#Post-traumatic stress disorder
Explore tagged Tumblr posts
Text



#Dating#interracial dating#coonery#courtney clenney#onlyfans model#miami#luxury condo#boyfriend#stabbing#second-degree murder#christian obumseli#edgewater#texas#police reports#arrest#hawaii#substance abuse#post-traumatic stress disorder
81 notes
·
View notes
Text
Understanding the Symptoms of PTSD: A Comprehensive Guide
Post-Traumatic Stress Disorder (PTSD) is a mental health condition triggered by experiencing or witnessing a traumatic event. Recognizing and understanding the symptoms of PTSD is crucial for providing support and effective treatment. This comprehensive guide will delve into the various symptoms of PTSD, the impact they have on individuals, and how to approach someone suffering from this condition, while also incorporating relevant keywords for a holistic understanding.
What is PTSD?
PTSD can develop after an individual experiences a traumatic event such as war, natural disasters, sexual assault, or serious accidents. The condition can cause significant distress and impair daily functioning. It's essential to understand the symptoms to provide appropriate support and avoid actions that could exacerbate the condition.
Symptoms of PTSD
PTSD symptoms are generally grouped into four categories: intrusive memories, avoidance, negative changes in thinking and mood, and changes in physical and emotional reactions. Each category encompasses a range of symptoms that can vary in intensity and duration.
1. Intrusive Memories
Intrusive memories are recurrent, unwanted memories of the traumatic event. They can include:
Flashbacks: Reliving the traumatic event as if it were happening again.
Distressing Dreams or Nightmares: Recurring dreams related to the traumatic event.
Severe Emotional Distress or Physical Reactions: Experiencing intense emotions or physical responses (e.g., heart pounding, sweating) when reminded of the traumatic event.
2. Avoidance
Avoidance symptoms involve steering clear of reminders of the traumatic event. This can manifest as:
Avoiding Places, Activities, or People: Staying away from situations that trigger memories of the trauma.
Refusing to Talk About the Event: Avoiding conversations or thoughts about the traumatic experience.
3. Negative Changes in Thinking and Mood
PTSD can cause significant shifts in mood and cognitive function, such as:
Negative Thoughts About Oneself or Others: Persistent negative beliefs about oneself, others, or the world.
Hopelessness About the Future: A sense of doom or bleak outlook on the future.
Memory Problems: Difficulty remembering important aspects of the traumatic event.
Difficulty Maintaining Close Relationships: Struggles with feeling connected to others.
Detachment from Family and Friends: Feeling emotionally numb or detached from loved ones.
Lack of Interest in Activities: Losing interest in activities once enjoyed.
Emotional Numbness: An inability to experience positive emotions.
4. Changes in Physical and Emotional Reactions
These symptoms are also known as arousal symptoms and can include:
Irritability or Anger Outbursts: Experiencing frequent irritability or angry outbursts.
Always Being on Guard: A heightened sense of being on alert or easily startled.
Self-Destructive Behavior: Engaging in risky or self-destructive activities.
Trouble Sleeping: Difficulty falling or staying asleep.
Trouble Concentrating: Problems with focusing or concentrating on tasks.
The Impact of PTSD
The symptoms of PTSD can have a profound impact on an individual’s life. They can affect relationships, work, and overall well-being. Understanding these impacts is essential for providing effective support.
Relationships
PTSD can strain relationships, as individuals may withdraw from loved ones or have difficulty expressing their feelings. This can lead to misunderstandings and emotional distance.
Work
The symptoms of PTSD, such as trouble concentrating and irritability, can interfere with job performance. Individuals may struggle with maintaining employment or performing daily tasks.
Overall Well-Being
PTSD can lead to other mental health issues, such as depression, anxiety, and substance abuse. The chronic stress associated with PTSD can also contribute to physical health problems.
What Not To Do to Someone With PTSD
When supporting someone with PTSD, it’s crucial to avoid actions that could exacerbate their symptoms. Here are some important considerations:
Do Not Pressure Them to Talk: Forcing someone to discuss their trauma can lead to increased distress. Let them share at their own pace.
