#autoimmunity
Explore tagged Tumblr posts
Text

#autoimmune#lupus#lupus warrior#spoonie#fibromyalgia#lupus advocate#lupus fighter#pots syndrome#postural orthostatic tachycardia syndrome#potsie#hypermobile ehlers danlos#ehlers danlos life#autoimmine disease#autoimmunity
76 notes
·
View notes
Link
17 notes
·
View notes
Text



ArthrImmusyc

An Immusyc term related to one's arthritis, whatever type/form one may have, affecting one's immune system in some way

Made with Immunol compromised/autoimmune arthritic conditions in mind such as rheumatoid, psoriatic, scleroderma, lupus, ankylosing spondylitis, gout and more.
Many people may have an undiagnosed arthritic condition and be autoimmune, this term is meant to encompass these people as well.

Tagging:
@sanguinaryfreaks , @hewasanamericangirl and @the-church-of-strabismus

This flag is meant for personal use, commercial use is not permitted.
Do not re-upload my flags anywhere, do not claim as your own etc.

#nemesies#coining blog#cpunk coining#crip coins#crypt flags#crypt terms#endos dni#flag coining#disabled coining#arthritis#arthritic conditions#autoimmune#autoimmunity#autoimmune arthritis#immusyc flags#immusyc terms#immune system#immusyc
7 notes
·
View notes
Text

