#post-traumatic stress therapy CBT
Explore tagged Tumblr posts
Text

#post traumatic growth#complex post traumatic stress disorder#ptsd recovery#complex ptsd#post traumatic stress disorder#ptsd#cptsd problems#just cptsd things#cptsd recovery#cpstd#psychiatrist#psychiatry#psychology#dbt skills#dbt therapy#dbt#cbt therapy
23 notes
·
View notes
Text
The Use of Virtual Reality to Treat PTSD: A New Frontier in Mental Health Care

Post-Traumatic Stress Disorder (PTSD) is a complex and often debilitating condition that affects millions of people worldwide. Traditional treatments such as cognitive-behavioral therapy (CBT) and medication have helped many, but not all individuals respond well to these approaches. That’s where new technologies like Virtual Reality (VR) are coming in, offering a cutting-edge way to treat PTSD that is showing promising results.
At New Insights Behavioral Health, we’re always exploring the latest innovations in mental health treatment to provide our patients with the best possible care. In this blog, we’ll dive into how VR is being used to treat PTSD and what this exciting technology could mean for the future of mental health care.
1. How Does Virtual Reality Help Treat PTSD?
Virtual Reality therapy, also known as Virtual Reality Exposure Therapy (VRET), is a form of exposure therapy that uses immersive VR environments to help individuals confront traumatic memories in a controlled, safe space. Exposure therapy has long been a proven method for treating PTSD by gradually desensitizing individuals to the triggers of their trauma. VR takes this concept a step further by placing patients directly in lifelike environments related to their trauma, allowing them to confront difficult emotions while under the guidance of a trained therapist.
The immersive nature of VR allows individuals to experience real-life scenarios in a way that talking about their trauma in a traditional therapy session might not. By safely re-experiencing the traumatic event in a virtual setting, individuals can work through their emotions and responses, gradually gaining more control over their symptoms.
2. Customizable and Controlled Therapy
One of the major benefits of using VR in PTSD treatment is the ability to customize the experience for each individual. Unlike traditional talk therapy, where patients are asked to recall their trauma through memory, VR offers a fully immersive environment tailored to the individual’s specific triggers. Whether it’s a combat scenario for veterans or a natural disaster for a survivor, the virtual environment can be adjusted to fit the needs of the patient.
This customization allows for a controlled form of exposure, ensuring that the patient is never overwhelmed during the process. The therapist can pause or adjust the session in real time, making the treatment highly flexible and patient-centered.
3. The Science Behind VR and PTSD Treatment
Virtual Reality’s ability to treat PTSD is supported by scientific studies showing that VRET can be as effective, if not more, than traditional exposure therapy. Research suggests that VR triggers the same psychological and emotional responses as real-life exposure, helping to rewire the brain’s response to trauma. By repeatedly confronting the traumatic event in a controlled VR environment, individuals can reduce the power of the traumatic memory and lessen their overall PTSD symptoms.
What we still don’t fully understand is why VR may be more effective for some individuals compared to traditional methods. One hypothesis is that the fully immersive nature of VR makes the experience more intense, helping to break through barriers that traditional therapy might not reach. While more research is needed, the early results are encouraging.
4. Who Can Benefit from VR Therapy for PTSD?
While VR therapy isn’t a one-size-fits-all solution, it’s proving to be an effective option for many individuals with PTSD who haven’t responded well to traditional treatments. Veterans, first responders, survivors of assault, and individuals who have experienced traumatic accidents or natural disasters may all benefit from VR exposure therapy.
Patients who have difficulty engaging in talk therapy or feel overwhelmed by the idea of reliving their trauma in a clinical setting might find VR to be a more approachable option. The technology allows for gradual exposure, with the therapist guiding the experience step by step.
5. The Future of Virtual Reality in Mental Health
Virtual Reality therapy is still a relatively new tool in the world of mental health treatment, but its potential is vast. As VR technology continues to advance, we can expect even more sophisticated and customizable treatments for PTSD and other mental health disorders. Researchers are also exploring how VR can be used to treat anxiety disorders, phobias, and depression, opening the door to a new era of therapy.
For individuals with PTSD, VR offers hope for a more interactive and personalized treatment approach. At New Insights Behavioral Health, we are excited to see how this technology evolves and how it can be integrated into a comprehensive mental health treatment plan. Our focus remains on providing innovative and compassionate care to help our patients achieve lasting recovery.
Final Thoughts
The use of Virtual Reality to treat PTSD represents a new frontier in mental health care. By offering immersive, customizable therapy sessions, VR provides a powerful tool for helping individuals confront and manage their trauma in a safe and controlled environment. While traditional treatments for PTSD remain effective, VR therapy offers an exciting alternative for those seeking a new approach to healing.
At New Insights Behavioral Health, we stay at the cutting edge of mental health care, incorporating the latest advancements to ensure the best possible outcomes for our patients. If you or a loved one is struggling with PTSD, we’re here to help you explore all available treatment options, including medication management and more – Contact us today and fill out a new patient form to get started.
#mental health#mental health conditions#therapy#medication management#healthcare#anxitey#emotions#cognitive behavioral therapy(cbt)#physical health#post traumatic stress disorder
0 notes
Text

Depression, anxiety, and stress are common mental health challenges that can significantly impact daily life. Depression involves persistent feelings of sadness and loss of interest, while anxiety is characterized by excessive worry and fear. Stress, often a response to life pressures, can exacerbate both conditions if unmanaged. Effective management techniques include regular physical activity, mindfulness, and healthy sleep habits. Cognitive Behavioral Therapy (CBT) and support from mental health professionals can also provide coping strategies and resilience. Prioritizing mental well-being through these practices can help individuals manage symptoms and improve overall quality of life.
#Mental health#Mindfulness#Burnout#Cognitive Behavioural Therapy (CBT)#Workplace stress#Chronic anxiety#Depression symptoms#Stress resilience#Panic attacks#Mental wellness#Stress management#Chronic stress#Post-traumatic stress disorder#Major depressive disorder#Antidepressant medications#Emotional wellbeing
0 notes
Text
How to Improve Your Sleep Quality Without Medication for People with Post-Traumatic Stress Disorder (PTSD)
Sleep is essential for overall health and well-being, but it can be a significant challenge for individuals with post-traumatic stress disorder (PTSD). Fortunately, there are effective strategies to improve sleep quality without relying on medication. In this article, we will explore five simple yet powerful techniques to help you enhance your sleep and promote a restful night’s rest. 1.…

View On WordPress
#(CBT-I)#Cognitive Behavioral Therapy for Insomnia#health#healthy lifestyle#mental health#post-traumatic stress disorder#ptsd#sleep#stress
0 notes
Text
Some free mental health/illness books to look at!
We love internet archive here
The Myth Of Normal
Organizing Solutions for People With Attention Deficit Disorder
Dying to please : anorexia, treatment and recovery
Self harm : the path to recovery
Dealing with depression : understanding and overcoming the symptoms of depression
The post-traumatic stress disorder sourcebook : a guide to healing, recovery, and growth
Borderline personality disorder demystified : an essential guide for understanding and living with BPD
Am I still visible? : a woman's triumph over anorexia nervosa
Back to life, back to normality : cognitive therapy, recovery, and psychosis
Panic attacks workbook : a guided program for beating the panic trick
The autistic brain : thinking across the spectrum
The addiction recovery skills workbook : changing addictive behaviors using CBT, mindfulness, and motivational interviewing techniques
The bipolar workbook : tools for controlling your mood swings
The anxiety & phobia workbook
Reclaiming yourself from binge eating : a step-by-step guide to healing
Your guide to schizophrenia
Overcoming social anxiety and shyness : a self-help guide using cognitive behavioral techniques
DBT Skills Training Manual: Handouts And Worksheets
Bipolar 101 : a practical guide to identifying triggers, managing medications, coping with symptoms, and more
49 tips and insights for understanding addiction
Understanding paranoia : what causes it, how it feels and what to do about it
The beginner's guide to eating disorders recovery
Paths to recovery : Alcoholic Anon's steps, traditions, and concepts
Psychosis : understanding and treatment
Skinny boy : a young man's battle and triumph over anorexia
The borderline personality disorder survival guide : everything you need to know about living with BPD
Recovery of your inner child
Living well on the spectrum : how to use your strengths to meet the challenges
Everyday mindfulness for OCD : tips, tricks & skills for living joyfully
Living with bipolar disorder : a guide for individuals and families
Coping with schizophrenia
Loosening the grip : a handbook of alcohol information
Don't feed the monkey mind : how to stop the cycle of anxiety, fear & worry
Coping with BPD : DBT and CBT skills to soothe the symptoms of borderline personality disorder
Understanding body dysmorphic disorder : an essential guide
How to deal with OCD
Dying of embarrassment : help for social anxiety & phobia
The Body Image Workbook For Girl Teens
Overcoming depression
Trichotillomania, skin picking, and other body-focused repetitive behaviors
Depression : what is it? : what to do?
