#Family history diabetes risk
Explore tagged Tumblr posts
Text
How Genetics Affects Type 2 Diabetes?
This article is originally published on Freedom from Diabetes website , available here. You want to know, is type-2 diabetes is genetic or not? The answer is yes. But it is depend upon some factors. It is something in your environment that actually triggers it. For proof, we can look at identical twins. They have identical genes. Yet if one twin gets type 2 diabetes, the other twin's risk is three in four at most. Lets understand genetic diabetes symptoms?
Frequent need to visit the washroom.
Increase in appetite
Fatigue
Lack of clarity in vision
Repeated infections
healing wounds
Now the question is type 2 diabetes genetic, can it be reversed or not. To know it please click here. If you found this blog useful, please recommend it and share it with others!
Also please connect with me on my website, Facebook page, and YouTube if you want to stay in touch or give me any feedback!
Thank you!
#Type 2 diabetes genetics#Genetic predisposition diabetes#Family history diabetes risk#Genetic variants diabetes#Heritability type 2 diabetes#Diabetes risk factors genetics#Genetic testing diabetes#Environmental factors diabetes
0 notes
Text
Diabetes in Young Adults: Causes and Solutions
Addressing the rise of diabetes in young adults requires comprehensive strategies that promote healthy lifestyle choices, including regular physical activity, balanced nutrition, stress management, and increased awareness of diabetes risk factors. Additionally, early detection through regular screenings and improved access to healthcare can help identify and manage diabetes at an earlier stage,…

View On WordPress
#blood sugar control#blood sugar monitoring#diabetes#diabetes advocacy#diabetes awareness#diabetes community#diabetes complications#diabetes counseling#diabetes diagnosis#diabetes education#diabetes in adolescents#diabetes lifestyle#diabetes management#diabetes medications#diabetes prevention#diabetes research#diabetes resources#diabetes risk factors#diabetes support#diabetes symptoms#diabetes technology#diabetes treatment#exercise for diabetes#family history of diabetes#gestational diabetes#glucose metabolism#glucose monitoring#healthy diet#healthy habits#healthy lifestyle
0 notes
Text
Type 2 Diabetes and Januvia: Managing Blood Sugar Levels Effectively
Welcome to the esteemed Well Health Hub, a premier repository of authoritative and exhaustive health-related knowledge. Within the confines of this discourse, we shall embark upon a profound exploration of the intricate intricacies inherent in Type 2 Diabetes, leaving no stone unturned in our quest to comprehend the manifold dimensions of this malady. Moreover, we shall endeavor to illuminate the…

View On WordPress
#Age#Blood Glucose Regulation#blood sugar levels#Blood Sugar Monitoring#Cardiovascular Health#Chronic Metabolic Disorder#Clinical Studies#Comprehensive Diabetes Management#diabetes awareness#Diabetes Management#Efficacy#Ethnicity#Family history#FAQs#gestational diabetes#Gestational Diabetes Risk#Health Information#healthcare#Healthcare provider#Holistic Approach#Incretin Hormones#Insulin Resistance#Januvia#Januvia Benefits#Januvia Dosage#Januvia Efficacy#Lifestyle Changes#medication#Medication adherence#obesity
0 notes
Text
[Spy x Family ch. 109 spoilers]
I just finished the chapter as of two minutes ago, and I have to tell you, I am having the best time getting to use whip out my psychology degree again.
Good people of tumblr, allow me to introduce to you:
Capgras delusion


It's interesting that Melinda disclosed that she was a patient of the hospital before. It is no small feat to be admitted into psychiatric care - especially in a hospitalised setting. Psychiatric hospitals typically deal with very high-risk disorders and behaviours, with many patients being admitted to hospital either for their own safety, or for the safety of those around them.
What has this got to do with capgras delusion?
Capgras delusion is a very serious psychiatric disorder in which a person believes that someone very close to them has been replaced with an impostor.
It is not uncommon for sufferers of capgras delusion to believe that their loved ones have been replaced by aliens, a doppelganger, or a clone.
It can be from many causes: psychosis, schizophrenia, brain damage, neurodegenerative disease. In very rare cases there have even been documented unexepcted triggers such as ketamine, diabetes, migraines, and urinary cystitis.
And, crucially; it is not unheard of for sufferers of capgras delusion to be physically agressive towards the perceived impostor.
(Is that why she was sent to psychiatry before? Is that why she is estranged from Donovan and the children? Is that why she is kept under very close watch? Or is there something more sinister going on?)
From this chapter alone, I wonder if we will see a link between Melinda's delusion, and her past experiences. If Endo chooses to take the scientific route, we may see a history of physical abuse that resulted in brain damage, or a history of psychological abuse that made Melinda vulnerable to psychosis.
I would be really interested to see if Melinda's current way of thinking may have originated from having an initially loving relationship with Donovan Desmond, but she saw a sudden change in behaviour in him to become the heartless warmonger we now know him to be, which could have pushed her into this delusional belief.
After all, how could the man she fell in love with (conjecture), have turned into such a monster? The only explanation must be that Donovan Desmond is not the Donovan she knew, and just an impostor, right?
....Right?
#melinda desmond#sxf manga spoilers#spy x family spoilers#spy x family#sxf#sxf manga#spy x family analysis#spy x family manga#spy x family manga spoilers#sxf spoilers#and if Endo goes the sci fi route with REAL aliens#i will have an absolute fit#with endos deep interest in psychology there is no way in hell he is going to rely on aliens#if his other choice was relying on humans#melinda is crazy confirmed
698 notes
·
View notes
Text
A brief guide to Testosterone HRT
If you’d like the one for Estrogen HRT, ask in the comments and you shall receive.
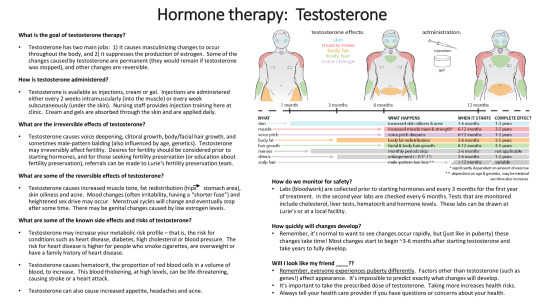
Image from the Transpeak Discord - unsure of actual source (a clinic?) (if anyone knows, please tell!)
Alternate text under the cut
Alt:
What is the goal of testosterone therapy?
Testosterone has two main jobs: It causes masculinizing changes to occur throughout the body, and it suppresses the production of estrogen. Some of the changes caused by testosterone are permanent (they would remain if testosterone was stopped), and other changes are reversible.
How is testosterone administered?
Testosterone is available as injections, cream, or gel. Injections are administered either every two weeks intramuscularly (into the muscle) or every week subcutaneously (under the skin). Nursing staff provides injection training here at clinic. Creams and gels are absorbed through the skin and applied daily.
What are the irreversible effects of testosterone?
Testosterone causes voice deepening, clitoral growth, body/facial hair growth, and sometimes male-pattern balding (also influenced by age and genetics). Testosterone may irreversibly affect fertility. Desires for fertility should be considered prior to starting hormones, and for those seeking fertility preservation (or education about fertility preservation), referrals can be made to Lurie’s fertility preservation team.
