#Neurology clinic
Explore tagged Tumblr posts
Text
The Link Between Sleep and Neurological Health: What You Need to Know

Sleep is a fundamental aspect of our daily lives, yet it is often overlooked in discussions about health and well-being. Emerging research highlights the profound impact of sleep on neurological health, revealing that the quality and duration of sleep significantly influence brain function and overall mental well-being. Understanding this relationship is crucial for maintaining a healthy brain and preventing neurological disorders.
The Importance of Sleep for Brain Function
During sleep, the brain undergoes vital processes that are essential for cognitive functioning and overall health. Sleep is divided into several stages, including rapid eye movement (REM) and non-REM sleep, each serving different purposes:
Memory Consolidation: During sleep, the brain consolidates memories, transferring information from short-term to long-term memory. This process is vital for learning and retention. Studies have shown that individuals who get sufficient sleep after learning new information perform better on memory tests than those who are sleep-deprived.
Detoxification: The brain has its own cleansing system, known as the glymphatic system, which becomes more active during sleep. This system helps clear waste products, including beta-amyloid and tau proteins, which are associated with Alzheimer's disease. Lack of sleep can hinder this detoxification process, increasing the risk of neurodegenerative diseases.
Emotional Regulation: Sleep is essential for regulating emotions and managing stress. Insufficient sleep can lead to increased irritability, anxiety, and depression, all of which can negatively impact neurological health. The brain's ability to process emotions and react appropriately is significantly impaired when sleep-deprived.
The Consequences of Sleep Deprivation
Chronic sleep deprivation can have serious implications for neurological health. Studies indicate a strong link between insufficient sleep and the development of various neurological disorders, including:
Cognitive Decline: Long-term sleep deprivation is associated with cognitive decline, increasing the risk of dementia and other cognitive disorders in older adults. Impaired cognitive function can manifest as difficulties with attention, problem-solving, and decision-making.
Mood Disorders: Poor sleep quality is closely linked to mood disorders such as anxiety and depression. These conditions can further exacerbate sleep issues, creating a vicious cycle that negatively impacts neurological health.
Increased Risk of Neurological Disorders: Research has shown that individuals who experience chronic sleep disturbances are at a higher risk for conditions like Parkinson’s disease and Alzheimer’s disease. The cumulative effects of sleep loss can lead to neuroinflammation and oxidative stress, contributing to the development of these disorders.
Tips for Improving Sleep Quality
Given the critical role of sleep in neurological health, it is essential to prioritize sleep hygiene. Here are some tips to improve sleep quality:
Establish a Sleep Routine: Aim to go to bed and wake up at the same time every day, even on weekends. This helps regulate your body’s internal clock and improves the quality of your sleep.
Create a Sleep-Inducing Environment: Ensure your sleep environment is dark, quiet, and cool. Consider using blackout curtains, earplugs, or white noise machines to minimize disturbances.
Limit Screen Time Before Bed: The blue light emitted by screens can interfere with the production of melatonin, the hormone responsible for regulating sleep. Aim to turn off electronic devices at least an hour before bedtime.
Practice Relaxation Techniques: Incorporate relaxation techniques such as meditation, deep breathing exercises, or gentle yoga into your bedtime routine to help calm your mind and prepare your body for sleep.
Be Mindful of Food and Drink: Avoid heavy meals, caffeine, and alcohol close to bedtime, as these can disrupt sleep. Opt for lighter snacks if you’re hungry before bed.
Seeking Professional Help
If you struggle with persistent sleep issues, it may be beneficial to consult a healthcare professional. Dr. Suzan Noori’s Neurology Clinic in Dubai specializes in diagnosing and treating neurological disorders, including those related to sleep. Our team of experts can provide comprehensive evaluations, personalized treatment plans, and recommendations for improving sleep quality and overall neurological health.
Understanding the vital connection between sleep and neurological health can empower you to make informed decisions about your sleep habits. Prioritizing restful sleep is not just a luxury; it’s a necessity for maintaining optimal brain function and overall well-being. At Dr. Suzan Noori’s Neurology Clinic, we are dedicated to helping you achieve better sleep and improved neurological health.
