#or like. childhood abuse is a significant risk factor
Explore tagged Tumblr posts
Text
Oppositional defiant disorder I hate you forever
#it shouldn’t exist! it’s a bad disorder and we should stop diagnosing it!#ooooh I get so mad#I’m writing a paper about it and I have had to put all of research away and fully stop thinking about it multiple times bc I’ll read some#crazy shit that pisses me off.#these papers will be like there’s a significant decrease in oppositional behaviors when treated with adhd meds#or like. childhood abuse is a significant risk factor#like no! maybe it’s just like. adhd (which causes irritability!!) or a fucking traumatized kid who doesn’t have right control over their#emotions. like there is no reason for this disorder to exist#I read in something that close to 60% of children diagnosed with adhd meet requirements for odd like maybe it’s fucking. the same thing#causing these issues. have we considered that maybe the disorder known for causing executive dysfunction is like. possibly causing this#executive dysfunction. have we considered this. anyone. has anyone had the thought.#like I understand not everyone with adhd experiences this. however. it’s certainly enough of a correlation that it’s like. bro wtf.#if it needs to be diagnosed it makes much more sense as a signifier on an adhd diagnosis so at least the kid can get access to#accommodations or meds if they need them. instead of being essentially labeled bad kid for life#bc even trying to talk to a doctor to get it off your record is literally taken as proof you have it which is so fucked. god I’m so mad#prsnl
3 notes
·
View notes
Text
Adrien Agreste and Borderline Personality Disorder
DISCLAIMER: I've been a bit low on spoons this week, so I haven't gathered as much evidence as I probably could have. Also, I am but a humble student in clinical psychology. This is mainly a thought compilation for @moonieratty!
To introduce the topic, without going into it too much, personality is described by features and behavioral patterns, or traits, consistent across situations and across time. Personality disorders are therefore enduring patterns of highly maladaptive traits evaluated in personal and sociocultural context (Dozois, 2019, p. 290).
Like other disorders, personality disorders have diagnostic criteria. The DSM is used primarily for diagnosis in the US and Canada while the ICD is used more widely in Europe and other places. I'm more familiar with the DSM, but I've included a brief section on the ICD to be comprehensive. It ended up a bit longer than anticipated, so let's go below the cut. Warning for discussions of abuse, self harm, and suicide, and a brief mention of substance use.
Overview of Borderline Personality Disorder
BPD is prevalent in a small percentage of the population, about 1-2% by varying estimates, and is characterized by instability across domains of emotions, identity, interpersonal relationships, and behavior. Its onset is usually in late adolescence or early adulthood and symptoms may diminish with age, after one's thirties or forties, especially with therapeutic intervention. Along with ASPD, it has been the focus of a lot of clinical research; it is unfortunately associated with high rates of non-suicidal self-injury and suicide (APA, 2022, pp. 754–755; Dozois, 2019, pp. 308–309).
Etiological factors for BPD include both biological and environmental disturbances. Of note to our discussion is the heightened risk for BPD in cases of child abuse or neglect, as well as growing up with another family member with a serious mental health condition (NHS, 2022). It's been well established that Gabriel is emotionally neglectful if not outright abusive toward Adrien in multiple ways, so this is a clear risk factor. In addition, although I won't argue definitively for Gabriel having a psychological condition, he did keep Emilie's body in the basement, so there is clearly some kind of disturbance going on.
From a cognitive-behavioral perspective, Linehan argues that BPD stems from families who consistently invalidate childhood emotional experiences and "oversimplify the ease with which life's problems can be solved," which may cause children to learn to seek attention and communicate with others through emotional outbursts (Dozois, 2019, p. 297). This rings true for Adrien and Gabriel as well.
I have to apologize for my son, Ladybug, he's like his mother. Way too overly dramatic. (Jackady)
It doesn't seem like this is the first time Gabriel has thought this, and labeling an emotional reaction as being overly dramatic is very much invalidation of it. As for emotional outbursts, Adrien has had quite a few, mostly as Chat Noir. More on this later.
To round out this first section, attachment theory proposes a connection between poor parent-child attachments and BPD relationship difficulties. Specifically, maladaptive behavior in relationships may stem from childhood development of an anxious-ambivalent attachment style, where intense fears of abandonment interfere with a strong desire for intimacy (Dozois, 2019, p. 310). You can clearly see this in Chat Noir's relationship with Ladybug, and I'm sure other people have discussed Adrien's attachment style more in depth, but suffice to say I think this is an apt description.
Argument from DSM-5-TR
In the DSM, personality disorders are primarily diagnosed on a categorical model. There are a few general criteria which I won't be going into, but I will highlight that personality disorders are stable and pervasive, and would be diagnosed only if they were leading to significant distress or dysfunction. Adrien's mental state is not great, so the latter shouldn't be a problem, but this show does not always pay attention to consistency, so I'm going to be speculating some. Everything in this section is cited to the relevant DSM entry unless otherwise stated.
The DSM characterizes BPD with instability in relationships, self image, and affects, as well as marked impulsivity. It has no exclusion criteria, so BPD can be and frequently is comorbid with other disorders like mood disorders, PTSD, and ADHD. Of the below criteria, five need to be met in order for a diagnosis to be made.
Frantic efforts to avoid real or imagined abandonment
Hey, where're you going? . . . So you're allowed to know her true identity, but I'm not? (Syren)
You're not really replacing me with a turtle, are you? (Anansi)
A lot of people have delved into Adrien's abandonment issues, which feature most prominently in his relationship with Ladybug. His fears of being replaced result in him seeking reassurance from Ladybug, and he can lash out if he does not receive the response he hopes for. Ladybug is his world, and he wants to be hers, so anything infringing on that feels to him like a threat of being abandoned, and he does not like it very much.
Impulsive behaviors like giving up his ring can be interpreted under this lens: he can avoid abandonment by doing the abandoning first. Then it will be him leaving, and not the other way around.
I also interpret Adrien's nightmare (Le Marchand de Sable) as being a fear of being alone as much as it is a fear of being trapped.
Unstable and intense interpersonal relationships alternating between extremes of idealization and devaluation
We'll be united, more powerful and free. We'll defeat Hawk Moth, then we can both run away to an island! Far away from everything. We will live off nothing but fruits, and we will have a little pet hamster and we will name it— (Le Patineur)
I just can't do this anymore. I give up… on everything. Even you . . . If I become Chat Noir again, Ladybug will just end up rejecting me, over and over. (Kuro Neko)
Even though Adrien mostly keeps his head on straight regarding what he's owed and not owed by other people, his relationship with Ladybug is full of highs and lows. He thinks Ladybug is the most amazing girl, but this can recoil quickly into feeling as though Ladybug doesn't care about him enough or isn't meeting his needs.
Furthermore, he developed this idealization of Ladybug as a potential lover or caregiver at one of their first meetings (Cœur de Pierre), and continually sought to spend time together and share the intimate details of their secret identities early on. These are all common to individuals with BPD, as is the switch from idealization to feeling as if the other person "does not care enough, does not give enough, or is not 'there' enough." Ladybug is the only person Adrien consistently projects this instability and intensity on, which might be something interesting to explore.
Identity disturbance: unstable self image or sense of self
When I was a kid, I always wanted to be what my parents wanted me to be! (Exauceur)
But, does that mean Chat Noir is who I really am? Deep down inside? (Kuro Neko)
With all the secret identities, it isn't surprising that Adrien fits this criterion, but canon even explicitly draws a link between Adrien's unstable sense of self and his childhood experiences. He doesn't know who he is, and he distracts from this by being Chat Noir, only to struggle even more when he feels useless and underlooked as his hero self. His behavior shifts dramatically between trying to prove himself with grand gestures and refusing to participate or lashing out. There is definitely something to discuss on this front.
Impulsivity in at least two potentially self-damaging areas
Giving you some extra time . . . I trust you to bring me back, m'lady. (Gamer 2.0)
There are only two liars left in Paris and one of them knows the ultimate way to catch her attention . . . Crazy about you, m'lady. (Mensonge)
This is walking a thin line between impulsivity and suicidal behavior, which would be excluded from this criterion, but I'll list self sacrifice here because I can see an argument for Chat Noir's impulsive behaviors being out of love or the desire to be useful. There may still be some self injurious intent or euphoria, but Chat Noir does have faith in Ladybug to bring him back eventually. Nevertheless, this is impulsive and unhealthy. Chat Noir jumps too quickly to this option to have thought it through.
I can't think of another area, because Adrien isn't old enough for reckless driving, spending, substance use, or sex. This is also a kids' show. Just presenting these options for fanfiction writers out there.
Recurrent suicidal or self mutilating behavior, gestures, or threats
I... I don't know what to do! (Chat Blanc)
This is all our fault . . . Cataclysm. (Culpabysse)
By itself, what happened in Chat Blanc would not be solid evidence, as that was an unprecedentedly traumatic situation. Combined with Culpabysse, though, there is a strong case to be made for at least passive suicidality for this to be able to come up as an option.
You could also interpret the self sacrifice in this category. Suicidal behavior in individuals with BPD is often preempted by fears of rejection or abandonment, so an interesting analysis could be made on this front.
Affective instability due to marked reactivity of mood
He's still only thinking of himself! I just want this terrible day to be over and done with! I hate Christmas! (Pire Noël)
Sorry! Sorry! I didn't mean to make you so mad. I get it. You're sick of me . . . No one can help me, Kagami. (Glaciator 2)
Adrien's prolonged episodes of anger and despair reflect a high reactivity to emotional stressors, especially interpersonal ones. In general, he just doesn't feel very well unless something is actively bringing him joy. Most of his outbursts are brief, though, and I will discuss them as part of a later criterion.
Chronic feelings of emptiness
I'm not Adrien, so I wouldn't know if this is the case, but I can say he has experienced at least one depressive episode (Kuro Neko) and emptiness would not be unfamiliar. You can look at him and decide.
Inappropriate, intense anger or difficulty controlling anger
How was your amazing evening with your "friends"? . . . What do you think? (Glaciator)
Why not? No one'll know if I quit. No one'll care! (Syren)
A two-person plan?! There's only one two-person plan, and that's Ladybug and me! (Sentibulleur)
Give me a break, Miss "I can't even come up with a superhero name"! (Hack-San)
Anger in individuals with BPD can manifest as bitterness, sarcasm, or recurrent verbal outbursts, which Chat Noir absolutely exemplifies. These outbursts are often followed by feelings of shame or guilt and contribute to a feeling of being bad. Chat Noir apologizes after being harsh in Glaciator, and I wouldn't be surprised if he felt badly about the other times. Again, these outbursts are often precipitated by interpersonal fears and perceived threats of abandonment. Unlike other symptoms, this specific one tends to be unique to BPD.
Transient, stress-related paranoid ideation or severe dissociation
I cannot recall any evidence for this but headcanon away, my friends.