Avoid Triggers: Be mindful of potential triggers and avoid exposing them to situations or conversations that might cause distress.
Do Not Dismiss Their Feelings: Acknowledge their emotions and avoid saying things like "get over it" or "move on."
Do Not Take Their Symptoms Personally: Understand that their reactions are related to their trauma and not a reflection of their feelings toward you.
Effective Support for Someone with PTSD
Providing support to someone with PTSD involves understanding their needs and offering compassionate assistance. Here are some strategies:
Be Patient and Understanding
Patience is key when supporting someone with PTSD. Understand that their recovery process can be lengthy and non-linear. Offer empathy and avoid placing expectations on their progress.
Encourage Professional Help
Encourage them to seek help from mental health professionals. Facilities like Pacific Neuropsychiatric Specialists (PNS) offer specialized care for individuals with PTSD. Professional therapy and counseling can significantly aid in managing symptoms.
Provide a Safe and Supportive Environment
Create a safe space where they feel comfortable and secure. This includes minimizing exposure to triggers and providing emotional support without judgment.
Learn About PTSD
Educate yourself about PTSD to better understand what your loved one is experiencing. This knowledge will enable you to offer more effective support and avoid actions that might cause harm.
Encourage Healthy Coping Mechanisms
Encourage the use of healthy coping strategies, such as exercise, mindfulness, and relaxation techniques. These can help manage stress and improve overall well-being.
Seeking Professional Help
Professional help is often necessary for managing PTSD. Various treatment options are available, including:
Cognitive Behavioral Therapy (CBT)
CBT helps individuals identify and change negative thought patterns and behaviors. It is highly effective for treating PTSD.
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is a specialized therapy that helps individuals process and integrate traumatic memories, reducing their impact.
Medication
Medications, such as antidepressants and anti-anxiety drugs, can help manage symptoms of PTSD. A healthcare provider can recommend appropriate medication based on individual needs.
Support Groups
Support groups provide a space for individuals with PTSD to share their experiences and receive support from others who understand their challenges.
The Role of Pacific Neuropsychiatric Specialists (PNS)
Pacific Neuropsychiatric Specialists (PNS) is dedicated to providing comprehensive mental health care, including specialized treatment for PTSD. PNS offers a range of services designed to address the unique needs of individuals with PTSD, including:
Individual Therapy: One-on-one sessions with experienced therapists to address specific symptoms and develop coping strategies.
Group Therapy: Support groups that provide a sense of community and shared understanding.
Medication Management: Assessment and prescription of appropriate medications to manage symptoms.
Integrated Care: A holistic approach that addresses both mental and physical health needs.
Conclusion
Understanding the symptoms of PTSD is essential for providing effective support and fostering recovery. By recognizing the various symptoms, offering compassionate support, and encouraging professional help, we can make a significant difference in the lives of those affected by PTSD. Remember, the journey to recovery is unique for each individual, and patience and understanding are key components of effective support.
For those seeking professional help, Pacific Neuropsychiatric Specialists (PNS) offers comprehensive and specialized care for PTSD. By leveraging the expertise of mental health professionals and utilizing effective treatment strategies, individuals with PTSD can achieve a better quality of life and improved mental health.
In conclusion, it is crucial to approach individuals with PTSD with empathy, understanding, and patience. Knowing What Not To Do to Someone With PTSD is as important as understanding the symptoms. By avoiding actions that could trigger distress and providing a supportive environment, we can help those affected by PTSD navigate their path to healing and recovery.
2 notes
·
View notes
Text
Mental disorders and criminal legal involvement: Evidence from a national diagnostic epidemiological survey
Open Access Peer-reviewed Research Article Jeffrey W. Swanson , Madeline Stenger, Michele M. Easter, Natalie Bareis, Lydia Chwastiak, Lisa B. Dixon, Mark J. Edlund, Scott Graupensperger, Heidi Guyer, Maria Monroe-DeVita, Mark Olfson, T. Scott Stroup, Katherine S. Winans, Marvin S. Swartz Published: April 9, 2025 https://doi.org/10.1371/journal.pmen.0000257 Abstract Large numbers of adults…
#Bipolar 1 Disorder#Generalized Anxiety Disorder#Major Depressive Disorder#Obsessive-Compulsive Disorder#Post-Traumatic Stress Disorder#Schizophrenia-Spectrum Disorder
1 note
·
View note
Text
Traumatic Brain Injuries after an auto accident - Palmer Litigation - St. George Attorneys
Discover the dangers and outcomes of traumatic brain injuries from vehicle collisions, along with their causes, warning signs, and the urgency of seeking medical attention.