0 notes
Text

Prime Neurology Clinic: Skilled, All-Inclusive Treatment
In Lucknow, Prime Neurology Clinic is a reputable and top choice for top-notch neurological care. Our specialty is offering thorough and empathetic care to people with a range of neurological disorders.
0 notes
Text
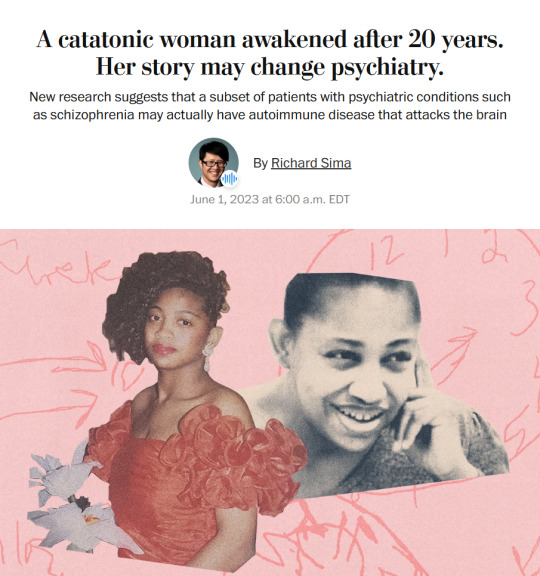
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes
Note
What is the difference between sociopath and psychopath?
OH! OH OH OH I LOVE THIS QUESTION. Also this is a massive explanation that really goes in-depth about neurology so I'll do a read more.
The main difference is that a psychopath is born with ASPD. A sociopath develops it during early (we're talking starting off as young as 2) childhood due to severe long-term (several years) abuse and neglect (generally from main caretakers).
There are also some nuances in how a socio's brain works in comparison to a psycho's. But the major difference that really determines all of the minor differences is that a psychopath doesn't necessarily have trauma related to their ASPD, and tends to have a lot less comorbid disorders. A sociopath ALWAYS has trauma that directly caused their ASPD and a fucking CVS receipt of comorbid disorders the large majority of the time.
There are also more sociopaths than there are psychopaths. The physiology of ASPD is that the brain's structure is different from an empathetic person. Specifically in the prefrontal cortex and the amygdala, because there's not enough activity in those areas for someone with ASPD. The prefrontal cortex is involved in decision-making, impulse control, and regulation of social behavior, and the amygdala is involved in emotion processing and fear response. Abnormalities in the amygdala contribute to a lack of empathy and increased aggression (aggression does NOT equal violence in this case, but rather an increased and pervasive level of negative emotion that makes you more likely to act out). Genetics have been proven to play a factor in how likely someone who was born empathetic would develop ASPD.
The difference here is that a psychopath is born with reduced blood flow to those areas. No trauma needed, that's just how they work.
On the contrary, a sociopath develops reduced blood flow to those areas because if you live in an environment that fosters the growth of anti-social traits and behaviors you are not exercising those parts of your brain. I'll go into a deep dive about the neurological aspects of how formative trauma turns into ASPD.
Chronic stress from abuse can impair the development of the prefrontal cortex; reduced activity or structural abnormalities in this area can lead to increased impulsivity and difficulty regulating emotions. The amygdala becomes hyperactive due to repeated exposure to threatening situations. This results in heightened aggression and reduced ability to empathize with others. Abuse can lead to a smaller hippocampus, impairing the ability to process emotions and increasing vulnerability to stress.
Chronic abuse elevates cortisol levels (the stress hormone), which can alter brain function and structure. Persistent high cortisol levels can damage the prefrontal cortex and hippocampus, exacerbating emotional and behavioral regulation issues. Serotonin and dopamine neurotransmitters regulate mood and behavior. Abuse can disrupt their levels, contributing to aggression, impulsivity, and difficulty experiencing pleasure or reward.
The autonomic nervous system (ANS) becomes hyperactive, leading to a state of constant alertness and readiness for perceived threats. This can cause chronic anxiety, irritability, and aggressive responses. Conversely, some individuals may develop a blunted stress response, showing reduced physiological reactions to stress. This can lead to a lack of fear or concern for consequences. (These two may combine so that safe things trigger stress and unsafe things do not).