What are some of the reversible effects of testosterone?
Testosterone causes increased muscle tone, fat redistribution (hips to stomach area), skin oiliness and acne. Mood changes (often irritability, having a “shorter fuse”) and heightened sex drive may occur. Menstrual cycles will change and eventually stop after some time. There may be genital changes caused by low estrogen levels.
What are some of the known side effects and risks of testosterone?
Testosterone may increase your metabolic risk profile — that is, the risk for conditions such as heart disease, diabetes, high cholesterol or blood pressure. The risk for heart disease is higher for people who smoke cigarettes, are overweight or have a family history of heart disease.
Testosterone causes hematocrit, the proportion of red blood cells in a volume of blood, to increase. This blood thickening, at high levels, can be life-threatening, causing stroke or a heart attack.
Testosterone can also cause increased appetite, headaches, and acne.
A low-detail diagram of the upper half of three bodies is displayed. From left to right, the bodies represent having been on testosterone for little to no time (a month or less), a medium amount of time (six to eight months) and a greater amount of time (a year or more).
The diagram is a visual representation of testosterone effects on the body. Hip mass shifts to the stomach area, The adam’s apple grows. Muscle mass grows and shoulders become broader. Facial and body hair grows on the arms, face, and assumably the legs not displayed in the image. The skin gets oily and acne appears on the face.
Testosterone affects: skin, muscle mass, body fat, body hair, voice change.
Increased skin oiliness and acne starts within 1-6 months of testosterone. Its complete effect can be within 1-2 years.
Increased muscle mass and strength starts within 6-12 months of testosterone. Its complete effect can be within 2-5 years. This effect is highly dependent on the amount of exercise one does.
Voice pitch deepening starts within 6-12 months of testosterone. Its complete effect can be within 1-2 years.
Body fat redistribution starts within 3-6 months of testosterone. Its complete effect can be within 2-5 years.
Facial and body hair growth starts within 6-12 months of testosterone. Its complete effect can be within 3-5 years.
Monthly periods stop within 2-6 months of testosterone.
Clitoral enlargement of 0.5 inches to 1 inch begins within 3-6 months of testosterone. Its complete effect can be within 1-2 years.
Male pattern hair loss starts when you have been on testosterone for over a year. Its complete effect date is variable. It depends on age and genetics, and can be minimal.
Sex drive also increases.
How do we monitor for safety?
Labs (bloodwork) are collected prior to starting hormones and every three months for the first year of treatment. In the second year, labs are checked every six months. Tests that are monitored include cholesterol, liver tests, hematocrit, and hormone levels. These labs can be drawn at Lurie’s or a local facility.
How quickly will changes develop?
Remember, it’s normal to want to see changes occur rapidly, but (just like in puberty) these changes take time! Most changes start to begin around 3-6 months after starting testosterone and take years to fully develop.
Will I look like my friend _____?
Remember, everyone experiences puberty differently. Factors other than testosterone (such as genes!) affect appearance. It’s impossible to predict exactly what changes will develop.
It’s important to take the prescribed dose of testosterone. Taking more increases health risks.
Always tell your health care provider if you have questions or concerns about your health.
#mod cole#trans#transmasc#transgender#trans man#ftm#transmasculine#trans guy#testosterone gel#testosterone#testosterone hrt#ftm hrt#trans hrt#hrt#hormone replacement therapy#testosterone replacement therapy#trans boy#transsexual#trans ftm#trans men#trans male#trans pride#transblr#transsexuality#trans masc#ftm trans#trans resources#trans resource#resources#has this already been posted on this blog? we’re about to find out
301 notes
·
View notes
Text
if you try to police disabled peoples' diets INCLUDING how they spend their money on food: i just want to ask why? what do you gain from this? like seriously, what do you actually gain from displaying holier-than-thou behavior toward another person's spending and dietary habits? who cares if you would spend your money "better"? you're not them. this is a form of abuse. you literally have no idea what the disabled person can safely digest and actually gains nutrients and energy from. you have no clue, even if you share the same disorder, you are not that person, nor are you their gastroenterologist or other specialist.
telling disabled people to "eat healthier," "eat more salads," "eat more fresh fruits," "eat more fresh vegetables," "eat more grains," and so on can not only be outwardly dangerous for people who have digestive issues like inflammatory bowel diseases, gastroparesis, irritable bowel disease, acid reflux, a history of ulcers, gastritis, and a long list of other digestive health issues, it can outright kill someone if they form a blockage. this can also injure, sicken or kill diabetics, people with non-diabetic low or high blood sugar, blood pressure issues, kidney and liver issues, and many other people.
not only that but you're potentially forcing a neurodivergent person to eat foods that nauseate, sicken, or disgust them, and for what? autistic people know what foods are safe for them to eat. adhd people need to find finds they can manage to keep in their homes without spoiling. dissociative people, people with ADHD, head trauma, develeopmental disorders, other people with memory issues, dementia, alzheimers, psychotic people, and other mental and cognitive health issues need foods they can prepare safely, because many mentally ill and neurodivergent people can't safe;y cook without risk of injury or damage to their home.
people who deal with allergies and intolerances are constantly struggling with being told how to eat when they are the ones who know their experience the most. NOBODY gives a fuck about people with allergies and literally nobody takes food intolerances seriously. i can't digest animal products OR byproducts anymore. i lost the ability. but sometimes i question "maybe i can try it again because this food is cheaper." well. i decided i was spending too much on groceries due to inflation and bought cow's milk instead of almond milk and got so sick it was something i had never seen before. i do NOT need to prioritize "saving money" over eating foods i can safely digest. i had an IBS attack early this morning because i ate some cheese- because it is a "cheap, easy source of protein."
some disabled people need to use certain services like pre-prepared foods being delivered to their homes, be it meals on wheels, or hello fresh. guilting these people for using the services because they could "just cook at home" is insulting to say the least. many of these services have tailored meals with consistent ingredients with limitations on contaminants with allergens.
here's the big one that everyone fucking hates but needs to accept immediately: some disabled people are too exhausted, in pain, dissociated, psychotic, unable to focus, unable to follow instructions, or in other ways unable to cook for themselves and need to use food delivery services like doordash and uber eats.
some disabled people can't or don't want to drive due to their disabilities! blind disabled people exist! para- and quadriplegics exist! people with hand tremors exist! working disabled people exist! amputees exist! disabled parents exist! disabled people who care for partners and family exist!
this one is sooooooo taboo and i'm sick of it. first of all, dashers and uber drivers are every day people who need to earn income. these are people's jobs and their lives are in fact on the line because this is a lot of drivers' primary income. enough with guilting people on this one. i'm fucking sick of it. y'all hate independently employed people and it shows. this isn't a luxury just relegated to rich white moms: disabled people need to have prepared, easy to eat foods delivered to our homes too. y'all need to leave people the fuck alone when it comes to takeout.
