read as having OCD despite all that. It's a spectrum, afterall, so the brain patterns would be too.
I think that if you have OCD yourself, you can do basically anything you want with this. As I said, you have an interesting concept that you can tackle from a bunch of different angles, and I would love to see a take on it by an author with OCD.
mod Sasza
65 notes
·
View notes
Text
Drs. Ziyad Al-Aly, Akiko Iwasaki and Eric Topol, along with other acclaimed researchers, have issued a position statement on Long COVID published yesterday in the journal Nature Medicine. This document provides a much-needed perspective on the continued dangers posed by the “forever COVID” policy enshrined in official public health policies.
This important review comes on the heels of the recent publication in the New England Journal of Medicine (NEJM) of a reference frame for the chronic disease. It was developed by the National Academies of Sciences, Engineering, and Medicine (NASEM) Committee on Examining the Working Definition for Long COVID.
The 2024 NASEM Long COVID definition is: “Long COVID is an infection-associated chronic condition that occurs after SARS-CoV-2 infection and is present for at least 3 months as a continuous, relapsing and remitting, or progressive disease state that affects one or more organ systems.”
Most importantly, previous documentation of a COVID infection is not required for the diagnosis. The NASEM report explains: “By now, most persons worldwide have had at least one episode of acute SARS-CoV-2 infection. A requirement for proof of diagnosis could wrongly exclude many patients …”
This closer approximation to a scientific definition of long COVID is an important step towards educating the public and issuing a call for action to address the viral assault on the global population.
The authors of the study, published in Nature Medicine, should be commended for giving urgency to an issue that Dr. Al-Aly has rightly called “the elephant in the room.” Yet as sincere as these appeals may be to take Long COVID seriously, they will not convince the bourgeois authorities who have already dismissed warnings about the acute stage of COVID-19.
The complex multisystem disorder that can affect nearly every organ system after a COVID infection spares no one across the age spectrum. It appears that even fetuses in utero are at increased risk of respiratory ailments if the mother was infected during pregnancy.
Considering our rapidly developing comprehension of the long-term health consequences of COVID, thanks to the exemplary work being done by these scientists, the policy of mass infection demanded by the financial oligarchy assumes an even more sinister and deranged character.
The “cardinal” symptoms of Long COVID include brain fog and memory changes, fatigue, rapid sudden onset of heart rate, significant sleep disturbances, and immense sense of discomfort and illness after exerting oneself. There are no cures and, worse, no diagnostic tools that can tell someone they have Long COVID. Only recently have healthcare workers and researchers begun to identify treatments for Long COVID, but there is an absence of randomized trials to guide these decisions.
The authors note, “Care for people with Long COVID varies widely across settings and practitioners. It is often challenged by lack of widespread recognition and understanding of Long COVID among medical professionals, constrained resources and competing demands on healthcare systems still recovering from the shock of the pandemic, lack of standardized care pathways, lack of definitive diagnostic and treatment tools, and a general pervasive pandemic fatigue with an urge to ‘move on.’” The last point is a byproduct of the impact of forcing the population to accept COVID as a permanent fixture of society.
On top of the horrific impact it has on an individual person, on a social scale, mass Long COVID leads to loss of productivity, disruption in the workplace and increased risk of occupational-related injury or fatalities. Cognitive impairment, even after mild infections, is common, and there can be dire consequences for workers in occupations where the slightest error or inattention can be devastating: truck drivers, electricians, airline pilots, first responders and more. To say nothing of the impact on the wider community.
The report makes reference to the 2022 US Brookings Institute estimates on the figure of 2 million to 4 million US adults who were out of work because of Long COVID. Add to this the Minneapolis US Federal Reserve Bank report from July 2022, finding that people with Long COVID had a 10 percent poorer chance of being employed, and when they were, worked 25 to 50 percent less than uninfected individuals.
On a global scale, the authors wrote, “On the basis of all the available data, a conservative estimate of the annual global economic toll of Long COVID could be around $1 trillion, amounting to 1% of the 2024 global GDP.” Other estimates are even higher: An economic study from 2022 placed the cost of Long COVID at $3.7 trillion, or $11,000 per capita for the US alone, amounting to 17 percent of the gross domestic product (GDP).
Most compelling in the Al-Aly et al. review was their assessment of the global cumulative incidence of Long COVID, which until now had been opaque.
Basing their estimates on meta-regression studies that pooled all the available evidence, they estimated that figure for the first four years of the pandemic at 409 million cases of Long COVID. The authors remarked, “It is crucial to emphasize that these estimates only represent cases arising from symptomatic infections and are likely to be conservative. The actual incidence of Long COVID, including cases from asymptomatic infections or those with a broader range of symptoms, is expected to be higher.”
By comparison, among the most common ailments afflicting the world’s population, heart and circulatory issues, affect around 620 million. This means that in only four years, Long COVID, as a disease, has risen nearly to the top of the global list. Furthermore, Long COVID, as a multi-organ disease process, will only exacerbate noncommunicable and communicable diseases that arise in the future.
Placing these figures into context, this week, based on wastewater data, infection modelers estimate that COVID infections have once again climbed above 1 million cases per day, a staggering figure, to which the CDC is completely indifferent. COVID modeler Dr. Mike Hoerger of the Pandemic Mitigation Collaborative, in a social media discussion with this writer, said that presently, on average, every American has been infected between three or four times.
In a rare show of concern, the World Health Organization (WHO) announced that COVID-19 was spreading across the globe, with positivity rates in Europe above 20 percent. In opening their August 6, 2024, news report on COVID, they warned, “The UN health agency is also concerned that more severe variants of the coronavirus may soon be on the horizon.”
The European continent is swimming in a river of infection, like the unfortunate Olympic athletes sickened by swimming in the polluted Seine. And as we have already noted, the Olympics themselves have been a superspreader event.
Knowing that reinfections, more severe disease, and remaining unvaccinated, all raise the risk of Long COVID, one can only watch the current wave of infections with alarm. These will be given further fuel as schools and universities begin to open their doors later this month. Furthermore, global COVID vaccinations have essentially come to a halt. Long COVID is the long tail of the ongoing pandemic that has no end.
Unique in the report by Dr. Al-Aly and colleagues is the raising of social issues affecting the global impact of Long COVID. In support of the UN Foundation’s Sustainable Development Goals (SDG), they raise the need to end poverty and hunger, improve access to health, provide quality education, improve working conditions and reduce inequalities. They also call for funding to support coordinated interdisciplinary research on Long COVID on a global footing.
The recognition of the social issues that need to be addressed is an important insight. However, the appeal to existing public health institutions and political processes to heed their warnings will not bear any fruit.
First and foremost, the “forever COVID” policy is not a misguided public health construct. It is a calculated and coordinated approach to ensure pandemic threats would not impede the unfettered accumulation of surplus value off the backs of the working class. If the sick and infirm fall by the wayside, these social losses are seen as financial gains by the class that seeks to extract from the working class every minute of their potential labor power and avoid the cost of their “lingering on.”
In this regard, Senator Bernie Sanders’ introduction of legislation titled the “Long COVID Research Moonshot Act of 2024” is simply political theater, aimed at deluding the public into thinking that the capitalist system is capable of reform. The bill would provide a paltry $1 billion in mandatory funding per year for 10 years to the National Institutes of Health (NIH) to support Long COVID research.
To think this legislation will see the light of day while social spending is being slashed to fund the forever wars is to look at the world through very thick rose-colored glasses. Those researchers and public health advocates who wish to promote the application of the scientific principles that guide their own work must recognize the necessity for a broader social perspective.
To address Long COVID, as the world Trotskyist movement has demanded, one must begin by eliminating COVID across the world. Despite the dismissal of such a perspective by capitalist governments and the corporate media, zero COVID is and remains the only viable solution.
Only one social class is capable of taking up and fighting for such a policy: the international working class. The fight against COVID and future pandemics, like the looming H5N1, must be integrated into the revolutionary mobilization of the working class against the capitalist system and the establishment of a socialist society, in which human needs, including the most basic concerns of healthy life, will be the basis of social policy, not private profit.
#long covid#covid#mask up#pandemic#covid 19#wear a mask#sars cov 2#coronavirus#still coviding#public health#wear a respirator
32 notes
·
View notes
Text
Switching Tips and Info
Hello! We’ve often said here that for our system, switching is involuntary and happens automatically or with the help of our gatekeeper. However, we often get asked here about switching, how it works, how to practice switching, and how to switch for the very first time. In general, we’re probably unequipped to confidently answer these questions. But we’ve decided to put together this post with information we’ve picked up from therapy, research, and learning from other systems. We hope this can help you and your system learn to switch more effortlessly!
Disclaimer: We are not an expert or clinician by any stretch of the word! We are one DID system sharing our experience and information we’ve picked up during our time in treatment and system spaces. This post comes from the perspective of a system with DID, though much of this advice could be potentially useful for all sorts of systems!
What is switching?
Switching is a common occurrence in systems when one headmate swaps places with another in order to perceive and interact with the world. Systems of all sorts can switch, not just those with dissociative disorders like DID or OSDD! Switching can look incredibly different from system to system, and may vary based on a wide variety of factors such as:
System origin
Previous history with switching
Degree of dissociative barriers
Comfort levels with fronting and switching for each headmate
The presence of a system manager or gatekeeper
Safety of the system overall
And more!
Do all systems switch?
No, not every system wants to switch or is capable of switching! Many systems exist with one primary fronter and many headmates who either cofront, are coconscious, or never front to experience the outside world at all. Switching is not a requirement to be a system, and it’s not even a requirement to have a dissociative disorder.
Many systems may find that headmates have switched before without noticing it! Before a system’s “syscovery,” headmates may lose time, experience identity shifts, or interact with other system members without ever realizing that they’re plural. In fact, an overwhelming majority of systems with disorders like DID and OSDD are covert, meaning their switches and other symptoms often go unnoticed by other people or the systems themselves!
How can I switch with my headmates?
We don’t have any surefire way to guarantee switching, as every system is unique and no two systems function in exactly the same way! However, here are some ideas for you and your headmates to try in order to help a switch occur.
1. Open communication
Communicate with as many headmates as you can on a regular basis. Keep an open dialogue, and talk to your headmates about fronting, what that might look like for them, and any worries they have about potentially fronting in the future. Try to address each headmate’s fears and concerns to the best of your ability before expecting them to front. Imagine together what it might look like for other headmates to front. Try to understand what happens to headmates in your system who aren’t fronting: do they enter your system’s headspace/inner world? Do they stop fully existing or enter a sort of stasis? Are they still able to perceive the outside world at all? Having a stable, steady line of communication and an understanding of how your system works can help make it easier to allow other headmates to front when the time comes!
2. Seek out a gatekeeper or system manager
Many, but not all, systems have members whose role is specifically to manage who fronts and control switches. Our own system has a gatekeeper who handles the majority of our switches! If you haven’t already, try to learn whether or not your system already has an established gatekeeper. If you do, establishing a connection with that headmate and communicating with them will be essential for switching in the future.
If your system doesn’t have a gatekeeper/manager, that’s fine! A headmate with this role is not required for system to experience switches. For those who do have them, however, cooperating with managers and gatekeepers can help make switching a smoother, more painless process!
3. Ensure safety
Don’t attempt to switch if your system is not 100% safe, and only try to switch after all headmates involved feel comfortable and secure. NEVER try to force a headmate to switch who doesn’t want to. Respect each other’s boundaries and rights to personal autonomy.
When you’re ready to try and purposefully switch, do so in a safe, comfortable, secluded environment. Try to limit distractions and opportunities for interruptions. Check in with headmates that you have access to, and ensure that everyone feels safe and comfortable before attempting to switch.
For minors, traumagenic systems, and those who currently live with abusers or those who have harmed them: it may be for the best to not attempt to switch until you’re in a situation where you are distanced from those who have caused you harm (be them parents, friends, loved ones, or anyone else). Unfortunately for many systems, this may mean waiting until you have moved out of your family’s home in order to put some space between you and your system’s abusers.
Trying to switch when you’re not 100% sure of your system’s safety could absolutely cause more harm than good! The safety and well-being of your system is more important than providing headmates with opportunities to purposefully switch. There will be plenty of time in your future to learn more about your system and attempt to manage switches! Until then, it’s probably best to allow your system to function in ways that ensure your safety and the safety of your headmates.
4. Use positive triggers
Positive triggers are external stimuli that can help bring certain headmates closer to the front by reminding the system about that headmate and what they enjoy. Having a wide range of positive triggers at your disposal can help make it easier to get a headmate to switch with you! Here are some examples of what positive triggers can look like:
Music for each headmate, including playlists, albums, artists, and songs
Stimboards, moodboards, inspiration boards, and other collections of images that speak out to each headmate
Cooking, preparing, or eating a food, snack, or beverage that a particular headmate enjoys
Engaging with hobbies, media, and activities that a particular headmate is known to like
And more! Get creative with your system and brainstorm different positive triggers you can incorporate into your lives in order to help facilitate switches in the future!
5. Manage expectations
Unfortunately, not all systems are able to switch. Some hosts and other frontstuck headmates may never be able to fully leave the front. Cofronting with another headmate and allowing them to make decisions and treat the body as their own can be a great way to allow other system members to front, even if it’s not a full-fledged “switch.” Switching can look incredibly different for different systems, and even for different headmates in the same system! So don’t be too discouraged if you or your frontstuck members aren’t able to switch out fully - cofronting and being coconscious are both valid ways for other headmates to experience the world.
Where can I learn more about switching?
There’s lots of information out there to help all kinds of systems start learning about or managing switches! Here are some links to websites where you can learn more.
Note: some sites which are geared towards created, spontaneous, or endogenic systems may suggest purposeful dissociation as a way to trigger a switch. While this may be useful for some systems, adding more dissociation to the lives of those already struggling with dissociative disorders is a very bad idea and should be avoided! So if you are diagnosed with a dissociative disorder (DID, OSDD, DPDR, etc.), suspect you may have a dissociative disorder, or suspect your system is trauma-formed, it may be best to avoid following advice from sites aimed towards paromacers, those with thoughtforms, and nontraumagenic systems. For everyone’s convenience, we have starred (*) links to guides which involve purposeful dissociation so systems who already have trouble with dissociation can avoid them! If you’re not sure whether or not your system has dissociation issues, it’s best to PLAY IT SAFE and avoid these kinds of guides. Please use critical thinking and your own discretion when reading about switching online!
Terminology note: some of these sites use “tulpa” language, which is known to be racist and culturally appropriative. Please keep this in mind when browsing these sites. In our personal life, we use “paro/paromancy” language instead to avoid causing further harm to marginalized groups.