Voices in Psychosis - Interdisciplinary Perspectives
The brain over binge recovery guide : a simple and personalized plan for ending bulimia and binge eating disorder
The ADHD advantage : what you thought was a diagnosis may be your greatest strength
How to survive your bipolar brain (and stay functional)
The Borderline Personality Disorder Workbook An Integrative Program To Understand And Manage Your BPD
Autistic Community And The Neurodiversity Movement
Taking charge of adult ADHD
Obsessive-compulsive disorders : a complete guide to getting well and staying well
Explaining depression
Bipolar disorder : a guide for patients and families
The cognitive behavioral workbook for depression : a step-by-step program
Overcoming worry and generalised anxiety disorder : a self-help guide using cognitive behavioral techniques
Insight into self harm
Get me out of here : my recovery from borderline personality disorder
Returning to happiness-- : Overcoming depression with your body, mind, and spirit
Food : the good girl's drug : how to stop using food to control your feelings
The autistic spectrum : characteristics, causes, and practical issues
Coping with an abusive relationship
Overcome depression
An introduction to coping with eating disorders
Feeling good : the new mood therapy
Driven To Distraction, Recognizing and Coping with Attention Deficit Disorder from Childhood through Adulthood
#mental health#positivity#self care#mental illness#self help#recovery#autism#autistic#actually autistic#neurodivergent#neurodiversity#bpd#thinspø#self h@rm#ed recovery#childhood trauma#trauma#addiction#adhd#schizophrenia#schizospec#paranoia#paranoid#psychosis#psychology#social anxiety#bipolar disorder#actually bipolar#Trichotillomania#ocd
124 notes
·
View notes
Text
Perception bias, round 2 Director's cut, Saigenos edition!
(or basically, how my brain jumps into another topic only loosely related to the original ask)
Thank you @itsmaferart For the wonderful ask again. :)
Warning: Long post ahead
-*-
Perception bias also serves another more...sinister purpose for Saitama. Psychological conditioning. There is potential evidence for deprivation of basic needs, conditioning for violence for protection and subliminal messages for suggestion, among other things.
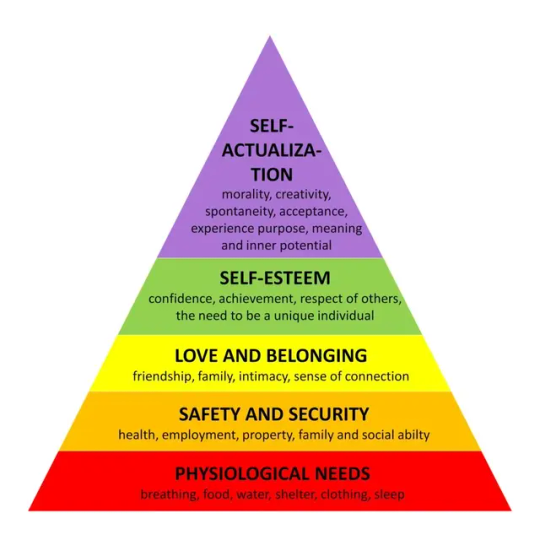
Being deprived of all these needs is akin to mental torture. But so is facing all of the underlying issues at once via hypnotherapy and cognitive behavioural therapy if the patient is sufficiently dysfunctional in a societal setting like Saitama happens to be. Especially if the therapies are performed...poorly.
CBT has shown to be the most effective intervention for people exposed to adverse childhood experiences in the form of abuse or neglect Criticism of CBT sometimes focuses on implementations (such as the UK which may result initially in low quality therapy being offered by poorly trained practitioners. However, evidence supports the effectiveness of CBT for anxiety and depression. Evidence suggests that the addition of hypnotherapy as an adjunct to CBT improves treatment efficacy for a variety of clinical issues. Post Traumatic Stress Disorder (PTSD) and its symptoms have been shown to improve due to implementation of hypnotherapy, in both long and short term. As research continues, hypnotherapy is being more openly considered as an effective intervention for those with PTSD.
In short, in order to heal mentally, Saitama may need to face mental torture because he has such strong willpower and such strong mental barriers shielding his vulnerabilities on a basic primal need. There only needs to be a sufficient trigger.
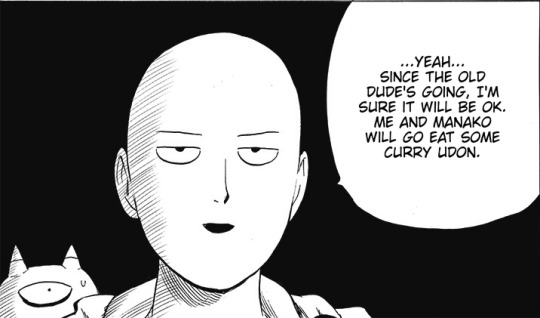
ONE sent Saitama home to restore his energy levels...because he's going to sorely need them for the upcoming confrontation.
Empty Void's ability to genjutsu people casually and cause parallel shifts in the reality and using these to abuse emotional dependencies is like a loaded Chekov's gun on Saitama's forehead. Because Saitama has been roleplaying to re-learn his emphatic skillset after he had suffered too much mental trauma.
That's why early Saitama did not even bat an eye when Beefcake killed his own brother but now he's empathizing with Hamukichi. That's what I call character progression.
Even a compulsive planner like Saitama cannot predict what will happen because he's not familiar with Blast's maladaptive coping methods deep down. Blast is great at masking because they are coping methods so he can bear with his guilt and other issues and just wants to do things on his own, without assistance.

This causes Saitama's perception bias about Blast who seems capable and emphatic, when he is in actuality unscrupulous and amorally indifferent if you really, REALLY study him hard enough.
My bro casually invited Saitama, who is sensitive to aggression, hostility and violence, to watch literal torture of human turned monsters, with an actual smile on his face. And justifying it with his end justify the means philosophy. That's awfully too close to being sadistic and cruel when you consider the ramifications.
They say "love is blind" and Saitama is wearing some rose tinted glasses on because Blast is straight up shady, but he does not see it because he's probably identifying with Blast so hard. Middle-aged, number 1# hero, powerful, confident, outwardly caring, intuitive, ruggedly handsome, positively masculine, secretly gay...you name it. Everything Saitama more than likely fantasies about being because he's so emotionally dependant on Genos and he wants to better himself for Genos due to all his insecurities.
Oh yeah time for some saigenos. *rubs hands*

The very first Genos tells him is to tell Saitama to hide in order to protect him. Saitama has a lot of dependency issues since he has been a small child because he was so emotionally lonely and never got the safety he needed to cope well in life. There are definitely some underlying anxieties or disorders laying about.
Second thing Genos does is show just how smart, capable, cool and devilishly attractive he can be when he gets passionate and engages in combat. Genos can get an awed reaction even from Saitama who's emotions were being blunted during their first spar.
Third is showing he's not gonna judge Saitama for completely embarassing himself, even if he was to get naked around him and lower his inhibitions and showing him it would be ok to trust him on the level of intimacy he craves so dearly. (Season 2 Blu-ray & Dvd: Saitama and the mysterious heroine)
Fourth is showing that Genos is also extremely resilient even when getting hurt...because Saitama hates to see others hurting and he doesn't want it to happen because of him.
And finally the fifth...is because Genos is just as emotionally lonely as he is, but he's unable to let go of his emotional dependencies because he trauma bonds so deeply. He would rather double KO for a Game Over screen than let the monsters win over him and his loved ones on pure principle and take those he trauma bonds with him, because emotional abandonment and guilt would kill him deep inside, so he would rather end it himself for a shred of agency before he withers away.
All these draw in Saitama like moth to a flame and he easily lets Genos into his life. Because he identifies with the lonely teenage boy Genos with traumas who is so familiar to him like coming home.
-*-
Despite everything that has happened to Saitama, he tries to remain optimistic. He's not naturally prone to cynicism unless under great amount of duress. The worst thing to do against him would be Genos emotionally betraying him, betray everything that he perceived in him since the first day they met.
But Saitama has perception bias towards Genos too...such as that Genos is no longer the small teenage boy who needs to be sheltered and cared for, but a battle-hardened soldier. Neither is he a lost naive little sibling in need of guidance or chaperone but an adult wanting mentorship where he can be truly open about his own issues. Would be such a shame if these wrong illusions about Genos were to be shattered...painfully. If Genos were to ever violate that implicit trust Saitama gives to him.
My brother in christ Saitama, he's not actually related to you and he's not your family member even if you'd love him enough to adopt him or something. Not letting go of this notion will spell trouble, like wonky image of relationships and intimacy.