the second someone poorer and more disabled than you does something you do regularly, suddenly you're sending articles and giving paragraphs and paragraphs of advice on how to spend money better and how the disabled person "just needs to eat rice, beans, ramen, and frozen vegetables" because disabled people are not allowed comfort NOR convenience in your eyes. this is absolutely asinine. stop it. EATING is not relegated to the privileged
disabled people are people and need to eat. why you are prioritizing money over a literal human need is beyond me this is sick behavior. why do you care so much more about the money than the person ?why is money more important than someone's safety to you? why would anyone rather see someone "spend money the right way" over a human being EATING FOOD and especially foods they KNOW won't make them sick. policing how any disabled person spends their money on food is also unnecessary and abusive. it serves nothing to gain and everything to lose. so what if you think a disabled person spends too much money on food? you do too- we all do: food should be fucking free. get over yourself and let disabled people eat. leave your greed at the door, stop feeling entitled over other peoples' finances and spending habits.
telling a disabled person how to "eat healthier" will not make you healthier, and it will not do them any good, either. all it does is serve to stroke your ego because you believed you ""helped"" someone but all you did was give unsolicited advice that will be forever moot because you do not live in that person's body. don't care if you know them personally: you ain't them. so back off, let disabled people eat. food ain't just for the rich. food ain't just for the abled. let people access food in ways that are safe for us or get the fuck out of our way because all you're doing is causing problems and making disabled people's health problems WORSE.
#cripple punk#fibromyalgia#disability culture#crip punk#chronically chill#cripplepunk#disabled culture#chronic pain#cpunk#actually disabled#disabled rights#ibs#ibd#crohns disease#crohns#irritable bowel syndrome#inflammatory bowel disease#autism#adhd#mental illness#neurodivergence#neurodiverse#psychosis#schizophrenia#our writing
352 notes
·
View notes
Text
Writing Notes: Color Blindness

Color blindness, also called color vision deficiency (CVD), is a group of conditions that affect the perception of color, characterized by the inability to clearly distinguish different colors of the spectrum.
The difficulties range from mild to severe.
Color blindness is a misleading term because people with color blindness are not blind. Rather, they tend to see colors in a limited range of hues; a rare few may not see colors at all.
There is no treatment or cure, and cannot be prevented.
Most color vision deficient persons compensate well for their abnormality and usually rely on color cues and details that are not consciously evident to persons with typical color vision.
Risk Factors
A family history of color blindness increases the risk since most color vision problems are inherited.
Another risk factor for color vision deficiency is aging:
The eye’s lens can darken and yellow over time, which can impair the ability of older adults to see dark colors.
Certain medications can also increase risk:
For example, the drug hydroxychloroquine (Plaquenil), used to treat rheumatoid arthritis, can cause color blindness.
Causes
Mutations in the CNGA3, CNGB3, GNAT2, OPN1LW, OPN1MW, and OPN1SW genes are known to cause color vision deficiency.
Color blindness is sometimes acquired.
Chronic illnesses that can lead to color blindness include Alzheimer disease, diabetes mellitus, glaucoma, leukemia, liver disease, chronic alcoholism etc.
Some medications such as antibiotics, barbiturates, anti– tuberculosis drugs, high blood pressure medications, and several medications used to treat nervous disorders and psychological problems may cause color blindness.
Industrial or environmental chemicals such as carbon monoxide, carbon disulfide, fertilizers, styrene, and some containing lead can cause loss of color vision.
Occasionally, changes can occur in the affected person’s capacity to see colors after age 60.
Symptoms
The inability to correctly identify colors is the only sign of color blindness.
It is important to note that people with red/green or blue varieties of color blindness use other cues such as color saturation and object shape or location to distinguish colors. They can often distinguish red or green if they can visually compare the colors. However, most have difficulty accurately identifying colors without any other references.
Most people with any impairment in color vision learn colors, as do other young children. These individuals often reach adolescence before their visual deficiency is identified.
Source ⚜ More: Writing Notes & References
#writing notes#color blindness#writeblr#dark academia#spilled ink#literature#writers on tumblr#writing reference#poets on tumblr#writing prompt#poetry#creative writing#writing inspiration#writing ideas#light academia#winslow homer#writing resources
84 notes
·
View notes
Text
Also preserved in our archive
By Amy Norton
The virus can trick your body into attacking itself.
Brittany Underwood was 37 when she was hit with COVID early in 2021. Her case was mild, and, like the mom she is, she took care of everyone else because of course the rest of her family had it too. It wasn’t until a couple weeks later that she started to feel lousy—wiped out, constantly thirsty, and dealing with weird issues like blurry vision in one eye.
When Underwood brought those symptoms to her doctor, he decided to run some blood tests. “My blood sugar was through the roof,” Underwood tells SELF. It was so high, in fact, she ended up in the hospital that same day, where they handed her a diagnosis that would change her life: type 1 diabetes.
This autoimmune disease is most often diagnosed by the age of 14—it used to be known as juvenile diabetes because it’s the type that most often hits kids, teens, and young adults. Because Underwood was approaching 40, her case was unusual. But her doctors raised a possible explanation: She’d just had COVID, and they suspected the infection might have triggered her diabetes.
Nearly four years later, we have a lot more than suspicions. In fact, the pandemic has been blamed for a spike in type 1 diabetes. New cases in kids and teens jumped up 16% in the first 12 months of the pandemic and 28% in the following year. (Before 2020, the typical increase was 2% to 3% per year.) And it’s not just type 1. Other autoimmune diseases—including rheumatoid arthritis (RA), psoriasis, and lupus—went up too. Exactly why that happens isn’t fully clear, Sonia Sharma, PhD, an associate professor at La Jolla Institute for Immunology, in La Jolla, California, tells SELF. “But,” she adds, “we do have some clues.”
When your immune system turns on you The idea that COVID could set off a chronic autoimmune disease might seem out there. But, Dr. Sharma says, “it’s not a new concept at all.” Autoimmune diseases are caused by a misguided immune system attack on the body’s own healthy tissue. For that to happen, a perfect storm of conditions has to come together. Genes definitely matter, Dr. Sharma says, since autoimmune diseases tend to run in families, and studies have tied certain genes to higher risks of the conditions. (Underwood says she has a family history of autoimmune diseases.) Your sex assigned at birth matters too: Autoimmune diseases are way more common in women than men, Dr. Sharma notes (though anyone can get them).
But those kinds of risk factors aren’t enough on their own. People have to be exposed to one or more “triggers” that tip the immune system into self-attack mode. And microbes are among those potential sparks, Akiko Iwasaki, PhD, professor of immunobiology at Yale School of Medicine, tells SELF.
Studies have linked a slew of infections—including super-common ones like the flu, cytomegalovirus, and Epstein-Barr virus—to various autoimmune diseases. Epstein-Barr, which eventually infects nearly everyone and is usually no big deal, may be the prime example: A recent study found that the infection likely plays a role in most cases of multiple sclerosis (an autoimmune disease that destroys the protective covering around nerve fibers).
There are different theories on exactly how it happens, but Dr. Iwasaki offers a (relatively) basic overview. First, she says, it’s a little known fact that everybody has some number of immune system cells that are “autoreactive,” meaning they’re capable of going rogue against you. Thankfully, they usually don’t. But in certain people, under certain circumstances, an infection might “activate” those autoreactive immune cells.