Abusive environments can impair the development of secure attachments, leading to difficulties in forming trusting relationships. This can foster detachment, manipulative behavior, and a lack of empathy. Inconsistent or abusive parenting can disrupt normal emotional development, making it difficult for individuals to manage their emotions and impulses. This can result in volatile behavior and poor emotional control. Abusive environments often model and reinforce antisocial behaviors. Children learn to cope with stress through aggression or manipulation, which can become ingrained patterns of behavior. Abusive environments can impede moral development, leading to difficulties in understanding and adhering to societal norms and rules. This can result in a disregard for others' rights and a propensity for criminal behavior.
Trauma and abuse can also alter gene expression through epigenetic changes, affecting the brain's development and function. These changes can increase the risk of developing ASPD by influencing genes involved in stress response, emotional regulation, and social behavior.
A lot of people who went through severe childhood abuse may experience anti-social symptoms without having full-blown ASPD. When I was younger I did a genetic test that led to some very fascinating results that now that I'm older and understand my disorder I understand how my ASPD ties directly into my genetic depression, or rather my genetic depression is caused by my ASPD.
I don't process/produce Vitamin B6, B9 (Folate), and B12. These vitamins are crucial for brain function and the production of neurotransmitters. Deficiencies lead to mood disorders, cognitive impairments, and other neurological issues. B vitamins are involved in synthesizing neurotransmitters like serotonin, dopamine, and norepinephrine, which regulate mood and behavior. These are neurotransmitters that act as natural painkillers and mood enhancers. B vitamins play a role in the metabolic pathways that produce endorphins. An inability to properly absorb, process, or produce B vitamins can disrupt these pathways, leading to lower endorphin levels, which can contribute to symptoms of depression and affect overall mental well-being.
Because of how specific my issue is I had to take a specialized blend of B Vitamins. Unfortunately once I turned 18 my parents stopped buying them for me and I haven't had the funds to purchase my own at all since I was cut off (which has led to my mental health tanking). I strongly suggest anyone who deals with anti-social traits in a way that is disruptive to their daily life to look into these. You can't generally find them at a drug store, but they're on Amazon for 25-ish USD for a month's worth bottle. Which is really good because when my parents were buying them two years ago or so they were 40$ a bottle.
I have been on all sorts of mood stabilizing medications, psychosis medications, anti-depressants, anxiety medication, etc. None of them worked because we didn't know what exactly was wrong with me. All it did was make it so I couldn't feel the negative emotions properly, so I was constantly numb. What the vitamins did for me is that they let me process passive endorphin exchange and metabolism for the first time in my life, which meant that there wasn't a drastic barrier between me and positive emotions.
I strongly suggest this for anyone who is also just dealing with mood instabilities/disorders because it helped immensely. I'm bipolar two and I wasn't dealing with any major manic episodes while I was on them for about two years, so it helped drastically in that aspect too.
I know this got a little off the rails, but sociopathy is such a hard disorder to deal with, and it's so demonized by the media. Just telling someone you're a clinical sociopath is enough for them to kick you out of their life, even though it has no reflection on your character and is just an outcome of a horrible, hell-like childhood. So I think it's important for ASPD voices to speak up about the disorder when they can and try to dispel some of the awful stigmatization.

#alex answers#answered ask#thanks for the ask!#clinical sociopathy#clinical psychopathy#psychology#neurology#sociopathy/psychopathy#sociopath vs psychopath#actually aspd#aspd safe#aspd awareness#mental health#mental heath awareness#mental illness#mental disability#disability pride month#aspd flag#aspd pride#apsd voices#sociopath#psychopath#actually antisocial#antisocial personality disorder#personality disorder#cluster b safe#cluster b illness#cluster b disorder
106 notes
·
View notes
Note
Good luck for Duncan's appointment tomorrow! I hope everything goes as smoothly as possible. Our thoughts are with you and the little man.