All in all, I think Adrien has a strong case for BPD presentation according to the DSM. Canon is not always consistent, but I think it presents an interesting and mostly coherent narrative for this lens. From this perspective, Adrien's behavior reflects a deep intolerance of being alone and a dependence on other people to define the self.
As a corollary, BPD behavioral patterns are frequently linked to self sabotage and self undermining right when a goal is about to be realized, which could manifest as dropping out of school right before graduating or ending a relationship when it seems to be going well. Food for thought. Individuals with BPD may also feel more secure with transitional objects like pets than with interpersonal relationships, which could reflect in Adrien's relationship with Plagg.
To add some subjective understanding to this clinical mumbo jumbo, I've added a source of genuine BPD experiences below (Mind, 2022).
Argument from ICD-11
With the release of the ICD-11, a dimensional model for diagnosis of personality disorders became the new standard. What this means is that individuals are no longer labeled as having 'histrionic' or 'dependent' or, indeed, 'borderline' personality disorders, but are rather assessed as having any form of personality disorder on a sliding scale of severity and with trait domain specifiers (Swales, 2022). To put it more simply, people are diagnosed only with a general personality disorder or personality difficulty which can be optionally specified as deviating on one of the personality traits in the Big Five model, which is well established in personality psychology.
This move has several benefits. Stigmatization related to particular personality disorders can be reduced, and differential diagnosis and comorbidity between personality disorders becomes irrelevant. However, people retain access to treatment and support. Evidence-based treatments like dialectical behavior therapy are particularly well established and crucial for BPD; for this pragmatic purpose, the ICD contains one additional specifier for borderline pattern personality disorder (Bach et al., 2022; Swales, 2022).
The DSM and ICD are designed to be compatible with each other in many ways, and in this case, the borderline specifier in the ICD is directly lifted from the criterion of the DSM (WHO, 2023, 6D11.5). Based on our previous discussion, Adrien would be equally qualified for a diagnosis in France. I would likely describe his personality disorder with moderate severity, where multiple areas of functioning are affected and self harming behaviors may be present, but not all areas or relationships may be equally impacted and traits are not as rigid and inflexible (WHO, 2023, 6D10.0–6D10.2).
Interestingly, the ICD includes three additional manifestations of borderline pattern which are optional and may vary across time (WHO, 2023, 6D11.5).
A view of the self as inadequate, bad, guilty, disgusting, and contemptible
An experience of the self as profoundly different and isolated from other people; a painful sense of alienation and pervasive loneliness
Proneness to rejection hypersensitivity; problems in establishing and maintaining appropriate levels of trust in relationships; frequent misinterpretation of social signals
I'm fascinated by the number of adjectives in here. I simplified very slightly, as I did with the DSM criteria, but I had to keep all these adjectives. Anyway, I won't elaborate for too many more paragraphs, so let's say sentimonster moment and leave it at that. I will spare you my mirrored Félix essay. For now.
Qualifications and Limitations
First of all, Adrien is a teenager. The distinguishing factor between a personality disorder and regular adolescent difficulties would be longevity and identity concerns beyond his developmental phase (APA, 2022, p. 758). Second of all, Adrien has a uniquely terrible home life and magical problems. Some of his behaviors could be normal considering his experiences and sociocultural context, and this matters when it comes to psychological evaluation. Take everything with a grain of salt!
More generally, the categorical model of the DSM has several issues, not to mention diagnostic issues related to culture, gender, and stigma. Some but not all of these issues are addressed by the dimensional model it includes in a later section, which shares theoretical foundations with the model of personality disorders in the ICD. Even so, issues remain. Diagnosis, access to treatment, and political statements are intrinsically linked in complex ways. I won't get into all of the nuances, but be safe, remember this is a fictional character, and keep an open mind.
REFERENCES:
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). https://doi.org/10.1176/appi.books.9780890425787
Bach, B., Kramer, U., Doering, S., di Giacomo, E., Hutsebaut, J., Kaera, A., De Panfilis, C., Schmahl, C., Swales, M., Taubner, S., & Renneberg, B. (2022). The ICD-11 classification of personality disorders: A European perspective on challenges and opportunities. Borderline Personality Disorder and Emotion Dysregulation, 9(1). https://doi.org/10.1186/s40479-022-00182-0
Dozois, D. J. A. (2019). Abnormal psychology: Perspectives (6th ed.). Pearson.
Mind. (2022, September). What does BPD feel like? https://www.mind.org.uk/information-support/types-of-mental-health-problems/borderline-personality-disorder-bpd/experiences-of-bpd/
National Health Service. (2022, November 4). Causes - Borderline personality disorder. https://www.nhs.uk/mental-health/conditions/borderline-personality-disorder/causes/
Swales, M. A. (2022). Personality disorder diagnoses in ICD-11: Transforming conceptualisations and practice. Clinical Psychology in Europe, 4(Special Issue). https://doi.org/10.32872/cpe.9635
World Health Organization. (2023). International statistical classification of diseases and related health problems (11th ed.). https://icd.who.int/
#miraculous ladybug#adrien agreste#ml meta#don't worry i read through far more sources than listed here#it's just standard citation procedure to include only in-text references and not readings for general subject comprehension#🌃#🌖#i'm using a hybrid parenthetical citation model which i think is most efficient and informative so just note this down#i can't believe i referenced kuro neko three times... what an episode#ml simon says#ml syren#ml anansi#ml sandboy#ml frozer#ml kuro neko#ml stoneheart#ml wishmaker#ml gamer 2.0#ml lies#ml chat blanc#ml guiltrip#ml santa claws#ml glaciator 2#ml glaciator#ml sentibubbler#ml hack san
108 notes
·
View notes
Text
But aspd-culture, what "causes" ASPD?
Well, that's hard to say as it is commonly a mix of nature and nurture, and we can't say for sure "this set of things will cause ASPD". I can, however, explain some serious risk factors that, if you relate to them and have this disorder, may have been a part of why you developed it.
TW for heavy topics, as you might have guessed.
Just a heads up that, if you have the disorder, this one is gonna be a rough read. A lot of things that you were told throughout your childhood should be "normal" and maybe that you even thought were helping you are gonna pop up here as things that heavily increase the chances of ASPD, and we're not just talking about abuse and neglect, though of course that is the first one I'm gonna get into because it's the most obvious and well-known risk factor. Do expect some other information you might not have been ready to hear, though.
So the first one, as I said, is maltreatment as a child. This can include many kinds of abuse, including verbal, emotional, physical, sexual, etc. There are some reasons to believe that sexual abuse in particular, especially long-term sexual abuse, significantly increases the chance of developing ASPD.
The next is neglect, which also comes with a significant risk of developing ASPD, especially if the neglect is related to both the emotional and physical needs of a child. If the child experiences neglect in regards to needs such as food, hygiene, shelter, medical care, etc, but does not experience emotional neglect, the risk of developing ASPD appears to be somewhat less than if the child experiences both.
Maltreatment and neglect before the age of 18 months is especially significant when it comes to risk of developing ASPD. Not greeting an infant, not properly showing emotion and "appropriate affect" to an infant, and in particular a lack of attachment from their mother (either due to her literally being absent or just emotionally absent and disconnected) during the first 18 months of life are less commonly thought of forms of neglect that seriously affect secure attachment and increase the risk of ASPD.
The third and last of the "expected" answers to this question is witnessing intimate partner violence during childhood, especially regularly or across multiple partners. This shows the child two things: one is a fear of the aggressor as well a need to tiptoe around someone who should be a secure caregiver to avoid danger, and the second is a disbelief that the victim of the violence is able to protect them from danger, either because they appear weak (children are supposed to believe until a surprising age that their parents are superhero levels of strong and unable to be intimidated or weakened) in the eyes of the child, or because the child does not want to bother them with their issues when they already have their own abuse to deal with. This is especially true in cases where the child successfully controls the violence where the adult cannot (think those kids who use themselves as human shields because the abuser doesn't dare touch the child for various reasons), as it makes them feel they are responsible for protecting both themself and their caregiver, which disrupts normal attachment.
Here's where we get to the less obvious, more specific stuff that can lead to ASPD. There are multiple studies showing that an excess of television (I know, but hear me out bc this isn't about violence on tv), specifically when it is being used as a stand-in parent, significantly increases risk of developing ASPD even when other factors are controlled. As someone with ASPD, I can 100% see how this is valid. I used television to try and understand what normal people were like, and in turn, I experience a weird type of affective "empathy" when shown emotions in the over-acted way that they do on sitcoms, even though I do not experience that empathy when shown normally expressed emotions either on tv or in real life.
It also makes sense to me because generally when TV becomes a stand-in parent, the child is watching other children be cared for in ways that they are not in real life. The child may then be led to believe (as I was) that caring about other people is something made up for TV, since that's the only time they see it. Once the brain develops the understanding of fantasy vs reality, if TV is the only time that a child sees secure attachment styles, loving and attentive caregivers, etc, the brain may falsely place that in the fantasy category. That can lead to the thought processes and attachment issues that are typical of pwASPD, including feeling as though only they can be trusted to look out for themselves, that irl relationships are supposed to be transactional vs emotional, etc. So if you, like I did, attempted to watch sitcoms and such like Full House, Boy Meets World, etc. as a way of understanding what a normal family is supposed to be like or to understand how people are supposed to interact with each other, it is very possible that that was a contributing factor to the development of your ASPD.
Another somewhat surprising one: show of hands on how many pwASPD grew up hearing "it's just a joke", "you have no sense of humor", and "lighten up, we're just teasing you" - either from other kids, caregivers, or both?
Teasing is believed to be another major factor in developing ASPD. Teasing can cause a child to feel insecure, unsafe, and attacked when coming from people the child does not have a secure attachment to, and can decrease chances of the child developing that secure attachment later. This is especially true if the teasing came from caregivers, and of course has a higher chance of affecting the child if they attempt to set boundaries around it and aren't respected in that. This leads to the child feeling attacked by the people they are supposed to go to for comfort, and the more people who tease the child, the more likely the child is to feel unsafe around people as a whole - leading to the mindset that all people are dangerous and that the only person the child can trust is themselves. This teasing also causes self-imposed isolation as a way of feeling secure, which reinforces again that people are inherently unsafe and the only person the child can trust is themself. So if you tried to communicate your distress, discomfort, etc. about being teased and were dismissed, especially by your caregivers, then that significantly increased the chance that you would go on to develop ASPD.