#Traumatic Brain Injuries in Auto Accidents#Traumatic Brain Injuries#TBI in Auto Accidents#Causes of TBI#post-traumatic stress disorder
0 notes
Text
Which Non-Invasive Treatment Can Help with PTSD and Anxiety?
Post-Traumatic Stress Disorder (PTSD) and anxiety are debilitating conditions that can make everyday life feel overwhelming. Many people with these conditions don’t find complete relief with traditional treatments alone. An alternative option, repetitive transcranial magnetic stimulation (rTMS), offers a non-invasive approach to managing PTSD and anxiety symptoms by directly stimulating the brain’s mood-regulating areas.
0 notes
Text

Depression, anxiety, and stress are common mental health challenges that can significantly impact daily life. Depression involves persistent feelings of sadness and loss of interest, while anxiety is characterized by excessive worry and fear. Stress, often a response to life pressures, can exacerbate both conditions if unmanaged. Effective management techniques include regular physical activity, mindfulness, and healthy sleep habits. Cognitive Behavioral Therapy (CBT) and support from mental health professionals can also provide coping strategies and resilience. Prioritizing mental well-being through these practices can help individuals manage symptoms and improve overall quality of life.
#Mental health#Mindfulness#Burnout#Cognitive Behavioural Therapy (CBT)#Workplace stress#Chronic anxiety#Depression symptoms#Stress resilience#Panic attacks#Mental wellness#Stress management#Chronic stress#Post-traumatic stress disorder#Major depressive disorder#Antidepressant medications#Emotional wellbeing
0 notes
Text
#Post-Traumatic Stress Disorder Treatment Market#Post-Traumatic Stress Disorder Treatment#treatment#disorder#traumatic#stress#Post-Traumatic Stress Disorder
0 notes
Text
Explore the complexities of postpartum PTSD and birth trauma. Learn about the symptoms, causes, and healing strategies to support new mothers in their journey towards recovery and well-being.
0 notes
Text
Stop Ruminating: an Angel Can End Rumination
Do you obsessively overthink things? Is your mind trapped in a loop of negativity? End Rumination. An Angel Can Help You Stop Ruminating. Continue reading Stop Ruminating: an Angel Can End Rumination

View On WordPress
#an angel can end rumination#Angel#angel help#angel-summoning session#angelic intervention#break cycle#break free#break the cycle of rumination#cycle#end rumination#help to stop ruminating#how to stop severe ruminations#let go of the past#negative thoughts#post-traumatic stress disorder#ruminating#rumination#rumination is a symptom of#ruminative#ruminative thoughts#schedule angel-summoning session#stop#stop ruminating#stop ruminating help#stress disorder#thoughts#what causes rumination#what does it mean when a person is ruminating#what does ruminating mean#what is the meaning of rumination
1 note
·
View note
Text
Sintomi somatici: una componente sottovalutata dei disturbi mentali conseguenti a traumi infantili
I sintomi somatici comprendono una varietà di disturbi fisici, che causano compromissione funzionale e grave disagio emotivo; possono o meno essere associati ad altre condizioni mediche diagnosticate. Questi includono sintomi come disturbi gastrointestinali, dolori muscolari (ad esempio alle braccia, alla schiena e mal di testa), effetti cardiopolmonari (ad esempio dolore al petto e vertigini) e…

View On WordPress
#benessere mentale#colon irritabile#disturbo psicosomatico#disturbo somatoforme#esperienze infantili avverse#post-traumatic stress disorder#salute mentale#salute pubblica#sintomi somatici#stress psicologico#trauma infantile
0 notes
Text
Seated Mediation
We tend to see body, breath, and mind separately, but in meditation they become one. The first thing to pay attention to is the body position during sitting. How you position your body has a lot to do with what happens with your mind and your breath.