(Yea Saitama please he's not actually related to you, even if it's kind of endearing that Saitama considers Genos to be as close like a family member)
It'll just get worse if Saitama confuses emotional intimacy with sexuality because of his bad upbringing when he's never had any friends and missing his parents too and all his role models have been aggressive and toxic people.
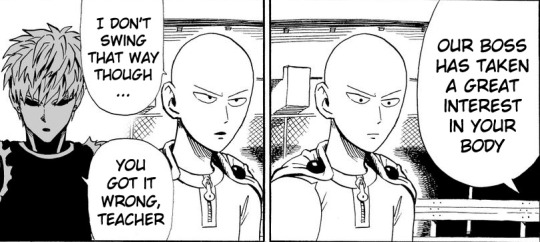
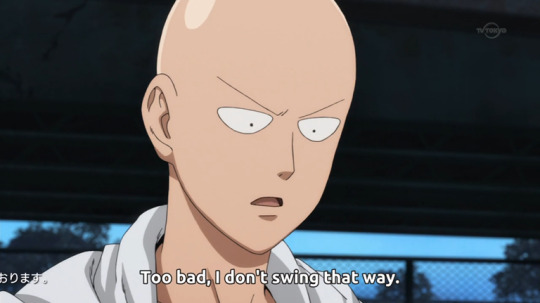
Funny how Saitama's first conclusion about Dr. Genus being interested in his body was sexual in nature and he immediately got defensive. He essentially revealed himself as someone who doesn't even know for sure which way he swings. Which would be quite classic for infj demi but I'll get to that if it becomes more relevant.
Genos naturally knows best though, poor guy looks so disappointed haha. Doesn't stop Genos from attempting every trick in the book besides outright throwing roses at Saitama and arranging dates to get into his good side and woo him, he dressed up so nicely for a spar haha. Dressing to impress, yup. And then he got himself new shiny body and practically walked weeks without a shirt on just so Saitama would see it. (Chapter 185: Updates) My guy has it down bad for Saitama, but Saitama seems oblivious to Genos indirect advances and Genos gave up and finally found a shirt to put on.
(I would pay to see Genos actually chuck roses at Saitama though.)
Even Saitama has to acknowledge that Genos is objectively a hottie though, because in the webcomic he says something along the lines of "he's not even pretty" about Amai-mask and it really makes you think the standards of who Saitama considers pretty when even ikemen like Amai-mask won't do.
-*-
Genos unfortunately is growing up some pretty large perception bias about Saitama after the time travel fiasco. His idolization of Saitama is becoming obsessive and objectifying, like Saitama can do no wrong and that Saitama is some kind of messiah.
Genos also does not take no for an answer. It would be incredibly damaging to both Saitama and Genos when this perception bias is broken when Saitama gets too much on his plate to handle. Like for example...Empty void's specialty, messing with emotional bonds and inducing traumatic events like the illusion of death to break any emotional bond, just like he did to Flashy flash and Sonic.
I do greatly anticipate how Empty Void's fight is going to proceed, we might be in for very big perceptional bias shifts all around, like Flash was forced to acknowledge that he's emotionally dependant on Sonic. (Chapter 201: You pass) And Saitama's idolization of Blast will come crashing down when he finds out what Blast is really up to.
I'll throw some funny perception bias at the end.

#opm#one punch man#saitama#genos#opm meta#saigenos#genosai#saitama x genos#perception bias#opm blast#empty void#flashy flash#emotional intimacy#long post
35 notes
·
View notes
Text
Free Resources for Survivors
Free Therapy in South Florida: ● Survivor’s Pathway Offers Individual and Group Therapy 33 SW 2nd Ave #901, Miami, FL 33130 (786) 275-4364 [email protected] ● Trauma Resolution Center Offers Individual and Group Therapy 2650 SW 27th Ave. Suite 200, Miami, FL 33133 (305) 374-9990 [email protected] ● SunServe Offers Individual and Group Therapy 2312 Wilton Dr, Wilton Manors, FL 33305 (954) 764-5150 [email protected]
9MusesArtCenter: Depression support group and therapeutic art classes ( located in Lauderhill)
Free Apps for Phones: “RAINN” - Gives survivors of sexual violence and their loved ones access to support, self-care tools, and information to help manage short term and long term effects of sexual violence.
“MyPlan Safety App” - myPlan can help you see things more clearly about a current relationship you are in, make decisions about safety, and find resources.
“Calm” - For guided meditations, sleep stories, music, and more
“What’s Up? A Mental Health App” - Utilizes Cognitive Behavioral Therapy and Acceptance Commitment Therapy methods to help you cope with depression, anxiety, anger, and stress.
“I am - Daily Affirmations” - Provides daily affirmations to build self esteem and change negative thought patterns.
“MindShift CBT - Anxiety Relief” - An anxiety management app using scientifically proven strategies based on Cognitive Behavioral Therapy (Must be 18+)
“PTSD Coach” - An app designed for people who have or may have Post-Traumatic Stress Disorder (PTSD)
“BellyBio Interactive Breathing” - A biofeedback app that monitors your breathing when you rest your device on your belly to help you breathe deeply.
“Bearable - Symptom Tracker” - Helps you keep track your symptoms associated with your health.
Free Hotlines: General: Trans Lifeline: (877) 565-8860 Trans Lifeline is a trans-led organization that connects trans people to the community, support, and resources they need to survive and thrive. The General Gay, Lesbian, Bisexual and Transgender (GLBT) National Hotline: (888) 843-4564 Provide telephone, online private one-to-one chat and email peer-support, as well as factual information and local resources for cities and towns across the United States. National Suicide and Crisis Lifeline Call or text 988 To get crisis/suicide support. Available 24/7 anywhere in the United States. Crisis Text Line:
Text START to 741-741 Crisis Text Line is free, 24/7 support for those in crisis. Text from anywhere in the USA to text with a trained Crisis Counselor. National Alliance on Mental Illness (NAMI) Helpline Hotline: 1 (800) 950-6264 Email: [email protected] Available Monday through Friday, 10:00am to 6:00pm Eastern Standard Time. The NAMI Helpline assists individuals and families who have questions about mental health disorders, treatment, and support services. U.S. National Domestic Violence Hotline: (800) 799-7233 (English and Spanish) (800) 787-3224 (TTY) They also have an online chat feature available. Operating around the clock, seven days a week, confidential and free of cost, the National Domestic Violence Hotline provides life saving tools and immediate support to enable victims to find safety and live lives free of abuse. Highly trained, experienced advocates offer compassionate support, crisis intervention information and referral services in over 170 languages. Rape Abuse and Incest National Network (RAINN): (800) 656-HOPE (800) 810-7440 (TTY) The nation’s largest organization fighting sexual violence, RAINN also carries out programs to prevent sexual violence, help victims and ensure that rapists are brought to justice. Substance Abuse and Mental Health Services Administration (SAMHSA) Helpline 1-800-662-HELP (4357) A confidential, free, 24/7 information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides
referrals to local treatment facilities, support groups, and community-based organizations. Domestic violence, sexual assault, and sex trafficking (916) 920-2952 Get 24/7 support and information from WEAVE, for survivors of sexual assault, domestic violence and sex trafficking. National Human Trafficking Hotline 1-888-373-7888 24 hours a day, 7 days a week, in more than 200 languages. All calls are confidential and answered live by highly trained Anti-Trafficking Hotline Advocates. Fenway Health Helpline LGBT Helpline (25+) 1-617-267-9001 Toll-free: 1-888-340-4528 Monday – Saturday 6 p.m. – 11 p.m. ET Fenway Health provides information, help, and referrals to LGBT callers. They also have a peer listening line. For Youth: National Runaway Safeline Hotline: 1 (800) 786 – 2929 Email: [email protected] Available 24 hours a day, 7 days a week via phone, email, forum, and online chat. The National Runaway Safeline provides crisis and support services for homeless and runaway youth in the United States. National Center for Missing and Exploited Children (NCMEC)
Hotline: 1 (800) 843 – 5678 Cyber Tipline: http://www.missingkids.com/gethelpnow/cybertipline NCMEC serves as a clearinghouse and comprehensive reporting center for all issues related to the prevention of and recovery from child victimization. ChildHelp National Child Abuse Hotline Hotline: 1 (800) 422 – 4453 Available 24 hours a day, 7 days a week via phone and text. The Childhelp National Child Abuse Hotline is dedicated to the prevention of child abuse. Serving the U.S. and Canada, the hotline is staffed 24 hours a day, 7 days a week with professional crisis counselors who—through interpreters—provide assistance in over 170 languages. The hotline offers crisis intervention, information, and referrals to thousands of emergency, social service, and support resources. All calls are confidential. Boystown USA – Your Life Your Voice Helpline Hotline: 1 (800) 448 – 3000 Text: Text VOICE to 20121 (hours vary) Available 24 hours a day, 7 days a week via phone, email, text, and online chat. Your Life Your Voice is a program of Boystown USA and is available to children, parents, and families who are struggling with self-harm, mental health disorders, and abuse. The Trevor Project: (866) 488-7386 Text START to 678-678 The Trevor Project is the leading national organization providing crisis intervention and suicide prevention services to lesbian, gay, bisexual, transgender and questioning (LGBTQ) young people ages 13-24. Love is Respect – National Teen Dating Abuse Hotline Hotline: 1 (866) 331 – 9474 Text: 22522
Available 24 hours a day, 7 days a week via phone, text, and online chat. Love is Respect offers information, support, and advocacy to young people who have questions or concerns about their dating relationships. Fenway Health Helpline Peer Listening Line (25 and under) 1-617-267-2535 Toll-free: 1-800-399-PEER Monday – Saturday 5:30 p.m. – 10 p.m. ET Fenway Health provides information, help, and referrals to LGBT callers. They also have a peer listening line. The GLBT National Youth Talkline (youth serving youth through age 25): (800) 246-7743 Provide telephone, online private one-to-one chat and email peer-support, as well as factual information and local resources for cities and towns across the United States. Others: SAGE LGBT Elder Hotline 1-877-360-LGBT (5428) Talk and be heard at the SAGE LGBT Elder Hotline. Connects LGBT older people with friendly responders. For LGBT elders and caretakers. Confidential support and crisis response, available 24/7. StrongHearts Native Helpline 1 (844) 762 – 8483 Available Monday through Friday, 9:00am to 5:30pm CST via phone. The StrongHearts Native Helpline is a safe, anonymous, and confidential service for Native Americans experiencing domestic violence and dating violence. Pathways to Safety International
Hotline: 1 (833) 723 – 3833 Email: [email protected] Available 24 hours a day, 7 days a week via phone, email, and online chat. Pathways to Safety International assists Americans experiencing interpersonal and gender based violence abroad. Womens Law Email hotline: https://hotline.womenslaw.org/ The Womens Law online helpline provides basic legal information, referrals, and emotional support for victims of abuse.