Intentional Switching (DID) from DIS-SOS
Switching and Passive Influence from DID-Research.org
*Fuliam’s Guide on how to switch from Tulpa.info*
*Malfael’s Guide to Switching from Tulpanomicon*
Our own resource post for questioning systems has lots of links to resources on dissociative disorders and other forms of plurality, many of which may have sections or advice on switching!
Questions? Comments? Something we missed?
We could write whole books on the many different aspects of switching, and how switches can vary from system to system and headmate to headmate. We’re sorry if we’ve left something out here that you or your system thinks is important! This post didn’t touch on passive influence, rapid switching, physical symptoms of switching, and many other switching-related topics. This is just a general overview with some advice on switching intentionally and voluntarily!
If you have any further questions, feel free to comment on this post or send us an ask and we’d be happy to answer to the best of our ability! We may not have all the answers, but we’re happy to share what we know. If you made it this far, thanks so much for reading! Stay well, and have a great day!
#multiplicity#plurality#pluralgang#actuallyplural#long post#dissociative identity disorder#other specified dissociative disorder#partial did#osdd#did#p did#switching#trauma mention#abuse mention
125 notes
·
View notes
Text
Leptospirosis: What it is, what it does, and how you can protect yourself and your pets.
People always have questions about leptospirosis (lepto) when they come into the clinic, especially in regards to the vaccine. This post will hopefully clear up those questions or any confusion regarding lepto and its vaccine, and why it's so serious. The information in this post comes from my formal education as a LVT, as well as other sources including the CDC, PAHO, and AVMA. If I missed anything or you see something that's incorrect, please let me know!
First and foremost: What is leptospirosis?
Leptospirosis is a bacterial disease that effects human and non-human animals. It's caused by bacteria in the genus Leptospira. In humans, it can cause a wide range of symptoms that can be very general. This leads to misdiagnoses. Animals such as dogs, livestock, and certain wildlife are all susceptible to infection.
How is leptospirosis spread?
Lepto is most often spread through contact with the urine of an infected animal. This is especially the case (but not the only case) with wild rodents. Infected dogs can seem healthy, but still pass the bacteria on in their urine. In urine-soaked soil, the bacteria can survive for weeks to months.
Dogs typically become infected when their mucous membranes or open wounds come into contact with urine or urine contaminated surfaces (like soil or water). Infection can also be spread through urine-contaminated bedding or food, or the tissues from the carcass of an infected animal. There have been rare instances where lepto has been transmitted by bite or breeding. A pregnant dog who is infected may pass the bacteria to her puppies through the placenta.
Humans contract lepto pretty much the same way: through contact with urine from an infected animal or urine-contaminated surfaces.
What are the signs and symptoms?
In humans:
High fever
Headache and muscle aches
Chills
Jaundice
Vomiting and diarrhea
Redness of the eyes
Abdominal pain
Rash
Humans can also be asymptomatic, which is particularly concerning. It usually takes anywhere from 2 days to 4 weeks post-exposure to the infection source before any symptoms are displayed. The illness begins abruptly and it may occur in 2 phases. The first phase is where you will see a lot of the general symptoms listed above. The person infected may recover for a period of time, but become ill again. The second phase is more severe, leading to kidney or liver failure, and possible meningitis. The illness can last a few days to 3 weeks or longer.
Without treatment, recovery can take several months.
In dogs:
Signs and symptoms may vary slightly depending on the strain of the infected bacteria. The signs are also very general in dogs, but the most common ones include:
Loss of appetite
Vomiting and diarrhea
Lethargy
Abdominal pain
Jaundice
Dehydration
Increased thirst and urination
Weight loss
Stiffness or muscle pain
The disease can also progress to kidney and liver failure in dogs, with damage to other organ systems also noted in the literature. Lepto can also cause bleeding disorders, which can lead to blood in urine, vomit, feces, or saliva, and petechiae on the mucous membranes or light colored skin.
Who is most at risk?
For humans, those who are most at risk include those who work with animals or outdoors where you come into contact with wildlife. The Pan American Health Organization (PAHO) also mentions that sewer workers and military personnel are at-risk populations. Farmers (and generally people who work with livestock) also make the list, as do veterinarians, veterinary technicians, and veterinary assistants.
For dogs, it's all of them. "All dogs are at risk of leptospirosis, regardless of age, breed, lifestyle, geographic location, time of year, and other factors." (source: AVMA)
Situations that can increase the risk of your dog contracting leptospirosis are listed below:
Exposure to drinking from slow-moving or stagnant water sources (this includes puddles)
Roaming on rural property
Exposure to wild animals or farm animals, even if it's only in the yard
Contact with other dogs (such as in urban areas, dog parks, boarding, or training facilities.
How is leptospirosis treated and diagnosed?
Disclaimer: I am NOT a medical doctor or DVM, but I am an LVT. If you think you're experiencing these symptoms, PLEASE go see your doctor. If you think your dog or any of your other animals are experiencing these symptoms, PLEASE take them to your vet.
Diagnosis in non-human animals:
Unfortunately, routine blood tests alone cannot diagnose leptospirosis. That's why it's important for your vet to use all information available to them (i.e. diagnostics, signs and symptoms, lifestyle, etc). There WILL be abnormal results for blood work, most likely high liver and/or kidney values and high white blood cell count. There are specific tests available for diagnosing lepto, such as the DNA-PCR and MAT tests. Both may be needed to reach or confirm a diagnosis. False negatives are possible, so your pet may be treated as if they have leptospirosis, even if the test results are negative. False positives are exceedingly rare.
Diagnosis in humans:
Leptospirosis is diagnosed in a similar fashion in humans. A physical exam, blood work, and urinalysis will likely be run. The same style of tests are used: DNA-PCR and MAT.
Treatment in non-human animals:
Leptospirosis is treated with antibiotics and supportive care. Doxycycline is most commonly used, and will likely be prescribed for 2 weeks or more. Supportive care includes hospitalization with IV fluids and management of electrolyte levels. Additional medications and procedures may be necessary.
Treatment in humans:
The treatment is similar in humans, with antibiotics (usually doxycycline). Your doctor may also suggest to take ibuprofen and monitor yourself at home for less severe cases. If the case is severe, then you'll likely spend time in the hospital. Additional medications or procedures may also be necessary.
Outcomes:
In non-human animals:
Leptospirosis is responsive to treatment with antibiotics. Complete recovery is possible, but some animals that survive may be left with chronic kidney and liver disease. Some animals may not survive if the infection has gotten to the point where it causes severe organ damage or the ability of blood to form clots.
In humans:
You can survive leptospirosis. Most cases have either very mild symptoms that go away on their own, or none at all. Without treatment, leptospirosis can cause kidney damage, meningitis, liver failure, trouble breathing, and even death. PLEASE go see a doctor if you think you're experiencing any of these symptoms, especially together.
Prevention
How can you prevent infection and protect your pets?
For dogs, there's the leptospirosis vaccine. This is an annual vaccine that vaccinates against multiple strains of Leptospira. If you're worried about your dog having a vaccine reaction, let your vet know and they can administer an injection of diphenhydramine (generic benadryl) beforehand, OR you can ask them what the appropriate dose is for your dog and give them the respective amount at home (in tablets or liquid). Vaccine reactions are uncommon, but if they do happen, it's usually immediately after exposure to the vaccine. You can ask to stick around in the lobby/waiting area of your vet clinic for a few extra minutes if you're still concerned.
Limit your dog's access to standing water. Don't let them drink from it. Prevent rodent problems where you can by properly storing food items in appropriate containers, securing your garbage, and patching up any access points into your house if you see them. Try to avoid contact with wildlife, when possible.
For humans, the recommendations remain similar. Don't wade or swim in stagnant water, ESPECIALLY if you have open wounds. Avoid contact with wildlife. WASH YOUR HANDS, often and appropriately. USE PPE if you work in a veterinary setting and properly clean and disinfect surfaces and equipment. Make sure you know or research the area that you're in if you like swimming and boating. Check to see if there have been any recent lepto infections. Cover your scrapes and wounds with waterproof bandages and wear water shoes if possible.
I hope this post answered a lot of your questions! Thanks for reading.
Sources under the cut.
Sources:
#animals#pets#dogs#leptospirosis#zoonotic diseases#infectious diseases#vet med#vetblr#petblr#dogblr#my posts
48 notes
·
View notes
Note
Hi, there, I was looking into willogenic systems and taking about them with my partner (who is the host of a traumagenic system), and they were really confused as to why someone would ever want to be part of system.
I was hoping you’d be able to elaborate, thanks
(This isn’t supposed to be any sort of an attack, just curiosity)
Thanks for the genuine curiosity! It is a confusing idea to many traumagenic systems because so often their systems are deeply intertwined with their trauma.
What's important to realize is that systems are widely varied, and people are widely varied. With the definition I use, the only requirement for being a system is being a group of people in one body. In many disordered traumagenic systems (especially ones not very far into recovery), this comes inherently bundled with stuff like amnesia, time loss, uncontrollable switches, depersonalization/derealization, loss of sense of self, flashbacks, trauma responses, difficulty in communication between alters, etc.
But this is not a universal thing that all systems experience. Not even all disordered systems. Hell, think DID vs OSDD-1. OSDD-1 is diagnosed because they're missing a part of the criteria for DID, either amnesia or distinct alters. And within a single diagnosis you can many different presentations. You may have one DID system who has alters who can all easily talk to one another, and a different DID system who has never heard their alters once in their life.
With that in mind, now think about a system that doesn't have the symptoms of a CDD. A system where you can remember what the others did without any dissociation, where past memories are shared equally, where communication is near seamless. That is the experience most willogenic, parogenic, and tulpamancy systems will have. While certainly not universal, most created systems experience levels of dissociation and amnesia similar to the general population. (I experience higher than average dissociation and amnesia, but that is not due to being a system and it does not affect my system's functions directly)
In my experience being a created system? My headmates know me better than I know myself, and I have never before felt internal love like I've felt from my headmates. My headmates have brought me out of deep depressive funks in 5 seconds flat. I have many different perspectives to draw from when making a decision. I feel more whole, more complete now as a system. I understand myself more and am more certain in my identity. I find that I am more introspective and at ease with myself.
But, like I said earlier, systems vary and people vary. Not everyone likes being more than one. I've met created systems whose plurality scares them and ones who regret becoming a system. On the flipside, my boyfriend has DID and I genuinely don't think they'd become a singlet for anything, including never having gone through their trauma. Some people just want to be systems, and some people just want to be singlets. Not all systems want to be systems and not all singlets want to be singlets.
Your partner may not want to be part of a system, even if they didn't have any disordered symptoms, and thats perfectly okay! I strongly believe any systems who want to become singlets should be supported. But, their experiences are not universal, and neither is mine for that matter. Not everyone wants the same thing.
I hope this helps your partner understand why someone might want to be part of a system! If they have more questions or would like to know more, I'm more than willing to help.
#ask#anon ask#question ask#created system#tulpamancy#willogenic#parogenic#plural#plural system#system#pluralgang#plurality
14 notes
·
View notes
Text
Adrien Agreste and Borderline Personality Disorder
DISCLAIMER: I've been a bit low on spoons this week, so I haven't gathered as much evidence as I probably could have. Also, I am but a humble student in clinical psychology. This is mainly a thought compilation for @moonieratty!
To introduce the topic, without going into it too much, personality is described by features and behavioral patterns, or traits, consistent across situations and across time. Personality disorders are therefore enduring patterns of highly maladaptive traits evaluated in personal and sociocultural context (Dozois, 2019, p. 290).
Like other disorders, personality disorders have diagnostic criteria. The DSM is used primarily for diagnosis in the US and Canada while the ICD is used more widely in Europe and other places. I'm more familiar with the DSM, but I've included a brief section on the ICD to be comprehensive. It ended up a bit longer than anticipated, so let's go below the cut. Warning for discussions of abuse, self harm, and suicide, and a brief mention of substance use.
Overview of Borderline Personality Disorder
BPD is prevalent in a small percentage of the population, about 1-2% by varying estimates, and is characterized by instability across domains of emotions, identity, interpersonal relationships, and behavior. Its onset is usually in late adolescence or early adulthood and symptoms may diminish with age, after one's thirties or forties, especially with therapeutic intervention. Along with ASPD, it has been the focus of a lot of clinical research; it is unfortunately associated with high rates of non-suicidal self-injury and suicide (APA, 2022, pp. 754–755; Dozois, 2019, pp. 308–309).
Etiological factors for BPD include both biological and environmental disturbances. Of note to our discussion is the heightened risk for BPD in cases of child abuse or neglect, as well as growing up with another family member with a serious mental health condition (NHS, 2022). It's been well established that Gabriel is emotionally neglectful if not outright abusive toward Adrien in multiple ways, so this is a clear risk factor. In addition, although I won't argue definitively for Gabriel having a psychological condition, he did keep Emilie's body in the basement, so there is clearly some kind of disturbance going on.
From a cognitive-behavioral perspective, Linehan argues that BPD stems from families who consistently invalidate childhood emotional experiences and "oversimplify the ease with which life's problems can be solved," which may cause children to learn to seek attention and communicate with others through emotional outbursts (Dozois, 2019, p. 297). This rings true for Adrien and Gabriel as well.
I have to apologize for my son, Ladybug, he's like his mother. Way too overly dramatic. (Jackady)
It doesn't seem like this is the first time Gabriel has thought this, and labeling an emotional reaction as being overly dramatic is very much invalidation of it. As for emotional outbursts, Adrien has had quite a few, mostly as Chat Noir. More on this later.
To round out this first section, attachment theory proposes a connection between poor parent-child attachments and BPD relationship difficulties. Specifically, maladaptive behavior in relationships may stem from childhood development of an anxious-ambivalent attachment style, where intense fears of abandonment interfere with a strong desire for intimacy (Dozois, 2019, p. 310). You can clearly see this in Chat Noir's relationship with Ladybug, and I'm sure other people have discussed Adrien's attachment style more in depth, but suffice to say I think this is an apt description.
Argument from DSM-5-TR
In the DSM, personality disorders are primarily diagnosed on a categorical model. There are a few general criteria which I won't be going into, but I will highlight that personality disorders are stable and pervasive, and would be diagnosed only if they were leading to significant distress or dysfunction. Adrien's mental state is not great, so the latter shouldn't be a problem, but this show does not always pay attention to consistency, so I'm going to be speculating some. Everything in this section is cited to the relevant DSM entry unless otherwise stated.
The DSM characterizes BPD with instability in relationships, self image, and affects, as well as marked impulsivity. It has no exclusion criteria, so BPD can be and frequently is comorbid with other disorders like mood disorders, PTSD, and ADHD. Of the below criteria, five need to be met in order for a diagnosis to be made.