As our School comes from Asian traditions, the basic meditation posture is to sit on a mat and cushion on the floor. For Westerners who are used to sitting in chairs, this can often cause discomfort. For this reason, our School allows for many variations to help students find a stable and comfortable posture for sitting meditation. There is absolutely no esoteric significance to the different positions. What is most important in sitting meditation is what we call mind sitting, rather than body sitting-how do we keep our mind just now? In order to do that, a good posture is useful and supports our practice.
Sitting Meditation
Place one or more cushions on a mat sit cross-legged position.
Using a chair. When sitting on a chair, your feet should not extend past the front edge of the row of mats in the row in which you are seated in a group practice setting. You may fold your mat and place it under your chair. You may use the mat for a footrest. For meditation purposes, it is best that you do not lean against the back of the chair, but sit toward the front of the seat, keeping your back erect. Your thighs should be parallel, flat on the floor. Straddling cushions. Stack several cushions on top of one another, straddling them as if riding a horse. Using a meditation bench. Meditation benches have a slanted seat with two legs. First kneel on your mat, then position the bench over your calves behind you, and sit. Keeping your spine straight and shoulders back and loose, tip your head forward very slightly, looking down at the floor at a 45-degree angle. Your eyes should be half open, looking at the floor in front of you.
Place your hands in your lap in in the maha mudra (see Hands below for full description).
Knees and spine
When sitting cross-legged, both knees should rest on the floor, though sometimes it takes a bit of time to be able to get the legs to drop that far. After a while the muscles will loosen up and the knees will begin to drop. To help that happen, sit on the front third on the cushion and adjust the height, shifting your body forward a little bit. The three points: the base of your spine (rear end) and both knees should touch the mat for stability. By imagining the top of your head pushing upward to the ceiling and by stretching your body that way, get your spine straight-then just let the muscles go soft and relax. With the buttocks up on the cushion and your abdomen naturally pushing out a little, there will be a slight curve in the lower region of the back. In this position, it takes very little effort to keep the body upright.
Face, Mouth, and Nose
Once you've positioned yourself, there are a few other things you can check on. The mouth is kept closed. If possible, breathe through your nose. The tongue is pressed lightly against the upper palate. This reduces the need to salivate and swallow. The eyes are kept lower, with your gaze resting on the ground about 70 to 100 cm in front of you. Your eyes will mostly covered by your eyelids, which eliminates the necessity to blink repeatedly. The chin is slightly tucked in, so that your though the position during sitting meditation looks very disciplined head is tilted down at a 45 degree angle. Although the position during sitting meditation looks very disciplined, the muscles should be soft. There should be no tension in the body. It doesn't take strength to keep the body straight. The nose is centered in line with the navel, the upper torso leaning neither forward or back.
Hands
The hands are folded in the maha . The dominant hand is held palm up holding the other hand, also the palms up, so that the knuckles of both hands overlap. The thumbs are lightly touching, thus the hands form an ova, which can rest on the upturned soles of your feet if you're sitting full lotus. If you're sitting Burmese, the maha can rest on your thighs. The center of the cosmos maha should be exactly in the place of your energetic center-danjeon (Kor.), hara (Jap) or tantien (Chi). The position of the hands helps turn your attention inward
Breathing
Pay attention to your breath is the basic foundation for meditation. Our breath is always with us, anytime, anywhere. The word "spirit" means breath. By breathing correctly, you can access "gong-ki"(Kor.)-air energy. How you breath breathe affects your you body and mind: when your mind is agitated, your breath is agitated, when your is agitated; when you're nervous, you breath quickly and shallowly; when your mind is at rest, the breath is deep, easy, and effortless.
During mediation, we encourage you to inhale and exhale through the nose and generally exhale twice as long as inhale,e.g. 3 seconds in, 6 seconds out, 5 seconds in, 10 seconds out. Breathing should be done naturally, not forced or with concentration. During sitting, it is also important to breath quietly, without making noise as it can distract others. Most important is to let breath become relaxed and naturally at ease.