Self Help Books: Use https://libgen.li/ to get these books for free: ● Written on the Body: Letters from Trans and Non-Binary Survivors of Sexual Assault and Domestic Violence by Lexie Bean ● It’s My Life Now: Starting Over After an Abusive Relationship or Sexual Violence by Meg Dugan and Roger R. Hock ● No More Secrets: Violence in Lesbian Relationships by Janice Ristock ● Can't Touch My Soul: A Guide for Lesbian Survivors of Child Sexual Abuse by Donna Rafanello ● Men Who Beat the Men Who Love Them: Battered Gay Men and Domestic Violence by David Island ● Dear Sister: Letters from Survivors of Sexual Violence by Lisa Factora-Borchers ● Unfuck Your Boundaries: Build Better Relationships Through Consent, Communication, and Expressing Your Needs by Faith G. Harper ● Learning Good Consent: On Healthy Relationships and Survivor Support by Cindy Crabb ● The Courage to Heal: A Guide for Women Survivors of Child Sexual Abuse by Ellen Bass, Laura Davis ● What Does Consent Really Mean? by Wallis, Pete Wallis, Joseph Wilkins ● Healing Invisible Wounds: Paths to Hope and Recovery in a Violent World by Richard F. Mollica
● Trauma Stewardship: An Everyday Guide to Caring for Self While Caring for Others by Laura van Dernoot Lipsky, Connie Burk ● I Can't Get Over It: A Handbook for Trauma Survivors by Aphrodite T. Matsakis ● In an Unspoken Voice: How the Body Releases Trauma and Restores Goodness by Peter A. Levine, Ph.D., Gabor Maté, MD ● The Emotionally Abusive Relationship: How to Stop Being Abused and How to Stop Abusing by Beverly Engel ● The Emotionally Abused Woman: Overcoming Destructive Patterns and Reclaiming Yourself by Beverly Engel, M.F.C.C. ● Healing from Trauma: A Survivor's Guide to Understanding Your Symptoms and Reclaiming Your Life by Jasmin Lee Cori, Robert Scaer, MD ● Dangerous Relationships: How To Identify And Respond To The Seven Warning Signs Of A Troubled Relationship by Noelle C. Nelson ● I Will Survive: The African-American Guide to Healing from Sexual Assault and Abuse by Lori S. Robinson, Julia A. Boyd ● Healing Sex: A Mind-Body Approach to Healing Sexual Trauma by Staci Haines ● The Rape Recovery Handbook: Step-By-Step Help for Survivors of Sexual Assault by Aphrodite T. Matsakis ● No Secrets No Lies: How Black Families Can Heal from Sexual Abuse by Robin Stone ● Surviving Childhood Sexual Abuse: Practical Self-help For Adults Who Were Sexually Abused As Children by Carolyn Ainscough, Kay Toon ● Even From A Broken Web: Brief, Respectful Solution-Oriented Therapy for Sexual Abuse and Trauma by Bob Bertolino, Ph. D., Bill O'Hanlon ● Why Does He Do That?: Inside the Minds of Angry and Controlling Men by Lundy Bancroft ● Getting Free: You Can End Abuse and Take Back Your Life by Ginny NiCarthy ● The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk, M.D. ● Psychological First Aid for People with Intellectual Disabilities Who Have Experienced Sexual Abuse: A Step-By-Step Programme by Aafke Scharloo, Simone Ebbers-Mennink, Martine Spijker-Van Spijker-Van Vuren ● Mejor sola que mal acompanada: For the Latina in an Abusive Relationship/Para la mujer golpeada by Myrna M. Zambrano Free Parks in South Florida: Broward: https://www.broward.org/Parks/Pages/default.aspx
Miami-Dade: https://www.miamidade.gov/global/recreation/park-directory.page Free Yoga Classes: ● Miami Beach near the 3rd Street lifeguard tower ○ Everyday at 7 a.m., or at 5 p.m. during fall and winter (6 p.m. in spring and summer)
● Jose Marti in Little Havana ○ Tuesdays at 6 p.m. ● The Underline’s Brickell Backyard Sound Stage Plaza. ○ Every Saturday morning at 9 a.m. ● Peacock Park ○ Every Wednesday at 6:30 p.m. ● Little Haiti Cultural Complex ○ Thursdays at 6 p.m. and Saturdays at noon ● Om & Vine ○ First Saturday of every month at 11 a.m. ● West Dade Regional Library ○ Tuesdays, find yoga for kids at 6:30 p.m., followed by hatha yoga for adults at 7 p.m.
● Maurice A. Ferré Park (formerly known as Museum Park) ○ Tuesdays at 6 p.m., Wednesdays and Fridays at 6:20 a.m. and 6 p.m., Saturdays at 9 a.m. and Sundays at 9:30 a.m.
● North Shore Park Bandshell ○ Mondays and Wednesdays at 6 p.m.
Free Meditation Classes ● Leaves & Roots Lounge - Kava Bar & Vegan Cafe - Guided Meditation and Sound Healing ○ In person every last Sunday of every month at 9am ○ https://www.eventbrite.com/e/leaves-roots-morning-meditation-and-sound- healing-tickets-658044397507?aff=ebdssbdestsearch
● Soul Dimension ○ Online every Wednesday at 1 PM ○ https://souldimension.org/breathe/
● Congregation for Sacred Practices ○ Online every Wednesday at 12 PM ○ https://www.eventbrite.com/cc/weekly-meditations-2318129 ● Brahma Kumaris ○ In person every Friday 7-8:30 PM ○ Coral Gables (LeJeune and 4th St SW) ○ https://miamibrahmakumaris.org/calendar/ ● Oneness Meditation Center North Miami Beach ○ In person every Wednesday from 6-8 PM ● Free Meditation North America ○ Online Saturdays from 9:45 PM-10:45 PM and Sundays from 9:45 AM to 11:00 AM ○ https://www.eventbrite.com/e/miami-meditation-for-peace-health-and- spiritual-growth-tickets-143153021541?aff=ebdssbdestsearch
● Stacey Freeman Sound Therapy New Moon Meditation ○ Every New Moon at 1 or 2 PM ○ https://www.eventbrite.com/e/sound-therapy-new-moon-meditation-miami- fl-tickets-562592718967?aff=ebdssbdestsearch
Free Reiki Classes ● Rev Julia Raether ○ Online every 2nd and 4th Tuesday of the Month at 7 PM ○ https://www.eventbrite.com/e/free-virtual-reiki-circle-tickets- 651179504427?aff=ebdssbdestsearch
● Oasira Initiative - Midnight Reiki ○ Online every Saturday at midnight ○ https://www.eventbrite.com/e/midnight-reiki-weekly-complimentary- session-tickets-712618038737?aff=ebdssbdestsearch
Places of Worship
● Coral Gables Congregational UCC ● Wag Buddharangsi Buddhist Temple ● Sunshine Cathedral ● United Church of Christ Fort Lauderdale
Misc:
Safety Planning
For mental health crisis:
Safety Planning for domestic violence ( from a partner, platonic person, friend parent or room mate while it centers romantic relationships it is not the only thing ive used it for ) : https://www.thehotline.org/plan-for-safety/create-your-personal-safety-plan/
EVA’S CASITA
Website: https://peersupportspace.org/respite Location: Orlando, FL Phone: 407-968-1288 Interest Form: https://docs.google.com/forms/d/e/1FAIpQLSeQIYttup8ffLvL3TcgC_LqG5P2hDcbcR-KU1Vc_mTuT0oT0w/viewform
Our LGBTQ+ led peer respite (welcoming all communities 18+, centering those not usually centered) is the first in Central Florida, the only of its kind in Florida, and the first intentionally focused on underserved communities in the nation. This is a space to take a no-cost, non-clinical break for 1 to 6 nights with voluntary self-driven, group, or 1:1 opportunities to connect with others navigating big feels or life struggles.