One that is currently debated as to if it is a factor or not is the presence of an overprotective mother, specifically if that over-protectiveness became a point of contention between you two as you became more independent. It's surprising because a major characteristic of children who develop ASPD is independence, and most hold the belief that only they will protect them, but the reasoning is sound imo. The reason for this one, from those who believe it is associated with ASPD, is that when a child goes through the normal process of asserting independence, if they are met with either fear tactics as a form of control or heavy anxiety from their maternal figure, the child learns to be insecure, anxious, and obsessive about protecting themselves because they are being taught that the world is not safe/that they are not capable enough to explore that world. This can lead to an overblown expectation of the danger in the real world and leads to anxiety and distress around outside people. This anxiety and nervousness about the world can lead to the child seeing everyone and everything else as a threat, a mindset that is commonly associated with ASPD. If that anxiety is later disproven (as it inevitably will be unless the child experiences significant trauma - itself a risk factor for ASPD), this causes a rift in the attachment to the caregivers in question, and can make the child distrust their judgement and ability to assess risk, which again affects how safe the child feels with them. This is especially true if the connection to their caregivers is weakened by inconsistency, abuse, neglect, or other factors.
Any inconsistent behavior from caregivers, in fact, is another risk factor for developing ASPD. Children need to be able rely on consistency and routine to feel secure and develop normally. If they are constantly uncertain of how safe they may be with one or both caregivers, they are more likely to learn the idea that the only person they can rely on is themself.
Note that all of this is based on the current scientific understanding of ASPD's development, which deals significantly in both stigmatized and entirely false beliefs about the disorder. However, I focused here on points that made sense to me as someone with it, and did my best to explain how these contribute to ASPD through that lens in addition to the potentially biased medical lens. Our understanding of psychology in general is always changing, but these are some risk factors that are commonly believed at the time of writing to increase the chances of developing ASPD.
Also worth noting is that all of these factors do not need to be present to have ASPD develop. These factors significantly increase the risk of developing ASPD, especially when combined with a genetic component, but I am in no way claiming that you have to have all or even any of these to have ASPD.
I hope this helped you understand this disorder and the people with it a bit better. If you know someone with ASPD, maybe this can help you process why they hold the beliefs they do, and if you have ASPD and feel comfortable, feel free to show or explain some of this to your friends if you think it may help them understand where you're coming from a bit more.
A lot of the stigma, I think, comes from the fact that people don't get what we went through that led our brain to believe our antisocial traits were the best way to protect ourselves. For some, a little more light shed on that subject may be all they need to be more compassionate about it. And if you went into this with a negative outlook on pwASPD, I understand. It's easy in the world we're in to end up with that thought process. I appreciate you reading this far and ask you to read just a bit further to the end.
Try if you can to imagine what it's like to be a kid who has been through more than most adults have in their entire life and gotten so little help that that little child believes no one in the world protects anybody else. Imagine what kind of a world we were picturing growing up in because at the time, that was all we had ever seen. It would be horrifying, right? Even worse than the already pretty sucky world we currently live in. Imagine being a child and thinking that every other kid is going through the same stuff you are at home and handling it so much better. And for some, imagine knowing that some don't or that they get help, but not knowing why your life is different. Would you want to live in that world? Would you be able to keep the innocent, childlike wonder? Would you not be angry and hurt and confused as to why you didn't deserve the help and the life other kids get? Many of us lived thinking that from painfully early ages.
Is it so far-fetched for us to think we needed to protect ourselves if everyone was like the sample size of people we had met? Is it so shocking, then, that our subconscious thought that the traits we have now would be the only way to keep us safe? Is it really that surprising that a child so rarely, if ever shown kindness and empathy, might grow up not knowing how to replicate that for other people?
Most of us looked down the barrel of a proverbial (for some of us, literal) g*n as a toddler to young child, so we put on a vest. How were we supposed to know that other children had never felt that unsafe? How were we supposed to know that someone was supposed to help us when they never did?
Just food for thought. Thanks for reading.
#this may be full of comma splices#because my phone keeps telling me to add commas everywhere#with its new grammar correct feature#so sorry about that#infodump#aspd-culture-is#aspd culture is#aspd culture#tw trauma#cw trauma#actually antisocial#actually aspd#antisocial personality disorder#aspd#aspd awareness#aspd traits#cluster b pd#actually cluster b#cluster b
125 notes
·
View notes
Text

Why religious belief provides a real buffer against suicide risk (David H Rosmarin, Psyche, Aug 07 2023)
"When John came to McLean Hospital for treatment, most of our team was convinced he would kill himself.
As a middle-aged white man with severe and chronic depression, significant physical pain, easy access to firearms, a long history of substance misuse, and childhood sexual abuse, he checked almost every box on the list of risk factors for suicide.
Furthermore, John (my patients’ names and details have been changed to protect privacy) reported passive suicidal ideation – fleeting thoughts that he would be better off dead than alive.
However, John did not attempt suicide during or after his care. He never developed a plan to end his life.
Despite his mood struggles and incredible physical discomfort, he remained staunchly committed to living for as long as possible.
When I asked John why he wasn’t more suicidal, he answered simply: ‘I could never do that, because I believe in God.’ (…)
First, the best-known predictor of suicide is hopelessness.
When people lose hope in a brighter future, they are more prone to taking their lives.
Spirituality can help prevent suicidal behaviour by promoting faith and hope.
Several years ago, my colleagues and I identified that acute psychiatric patients with depression were significantly more likely to benefit from cognitive and dialectical behaviour therapy if they believed in God.
More centrally, we found that belief in God predicted greater belief in treatment and hope that one would eventually get better.
Faith in God facilitates the belief that things can improve, even when people are at a low point in life.
Another key predictor of suicide is impulsivity.
A surprisingly high number of suicide attempts occur suddenly: one study found that more than 40 per cent of attempts had manifested within 10 minutes of someone deciding to take their life.
Religion can help prevent suicide by promoting self-control, since religious beliefs and values tend to create a buffer against prepotent or spontaneous thoughts and urges. (…)
My favourite explanation for how spirituality and religion may protect against suicide originates from the work of Viktor Frankl – the Austrian psychiatrist who survived the Nazi concentration camps, and observed that having a sense of meaning and purpose is a key predictor of human wellbeing.
When my patients perceive their anxiety, depression or other problems as being potentially constructive in their lives – when they view their struggles as an opportunity to grow in terms of self-awareness, connection with others, or resilience – they rarely (if ever) display significant suicidality.
While this philosophical perspective is technically agnostic, in practice it often dovetails with and even emanates from spiritual and religious teachings."
18 notes
·
View notes
Link
#Adolescents#Alcohol#Anxiety#CelebratingYourGiftofLife#Childhood#Depression#JamesDonaldson#JamesDonaldsonnotes:Welcometothe“nextchapter”ofmylife…beingavoiceandanadvocateformentalhealthawarenessandsuicideprevention#JamesDonaldsonMentalHealth#JamesDonaldsononMentalHealth#Men#MentalChallenges#MentalHealth#MentalHealthConditions#MentalHealthCrisis#MentalHealthDisorders#MentalHealthIssues#MentalHealthServices#MentalHealthStigma#MentalIllness#MentalIssues#Stigma#SubstanceAbuseDisorders#SubstanceUse#SubstanceUseDisorder#Suicide#SuicideRates#Trauma#WHO#woman
0 notes
Text
Understanding the Link Between Mental Health and Addiction
The relationship between mental health and addiction is complex and deeply interconnected. Many individuals struggling with substance use disorders also face mental health challenges, and vice versa. This dual condition, known as co-occurring disorders or dual diagnosis, requires a comprehensive approach to treatment. Understanding the link between mental health and addiction is crucial for effective recovery and long-term wellness.

How Mental Health Issues Contribute to Addiction
Mental health conditions such as depression, anxiety, bipolar disorder, and PTSD often increase the risk of developing an addiction. Many individuals turn to drugs or alcohol as a way to self-medicate, seeking temporary relief from emotional pain, stress, or trauma. While substances may provide short-term relief, they often exacerbate mental health symptoms over time, creating a vicious cycle of dependency.
Unresolved trauma is another significant factor in the link between mental health and addiction. Childhood abuse, neglect, or other traumatic experiences can leave lasting emotional scars, making individuals more susceptible to using substances as a coping mechanism.
How Addiction Affects Mental Health
Substance abuse can profoundly impact mental health, often leading to the development or worsening of mental health disorders. Chronic substance use alters brain chemistry, impairing mood regulation, decision-making, and stress response. Over time, this can result in anxiety, depression, or even psychosis, depending on the substance and duration of use.
Addiction also introduces stressors such as financial instability, damaged relationships, and legal troubles, all of which take a toll on mental well-being. The stigma and isolation associated with addiction further contribute to feelings of hopelessness and low self-worth.
The Importance of Dual Diagnosis Treatment
For individuals with co-occurring mental health and addiction issues, treating one condition without addressing the other often leads to relapse. Integrated dual diagnosis treatment is essential for addressing both conditions simultaneously. This approach ensures that individuals receive therapy, medication management, and support tailored to their unique needs.
Comprehensive dual diagnosis treatment often includes:
Therapy: Techniques like cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT) help individuals address underlying issues and develop healthier coping strategies.
Medication Management: When appropriate, medications can be used to manage mental health symptoms alongside addiction treatment.
Holistic Approaches: Practices like mindfulness, yoga, and art therapy can promote emotional healing and stress relief.
Support Groups: Peer support groups provide a sense of community and understanding, helping individuals navigate their recovery journey.
Breaking the Cycle of Stigma
The stigma surrounding both mental health and addiction often prevents individuals from seeking the help they need. Education and awareness are key to breaking this cycle. By fostering open conversations and promoting understanding, we can create an environment where individuals feel safe seeking treatment without fear of judgment.
Conclusion
The link between mental health and addiction underscores the importance of a holistic, integrated approach to recovery. By addressing both conditions simultaneously and with equal priority, individuals can achieve meaningful and lasting progress. Understanding and compassion from family, friends, and society play a critical role in supporting those facing these challenges. With the right treatment and support, recovery and mental wellness are achievable, leading to a brighter and more fulfilling future.
1 note
·
View note
Text
The Link Between Addiction and Mental Health in Men

Addiction and mental health are intricately connected, and understanding the ways in which they influence one another is crucial, especially when considering men’s health. Men often experience mental health challenges and substance use disorders in ways that are deeply intertwined, yet society has often overlooked the importance of addressing both aspects together. In this article, we will explore the link between addiction and mental health in men, considering risk factors, the impact of societal expectations, and how treatment strategies can help break the cycle of suffering.
Understanding Addiction and Mental Health in Men
At its core, addiction is a chronic condition marked by compulsive substance use, despite harmful consequences. It can manifest through various substances, such as alcohol, prescription drugs, or illicit substances like cocaine or heroin. Addiction often leads to a cycle where individuals feel compelled to use substances to cope with emotional distress, leading to more severe mental health issues.
Mental health, on the other hand, encompasses a person’s emotional, psychological, and social well-being. It affects how individuals think, feel, and act, and it determines how they cope with stress, relate to others, and make choices. Mental health conditions in men often include depression, anxiety, post-traumatic stress disorder (PTSD), bipolar disorder, and personality disorders. When mental health issues persist, they can increase vulnerability to developing substance use disorders, and vice versa.
