#neurology and neuroscience
Explore tagged Tumblr posts
Link
I wonder when/if they will be able to play Doom...
1 note
·
View note
Text


this is my oc neuro, its a neuron and i wanted to make it look like a diagram ^_^
its meant to be a cat looking thing
woah htis is geting attentoin thank yall1!! follow if u wanna see more o f this gober.. an its friends..!
#artists on tumblr#neurons#neuro#neuron#myart#moeart#moe art#cats#anime#cells at work#cells#biology#art#new artist#neuro and hemo#oc#digital artist#small artist#medicine#neurology#neuroscience#cat#my art#original character#brain#medical#medical illustration#medart#sciart#medical art
1K notes
·
View notes
Text
A newly discovered communication pathway linking far-flung nerve centers within the brain and skull, and the body beyond, could provide a new target to stop migraine pain in its tracks. Researchers have long tried to pinpoint where migraines begin in the brain, and how these one-sided, nauseating headaches induce pain and other symptoms, such as vomiting. Understanding this would help find new ways to prevent migraines from happening or at least ease the searing pain once it starts.
Continue Reading.
1K notes
·
View notes
Text
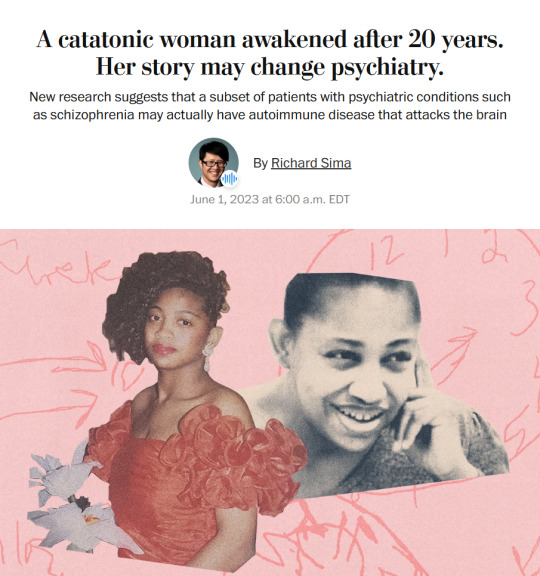
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes
Text

cms - Aysel for @/jimengxi (twitter)
#illustration#dark fantasy#fantasy illustration#art nouveau#science#gothic#sketch#art#medcore#victorian#neuroscience#neurology#neuroart#neurosurgeon#skeleton#monstercore#doctor#dark academia#horror#creatures#rabbit#bunny#surgery#surgeon#oc art#art commisions#academia aesthetic#classic academia#scientific illustration#sciencecore
320 notes
·
View notes
Text
My neuro science teacher arrived two minutes late the first day, proceeded to ask “okay what class is this?”
Then when answered he just. started lecturing. he never took out notes.
About half way through he recommended a textbook but told us to pirate it because the author was a dick to him at a conference.
He has also said “brains are dumb and they hate you. Don’t trust them”
Should I be concerned?
#college#college classes#neurology#neuroscience#professor#I don’t know how to react#this is a high level class
745 notes
·
View notes
Text

"The main areas of serotonin research provide no consistent evidence of there being an association between serotonin and depression, and no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations. Some evidence was consistent with the possibility that long-term antidepressant use reduces serotonin concentration."