#transgender#mental health#self harm#suicide#resources#ill get more on a doc when im...at some point#i only kno florida#south florida#safety planning#the plan is to look at more states but also keep myself being a person so its...ill work on it
5 notes
·
View notes
Note
Hey! I have a few questions about your experiences with final fusion. How would you describe your experience with amnesia before and after the fusion? Also how did you know you finally fused and not just front stuck? Last question, did you regain the memories from childhood? (You can ignore the last question if it’s too personal)
We get front stuck a lot and then convinced we are better only to have a large amnesia chunk 😭 Thank you and congratulations on your healing journey!! That’s awesome!
Hi! These are some great questions :)
1. Amnesia has always been a tricky thing for me, because unless a detail is pointed out to me, I don't realize when I have had an amnesia gap in my memory. In my general day-to-day life pre-fusion, we worked as a team with set schedules for going to work and other things like appointments and were generally responsible and reliable enough to know that we'd gone to work and that we hadn't missed appointments and other things. I had extensive therapy for ADHD and medication in my teenage years and so I had developed a lot of coping mechanisms that helped this aspect, even if it was supposed to help for ADHD, the strategies ended up helping with my DID symptoms as well. The main types of Amnesia we had were traumatic memories locked to specific alters or subsystems, or childhood and adulthood memories that were locked to specific alters that weren't pertinent to daily life such as tasks required for work.
The biggest Amnesia we would have problems with in regards to work were meeting new clients and forgetting they existed or having a change to our schedule or a meeting that was outside our regular routinely schedule. I chalked that up to simply being forgetful until I realized I had did, and then there was a lot of journaling and more prompts to try and mitigate this though not every altar was 100% successful at communicating these.
due to our teenage years being on and off, paid and unpaid therapy programs that we fortunately had access to, even though these therapies were for things like ADHD or simple depression and suicidal Tendencies, I think a lot of the CBT and general talk therapy and mild dabbling in DBT strategies helped us be able to function more as one unit than we probably would have had we had zero therapy until adulthood. I think it helped our main cast of frequent fronters share a lot more memory and have a lot less full blackout Amnesia, and was a contributor to us originally thinking we had osdd1b rather than full DID.
Post fusion, I do have a lot less memory gaps, though. I still do dissociate and I still frequently forget things, especially if it's in regards to a stressful situation or happened at a time that was high stress in my environment. environment. still do forget new clients a lot, though. I at least remember they exist now. I frequently don't remember that first meeting with them until I've met with them a couple more times. I can't picture their face, or anything about them, such as their age or gender without prompting or reviewing notes. My partner tells me that I do forget some conversations we've had, sometimes very minor conversations, and sometimes more important things that I've been wanting to talk about and we finally have a conversation about it and a few days later I will bring up the conversation again, not remembering it was already resolved. I would say this happens at least 80% less, and doesn't really interfere in my day-to-day life to the point where it's a focus of any therapy or something that I'm trying to improve.
2. I will reblog this later on with maybe a little bit of the recount of my final fusion, because I remember essentially live blogging it on discord haha.
it was a very blurry and dissociative fusion, where I knew something was going on, but originally I thought I was splitting- for the first time in quite a long time. it took me a couple hours to realize that our final two alters were fusing together, and I didn't feel like I deserved it at first.
it was hard to accept that I had healed to the point where I truly was ready for that final fusion, especially after just earlier that day (or sometime that week?) saying that I was all right if we stayed as two and weren't able to fuse. We had made peace with that, so fusing so soon after that peace was very surprising and unexpected, which made it harder to wrap my head around.
There was a sense of finality to it, aside from the anxiety of whether this fusion would last or whether we would split apart shortly after, or whether an entirely new split would happen where since we had come together, we wouldn't exactly go back to the two we had, were we to split again.
but after a few weeks we were able to accept that fusion. I was myself together and there was a lot more of the older alters that had fused that we kind of had lost the touch of, or the sense of, in those larger fusions that we were now able to feel again as one whole.
Stem, one of the final two to fuse, had stayed dominant as an alter back from when we were over 90 parts- and she was the co-host right up until being one of the final two to fuse.
Since her personality was so dominant, a lot of the fragments and other alters that she had fused with had been so in the background of their fusion with her, that there wasn't really a sense of those other alters. After Leafy and Stem fused together, a lot of those older alters that we had enjoyed the presence of, who had very specific traits, or ways of thinking, or moods, were now present again and noticeable. So I'd say aside from the anxiety and the doubts that come with not being able to be certain about anything ever (and our OCD that comes with uncertainty) , we were able to work through all of that and truly accept that. Yes, we had final fused.
3. within my therapy, mainly EMDR, to process my traumas to be able to heal and fuse, memory regaining was never a focus or a stressor of mine. between alters across the system we actually retained quite a few memories, but as we developed a sort of timeline of our memories, we realized that a lot of what we thought were memories were actually just fact memorization about our life. For instance, we remembered a lot of our birthday parties, such as in third grade, I had my birthday party at a bowling alley. but aside from looking at photo albums and knowing that location in my memory and being able to know which people had attended, based on looking at those photos, I didn't actually have any internal memories of that bowling party. I know what bowling is like so I can imagine that, I know what being nine is like so I can remember most of how I felt to be a 9-year-old, I can remember what the taste of cake is like, but I had no physical actual remembrance of that event despite knowing it happened.
and that is essentially how my entire memory works aside from very few key memories. Even just having moved in March, I can remember where I lived before I moved in March, but I can no longer remember how it felt to run my daily routine in my old house, what it was like to use the bathroom there or go to bed there or cook and eat there. I don't actually have any physical memory of how it was to be there and live there.
Moving back to your question, however, I might say I remember less of my childhood now than I did pre-fusion, and that is because it is no longer a focus of my life. I find in my day-to-day now I care less about and need to remember less about my childhood and my past to live my current life. prior to fusing or even accessing any type of trauma and coping therapy, I was obsessed with documenting and finding every memory, benign or traumatic that I had in my childhood up into my current age. there was a lot of documentation on discord, private servers and plural kit, sharing which alter remembered which years of my life, which events which traumas or whether they were a memory holder for non-traumatic events. there was also an emphasis on letting those alters front more because they remembered more and I enjoyed remembering and knowing guaranteed facts about my life, especially the nicer memories.
I don't know if this is because we thought that these would be entirely necessary to heal, or because the system community does have an emphasis on trauma holders and memory holders, at least in the circles I was in, or just because that was something I as an entire system valued.
anytime a memory had been triggered by the current alter fronting, there would be an immediate mental documentation of said memory, and a physical notation of the memory were it possible in the moment to do so, followed by digging to try and find more memories. in a lot of ways, this probably wasn't helpful and a number of times, by our own mind and also external factors in people in the community, I believe that we misremembered or had been led to believe that there were more to certain memories than there were in reality (for example, certain trauma types that we had not been through, but had been led to believe and had dug and read into certain memories more than necessary to pretend that they were there).
(*pretend isn't exactly the correct word here as I was never trauma faking, and I never claimed anything out loud that I wasn't 100% sure I did experience, but it was apparent that these memories were shakier than others, and they felt more like lies than true memories compared to the other things that we did remember, if that makes sense.)
Post fusion, these random triggers of old memories are so much less frequent than they were when they were scattered across different alters of the system. Before, I would be very nostalgic and frequently have very sudden intrusions of old memories and feelings or remember lost media from my childhood etc. anything from the weather to a word someone used to a specific color could trigger these memories straight to the forefront. this happens much less now than it used to, to the point where it's actually much more noticeable if I do have a day where I remember something specific, compared to pre-fusion where it was near everyday.