Frantic efforts to avoid real or imagined abandonment
Hey, where're you going? . . . So you're allowed to know her true identity, but I'm not? (Syren)
You're not really replacing me with a turtle, are you? (Anansi)
A lot of people have delved into Adrien's abandonment issues, which feature most prominently in his relationship with Ladybug. His fears of being replaced result in him seeking reassurance from Ladybug, and he can lash out if he does not receive the response he hopes for. Ladybug is his world, and he wants to be hers, so anything infringing on that feels to him like a threat of being abandoned, and he does not like it very much.
Impulsive behaviors like giving up his ring can be interpreted under this lens: he can avoid abandonment by doing the abandoning first. Then it will be him leaving, and not the other way around.
I also interpret Adrien's nightmare (Le Marchand de Sable) as being a fear of being alone as much as it is a fear of being trapped.
Unstable and intense interpersonal relationships alternating between extremes of idealization and devaluation
We'll be united, more powerful and free. We'll defeat Hawk Moth, then we can both run away to an island! Far away from everything. We will live off nothing but fruits, and we will have a little pet hamster and we will name it— (Le Patineur)
I just can't do this anymore. I give up… on everything. Even you . . . If I become Chat Noir again, Ladybug will just end up rejecting me, over and over. (Kuro Neko)
Even though Adrien mostly keeps his head on straight regarding what he's owed and not owed by other people, his relationship with Ladybug is full of highs and lows. He thinks Ladybug is the most amazing girl, but this can recoil quickly into feeling as though Ladybug doesn't care about him enough or isn't meeting his needs.
Furthermore, he developed this idealization of Ladybug as a potential lover or caregiver at one of their first meetings (Cœur de Pierre), and continually sought to spend time together and share the intimate details of their secret identities early on. These are all common to individuals with BPD, as is the switch from idealization to feeling as if the other person "does not care enough, does not give enough, or is not 'there' enough." Ladybug is the only person Adrien consistently projects this instability and intensity on, which might be something interesting to explore.
Identity disturbance: unstable self image or sense of self
When I was a kid, I always wanted to be what my parents wanted me to be! (Exauceur)
But, does that mean Chat Noir is who I really am? Deep down inside? (Kuro Neko)
With all the secret identities, it isn't surprising that Adrien fits this criterion, but canon even explicitly draws a link between Adrien's unstable sense of self and his childhood experiences. He doesn't know who he is, and he distracts from this by being Chat Noir, only to struggle even more when he feels useless and underlooked as his hero self. His behavior shifts dramatically between trying to prove himself with grand gestures and refusing to participate or lashing out. There is definitely something to discuss on this front.
Impulsivity in at least two potentially self-damaging areas
Giving you some extra time . . . I trust you to bring me back, m'lady. (Gamer 2.0)
There are only two liars left in Paris and one of them knows the ultimate way to catch her attention . . . Crazy about you, m'lady. (Mensonge)
This is walking a thin line between impulsivity and suicidal behavior, which would be excluded from this criterion, but I'll list self sacrifice here because I can see an argument for Chat Noir's impulsive behaviors being out of love or the desire to be useful. There may still be some self injurious intent or euphoria, but Chat Noir does have faith in Ladybug to bring him back eventually. Nevertheless, this is impulsive and unhealthy. Chat Noir jumps too quickly to this option to have thought it through.
I can't think of another area, because Adrien isn't old enough for reckless driving, spending, substance use, or sex. This is also a kids' show. Just presenting these options for fanfiction writers out there.
Recurrent suicidal or self mutilating behavior, gestures, or threats
I... I don't know what to do! (Chat Blanc)
This is all our fault . . . Cataclysm. (Culpabysse)
By itself, what happened in Chat Blanc would not be solid evidence, as that was an unprecedentedly traumatic situation. Combined with Culpabysse, though, there is a strong case to be made for at least passive suicidality for this to be able to come up as an option.
You could also interpret the self sacrifice in this category. Suicidal behavior in individuals with BPD is often preempted by fears of rejection or abandonment, so an interesting analysis could be made on this front.
Affective instability due to marked reactivity of mood
He's still only thinking of himself! I just want this terrible day to be over and done with! I hate Christmas! (Pire Noël)
Sorry! Sorry! I didn't mean to make you so mad. I get it. You're sick of me . . . No one can help me, Kagami. (Glaciator 2)
Adrien's prolonged episodes of anger and despair reflect a high reactivity to emotional stressors, especially interpersonal ones. In general, he just doesn't feel very well unless something is actively bringing him joy. Most of his outbursts are brief, though, and I will discuss them as part of a later criterion.
Chronic feelings of emptiness
I'm not Adrien, so I wouldn't know if this is the case, but I can say he has experienced at least one depressive episode (Kuro Neko) and emptiness would not be unfamiliar. You can look at him and decide.
Inappropriate, intense anger or difficulty controlling anger
How was your amazing evening with your "friends"? . . . What do you think? (Glaciator)
Why not? No one'll know if I quit. No one'll care! (Syren)
A two-person plan?! There's only one two-person plan, and that's Ladybug and me! (Sentibulleur)
Give me a break, Miss "I can't even come up with a superhero name"! (Hack-San)
Anger in individuals with BPD can manifest as bitterness, sarcasm, or recurrent verbal outbursts, which Chat Noir absolutely exemplifies. These outbursts are often followed by feelings of shame or guilt and contribute to a feeling of being bad. Chat Noir apologizes after being harsh in Glaciator, and I wouldn't be surprised if he felt badly about the other times. Again, these outbursts are often precipitated by interpersonal fears and perceived threats of abandonment. Unlike other symptoms, this specific one tends to be unique to BPD.
Transient, stress-related paranoid ideation or severe dissociation
I cannot recall any evidence for this but headcanon away, my friends.
All in all, I think Adrien has a strong case for BPD presentation according to the DSM. Canon is not always consistent, but I think it presents an interesting and mostly coherent narrative for this lens. From this perspective, Adrien's behavior reflects a deep intolerance of being alone and a dependence on other people to define the self.
As a corollary, BPD behavioral patterns are frequently linked to self sabotage and self undermining right when a goal is about to be realized, which could manifest as dropping out of school right before graduating or ending a relationship when it seems to be going well. Food for thought. Individuals with BPD may also feel more secure with transitional objects like pets than with interpersonal relationships, which could reflect in Adrien's relationship with Plagg.
To add some subjective understanding to this clinical mumbo jumbo, I've added a source of genuine BPD experiences below (Mind, 2022).
Argument from ICD-11
With the release of the ICD-11, a dimensional model for diagnosis of personality disorders became the new standard. What this means is that individuals are no longer labeled as having 'histrionic' or 'dependent' or, indeed, 'borderline' personality disorders, but are rather assessed as having any form of personality disorder on a sliding scale of severity and with trait domain specifiers (Swales, 2022). To put it more simply, people are diagnosed only with a general personality disorder or personality difficulty which can be optionally specified as deviating on one of the personality traits in the Big Five model, which is well established in personality psychology.
This move has several benefits. Stigmatization related to particular personality disorders can be reduced, and differential diagnosis and comorbidity between personality disorders becomes irrelevant. However, people retain access to treatment and support. Evidence-based treatments like dialectical behavior therapy are particularly well established and crucial for BPD; for this pragmatic purpose, the ICD contains one additional specifier for borderline pattern personality disorder (Bach et al., 2022; Swales, 2022).
The DSM and ICD are designed to be compatible with each other in many ways, and in this case, the borderline specifier in the ICD is directly lifted from the criterion of the DSM (WHO, 2023, 6D11.5). Based on our previous discussion, Adrien would be equally qualified for a diagnosis in France. I would likely describe his personality disorder with moderate severity, where multiple areas of functioning are affected and self harming behaviors may be present, but not all areas or relationships may be equally impacted and traits are not as rigid and inflexible (WHO, 2023, 6D10.0–6D10.2).
Interestingly, the ICD includes three additional manifestations of borderline pattern which are optional and may vary across time (WHO, 2023, 6D11.5).
A view of the self as inadequate, bad, guilty, disgusting, and contemptible
An experience of the self as profoundly different and isolated from other people; a painful sense of alienation and pervasive loneliness
Proneness to rejection hypersensitivity; problems in establishing and maintaining appropriate levels of trust in relationships; frequent misinterpretation of social signals
I'm fascinated by the number of adjectives in here. I simplified very slightly, as I did with the DSM criteria, but I had to keep all these adjectives. Anyway, I won't elaborate for too many more paragraphs, so let's say sentimonster moment and leave it at that. I will spare you my mirrored Félix essay. For now.
Qualifications and Limitations
First of all, Adrien is a teenager. The distinguishing factor between a personality disorder and regular adolescent difficulties would be longevity and identity concerns beyond his developmental phase (APA, 2022, p. 758). Second of all, Adrien has a uniquely terrible home life and magical problems. Some of his behaviors could be normal considering his experiences and sociocultural context, and this matters when it comes to psychological evaluation. Take everything with a grain of salt!
More generally, the categorical model of the DSM has several issues, not to mention diagnostic issues related to culture, gender, and stigma. Some but not all of these issues are addressed by the dimensional model it includes in a later section, which shares theoretical foundations with the model of personality disorders in the ICD. Even so, issues remain. Diagnosis, access to treatment, and political statements are intrinsically linked in complex ways. I won't get into all of the nuances, but be safe, remember this is a fictional character, and keep an open mind.
REFERENCES:
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). https://doi.org/10.1176/appi.books.9780890425787
Bach, B., Kramer, U., Doering, S., di Giacomo, E., Hutsebaut, J., Kaera, A., De Panfilis, C., Schmahl, C., Swales, M., Taubner, S., & Renneberg, B. (2022). The ICD-11 classification of personality disorders: A European perspective on challenges and opportunities. Borderline Personality Disorder and Emotion Dysregulation, 9(1). https://doi.org/10.1186/s40479-022-00182-0
Dozois, D. J. A. (2019). Abnormal psychology: Perspectives (6th ed.). Pearson.
Mind. (2022, September). What does BPD feel like? https://www.mind.org.uk/information-support/types-of-mental-health-problems/borderline-personality-disorder-bpd/experiences-of-bpd/
National Health Service. (2022, November 4). Causes - Borderline personality disorder. https://www.nhs.uk/mental-health/conditions/borderline-personality-disorder/causes/
Swales, M. A. (2022). Personality disorder diagnoses in ICD-11: Transforming conceptualisations and practice. Clinical Psychology in Europe, 4(Special Issue). https://doi.org/10.32872/cpe.9635
World Health Organization. (2023). International statistical classification of diseases and related health problems (11th ed.). https://icd.who.int/
#miraculous ladybug#adrien agreste#ml meta#don't worry i read through far more sources than listed here#it's just standard citation procedure to include only in-text references and not readings for general subject comprehension#🌃#🌖#i'm using a hybrid parenthetical citation model which i think is most efficient and informative so just note this down#i can't believe i referenced kuro neko three times... what an episode#ml simon says#ml syren#ml anansi#ml sandboy#ml frozer#ml kuro neko#ml stoneheart#ml wishmaker#ml gamer 2.0#ml lies#ml chat blanc#ml guiltrip#ml santa claws#ml glaciator 2#ml glaciator#ml sentibubbler#ml hack san
111 notes
·
View notes
Note
ok I was gonna ask about your charlie scully one (still am I guess lol) but I must know your thoughts on the autism question, a while back there was a fandom-wide twitter spat over whether or not mulder and scully were autistic, and I was leaning against it but that was before I figured that out about myself, and most of my moots are in favor of it, and idk really what to think lol so your insight would be much appreciated🙏🏻 (also if I wasn’t so goddamn busy I would do all of that research for you lmao)
You should do it!! Even if one day my project comes to fruition!
My leanings on the autism question: no. But I'd have to prove or disprove my own theory if I wrote up that post; and in order to do that, I'd have to have a clearer understanding of the diagnosis, its symptoms (and symptoms that are commonly misdiagnosed), and its identifiable characteristics.
The "problem" is: the new understanding of autism and other disorders are now framed on a spectrum. In order for me to break down the topic, I'd have to ingest lots and lots of autism content from clinically licensed professionals and hear what they look for, broadly, when forming a diagnosis; then, I'd have to search up what the fandom perceives Mulder and Scully's autistic traits to be; then, I'd have to compare and contrast the strength of each claim; then I'd have to balance the whole. Currently, I'm ingesting new autistic creators that are breaking down barriers of what autism is perceived to be (and that's been helpful); and I have a few other licensed professionals I'd need to catch up on (one who even has the diagnosis herself.) In short: tons of layman research.
More importantly: who would be interested in my post, realistically? I don't have doctorate (or training), for one. Second, it's a rather popular thought that Mulder or Scully have some sort of diagnosis (besides trauma-- canon agrees with that one.) The rule dictates everyone has a right to their own opinion; and since that's the case, where would my post fit in?
Realistically, the 90s FBI wouldn't have recruited Scully out of medical school if they suspected she had autism. Mulder perhaps, but only because of Bill Mulder's (or CSM's) connection. There's a program just instituted (2021) by the Feds that is working on recruiting people with autism into their pilot program. And according to studies I've learned about from autism creators (that they've gleaned from the professionals), a neurotypical brain automatically senses something "off" or "different" about a neurodivergent brain, which can lead to ostracization (or bullying in children... and adults.) 90s Scully would have had to learn to mask her autism so well that not only was she never diagnosed but she attracted the attention of the FBI recruitment office-- not a small feat for a woman in the 90s-- and was able to keep it through their very strict recruitment circuit. (Fyi, the man who inspired "Catch Me if You Can" tried to get in with a law degree and was still turned down.)
Also, Mulder and Scully face back-to-back stimulating environments; and go right back to work without time to decompress (which is a feat nearly unachievable.) I'm not an expert-- far from it-- but the common denominator I'm finding from professionals and diagnosed individuals is that overstimulation is a key factor in autism. To varying degrees, yes, but still. Overwhelm and meltdowns are parts of the diagnosis that have to be factored in. Anecdotally, I've read one person who states she becomes better in high-stress situations than her peers because of her hyperfocus; but she seems to be an outlier (I presume.) I'd need to do more research on differing degrees of overwhelm and meltdowns (not everyone manifests overwhelm or a meltdown in the same way, of course); but since the field is still swamped with more information regarding "stereotypical" autism (a.k.a. boys who show the most extreme signs), it would take me a bit to narrow things down even more.
Lastly, we can all probably agree CC didn't write Mulder and Scully with an autism diagnosis. He definitely gave Mulder PTSD in the Pilot; and Scully's trauma from her abduction was written in later. The personal theories branch off from there; and, again, in order to finalize a perspective one way or another, a licensed professional would probably have to watch the show (or more than one season) and make a conclusion; otherwise, my "research" could be written off as another form of headcanon. And since professionals are professional, they'd probably abstain from forming an opinion either way.