- The serotonin theory of depression: a systematic umbrella review of the evidence
https://www.nature.com/articles/s41380-022-01661-0
#sociology#psychology#mens mental health#mental health awareness#psychiatry#socialism#communism#biology#neurology#neuroscience#science memes#science#therapy#neurodivergent#neurodiversity
81 notes
·
View notes
Text

aww-ction potential
#art#digital art#artwork#anthro art#character design#furry#furry art#my art#original character#furry anthro#cat#kitty#kitten#neuron#neurology#neuroscience#illustration#illustrator#artists on tumblr
75 notes
·
View notes
Text





Brain Images Just Got 64 Million Times Sharper (Ultra-Sharp Brain Scan, Duke University)
#brain#neurology#neuroscience#brain imaging#medicine#medical#medical imaging#scientific imaging#biology#anatomy
130 notes
·
View notes
Text
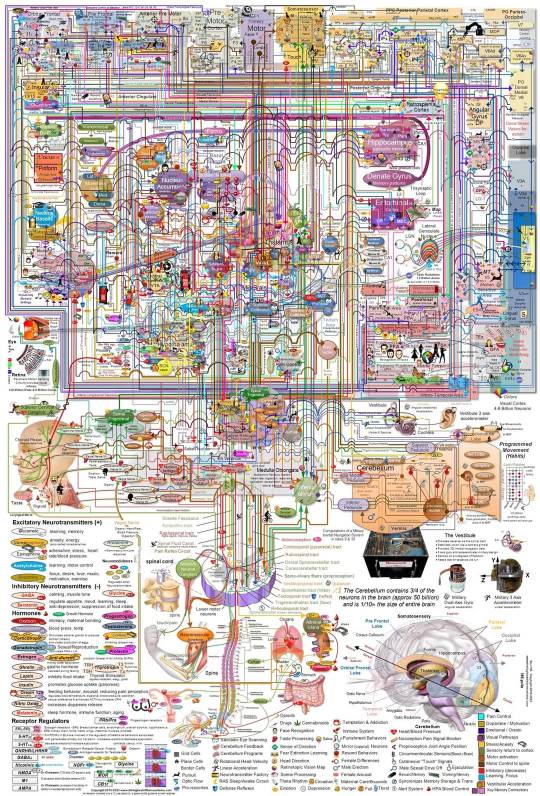
A full map of the human brain. Since it has a lot of information, you may want to go to the source to see it in higher resolution and to download it. The link is
https://www.thehighestofthemountains.com/images/thehighestofthemountains_brain_map_135a-185px.jpg
212 notes
·
View notes
Text
neuro family


#anime#art#artists on tumblr#moe art#moeart#anime art#biology#cells#cells at work#my art#neuro#neurons#original charater art#neurology#neuroscience#neuron#traditional art#cats#cat#cute cats#cats of tumblr
92 notes
·
View notes
Text

rushing a lab report from start to finish the day before it’s due — 09.29.24
#college#premed#studyblr#study motivation#studyspo#study blog#organic chemistry#biology#orgo#cell biology#undergrad student#undergraduate#neuroscience#neurology
32 notes
·
View notes
Text
"Caring for a pet helps stave off cognitive decline for people over 50 who live on their own, according to a new study of almost 8,000 participants.
Researchers found that pet ownership was associated with slower rates of decline in verbal memory and verbal fluency among the older adults who were living alone.
The study included 7,945 mostly-white British participants from the English Longitudinal Study of Ageing with an average age of 66.
Followed over an eight year period, more than a third of the group (35.1 percent) owned pets; about 30% of the group lived alone.
Previous studies suggested that solitary living is a risk factor for developing dementia and cognitive decline, but among those folks, raising dogs or cats was related to reduced loneliness.
Some research has found that pet ownership is associated with better verbal memory and executive function, but others failed to find any evidence.
The new research published in JAMA Network aimed to further explore the association between aging by oneself—a trend which has been on the rise over the past few decades—and pet ownership. And the results were clear.
“Pet ownership offset the associations between living alone and declining rates in verbal memory and verbal fluency,” said study corresponding author Professor Ciyong Lu, of Sun Yat-sen University in Guangzhou, China.
It was “a significant modifier” in all 3 associations—composite verbal cognition, verbal memory, and verbal fluency.
“Pet ownership was associated with slower rates of decline among older adults living alone.”
But owning a cat or dog did not make any difference for older people who lived with other people.
“These findings suggest that pet ownership may be associated with slower cognitive decline among older adults living alone.”
Prof. Lu is now calling for clinical trials that could help inform public health measures to address dementia among the elderly."
-via Good News Network, November 30, 2023
#dementia#alzheimers#neurology#neuroscience#medical news#aging#cognitive functions#psychology#healthcare#memory#united kingdom#uk#good news#hope
296 notes
·
View notes
Text
Is the Brain a Driver or a Steering Wheel?