Research consistently shows a strong connection between addiction and mental health in men. Substance use disorders can be both a cause and a consequence of mental health problems. In other words, a man struggling with mental health might use substances to self-medicate, and over time, the addiction worsens the underlying psychological issues. Alternatively, the physiological changes caused by addiction can exacerbate or even trigger mental health conditions.
The Intersection of Addiction and Mental Health in Men
1. The Role of Trauma
Trauma plays a significant role in the development of both addiction and mental health disorders in men. For many men, trauma often occurs in childhood or during significant life events, such as abuse, the loss of a loved one, or exposure to violence. Unresolved trauma can lead to a variety of mental health conditions, including depression, anxiety, and PTSD. The emotional pain associated with these conditions can feel unbearable, leading some men to turn to substances as a means of numbing or escaping.
For example, research suggests that men who experience childhood abuse are at a higher risk of developing substance use disorders later in life. Additionally, men who have served in combat or experienced other forms of violence often face PTSD, and self-medication with alcohol or drugs can become a coping mechanism. However, this only perpetuates the cycle of addiction, as the underlying trauma continues to affect mental health.
2. Societal Expectations and Masculinity
Society often places pressure on men to adhere to traditional notions of masculinity, which can impact their mental health. In many cultures, men are expected to be stoic, emotionally strong, and self-reliant. As a result, many men may struggle with expressing vulnerability or seeking help when facing mental health challenges. This societal expectation of toughness can prevent men from addressing their emotional struggles and seeking proper treatment.
Instead of openly discussing their feelings, many men may use substances to cope. This self-medication is sometimes seen as a way of asserting control or "toughening up" in the face of emotional distress. However, this societal pressure to conform to certain masculine ideals often leaves men isolated and unwilling to admit they need help. The stigma surrounding men’s mental health and addiction only reinforces these harmful behaviors, making it difficult for them to seek assistance.
3. The Biochemical Connection
Addiction and mental health disorders in men also share a biochemical connection. Mental health conditions such as depression, anxiety, and bipolar disorder often involve imbalances in brain chemicals, such as serotonin, dopamine, and norepinephrine. Similarly, addiction involves the brain’s reward system, which is regulated by dopamine. When a person repeatedly uses drugs or alcohol, the brain’s natural chemical processes are disrupted, leading to addiction.
For example, a man with depression might have low levels of serotonin, leading him to feel persistent sadness and lack of motivation. He may turn to alcohol or drugs to temporarily alleviate these feelings. However, the substance use can further deplete serotonin levels, exacerbating the depression. This biochemical loop is a common issue for many individuals, especially men who are trying to manage both addiction and mental health conditions.
4. The Impact of Co-Occurring Disorders
Co-occurring disorders, or dual diagnosis, refer to the simultaneous presence of both a substance use disorder and a mental health condition. In men, this dual diagnosis is more common than people might think, yet it is often underdiagnosed or misdiagnosed. Men with co-occurring disorders tend to experience more severe symptoms, including heightened risk of suicide, criminal behavior, and social isolation.
One of the challenges of treating co-occurring disorders is that mental health professionals may focus on the mental health aspect while addiction specialists focus on substance abuse, but both conditions need to be addressed together for effective treatment. Men with co-occurring disorders may find it difficult to access appropriate care, as traditional treatment programs may not be equipped to handle both aspects of their condition simultaneously.
Risk Factors for Addiction and Mental Health Issues in Men
Certain risk factors make men more susceptible to experiencing addiction and mental health problems. Understanding these factors can help identify individuals who may be at higher risk and encourage early intervention.
1. Genetics and Family History
Genetics can play a significant role in both addiction and mental health disorders. A family history of substance abuse or mental illness increases the likelihood that a man will develop similar issues. Studies have shown that men with a first-degree relative who struggles with addiction or a mental health condition are at a higher risk of developing these conditions themselves.
2. Environmental and Social Factors
The environment in which a person grows up can greatly influence their mental health and susceptibility to addiction. Growing up in a home with substance abuse or mental health issues, or in an environment where substances are readily available, increases the risk of developing these disorders. Additionally, experiencing social isolation, poverty, or chronic stress can also contribute to the development of mental health and addiction problems.
3. Chronic Stress
Men who are exposed to chronic stress—whether from work, family pressures, or societal expectations—are at higher risk of developing both addiction and mental health issues. Chronic stress increases cortisol levels, which can lead to anxiety, depression, and other psychological challenges. To cope with these overwhelming feelings, men may turn to substances as a way to manage stress, reinforcing the addiction cycle.
Addressing Addiction and Mental Health in Men: Treatment Approaches
1. Integrated Treatment for Co-Occurring Disorders
The most effective approach for treating men with both addiction and mental health issues is integrated treatment. Integrated treatment involves addressing both disorders simultaneously rather than treating them in isolation. This approach allows for a more holistic and individualized care plan, which can lead to better outcomes.
Integrated treatment often combines psychotherapy, medication, and group therapy to address both the addiction and the mental health disorder. Cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT) are commonly used to help individuals understand the root causes of their addiction and mental health challenges, while also developing healthier coping mechanisms.
2. Support Groups and Peer Support
Peer support plays a crucial role in helping men manage both addiction and mental health conditions. Support groups, such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), provide a safe space for individuals to share their experiences and learn from others who have been through similar struggles. These groups are often instrumental in helping men feel less isolated and more empowered to seek help.
3. Mindfulness and Stress Reduction
Mindfulness practices and stress reduction techniques, such as meditation, yoga, and deep breathing, can help men manage both their addiction and mental health conditions. These practices encourage men to stay present in the moment and reduce the anxiety or depression that may contribute to substance use.
4. Reducing the Stigma Around Men’s Mental Health
Reducing the stigma around mental health and addiction is key to encouraging more men to seek treatment. Campaigns that focus on deconstructing traditional notions of masculinity and promoting emotional openness can help men feel more comfortable seeking support. Normalizing mental health struggles and substance abuse as treatable conditions can go a long way in breaking down barriers to treatment.
Conclusion
The link between addiction and mental health in men is complex, yet understanding this connection is crucial in order to effectively address both issues. Trauma, societal expectations, and biochemical imbalances all play significant roles in the development of both addiction and mental health disorders. By focusing on integrated treatment approaches, reducing stigma, and providing support, we can better assist men in breaking the cycle of addiction and mental health challenges. With the right help and support, men can regain control of their lives and work towards lasting recovery and improved mental well-being.
Robert Weigel
Works Cited: “addiction and mental health in Men” prompt, ChatGPT, 20 July version, Open AI, 20 July 2023, chat.openai.com/chat
0 notes
Text
Social Determinants of Health Industry: Global Social Determinants Have Significant Impact on Public Health

Income and Social Status
Research shows a strong and consistent association between socioeconomic factors like income, wealth and education level with physical and mental health as well as mortality rates across countries. People with lower income and social status face higher health risks and have poorer health outcomes than those with higher socioeconomic positions. The gap in health outcomes between socioeconomic groups is growing in both developed and developing nations. Several studies show that income and wealth are direct determinants of nutrition, living conditions, health behaviors and access to healthcare. People living in poverty experience higher stress levels which can accelerate disease processes. Lack of financial resources also limits choices and capacities to avoid health risks. Social Determinants of Health Industry Work Environment
Global Social Determinants of Health type of work done, its physical and chemical hazards, job security and control over work processes and schedules are important social determinants. People in manual labor, manufacturing and service jobs are at greater risk of work-related stress, injuries and exposure to toxins. Lack of employment security due to contract work or frequent lay-offs increases stress and associated health issues. Higher control over work, its flexibility and social support positively impacts mental well-being. Long work hours, shift work and heavy physical labor contribute to chronic diseases if prolonged over years without adequate rest or safety measures. Exposure to workplace hazards and toxic substances like asbestos, chemicals and extreme noise levels raise disease probabilities. Early Life Conditions
Experiences during prenatal period and early childhood have profound influence on health in later years. Adverse experiences like low birthweight, malnutrition, toxic stress from violence or abuse, lack of cognitive and social stimulation impact brain development and lay the foundation for diseases in adulthood. Epigenetic changes caused by early life stress get passed on to subsequent generations. Favorable physical and social environments during developmental periods strengthen physical and mental health through life. Ensuring parents have resources and community support to provide nurturing care and fulfilling environments for young children is crucial. Social Support Networks
Availability of social connections and relationships determines access to practical and emotional support systems. Strong connections within social networks positively impact both physical and mental well-being. The inverse is also true - loneliness and social isolation are established risk factors for several illnesses including depression, anxiety, cardiovascular diseases and dementia. Living alone, lack of friends or involvement in community activities heighten risks. Having trusting relationships where people feel cared for and that they matter is integral to health across the entire lifespan. Addiction
Substance abuse including alcohol, tobacco, drugs and new addictive behaviors like gambling pose high economic costs to nations and communities. Addiction undermines health and social functioning in individuals. Emerging evidence indicates genetic predispositions and social influences together influence addiction risks. Family history, childhood trauma and lack of opportunities are acknowledged precursors that drive people towards addiction seeking behaviors. Media portrayal and marketing of risky substances normalize and glamorize usage especially among vulnerable sections. Addiction affects health directly and damages vital social roles and relationships amplifying its harmful impacts. Built Environment
Where people live, physical surroundings and neighborhood qualities substantially affect health. Aspects like urban design, public transportation options, infrastructure for walking and cycling, access to fresh foods and green spaces, air and water quality influence lifestyle patterns. Disadvantaged neighborhoods with higher crime rates, vacant buildings, liquor stores and fast food dominate food options encourage sedentary living and unhealthy diets. Lack of community resources like public parks force people indoors and away from physical activities. These attributes of built environments disproportionately impact lower socioeconomic communities concentrating health issues. Social Determinants of Health Industry Health Policies
Policies addressing social and commercial determinants are central to tackling health inequities. Strong public health systems providing universal preventive services and treatment can buffer vulnerabilities linked to socioeconomic disadvantages. Paid sick leaves, parental benefits, labor protection laws improve health of disadvantaged groups. Investments in public education strengthen social mobility and economic participation. Regulations curbing tobacco and junk food marketing protect populations. Universal basic income schemes alleviate poverty induced health risks. Progressive tax structures funding robust welfare programs also achieve redistribution of resources minimizing socioeconomic health gaps across societies. In this article aimed to discuss some key social determinants of health and their underlying pathways of influence across global populations based on extensive research evidence. It highlighted the graded association between socioeconomic factors like income, education and occupation with various health conditions. The impacts of early life experiences, addiction risks, built environments and health policies were also reviewed. Strong social factors like income inequality, lack of community support systems or hazardous neighbourhoods concentrating in disadvantaged communities create health inequities affecting nations' social and economic progress. A holistic, multisectoral approach is necessary to tackle root determinants and alleviate health disparities worldwide.
Get more insights on, Global Social Determinants of Health
For Deeper Insights, Find the Report in the Language that You want.