“Once they’re activated,” Dr. Iwasaki explains, “they can divide and travel to different tissues in the body, and may start to attack your own cells.” All of that, she adds, is more likely to happen when an infection generates lots of inflammation in the body. An ordinary cold probably won’t do that, but COVID might.
How big is the risk? Even though it can seem like we’ve been living with COVID forever, it’s still a very new thing. Because of that, Dr. Sharma says, it’s only recently that studies have been able to turn up strong evidence that the infection does trigger autoimmune diseases.
That includes this 2023 study of close to 4 million Americans. It found that people diagnosed with COVID had higher odds of developing autoimmune diseases over the next six months, versus COVID-free people. On average, they were roughly three times more likely to be diagnosed with conditions like RA, lupus, psoriasis, celiac disease, and type 1 diabetes.
Really important to point out here: Although three times more likely might sound huge, the risk of any one person developing an autoimmune disease after COVID is still low, Sara Martin, MD, medical director of Vanderbilt University Medical Center’s Adult Post-Acute COVID Clinic, in Nashville, tells SELF.
Another 2023 study, published in Clinical Rheumatology, helps put things into context. It found that of 565,000 people with COVID and no history of autoimmune disease, 1% were diagnosed with an autoimmune condition over the next 3 to 15 months. That was 43% higher than the rate among people who didn’t have COVID during the same period. Although that sounds like a lot, it was an increase from roughly 11 to 15 cases per 1,000 people per year. So…not a huge amount, but not something to dismiss either. And if you’re one of the unlucky people who does develop an autoimmune condition, that’s a heavy toll.
“All of a sudden I had this huge life-altering thing,” Underwood says of her diabetes diagnosis. People with type 1 have to take insulin injections every day to stay alive. So Underwood was forced to quickly learn the intricacies of carb counting, adjusting insulin doses, timing meals to avoid dangerous blood sugar drops—and managing them when they did happen. Time and experience, as well as connecting with other people with type 1 diabetes, have taught Underwood a lot. “But I’m still learning, three years later,” she says. “It’s just a constant thing. You can’t take a day off.”
Is there a way to protect yourself? At this point, many of us have had COVID more times than we’d prefer. So does your immune system get used to the virus, and maybe make an autoimmune reaction less likely?
Unfortunately, Dr. Iwasaki says, there’s reason to believe the answer is no. That’s based on what researchers have learned about long COVID, a collection of symptoms like extreme fatigue and brain fog that hits many people post-infection. Prior bouts of COVID do not seem to lower the odds of developing long COVID (and the risk might even go up each time you’re infected). Long COVID, Dr. Iwasaki notes, is different from autoimmune diseases like type 1 diabetes and RA because the cause isn’t clear and may be due in part to direct damage caused by the virus. But she and other researchers have found that autoimmune reactions to COVID infection may also be behind long COVID symptoms, at least in some people. “I think that’s one clue that reinfection would not lower the risk of autoimmune disease,” Dr. Iwasaki says.
Okay, now for the good news: COVID vaccination might be protective. For one, Dr. Martin says, research shows that vaccination can lower the risk of long COVID, and the more vaccine doses you get, the greater the protection.
There’s also this large study published last year by researchers in China, which found that although COVID was associated with an increase in many autoimmune conditions, those risks were lower among people who’d gotten at least two COVID vaccine doses, versus unvaccinated people.
It’s “absolutely” plausible that vaccination helps, Dr. Sharma says. Vaccination, she explains, primes your immune system to stop the COVID virus “at the front door”—your respiratory tract—so that it can’t hitch a ride around the body, churning up inflammation and, potentially, an autoimmune reaction. And while people can develop autoimmune disease after a mild case of COVID (as Underwood did), research suggests that the odds might be substantially greater if you become severely ill.
“We already recommend vaccination for everyone,” Dr. Martin points out. “It reduces the potential for severe COVID, and we know it also reduces the risk of long COVID.” If you’re worried about autoimmune disease (say, because you have a family history of them), Dr. Martin says that’s one more reason to stay up-to-date on your COVID shots.
#mask up#covid#pandemic#public health#wear a mask#covid 19#wear a respirator#still coviding#sars cov 2#coronavirus#Long covid#diabetes#covidー19#covid conscious#covid is airborne#covid pandemic#covid isn't over#covid19#covid news
51 notes
·
View notes
Text
I'm Losing You... (But We're Filling the Cracks)
Having a family isn't always as easy as fairy tales make it seem. But sometimes, you just need a little bit of love... and a little bit of science.
Warnings: read chapter 1 for warnings.
Taglist: @phsycochan | @mirillua | @augustanna | @chaixsherlock | @whore-of-many-hot-men | @nerdisthenewcool | @lilypadmomentum

Chapter 25
[Prev] [Next]
The shock did not go away. If anything, it packed its bags and moved into your home.
You stood in front of the mirror in your bathroom dressed in only your bra and underwear. Law stood behind you, leaning against the door frame with his arms crossed over his chest. The air in the room was stifling as you gazed at the bump that had already started showing in your belly.
You had an approximate due date. May 22nd.
You were officially, according to your implantation date and calculations done by Robin, on your ninth week of pregnancy. Your hCG levels in each blood test had increased as expected, and your babies had heartbeats.
Your babies. Plural.
Your symptoms were exacerbated by the fact that you had not one, but two embryos inside you. Breast tenderness, backaches, nausea, dizziness, the whole nine yards.
Though, if you were being fair to yourself, your dizziness could easily have been a side effect of being labeled as ‘extremely high risk.’ Due to your history, and now due to being pregnant with multiples, you were given strict instructions to be much more present at your doctor’s office. You were given prenatal vitamins to begin taking daily every single morning. You were given foods to avoid in order to lower your risk of developing gestational diabetes. You were also given foods more encouraged to eat. Raise your blood iron. Raise your sodium, but not too much. Eat an increase of around 1000 calories a day to support the growth of two placentas and two babies. Watch out for spotting, bleeding, pelvic pain, irregular bowel movements. Watch out for headaches and weight gain or discolored urine, you might die. Keep an eye on your mental health, what stresses you, stresses the babies. But mostly, be excited!
Yeah, right.
Your hand traced the small bump in your belly.
“You know…” you began, making Law perk his head up to listen to you. “I always thought that seeing a baby bump would be the most exciting moment of my life… but I’ve never been more scared. Ever.”
Law approached you from behind, wrapping his hands around your bare waist and resting his chin on the crown of your head. His scent enveloped you like a blanket, instantly warming your skin and calming your heightened nerves. One of his hands traveled down the skin of your abdomen, resting on top of where yours lay above your uterus.
“I can’t lie to you… I am, too,” he added, his voice heavy with thought.
“Am I a bad person for not being excited?” you asked, your voice surprisingly stable despite the racing heart in your chest. “I mean, I am excited. So far their hearts are still beating… but…”
“You’re not a bad person at all,” replied your husband, planting a kiss to the back of your head. “It’s perfectly rational that you feel scared.”
“Terrified…” you clarified for the both of you. “I feel terrified.”