This three part series summarizes what science knows, or thinks it knows, about consciousness. In Part 1 What Does Quantum Physics Imply About Consciousness? we looked at why several giants in quantum physics - Schrodinger, Heisenberg, Von Neumann and others - believed consciousness is fundamental to reality. In Part 2 Where Does Consciousness Come From? we learned the "dirty little secret" of neuroscience: it still hasn't got a clue how electrical activity in the brain results in consciousness.
In this concluding part of the series we will look at how a person can have a vivid conscious experience even when their brain is highly dysfunctional. These medically documented oddities challenge the materialist view that the brain produces consciousness.
Before proceeding, let's be clear what what is meant by "consciousness". For brevity, we'll keep things simple. One way of looking at consciousness is from the perspective of an outside observer (e.g., "conscious organisms use their senses to notice differences in their environment and act on their goals.") This outside-looking-in view is called behavioral consciousness (aka psychological consciousness). The other way of looking at it is the familiar first-person perspective of what it feels like to exist; this inside-looking-out view is called phenomenal consciousness (Barušs, 2023). This series is only discussing phenomenal consciousness.
Ready? Let’s go!

Source: Caltech Brain Imaging Center
A Hole in the Head
Epilepsy is a terrible disease in which electrical storms in the brain trigger seizures. For some people these seizures are so prolonged and frequent that drastic action is needed to save their lives. One such procedure is called a hemispherectomy, the removal or disconnection of half the brain. Above is an MRI image of a child who has undergone the procedure.
You might think that such radical surgery would profoundly alter the memory, personality, and cognitive abilities of the patient.
You would be wrong. One child who underwent the procedure at age 5 went on to attend college and graduate school, demonstrating above average intelligence and language abilities despite removal of the left hemisphere (the zone of the brain typically identified with language.) A study of 58 children from 1968 to 1996 found no significant long-term effects on memory, personality or humor, and minimal changes in cognitive function after hemispherectomy.
You might think that, at best, only a child could successfully undergo this procedure. Surely such surgery would kill an adult?
You would be wrong again. Consider the case of Ahad Israfil, an adult who suffered an accidental gunshot to the head and successfully underwent the procedure to remove his right cerebral hemisphere. Amazingly, after the five hour operation he tried to speak and went on to regain a large measure of functionality - and even earn a degree - although he did require use of a wheelchair afterwards.
Another radical epilepsy procedure, a corpus collosotomy, leaves the hemispheres intact but severs the connections between them. For decades it was believed that these split-brain patients developed divided consciousness, but more recent research disputes this notion. Researchers found that, despite physically blocking all neuronal communication between the two hemispheres, the brain somehow still maintains a single unified consciousness. How it manages this feat remains a complete mystery. Recent research on how psychedelic drugs affect the brain hints that the brain might have methods other than biochemical agents for internal communication, although as yet we haven't an inkling as to what those might be.
So what's the smallest scrape of brain you need to live? Consider the case of a 44-year-old white collar worker, married with two children and with an IQ of 75. Two weeks after noticing some mild weakness in one leg the man went to see his doctor. The doc ordered a routine MRI scan of the man's cranium, and this is what it showed.
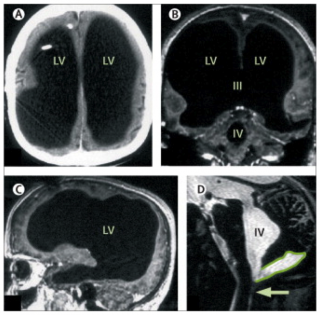
Source: The Lancet
What you are seeing here is a giant empty cavity where most of the patient's brain should be. Fully three quarters of his brain volume is missing, most likely due to a bout of hydrocephalus he experienced when he was six months old.

Artist: Tom Wright
Last Words
Many unusual phenomena have been observed as life draws to an end. We're going to look at two deathbed anomalies that have neurological implications.