Thank you!! I am so very excited and if I told him what’s happening tmrw he would be so very NOT excited! His appointment is at 10:00am and then we’ve got an hour and a half drive back home.
I will make sure to update you guys as soon as I can with how the consult went! I’m also going to make sure I specifically request his scans when he has them done tmrw, not just their finding/notes
#idk how the neurology department at Madison is but a lot of times when other clinics send us records they skip things like radiographs#and A) I want to see them B) Doc wants to see them#and C) I want to show you guys#my post#Duncan#ask
104 notes
·
View notes
Text
On land my body barely functions, I struggle to walk, struggle to balance, my limbs feel as though I were another experiment of Dr Frankenstein, they do not feel my own, instead crudely attached to me and barely functional. But in the water, suddenly that all changes, I am fluid and agile, my body moves, not perfectly as I am a bit too buoyant and I cannot hold my breath as long as I would like and my blowholes face the wrong direction, but so much better and I can move normally and naturally and comfortably. I love to swim, and be in the water, someday I will return to the water, forever~
#functional neurological disorder#conversion disorder#physically disabled#therian#therianthropy#nonhuman#whale therian#cetacean therian#clinical zoanthropy#clinical lycanthropy
10 notes
·
View notes
Text
hey, unfriendly reminder to always vaccinate your pets for rabies bare fucking minimum. i don’t care about what you say otherwise. go to a shelter or a low cost vaccine clinic. if you can’t afford vaccines, don’t have a pet. i am begging you, please just fucking vaccinate your pets BARE MINIMUM for rabies. i don’t care if your dog or cat is indoor only. things happen, and when they do, your pet gets decapitated and you cannot get the body back. you don’t get the ashes back. trust me, just get a rabies shot for your pet.
#lost.txt#tw for animal death#we had an infected animal at the clinic today#and like it was entirely preventable#just $35 for a rabies shot#the pet had been exposed to a bat a month prior#and they hadn’t vaccinated the pet because it was an indoor only animal#they didn’t even call after exposure#it was only when the animal was showing neurological and physical symptoms that they brought it in#and the humans have been exposed to both the bat and their pet#so it’s just terrible all around#literally this could have been prevented and it’s so fucking tragic
17 notes
·
View notes
Text
930pm will hit and well-adjusted neurotypicals will be like Yawn oh gosh I’ve been u p since six a m can y ou believ it
#healthy people are such an enigma to me#neurotypicals be like#sleep disorder#sleep deprivation#sleep deprived af#sleep deprived thoughts#trauma disorders#trauma symptoms#adhd autistic#neurodiversity#neurodivergent#did osdd#personality disorders#mood disorders#psychotic disorders#neurological disability#comorbid conditions#comorbidities#clinical depression#traumagenic#depression and anxiety#manic depressive#mental health representation#audhd problems#bpd thoughts#trauma recovery#complex trauma#cptsd recovery#audhd#forever sleepy
11 notes
·
View notes
Text
unfortunately, I have had another seizure - I did go to a&e this time and i’m no closer to getting any actual scans done or being seen by a neurologist, but I do have some diazepam for next time it happens 🙄
#got my gp clinic neurological examination tomorrow morn tho and will ask them to call the hospital and request my appointment be pushed#as suggested by the doctor I saw at a&e at THAT SAME HOSPITAL today who couldn’t do it because - for real - he didn’t know the number#we persevere#seizure saga
7 notes
·
View notes
Text
such a disarming experience to be right where you’re supposed to be
#checking in for a neurology appt and making small talk with the nurse#mentioned i had a lot of appointments today and then clarified i have a lot of regular appointments for my dbt therapy group#she was immediately interested and started asking me more about it. said she knew someone who could use it#so i told her a bit about how it works and how it’s helped me and she was just blown away#i gave her the clinic number so she could pass it along#she was so grateful she teared up a little bit and asked if she could hug me#i really hope her person starts group. i hope i get to see them#personal
2 notes
·
View notes
Text


1/18/2023
I have the day off from clinic but I have 5 hours of zoom lectures and workshops instead... It's ok though because this means I can wake up later than 5:30 am :')
Also I honored my neurology rotation! I feel like it's an external validation that I am actually making progress this year even though I feel pretty dumb on a daily basis. I've been trying hard on every rotation, but it really paid off this time!