Thus, the scales have been put before you: time requirements and lukewarm reception weigh against it; putting my ideas out there for me and the mutuals to puzzle over weigh for it.
#asks#agent-troi#thanks for droppin in~#I had a proper sitdown to flesh my thoughts out#hopefully they're coherent-- did a lot of paragraph swapping#this was fun
14 notes
·
View notes
Text
Childhood OCD
Obsessive-Compulsive Disorder (OCD) is a mental health condition that affects people of all ages, including children. While it was once believed to be rare in childhood, research now suggests that OCD can manifest in children as young as preschool age. Understanding OCD in children is essential for early identification, intervention, and support.
OCD is characterized by intrusive thoughts, images, or urges (obsessions) that cause significant distress, as well as repetitive behaviors or mental acts (compulsions) aimed at reducing this distress or preventing a feared outcome. In children, these obsessions and compulsions can vary widely in content and intensity, making the disorder sometimes challenging to recognize.
One common misconception is that childhood OCD only revolves around cleanliness or organization. While these themes are prevalent, children with OCD can experience a broad range of obsessions and compulsions. For instance, a child may have obsessions related to harm or contamination fears, leading to compulsive rituals such as excessive handwashing or seeking reassurance from caregivers. Others may experience obsessions about symmetry or orderliness, leading to compulsions like arranging objects in a specific way.
Recognizing OCD in children can be complicated by the fact that many youngsters engage in rituals or exhibit repetitive behaviors as part of typical development. However, in OCD, these behaviors are more frequent, distressing, and time-consuming, often interfering with daily functioning and causing significant impairment in academic, social, and family domains.
Moreover, children with OCD may experience shame or embarrassment about their symptoms, leading them to hide their struggles from others. This can delay diagnosis and treatment initiation, exacerbating the impact of the disorder on the child's well-being and quality of life.
Understanding the factors contributing to childhood OCD is crucial for addressing the condition effectively. While the exact cause of OCD remains unclear, research suggests a combination of genetic, neurobiological, and environmental factors may play a role. Children with a family history of OCD or other anxiety disorders may be at a higher risk of developing the condition. Additionally, certain life stressors, such as major transitions or traumatic events, can trigger or exacerbate symptoms in susceptible individuals.
Furthermore, neuroimaging studies have provided insights into the brain circuits involved in OCD, highlighting abnormalities in regions responsible for regulating fear, anxiety, and repetitive behaviors. These findings contribute to a better understanding of the underlying mechanisms driving the disorder and inform the development of targeted interventions.
In conclusion, childhood OCD is a complex and often misunderstood condition characterized by intrusive thoughts and repetitive behaviors that cause significant distress and impairment. Recognizing the diverse manifestations of OCD in children, understanding its contributing factors, and addressing the associated stigma are essential steps toward providing effective support and interventions for affected youngsters. By raising awareness and promoting early identification and intervention, we can help improve outcomes and enhance the well-being of children living with OCD.
Recognizing Symptoms in Children with OCD:
1. Obsessive Thoughts: Children with OCD may experience intrusive thoughts, images, or urges that cause significant distress or anxiety. These thoughts can be persistent and difficult to control.
2. Compulsive Behaviors: Children often engage in repetitive behaviors or mental acts in response to their obsessive thoughts. These compulsions may include rituals such as handwashing, checking, counting, or arranging objects in a specific order.
3. Fear of Contamination: Many Children with OCD have an intense fear of germs or contamination. They may avoid touching certain objects or refuse to share items with others.
4. Need for Symmetry or Order: Some children with OCD feel compelled to arrange objects in a particular way or follow strict routines to maintain a sense of symmetry or orderliness.
5. Hoarding: Hoarding behaviors, such as collecting excessive amounts of items or refusing to throw away possessions, can be a symptom of OCD in children.
6. Reassurance-Seeking: Children with OCD may constantly seek reassurance from parents, teachers, or other caregivers to alleviate their anxiety or doubts about specific concerns.
7. Avoidance: Children may avoid situations or activities that trigger their obsessive thoughts or provoke anxiety. This avoidance can interfere with academic, social, or family functioning.
8. Time-Consuming Rituals: Rituals or compulsions may consume a significant amount of the child's time, leading to disruptions in daily routines or difficulty completing tasks.
9. Emotional Distress: Children with OCD often experience emotional distress, including feelings of guilt, shame, or embarrassment related to their symptoms.
10. Impact on Relationships: OCD symptoms can strain relationships with family members, peers, or teachers due to the child's need for reassurance, avoidance behaviors, or difficulties participating in typical activities.
Common Obsessions and Compulsions in Children with OCD:
1. Fear of Contamination: Obsession with germs, dirt, or illness, leading to compulsive handwashing, avoidance of touching certain objects, or refusal to share items with others.
2. Perfectionism: Obsession with achieving perfection or avoiding mistakes, leading to compulsive checking behaviors, such as repeatedly checking homework or belongings.
3. Symmetry and Order: Obsession with symmetry or orderliness, leading to compulsive arranging or organizing of objects in a specific way.
4. Intrusive Thoughts: Obsession with disturbing or taboo thoughts, images, or impulses, leading to compulsive mental rituals or avoidance behaviors.
5. Fear of Harm: Obsession with causing harm to oneself or others, leading to compulsive avoidance of specific activities or places perceived as dangerous.
6. Religious or Moral Concern: Obsession with religious or moral beliefs, leading to compulsive praying, confessing, or seeking reassurance from religious figures or authority figures.
7. Superstitions: Obsession with specific superstitions or rituals believed to prevent harm or bring good luck, leading to compulsive behaviors to fulfill these beliefs.
8. Counting and Number Rituals: Obsession with certain numbers or numerical patterns, leading to compulsive counting or arranging objects in specific numerical sequences.
9. Hoarding: Obsession with accumulating and saving items, leading to compulsive hoarding behaviors and difficulty discarding possessions.
10. Excessive Doubt: Obsession with uncertainty or doubt, leading to compulsive seeking of reassurance or repetitive questioning of decisions or actions.
Factors Contributing to Childhood OCD:
1. Genetic Predisposition: There is evidence to suggest that genetics play a significant role in the development of OCD. Children with a family history of OCD or other anxiety disorders are more likely to develop the condition themselves, indicating a genetic predisposition.
2. Environmental Triggers: Stressful life events, traumatic experiences, or major life transitions can trigger or exacerbate OCD symptoms in susceptible individuals. Examples of environmental triggers include moving to a new home, starting a new school, experiencing a loss or trauma, or significant family changes.
3. Brain Circuitry Abnormalities: OCD is associated with dysregulation in specific brain circuits involved in regulating fear, anxiety, and repetitive behaviors. Dysfunction in these circuits, including the orbitofrontal cortex, anterior cingulate cortex, and striatum, contributes to the development and maintenance of OCD symptoms.
4. Childhood Adversity: Adverse childhood experiences, such as physical or emotional abuse, neglect, or chronic stress, can increase the risk of developing OCD later in life. These experiences may disrupt normal brain development and contribute to the development of anxiety disorders, including OCD.
5. Parenting Styles: Parenting behaviors and family dynamics can influence the development of OCD symptoms in children. Overly critical or controlling parenting styles, excessive emphasis on cleanliness or orderliness, or inconsistent responses to a child's anxiety may contribute to the development or exacerbation of OCD symptoms.
6. Psychological Factors: Certain personality traits, such as perfectionism, high levels of anxiety or neuroticism, and difficulty tolerating uncertainty, may increase the risk of developing OCD. These psychological factors interact with genetic and environmental influences to contribute to the onset and severity of OCD symptoms.
7. Medical Conditions: In some cases, medical conditions or neurological disorders may be associated with the development of OCD symptoms in children. For example, autoimmune disorders, streptococcal infections (PANDAS/PANS), or neurological conditions affecting brain function may trigger or exacerbate OCD symptoms in susceptible individuals.
8. Peer Influence: Peer relationships and social dynamics can also influence the development of OCD symptoms in children. Peer pressure, social comparison, or exposure to peers with anxiety or OCD-related behaviors may contribute to the development or reinforcement of OCD symptoms in vulnerable individuals.
Understanding these factors contributing to childhood OCD is essential for early identification, intervention, and support to promote optimal outcomes for affected children and families.
Impact on Daily Life and Relationships with a child suffering for OCD
The impact of OCD on a child's daily life and relationships can be profound and far-reaching. OCDsymptoms often consume a significant amount of time and energy, leading to disruptions in various aspects of the child's life. For instance, compulsive rituals such as excessive handwashing, checking, or arranging objects may take up hours each day, interfering with academic performance, extracurricular activities, and social interactions. The need to repeat tasks or seek reassurance can also lead to difficulties completing homework assignments, participating in group activities, or maintaining friendships. Additionally, avoidance behaviors stemming from OCD-related fears can limit the child's participation in everyday experiences, such as attending school events, going to public places, or engaging in recreational activities.
Moreover, OCD can strain relationships within the family. Parents and siblings may struggle to understand the child's compulsive behaviors or may become frustrated by the need to accommodate the child's rituals or reassurance-seeking. Family members may experience stress or tension as they try to navigate the challenges posed by the child's OCD symptoms, leading to conflicts or disruptions in communication. Siblings may feel neglected or resentful of the attention given to the child with OCD, further straining family dynamics.
Childhood OCD: In addition to family relationships, OCD can impact the child's relationships with peers and teachers. Peers may perceive the child's rituals or avoidance behaviorsas odd or eccentric, leading to social ostracism or teasing. Teachers may struggle to accommodate the child's needs in the classroom, particularly if OCD symptoms interfere with academic performance or disrupt the learning environment. As a result, children with OCD may experience feelings of isolation, low self-esteem, and a sense of alienation from their peers, exacerbating the emotional toll of the disorder.
Overall, the impact of OCD on a child's daily life and relationships underscores the importance of early identification, intervention, and support. By addressing OCD symptoms comprehensively and providing appropriate resources and accommodations, we can help mitigate the negative consequences of the disorder and improve the child's overall quality of life and well-being.
Childhood OCD Diagnosis and Evaluation Methods:
Diagnosing childhood OCD typically involves a comprehensive evaluation by mental health professionals, such as psychiatrists, psychologists, or licensed clinical social workers. Here are some common diagnosis and evaluation methods used for childhood OCD without medication:
1. Clinical Interviews: Mental health professionals conduct thorough interviews with the child and their parents or caregivers to gather information about the child's symptoms, onset, duration, and severity. These interviews may use structured diagnostic interviews or open-ended questioning to assess the presence of OCD symptoms and their impact on the child's daily life.
2. Symptom Assessment Scales: Clinicians may use standardized rating scales, such as the Children's Yale-Brown Obsessive-Compulsive Scale (CY-BOCS) or the Obsessive-Compulsive Inventory-Child Version (OCI-CV), to quantify the severity of OCD symptoms and track changes over time. These scales help provide an objective measure of symptom severity and treatment progress.
3. Behavioral Observation: Observing the child's behavior in various settings, such as home, school, or clinic, can provide valuable insights into the nature and frequency of OCD symptoms. Clinicians may observe the child engaging in compulsive rituals, avoidance behaviors, or reassurance-seeking interactions with parents or peers.
4. Collateral Information: Gathering information from multiple sources, including parents, teachers, and other caregivers, helps provide a comprehensive understanding of the child's symptoms and their impact across different contexts. Collateral information can corroborate the child's self-reported symptoms and provide additional insight into the functional impairment caused by OCD.
5. Assessment of Functional Impairment: Evaluating the extent to which OCD symptoms interfere with the child's daily functioning, academic performance, social relationships, and overall quality of life is essential for making an accurate diagnosis. Clinicians assess the degree of impairment caused by OCD symptoms and their impact on the child's ability to meet developmental milestones and participate in age-appropriate activities.
6. Differential Diagnosis: Given the overlap between OCD and other mental health conditions, such as anxiety disorders, tic disorders, or autism spectrum disorder, clinicians conduct a thorough differential diagnosis to rule out alternative explanations for the child's symptoms. This process involves considering the presence of comorbid conditions and distinguishing between OCD and other psychiatric disorders with similar symptom presentations.
7. Cultural Considerations: Clinicians take into account cultural factors and familial beliefs that may influence the expression and interpretation of OCD symptoms within the child's cultural context. Cultural sensitivity and awareness help ensure that diagnostic assessments are culturally appropriate and respectful of the child's background and experiences.
By utilizing these diagnosis and evaluation methods, mental health professionals can accurately identify childhood OCD and develop tailored treatment plans to address the child's unique needs and challenges. Early diagnosis and intervention are crucial for improving outcomes and minimizing the long-term impact of OCD on the child's well-being and functioning.
Childhood OCD Support Strategies for Parents and Families:
Support strategies for parents and families of children with OCD are crucial for managing the condition effectively and promoting the child's well-being. Here are some helpful strategies:
1. Education and Understanding: Parents and family members should educate themselves about OCD, including its symptoms, causes, and treatment options. Understanding the nature of the disorder can help reduce stigma, increase empathy, and improve communication within the family.
2. Open Communication: Encourage open and honest communication within the family about the child's OCD symptoms, feelings, and experiences. Create a safe and supportive environment where the child feels comfortable discussing their struggles and seeking help when needed.
3. Normalize Feelings: Validate the child's feelings of anxiety, fear, or frustration associated with OCD. Let them know that it's okay to feel this way and that they are not alone in their struggles. Avoid minimizing or dismissing their concerns, and instead, offer empathy and reassurance.
4. Set Realistic Expectations: Be mindful of setting realistic expectations for the child's behavior and progress in managing OCD symptoms. Recognize that recovery from OCD is a gradual process, and setbacks may occur along the way. Celebrate small victories and offer encouragement and support during challenging times.
5. Establish Routines: Create a structured and predictable routine at home to help the child feel more secure and in control. Consistent routines can reduce anxiety and provide a sense of stability for children with OCD.
6. Encourage Independence: Encourage the child to take small steps towards independence and self-management of OCD symptoms. Offer guidance and support as needed, but also allow them opportunities to practice coping skills and problem-solving strategies on their own.
7. Avoid Accommodation: While it's natural to want to help alleviate the child's distress, avoid enabling compulsive behaviors or providing excessive reassurance. Instead, encourage the child to face their fears gradually and tolerate discomfort without engaging in rituals.
8. Promote Self-Care: Encourage self-care practices for both the child and family members. Make time for relaxation, enjoyable activities, and stress-reducing techniques such as mindfulness, deep breathing exercises, or physical exercise.