You and Law made eye contact in the mirror. The way he had his arms wrapped around you reminded you of a security blanket given to trauma victims in an ambulance. The thought made a wry smile break out onto your lips, making your husband cock an eyebrow.
“What’s got you smiling all of a sudden?” he asked with a slight upward turn to the corner of his mouth.
You mustered out a dry chuckle. “You’re my trauma victim security blanket.”
The randomness of your sentence made Law’s shoulders bounce slightly as he laughed, holding you closer to him. “I know it’s really hard for you to do so, but I think we should both try as hard as we can to think positively. It’ll probably be healthier for you.”
You looked up at him, a smirk dancing over your face. “That sounds crazy coming from you.”
You yelped in surprise as Law scooped you into his arms and carried you to your shared bedroom before plopping you down on your mattress, him sprawling out beside you. “What was that for?”
“So you wouldn’t stress yourself out in the mirror,” he replied, his voice hoarse yet tender as he stared at you from his pillow. “I’m being serious, though. I know the stakes are high, but there’s gotta be things we can think about to prevent you from getting stressed.”
You turned your body to lay on your back, lacing your hand with his as you stared at your ceiling. “Any examples?”
Law hummed in thought, glancing around the room. His eyes landed on your framed, signed Sora poster. The frame had a very small crack in it from being moved out of your sophomore year dorm room, but the poster inside was still in perfect condition. “Think about our kids watching Sora. Maybe we can dress them up as Sora and Stealth Black for Halloween.”
The tender thought almost immediately made you smile. Your mind flooded with even more thoughts of Law as a dad, tailoring Halloween costumes for his kids and making them feel perfect. Your thoughts of Law with one baby had now evolved into thoughts of him with two, rocking two armfuls of swaddled infants to sleep, kissing their little foreheads, pushing them in a double stroller. Your eyes began to well with tears which you quickly blinked away, choosing instead to push yourself up and roll over, hooking one of your legs in between Law’s and laying across his chest. His arms instinctively wrapped around your waist, tracing invisible patterns into the skin of your back.
“I get really happy thinking about you as a dad,” you sighed. “You’re gonna be so amazing.”
Law chuckled, his chest rumbling. “That’s the kind of positivity I’m talking about.”
You giggled. “I mean it, though. Remember before we got married and you said you were so scared to have kids one day? Because you didn’t want them to go through what we had?”
His face fell slightly, recalling the memory. He was still in the middle of his residency program, and you were jumping job to job with random, unstable freelance gigs. It wasn’t the instability of your lives that made him weary, however. Rather, it was the looming anxiety that everything good in Law’s life would someday be snatched away from him. And that had happened to you, twice.
But when he stepped back and thought about the broader picture, it got easier for him to see clearly. How you put up with his shitty attitude when you first met. How quickly you opened yourself up to him, exposing your deepest fears and troubles and being patient with him when he struggled to reveal his own worries to you. How you told him you loved him after only five months, terrified that you were going to scare him off, and all he could do in response was give you the most awkward, inexperienced kiss you had probably ever received. And you stayed by his side even when it took him almost a full year to say those three little words back.
You brushed your fingers along Law’s cheek, tracing the soft hair of his sideburns before hooking around his head and burying into the fluffy black wisps behind his ear. You pressed a smattering of kisses across his jaw and cheekbones, over his nose and finally on his lips. “When I think about positive things, I think of you.”
Law’s lips broke into a wide smile, the kind of smile he only ever showed you. The kind of smile that wrinkled the skin around his eyes and revealed the single small dimple he had on his right cheek.
A sudden ringing from his phone on the bedside table startled the two of you out of your lovestruck daze. With a grumble, he reached over and grabbed the device, you rolling off of him and sitting criss-cross on your side of the bed. He tapped the answer button and pressed the phone to his ear. You could just barely make out the words spoken on the other end. After a brief goodbye, Law hung up the call and uttered a heavy sigh before standing up and grabbing his uniform coat.
“Emergency surgery?” you asked. You were only slightly disappointed with the interruption of your intimate moment, but it was nothing you weren’t already used to.
He nodded with a frown before walking back over to you and stealing a quick kiss from your lips. “Patient just came into the ED with a STEMI. I’ll be back as soon as I can.”
“Don’t worry about me, go save the world,” you said with a smile. He tossed you a somber grin as he stepped into his shoes, grabbed his work bag, and booked it out the door. Living two minutes away from the hospital by car definitely had its perks.
You were surrounded by silence in your apartment when the front door was closed behind your husband. With a sigh, you stood from the bed and paced toward Law’s wardrobe, opening the bottom drawer and pulling out one of his old sweatshirts. It had a custom design on the front of it, one that he also had tattooed on his back. His living situation after he lost his biological family wasn’t ideal, but the little ways he held onto the memory of his adoptive father always brought a smile to your face. You pulled the hoodie over you, taking off your bra underneath it and throwing it onto the end of your mattress, tiredly rubbing your sore breasts underneath the soft cotton of his shirt. You turned around to face the rest of your bedroom.
The pregnancy journal that you barely started writing in was placed on top of Law’s desk. With a deep breath, you grabbed the book, a pen, and a roll of white-out tape and proceeded to your couch in the living room.
You smiled at the sight of Bepo, stomach completely upward facing and paws outstretched as he snoozed away on his dog bed. You had a feeling Bepo was going to be an absolutely incredible big brother.
You leaned against a pillow rested along the arm of the couch and propped up your knees to place the book on your thighs. You finally mustered up your anxieties and opened the cover.
“Nothing but positivity,” you muttered to yourself. You uncapped the pen and started writing.


#x reader#reader insert#fem reader#law x reader#trafalgar law x reader#one piece x reader#op x reader#trafalgar d water law x reader#trafalgar d water law#trafalgar law#i'm losing you
83 notes
·
View notes
Text
The Supreme Court on Monday turned down an appeal from California prison officials who sought immunity from lawsuits for having transferred inmates with COVID-19 to San Quentin in May 2020, setting off an outbreak that killed 26 prisoners and one guard.
The justices denied the appeals with no comment or dissent.
The transfer decision was later lambasted by state lawmakers as a "fiasco," "abhorrent" and "the worst prison health screw-up in state history."
The California Institution for Men in Chino had been hit hard by COVID-19. Nine of its inmates had died and about 600 were infected in May 2020.
San Quentin then had no known cases at that time. In an effort to prevent further harm at CIM, prison officials decided to move 122 inmates from Chino north to San Quentin.
Within days, San Quentin reported 25 COVID cases among the 122 new arrivals. Within three weeks, the virus spread to 499 others.
By early September, at least 2,100 inmates and 270 staff had tested positive.
The state now faces four major lawsuits from the families of those who died as well as from inmates and staff who were infected but survived.
Those lawsuits can proceed now that the federal courts in California and the Supreme Court have denied the state's claim that prison officials had "qualified immunity" that shielded them from being sued.
"The state has had its due process all the way to the Supreme Court. They're not getting off on a technicality," Michael J. Haddad, the attorney for the families, said in response to the court's order. "Now it's time to face the facts. Prison administrators killed 29 people in what the 9th Circuit called a ‘textbook case’ of deliberate indifference.”
