#hypoxia
Explore tagged Tumblr posts
Text
Humans are not yet done cooking. We're continuing to evolve and adjust to the world around us, the records of our adaptations written in our bodies. We know that there are some environments that can make us unwell. Mountain climbers often succumb to altitude sickness – the body's reaction to a significant drop in atmospheric pressure, which means less oxygen is taken in with each breath. And yet, in high altitudes on the Tibetan Plateau, where oxygen levels in the air people breathe are notably lower than lower altitudes, human communities thrive.
Continue Reading.
145 notes
·
View notes
Text
Click & Detect
Click3D: a method using click chemistry (a class of reactions that make molecules observable) that achieves high-resolution 3D fluorescence imaging of whole organs at unprecedented depth – for example, imaging hypoxia (inadequate tissue oxygen) in a tumour (as shown here) or in the mouse whole brain
Read the published research article here
Video from work by Iori Tamura and colleagues
Department of Chemistry and Biotechnology, Graduate School of Engineering, The University of Tokyo, Bunkyo-ku, Tokyo, Japan
Video originally published with a Creative Commons Attribution 4.0 International (CC BY-NC 4.0)
Published in Science Advances, July 2024
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#immunofluorescence#cancer#biology#3d image#imaging#hypoxia#brain#neuroscience#click chemistry#click#chemistry
12 notes
·
View notes
Text
James gives off Jake Peralta vibes in that B99 episode with the Safe House




ARE THEY HYPOXIC ??
#“i shot a watermelon once”#“it's everything you'd want it to be”#b99#the expanse#quotes#fandom quotes#james holden#my blorbos#bobbie draper#naomi nagata#hypoxia
489 notes
·
View notes
Text
youtube
#Tumor microenvironment#cancer cells#stromal cells#immune cells#extracellular matrix#fibroblasts#macrophages#T cells#hypoxia#angiogenesis#vascularization#inflammation#oxidative stress#epithelial-mesenchymal transition#metastasis#cytokines#growth factors#exosomes#immune evasion#drug resistance.#Youtube
0 notes
Text
Dementia: Can You Prevent it?
As I get older, every time I forget something I wonder if dementia is imminent. Forgetfulness is common as we age, but just how forgetful is normal, and what level is more worrisome? We all joke about having “senior moments” but when do the jokes become reality? What is Dementia The Center for Disease Control and Prevention (CDC) describes dementia as the following: Dementia is not a specific…
0 notes
Text

The Science Research Manuscripts of S. Sunkavally, p 538.
#mas extinction#heavy water levels#comet Hale Bopp#third tail#sodium ions#hypernatraemia#crosslinking of collagen#atherosclerosis#hypoxia#radioprotection#birds#height of flight#influenza pandemic#ventricular fibrillation#Roy Walford#Cynolebias bellotti#autoimmunity#IDDM#killer cells#hypothermia
0 notes
Text
We're basically just allergic to showers at this point. We get so hypoxic that our hands—and our feet, if we're in there long enough—turn blue. (Cyanosis, yippee.) Not to mention, our heart right skyrockets and we start to feel faint, and it's so bad to the point that we have to sit down for either a super long time or until we're done bathing.
Yay, medical issues!
Front: Evan (xe/they), Riley (they/them), Michael (he/corpse/death)
#tw hypoxia#hypoxia#RAD#reactive airway disorder#reactive airway disease#possible POTS#osdd#osdd system#plural#system
0 notes
Text
Hypoxic Love

0 notes
Text
guide to character ages
just so the timeline is a little clearer to people :)
Starkiller - 22
Hypoxia - 20
Calypso (Sofie) - 25, and she was recruited into the team at 18
Hemera (Zoey) - 23, and she was recruited at 17
Nyx (Marquis) - 25, and he was recruited at 19
Atropos (Maia) - 20, and she was recruited at 15
Calypso was recruited first, at 18, then a year later Hemera and Nyx joined. Three months after that, Atropos was added. They trained together for two years, and have been working together in the field for three more at the start of the comic.
#good guys#bad guys#starkiller#TheCuspOfBrilliance#comic#jaybee#this is borderline nonsensical#calypso#hemera#nyx#atropos#hypoxia
0 notes
Text
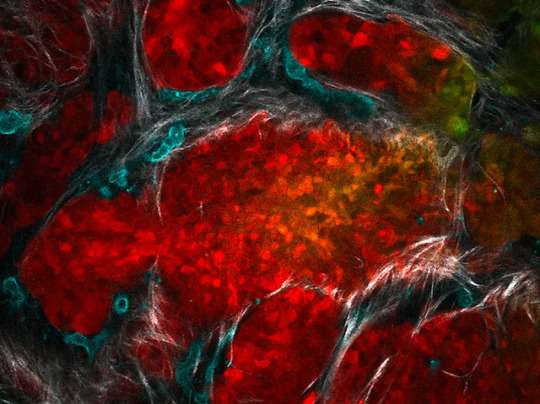
Seeing Low Oxygen
Visualising tumour cell oxygen deprivation (hypoxia) in a living mouse model with pancreatic cancer using a new fluorescence microscopy approach
Read the published research paper here
Image from work by Timothy Samuel and colleagues
Princess Margaret Cancer Centre, University Health Network, Toronto, Canada
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in Science Advances, June 2023
You can also follow BPoD on Instagram, Twitter and Facebook
7 notes
·
View notes
Text
youtube
youtube
#hyperbaric chamber#hyperbaric oxygen chamber#hyperbaric oxygen#health#chronic illness#chronic pain#periodicty is the key#self help#sound healing#healing frequencies#scalar field#hypoxia#nervous system
0 notes
Text
I always worry I'm not gonna wake up and the fact it's not unrealistic or exaggerated kinda sucks. I genuinely might not wake up tomorrow.
My will drop as low as 79% in my sleep, and doctors don't even care. I can't move in the morning, and I'm losing more and more memory and speech.
0 notes
Text
Hypoxia
Have you ever been low on air? Not enough to worry about death or unconsciousness, but enough that you can't help but laugh. Normal breathing isn't enough, so your body must think the convulsions might help. You want to be free, to breath normally, but they won't stop sitting on your chest. After all, you are laughing, so it must be a fun game. You want it to stop, but at least you are getting attention, acknowledged as a person, as someone who exists in this world.
0 notes
Text
youtube
#Hypoxia#cancer#tumor microenvironment#HIF-1α#HIF-2α#angiogenesis#tumor vasculature#metabolic reprogramming#epithelial-to-mesenchymal transition#therapy resistance#VEGF#immune evasion#radiotherapy resistance#chemotherapy resistance#tumor oxygen deprivation#genomic instability#epigenetics#oncology research#targeted therapies#precision oncology.#Youtube
0 notes
Text