9. Seek Professional Help: Connect with mental health professionals who specialize in treating childhood OCD, such as psychologists, psychiatrists, or therapists. Professional support can provide guidance, evidence-based interventions, and additional resources to help manage OCD symptoms effectively.
10. Connect with Support Groups: Consider joining support groups or online communities for parents and families of children with OCD. Sharing experiences, strategies, and resources with others who understand can provide valuable emotional support and practical advice.
By implementing these support strategies, parents and families can play a crucial role in helping children with OCD manage their symptoms, build resilience, and lead fulfilling lives. Collaboration with mental health professionals and access to appropriate treatment resources are essential components of comprehensive support for children with OCD and their families.
Coping Techniques for Children with OCD:
Coping techniques for children with OCD are essential for helping them manage their symptoms and improve their quality of life. Here are some effective coping strategies:
1. Identify Triggers: Help the child identify triggers or situations that worsen their OCD symptoms. Understanding what sets off their obsessions or compulsions can empower the child to anticipate and prepare for challenging situations.
2. Practice Mindfulness: Teach the child mindfulness techniques, such as deep breathing exercises, meditation, or progressive muscle relaxation. Mindfulness helps increase awareness of the present moment and promotes a sense of calmness and inner peace.
3. Encourage Exposure and Response Prevention (ERP): Gradually expose the child to feared situations or triggers while resisting the urge to engage in compulsive rituals. Encourage them to confront their fears in a systematic and controlled manner, gradually building tolerance to anxiety-provoking stimuli.
4. Use Distraction Techniques: Encourage the child to engage in enjoyable and distracting activities when they experience OCD-related anxiety or urges. Activities such as drawing, listening to music, playing sports, or spending time with pets can help shift focus away from obsessions and compulsions.
5. Challenge Negative Thoughts: Teach the child to challenge negative or irrational thoughts associated with OCD. Help them recognize cognitive distortions and reframe their thinking by replacing irrational beliefs with more realistic and balanced perspectives.
6. Develop Coping Statements: Help the child develop coping statements or affirmations to use when facing OCD-related challenges. Encourage them to repeat positive affirmations such as "I can handle this" or "This feeling will pass" to help build resilience and self-confidence.
7. Use Relaxation Techniques: Teach the child relaxation techniques such as visualization, guided imagery, or progressive muscle relaxation to help reduce overall anxiety levels and promote relaxation.
8. Set Realistic Goals: Encourage the child to set realistic and achievable goals for managing their OCD symptoms. Break down larger goals into smaller, manageable steps, and celebrate each success along the way.
9. Create a Supportive Environment: Foster a supportive and understanding environment at home and school where the child feels safe to express their feelings and seek help when needed. Validate their experiences and provide encouragement and reassurance during challenging times.
10. Seek Professional Help: Encourage the child to seek support from mental health professionals who specialize in treating OCD. Therapy, such as Cognitive Behavioral Therapy (CBT) or Exposure and Response Prevention (ERP), can provide valuable tools and strategies for managing OCD symptoms effectively.
By incorporating these coping techniques into the child's daily routine and providing ongoing support and encouragement, parents and caregivers can help children with OCD build resilience, reduce distress, and improve their overall well-being.
Addressing Stigma and Misconceptions around childhood OCD:
Addressing stigma and misconceptions surrounding childhood OCD is essential for fostering understanding, empathy, and support for affected children and their families. Here are several strategies to address stigma and misconceptions:
1. **Education and Awareness Campaigns:** Organize educational events or awareness campaigns in schools, communities, and healthcare settings to increase understanding of OCD, its symptoms, and its impact on children and families. Provide accurate information about the prevalence, causes, and treatment options for OCD to dispel myths and misconceptions.
2. Personal Stories and Testimonials: Encourage individuals with lived experience of childhood OCD, as well as their family members, to share their stories and testimonials openly. Personal narratives can humanize the experience of living with OCD, challenge stereotypes, and reduce stigma by demonstrating that OCD is a real and treatable mental health condition.
3. Media Representation: Advocate for accurate and sensitive portrayals of OCD in the media, including television shows, movies, and news articles. Work with media outlets to ensure that depictions of OCD are realistic, respectful, and free from sensationalism or stereotypes.
4. Training for Healthcare Providers: Provide training and professional development opportunities for healthcare providers, including pediatricians, therapists, and school counselors, to increase their awareness and understanding of childhood OCD. Ensure that healthcare professionals have the knowledge and skills to recognize, diagnose, and treat OCD effectively.
5. School-Based Programs: Implement school-based programs and initiatives to promote mental health awareness and destigmatize OCD and other mental health conditions among students, teachers, and staff. Offer resources, workshops, and support groups to educate school communities about OCD and provide strategies for supporting students with the condition.
6. Peer Support Groups: Facilitate peer support groups or online forums where children and adolescents with OCD can connect with others who share similar experiences. Peer support can reduce feelings of isolation, provide validation and encouragement, and foster a sense of belonging and acceptance.
7. Anti-Stigma Campaigns: Collaborate with mental health organizations, advocacy groups, and community leaders to launch anti-stigma campaigns that challenge negative attitudes and stereotypes surrounding OCD. Promote messages of acceptance, empathy, and inclusion to create a more supportive and understanding society for individuals with OCD.
8. Language Matters: Encourage the use of person-first language and respectful terminology when discussing OCD and mental health. Avoid stigmatizing language or derogatory terms that contribute to misconceptions or negative stereotypes about OCD.
9. Policy Advocacy: Advocate for policies and legislation that prioritize mental health education, access to treatment, and anti-stigma initiatives for children and families affected by OCD. Work with policymakers to ensure that mental health services are adequately funded and integrated into healthcare systems.
By implementing these strategies and fostering open dialogue and understanding, we can challenge stigma and misconceptions surrounding childhood OCD, promote acceptance and support, and create a more inclusive and compassionate society for all individuals living with mental health conditions.
Conclusion: Hope and Strategies for Managing Childhood OCD
In conclusion, while childhood OCD can present significant challenges for affected children and their families, there is hope and a range of strategies available for managing the condition effectively. By raising awareness, promoting understanding, and challenging stigma and misconceptions surrounding OCD, we can create a supportive and inclusive environment where children feel empowered to seek help and access appropriate treatment. Education, early intervention, and evidence-based therapies such as Cognitive Behavioral Therapy (CBT) and Exposure and Response Prevention (ERP) offer effective tools for managing OCD symptoms and improving quality of life. Additionally, fostering open communication, providing emotional support, and encouraging resilience-building skills can help children with OCD navigate their challenges with confidence and self-compassion. By working together as a community, we can ensure that children with OCD receive the support and resources they need to thrive, ultimately fostering a brighter and more hopeful future for all individuals affected by this condition.
#ocdtreatment#actually ocd#oc development#obsessive compulsive disorder#ocd awareness#ocd tag#ocdinchildren#ocd therapist#ocdcounsellor#ocdpsychologist
2 notes
·
View notes
Text
NFL Machine: 2023 to 2024 False Narratives

While the young players in tonight's draft will be full of excitement and hope, the promise of a boyhood dream on the cusp of being fulfilled, a literal lifetime of sacrifice, blood, sweat and tears finally culminating in the dream of playing in the NFL, walking across that stage, shaking Roger Goodell's hand, putting on that team jersey with their name on the back and putting on their team hat, smiling for the cameras, their childhood dream coming true...
The fact of the matter is, a lot of these same men once they have exited the league, the majority of whom will do so within 3 years, and even the Pro Bowlers who play an average of 12 seasons, may not be smiling in 10 to 15 years after their playing career is over as that is typically where neurological symptoms of diseases like CTE, early-onset dementia, Parkinson's, ALS and Alzheimer's begin to surface from repetitive head trauma caused by subconcussive hits.
Not concussions -- the hundreds of thousands of subconcussive hits these men endure during spring training, training camps, practices, drills, scrimmages and games from Pop Warner in their youth, to high school and college as young men all the way to the professional level in the NFL.
While positions vary, and linemen, linebackers and running backs obviously take more hits than a quarterback or wide receiver, the fact is that every single person that plays the sport of tackle football is required to block and tackle and plays are only blown dead by a whistle if you take the ball carrier to the ground and physically stop their forward progress. You could also force a fumble, intercept a pass, the QB could slide or run out of bounds or throw the ball away -- but the inherent nature of football, unlike its predecessor rugby, is that every single square inch must be fought for and defended. Naturally, that results in some type of contact on nearly every play.
The majority of concussions at the NON-professional level -- UNpaid WITHOUT health insurance -- in high school and college occur during practice which means they are entirely preventable but still to this day only the Ivy League conference and one other university has removed hitting from their practices.
That is a lot of hits and they do add up and they do take their toll later on.
While not every football player develops a neurological disorder from playing football, and while there is an obvious selection bias in the brains autopsied for CTE by Dr. McKee as those players were already exhibiting symptoms or else they would not have had their brains donated to be tested in the first place, there has been a link proven at this point by Dr. Bennet Omalu and Dr. McKee that repetitive subconcussive head trauma absolutely can cause CTE and that every year of playing tackle football adds to the risk.
That is irrefutable at this point.
What we don't know is why some players develop neurological disorders and others don't -- but it isn't a question anymore that the more subconcussive hits a player endures, the more likely it is that they will be diagnosed later with a degenerative neurological disorder.
There is no test currently that can diagnose CTE in a living person as it can only be confirmed via autopsy posthumously.
So, we don't have a definitive way of knowing who does and doesn't have CTE until that individual dies and an autopsy is performed specifically looking for the tau proteins that form in individuals with CTE.
So, the link has been proven and the risk is there -- what we don't yet know is how many tackle football players have CTE?
All linemen? Most linebackers? Most runningbacks? Quarterbacks who take a lot of sacks? Other position players who play for more than a decade? NFL and college players who start tackle football between 5 and 8 years old versus waiting until high school?
While we won't know the prevalence of CTE until a test for living players is developed, we certainly know the risks, and instead of the NFL doing something to mitigate that risk, they have their team doctors lying to Tua and telling him that quarterbacks don't develop CTE, it is more a thing that happens to linemen and runningbacks when Miami's own former quarterback, Morrell, the back up to Griese during Miami's famed undefeated 1972 season literally died with the most advanced form of CTE, Stage IV.
And while Morrell played during an era where quarterbacks were unprotected by the rules, there have been college quarterbacks diagnosed with CTE, so for the team doctor to tell Tua when he was contemplating retirement that he has nothing to worry about because he is a quarterback and CTE isn't seen amongst players in the position he plays is an audacious lie.
With the NFL draft being tonight, I wanted to share a document that I put together of last year's season (2023 to 2024) where I documented in NFL games I watched any hits that seemed to lead to a concussion where the player either wasn't evaluated or passed the protocol too quickly or where the player was temporarily removed from play only to re-enter the game later or where the player finished the game only to report concussion symptoms after the game or in the following days to the team's facility.
I also notated where the announcers explicitly took place in creating false narratives for the viewer and I will include clips and/or images of the hits I am referencing when I have them.
Specifically, the announcers would either gloss over egregious, sometimes helmet to helmet hits, or there were times I saw a player collapse (Amazon Prime Black Friday game) and even having seizures (Cowboys game late season) and we were never provided with an update by the announcers and, in the latter case, the announcers never even mentioned that the Cowboys player was visibly seizing on the field (I tried to find footage of the hit on Youtube, Twitter & Reddit and was unable to).
In this post, what you will see is that the NFL is a machine that is constantly propagandizing both its viewers and players through the announce team, play by play and color commentating, as well as pre-game shows like Game Day Morning (NFL Network) and Sunday Morning Countdown (ESPN) by either minimizing, justifying, glossing over and/or glamorizing the violence on the field.
You will also see teams continuously lying about player injuries, especially concussions, dishonestly claiming after the game that a player had a knee injury when he clearly lowered his helmet to deliver the hit then promptly proceeded to collapse on the field (Amazon Prime Black Friday game) yet Miami stated the player had a "knee injury" after the game.
There are many, many other examples like this which should remind you of Miami lying two seasons ago that Tua had a "back injury" when he clearly had suffered a concussion as he was wobbly (classic ataxia symptoms) and struggled to get up and had to have multiple players assist him just to stand yet he still finished that game against the Buffalo Bills.
2023 to 2024 False NFL Narratives 11/24/2023 - Dolphins vs Jets On October 23rd, 2023, Jevon Holland fell to turf after colliding with fellow Dolphins defender vs Eagles.
He was on the turf for several minutes then evaluated in the lockerroom for a concussion by the UNC (unafilliated neurological consultant) and he cleared the test and was put back in the game.
The next morning (Monday), Coach Josh McDaniels confirmed that Holland had reported concussion symptoms and had been entered into the concussion protocol. He cleared the protocol a week later on November 1st and rejoined the secondary.
Tonight, approximately one month after Holland sustained a concussion against the Eagles, during the inaugural Black Friday game on Amazon Prime on November 24th, late in the 4th quarter, Holland lowered his helmet to deliver a tackle and immediately collapsed to the turf.
Earlier in the game, Holland had had a 99 yard pick 6 touchdown.
The broadcast stepped away to a commercial break directly after the above hit occurred and, when they returned, there was no update on Holland as they displayed a graphic on screen displaying the current AFC playoff picture and returned to the in-game action without providing commentary on Jevon Holland, who we had just seen collapse to the turf after lowering his helmet and delivering a hit just prior to the break.
The game concluded, and while Al Michaels & Kirk Hebstreit commented on Hollands incredible 99 yard pick 6, they never provided an update on how Holland was doing, if he had been evaluated for a concussion or if he had been ruled out of the game with a concussion.
In other words, the announce team acted like Holland had never collapsed to the field after lowering his helmet to deliver a hit.
As the game concluded, Al mentioned that the sideline reporter would be interviewing Jevon Holland about his 99 yard pick 6.
Holland was lucid, clear eyed and seemed 100% in control of his faculties.
There was no mention of him lowering his helmet earlier to deliver the tackle that left him collapsed and lying motionless on the turf.
Miami Dolphins claimed after the game that Jevon Holland had injured his knee, but during the broadcast of the game, a slow motion replay clearly showed that Holland lowered his helmet to deliver a tackle then he collapsed to the turf afterwards.
This is eerily similar to when Tua Tugavoila, Miami Dolphins QB, fell to the turf after a hard hit vs Buffalo Bills on a Sunday afternoon game two seasons ago, and had difficulty getting up, was visibly wobbly, stumbled, and had to be assisted up by several Dolphins players.
It was reported by Miami during the game at halftime that Tua had suffered a "back injury" and that he had experienced "back spasms" that made it difficult for him to walk when very clearly Tua had displayed concussion symptoms after being hit which included ataxia, a loss of motor control/instability.