Center
It is important to bring your attention to your center-danjeon (Kor.) tantien (Chi.) hara (Jap.). Your center is located two inches below the naval at the central axis of your body, and is the exact middle point if measured from the top of your head to the bottom of your feet. It's the physical and spiritual energy center of the body. Put your attention there during your practice. As you practice sitting meditation more, you'll become more aware of your center as it becomes stronger. In Zen we say, "This is your don't know center ", the center of our just do it or willpower center.
Discomfort and changing positions
Once in a particular sitting position,you should stay that way until you feel the need to change positions. During a sitting period, if physical pain or drowsiness becomes a distraction, you may stand up for relief. First, do a sitting bow, then quietly stand up, remaining in standing meditation until the discomfort passes. When you are ready, do a standing bow and quietly sit down. Additionally, you may use the standing meditation posture as a transition between different sitting positions. For example, if you experience a lot of pain sitting cross-legged and need to change positions, do a sitting bow, stand up quietly, bow, and then sit down in a kneeling position.
Mind
What you do with your mind is the most important part of meditation. Zen means understanding your true self-what
am I? In order to do that, meditation techniques help us to become clear in the present moment. Below are some simple basic techniques that can start you off with a meditation practice at home. For detailed instructions, please visit one of our Zen centers for an orientation.
Technique 1: Clear mind, clear mind, don't know
This exercise is usually suggested for beginners. When you inhale, repeat quietly inside your mind, "clear mind, clear mind, and as you exhale, say, "I don't know ". Your exhalation with "don't know" should be drawn out about twice as long as your inhalation. It may be unfamiliar at first but if you gently pay attention to each breath and be aware of the words repeated , the exhalation will slowly become longer and more relaxed. If thinking or emotions appear, that's not a problem, just return to your breath and the simple exercise. This technique brings together body, breath and mind in one place, in the present moment. When the words are clear, and you are aware of your breath and can feel your body, then your mind is clear. You can try this method of 10 minutes each time during the sitting and if comfortable, extend to 20 or 30 minutes.
Technique 2: Counting the breath
This practice, often recommended for beginners, brings attention to each breath and helps to still and focus the mind. The count may be done on either the inhalation or exhalation. The count is done either up to three or up to ten and then repeated for the duration of the sitting period. If the count is lost, then the practitioner returns to one and starts again.
Technique 3: Mantra practice
Using a mantra to calm the mind and strengthen the center is another technique used by Zen practitioners. A mantra is a tool to keep our mind clear, while sitting or doing our everyday moment to moment activities. A common mantra to use is repeating "Kwanseum Bosal" (Kor for Bodhisattva of Compassion), the Buddhist name for the emantra of our own compassionate heart. This used technique is to recite the mantra quietly to oneself, repeating it constantly, paying attention to it and allowing all other thinking thinking to drop away. This takes some practice since it is very easy to let one part of the brain "chant" the mantra while the other part is thinking about dinner or going to the movies. When this happens, gently bring the mind back to the mantra without any judgment. When doing mantra practice, it is important to make your direction clear. When the mantra is not clear or there is a lot of thinking, simply ask, "who is repeating this mantra?" This will help bring you back to the present moment and become clear. During sitting, when your mantra is clear, your breath is even and natural, you are aware of your body and you see the floor clearly in front of you, then your mind is clear. For doing mantra practice, we recommend you consult your guiding teacher.
0 notes
Text
LIFE IS HARD TO FIND LOVE

The best life coach helping individuals to experience phenomenal healing to break all the chains ceasing to find the true love of their life.
Know more: https://lightangelic.com/life-is-hard-to-find-love/
0 notes
Text
The Best rTMS Treatment for Post-Traumatic Stress Disorder and Obsessive-Compulsive Disorder.