Japanese Korean
About Author:
Vaagisha brings over three years of expertise as a content editor in the market research domain. Originally a creative writer, she discovered her passion for editing, combining her flair for writing with a meticulous eye for detail. Her ability to craft and refine compelling content makes her an invaluable asset in delivering polished and engaging write-ups.
(LinkedIn: https://www.linkedin.com/in/vaagisha-singh-8080b91)
#Coherent Market Insights#Digital Technology Adoption#Access to Care Disparities#Social Impact Partnerships#Rising Healthcare Expenditure
0 notes
Text
Physical and sexual violence, childhood sexual abuse and HIV/STI risk behaviour among alcohol-using women engaged in sex work in Mongolia
Background
Although low, HIV prevalence in Mongolia could increase without strategic prevention strategies. Female sex workers (FSWs) often experience barriers to prevention, including interpersonal violence. This study investigated if childhood sexual abuse (CSA) or recent physical or sexual violence was associated with HIV sexual risk behaviours and if CSA modified associations between recent violence and HIV sexual risk behaviours.
Methods
Two-hundred twenty-two women who: (1) were at least 18 years old and clients at the National AIDS Foundation; (2) reported vaginal or anal sex in the past 90 days in exchange for money or goods; and (3) met criteria for harmful alcohol use in the past year were enrolled. In-person interviews assessed sexual risk behaviours and violence in childhood and adulthood. Negative binomial regression, ordinary least squares regression, and modified Poisson regression were performed.
Results
Sexual risk with paying partners was associated with penetrative CSA and sexual violence by paying partners. CSA and recent violence were not associated with sexual risk behaviours with intimate partners. CSA modified the association between recent sexual violence and unprotected sex with intimate partners.
Conclusion
Findings highlight the need for integrated violence and sexual risk reduction services to ensure safe and effective prevention for FSWs.
Keywords: Violence, HIV, Alcohol, Sex work
Introduction
Although the prevalence of HIV in Mongolia is low, Mongolia is at high risk of experiencing an HIV epidemic if rapid and strategic HIV prevention strategies are not instituted (UNGASS, 2010). One hundred cases of HIV have officially been reported, representing less than 0.1% of the adult population (Joint United Nations Programme on HIV/AIDS [UNAIDS] Mongolia, 2012). This represents a significant increase from just five reported cases as of 2004 (UNAIDS Mongolia, 2012).
A constellation of factors makes Mongolia vulnerable to rapid HIV spread. Mongolia is bordered by Russia to the North and China to the South and East, two countries with increasing numbers of people living with HIV/AIDS. Of new HIV infections in Eastern Europe and Central Asia, almost 90% occur in Russia or the Ukraine (UNAIDS, 2011). In China, while national HIV prevalence remains low, the number of people living with HIV/AIDS continues to increase (Ministry of Health of the People’s Republic of China, 2012). Moreover, groups at elevated risk of contracting HIV in China (e.g., female sex workers, men who have sex with men) report high rates of HIV sexual risk behaviours (Ministry of Health of the People’s Republic of China, 2012). A regional highway is under construction in Mongolia. Once completed, this highway will provide a trade route between Russia and China through Mongolia, likely increasing the migration of workers through Mongolia. Increased migration of workers has been associated with growing HIV epidemics across geographic boundaries on other continents (Elbright, Altantsetseg, & Oyungerel, 2003; Fages, 1999; Hagan & Dulmaa, 2007; UNAIDS, 2001).
In addition, since 1990 Mongolia has experienced a difficult economic transition from a centrally planned (Soviet-supported) to a free market economy, resulting in 27% of the population living below the poverty line (World Bank, 2013). Mongolia has a total population of 2.8 million, 40% of whom live in the capital city of Ulaanbaatar (World Bank, 2013). Ulaanbaatar has experienced increased alcoholism, unemployment and homelessness, a deteriorating health and social services system, and substantial increases in survival sex work among women (Davaalkham et al., 2009; National AIDS Foundation [NAF], 2001, 2003; Purevdawa et al., 1997). Sex work remains illegal in Mongolia, according to the 1998 Mongolian Law against Pornography and Prostitution which banned the organisation and facilitation of prostitution (Carlson, Tsai, Aira, Riedel, and Witte, forthcoming). Despite this law, there are approximately 4,000 commercial sex workers in Ulaanbaatar, the majority of whom are female (UNICEF, 2006). The number of women engaging in sex work in Mongolia fluctuates seasonally with many women engaging in sex work only during warmer summer months (Carlson et al., forthcoming).
In Mongolia, HIV primarily remains clustered among high risk groups including female sex workers (FSWs) and men who have sex with men. Although the most recent Behavioural Surveillance Survey reported a 0% prevalence of HIV among FSWs surveyed, half of all reported female cases of HIV are among FSWs whose paying partners are considered a bridge population in Mongolia (UNAIDS Mongolia, 2012). Because rates of new sexual partner acquisition among FSWs are significantly higher than the general population, FSWs often serve as drivers of HIV in low prevalence settings, contributing disproportionately to the spread of HIV into the general population (Anderson, 1999; Morris and Ferguson, 2006; World Health Organization [WHO], 2011). Given the transmission dynamics of HIV, FSWs are uniquely positioned to prevent a generalised HIV epidemic in low prevalence settings such as Mongolia.
Alcohol use among FSWs is prevalent and normative across countries and commonly used by FSWs to facilitate participation in commercial sex. FSWs are often encouraged or coerced to drink alcohol by clients and pimps (Markosyan et al., 2007). FSWs often report using alcohol while looking for clients and having sex while intoxicated (Chersich et al., 2007; Markosyan et al., 2007; Nishigaya, 2002; Rogers, Ying, Xin, Fung, & Kaufman, 2002). Alcohol use has been consistently associated with violence and HIV risk behaviours among FSWs including unprotected sex, anal sex, STIs, and HIV (Chersich et al., 2007; Li, Li, & Stanton, 2010; Scorgie et al., 2010; Wechsberg, Luseno, & Lam, 2005; Wechsberg, Luseno, Lam, Parry, & Morojele, 2006; WHO, 2011; Yadav et al., 2005).
Studies of sex workers across the globe highlight that multiple traumas, including childhood sexual abuse (CSA) and intimate partner violence (IPV), are associated with HIV sexual risk behaviours among this population (El-Bassel et al., 2003; Paone, Cooper, Alperen, Shi, & Des Jarlais, 1999; Shahmanesh et al., 2009; Surratt, Kurtz, Weaver, & Inciardi, 2005; Ulibarri et al., 2009). FSWs are at particularly high risk of physical and sexual violence from paying and non-paying partners, managers, and the police (Decker et al., 2010; Karandikar & Prospero, 2010; Open Society Institute, 2009; Rhodes, Simic, Baros, Platt, & Zikic, 2008; Simic & Rhodes, 2009; Swain, Saggurti, Battala, Verma, & Jain, 2011). Violence has been consistently associated with increased HIV risk among FSWs, including increased risk of sexually transmitted infections (STIs), anal sex, and unprotected sex (Decker et al., 2012; Simic & Rhodes, 2009; Swain et al., 2011; Ulibarri et al., 2011).
Experiences of violence contribute significantly to increasing women’s risk of HIV acquisition through biological, behavioural, and social mechanisms (Adimora et al., 2013; El-Bassel et al., 2003; Surrat et al., 2005). Violence is often linked to conflicts over condom negotiation (Wingood, Hunter-Gamble, & DiClemente, 1993). Coercive sex puts women at increased risk of contracting an STI, as they have less control over the situation and safe sexual practices. STIs, in turn, enhance the probability of HIV transmission during unprotected sex (Choi, Chen, & Jiang, 2008). The prevalence of STIs is high and increasing in Mongolia (Davaalkham et al., 2009; Hagan & Dulmaa, 2007). STIs are currently the most prevalent type of communicable disease in Mongolia (UNGASS, 2010).
Research on violence against FSWs in Mongolia remains limited. One study examined the prevalence of violence among FSWs in Mongolia before and after implementing a risk reduction intervention. At baseline, across intervention groups, 38%–52% of FSWs reported recent physical violence from an intimate partner, 50%–62% reported recent physical violence from a paying partner, 12%–16% reported recent sexual violence from an intimate partner, and 26%–36% reported recent sexual violence from a paying partner (Carlson, et al., 2012).
In addition to violence during adulthood, FSWs are more likely to have experienced CSA compared to women not engaged in sex work (Foti, 1995; James & Meyerding, 1977; Potter, Martin, & Romans, 1999). CSA has been associated with HIV sexual risk behaviours, including multiple sexual partners, unprotected sex, anal sex, STI symptoms, and early sexual debut (Lalor & McElvaney, 2010). In addition, women who experience CSA are at increased risk of sexual violence in adulthood from intimate partners (Classen, Palesh, & Arggarwal, 2005; Dunkle et al., 2004; Fanslow, Robinson, Crengle, & Perese, 2007; Fergusson, Horwood, & Lynskey, 1997; Messman-Moore & Long, 2003).
Given that violence is highly prevalent among FSWs and associated with HIV sexual risk behaviours, greater understanding of the nature of these relationships is needed. Recent evidence indicates that, among FSWs, HIV risk may differ by type of violence. For example, among FSWs in Moscow, violence perpetrated by paying clients, but not pimps, was associated with increased STI prevalence (Decker et al., 2012). In addition, despite the high prevalence of both CSA and recent violence against FSWs, little is known about the combined influence of CSA and recent violence on sexual risk behaviours. More specifically, whether CSA interacts with recent sexual or physical violence to further increase FSWs’ risk of engaging in sexual risk behaviours remains understudied. Greater understanding of interactions between violence during childhood and adulthood with sexual risk behaviours is needed to develop effective and appropriate HIV prevention strategies for FSWs, particularly for those with extensive histories of violence. Such information can be used to inform more relevant HIV prevention intervention components targeting FSWs and avoid escalation of HIV transmission in other countries at similarly high risk of experiencing an HIV epidemic, particularly countries with rapidly growing economies like Mongolia.
The purpose of this study is to investigate if (1) CSA is associated with HIV sexual risk behaviours; (2) recent physical or sexual violence is associated with HIV sexual risk behaviours; and (3) CSA modifies the association between recent violence and HIV sexual risk behaviours among FSWs in Mongolia.
Methods
Sample
Data were collected from women receiving services at the National AIDS Foundation (NAF) in Ulaanbaatar, Mongolia. Founded in 2000, NAF is the central resource and distribution source for NGO education and training in HIV/STI risk reduction and transmission information in Mongolia. Data are part of a parent study recruiting women for a randomised clinical trial testing the efficacy of an HIV/STI prevention intervention to reduce alcohol abuse and sexual risk behaviours among FSWs (Witte et al., 2011).