One very very important thing to note about my childhood memories and my ability to process trauma and fuse, is that the memories were very, very much not necessary to being able to process the traumas I went through. I processed quite a few traumas that I had very few details on, or even just a feeling and they were processed in the exact same way that the memories I did have vivid recollection of were processed.
I healed my trauma through EMDR therapy, which is a very intense therapy that tired me out and kept me on edge for the year and a bit I did it, but from my understanding, other trauma therapies such as PE also would be able to process these traumas with lack of memory in the same way.
emdr focuses on a negative cognition you have about yourself from the result of a trauma you faced, and helps you process that cognition and replace it with a better, healthier one. For instance, someone who went through a trauma may have the cognition "if I had been smarter I wouldn't have gone through that. I am weak and I am stupid."
emdr asks you to question that cognition and replace it with what you would rather believe about yourself, such as "going through that didn't make me weak." "I am still strong." "I am safe now" or any other number of positive, healthy beliefs that fit you and your worldview. Now of course a lot of people reading this probably think "oh of course me going through that didn't make me stupid, it wasn't my fault." and I knew that as well. I knew that a lot of my traumas were not my fault and that they didn't make me weaker or worse than anyone else, but it didn't matter with the logical side of my brain said. it mattered how I felt about the events emotionally. and looking into a lot of those traumas, I did have negative emotional beliefs about them despite logically knowing that they didn't make me any worse or better than anyone else.
and that's why you don't need to remember the event itself to be able to process. you just need to know how you feel about the traumas. For all of my targets. I had a traumatic memory that went along with the cognition , but I suspect that even just a vague notion or vague example that wasn't a specific memory would still be enough to successfully process one of these cognitions.
So, in conclusion, this ramble was just to say if you asked your final question because of worry or anxiety about needing to remember things, I promise you will be able to heal without remembering everything and I promise that your life will not be wasted or worth less because you remember less of your childhood. You can still make new memories and live a life you're proud and happy with without needing to know everything from your past.
I hope it's okay. this answer was so long! They was a really good questions so thank you for that :)
#final fusion#fusion#actually system#actually did#did osdd#did system#pro recovery#diary#leafy answers#pluralgang
9 notes
·
View notes
Text
We're all on the mental illness spectrum in some way or another, because life is not an easy feat, with different kinds of stresses throughout, from birth to retirement. Some of us have better or worse than others, and mental health is so complex that we can still relate to each other in some aspects, either minimal or substantial. Stephanie Foo wrote a great book about her own experience as a person recovering from C-PTSD (Complex post-traumatic stress syndrome), and even though I can't imagine how it feels to have a particular mental health issue, I still found myself relating to her in terms of how I deal with my own mental state.

C-PTSD is not a very well-known illness, and it's not the standard PTSD that we all know of.
PTSD is a punctual stress disorder that manifests at a point in time due to a certain trigger, recognized by your brain as a potential threat based on past trauma. Complex PTSD, however, is an ongoing state of sneaky hypervigilance that manifests as anxiety, depression, anger, and dread. This constant and persistent malfunctioning seeps into your personhood, work, and relationships. It usually results from chronic long-term abuse, particularly in childhood.
PTSD can be treated and alleviated with medication and therapy, particularly with CBT (cognitive behavioral therapy), unlike C-PTSD for which there is no consensus yet on what it takes to control it, besides the medication for the resulting symptoms above-mentioned.
Stephanie tells the story of how she managed to reconfigure the way she lives with C-PTSD, before her diagnosis, and after. She shows how small self-care habits and routines, relieved some of the pain, but not the underlying base of suffering. With trial and error, she exerted tremendous effort to look for the most effective solution.
It was therapy, that made a huge impact, but it took the right therapist for it to happen.
You can keep me engaged in anything if your writing is worth it. Stephanie is a journalist and a great writer. She's smart, witty, and pretty self-aware. She can bridge the gap between her and her reader (me) by explaining her state of mind and her pain in a clear, though not very detailed way. I could better imagine what she was going through, without getting overwhelmed.
She talks about how race, class, and politics contributed to her abuse, and how Asians are good at preserving the generational trauma. She also spent some pages talking about how lackluster the healthcare system is, how minorities' pain is usually dismissed, and how healthcare providers are so undertrained in managing mental health problems, especially when they're associated with physical ones.
Even if I don't think I have C-PTSD (I have some other issues, though), there are aspects of Stephanie's story I could relate to: Her broken relationship with her father, and her attempts to repair and maintain relationships, which only works with practice.
My favorite part of the book was her sessions with her therapist in the last few chapters. It baffles me how the most subtle behaviors, gestures, and mimics can show how strong and deep-rooted trauma can be. It takes a good, observant, and empathetic therapist to bring it to the surface.





#book review#booklr#bookstagram#must read#books#booktok#conflict resolution#stephanie foo#what my bones know#mental health#complex ptsd#c ptsd#ptsd#ptsd recovery#childhood trauma#trauma#chinese#generational trauma#nonfiction#biography
5 notes
·
View notes
Text
Understanding Trauma and Exploring Strategies for Healing
Shaina Tranquilino
October 24, 2023

Trauma is a powerful, life-altering experience that can leave lasting emotional, psychological, and even physical scars. It can be caused by various events such as accidents, abuse, violence, natural disasters, or the loss of a loved one. While each person's experience with trauma is unique, it often leads to feelings of fear, helplessness, and disrupted daily functioning. However, there is hope for healing and growth. In this blog post, we will delve into what trauma is and explore strategies to navigate through its aftermath.
Defining Trauma: Trauma refers to an event or series of events that overwhelm an individual's ability to cope effectively. It disrupts their sense of safety and security. Such experiences trigger intense emotions and physiological responses that may persist long after the traumatic event has occurred. Common symptoms include intrusive thoughts, nightmares, flashbacks, hypervigilance, anxiety disorders, depression, mood swings, and difficulty trusting others.
Recognizing the Impact: It's crucial to acknowledge that everyone processes trauma differently; what may be traumatic for one person might not have the same effect on another. Therefore, it's essential to validate personal experiences and offer support without judgment or comparison. Understanding the impact of trauma helps individuals develop empathy towards themselves and others who have gone through similar challenges.
Strategies for Healing:
Seek Professional Help: Trauma recovery often requires professional assistance from therapists specializing in trauma-focused therapy techniques like Eye Movement Desensitization and Reprocessing (EMDR), Cognitive Behavioral Therapy (CBT), or Dialectical Behavior Therapy (DBT). These therapeutic approaches empower individuals to process their trauma safely while developing coping mechanisms.
Practice Self-Care: Engaging in self-care activities can promote healing by nurturing your mind, body, and spirit. This includes getting adequate restorative sleep, maintaining a balanced diet rich in essential nutrients, exercising regularly, and engaging in activities that bring joy and relaxation. Self-care also encompasses setting healthy boundaries, practicing mindfulness or meditation, and seeking support from loved ones.
Connect with Support Networks: Sharing your experiences with trusted friends, family members, or support groups can reduce feelings of isolation and provide a sense of belonging. Surrounding yourself with empathetic individuals who validate your emotions helps rebuild trust and foster a supportive environment for healing.
Cultivate Resilience: Building resilience is an integral part of trauma recovery. Engaging in activities such as journaling, art therapy, or participating in support groups can enhance self-awareness and personal growth. Seeking out positive role models who have overcome similar traumas can inspire hope and motivate you to move forward.
Practice Mindfulness Techniques: Incorporating mindfulness techniques into your daily routine can help manage stress levels and regulate emotional responses triggered by traumatic memories. Breathing exercises, grounding techniques, yoga, or meditation can promote relaxation, self-reflection, and emotional stability.
Trauma is a harrowing experience that disrupts lives but navigating through it is possible with proper understanding and support. Healing from trauma requires patience, self-compassion, professional guidance, and the implementation of various coping strategies tailored to individual needs. Remember that everyone's journey is unique; there is no predefined timeline for healing from trauma. By embracing these strategies and cultivating resilience within ourselves, we can embark on a path towards healing, growth, and reclaiming our lives.