At FeelLightRTMS, we specialize in innovative treatments for mental health conditions such as Post-Traumatic Stress Disorder and Obsessive-Compulsive Disorder. Our advanced rTMS therapy offers a non-invasive and effective solution for those struggling with these challenging disorders. By targeting specific areas of the brain, we help reduce symptoms and improve overall quality of life. Discover how FeelLightRTMS can help you or your loved ones find relief from Post-Traumatic Stress Disorder and Obsessive-Compulsive Disorder. Contact us today to learn more about our personalized treatment plans.
0 notes
Text
My poor, sensitive nervous system... 😭
Gotta make sure to get plenty of rest!
#sensory issues#sensory overload#autism#autism spectrum disorder#autistic#actually autistic#autistic experiences#neurospicy#autism memes#autistic culture#autistic things#neurodivergent memes#autistic memes#memes#autism awareness#autism things#autism experiences#post traumatic stress disorder#actually traumatized#trauma#trauma survivor#fight or flight#nervous system#adrenaline#autistic burnout#autistic community#mentally tired#tired#tism posting#its the tism
3K notes
·
View notes
Text
What is the Primary Difference Between Acute Stress Disorder and Post-Traumatic Stress Disorder?
Understanding the differences between Acute Stress Disorder (ASD) and Post-Traumatic Stress Disorder (PTSD) is crucial for having a basic understanding of the impact of stress on mental health.
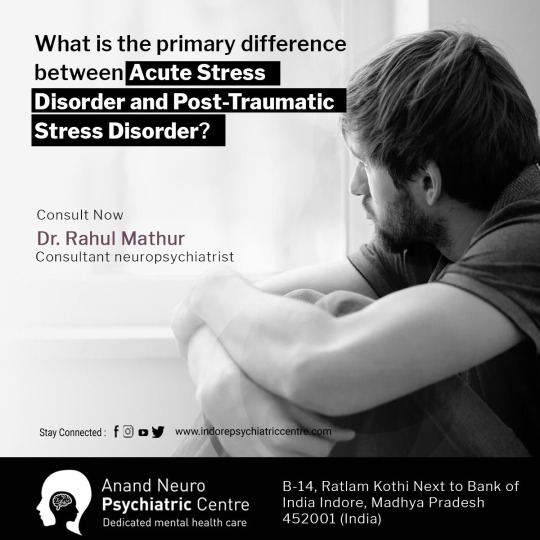
Time Frame:
Acute Stress Disorder: This occurs shortly after a traumatic event, typically within three days to a month.
Post-Traumatic Stress Disorder: PTSD develops if the symptoms persist for more than a month, lingering beyond the initial shock.
Symptom Duration:
Acute Stress Disorder: Symptoms last for a minimum of three days but can extend up to a month.
Post-Traumatic Stress Disorder: For PTSD, symptoms endure for at least a month, affecting daily life and functioning.
Intensity of Reactions:
Acute Stress Disorder: Initial reactions to trauma are intense but may subside as time passes.
Post-Traumatic Stress Disorder: Symptoms are persistent and may intensify over time, significantly impacting daily activities and relationships.
Read More: and Contact on 8818812800
#What is the Primary Difference Between Acute Stress Disorder and Post-Traumatic Stress Disorder?#Acute Stress Disorder#Stress Disorder#Post-Traumatic Stress Disorder#What are the Signs of Post-Traumatic Stress Disorder#Signs of Post-Traumatic Stress Disorder#ptsd#Symptoms of Post Traumatic Stress Disorder#Symptoms of ptsd#Causes of Post Traumatic Stress Disorder#Causes of PTSD#Treatment Post Traumatic Stress Disorder (PTSD)#Treatment Post Traumatic Stress Disorder#Treatment of PTSD#What are the 5 symptoms of PTSD?#What are the 7 symptoms of PTSD?#Can a person with PTSD live a normal life?#क्या PTSD वाला व्यक्ति सामान्य जीवन जी सकता है?#Post-traumatic Stress Disorder in Children#what are the 17 symptoms of ptsd?#post traumatic stress disorder dsm-5#post traumatic stress disorder icd-10#long-term effects of ptsd#ptsd symptoms in women#acute stress disorder#causes of ptsd#acute stress disorder symptoms#acute stress disorder dsm-5#acute stress disorder treatment#acute stress disorder vs ptsd
1 note
·
View note