The first is terminal lucidity, sometimes called paradoxical lucidity. First studied in 2009, terminal lucidity refers to the spontaneous return of lucid communication in patients who were no longer thought to be medically capable of normal verbal communication due to irreversible neurological deterioration (e.g., Alzheimers, meningitis, Parkinson's, strokes.) Here are three examples:
A 78-year-old woman, left severely disabled and unable to speak by a stroke, spoke coherently for the first time in two years by asking her daughter and caregiver to take her home. She died later that evening.
A 92-year-old woman with advanced Alzheimer’s disease hadn’t recognized her family for years, but the day before her death, she had a pleasantly bright conversation with them, recalling everyone’s name. She was even aware of her own age and where she’d been living all this time.
A young man suffering from AIDS-related dementia and blinded by the disease who regained both his lucidity and apparently his eyesight as well to say farewell to his boyfriend and caregiver the day before his death.
Terminal lucidity has been reported for centuries. A historical review found 83 case reports spanning the past 250 years. It was much more commonly reported in the 19th Century (as a sign that death was near, not as a phenomenon in its own right) before the materialist bias in the medical profession caused a chilling effect during the 20th Century. Only during the past 15 years has any systematic effort been made to study this medical anomaly. As a data point on its possible prevalence a survey of 45 Canadian palliative caregivers found that 33% of them had witnessed at least one case of terminal lucidity within the past year. Other surveys found have that the rate of prevalence is higher if measured over a longer time window than one year, suggesting that, while uncommon, terminal lucidity isn't particularly rare.
Terminal lucidity is difficult to study, in part because of ethical challenges in obtaining consent from neurocompromised individuals, and in part because its recent identification as a research topic presents delineation problems. However, the promise of identifying new neurological pathways in the brains of Alzheimer's and Parkinson's patients has gotten a lot of attention. In 2018 the US National Institute on Aging (NIA) announced two funding opportunites to advance this nascent science.
Due to the newness of this topic there will continue be challenges with the data for some time to come. However, its impact on eyewitnesses is indisputably profound.

Artist: Tom Wright
Near Death Experiences
The second deathbed anomaly we will take a look at are Near-Death Experiences (NDEs.) These are extraordinary and deeply personal psychological experiences that typically (but not always) occur during life-threatening emergencies such as cardiac arrest, falls, automobile accidents, or other traumatic events; they are also occasionally reported during general anesthesia. Much of the research in this area has focused on cardiac arrest cases because these patients are unconscious and have little to no EEG brain wave activity, making it difficult to account for how the brain could sustain the electrical activity needed to perceive and remember the NDE. This makes NDEs an important edge case for consciousness science.
NDEs are surprisingly common. A 2011 study published by the New York Academy of Sciences estimated that over 9 million people in the United States have experienced an NDE. Multiple studies have found that around 17% of cardiac arrest survivors report an NDE.
There is a remarkable consistency across NDE cases, with experiencers typically reporting one or more of the following:
The sensation of floating above their bodies watching resuscitation efforts, sometimes able to recall details of medical procedures and ER/hallway conversations they should not have been aware of;
Heightened sensations, including cases of blind people who report the ability to "see" during the NDE;
Extremely rapid mental processing;
The perception of passing through something like a tunnel;
A hyper-vivid life review, described by many experiencers as "more real than real";
Transcendent visions of an afterlife;
Encounters with deceased loved ones, sometimes including people the experiencer didn’t know were dead; and
Encounters with spiritual entities, sometimes in contradiction to their personal belief systems.
Of particular interest is a type of NDE called a veridical NDE. These are NDEs in which the experiencer describes independently verifiable events occurring during the period when they had minimal or no brain activity and should not have been perceived, let alone remembered, if the brain were the source of phenomenal consciousness. These represent about 48% of all NDE accounts (Greyson 2010). Here are a few first-hand NDE reports.
A 62-year-old aircraft mechanic during a cardiac arrest (from Sabom 1982, pp. 35, 37)
A 23-year-old crash-rescue firefighter in the USAF caught by a powerful explosion from a crashed B-52 (from Greyson 2021, pg. 27-29)
An 18-year-old boy describes what it was like to nearly drown (from the IANDS website)
There are thousands more first person NDE accounts published by the International Association for Near-Death Studies and at the NDE Research Foundation. The reason so many NDE accounts exist is because the experience is so profound that survivors often feel compelled to write as a coping method. Multiple studies have found that NDEs are more often than not life-changing events.