The defense of qualified immunity often shields police officers from lawsuits. The justices have said that police and other government officials may be sued for violating the constitutional rights of individuals, but only if they knowingly violated a "clearly established" right.
Courts have said that police officers frequently must make split-second decisions on whether, for example, a suspect being pursued has a gun. For that reason, the courts sometimes shield officers from being sued for an "unreasonable seizure" if an officer shoots a fleeing person based on the mistaken belief that the suspect was armed.
The pending prison cases are quite different, lawyers for the families said, because prison officials decided to make the transfers without taking the precautions that were understood as needed at the time.
Sgt. Gilbert Polanco, the guard who died, was 55 years old and had worked at San Quentin for more than two decades. He had multiple health conditions, including obesity, diabetes and hypertension, which put him at high risk if he were to contract COVID-19.
His duties during the pandemic included driving sick inmates to local hospitals, but lawyers said prison officials refused to provide him or the inmates with personal protective equipment.
In late June 2020, he contracted COVID-19, and after a lengthy hospital stay, he died in August.
In Polanco's case, the lawsuit alleges he lost his life because of a "state-created danger."
The U.S. 9th Circuit Court of Appeals said prison officials had affirmatively exposed Polanco to a danger he would not have faced otherwise and failed to take steps to protect him from the danger they had created.
The Supreme Court in the past had also ruled that prisoners have a right to be protected against "the unnecessary and wanton infliction of pain," including as a result of "deliberate indifference to their serious medical needs." Lawyers for the San Quentin inmates said prison officials can be held liable under that standard.
California state attorneys urged the Supreme Court to review and reverse the 9th Circuit decisions that rejected a qualified immunity defense for the prison officials.
"The facts of these cases are undeniably tragic," they said. But in "the early months of the COVID-19 pandemic, when little was known about the disease and testing supplies were limited, the defendant officials attempted to protect the lives of scores of vulnerable inmates who were confined in a prison where the virus was rampant."
With the benefit of hindsight, they agreed their actions may be judged as mistaken, but "no clearly established law placed them on notice that their alleged mismanagement of the COVID-19 pandemic at San Quentin prison was unconstitutional."
16 notes
·
View notes
Note
Hi! Somewhat random question brought up by a different post. Is it true that gastric bypass surgery can prevent/stop diabetes? I understand that it’s not great for a person’s body in general, but my mom (a healthcare worker but not a dr/nurse) believes that the reason my dad doesn’t have diabetes despite being a large person is because of his gastric bypass. It might also be important to note that there’s no family history of it in his family aside from a half brother.
Again, I know it’s kind of random, but I thought you had some very good info on your post about fat phobia and the science behind fatness and wondered if this was something you knew about as well.
Good question! I did a (very) little bit of digging and came up with this article--although gastric bypass can lead to remission from diabetes and decrease hyperglycemia, there's a recurrence of risk down the road, and that recurrence is not necessarily linked to weight. That suggests to me that people who are susceptible to abnormal blood sugar processing remain at risk, though the risk may be decreased by gastric bypass surgery. It's similar to how people who develop gestational diabetes (abnormal blood sugar processing during pregnancy) are at higher risk for diabetes in the future, even if their gestational diabetes resolves after the pregnancy.
24 notes
·
View notes
Text
Tomiko Itooka: The World’s Oldest Person at 116 Age

Tomiko Itooka, a 116-year-old Japanese woman has been officially recognized as the world's oldest living person following the passing of 117-year-old Maria Branyas Morera. https://twitter.com/PopCrave/status/1825979850886086722

Also Read: Research Links Red Meat Consumption with Increased Risk of Type 2 Diabetes Tomiko Itooka was born on May 23, 1908 in Osaka, Japan. This was the same year that the Eiffel Tower transmitted its first radio message and when the Wright Brothers made their public flights in Europe and America. Raised in Osaka, Itooka grew up alongside her siblings and attended both elementary and high school in the city. At the age of 20, she married and eventually had four children. Tomiko Itooka worked as a manager in her husband’s textile factory, which was located in South Korea during World War II. This role would have required responsibility during such a period. Tomiko Itooka’s husband passed away in 1979. During World War II, Tomiko managed the office of her husband’s textile factory. This responsibility showcased her ability to go through one of the challenging periods in modern history. The war had effects on her and her family, but her resilience helped them to recover in the post-war era. Tomiko’s love for physical activities, particularly mountain climbing is one of the extraordinary aspects of her life. She scaled Japan’s 3,067-meter Mount Ontake twice. She climbed the mountain in sneakers instead of hiking boots. Even into her 70s, Tomiko continued her passion for climbing. Her dedication to staying active extended beyond mountain climbing, she completed the Saigoku Kannon Pilgrimage twice in her 80s. This involves visiting 33 Buddhist temples across the Kansai region. At 100 years old, Tomiko Itooka continued to defy expectations by walking up the lengthy stone steps of Ashiya Shrine without the aid of a cane. This ability to remain physically active at such an advanced age is considered one of the factors contributing to her longevity. Tomiko Itooka’s extraordinary life gained international recognition when she was named the world’s oldest living person at the age of 116. This title came following the death of Spain’s Maria Branyas Morera, who passed away at the age of 117. The Gerontology Research Group known for validating the ages of supercentenarians confirmed her birthdate and age, placing her at the top of their World Supercentenarian Rankings List. https://twitter.com/ThePopFlop/status/1825869923064619506 Also Read: The Hidden Dangers of Stealthy Saturated Fats and Sugars Since 2019 Tomiko Itooka has resided in a nursing home in Ashiya, Hyogo Prefecture. Despite her advanced age she remains mentally sharp and communicates clearly, though she has become hard of hearing. Every morning, Tomiko Itooka starts her day with a popular yogurt-flavored drink called Calpis. Her favorite food is bananas, which she enjoys regularly. This simple diet combined with her active lifestyle may have contributed to her longevity. Tomiko Itooka celebrated her 116th birthday three months before being recognized as the world’s oldest person. The celebration included receiving flowers, a cake and a card from the city’s mayor. At the age of 100, Itooka demonstrated her enduring physical strength and independence by walking up the lengthy stone steps of the Ashiya Shrine without the aid of a walking stick. This feat underscores her physical vitality and determination to remain active well into her centenarian years. Itooka reached the milestone age of 110 in May 2018 she earned the title of supercentenarian. The Gerontology Research Group, a non-profit organization dedicated to researching human longevity. Following the death of Maria Branyas Morera at the age of 117, Tomiko Itooka has been officially declared the world’s oldest living person by Guinness World Records. While Tomiko Itooka is the current oldest living person, she joins a list of supercentenarians who have been recognized by Guinness World Records. The previous titleholder, Maria Branyas Morera lived through the 1918 flu pandemic, two world wars and the Spanish Civil War. The oldest verified person in history, Jeanne Louise Calment of France lived to be 122 years and 164 days old, passing away in 1997. https://twitter.com/shanghaidaily/status/1826074107492127115 Also Read: Cholera Outbreak in Sudan has Killed At Least 22 People
Top Sources Related to Tomiko Itooka: The World’s Oldest Person at 116 Age (For R&D)
Guinness World Records: 116-year-old Japanese woman confirmed as world’s oldest living personTomiko Itooka is now the world’s oldest living person, following the death of 117-year-old Maria Branyas Morera. Euronews:

Meet Tomiko Itooka: The world’s oldest person at 116Born in the same year that saw the Wright Brothers’ initial public flights, Tomiko Itooka has a life as remarkable as her age. AL Jazeera: At 116, Japanese woman set to be named world’s oldest person | Health News | Al JazeeraWe use cookies and other tracking technologies to deliver and personalize content and ads, enable features, measure site performance, and enable social media sharing. You can choose to customize your preferences.Learn more about our Cookie Policy. USA Today:

Japanese woman, 116, set to take title of oldest person the worldTomiko Itooka, 116, is now the oldest person in the world, Guinness World Records says, following the death of a woman who was 117. She loves bananas. AP News: A Japanese woman who loves bananas is now the world’s oldest personTomiko Itooka is now the world’s oldest living person at age 116. Guinness World Records confirmed the Japanese woman’s status Thursday, following the death of 117-year-old Maria Branyas. The Straits Times:

Japanese woman, 116, to be named world’s oldest personMs Tomiko Itooka, who was born in 1908, used to be a mountaineer. Read more at straitstimes.com. Read the full article
7 notes
·
View notes
Text
North Korean dictator Kim Jong-un is apparently in need of medicine.