Despite how obvious this was during the broadcast, Tua was never evaluated for a concussion and Miami Coach McDaniels defended the lack of even evaluating Tua for a concussion in the press conference after the game.
Four days later, Tua and the Dolphins faced the Bengals on Thursday Night Football at Paycor Stadium.
Tua sustained another very hard hit and slammed his helmet against the turf and immediately went into a fencing response.
He was put on a board and immediately ruled out of the game and taken to a local hospital where he was diagnosed with a concussion.
The Amazon Prime broadcast did mention that the head impact Tua clearly appeared to sustain on four days prior on Sundays game against the Bills which he then went unevaluated for and played through and there was additional speculation whether both head impacts occuring in four days could have led to Tuas fencing response with the hit he sustained during that current nights game against the Bengals.
After sustaining his second concussion in four days against the Bengals on Thursday Night Football and exhibiting a fencing response, a few weeks later, Tua received another very hard hit and he appeared to be concussed but he was unbelievably never evaluated.
Tuas QBR prior to the hit was over 100, his QBR after the hit was under 60.
Tua admitted after the game that he couldnt remember any of the plays he had just called during the game.
Despite all this, Tua was never evaluated for a concussion or ruled out of the game despite suffering a serious concussion a few weeks earlier vs the Bengals that led to a fencing response and him being evaluated at a hospital only four days after sustaining a hard hit Sunday vs the Bills which resulting in Tua stumbling and having to be helped to his feet by several fellow Dolphins for which he was never evaulated for nor removed from the game.
Still no concussion evaluation during the game although Tua admitted after the game he couldnt remember any of the plays he had just called during the game and his QBR in the game was over 100 prior to the hit and under 60 after the hit. And he had already suffered two concussions in four days just a few weeks prior to this game.
Still no concussion evaluation.
The next day, on Good Morning Football on the NFL Network, the hosts announced that Tua had reported concussion symptoms that morning when he reported into the team facility.
Tua was diagnosed with a concussion, placed on Injured Reserve, and ruled out for the rest of the season.
Even with all of this occurring to Miamis quarterback just last season, even with Jevon Holland falling to the turf after colliding with a fellow Dolphin on October 23rd vs the Eagles and lying on the turf for several minutes motionless and even after Holland was evaluated for a concussion in the lockerroom then allowed to return to play in that same game, even after Holland reported concussion symptoms the very next morning to Miamis training staff (just like Tua did last season) and they ruled him out with a concussion for a week, even after they cleared Holland on November 1st and Holland returned to play, even when Holland lowered his head approximately a month after sustaining the concussion against the Eagles on Amazon Prime's Black Friday game to deliver a tackle which once again left him motionless on the turf, Holland was still not evaluated for a concussion and he was instead incorrectly diagnosed after the game with a "knee" injury.
This is a systemic problem with the Miami Dolphins, their head coach Josh McDaniels, their training staff, the unaffiliated neurotrauma consultants (UNC) and independent spotters -- they have all failed.
Did the NFLPA, the players union, step in on Holland's behalf and intercede as they did with Tua the season prior which led to the "Tua rule" and ataxia being added to the list of "no-go" symptoms in the NFL's concussion protocol that if exhibited automatically removes a player from the game? You know the answer to that because unless you are a Dolphins fan, you have no idea who Holland is.
Miami is reckless with their players health and we have seen this play out multiple times now in back to back seasons.
Will the NFL do anything?
Will the NFLs top medical director say anything? Last season, the NFLs top medical director did admit that Tua "did not look like" he sustained a back injury.
Okay -- thats it?
No fines, suspensions, warnings or loss of draft picks for Miami's head coach and their trainers?
The UNC that cleared Tua last season and cleared Holland in October -- why havent they been fired?
The independent spotters that missed Tuas concussion last season and Hollands concussion last month should be fired.
Who protects these men from themselves AND their coaches, trainers, independent spotters, unaffiliated neurotrauma consultants, Roger Goodell, the NFL machine and the purposely oblivious fans and often neutered and ineffective NFL Players Association?
11/30/23 - Dallas vs Seattle On November 30, 2023, Dallas played Seattle on Amazon Prime Thursday Night Football.
During the third quarter, Tony Ferguson (#87, Tight End) caught a pass from Dak Prescott on the 5 yard line and Quandre Diggs (#6, Safety) hit him helmet to helmet.
It was an egregrious hit that Al Michaels commented on the broadcast.
However, there was no flag.
This is extraordinary given that Seattle & Dallas were the two most penalized teams as of that current season in the NFL.
Carissa Thompson even said during halftime that the laundry was flying like crazy.
Additionally, Bobby Wagner (#54, Linebacker) was called for pass interference for defending a pass to Tony Pollard that was nowhere even close to DPI.
Literally, even the Amazon Prime broadcast stated there was nothing there and it wasnt pass interference.
So, an egregious gratuitious helmet to helmet hit -- let 'em play!
But for the crime of playing defense, Wagner gets hit with DPI.
One of those plays -- helmet to helmet hits -- causes concussions and permanent brain damage and was supposed to be legislated out of the sport.
Pass interference doesnt cause the players' jelly and egg yolk-like unprotected brains to move around violently and rupture against the inside of their sharp and bony skulls.
Yet pass interference is what gets the yellow flag and what gets penalized.
Permanent irreversible and preventable brain damage is nbd.
11/9/23 - Panthers vs Bears Hayden Hurst (TE, Carolina Panthers) suffered an extremely hard yet legal hit from Jaquan Brisker vs the Bears on 11/9/23 that caused Post Traumatic Amnesia.
Hayden Hurst's father tweeted the following on 12/6/23: "@haydenrhurst has been diagnosed with Post Traumatic Amnesia by an independent neurologist as a result of the hit he took in Chicago November 9. Slow recovery, don’t know when he’ll be back. Prayers appreciated!"
Per the above linked video, the hit was hard but perfectly legal. There is no way to legislate hits like this out of the game without removing tackling.
Post Traumatic Amnesia has happened in an NFL game before, even if it wasn't diagnosed as such at the time.
Troy Aikman still to this day does not remember winning an NFC Championship Game for the Cowboys in the mid 90s.
He was concussed so hard that when he arrived at the hospital after the game, he asked if the Cowboys had won the game.
Aikman says to this day, he watches the game back, but he doesnt remember himself playing in it while literally watching himself play.
Joe Burrow told Colin Cowherd on The Volume podcast during the 2022 to 2023 season that there are entire quarters and halves in college games he played that he doesnt remember due to extremely hard hits that happened during the course of those games.
Burrow claimed that he was strictly talking about his LSU days and that this hadn't happened to him in the NFL.
Cowherd replied that he wasnt surprised and that Drew Bledsoe and Trent Dilfer had personally told him in the past there were entire games they couldnt remember due to how hard they had been hit.
Cowherd said it may be a part of the game fans dont typically know about but he agreed with Burrow that it was extremely common.
Is this level of violence acceptable?
Hurst now has anterograde (post traumatic) amnesia not from a car accident or an explosion in a war or a physical assault but from the sport of football itself.
Unbelievably, the Panthers have confirmed that Hurst is already back at practice as of 12/6/23 and Hurst advised that, far from the hit being career ending as many observers and journalists rightfully wondered, that he would be "back in a week or two" but not before confirming he still has 4 hours of memory from the game when he was hit (11/9/23) that he doesnt recall at all -- aka he is still suffering from the effects of anterograde (post traumatic) amnesia.
I realize some people never regain their memories of the lost time -- but should he already be jumping back in with the live bullets less than a month later in padded practice?
It hasnt even been a month and hes already back at practice and Hurst says he may play next week!
That is totally reckless.
It unbelievably gets worse -- Hurst was not removed from the game after receiving the hit from Brisker that later caused the anterograde (post-traumatic) amnesia and returned to play the rest of the game on 11/9/23.
Per the Panthers, Hurst didnt enter the concussion protocol until the next day after the game (11/10/23).
So, how many more hits did an already concussed Hurst suffer when he returned to play after the Brisker hit?
Could there have been a second concussion?
Once you are concussed, it takes much less head impact to sustain a second concussion.
When Hurst reported concussion symptoms the next day at the team's training facility and the Panthers entered him into the concussion protocol, is it possible that unbeknownst to himself and the training staff, that he could have been reporting symptoms for two concussions?
Since Hurst was irresponsibly allowed to return to the game and continue playing after the Brisker hit, we will never know.
From ESPN.com on 12/7/23: Hurst entered the protocol during the Thursday night game after taking a hit that caused his head to hit the ground. He re-entered the game and wasn't placed into the protocol until the next day.
He later was told by the independent neurologist that he was suffering from post-traumatic amnesia.
"That's what I was told by the neurologist but sounds way worse," Hayden said.
Post-traumatic amnesia, according to the Cleveland Clinic, is amnesia that develops after an injury. It can involve multiple forms of amnesia. It can invoke confusion and frustration in those impacted because they have difficulty remembering where they are, how they got there or any new information since the injury.
"I'm doing better each day," Hurst wrote ESPN on Thursday in a text message. "It's not going to end my career, just being cautious as I come back. Should be another week or two."
"I appreciate everyone reaching out & checking on me. I suffered a pretty nasty concussion against the Bears a few weeks ago & don't remember up to 4 hours after the game. Scary situation but the Panthers have been incredible walking me through this process," he wrote on X.
He added in a follow-up post: "While it was scary, it is NOT career ending. I'm starting my return to play this week, so fingers crossed I make it back for the last few weeks! God Bless & Keep Pounding !!!!"
Keep pounding???
12/11/23 - Texans vs Jets On 12/11/23, CJ Stroud (QB - Texans - Offensive Rookie of the Year) slammed the back of his head against the turf at MetLife Stadium and was entered into the concussion protocol and was removed from the game.
It is well documented at this point that 1/4 of all concussions occur from the players heads slamming against the turf - 1/4!
25% of all concussions in football, permanent brain damage, are caused by the players heads slamming against the turf!
Replace all turf in all NFL stadiums with grass!
Soccer players have refused to play on turf in the World Cup so they are switching the turf out for grass then literally switching it right back to turf for NFL players -- how wrong is that?!
The owners have the money and, as has been proven, for the World Cup they can and will remove the turf and replace it with real grass.
They just dont give a damn about players in their own league!
The NFL Players Association has tried to get turf replaced with grass in their CBAs to no avail.
On top of the unnecessary permanent brain damage, it has also been proven that 36% more injuries happen on turf vs grass.
Cleats get caught. Players get caught.
They slip and slide.
Tendons and ligaments tear.
And the NFL owners dont give a damn.
So, the injuries and permanent brain damage continue.
Additionally, the Texans coach was asked post-game if CJ Stroud would be playing next Sunday.
He had just been concussed that same night, removed from the game & entered into the concussion protocol and the coach was already being asked if Stroud would be playing in exactly one week.
Its disgusting, infuriating & fucking terrifying that this decision is left to individual team trainers, coaches & UNC (independent neurotrauma consultants).
NFL has NO mandatory time off after a concussion -- the only professional American sport that doesnt have a mandatory sit out time period for a concussion like the NBA, MLB, MLS, NHL, UFC & boxing all do -- all you have to do is "clear the protocol" and you can be back at a padded practice a few days later Wednesday then playing in a game Sunday.
For that to be happening with everything we know about CTE is terrifying, infuriating, disgusting, inhumane, fucking reckless, disingenuous and a fucking slap in the face to every player who has died from CTE, who has committed suicide, who has harmed themselves, their families, their friends, their neighbors & strangers.
Week 11 - 12/4/23 On 12/4/23, a week prior to the hit that caused the concussion on 12/11/23, CJ Stroud suffered a hard hit against the Denver Broncos.
Two concussions in one week but this one was undiagnosed yet clear as day from watching the broadcast.
He needed help from teammates to get back to his feet and he appeared wobbly afterwards.
Stroud wasnt checked for a concussion and played out the duration of the game.
During another play against the Broncos in the same game on 12/4/23, Stroud briefly rolled his eyes to the back of his head, closed them for a few seconds then appeared unsteady once he stood back up.
Although none of the Texans trainers or independent spotters reacted to this, one of the refs motioned a Texans trainer over to check on Stroud.
The trainer checked Stroud on the sideline then he was immediately put back in the game.
The following Sunday (12/11/23) vs the Jets, Stroud suffered an extremely hard late hit from Quinnen Williams. The back of his head slammed against the MetLife turf and he laid on the field for several seconds before being ruled out with a concussion.
Week 13 is coming up this weekend and Houston has a chance to make the playoffs.
Although Stroud was entered into the NFLs concussion protocol Sunday (12/11/23), it appeared given Stroud seemingly briefly losing consciousness, appearing wobbly and needing two teammates to help him to his feet the previous week against the Broncos on 12/4/23, that Stroud suffered concussions back to back two weeks in a row -- the one against the Jets on 12/11/23 was diagnosed and the one against the Broncos on 12/4/23 wasnt.
Stroud was also in MVP discussions leading up to Sundays (12/11/23) game vs the Jets and is on pace to potentially break some rookie records.
So, there was pressure for the Texans coach to start Stroud and not Mills or Keenum that Sunday against the Titans.
Thankfully, when asked if the Texans will play Stroud Sunday, the head coach said he is going to put Strouds health and career longevity above any "win now" demands.
However, many Texans fans disagreed with this and have stated online if Stroud clears the protocol, since the Texans havent ruled him out of Sundays game, if hes medically cleared then he should be out there as he obviously gives the Texans the best chance to win on Sunday and keeps their playoff hopes alive.
Here lies one of the existential dilemmas facing the NFL: why is this decision left up to the coaches?
Because the NFL is the only professional sport in America -- out of the NBA, MLB, MLS, NHL, UFC & professional boxing -- that doesnt mandate a specific time off period once an athlete sustains a concussion.
Literally, Stroud could have done a full padded practice three days later that Wednesday if his coach wasnt looking out for his well-being and cared more about keeping Houstons playoff chances alive then whether Stroud will be able to remember his own name in 25 years.
Stroud has been concussed two weeks in a row -- against Denver last Sunday (12/4/23) and this past Sunday against the Jets (12/11/23).
What would have happened if the Texans HC felt differently and Stroud played Sunday?
What if he lost consciousness again and sustained a third concussion in three weeks?
What if he died on the field from Second Impact Syndrome vs the Titans on Sunday and, unlike Damar Hamlin, what if he didnt come back?
Thats where tackle football is headed.
Flag football has been added to the 2028 Olympics.
NCAA has added flag football as a collegiate sport eligible for scholarships.
The Pro Bowl this season and last were flag with no tackling.
There is a sea change coming as the CTE test in living players will be available in 3 years max per Dr. Ann McKee, the famed CTE researcher at Boston University.