#trauma awareness#healing journey#understanding trauma#heal from within#recovery steps#healing takes time#break the silence#overcoming adversity#share your story#share your experiences#emotional wellbeing#physical wellbeing#mental wellness#resilience building#mental health matters
2 notes
·
View notes
Text

#cptsd recovery#cptsd problems#cptsd#complex post traumatic stress disorder#complex ptsd#psychiatrist#psychiatry#psychology#post traumatic stress disorder#trauma therapy#cbt therapy#dbt therapy#dbt#cognitive behavioral therapy
12 notes
·
View notes
Text
Licensed Mental Health Counselor In New York

Maria Ruiz De Toro, LMHC
Licensed Mental Health Counselor and Supervisor
Are you experiencing emotional pain? Symptoms are not the problem but the solution! By listening to ourselves and reviewing intimate issues, relational patterns and life experiences, in a structured and organized manner; we can better understand out pain and symptoms, heal and gain insight to resolve our conflicts, be more emotionally consistent and work towards supporting out real self. I welcome you to work on this process. I utilize a variety of therapeutic approaches, including insight oriented, psychodynamic and experiential therapies, and evidence-based treatment such as cognitive behavioral therapy.
Please know that one of the strengths of my work entails sorting through life events, including child history and relationships, and helping you to reframe and restructure them into healthier perceptions and positive internalized realities that promote growth.
I believe that including the person’s style and personal interests is essential during the healing process. I also incorporate art interventions and body awareness techniques into my practice. As an international psychotherapist I have lived in and traveled to different parts of the world, including Asia, Europe, and the Americas and I have worked with a culturally diverse caseload throughout my career.
Areas of Expertise:
Anxiety and Depression
Family Therapy and Couples Therapy
Post Traumatic Stress Disorder (PTSD)
Parenting Issues
Developmental Crisis
Life transitions/Moves and Changes
Acculturation and Adjustment
Child and Adolescent Psychotherapy
Education and Experience:
M.A., Brooklyn College, The City University of New York
Interpersonal Psychoanalysis, William Alanson White Institute of Psychiatry
Wellness Self-Management, Columbia University, New York State Institute
Family Therapy and Systemic Approach, Ackerman Institute
Foundations in Marriage and Family Therapy.
Alternatives for Families: Cognitive Behavioral Therapy, St. John’s University
Trauma Focused CBT (Web), Medical University of South Carolina
Mental Health and Family Therapy Training, Roberto Clemente Center NY
Intake Coordinator
New York State License 006853
Click here to schedule an appointment with Maria.
#Mental health counselor#licensed mental health counselor#mental health services#mental health treatment
2 notes
·
View notes
Text
Professional PTSD Help: 5 Essential Steps to Recovery Today Imagine waking up in the middle of the night, heart racing and drenched in sweat, haunted by memories you wish you could forget. This experience is all too common for individuals suffering from Post-Traumatic Stress Disorder (PTSD). Whether the trauma stems from combat, accidents, assault, or natural disasters, PTSD can profoundly affect every aspect of life, including relationships, work, and emotional well-being. This article aims to provide clarity on the path to recovery, presenting you with five essential steps that can lead to a more hopeful and fulfilling life. Understanding the Core Issue Before diving into actionable steps, it's crucial to understand what PTSD is and how it manifests in daily life. PTSD is an anxiety disorder that can occur after experiencing or witnessing a traumatic event. Symptoms often include: Intrusive Memories: Unwanted, distressing memories of the trauma. Avoidance: Steering clear of reminders or conversations about the event. Negative Changes in Thoughts and Mood: Experiencing feelings of hopelessness, detachment, or difficulty trusting others. Hyperarousal: Being easily startled, feeling tense, or experiencing difficulty sleeping. Statistics and Research According to the U.S. Department of Veterans Affairs, approximately 7-8% of the population will experience PTSD at some point in their lives. The National Center for PTSD reports that around 10% of women and 4% of men may develop PTSD after a traumatic event. Studies have shown that social support can significantly affect recovery outcomes, highlighting the importance of seeking help. Understanding these facets of PTSD helps demystify the experience, making it easier to confront and manage. As you navigate through recovery, knowing you are not an anomaly can instill some comfort. Practical Tips and Strategies Recovery from PTSD often requires a multifaceted approach. Here are five essential steps you can take: Step 1: Seek Professional Help Engaging with a mental health professional trained in PTSD treatment can provide tailored strategies for managing symptoms. Various forms of therapy are particularly effective: Cognitive Behavioral Therapy (CBT): Helps identify and challenge negative thought patterns. Eye Movement Desensitization and Reprocessing (EMDR): Involves reprocessing traumatic memories. Exposure Therapy: Gradually exposes you to trauma-related stimuli to reduce fear. Example: Consider Emily, a combat veteran who sought help after years of numbing her pain with isolation. She found a therapist specializing in PTSD who guided her through EMDR. This process allowed her to confront her memories in a safe environment, leading to significant improvements in her daily functioning. Step 2: Build a Support Network Strong relationships can aid recovery significantly. Reach out to friends, family, or support groups who understand or have experienced similar challenges. Talk to Trusted Individuals: Share your experiences with people who are patient and empathetic. Join a Support Group: Connecting with others who are navigating similar paths can create a sense of community and understanding. Example: After realizing she couldn't cope alone, Sarah, a survivor of a traumatic accident, joined a local PTSD support group. Sharing her story with others helped her feel validated and understood, which was integral to her healing. Step 3: Develop Coping Strategies Implement practical coping mechanisms to help manage symptoms and prevent overwhelming distress. These can include: Mindfulness Techniques: Practices like meditation and deep breathing can ground you and relieve anxiety. Physical Activity: Exercise has been shown to reduce symptoms of PTSD by increasing endorphin levels. Journaling: Writing about your feelings and experiences can help process trauma. Example: Mark started a daily routine where he spent ten minutes in the morning practicing mindfulness, followed by a short walk.
Over time, these small habits led to reduced anxiety and improved focus throughout his day. Step 4: Educate Yourself Knowledge is power. Understanding PTSD will enable you to better manage symptoms and make informed decisions about your treatment. Read Books and Articles: Resources such as "The Body Keeps the Score" by Bessel van der Kolk can provide insight into the physical effects of trauma. Stay Current with Research: Following developments in PTSD research can introduce new strategies for recovery. Example: After researching trauma and its effects, Jessica discovered specific techniques that resonated with her. This knowledge empowered her to engage more effectively with her therapist and implement what she learned in daily practices. Step 5: Set Realistic Goals Recovering from PTSD is not an overnight process. Establishing manageable and realistic goals can provide structure and a sense of achievement. Small Wins: Set daily or weekly goals, such as attending a therapy session or trying a new coping strategy. Track Progress: Keep a journal to monitor your journey, documenting both successes and setbacks. Example: Leo faced challenges in maintaining motivation. By setting a simple goal to attend one therapy session each week and gradually increasing engagements in social activities, he acknowledged his growth and progress. Overcoming Challenges While the path to recovery may seem daunting, recognizing obstacles is a critical part of the healing process: Stigmas Surrounding Mental Health: Many people grapple with societal perceptions of PTSD, which can deter them from seeking help. Solution: Educate yourself and others. Sharing personal experiences can promote understanding and diminish stigma. Reluctance to Share Feelings: Vulnerability can feel daunting, particularly for those used to suppressing emotions. Solution: Start small. Write a letter to someone you trust where you express your feelings without fear of judgment. Challenges in Maintaining Routine: PTSD can disrupt daily functioning, making it difficult to stick to treatment plans. Solution: Create a structured schedule. Having a daily plan can instill a sense of normalcy and control. Conclusion The journey to recovery from PTSD is undeniably challenging but also profoundly transformative. By taking these five essential steps—seeking professional help, building a support network, developing coping strategies, educating yourself, and setting realistic goals—you can build a pathway to healing. Recognizing that recovery is not linear can help you navigate this process with compassion toward yourself. Focus on the steps you can take today; every small action can contribute to your progress. Reflect on this: What small step can you take today to start moving toward recovery? Whether that’s reaching out for help or dedicating five minutes to mindfulness, every effort counts. Your path to healing begins with the decision to take that first step.
0 notes
Text
How VR Therapy is Changing the Landscape of Mental Health Treatment?

VR therapy has proven to be a cornerstone in mental health treatment. By immersing patients into immersive visual virtual environments, this technology enables a level of assessment & therapeutic intervention that makes the diagnosis simpler for medical professionals. This innovative tool not only enhances exposure-based treatments in a safe & controlled setting but also aligns to educate healthcare professionals, patients, & public in general. The upsurge of VR therapy in healthcare reflects a growing acknowledgment of its benefits & applications.
A New Era in Mental Health Care
Virtual reality, a technology once confined to gaming and entertainment, is now making significant inroads into healthcare, particularly mental health treatment. VR therapy utilizes immersive simulations to create controlled environments where patients can confront fears, practice coping mechanisms, or simply relax. This level of customization and control enables therapists to address specific issues in a way that was previously unimaginable.
Traditional mental health treatments, while effective, often rely on verbal communication or exposure in real-world settings. These methods can be intimidating for patients or logistically challenging for therapists to implement. It bridges this gap by offering an environment that feels real but is entirely safe and controlled. For instance, someone with a fear of flying can experience a simulated flight, gradually desensitizing themselves to their phobia without stepping onto an actual airplane.