A full discussion of NDEs is beyond the scope of this post. For a good general introduction, I highly recommend After: What Near-Death Experiences Reveal about Life and Beyond by Bruce Greyson, MD (2021).

The Materialist Response
Materialists have offered up a number of psychological and physiological models for NDEs, but none of them fits all the data. These include:
People's overactive imaginations. Sabom (1982) was a skeptical cardiologist who set out to prove this hypothesis by asking cardiac arrest survivors who did not experience NDEs to imagine how the resuscitation process worked, then comparing those accounts with the veridical NDE accounts. He found that the veridical NDE accounts were highly accurate (0% errors), whereas 87% of the imagined resuscitation procedures contained at least one major error. Sabom became convinced that NDEs are real. His findings were replicated by Holden and Joesten (1990) and Sartori (2008) who reviewed veridical NDE accounts in hospital settings (n = 93) and found them to be 92% completely accurate, 6% partially accurate, and 1% completely inaccurate.
NDEs are just hallucinations or seizures. The problem here is that hallucinations and seizures are phenomena with well-defined clinical features that do not match those of NDEs. Hallucinations are not accurate descriptions of verifiable events, but veridical NDEs are. Also, it would be extraordinary to say the least that so many people would be hallucinating in similar ways.
NDEs are the result of electrical activity in the dying brain. The EEGs of experiencers in cardiac arrest show that no well-defined electrical activity was occurring that could have supported the formation or retention of memories during the NDE. These people were unconscious and should not have remembered anything.
NDEs are the product of dream-like or REM activity. Problem: many NDEs occur under general anesthesia, which suppresses dreams and REM activity. So this explanation cannot be correct.
NDEs result from decreased oxygen levels in the brain. Two problems here: 1) The medical effects of oxygen deprivation are well known, and they do not match the clinical presentation of NDEs. 2) The oxygen levels of people in NDEs (e.g., during general anesthesia) has been shown to be the same or greater than people who didn’t experience NDEs.
NDEs are the side effects of medications or chemicals produced in the brain (e.g. ketamine or DMT). The problem here is that people who are given medications in hospital settings tend to report fewer NDEs, not more; and drugs like ketamine have known effects that are not observed in NDEs. The leading advocate for the ketamine model conceded after years of research that ketamine does not produce NDEs (Greyson 2021, pg. 110).

Summing Up
In coming to the end of this series, let's sum up what we discussed.
Consciousness might be wired into the physical universe at fundamental level, as an integral part of quantum mechanics. Certainly several leading figures in physics thought so - Schrodinger, Heisenberg, Von Neumann, and more recently Nobel Laureates Roger Penrose, Eugene Wigner, and physicist Henry Stapp.
Materialist propaganda notwithstanding, neuroscience is no closer to identifying Neural Correlates of Consciousness (NCCs) than it was when it started. The source of consciousness remains one of the greatest mysteries in science.
Meanwhile, medical evidence continues to pile up that there is something deeply amiss with the materialist assumption that consciousness is produced by the brain. In a sense, the challenge that NDEs and Terminal Lucidity pose to consciousness science is analogous to the challenge that Dark Matter poses to physics, in that they suggest that the mind-brain identity model of classic materialist psychology may need to be rethought to adequately explain these phenomena.
Ever since the Greeks, science has sought to explain nature entirely in physical terms, without invoking theism. It has been spectacularly successful - particularly in the physical sciences - but at the cost of excluding consciousness along with the gods (Nagel, 2012). What I have tried to do in this series is to show that a very credible argument can be made that materialism has the arrow of causality backwards: the brain is not the driver of consciousness, it's the steering wheel.
I don't think we are yet ready to say what consciousness is. Much more research is needed. I'm not making the case for panpsychism, for instance - but I do think consciousness researchers need to throw off the assumption drag of materialism before they're going to make any real progress.