A total of 270 women were recruited and screened from 2008 to 2009. Women were eligible for the study if they: (1) were at least 18 years of age; (2) were currently enrolled in the NAF programme; (3) reported having engaged in vaginal or anal sexual intercourse in the past 90 days in exchange for money, alcohol, or other goods; and (4) met criteria for harmful alcohol use in the past year [score of eight or above on the Alcohol Use Disorders Identification Test (AUDIT), an internationally validated screening measure for alcohol problems in the past year, where a score of at least 8 or more indicates hazardous or harmful alcohol consumption] (Saunders, Aasland, Babor, DeLaFuente, & Grant, 1993). Of those screened, 41 women were excluded because they did not meet one or more of the eligibility criteria. Of the remaining 229 eligible women, 222 (97%) completed informed consent and baseline interviews. Research assistants administered baseline surveys lasting 60 to 90 minutes in a private setting. Assessments were administered using a computer-assisted personal interviewing (CAPI) method.
Assessment
The assessment interview was designed to elicit self-reported data. Measures were translated into Mongolian from English and then back-translated for accuracy. The assessment was pilot tested with seven NAF and research project staff and determined to have adequate face validity.
Sociodemographics
Sociodemographic variables included: age, race/ethnicity, education, employment status, income, marital status, having an intimate partner, current housing situation, and whether exchanging sex for money was the primary source of income.
Sexual Risk Behaviours
Using a method consistent with the Timeline Followback, participants provided data on the proportion and number of times they engaged in unprotected vaginal and anal sex with paying partners and intimate partners in the past 90 days (Sobell & Sobell, 1992). Measures were assessed separately for paying and intimate partners. A paying partner was defined as someone with whom you have sex in exchange for money, alcohol or other goods. An intimate partner was defined as a spouse, boyfriend, lover, or regular sexual partner who is not a paying partner.
Physical and Sexual Violence
To examine IPV as well as violence related to sex work, an adaptation of the Revised Conflict Tactics Scale was used which combined questions from similar categories (moderate vs. severe) assessing lifetime and recent physical and sexual violence perpetrated by intimate or paying partners (Straus, Hamby, Boney-McCoy, & Sugarman, 1996). ‘Mild’ violence questions, psychological aggression and negotiating behaviours were dropped to reduce questionnaire length. Recent violence was defined as violence that occurred within the past 90 days. The Cronbach’s alpha for the modified scale was 0.75 and 0.76 when measuring violence from intimate and paying partners, respectively.
Childhood Sexual Abuse
CSA was measured using a modified version of the Childhood Sexual Abuse Interview (CSAI). The modified CSAI consisted of 7 of the original 11 items which assessed experiences with someone 5 or more years older than the respondent, ranging from an attempt to have intercourse to forced intercourse. Exposure variables considered less severe and perhaps with less face validity in the Mongolian context were dropped. Each item was scored by assigning ‘1’ for the presence or ‘0’ for the absence of the item. Any CSA was measured by summing the seven items. A summed score of 0 was coded as no CSA; a summed score greater than 0 was coded as positive for any CSA. Penetrative CSA was quantified using four items from the CSAI (i.e., did anyone ever put his penis in your mouth or put their mouth on your private sexual parts, have intercourse with you against your will, insert an object into your vagina or put their penis or object in your bottom?) (Finkelhor, 1978; Sgroi, 1982). A summed score of 0 on these four items was coded as no penetrative CSA; a summed score greater than 0 on these four items was coded as positive for penetrative CSA. The Cronbach’s alpha for the modified scale was 0.72.
Data analysis
Data were collected using a computer-assisted data entry program. A faulty gate question to a single section of the assessment was discovered that affected the first 30 participants. Sexual risk variables with paying partners were missing for these participants. Bivariate analyses were conducted comparing those with and without missing data. There were no significant differences between groups in relation to reported alcohol use, sexual risk with trust partners or experiences of violence. However, those with missing data were significantly younger than those without missing data. No other significant sociodemographic differences were identified. Because the dates that participants completed the assessment were not conditioned on any particular variable, data were missing at random and multiple imputation was performed to complete the data set prior to analyses (Rubin, 1987).
Univariate statistics were used to describe sociodemographic characteristics, sexual behaviours, frequency and types of violence. Negative binomial regression was performed to estimate the incidence rate ratio (IRR) of unprotected vaginal and anal sex in the past 90 days. Ordinary least squares (OLS) regression was performed to estimate the b coefficient of the proportion of unprotected vaginal or anal sex in the past 90 days. Modified Poisson regression was performed to estimate the relative risk reduction (RRR) of the prevalence of unprotected vaginal or anal sex in the past 90 days. All analyses were adjusted for age, education, income, marital status, and alcohol use and performed separately for intimate and paying partners. Effect measure modification of the association between recent violence and HIV sexual risk behaviour by CSA was assessed by examining the magnitude and significance of product terms between recent physical or sexual violence and CSA.
Results
Sociodemographics
Descriptive statistics for the study sample are provided in Table 1. The average age of respondents was 34 years (range 18–67); the average age of initiation of sex work was 28 years (range 14–50). Participants were relatively well-educated with 64% having completed secondary school. Almost all (99%) participants were unemployed in formal sectors and reported sex work as their main form of income (93%). Most (60%) participants reported being divorced, widowed, or separated. Forty-four per cent of respondents reported currently having an intimate partner. Because eligibility was limited to women who scored 8 or higher on the AUDIT, all women in the sample were alcohol users. The overwhelming majority (93%) of women screened positive for alcohol dependence (i.e., scored 20 or greater on AUDIT).
0 notes
Text
What is hoarding disorder
Hoarding disorder is a serious mental health condition characterized by the persistent difficulty of discarding or parting with possessions, regardless of their actual value. People with hoarding disorder accumulate excessive amounts of items, often to the point where their living space becomes cluttered and unsafe. While it's easy to assume that hoarding is just a matter of being messy or disorganized, it’s actually a complex psychological condition that can have significant impacts on a person’s quality of life.
At its core, hoarding disorder is about more than just keeping things. It’s about an intense emotional attachment to objects and the anxiety that arises from the thought of letting go of them. Individuals with hoarding disorder often experience significant distress when they are faced with the idea of discarding possessions, even those that might seem completely unnecessary or even harmful. The items might be anything from newspapers, old clothing, broken appliances, to even things that others would consider trash, but the person with hoarding disorder sees them as important, valuable, or irreplaceable.
Key Signs and Symptoms of Hoarding Disorder
There are a few key signs that are commonly observed in individuals with hoarding disorder:
Difficulty Discarding Items: The most noticeable symptom is an overwhelming difficulty in letting go of possessions. This is true even when the items are not useful or necessary. Hoarding behaviors can be driven by a variety of reasons, including sentimental attachment, fear of wasting something, or the belief that items may be needed in the future.
Excessive Clutter: Over time, the accumulation of items leads to severe clutter in the home or workspace. The clutter can interfere with daily activities, such as cooking, cleaning, or even walking through the house. In extreme cases, it can cause safety hazards, blocking exits, and posing fire risks.
Emotional Distress: Individuals with hoarding disorder often feel anxious, distressed, or even overwhelmed at the thought of discarding items. The items are viewed as part of the person’s identity or a source of comfort, and letting go of them can cause feelings of loss, guilt, or anxiety.
Impaired Functioning: The hoarding behavior can significantly impair an individual’s ability to live a normal, functional life. It can strain relationships with family members, make it difficult to work, and can even cause legal or health issues due to unsafe living conditions. The disorder can lead to social isolation as people with hoarding tendencies may feel embarrassed or ashamed about the state of their homes.
Indecision and Perfectionism: Many individuals with hoarding disorder also struggle with indecision and perfectionism, often feeling paralyzed by the thought of making the wrong choice when it comes to discarding or organizing items. This can make cleaning or decluttering feel like an overwhelming, insurmountable task.
Causes of Hoarding Disorder
While the exact cause of hoarding disorder is not completely understood, research suggests that it can stem from a combination of genetic, psychological, and environmental factors. Some potential contributors include:
Genetics: Studies have shown that hoarding disorder can run in families, suggesting that there may be a hereditary component. People with a first-degree relative who has hoarding disorder may be more likely to develop the condition themselves.
Trauma and Stress: Past experiences, especially traumatic ones like the death of a loved one, childhood abuse, or emotional neglect, can contribute to hoarding behaviors. Hoarding may serve as a coping mechanism, a way to deal with overwhelming feelings of loss or emotional distress.
Brain Functioning: Some research suggests that individuals with hoarding disorder may have abnormalities in certain areas of the brain that control decision-making, organization, and emotional regulation, making it more difficult for them to make choices about possessions.
Psychological Factors: People with hoarding disorder often experience feelings of anxiety, depression, and perfectionism, which can contribute to the accumulation of items. Additionally, the emotional attachment to objects can be so strong that the thought of discarding something feels like a loss, triggering anxiety and distress.
Treatment of Hoarding Disorder
The good news is that hoarding disorder is treatable, though it can be a long and challenging process. Treatment typically involves a combination of Cognitive Behavioral Therapy (CBT) and other supportive approaches. CBT for hoarding disorder helps individuals identify and change the thought patterns that drive hoarding behavior. It teaches people how to make decisions about possessions, manage their anxiety around discarding items, and gradually reduce the clutter in their lives.
In some cases, medication may be prescribed to address symptoms of anxiety, depression, or obsessive-compulsive tendencies, which often co-occur with hoarding disorder. However, therapy remains the cornerstone of treatment. Support groups, where people can share their experiences and provide encouragement, can also play a critical role in recovery.
Impact on Life
Hoarding disorder is more than just a personal challenge; it can have wide-reaching effects on a person’s social and physical health. The clutter can make daily tasks nearly impossible, contribute to unsanitary living conditions, and create emotional strain on relationships with family members and friends. The accumulation of items can also pose serious health and safety risks, such as trip hazards, fire dangers, and even mold or pest infestations.
Additionally, hoarding can contribute to social isolation. People with hoarding disorder may feel too embarrassed to invite others into their home, or they may withdraw from social activities because of the clutter. As a result, the individual may feel alone and disconnected, which can further exacerbate the emotional distress tied to hoarding.
0 notes
Text
What are the current theories on the development of schizophrenia?
Current theories on the development of schizophrenia suggest a combination of genetic, environmental, and neurobiological factors. Genetics plays a significant role, with research indicating a higher risk in individuals with a family history of the disorder. Neurobiologically, imbalances in neurotransmitters like dopamine and glutamate are thought to contribute to the symptoms. Structural abnormalities in the brain, such as enlarged ventricles, have also been linked to the disorder. Environmental factors, including prenatal exposure to viruses, childhood trauma, or substance abuse, may increase the risk of developing schizophrenia. Understanding these theories helps in creating more effective treatments and interventions. For expert support and evaluation, visit https://www.delhimindclinic.com/ or explore options on https://www.bestpsychiatristsindelhi.com/ to connect with top psychiatrists in Delhi for personalized care and treatment.