#emgoesmed#studyblr#studyspo#med studyblr#med student#med school#ms3#clinical rotations#neurology#family medicine#latte#coffee#chocolate chip cookies#baking#cozy
29 notes
·
View notes
Text
huge thanks if you vote and/or rb, seriously it's greatly appreciated. Feel free to tag your conditions/disorders/meds, but do not feel obligated!
#did osdd#mental health#audhd#asd#adhd#actually autistic#borderline personality disorder#bpd#bipolar 1#bipolar 2#mental illness#mental health matters#cptsd recovery#cptsd#ptsd#chronic illness#neurological disorder#neurological disability#depression#clinical depression#anxiety#panic disorder#neurodiversity#helth care#perscription#medication#dissociative identity disorder#adhd autistic
10 notes
·
View notes
Text
1 note
·
View note
Text
Alzheimer's Disease: biomarkers and neuroimaging markers cheatsheet for research articles
As Alzheimer's Disease (AD) research skews toward understanding the brain than the pathogenic proteins, studies exploring biomarkers and neuroimaging are hopeful toward developing a method for successful prevention of AD. A biomarker is a molecule, whose presence indicates abnormality or disease, and thus, is crucial in diagnostic procedures. Levels of certain molecules is notably altered in cerebrospinal fluid and in blood plasma, which helps in diagnosing the occurrence of AD. Neuroimaging involves the use of techniques such as magnetic resonance imaging and computed tomography to observe neuronal activity in the brain. This is good news, especially for AD, as the asymptomatic stage of the disease can be identified early enough.
Although the exact function and involvement in clinical practice is not profuse, altered concentrations of these biomarkers in plasma or cerebrospinal fluid encourage further research:
Amyloid and tau serve as the unsurprising biomarkers of AD pathology.
Neurofilament-light chain (NF-L) and visinin-like protein-1 (VILIP-1) are the most promising biomarkers of neuronal injury.
Post-synaptic protein neurogranin (Ng) and pre-synaptic proteins synaptosome-associated protein-25 (SNAP-25) and synaptotagmin-1 (Syt-1) are considered major biomarkers of synaptic injury.
Brain and CSF levels of tumor necrosis factor alpha (TNF-α) and increased levels of interleukin group of proteins (ILs) indicate intensified microglial response to neuroinflammation.
TREM2 receptor and YKL-40 glycoprotein are also reliable indicators of inflammation and impaired clearance of amyloid beta.
Heart-type fatty acid-binding protein (hFABP) could be a marker for pathology in blood vessels supplying the brain. Some vascular markers also show potential as markers of vascular injury in AD: von Willebrand factor (vWF) and monokine induced by γ-interferon (MIG, also known as CXCL-9).
Concentrations of TAR-DNA binding protein (TDP-43) in the brain and plasma and serum indicate, even contribute to, inflammation, mitochondrial dysfunction, and neuronal/synaptic injury in AD.
Neuroimaging techniques reveal structural, functional, and diffusion-related activities of the neurons. To identify them, markers are tracked in images obtained. Each marker is determined with the activity and biochemistry of the group of/individual neurons being studied.
Structural MRI will show location and severity of atrophy which can be identified in grey scale images by applying programs that create analogous color grading.
Functional MRI relies on blood oxygenation level dependent (BOLD) signal which reflects changes in blood oxygenation levels in response to neural activity.
Diffusion weighted imaging (DWI) focuses on diffusion of water molecules. A tensor model is applied to images obtained from DWI. The diffusion tensor imaging (DTI) metrics thus obtained help in studying connectivity through structural integrity of white matter tracts.
Tractography involves 3-D reconstruction of white matter as observed in DWI, which provides a more detailed look into a patient’s neural networks.
In positron emission tomography (PET), markers are identified and labelled so their features or functions can be traced during this procedure to obtain a resulting PET scan. The imaging procedure is named according to its marker: amyloid-PET, tau-PET, FDG-PET, inflammation-PET, receptor-PET.