It will be up to you, the scientists of tomorrow, to make those discoveries. That's why I'm posting this to Tumblr rather than an academic journal; young people need to hear what's being discovered, and the opportunities that these discoveries represent for up and coming scientists.
Never has Planck's Principle been more apt: science advances one funeral at a time.
Good luck.
For Further Reading
Barušs, Imants & Mossbridge, Julia (2017). Transcendent Mind: Rethinking the Science of Consciousness. American Psychological Association, Washington DC.
Barušs, Imants (2023). Death as an Altered State of Consciousness: A Scientific Approach. American Psychological Association, Washington DC.
Batthyány, Alexander (2023). Threshold: Terminal Lucidity and the Border of Life and Death. St. Martin's Essentials, New York.
Becker, Carl B. (1993). Paranormal Experience and Survival of Death. State University of New York Press, Albany NY.
Greyson, Bruce (2021). After: A Doctor Explores What Near-Death Experiences Reveal about Life and Beyond. St. Martin's Essentials, New York.
Kelly, Edward F.; Kelly, Emily Williams; Crabtree, Adam; Gauld, Alan; Grosso, Michael; & Greyson, Bruce (2007). Irreducible Mind: Toward a Psychology for the 21st Century. Rowman & Littlefield, New York.
Moody, Raymond (1975). Life After Life. Bantam/Mockingbird, Covington GA.
Moreira-Almeida, Alexander; de Abreu Costa, Marianna; & Coelho, Humberto S. (2022). Science of Life After Death. Springer Briefs in Psychology, Cham Switzerland.
Penfield, Wilder (1975). Mystery of the Mind: A Critical Study of Consciousness and the Human Brain. Princeton Legacy Library, Princeton NJ.
Sabom, Michael (1982). Recollections of Death: A Medical Investigation. Harper and Row Publishers, New York.
van Lommel, Pim (2010). Consciousness Beyond Life: The Science of the Near-Death Experience. HarperCollins, New York.
#consciousness#cognitive science#near death experiences#nde#terminal lucidity#terminal illness#cognitive neuroscience#paradoxical lucidity#hemispherectomy#corpus collosotomy#psychadelic#psychonaut#psychonauts#psilocybin#lsd#ketamine#materialism and its discontents#neurology#neuropsychology#philosophy of mind#brain#quantum physics#consciousness series
104 notes
·
View notes
Text
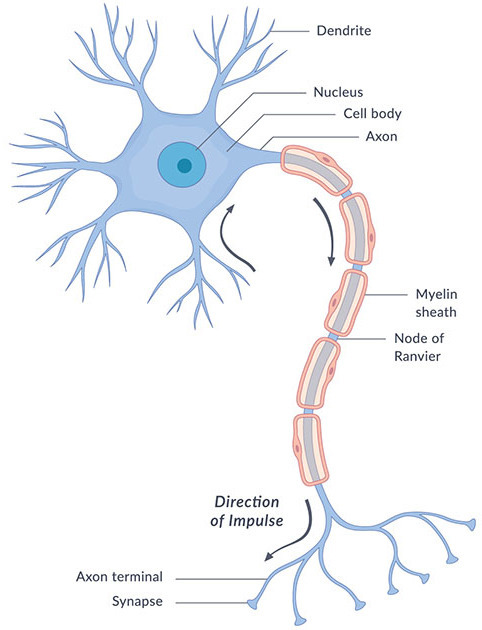
Unraveling the Wonders of the Neuron and Brain (Part 1)
Hey there, Tumblr fam! Today, let's dive deep into the intricate world of neurons and the brain. 🧠✨
Anatomy of a Neuron
Neurons are the building blocks of the nervous system, responsible for transmitting information throughout your body. They have a unique structure, consisting of three main parts:
Cell Body (Soma): This is like the neuron's control center. It contains the nucleus, which houses the cell's DNA and controls its activities.
Dendrites: These branch-like extensions protruding from the cell body are the neuron's antennae. They receive signals from other neurons or sensory receptors, transmitting these signals to the cell body.