That CTE test, once available, is going to confirm CTE in almost all current NFL and many college and high school linemen, most linebackers and running backs, many tight ends and some quarterbacks, wide receivers and defensive backs.
This is all coming.
Its why the Pro Bowl game is now flag football.
If I know this, the NFL knows this.
Its why you keep seeing flag football commercials with female players with the NFL's biggest stars like George Kittle and Tua Tugavailoa.
The NFL knows its where the sport is going in 10 to 15 years so theyre gearing up for it now.
CTE test in living athletes will eliminate the NFL's feeder systems (high school & Pop Warner) because the lower level leagues will not be able to be insured once its revealed that the vast majority of linemen, linebackers as well as a sizable amount of running backs as well as some tight ends, quarterbacks, wide receivers and defensive backs who are currently playing have CTE.
CTE has been found in non-professional tackle football players at the high school level as young as 17.
The NFL knows tackle football is going away and will be replaced by flag.
So then why not implement some changes now before we get served a live death on Monday Night Football along with our Buffalo Wild Wings?
Eliminate kickoff and place the ball at the 35 yard line.
66% of all injuries occur during kickoff.
Eliminate QB sneaks and onside kicks.
Institute weight limits to get rid of lopsided matchups of 100+ pounds (tight ends vs linemen, etc.).
Replace artificial turf with grass as turf causes 25% of all concussions and 36% more injuries.
But the NFL wont do any of the above.
Just like CJ Stroud potentially getting concussed again had the Texans HC played him and possibly dying against the Titans, the NFL just doesnt care.
12/17/23 - Browns vs Bears During Week 15, on 12/17/23, the Browns played the Bears. Towards the end of the fourth quarter, Za'darius Smith (Browns, DE) accidentally collided helmet to helmet with fellow Browns defender Myles Garrett (Browns, DE).
It was an extremely hard hit and Smith laid on the turf motionless for several seconds afterwards then the broadcast cut away for an injury timeout.
When the broadcast resumed, we were informed by the announce team that Smith was in the blue medical tent.
This was towards the end of the game so no additional updates on Smith were provided.
I googled Smith the following day (Monday - 12/18/23) and here is the first link I saw: "Cleveland Browns defensive end Za’Darius Smith exited the win in the final moments against the Chicago Bears. Smith was injured when he collided with Myles Garrett on a stunt in the game’s closing seconds. Smith was blindsided and stayed on the field for quite a while before being moved to the medical tent. His injury wasn’t disclosed in the immediate aftermath of the game. The Browns cannot afford to lose Za’Darius Smith for multiple games. The team has lost over 15 players to injured reserve."
The Cleveland Browns wont tell you but I will -- the incredibly hard accidental hit to the head that Smith suffered when he collided with Garrett and collapsed motionlessly to the turf for several sustained moments before being taken to the blue medical tent was 100% a concussion.
The reason the Browns "didnt disclose" Smiths injury in the "immediate aftermath of the game" is because they know he was concussed but they have already lost 15 players to injured reserve, its December football and a very tight race in the AFC North heading into the end of the season so they dont want to enter Smith, their best rusher behind Garrett, into the concussion protocol.
Even though he should have been. Even though he was concussed.
12/17/23 - Cowboys vs Bills During Week 15 (12/17/23), the Cowboys played the Bills on Sunday Night Football.
Donovan Wilson (#6, Cowboys) is a safety for the Dallas Cowboys.
Wilson was injured during a play and the broadcast briefly showed him convulsing on the field right before a commercial break but commentary didnt say anything.
Wilson was removed from play and evaluated for a concussion then he returned to the game late in the second quarter.
I tried to find footage of Wilsons injury and subsequent convulsions on the turf but I could not find footage of Wilson going down and momentarily convulsing on the field on twitter, youtube or reddit.
At the end of the day, convulsing on the turf after a hard hit and then being evaluated for a concussion should be enough to get you ruled out of the game.
Instead, Wilson was evaluated for a concussion -- after convulsing on the turf for several sustained moments -- then returned to the game.
12/21/2023 - Rams vs Saints On Amazon Prime Thursday Night Football, the Rams faced the Saints on December 21, 2023.
After a hard tackle, the running back for the Rams, Kyren Williams' (#23), helmet popped off and a player landed very hard on him with his full weight.
Williams was slow to get up.
Williams was then shown entering the blue medical tent and the broadcast mentioned he was being checked out.
Kyren then almost immediately exited the tent and reentered the game.
There was no additional commentary regarding Williams' helmet popping off after the hard tackle, the player landing on him after, him being slow to get up, him being checked out in the blue medical tent then him immediately exiting the tent and then reentering the game.
Was Williams checked for a concussion in the blue medical tent?
Did Williams clear the concussion protocol that quickly?
It was a huge career defining game for Williams, after he had made several mistakes in the previous weeks game, as he scored a touchdown and had several big runs.
Williams was interviewed on the sidelines after the game as one of the key reasons for the Rams victory.
What hit? What blue medical tent? What concussion?
12/17/23 - Jaguars vs Ravens "Pederson said Lawrence suffered the concussion on a scramble up the middle with five minutes remaining in the Jaguars' 23-7 loss to Baltimore last Sunday (12/17/23).
Lawrence did not leave the game but completed only one of his seven pass attempts after that play."
This is proof that Lawrence was concussed!
Just like with Tua the season prior when he suffered his third concussion that season and, during the game, his QBR went from 100 to 60 yet he was never even evaluated for a concussion.
Lawrence didnt complete 6 out of 7 passes after the hit.
He was never checked for a concussion.
He never was checked for a concussion in the blue medical tent or on the sidelines.
Per Pederson, Lawrence self-reported symptoms after the game and it was immediately apparent that the concussion was sustained on the scramble up the middle.
Pederson said Lawrence self-reported symptoms after the game and was placed in the concussion protocol.
Lawrence did not practice that Wednesday or Thursday.
Lawrence cleared concussion protocol the following week exactly seven days after suffering his concussion and was cleared to play against the Buccaneers on 12/24/23.
12/31/23 - Bengals vs Chiefs "Pacheco was forced out of the game on Christmas Day due to the accidental blow he took to the head from a teammate as his helmet was knocked off and fell backward. The impact from the defender caused a nasty collision as the independent doctor ushered Pacheco off the field for further examination and was later ruled out for the rest of the day."
Pacheco cleared concussion protocol and played on New Years Eve against the Bengals on 12/31/23 than six days after the concussion he suffered on Christmas Day -- less than a week!
Pacheco cleared concussion protocol in six days!
That is ridiculous and absurd.
Unfortunately, the NFL's concussion protocol is five stages and each stage can be cleared in just one day.
So, technically, a player can actually clear concussion protocol in just five days.
That is a totally reckless, dangerous and insane concussion protocol!
There is no literal way that anyone can clear concussion protocol in less than a week and be recovered enough to play a violent and collision-filled sport like football with guaranteed head impacts, hits to the head, hard tackles and required blocking and tackling on every play that result in subconcussive head impacts.
1/7/24 - Saints vs Falcons During Week 18, on Sunday afternoon (1/7/24), the Saints were playing the Falcons in the last week of the regular season -- win or go home for both teams so there was a lot on the line.
Algiers (Falcons, Tight End) collided with Avante Taylor (Saints, Safety, #1) helmet to helmet.
Taylor dropped to the turf without body control and lay still for several moments.
Noone called timeout to check on him and the next play was about to start.
The independent spotter signalled for a timeout and pulled Taylor to check him in the blue medical tent.
Despite the high stakes in the game for both teams and the high adrenaline inherent in the "win and youre in" nature of football, the system worked as designed for once when the Saints' coach and trainers did not call for an injury timeout but the independent spotter did the right thing and called for a timeout. Thats why the spotters are there and why they are independent and unaffiliated from the team.
Later on in the same game (Week 18 - Saints vs Falcons, 1/7/24), Tyrann Matthieu (Saints, Safety) lowered his shoulder for a very hard hit against Drake London (Falcons, #5, WR).
This was a legal hit as Matthieu delivered it textbook style with a lowered shoulder but it was an extremely hard hit.
London was very shaken up after the hit.
London was never checked on the sidelines or in the blue medical tent but he most definitely should have been evaluated for a concussion.
The independent spotter who earlier in the same exact game did such an exemplary job signalling to the ref and calling timeout to check on Taylor even though his own teams coach and trainer neglected to do so was nowhere to be found to do the same for London who also needed to be evaluated for a head injury.
The hit by Matthieu to London occurred on 4th down so perhaps the thinking was, they're coming off the field anyway, he'll be okay once he can catch his breath on the sidelines.
You cant "catch your breath" from a concussion.
2023 NFC Wildcard Playoff Game - Rams vs Lions Matthew Stafford (QB, Rams) was tackled by Aidan Hutchinson (Lions) and then a second defender came in and hit Stafford very hard in the ribs then Stafford hit his head hard after falling to the turf during the 2023 NFC Wildcard Playoff game.
This is the picture that started this post.
Stafford immediately grimaced and was in obvious pain & discomfort.
Stafford was then shown on the sidelines being walked into the blue medical tent.
The broadcast mentioned Stafford looked hurt and Collinsworth added that Stafford had hit his head hard on the turf.
When the broadcast resumed, they replayed Stafford slamming his head against the turf.
It was clear that Stafford was concussed and seemed to exhibit a brief fencing response.
The broadcast showed Stafford walking into the blue medical tent holding his side.
The broadcast then announced that Stafford exited the blue medical tent as Nucua (WR, Rams) entered the tent to be evaluated.
After Nucua exited the medical tent, Tirico announced the UNC (unaffiliated neurotrauma consultant) called a medical timeout to ensure that Nucua (RB, Rams) had been evaluated -- this was the right action by the UNC as Nucua had been shown on the broadcast as slow to get up.
However, Stafford had been shown in a slow motion replay slamming his head very hard against the turf, after which he seemed to briefly exhibit a fencing response and Collinsworth commented during the replay how hard Stafford had hit his head against the turf -- if Collinsworth saw it and we in the audience saw it why didnt any of the UNC or independent spotters see it?
Why didnt the UNC or independent spotters call a medical timeout to ensure that Stafford had been evaluated for a concussion?
Because this was the Sunday Night game of Wildcard Playoff weekend and it was the most Hollywood-esque anticipated storyline -- each QB used to play for the opposing team in the matchup for the first time ever in playoff history -- Stafford played 12 seasons for the Lions, then they traded him to the Rams and the very next season, he won the Super Bowl with the Rams and this was his first time back playing against Detroit -- Goff had played multiple seasons with the Rams, the Rams traded him to the Lions, Goff then took the Lions to the playoffs -- so, stakes were high on both sides and the Lions had not won a playoff game since 1991 and the game was in Detroit. Eminem was there and did the intro for SNF. And exactly none of that meant that Stafford wasnt concussed, didnt briefly exhibit a fencing response and shouldnt have been evaluated for a concussion -- but he wasnt.
1/20/24 - Divisional Round - Niners vs Packers Deebo Samuel (WR, 49ers) suffered an extremely hard hit to the side of his helmet and he was very slow getting up.
There was an injury TO & commercial break.
Once the broadcast returned, Deebo Samuel got checked in the blue medical tent.
Deebo reentered and then left the game several times.
With 9:40 left in the 2nd quarter, Deebo was shown running into the lockerroom.
With 4:09 remaining in the second quarter, Erin Andrews reported that Deebo was questionable to return with a shoulder injury.
Erin also advised that Deebo had previously missed two games earlier in the season due to a shoulder injury.
However, the replay of the hit Deebo suffered clearly showed a helmet to helmet hit against him.
We then saw Deebos shoulder being examined on the sidelines and Erin Andrews advised that he had previously injured his shoulder earlier this season and missed some time.
Deebo was then shown in the lockeroom at halftime without his pads.
When the game resumed after halftime, we were advised that Deebo had undergone some xrays of his shoulder.
We then saw Deebo on the sidelines in a hoodie and Erin Andrews reported that Deebo was still questionable to return to the game.
Deebo did not return to the game.
Chris Rose advised during NFL Gameday Final that Deebo had been checked for a concussion during the game and was cleared before being removed from the game due to a shoulder injury.
Per replay of the hit, however, the head impact Deebo suffered was due to a hard hit to the side of his helmet where he was slow to get up.
This is is the same hit they also claim he hurt his shoulder on and the shoulder injury is why he was officially ruled out of the game.
I think Deebo also had a concussion from the hit by Greenlaw and they covered it up by saying he reinjured his shoulder.
In the same game, Tucker Craft (TE, Packers) was hit extremely hard by Dre Greenlaw (49ers) on the side of his helmet as he blocked for Jordan Love (QB, Packers).
Craft was shown on his knees holding his head and was very slow to get up.
There was an injury TO and the broadcast went to commercials.
Upon returning to the broadcast, Greg Olsen (color commentator) advised that Craft had been slow getting up prior to the commercial break and that he was on the sideline, getting his eye checked out and that he appeared to "just need to take a breath".
Kevin Burkhardt (play by play announcer) then quickly advised that Craft had actually just entered the blue medical tent and he was getting checked out.
1/20/24 - Divisional Round - Bills vs Chiefs Shakir (WR, #10, Bills) suffered an extremely hard hit where he was sandwiched between two defenders then hit very hard.
Tony Romo stated on the broadcast that he could "hear the hit all the way up in the broadcast booth".
Shakir was shown on the turf holding his head.
Romo then advised the broadcast would be stepping away and there was an injury timeout and the broadcast went to commercials. When the broadcast returned, Shakir was shown jogging on the sidelines and Nantz announced that Shakir was jogging into the lockerroom.
Tracy Wolfson then announced that Shakir was being evaluated for a shoulder injury.
It was an extremely hard hit and he was holding his head when he fell to the turf -- not his shoulder.
Shakir most likely had a concussion and, just like Deebo Samuel during the playoffs and Tyler Brate (Bucs, TE) the previous season, they lied and claimed it was a shoulder injury.
Just like Tua's "back injury" the previous season vs the Bills on Sunday -- before he was concussed a second time four days later against the Bengals on Thursday Night Football -- undiagnosed concussion Thursday vs the Bills where he finished the game -- then a diagnosed concussion four days later against the Bengals where he exhibited a fencing response & was stretchered off the field, right?
Shakir returned to the game in the 4th quarter with under 5 minutes to go.
In the same game, in the first quarter of Chiefs vs Bills, Mike Edwards (S, #21, Chiefs) took a hard hit and was very slow getting up.
It was then announced on the broadcast that he was evaluated for a concussion and that he was entered into the concussion protocol.
Edwards was then ruled out of the game with a concussion in the 2nd quarter with 8 minutes left. The concussion protocol worked correctly in this instance as Edwards never returned to play and was subsequently ruled out of the game.