FDA approved drugs Galantamine, Rivastigmine, and Donepezil alleviate symptoms such as memory loss and confusion in mild to moderate AD, although their effects seem to be negligible. They also cause nausea and vomiting as side effects and are not suitable for every patient. Recently approved drugs, Aducanumab and Lecanemab focus on removing accumulated amyloid. Their effectiveness is still doubted on the basis of studies finding that targeting amyloid has little to do with curbing the actual progression of the disease.
bibliography -
Tarawneh R. Biomarkers: our path towards a cure for Alzheimer disease. Biomarker insights. 2020 Nov;15:1177271920976367.
Cavedo E, Lista S, Khachaturian Z, Aisen P, Amouyel P, Herholz K, Jack Jr CR, Sperling R, Cummings J, Blennow K, O’Bryant S. The road ahead to cure Alzheimer’s disease: development of biological markers and neuroimaging methods for prevention trials across all stages and target populations. The journal of prevention of Alzheimer's disease. 2014 Dec;1(3):181.
Medications for Alzheimer's Disease Stanford Healthcare. Accessed 21-04-2023.
#aging#alzheimers#dementia#neuroscience#clinical medicine#diagnostics#diagnosis#brain injuries#neurological conditions#neurodegenerative disorders#neurodegeneration#neurons#neurology#brain research#neurological disease#neurological disorders and injuries#chronic illness#neuroinflammation#neuroimaging#science#science side of tumblr#research paper#academic writing
7 notes
·
View notes
Text
Orthopedic physiotherapy in Gurgaon| EEZ ALIGN

Orthopedic physiotherapy, also known as ortho physiotherapy, focuses on the assessment and treatment of musculoskeletal conditions. Professionals in this field employ a variety of therapeutic techniques to address issues such as joint pain, fractures, and muscle injuries. Tailored exercise programs help improve flexibility, strength, and mobility, while manual therapies like massage and joint mobilization aid in pain management. Ortho physiotherapy in Gurgaon plays a crucial role in post-surgical rehabilitation, guiding patients toward optimal recovery. With a holistic approach, practitioners empower individuals to regain functionality and lead a pain-free life. If you're experiencing musculoskeletal challenges, consult with an orthopedic physiotherapist for personalized care and rehabilitation strategies.
To know more-
#best physiotherapy clinic near me#benefits of neurological physiotherapy#physiotherapy clinic#neuro physiotherapy centre#best chiropractor gurgaon#chiropractic care#neuro physiotherapy near me#physiotherapy clinic in gurgaon#physiotherapy centres in gurgaon#chiropractor clinic in gurgaon
2 notes
·
View notes
Text
I know that with things like FND (and also schizophrenia) that progress and management isnt always steady or linar but sometimes things are really frustrating. For around 14 months or so I was able to walk almost entirely without crutches or mobility aids. At one point I think I went three or four months without needing any. In the past two months my walking seems to have deteriorated so much. Sometimes it seems fine, and other times even my main crutches are really not sufficient on their own because the forearm cuffs are plastic and bend. It feels almost as though my legs and arms were not my own, but poorly made prosthetics crudely attached to me which bend and spring (like the robots from early mid 2000s animation).
There is a certain irony, or maybe it isnt ironic at all, that once I am in the water and it stabilizes me I can move fluidly and naturally, I am quick and agile. But coming out of the water it takes me a few moments to relearn how to use my legs and at times I need to be near carried out of the water to hold myself up. And in another irony is that while my legs to me often feel as though they were some sort of prosthetic, when I put on a well fitting fin, the fin feels as though it were part of my body, fat more real than my legs when I am out of the water.
I know with these things it is rarely straightforward progress, and the improvements I have made compared to five years past are little short of a miracle. But the struggles again to walk are really very frustrating. But then I dont know what can be done but to just keep carrying on. What would doctors do? Run more tests before giving up again? Put me on more antipsychotics? Theyve never been helpful before.
#actually schizophrenic#schizophrenia#clinical zoanthropy#fnd#functional neurological disorder#conversion disorder#disability#mobility issues#therian#therianthropy
6 notes
·
View notes