0 notes
Text
Overcoming Self-Esteem Issues with Dr. Karen Hawk: Empowering Individuals to Embrace Their True Worth
Self-esteem plays a fundamental role in shaping our lives. It is the lens through which we view ourselves, our abilities, and our potential. When we have healthy self-esteem, we feel confident, capable, and worthy of love and respect. However, when self-esteem is low, it can hinder our ability to take risks, pursue our goals, and maintain healthy relationships. Low self-esteem can manifest in a variety of ways, from feelings of inadequacy and self-doubt to perfectionism and self-sabotage. It can be rooted in past experiences, negative self-talk, or the impact of societal expectations.
Dr. Karen Hawk, a compassionate and experienced counselor, offers a safe space for individuals struggling with self-esteem issues. Through personalized counseling sessions, she helps clients uncover the underlying causes of their low self-worth, challenge their negative beliefs, and develop the tools necessary to cultivate lasting self-confidence. With Dr. Hawk’s guidance, individuals can learn to embrace their inherent value, build resilience, and foster a more positive self-image.
Understanding the Roots of Low Self-Esteem
Low self-esteem doesn’t develop overnight. It is often the result of a combination of internal and external factors that influence how we perceive ourselves. Some common causes of low self-esteem include:
Negative Childhood Experiences: Early life experiences, such as criticism, neglect, or emotional abuse, can significantly impact one’s sense of self-worth. Children who grow up in environments where they are consistently criticized, neglected, or made to feel inferior may internalize these messages and carry them into adulthood.
Unrealistic Expectations: Societal pressure to meet certain standards—whether in appearance, success, or behavior—can create unrealistic expectations that lead to feelings of inadequacy. The constant comparison to others, especially in the age of social media, can exacerbate feelings of low self-esteem.
Past Failures or Rejection: Past experiences of failure, rejection, or disappointment can contribute to negative self-beliefs. When individuals face setbacks or experience significant disappointments, they may internalize these events as evidence of their inadequacy, rather than as opportunities for growth.
Negative Self-Talk: People with low self-esteem often engage in harsh self-criticism and negative self-talk. This internal dialogue, which may include thoughts like “I’m not good enough” or “I’ll never succeed,” reinforces the belief that they are not worthy of success, love, or happiness.
Toxic Relationships: Relationships that are emotionally abusive, dismissive, or manipulative can also take a toll on self-esteem. Constant criticism, emotional neglect, or devaluation from others can chip away at one’s sense of self-worth.
Perfectionism: Perfectionism often stems from an underlying fear of failure or rejection. People with perfectionistic tendencies may set impossibly high standards for themselves, which, when unmet, reinforce feelings of inadequacy and worthlessness.
Dr. Karen Hawk’s Approach to Healing Low Self-Esteem
Dr. Hawk’s approach to addressing self-esteem issues is rooted in compassion, understanding, and empowerment. She provides a supportive environment where clients feel safe to explore their feelings of self-doubt and inadequacy. Dr Karen Hawk psychologist Arizona believes that everyone has inherent worth and potential, and her goal is to help clients rediscover and embrace their authentic selves.
The following are key aspects of Dr. Hawk’s approach to improving self-esteem:
Identifying the Root Causes: The first step in addressing low self-esteem is identifying its root causes. Dr. Hawk works with clients to uncover past experiences, negative beliefs, and patterns of behavior that contribute to their self-esteem issues. By understanding the origins of their feelings of inadequacy, clients can begin to challenge and shift these beliefs.
Challenging Negative Self-Talk: Dr. Hawk teaches clients how to identify and challenge negative self-talk. Many individuals with low self-esteem engage in automatic, self-critical thoughts that reinforce their feelings of unworthiness. Through cognitive-behavioral techniques (CBT), Dr. Hawk helps clients reframe these thoughts and replace them with more realistic, positive affirmations.
Building Self-Compassion: One of the most important aspects of healing low self-esteem is learning to practice self-compassion. Dr. Hawk encourages clients to treat themselves with the same kindness and understanding they would offer to a friend facing similar struggles. By developing self-compassion, individuals can begin to soften their inner critic and cultivate a healthier relationship with themselves.
Embracing Imperfection: Perfectionism is often closely tied to low self-esteem. Dr. Hawk works with clients to reframe their perception of imperfection, helping them understand that making mistakes and having flaws are natural parts of being human. Embracing imperfection allows individuals to let go of unrealistic expectations and accept themselves as they are, flaws and all.
Setting Realistic Goals: Dr Karen Hawk psychologist helps clients set realistic, achievable goals that align with their values and strengths. When individuals with low self-esteem set and achieve small goals, it can boost their confidence and sense of accomplishment. These successes, no matter how small, serve as proof that they are capable and deserving of success.
Cultivating Self-Worth Through Action: Building self-esteem requires more than just changing one’s thoughts. Dr. Hawk encourages clients to take positive actions that reinforce their sense of self-worth. This might include pursuing hobbies, engaging in physical activity, or taking steps toward personal or professional goals. By taking action that reflects their values and strengths, individuals can create a stronger sense of self-worth.
Healing from Past Trauma: Often, low self-esteem is tied to past trauma or negative experiences. Dr. Hawk uses a trauma-informed approach to help clients process past hurt and heal from emotional wounds. By addressing the root causes of low self-esteem, clients can begin to release the shame and guilt that may be holding them back from embracing their true value.
Fostering Healthy Relationships: Dr. Hawk recognizes that healthy relationships play a critical role in supporting self-esteem. She helps clients identify toxic relationships or negative dynamics that may be contributing to their feelings of unworthiness. Through counseling, individuals can learn to set boundaries, communicate their needs, and cultivate relationships that are supportive and nurturing.
Building Lasting Self-Confidence
Karen Hawk psychologist Arizona helps individuals take concrete steps to build lasting self-confidence and develop a stronger sense of self-worth. Self-confidence is not about being perfect or never feeling insecure; it’s about trusting in one’s abilities, accepting imperfections, and believing in one’s value despite setbacks or challenges.
Some strategies that Dr. Hawk uses to build self-confidence include:
Celebrating Successes: Dr. Hawk encourages clients to celebrate even their smallest victories. Whether it’s completing a task, making progress in therapy, or simply getting through a challenging day, acknowledging success boosts confidence and reinforces the belief that they are capable.
Developing a Growth Mindset: A growth mindset is the belief that abilities and intelligence can be developed through effort and learning. Dr. Hawk works with clients to foster this mindset, encouraging them to view challenges as opportunities for growth rather than as reflections of their worth. By shifting their perspective, individuals can approach life with a sense of curiosity and resilience.
Practicing Mindfulness: Mindfulness practices help individuals stay grounded in the present moment, reducing the impact of negative thoughts and worries about the future. Dr. Hawk teaches mindfulness techniques that help clients focus on their strengths, celebrate their progress, and build emotional resilience.
Creating Positive Affirmations: Karen Hawk psychologist helps clients create personalized positive affirmations that reflect their strengths, values, and goals. Repeating these affirmations daily can help individuals reprogram their self-perception and reinforce their belief in their worth and capabilities.
The Journey to Empowerment and Self-Acceptance
The journey toward improved self-esteem and self-confidence is an ongoing process that requires patience, commitment, and support. With Dr. Hawk’s guidance, individuals can begin to heal from past hurts, challenge negative beliefs, and embrace their inherent worth. By focusing on self-compassion, imperfection, and positive action, clients can build lasting self-esteem and live more fulfilling lives.
Through therapy, individuals not only learn to embrace their true selves but also develop the skills and resilience necessary to navigate life’s challenges with confidence. Dr. Karen Hawk is committed to helping clients break free from self-doubt, unlock their full potential, and live empowered, authentic lives.
Conclusion: Embracing Your True Worth
Low self-esteem can be a heavy burden, but it doesn’t have to define your life. With the right support, it is possible to rebuild a strong sense of self-worth and live with confidence and authenticity. Dr. Karen Hawk’s compassionate and empowering approach to self-esteem counseling helps individuals uncover their value, heal from past wounds, and embrace their true worth.
Whether through challenging negative self-talk, healing from past trauma, or setting realistic goals for personal growth, Dr. Hawk’s guidance provides the tools needed to foster lasting self-esteem. Through this transformative process, clients can step into their power, rediscover their inner strength, and live with the confidence and self-assurance they deserve.
0 notes
Text
Is Psychopathy Genetic? Nature vs. Nurture Debate

Psychopathy is a complex personality disorder that is often characterised by manipulative behaviour, lack of empathy, and a disregard for the rights and feelings of others. But what causes someone to develop these traits and tendencies? Is psychopathy simply a result of environmental factors, or could there be a genetic component at play? Numerous studies have been conducted over the years to examine the potential genetic link to psychopathy. While environmental factors such as childhood trauma and upbringing certainly play a role in the development of psychopathic traits, research has shown that genetics may also play a significant role in shaping a person's susceptibility to developing psychopathy. One study published in the Journal of Abnormal Psychology found that individuals with a parent or sibling who exhibited psychopathic traits were more likely to display similar traits themselves, suggesting a genetic predisposition to psychopathy. Another study published in the Journal of Criminal Justice found that genetic factors accounted for 46% of the variation in psychopathic traits among participants. These findings suggest that psychopathy may indeed have a genetic component, with certain genes predisposing individuals to developing psychopathic traits. However, it's important to note that genetics alone do not determine the development of psychopathy. Environmental factors such as childhood abuse, neglect, and exposure to violence also play a significant role in shaping a person's personality and behaviour. Furthermore, not everyone with a genetic predisposition to psychopathy will go on to exhibit the full range of psychopathic traits. Factors such as upbringing, social support, and access to mental health resources can all influence whether someone with genetic risk factors for psychopathy ultimately develops the disorder. In conclusion, while psychopathy may have a genetic component, it is a complex disorder that is influenced by a multitude of factors. More research is needed to fully understand the interplay between genetics and environmental factors in the development of psychopathy. By better understanding the root causes of psychopathy, we can work towards more effective prevention and intervention strategies for individuals at risk of developing this disorder. Read the full article
0 notes
Text
Comprehensive Guide to Overcoming Depression: Seeking Psychologist Therapy in Bilaspur

Introduction
Depression is a serious mental health condition that can significantly impact one's quality of life. It is essential to address it with the right professional help. If you or someone you know is struggling with depression, seeking psychologist therapy in Bilaspur is a crucial step towards recovery. This comprehensive guide aims to provide an in-depth understanding of depression, its symptoms, causes, and available treatment options.
Understanding Depression
Depression is more than just feeling sad or having a bad day. It is a persistent condition that affects how you feel, think, and handle daily activities. Recognizing the need for professional help and understanding the severity of the condition is the first step towards recovery.
Recognizing the Symptoms of Depression
Identifying the symptoms of depression can help you seek help early. Here are the common signs:
Emotional Symptoms
Persistent Sadness: A continuous feeling of sadness or emptiness.