I. Polycythemia Diagnosis:
A. Clinical Assessment:
• The diagnostic process for polycythemia commences with a thorough examination of medical history and physical condition to detect signs indicative of erythrocytosis, assess potential risk factors (e.g., smoking habits, family history of thrombosis), and uncover underlying causes.
• Special attention should be given to symptoms of hyperviscosity syndrome (e.g., headaches, dizziness), skin manifestations (e.g., erythromelalgia), and signs of organ enlargement (e.g., splenomegaly, hepatomegaly).
B. Laboratory Tests:
• Laboratory investigations are crucial for diagnosing polycythemia and understanding its underlying mechanisms. Essential tests include a complete blood count (CBC) with differential, examination of peripheral blood smear, and measurement of serum erythropoietin levels.
• Additional tests, such as JAK2 mutation analysis, bone marrow biopsy, and molecular testing for other mutations associated with myeloproliferative neoplasms (e.g., CALR, MPL), may be necessary to confirm the diagnosis of PV and rule out alternative causes.
C. Imaging Techniques:
• Imaging methods like ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) may be used to evaluate organ enlargement (e.g., splenomegaly, hepatomegaly) and identify potential underlying factors for secondary polycythemia (e.g., renal tumors).
II. Polycythemia Treatment:
Management of polycythemia aims to alleviate symptoms, lower the risk of thrombotic complications, and prevent disease progression. Treatment approaches may vary depending on the underlying cause and severity, often involving a combination of strategies:
A. Phlebotomy (Venesection):
• Phlebotomy is the primary treatment for PV, involving the removal of excess blood to achieve target hematocrit levels (<45% in men, <42% in women).
• Regular phlebotomy sessions usually start at diagnosis and are adjusted based on individual response and disease activity.
B. Cytoreductive Therapy:
• Drugs like hydroxyurea, interferon-alpha, and ruxolitinib may be used in PV patients who do not respond to or cannot tolerate phlebotomy.
• These drugs work by suppressing abnormal hematopoietic proliferation and reducing the risk of blood clotting, with hydroxyurea being the most commonly used and studied cytoreductive drug in PV.
C. Antiplatelet Therapy:
• Aspirin and other antiplatelet drugs are often prescribed to PV patients with a history of blood clots or other high-risk factors to lower the risk of arterial thrombosis.
• Aspirin is usually started at low doses (e.g., 81 mg daily) and may be combined with cytoreductive therapy for better thromboprophylaxis.
D. Treating Underlying Conditions:
• Management of secondary polycythemia focuses on addressing the root cause to relieve hypoxia-induced erythropoiesis and prevent disease progression.
• Interventions may include oxygen therapy for patients with chronic respiratory problems, correction of hemoglobin disorders or other genetic issues, and surgical removal of erythropoietin-secreting tumors.
E. Lifestyle Changes:
• Lifestyle adjustments such as quitting smoking, maintaining a healthy weight, regular physical activity, and proper hydration are vital for improving clinical outcomes and reducing cardiovascular risks in polycythemia patients.
Doctors suggest undergoing regular health checkups for the early diagnosis and treatment of polycythemia. You can choose to undergo a regular full body health checkup at Jaslok Hospital Mumbai, which is one of India's best hospitals for the early detection and management of blood disorders.
#polycythemia#headache#dizziness#CBC#biopsy#splenomegaly#hepatomegaly#phlebotomy#cytoreductive therapy#hematopoietic proliferation#aspirin#antiplatelet therapy#hypoxia#respiratory problems#blood disorders#full body health checkup#regular health checkups
0 notes
Photo

Climate Change Impact: Oxygen Depletion Threatens Marine Life | CeBoz.com
Rising temperatures from climate change depleting oxygen in coastal waters, threatening marine life
0 notes