Malina: What is life? Me: Whatever can’t be lived.
I am writing with my burnt hand about the nature of fire
#ingeborg bachmann#malina#selfportrait#selfshot#the mirror scene#antique mirror#Giacomo Manzoni#Werther Schroeter#homemade landscapes#i wear my heart on my skin#inflamed#autoimmunity
4 notes
·
View notes
Text
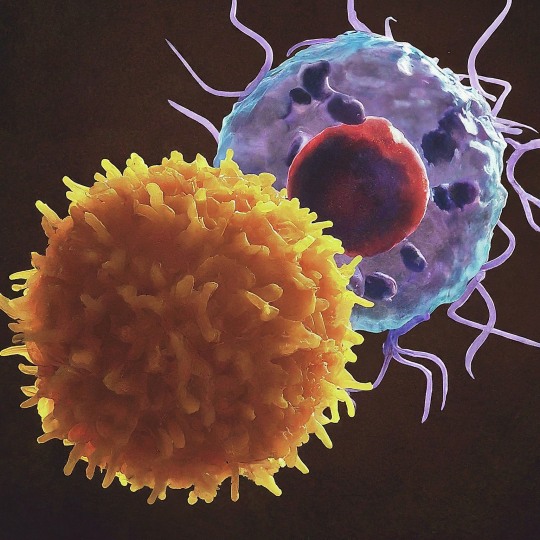
The T Cell Landscape
T cells, a critical component of the adaptive immune system, stand as the body's elite force in combatting infections and diseases. These specialized lymphocytes boast remarkable diversity, each type playing a distinct role in orchestrating a targeted and effective immune response.
T cells, like all blood cells, originate from hematopoietic stem cells residing in the bone marrow. However, their training ground lies within the thymus, a specialized organ located in the chest. Here, they undergo a rigorous selection process known as thymocyte education. During this process, immature T cells, called thymocytes, are presented with self-antigens (molecules unique to the body) by special cells. Thymocytes that bind too strongly to these self-antigens are eliminated, preventing them from attacking healthy tissues later. Only thymocytes that demonstrate the ability to recognize foreign invaders while exhibiting tolerance to self are released into the bloodstream as mature T cells.
Following this rigorous training, mature T cells exit the thymus and embark on their patrol, circulating throughout the bloodstream and lymphatic system. They remain vigilant, constantly scanning for their specific targets �� antigens. Antigens are foreign molecules, such as fragments of viruses, bacteria, or even cancerous cells, that trigger the immune response.
The hallmark of a T cell is its T cell receptor (TCR), a highly specialized protein complex embedded on its surface. This receptor acts like a lock, uniquely shaped to fit a specific antigen, the "key." Each T cell develops a unique TCR capable of recognizing only a single antigen, enabling a highly specific immune response.
But how do T cells encounter these hidden antigens lurking within infected or cancerous cells? This critical role is played by antigen-presenting cells (APCs). APCs, such as macrophages and dendritic cells, engulf pathogens or abnormal cells, break them down into smaller fragments (peptides), and present them on their surface complexed with major histocompatibility complex (MHC) molecules. MHC molecules act as identification tags, allowing T cells to distinguish between "self" and "non-self." When a T cell's TCR encounters its specific antigen bound to an MHC molecule on an APC, a dance of activation begins. The T cell becomes stimulated, and a cascade of signaling events is triggered. This leads to the T cell's proliferation, producing an army of clones specifically tailored to combat the recognized threat.
T cells are not a single, monolithic entity. They comprise a diverse population, each type with a specialized function:
Helper T Cells (Th Cells):
Helper T cells, often abbreviated as Th cells, play a central role in coordinating immune responses. They express the CD4 surface marker and can recognize antigens presented by major histocompatibility complex class II (MHC-II) molecules. Subtypes of helper T cells include Th1, Th2, Th17, and regulatory T cells (Tregs), each with distinct functions and cytokine profiles.
Th1 cells mediate cellular immunity by activating macrophages and cytotoxic T cells, crucial for defense against intracellular pathogens.
Th2 cells are involved in humoral immunity, promoting B cell activation and antibody production, thus aiding in defense against extracellular parasites.
Th17 cells contribute to the immune response against extracellular bacteria and fungi, producing pro-inflammatory cytokines. Regulatory T cells (Tregs) maintain immune tolerance and prevent autoimmunity by suppressing excessive immune responses.
Cytotoxic T Cells (Tc Cells):
Cytotoxic T cells, also known as Tc cells or CD8+ T cells, are effector cells responsible for directly killing infected or aberrant cells. They recognize antigens presented by MHC class I molecules on the surface of target cells. Upon activation, cytotoxic T cells release perforin and granzymes, inducing apoptosis in target cells and eliminating the threat.
Memory T Cells:
Memory T cells are a long-lived subset of T cells that persist after the clearance of an infection. They provide rapid and enhanced immune responses upon re-exposure to the same antigen, conferring immunological memory. Memory T cells can be either central memory T cells (TCM), residing in lymphoid organs, or effector memory T cells (TEM), circulating in peripheral tissues.
γδ T Cells:
Unlike conventional αβ T cells, γδ T cells express a distinct T cell receptor (TCR) composed of γ and δ chains. They recognize non-peptide antigens, such as lipids and metabolites, and are involved in immune surveillance at epithelial barriers and responses to stress signals.
Beyond the Battlefield: The Expanding Roles of T Cells: The remarkable capabilities of T cells have opened doors for several groundbreaking applications in medicine:
Vaccines: By presenting weakened or inactivated forms of pathogens, vaccines "train" the immune system to generate memory T cells. This prepares the body to recognize and rapidly eliminate the real pathogen upon future exposure, preventing disease.
Cancer immunotherapy: CAR T-cell therapy, a revolutionary approach, genetically engineers a patient's own T cells to express chimeric antigen receptors (CARs) that recognize and target specific cancer cells. These "supercharged" T cells are then reintroduced into the patient, unleashing a potent attack against the tumor.
Autoimmune disease treatment: Researchers are exploring ways to manipulate T cells to suppress harmful immune responses that underlie autoimmune diseases like rheumatoid arthritis and multiple sclerosis.
The diverse array of T cells underscores the immune system's complexity and adaptability in mounting tailored responses against a myriad of threats. From orchestrating immune reactions to maintaining tolerance and establishing long-term immunity, T cells play multifaceted roles in safeguarding the body's health. Understanding the intricacies of T cell biology not only sheds light on immune-mediated diseases but also paves the way for developing novel therapeutic strategies harnessing the power of the immune system.
T cells represent a fascinating aspect of immunology, with their diversity and specificity driving the complexity of immune responses. As research advances, further insights into T cell biology promise to revolutionize immunotherapy and enhance our ability to combat diseases ranging from infections to cancer. By understanding and harnessing their power, we can unlock new avenues for protecting and improving human health.
#science sculpt#life science#science#molecular biology#biology#biotechnology#artists on tumblr#t cells#T helper cells#autoimmune#autoimmunity#helathcare#immunology#immunotherapy#medical care#cancer#human health#research#scientific research#the glass scientists#scientific illustration#research scientist
11 notes
·
View notes
Text

The Science Research Notebooks of S. Sunkavally, p431.
#neuropathy#paresthesia#demyelination#diabetic neuropathy#fibroblasts#interferon#cortisol#autoimmunity#sleep#ionic product of water#gammapathy#satyendra sunkavally#theoretical biology#manuscript#diaries#cursive handwriting
2 notes
·
View notes
Text

#biology memes#studyblr#autoimmunity#i love nerd humor#my creativity peaked at their hair as t cell receptors#anyway studying for finals is going well
19 notes
·
View notes
Text
Mikhaila Peterson Reports Back After 5 Years on Carnivore Diet
youtube
#Mikhaila Peterson#Carnivore Diet#autoimmunity#mental health#women's health#health#videos#Kent Carnivore
4 notes
·
View notes
Text
Autoimmune - 6