Axon: Think of the axon as the neuron's transmission line. It's a long, slender, cable-like structure that carries signals away from the cell body, toward other neurons or target cells.
At the end of the axon, you'll find axon terminals, where neurotransmitters are released to communicate with the next neuron or target cell.
Physiology of a Neuron
Neurons are all about transmitting information through electrical impulses and chemical signals. Here's a quick rundown:
Resting Membrane Potential: Neurons have a resting state where the inside is negatively charged compared to the outside due to the uneven distribution of ions (like sodium and potassium) across the cell membrane. This creates a potential difference called the resting membrane potential.
Action Potential: When a neuron receives a strong enough signal (usually from dendrites), it can generate an action potential—a rapid change in membrane potential. This electrical signal travels down the axon like a wave.
Synaptic Transmission: When the action potential reaches the axon terminals, it triggers the release of neurotransmitters into the synapse, the tiny gap between neurons. These chemicals bind to receptors on the next neuron, initiating a new electrical signal.
The Marvelous Brain
Now, let's shift our focus to the brain—the command center of your entire nervous system. 🌟
Your brain consists of various regions, each with specific functions. Here are a few key areas:
Cerebrum: This is the largest part and is divided into two hemispheres, each responsible for various cognitive functions like thinking, memory, and sensory perception.
Cerebellum: Located at the back of your brain, it plays a crucial role in balance, coordination, and fine motor skills.
Brainstem: Situated at the base of the brain, it controls basic life-sustaining functions like breathing and heart rate.
Hippocampus: Essential for memory formation and storage.
Amygdala: Involved in processing emotions and emotional memories.
And there's so much more to explore!
References:
Bear, M. F., Connors, B. W., & Paradiso, M. A. (2016). "Neuroscience: Exploring the Brain." Lippincott Williams & Wilkins.
Purves, D., et al. (2017). "Neuroscience." Sinauer Associates, Inc.
Kandel, E. R., Schwartz, J. H., & Jessell, T. M. (2012). "Principles of Neural Science." McGraw-Hill Education.
These references will provide you with in-depth insights into the fascinating world of neurons and the brain. Remember, your brain is a universe waiting to be explored! 🌌💡🔬
Stay curious, Tumblr pals! 😊🧠

#neuroscience#biology#science#college#education#school#student#medicine#doctors#health#healthcare#neurology#brains#psychology#psychiatry
167 notes
·
View notes
Text
NEURO CRITICAL - GENDER CRITICAL AUTISTICS
NEURO CRITICAL - understanding Neurological Reality and Neurological Differences between Brains
GENDER CRITICAL - understanding Biological Reality and Biological Differences between Sexes
NEURO CRITICAL
Understanding Neurological Differences between Brains
Acknowledgment that Brains Matter
Builds the foundation for all neurological understanding, education, advocacy, rights, eg. Autism Advocacy
People cannot change brains
Neuro Affirming Care affirms that you are your neurology and doesn’t try to “fix” it, instead it embraces acceptance
This is called Neurological Reality
This is not Neurophobia
Evidence based.
A conversation between a Neuro Critical person and a Neuro-denier:
What’s the difference between an Autistic person and a Narcissist?
“Nothing! You’re not allowed to talk about differences, that’s neurophobic! You bigot!”
What about the differences between Autism and Schizophrenia? You know, so you can treat them with the correct support or medication? Is it okay to be Neuro Critical in these circumstances?
“No, you right wing monster! You’re not being progressive!”
Am I allowed an Autism-only space where I am free to associate with other autistic people and be free from stigma?
“No, for god’s sake are you not listening!? People who are not autistic reserve the right to invade those spaces and there’s nothing you can do about it!”
Oh shit, looks like all the Autism Advocates are about to be in big trouble! Turns out they’ve been pedaling a false narrative that autism exists and is somehow different to things that are not autistic. Oops! All that research gone to waste! They best start denying everything they know before they get found out for being bigots! STOP AUTISM ADVOCACY! It’s not inclusive to people who are not autistic!