However, later in the same game, the concussion protocol failed spectacularly again -- remember, it had already failed earlier in the game when Shakir (WR, Bills) was allowed back into the game with a clear concussion in the 4th quarter with less than 5 minutes to go.
Knox (#88, Bills) taken out of game to be checked. Hard hit, slow getting up.
L'Jarius Sneed (Chiefs) also was "a bit shaken up" on the same play as Knox (#88, Bills) per the broadcast but Sneed stayed in for the next play and he wasnt evaluated.
Tracy Wolfson then advised that Knox was checked in the blue tent for a head impact and she said it "remained to be seen"whether or not he would come back in to the game.
Nantz then interrupted Wolfson and advised that Knox was already back in the game.
AFC Championship Game - 1/28/24 - Chiefs vs Ravens Mike Edwards (Chiefs, S, #21) slow to get up and walked to the sidelines.
The broadcast stated he had been knocked out of last week's game vs the Bills with a concussion as I notated within this document two pages up -- two concussions in 8 days!
NFC Championship Game - 1/28/24 - 49ers vs Lions Dre Greenlaw (49ers, 2nd Quarter) delivered an extremely hard hit and appeared to injure his shoulder.
Greenlaw struggled to get up from the field.
He limped off and then slumped down on the sidelines and was in significant pain.
He was surrounded by trainers who removed his helmet.
The broadcast mentioned that his shoulder appeared to take the brunt of the hit and that Greenlaw was receiving a lot of attention on the sidelines.
The broadcast then cut away to commercials.
Upon returning from commercials, the broadcast announced that they were concerned about Greenlaw and that Erin Andrews had an update on how he was doing.
Erin advised that Greenlaw suffered a stinger after the tackle on #87.
Andrews further advised that despite suffering a stinger, Greenlaw essentially ran out of the blue medical tent and the broadcast showed a slow mo of Greenlaw running to his teammates on the sidelines.
Andrews further commented that people say that when Greenlaw hits you, he runs right through you, and the broadcast replayed Greenlaws hit on the Lions player (#87).
The broadcast then showed Greenlaw on the sidelines receiving a shoulder massage from a trainer while another trainer removed his jewelery.
Greenlaw returned to the game in the same quarter (2nd quarter) with 7:45 remaining.
After suffering a stinger that caused him to collapse and drop to one knee on the sidelines in agonizing pain, Greenlaw returned to the game within five minutes and was shown delivering hard hits.
Greenlaw was in the blue medical tent for less than a minute.
The broadcast then advised that Greenlaw was the 49ers enforcer.
What stinger?
Later on in the same game, Brock Purdy (QB, 49ers) was tackled by 3 Lions defenders.
Purdy was shown crushed underneath the defender flat on his back on the turf, his helmet partially off as it was an incredibly hard hit.
The announcer conceded that the Lions "probably got away" with not getting a RTP call and that the crowd had noticed it and reacted to the missed penalty.
As the broadcast went to commercials, Brock Purdy was shown walking to the sidelines in slow motion with a bloody lip.
The broadcast stated again that the Lions had gotten away with a missed penalty and Purdy had a "bloody lip and all".
After commercials, the announce booth asked Dean Blandino (rules analyst) if the refs missed a RTP penalty on the last drive.
They replayed the hit against Purdy and Blandino advised that Houston (#41, Lions), lowered his head after Purdy had been tackled to the ground with force.
Blandino advised he believed that the refs missed the penalty and Houston (#41, Lions) should have been flagged for RTP.
Later on in the same game, McCaffrey (RB, 49ers) had a very physical run where he got within a few yards of the end zone.
When he was tackled to the ground, he landed hard on his head.
The broadcast showed him a bit slow to get up.
The broadcast then mentioned that McCaffrey landed on his head on the last play and that that was probably why he headed to the sidelines because he "needed a break".
Did he need a break or did he have a concussion?
After the 49ers scored a touchdown, their sideline was shown celebrating while the stadium erupted.
While McCaffreys teammates cheered, he was shown on the sideline with trainers working on his neck as he grimaced in pain.
The broadcast did not mention this as the stadium and 49ers were still celebrating the touchdown and, instead, advised that the Lions would need to score soon as there were 3 minutes left in the game.
What neck injury? What concussion?
The NFL Draft: Exploited Dreams As is probably clear from the above, I won't be watching the draft tonight. I have previously written articles on my tumblr questioning why I continued to watch the NFL despite all of the violence, dehumanization, head trauma, permanent brain damage, unguaranteed contracts, exploitative players union and commodification of players as products to be consumed.
For the past 13 years, I have watched football every Sunday from 9 am (Gameday Morning) or 10 am (Sunday Morning Countdown), the 1 pm, 4 pm and 8 pm games and Gameday Final -- from 9 am or 10 am to 12:30 am every Sunday; Mondays, pre-game on ESPN, Monday Night Football then ESPN post-game -- 7 pm to 12:30 am and Thursdays pre-game on Amazon, Thursday Night Football then Amazon post game -- 6:30 pm to 12:30 am.
28 hours of football a week, every single week, and me and my husband -- the only reason I ever got into football as I hated it prior to meeting him -- would make a different dip every week which we would then watch all day while we watched all the games. It was definitely our couples routine.
That was 2011 when I started watching football with my husband and slowly became a fan of the physical courage, larger than life personalities, confidence, swag, charisma, courage, physicality, calm under pressure and the general hypnotic and quixotic thrilling allure of the game, the spectacle of it all, the violent chess game that required aggression and strategy all appealed to me.
But I could never get over the helmets crashing, violence, injuries and concussions.
I bought Nate Jackson's book, Slow Getting Up, in 2016 -- he is a former TE for the Denver Broncos -- and that started nearly a decade's worth of research which has involved reading thousands of academic, scholarly and scientific journal articles, books, blogs and studies and conversing with attorneys via email who have been involved in litigation against the NFL.
Despite being a huge Joe Burrow, Bengals and Eagles fan, the amount of research, and the limitless depths and levels to the NFL's deception and depravity have finally served to mostly turn me off from the NFL.
I have previously attended Eagles and Ravens games in person. I have a Joe Burrow t-shirt, orange and black beaded necklace, sunglasses and cat ears as well as Eagles t-shirts and Super Bowl shirts and I attended the Eagles parade live when they won the Super Bowl in 2018.
From all of the above, I have decided to minimize my interactions with the NFL.
Over 85% of players who have applied for payouts under the NFL's $765 million concussion settlement have been denied. That's not okay.
The race norming bias where the NFL assumed that Black players were less intelligent so if they didn't fail their neurological assessments spectularly, they were denied disability benefits. That's not okay.
It's a long list that as you can see from this post kept getting longer and I could no longer put up with the racism, exploitation, lies, denials, gaslighting, subterfuge, underhandedness of the NFL.
The NFL is too similar to Israel - who they staunchly support while they murder 35,000 Palestinian civilians in a genocide yet the NFL would only give a moment of silence to the Israeli civilians who lost their lives -- 4,000 to 35,000.
Do the math that the NFL refuses to do.
The NFL's treatment of Colin Kaepernick.
Goodell's disgusting statements on George Floyd.
The NFL's treatment of players who chose to kneel during the anthem as is their right per the first amendment.
The NFL's racist dog whistles to its mostly aging and white audience regarding Trump, Israel, zionism & Black Lives Matter.
Its a long list that only gets longer.
Their exploitation of Damar Hamlin.
I have decided to go from watching nearly 30 hours of NFL programming a week every week for 4 months to only watching Eagles vs Cowboys, Bengals vs Chiefs, Eagles MNF & SNF games, Bengals SNF & MNF games, the AFC & NCF Championships and the Super Bowl.
I prefer this to zealotry and trying to just cut it all off -- I would rather cut off 90% of my NFL watching then try to go for 100%, fail and then things stay the way they were for the past 13 years.
I have unfollowed the Bengals, Eagles & NFL accounts on all social media and also unsubscribed from their newsletters.
I will not attend any more games at Lincoln Financial Field nor will I attend another parade if the Eagles win another Super Bowl.
I also won't be watching the draft tonight nor tracking who the Bengals or Eagles select.
I can't unsee these young men tonight, full of hope promise dreams and ambitions, twenty to thirty years from now unable to work, talk, remember their playing careers, their wives & childrens names.
I can no longer embrace these young determined men lured by the bright lights and big money of the NFL being exploited for their courage, physicality, talents, intelligence, strength & heroic feats on the field.
#nfl#nfl football#nfl draft#football#roger goodell#concussions#cte#anti blackness#anti capitalist#labor rights#exploitation#head injury#league of denial#espn#workers rights#militarism#military industrial complex#propaganda#false narrative#misinformation#gaslighting#black lives matter#modern day slavery#corporate slave#corporate greed
5 notes
·
View notes
Text
How to Overcome Maladaptive Daydreaming

Let’s first understand that maladaptive daydreaming is an instance where you find yourself constantly daydreaming for an extended period of time, to the point that it distracts you from your day-to-day activities. You may do this for hours consecutively or have moments where you escape into this imaginary world.
Stopping MDD (Maladaptive Daydreaming Disorder) is a complex process that requires a nuanced understanding of its underlying mechanisms. Unlike some conscious behaviors or habits that you can simply decide to quit, MDD operates differently. It's crucial to recognize that MDD is not the root cause itself but rather a symptom of underlying psychological and emotional processes.
Initially, MDD often begins innocently with what can be termed 'normal daydreaming.' Daydreaming, in moderation, is a natural and even healthy human activity. It allows the mind to wander, explore creative ideas, and occasionally escape from the demands of everyday life. During this phase, daydreaming remains a controllable and manageable activity for most individuals.
However, for some, especially when confronted with stress, anxiety, or other emotional triggers, daydreaming can evolve into a means of coping. This shift occurs gradually, often unnoticed, as daydreams start to offer a refuge from reality. The daydreams may be populated with pleasant or idealized scenarios, which serve as an enticing escape from the challenges and stresses of daily life.
As this pattern persists and deepens, it can transform into what we now term as 'maladaptive daydreaming.' At this stage, daydreaming becomes increasingly uncontrollable. It's as if there's an involuntary, subconscious pull toward these immersive fantasies that can overpower your conscious efforts to resist them. This involuntary pull happens beyond your immediate awareness, making it challenging to simply 'snap out of it.'
Imagine it as a powerful current in a river. Initially, you could swim against it, but as it grows stronger, it becomes nearly impossible to fight. You may still recognize that it's happening, but the ability to consciously stop or control it diminishes. The daydreams become a compelling force that pulls you in, often without your conscious consent or awareness.
Dealing with the Root Cause
One of the primary factors that propel maladaptive daydreaming is emotional triggers in one's real life. These triggers often include stress, anxiety, and boredom. When individuals are confronted with these emotional states, they may turn to daydreaming as a coping mechanism. It provides an escape from the overwhelming emotions or a way to fill a void left by boredom.
Crucially, it's essential to understand that these triggers are not the root causes of maladaptive daydreaming but rather catalysts. They set the stage for excessive daydreaming to become a problem. Therefore, merely attempting to suppress daydreaming without addressing these emotional triggers is unlikely to yield long-term success.
Each individual has unique coping mechanisms for dealing with stress, trauma, or emotional struggles. For some, it manifests as maladaptive daydreaming, while others might resort to toxic relationships or even substance addiction. The choice of coping mechanism can vary widely from person to person, depending on their life experiences and psychological makeup.
In summary, the path to stopping maladaptive daydreaming is not a simple one. It involves recognizing that daydreaming is often a symptom of deeper emotional struggles and triggers. To break free from this behavior, it's essential to address these root causes, seek professional guidance, and develop healthier coping mechanisms. This process needs conscious effort and dedication but it offers a more sustainable and lasting solution to overcome maladaptive daydreaming and regain control of one's life.
Note from the Author
If you’re ready and you’d like my help with overcoming and managing maladaptive daydreaming without spending years in therapy, then you can book a FREE BREAKTHROUGH CALL with me HERE. Happy healing 💙💙. Feel free to share and comment! Use this information with caution, it comes from my own thoughts & bias, experiences and research😊.
#actually maladaptive#actually madd#madd#obsessive daydreaming#maladapting daydreaming disorder#maladaptive daydreaming#daydreaming#intrusive daydreaming#immersive daydreaming
17 notes
·
View notes
Text
if we’re friends but you don’t agree with the following statements, then, sorry, i don’t think we can be friends.
fat people are not inherently bad/immoral just because they’re fat; fatness does not automatically equate to badness/immorality. << moreover, saying that does not imply that non-fat people are inherently bad/immoral, it simply clarifies that no one is inherently bad/immoral based on their body type/physical appearance.
someone’s physical appearance should not dictate how you treat them and/or whether or not they are worthy of respect, acceptance, love, etc.
health is not an indicator of morality/worth; if you wouldn’t shame a smoker for smoking, then you shouldn’t shame an overweight person for their diet nor an underweight person for their diet. shaming never helps, it typically only makes things worse. if you’re not in their medical support system (their primary care provider, a specialist they’ve either been referred to or specifically sought out, etc.), then you have no right to comment on another person’s diet or activity level; the way they actually eat and the amount of daily activity they actually get is 1) irrelevant to their worth of fair treatment and respect and 2) probably much different than how you perceive it to be (we only see a snapshot of other people’s lives, we can’t possibly know the full story).
the body acceptance/positivity/neutrality movements are meant for ALL bodies, so people of all body types should be able to benefit from them.
you are not more hygienic if you chose to remove your body hair. likewise, you are not less hygienic if you chose not to remove your body hair (or not to remove all of it). the removal of body hair should ultimately be treated a matter of personal preference and not a marker of cleanliness.
sloped/curved/downturned noses are just as beautiful as upturned or “button” noses
acne is not always a sign of poor hygiene, it can be caused by sooo many other factors (diet, hormones, pollution, etc.), none of which should be used to determine your worth.
a bisexual or pansexual or demisexual person in a heterosexual relationship is NOT a straight person. a bisexual or pansexual or demisexual person in a homosexual relation is NOT gay/a lesbian. bisexual, pansexual, and demisexual people retain their bisexual, pansexual, or demisexual identities regardless of who their partners are.
a non-binary person is not a woman simply because they’re femme-presenting. a non-binary person is not a man simply because they’re masc-presenting. a non-binary person is just that: a non-binary person, regardless of what clothes they wear, what hairstyle they have, etc.
your worth is not defined by your productivity level. you are not a bad person for taking time off. you are not a bad person for needing a break.
just because someone does not behave exactly like the one neurodivergent person you know, that does not mean they aren’t neurodivergent. both autism and adhd vary widely in terms of symptoms and each person experience with one of both disorders can look very different.
7 notes
·
View notes