#cam.txt#anti endo#anti endo userboxes#anti endogenic#disabled system#system punk#system userbox#system boxes#this system#sys blog#system blog#userbox blog#autoimmunities#autoimmine disease#autoimmunity#autoimmune#bahcets disease#fibromyalgia#gpa#mixed connective tissue disease#mctd#granulomatosis with polyangiitis
2 notes
·
View notes
Text
Which autoimmune archetype are you? 🤔
Find out your autoimmune profile by taking our short quiz here: https://brightlythrive.com/take-our-quiz/

#autoimmunity#autoimmuneconditions#chronicillness#strategies#healing#community#meal planning#alternative therapy#holistic health
2 notes
·
View notes
Text

#autoimmune#lupus#lupus warrior#spoonie#fibromyalgia#lupus advocate#lupus fighter#pots syndrome#postural orthostatic tachycardia syndrome#potsie#autoimmine disease#autoimmunity#hypermobile ehlers danlos#ehlers danlos life#lupusadvocate
33 notes
·
View notes
Text
Several of the most prevalent new-onset autoantibodies have, to our knowledge, not been described previously, including the three with the highest prevalence, i.e., anti-CCDC63 (coiled-coil domain-containing protein 63), anti-TRIM63 (E3 ubiquitin-protein ligase TRIM63), and anti-SNURF (SNRPN upstream reading frame protein)
24 notes
·
View notes
Text
...Some people know me as hope...
So cower at the man I've become when I sing from the top of my lungs
That I won't retire, I'll stand in your fire, inspire the meek to be strong
And when I am gone, I will rise in the music that I left behind
Ferocious, persistent, immortal like you, we’re a coin with two different sides
youtube
#powerful#this is so beautiful#this is raw#real#Ren#singer#“Hi Ren”#mental health#mental illness#struggles with health#struggles with physical health#struggles with mental health#guitar#music recs#spoken word#poetry#autoimmunity#eternal dance#we are human beings#watch it and rewatch it#Youtube
7 notes
·
View notes
Text
I think what people underestimate most about chronic and repeated childhood trauma is that it truly effects every single proportion of you.
There is some theory at the moment that a component of depression is inflammation. This isn’t just out of left field, since clinical encephalitis is well demonstrated to cause psychosis. Encephalitis is inflammation of the brain and it causes neuropsychiatric symptoms like you have never seen before- and is usually quite hard to detect on labs until someone starts having siezures- by which point you’re in shit.
This is partly why fibromyalgia symptoms are treated with antidepressants, and why depression can have some wicked somatic symptoms- they’re not two seperate things- treat the body to treat the brain, or if the brain is convinced the body is being hurt because you feel some sort of pain all the time- emotional or psychological- treat the brain.
It’s not as simple as one thing causing the other either. Inflammation is a mistaken immune response. One of the major effects of cortisol, the hormone released when you are chronically stressed, is that you stop producing things you don’t need to produce. Processes stop working where they should and can even affect your immune system. Recurrent trauma stops your body from producing it’s own natural inflammatories.
Stress also causes epigenetic changes. These are heritable. These can mute and activate genes- most notably those responsible for stopping cancer. It is possible for your mother or father to have a stressful period in life, epigenetic changes to happen, and then for you to be born with those already happening.
The majority of autoimmune conditions have stress- acute or chronic- as a major trigger factor. Stress isn’t just in the head. You produce hormones, you make protiens, you make antibodies- sometimes ones you shouldn’t. Mental and physical health aren’t too seperate, especially not when it comes to this area.
What I’m saying is that what you’ve gone through isn’t just in your head. Chances are it’s in your body as well. So don’t expect to just feel it in your head.
7 notes
·
View notes
Text
Snippets—Women and autoimmune disease, the first wine, early Americans, and how cats purr
For Sunday: snippets of science news on some of my favourite things in life (well, the favourite things we can talk about in polite company): cats, wine, and humans in the Americas, plus one of my ongoing personal concerns, autoimmune disease. Some weight
Some of this stuff dates from late last year when I was too busy with Menewood stuff to comment. But as some of my favourite things in life (well, the favourite things we can talk about in polite company) are cats, wine, and history, and as one of my ongoing personal concerns is autoimmune disease, I thought, Eh, let’s combine them. We’ll start with the weighty stuff first then lighten up a…
View On WordPress
2 notes
·
View notes