People who advocate for Autism are what we call Neuro Critical, and this means they believe there are differences between brains and that you can’t change brains and that brains matter in certain circumstances. EVIL BASTARDS! They must be stopped from spreading this hateful rhetoric! Join me in the latest Social Justice Movement by spreading the word that Neuro Critical = Neurophobia. Let’s not allow them to spread hate and misinformation about brains! It’s bad for society and we don’t need to accept the brains we’re born with, nor should being born autistic matter - it doesn’t! I don’t recognize your autism at all! That would make me neurophobic wouldn’t it? Duh!
*****
Imagine if we told autistic people that people who understand the difference between autistic ppl and neurotypical ppl (Neuro Critical) is akin to hate? Autistic ppl wouldn't stand a chance at forging connections with other people in society if they thought neuro critical was hateful and bigoted. Nor would they be able to advocate for autism if it was classified as Neurophobia to talk about autism and exclude neurotypicality from autism research or autism-only spaces. Neuro Critical in this sense builds the foundation that enables Autism Advocacy - highlighting the neurological differences between autistic and neurotypical so we can provide tailored, appropriate support when and where necessary. (OMG, such a confusing concept, it must be phobia! It's just like those transphobic Gender Critical’s talking about biology and stuff!).
Autism Advocates need to join in the conversations and not shut down Gender Critical Autistic Voices, especially if that is because you are misinformed about what gender critical is. (Does seeing this comparison between NEURO CRITICAL & GENDER CRITICAL help you see how perfectly ordinary it is and based in reality, not phobia?)
We should be engaging with each other and having meaningful discussions, respectful arguing of points and nuanced perspectives that allow for open dialogue and curious minds to come together and learn.
*
You may be wondering why I left the word IMMUTABLE out of this?
Gender Critical talks about the immutability of sex. This is not the same in brains.
“No, the brain is not immutable…but is instead a dynamic organ that changes throughout life. This process is known as neuroplasticity, which is the brain's ability to adapt, evolve, and grow throughout life. The brain's ability to change is due to its ability to grow new nerve connections in response to sensory stimulation from the environment. This process can be seen in many ways, such as when someone learns a new language, recovers from an injury, or adapts to a new environment. The brain's health can also be improved by making certain lifestyle choices, such as: Eating a healthy diet, Getting enough sleep, Exercising regularly, Relaxing the mind, and Building a network of friends and family.” Brains, unlike sex, are not immutable. Brains are neuroplastic which means they can change, such as they can repair themselves after injury/trauma, we can learn and expand and create new neural pathways etc. However, we cannot for example stop being autistic. Nor can someone turn into an autistic person. Nor should we ever deny a patient's autism when helping them. We ARE autistic neurologically and THAT cannot be changed. My words on this image are in reference to neuro affirming care for autistic ppl which works WITH your autism, not against it. Autism therapies used to be based on helping you be more neurotypical (as in, less autistic aka conversion therapy) which was harmful to autistic ppl. This is not talking about therapy for things like overcoming trauma, unlearning bad behaviours, help with OCD, etc, which we can help to change through therapy and with the helpful reality of our brains being neuroplastic to allow these changes with practice. The only way you can help your brain is by accepting it, understanding it and working with it and appropriately pushing it to get better. We wouldn’t deny a depressed person is depressed, we would seek to understand their depression and help them learn new ways to get through depression and build new neural pathways to a healthier mental health. We wouldn’t deny an autistic person is autistic. We work with reality and grow and expand from there. Gender affirming care goes against biology and affirms we are not our biology - which is harmful. At no point ever has a person biologically changed sex. They are not plastic like brains with the ability to change like that - just like you can’t change from autistic to not autistic.

#autistic voices#autistic#autism#gender#identity#neurodiverse#gender critical#identity politics#neurodiversity#gender non conforming#nerf#terfblr#terfsafe#terfism#terfsruntumblr#radical feminist safe#radblr#feminism#radical feminist community#gender critical feminism#gender critical feminist#radical feminism#radical feminists do interact#neurodivergent#actually neurodiverse#neurospicy#neurodiverse stuff#neuroscience#neurology#gender stuff
25 notes
·
View notes