Applications in Mental Health

1. Phobia Treatment
One of the most well-documented uses of VR therapy is in treating phobias. Exposure therapy, a common approach for addressing fears, often involves confronting the object or situation causing anxiety. This therapy enhances this process by allowing patients to face their fears in a virtual setting. Whether it’s heights, spiders, or crowded spaces, VR simulations can recreate these scenarios with remarkable realism, providing a safe yet effective exposure experience.
2. Post-Traumatic Stress Disorder (PTSD)
PTSD has long been a challenging condition to treat, especially for veterans and trauma survivors. VR therapy has emerged as a game-changer in this area by providing controlled environments where patients can revisit traumatic events at their own pace. This approach, known as Virtual Reality Exposure Therapy (VRET), enables individuals to process their experiences in a therapeutic context, guided by trained professionals.
3. Anxiety and Stress Management
In today’s fast-paced world, anxiety and stress are prevalent across all demographics. VR therapy offers immersive relaxation environments, such as tranquil beaches, serene forests, or calming music-scapes. These settings help individuals reduce stress and practice mindfulness techniques. For corporate leaders and startup founders navigating high-stress environments, such therapeutic tools can be invaluable.
4. Cognitive Behavioral Therapy (CBT)
VR therapy enhances Cognitive Behavioral Therapy by allowing patients to practice coping strategies in simulated real-world scenarios. For instance, someone struggling with social anxiety can practice public speaking or interacting with strangers in a virtual environment, building confidence and reducing fear over time.
5. Adolescent Mental Health
The potential of VR therapy extends to younger demographics as well. Adolescents facing mental health challenges often engage better with technology-driven interventions. Gamified VR experiences can make therapy more appealing to younger patients, fostering engagement and adherence to treatment plans.
Benefits
1. Customization and Precision
VR therapy allows for highly tailored treatment plans. Therapists can adjust the intensity and complexity of simulations to suit individual needs, ensuring a personalized approach. This precision makes it particularly effective for conditions like PTSD, where gradual exposure is crucial.
2. Accessibility
As VR technology becomes more affordable, the accessibility of the therapy is increasing. Remote sessions are also becoming viable, enabling patients in underserved areas to receive high-quality care without traveling.
3. Measurable Progress
VR platforms often include tracking and analytics tools, allowing therapists to monitor progress in real time. Data on patient reactions, time spent in simulations, and behavioral improvements provide valuable insights for refining treatment.
4. Enhanced Engagement
For many patients, traditional therapy can feel abstract or disconnected from real-life challenges. VR therapy’s immersive nature fosters deeper engagement, as patients feel directly involved in their treatment.
Challenges and Considerations
While the promise of the therapy is immense, it is not without challenges. Initial costs of VR equipment can be a barrier for some clinics, although prices are steadily decreasing. Additionally, therapists must undergo specialized training to use VR tools effectively and ensure patient safety. Ethical concerns, such as data privacy and the potential for over-reliance on technology, must also be addressed as the field evolves.
Moreover, this therapy may not be suitable for everyone. Patients with certain neurological conditions or severe motion sickness may find the immersive nature of VR disorienting. Careful screening and a collaborative approach between patient and therapist are essential to ensure its suitability.
The Future in Mental Health
As VR technology continues to advance, its applications in mental health are likely to expand. The integration of artificial intelligence (AI) promises to enhance this therapy further by enabling real-time adaptation to patient responses. For example, AI could adjust the difficulty level of a simulation based on a patient’s anxiety levels, ensuring optimal therapeutic outcomes.
Furthermore, the therapy is poised to become a cornerstone of telehealth initiatives. By combining VR with remote care platforms, therapists can reach patients who face geographical or logistical barriers to in-person treatment. This hybrid model has the potential to democratize access to mental health care on a global scale.
Conclusion
VR therapy is revolutionizing the mental health landscape, offering innovative solutions for conditions ranging from phobias to PTSD. By providing safe, controlled, and immersive environments, it enables therapists to deliver personalized and effective care. While challenges remain, the benefits of VR therapy—including accessibility, engagement, and measurable outcomes—underscore its potential as a transformative tool in mental health treatment.
For C-suite leaders, entrepreneurs, and managers, the rise of this therapy represents not just a leap in healthcare innovation but also an opportunity to invest in and support technologies that enhance well-being. As mental health continues to gain recognition as a critical component of overall health, embracing tools like this therapy can pave the way for a more inclusive and effective approach to care.
Uncover the latest trends and insights with our articles on Visionary Vogues
0 notes
Text
Transforming Mental Health: Exploring Effective Therapy for Modern Challenges
Understanding Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy Texas has garnered widespread recognition as a transformative tool in mental health care. It is grounded in the principle that thoughts, feelings, and behaviors are interconnected, and by changing negative thought patterns, individuals can significantly improve their mental health. CBT is particularly effective for addressing issues such as anxiety, depression, and post-traumatic stress disorder.
In a typical CBT session, therapists guide individuals to identify irrational beliefs and replace them with realistic and constructive alternatives. For instance, someone struggling with feelings of inadequacy can learn to challenge those thoughts, replacing self-doubt with affirmations of capability. This structured, goal-oriented approach has made CBT a preferred choice for countless individuals in Texas.
The Role of CBT in Everyday Life
Beyond the therapy room, Cognitive Behavioral Therapy Texas equips individuals with practical skills to navigate daily challenges. Techniques like mindfulness, journaling, and cognitive restructuring empower individuals to cope with stressors more effectively. These tools foster resilience, enabling a proactive approach to mental well-being.
One of CBT's unique strengths lies in its adaptability to diverse situations. Whether dealing with workplace pressure or interpersonal conflicts, individuals can apply the principles learned in therapy to improve outcomes. This flexibility has cemented CBT’s reputation as an indispensable resource for fostering emotional health.
Decoding Therapy for Perfectionism
In Nevada, many individuals grapple with the relentless pursuit of perfection—a mindset that often leads to anxiety and burnout. Therapy for perfectionism addresses the underlying issues driving these behaviors. This form of therapy focuses on helping individuals redefine their self-worth, independent of external achievements, and encourages them to embrace imperfection as a natural part of life.
Therapy for Perfectionism Nevada delves into thought patterns that fuel the need for flawless execution. By challenging these beliefs, individuals learn to set realistic expectations and develop self-compassion. This process alleviates the pressure of unattainable standards and fosters a healthier relationship with personal growth and success.
The Impact of Therapy on Perfectionism
The transformative power of Therapy for Perfectionism Nevada extends beyond alleviating anxiety. It promotes a mindset shift that encourages balance and self-acceptance. Individuals often find that by addressing their perfectionist tendencies, they unlock greater creativity and productivity in various aspects of their lives.
0 notes
Text
Please don’t read this as me dismissing CPTSD. I have it myself. There are a few semantic issues I take with the previous posts that I feel the need to point out to reblog its otherwise incredibly important messages.
As the reblog before mine sort of corrected, CPTSD stands for Complex Post-Traumatic Stress Disorder and not Chronic Post-Traumatic Stress Disorder. I feel that accuracy is always important and since this is a topic where we want little confusion that clarification is warranted.
I don’t know what the reblog before mine means by “a toxic but not abusive relationship”. CPTSD is caused by consistent abuse. “Toxic” isn’t really a legal or medical term we can lean on but consistently harmful behaviour is certainly abuse.
I also want to call attention to the fact that causing CPTSD in a person is harming them. CPTSD means severe impairment to the development of the brain. It means disability. It means often suffering from the symptoms for life, with those few who end up considered “cured-ish” having to go through therapy for a decade, sometimes more, sometimes less. Abusing someone, regardless of method, is harmful.
Also, I want to put out there that it’s not uncommon for people who suffered the conditions that cause CPTSD to also have suffered larger traumatic events that could cause PTSD. You can have both. Also, what can cause CPTSD and PTSD seems to vary from person to person, environment to environment. Even twins who go through the same events can come out with different results, with some developing CPTSD or PTSD and some not.
All of this is relatively new in the field of psychology and you’ll find that few therapists have the knowledge to adequately identify or treat these issues. To top it off, it seems like somatic therapy is effective for some people and your typical CBT or DBT is harmful to many, and CBT especially is incredibly commonly the only therapy on offer. So… stay safe out there. If you can help it, don’t let an inexperienced, uninformed therapist harm you even further.
I love you.
Folks have got to understand that they probably aren't messed up by some Secret Big Trauma that they just can't remember; but rather by a million tiny microtraumas that they do mostly remember but don't even register as traumatic because nobody actually understood that these things would cause trauma, much less stack on each other over the years.
145K notes
·
View notes