Kim drinks too much, eats too much, and smokes too much. He is a psychopath who once had an official stripped naked and eaten by dogs. So if you were his doctor, would you tell him that something is wrong with him and that he needs to adjust his lifestyle?
Kim spends a huge amount of money developing nuclear weapons but neglects healthcare – especially public health. North Korea had a disastrous response to COVID-19, even worse than that of the Trump administration. So even the Kim clan, communist absolute monarchs, can't rely on internal health providers and medicines.
North Korean leader Kim Jong Un has regained weight and appears to have obesity-related health problems such as high blood pressure and diabetes, and his officials are looking for new medicines abroad to treat them, South Korea’s spy agency told lawmakers Monday. The 40-year-old Kim, known for heavy drinking and smoking, comes from a family with a history of heart problems. Both his father and grandfather, who ruled North Korea before his 2011 inheritance of power, died of heart issues. Some observers said Kim, who is about 170 centimeters (5 feet, 7 inches) tall and previously weighed 140 kilograms (308 pounds), appeared to have lost a large amount of weight in 2021, likely from changing his diet. But recent state media footage show he has regained the weight. On Monday, the National Intelligence Service, South Korea’s main spy agency, told lawmakers in a closed-door briefing that Kim is estimated to weigh about 140 kilograms (308 pounds) again and is in a high-risk group for heart disease, according to Lee Seong Kweun, one of the lawmakers.
There is already speculation about Kim Jong-un's successor. He has a tween daughter who seems to be the favorite at this point.
The NIS in its Monday briefing maintained its assessment that Kim’s preteen daughter, reportedly named Kim Ju Ae, is bolstering her likely status as her father’s heir apparent. But the NIS said it cannot rule out the possibility that she could be replaced by one of her siblings because she hasn’t been officially designated as her father’s successor. Speculation about Kim Ju Ae, who is about 10 or 11 years old, flared when she accompanied her father at high-profile public events starting in late 2022. State media called her Kim Jong Un’s “most beloved” or “respected” child and churned out footage and photos proving her rising political standing and closeness with her father. The NIS told lawmakers that at least 60% of Kim Ju Ae’s public activities have involved attending military events with her father.
If Kim Jong-un suddenly dies, there's the potential for a succession battle which could be like House of the Dragon but with nukes.
#north korea#dprk#kim jong-un#kim ju-ae#kim's health#north korea succession#communist absolute monarchy#healthcare#dictatorships#북한#김주애#김정은#계승
8 notes
·
View notes
Text
Something I will never get over is how POTS is destroying my health right now.
This is necessary information for my post and I'm not trying to illness Olympics, but my resting heart rate is around 65, an average heart rate increase upon changing positions is 40-70 for me, and my walking heart rate is typically 130s-140s. I've seen it get as high as the 170s. This chronic tachycardia and heart overcompensation increases my risk of heart disease, stroke, and cardiac arrest.
My doctors recommended to me beta blockers to hopefully decrease my tachycardia and my fainting episodes. My issue with this is that I increase my risk of Type 2 Diabetes. Beta blockers have a tendency to reduce one's sensitivity to insulin, increasing the risk of developing Type 2. My risk is increased already without this medication due to my family history. There's still a chance I still faint on this medication due to bradycardia. I could not be decreasing my fainting spells at all.
It's not a guarantee I develop any of these conditions, but I increase my risk of either case everyday depending on whether I decide to get on beta blockers or not. I despise the fact that I have to essentially pick which conditions I might want in the future. This decision is only one I have to make because I caught some sort of viral illness in sophomore year of high-school and developed POTS because of it.
I'm chronically ill and I will continue to get more chronically ill and more disabled everyday I live.
#starlit speaks#potsie#pots patient#pots syndrome#pots#postural orthostatic tachycardia syndrome#tachycardiac#tachycardia#chronically ill#chronic illness#vent post
5 notes
·
View notes
Text
Leave Those Kids Alone - Published Aug 29, 2024
Bullying a child for wearing a mask exposes a stark hypocrisy in some people's view of personal freedom.
If someone bullies a person for wearing a hijab, they face consequences. If they bully a person for wearing a turban, they will be sanctioned according to the rules of their institution or laws that punish racism and discrimination. Most people view the racist bully with disdain because society has determined that targeting someone based on their race or religion is inherently a bad thing.
But what about people who wear masks?
A recent social media thread1 outlined the abuse suffered by a child at the hands of fellow students and adult staff for wearing a mask to protect against the risk of respiratory infection. Replace mask with turban, hijab, crucifix or Star of David and see how you feel about the victimized child and the people who’ve been bullying them. Talk to members of the COVID-safe community and you’ll understand that this sort of bullying is commonplace.
There is never any justification for targeting someone based on their personal choices, attire or appearance. A child or adult who chooses to wear a mask is doing so for their own reasons. They might be immune compromised or have a family member who is immunosuppressed. Diabetes puts people at higher risk of poor outcomes of COVID-19 and other infections2. Perhaps they have a family member with diabetes, or perhaps they themselves live with the condition. Maybe they have an autoimmune disease or a family member who does. Or perhaps they just want to avoid participating in the largest experiment in human history.
Whatever their reason, it is private and none of anyone else’s business. Bullying is often portrayed as the strong picking on the weak, but it is usually the weakest members of society who engage in bullying. Those who seek to externalize the way they feel about themselves, to draw attention away from their own flaws or downplay their own fears.
Mask wearing is backed by science. It has been shown to be almost wholly effective at preventing infection3,4. And there are thousands of scientific studies that demonstrate the short- and medium-term harms of COVID-19 infection5. The long-term impacts of this virus are yet to come, but we do know that SARS-COV-2, the virus that causes COVID-19 results in a rise in autoantibodies even in children6-8. Autoantibodies are components of the immune system that attack the self.
Children who have had COVID-19 are at higher risk of a diverse range of autoantibodies, including those implicated in diabetes6-8. The long-term harms are yet to be determined, but at the very least, societies can expect a rise in autoimmune disease.
The ignorant among us believe infection is a good thing, that it trains the immune system and makes us stronger. We’ve previously written about the error of this belief9. If infection made us stronger, the areas of the world that have the most disease would have the best population health and life expectancy. The opposite is true. In fact, both COVID-19 specifically and infection of any sort more generally have been found to age the immune system, a discovery which may upend conventional views of the immune system as a ‘muscle’9-14.
Take a moment to think about your immune system and the layers involved. We know that infections often deplete immune cells. COVID-19 is particularly well studied in this regard and has been found to deplete dendritic cells, T cells, and other immune cells15,16. Whether transient or longer term, this depletion will leave people more vulnerable to infection and might explain the rise in prevalence of other diseases experienced since the arrival of COVID-1917,18.
In addition to depleting the immune system, COVID-19 is implicated in the creation of autoantibodies19,20, meaning the immune system is being mistrained to attack the body, further weakening the host, and in some cases, causing long-term autoimmune disease, which also further weakens the host.
Some viruses exploit the aftermath of another infection. Dengue has been demonstrated to use antibodies created by prior dengue infection or COVID-1921,22 infection to infect the host more effectively, a process known as antibody dependent enhancement. This phenomenon is also seen in relation to Zika, West Nile Virus and HIV23-26.
In short, there are many ways in which an infection can impact a person and make them more vulnerable to other infections. So, the child who chooses to mask should be commended for taking responsibility for their health and the health of those around them. Under no circumstances should they be bullied or singled out, often by people whose connection to science and current affairs is so feeble that they believe COVID-19 has ‘gone away’ and are shocked when they are reinfected.
In 2020 and 2021, when members of the John Snow Project hypothesized about the long-term impacts of SARS-COV-227, it seemed implausible that a ‘common cold’ could cause so many issues. SARS-COV-2 is not and never will be a common cold. More and more people are noticing an uptick in illness28-37. People are sick more often with a wider variety of illnesses. This was predictable because the mechanisms by which this would happen were understood in 2020. What was also predictable was the rise in all-cause mortality that continues to be seen around the world38,39. We are also likely to see a significant rise in autoimmune diseases over the long-term and a general increase in ill health40.
Instead of bullying a child strong enough to be the only person wearing a mask in school, those being cruel should show some humility and confront the possibility the child might be better informed about human health or have private reasons for continuing to be cautious. Public health bodies and public institutions should do more to protect personal choice and prevent bullying and stigmatization for masking. After all, we are living in a world of individual responsibility and an individual should not be penalized for choosing to be responsible.
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#public health#still coviding#wear a respirator
12 notes
·
View notes
Text
How Regular Exercise Reduces the Risk of Diabetes
Diabetes is a significant health concern affecting millions globally, but the good news is that regular exercise can play a pivotal role in reducing the risk of developing this chronic condition. Regular physical activity is beneficial not only for weight management and cardiovascular health but also for blood sugar regulation and insulin sensitivity. In this article, we will explore how regular exercise helps reduce the risk of diabetes and provide tips for incorporating exercise into your daily routine.

Understanding Diabetes and Its Risk Factors
Diabetes, particularly type 2 diabetes, occurs when the body becomes resistant to insulin or when the pancreas is unable to produce enough insulin. This leads to elevated blood sugar levels, which can cause serious health complications over time. Risk factors for type 2 diabetes include obesity, a sedentary lifestyle, poor diet, and a family history of diabetes.
The Role of Exercise in Diabetes Prevention
Improves Insulin Sensitivity: Regular exercise helps improve the body’s sensitivity to insulin. When you exercise, your muscles use more glucose, reducing blood sugar levels. Over time, this increased glucose uptake by muscles makes your body more responsive to insulin, thereby reducing the risk of insulin resistance.
Helps with Weight Management: Maintaining a healthy weight is crucial in preventing diabetes. Exercise helps burn calories, build muscle, and reduce body fat. Even modest weight loss can have a significant impact on reducing diabetes risk. For individuals who are overweight or obese, losing 5-10% of body weight can greatly improve insulin sensitivity and lower blood sugar levels.
Regulates Blood Sugar Levels: Physical activity helps regulate blood sugar levels by promoting the uptake of glucose into muscle cells. Both aerobic exercises, such as walking, running, and swimming, and resistance training, such as weightlifting, are effective in managing blood sugar levels. Regular exercise also helps to stabilize blood sugar levels throughout the day, reducing the risk of spikes and crashes.
Reduces Visceral Fat: Visceral fat, the fat stored around internal organs, is strongly linked to insulin resistance and type 2 diabetes. Regular exercise helps reduce visceral fat, improving overall metabolic health and lowering diabetes risk.
Enhances Cardiovascular Health: People with diabetes are at a higher risk of developing cardiovascular diseases. Regular exercise strengthens the heart and improves circulation, reducing the risk of heart disease, stroke, and other cardiovascular complications.
Types of Exercise for Diabetes Prevention

Aerobic Exercise: Activities like brisk walking, running, cycling, swimming, and dancing increase your heart rate and help burn calories. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week.
Resistance Training: Strength training exercises, such as weightlifting, bodyweight exercises (e.g., push-ups, squats), and resistance band workouts, help build muscle mass and improve insulin sensitivity. Incorporate resistance training at least two days a week.
Flexibility and Balance Exercises: Activities like yoga and tai chi enhance flexibility and balance, reducing the risk of injuries and improving overall physical fitness. These exercises also promote relaxation and stress management, which are important for diabetes prevention.
Tips for Incorporating Exercise into Your Routine
Start Slow: If you’re new to exercise, start with small, manageable goals. Gradually increase the intensity and duration of your workouts as your fitness level improves.
Find Activities You Enjoy: Choose exercises that you enjoy to make it easier to stick with your routine. Whether it’s dancing, hiking, or playing a sport, enjoyment will keep you motivated.
Make It a Habit: Consistency is key. Schedule regular workout sessions and treat them as non-negotiable appointments.
Stay Active Throughout the Day: Incorporate physical activity into your daily routine by taking the stairs, walking during breaks, or cycling to work.
Monitor Progress: Keep track of your workouts and progress. Celebrate milestones to stay motivated.
Conclusion
Regular exercise is a powerful tool in reducing the risk of diabetes. By improving insulin sensitivity, aiding in weight management, regulating blood sugar levels, reducing visceral fat, and enhancing cardiovascular health, physical activity provides a comprehensive approach to diabetes prevention. Start incorporating regular exercise into your daily routine today to enjoy its numerous health benefits and significantly reduce your risk of developing diabetes.
WE SUGGEST YOU TO BEST SOLUTION FOR BLOOD SUGAR.CLICK TO KNOW MORE HERE
#blood sugar treatment#diabetes treatment#diabetes#type 2 diabetes#blood sugar control#supplements health#sugar control
7 notes
·
View notes