Hopelessness: Feeling that nothing will ever get better.
Loss of Interest: Lack of interest in activities that were once enjoyable.
Physical Symptoms
Fatigue: Constantly feeling tired or lacking energy.
Sleep Disturbances: Insomnia or excessive sleeping.
Appetite Changes: Significant weight loss or gain due to changes in eating habits.
Physical Aches: Unexplained pains and aches.
Cognitive Symptoms
Difficulty Concentrating: Trouble focusing or making decisions.
Memory Problems: Forgetfulness or difficulty recalling information.
Suicidal Thoughts: Frequent thoughts about death or self-harm.
Causes of Depression
Understanding the causes of depression can aid in finding the right treatment. Here are some primary factors:
Genetic Factors
Depression can run in families, indicating a hereditary component. If you have a family history of depression, you might be at higher risk.
Environmental Factors
Life Stressors: Major life changes, such as losing a loved one, can trigger depression.
Work-Related Stress: High-stress jobs or unemployment can contribute to depression.
Social Isolation: Lack of a supportive social network can increase the risk.
Psychological Factors
Personality Traits: Individuals with low self-esteem or a pessimistic outlook are more susceptible.
Traumatic Experiences: Childhood trauma or abuse can lead to depression later in life.
Types of Depression
Different types of depression require different treatment approaches. Here are some common types:
Major Depressive Disorder (MDD)
Characterized by severe depressive episodes lasting at least two weeks.
Persistent Depressive Disorder (PDD)
A chronic form of depression lasting for at least two years, with less severe but longer-lasting symptoms than MDD.
Bipolar Disorder
Includes episodes of depression alternating with periods of mania (extreme highs).
Seasonal Affective Disorder (SAD)
Depression that occurs at specific times of the year, usually in winter.
Seeking Professional Help
If you identify with any of these symptoms or types, it is crucial to seek professional help. Psychologist therapy in Bilaspur offers tailored treatment plans to address and manage depression effectively.
Treatment Options for Depression
Several effective treatments can help manage and overcome depression. Here are the primary options:
Psychotherapy
Cognitive-Behavioral Therapy (CBT): Helps change negative thought patterns and behaviors.
Interpersonal Therapy (IPT): Focuses on improving communication and relationships.
Psychodynamic Therapy: Explores past experiences to understand current issues.
Medication
Antidepressants: Medications like SSRIs and SNRIs help regulate mood.
Mood Stabilizers: Particularly useful for bipolar disorder.
Antipsychotics: Used alongside other medications for severe depression.
Lifestyle Changes
Regular Exercise: Physical activity can improve mood and reduce stress.
Healthy Diet: A balanced diet helps maintain stable energy levels.
Adequate Sleep: Ensuring quality sleep is essential for mental health.
Mindfulness and Relaxation: Practices like meditation and yoga can help manage symptoms.
Self-Help Strategies
In addition to professional treatment, self-help strategies can support recovery:
Mindfulness and Meditation
Practicing mindfulness can help manage stress and improve overall well-being.
Journaling
Writing about your thoughts and feelings can help process emotions and identify patterns.
Social Support
Connecting with friends, family, or support groups provides essential emotional support.
Time Management
Effective time management can reduce stress and prevent feelings of being overwhelmed.
Limiting Caffeine and Alcohol
Both substances can worsen depressive symptoms, so limiting their intake can help.
When to Seek Immediate Help
If you experience severe symptoms or have thoughts of self-harm, it is crucial to seek immediate help. A psychology counsellor in Bilaspur can provide the urgent care and support needed in such situations.
Conclusion
Depression is a serious condition that requires professional intervention. Recognizing the symptoms and understanding the causes can lead to effective treatment. Psychologist therapy in Bilaspur offers comprehensive support to help manage and overcome depression. If you or a loved one is struggling with depression, don’t hesitate to seek help. A psychology counsellor in Bilaspur is available to guide you through the journey towards recovery. Remember, taking the first step towards getting help is the most important step you can take. Reach out today and start your path to a healthier, happier life.
0 notes
Text

Teenage depression is a serious mental health issue that affects many adolescents, impacting their emotional, functional, and physical well-being. As an educational expert, it is crucial to provide parents and students with the necessary information to recognize and address this condition effectively. This article aims to offer a comprehensive overview of teenage depression, its symptoms, causes, risk factors, and treatment options, while emphasizing the importance of early intervention and support.
What is Teenage Depression?
Teenage depression goes beyond the typical moodiness associated with adolescence. It is a persistent feeling of sadness, hopelessness, and a lack of interest in activities that were once enjoyable. This condition can interfere with a teenager's daily life, causing emotional, functional, and physical problems.
Symptoms of Teenage Depression
Recognizing the signs of teenage depression is the first step towards getting help. Symptoms can vary in severity and may manifest differently in teens compared to adults. Key symptoms include:
Emotional Changes
Persistent sadness, crying spells
Feelings of hopelessness or emptiness
Irritability, frustration, or anger over minor issues
Loss of interest in activities
Low self-esteem, feelings of worthlessness or guilt
Extreme sensitivity to rejection or failure
Trouble concentrating, making decisions, or remembering things
Thoughts of death, dying, or suicide
Behavioral Changes
Fatigue, loss of energy
Insomnia or excessive sleeping
Changes in appetite, weight loss or gain
Use of alcohol or drugs
Agitation or restlessness
Frequent complaints of physical aches and pains
Social withdrawal, poor school performance
Neglect of personal hygiene
Risky or self-destructive behavior, such as self-harm
Causes of Teenage Depression
The exact cause of teenage depression is not known, but several factors may contribute to its development:
Biological Factors
Brain Chemistry: Imbalances in neurotransmitters can affect mood regulation.
Hormonal Changes: Puberty and other hormonal changes can trigger depression.
Inherited Traits: Family history of depression increases the risk.
Environmental Factors
Trauma and Abuse: Physical, emotional, or sexual abuse during childhood.
Stressful Life Events: Death of a loved one, parental divorce, or other significant changes.
Bullying and Cyberbullying: Persistent bullying can lead to feelings of helplessness and depression.
Psychological Factors
Negative Thinking Patterns: Learned helplessness and negative thinking can contribute to depression.
Low Self-Esteem: Persistent negative self-perception and self-criticism.
Risk Factors for Teenage Depression
Certain factors can increase the likelihood of developing depression in teenagers:
Having issues that negatively impact self-esteem, such as obesity or academic problems
Witnessing or being a victim of violence or abuse
Having other mental health conditions like anxiety, ADHD, or eating disorders
Chronic physical illnesses such as diabetes or asthma
Personality traits such as low self-esteem or being overly self-critical
Substance abuse
Unsupportive environments, especially for LGBTQ+ teens
Complications of Untreated Depression
If left untreated, teenage depression can lead to severe complications, including:
Substance misuse
Academic problems
Family conflicts and relationship difficulties
Suicide attempts or suicide
Prevention and Treatment
While it may not be possible to prevent depression entirely, certain strategies can help reduce the risk and mitigate the effects:
Prevention Strategies
Encourage stress management and resilience-building activities.
Promote self-care, including healthy sleep routines and responsible electronics use.
Foster strong social support networks.
Treatment Options
Effective treatment for teenage depression often involves a combination of approaches:
Psychotherapy
Cognitive Behavioral Therapy (CBT): Helps teens recognize and change negative thought patterns.
Family Therapy: Addresses family dynamics that may contribute to depression.
Interpersonal Therapy (IPT): Focuses on improving relationships and communication skills.
Medication
Antidepressants can be effective but require careful monitoring for side effects, especially in young people.
Lifestyle Changes
Encourage regular physical activity.
Promote a balanced diet rich in nutrients that support brain health.
Ensure adequate sleep and limit screen time.
Supporting a Depressed Teen
Parental support plays a critical role in the recovery process. Here are some practical tips for parents:
Communication
Open a dialogue by expressing concern and willingness to listen without judgment.
Be patient and persistent, even if your teen initially resists discussing their feelings.
Validate their emotions and avoid minimizing their experiences.
Encouraging Social Connection
Help your teen maintain relationships with friends and family.
Limit social media use and encourage face-to-face interactions.
Involve your teen in activities that align with their interests and talents.
Professional Help
Seek the guidance of a mental health professional if symptoms persist or worsen.
Involve your teen in treatment decisions to increase their engagement and motivation.
Self-Care for Parents
Take care of your own mental and physical health.
Reach out to support groups or therapists for yourself if needed.
Keep open lines of communication with other family members and ensure siblings are also supported.
Conclusion
Understanding and addressing teenage depression is crucial for the well-being of adolescents. By recognizing the symptoms, understanding the causes and risk factors, and seeking appropriate treatment, parents and educators can help teens navigate this challenging period. Early intervention and ongoing support are key to helping teenagers overcome depression and lead fulfilling lives. At Ecole Globale Schools, we are committed to providing a supportive environment where every student can thrive.
0 notes
Text
Risk Factors for Developing BPD
It can be entirely biological, which isn't exactly avoidable. However, it can also stem from childhood trauma, abuse, or significant time in an invalidating environment.

The main cause is a combination of two things.
1 - Biological Vulnerability - about 50% is caused by this. If you have a directly related relative with it, you're about 10 times more likely to develop it.
2 - Coming from an Invalidating Environment. Even the greatest of parents... Not knowing how to handle a child with it will inevitably cause harm. The BEST thing you can do is educate yourself on how to help the child. They don't know how to regulate their emotions and need your help to figure it out..
Criticism, however, can cause them to subconsciously try to ignore their emotions entirely, seeing them as "always wrong" or "always leading them to trouble." This causes what's known as dissociation. (blank... empty.. nothing.. )
Not everybody has both of these. Your chances just go up significantly if you are exposed to these things.
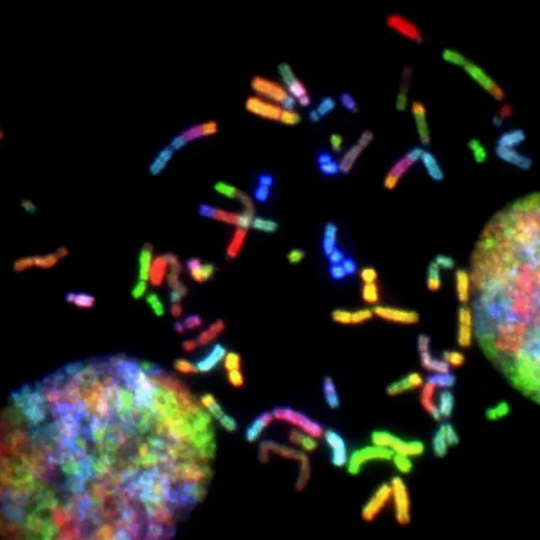
It Can Be Completely Biological
Studies have shown changes in areas of the brain that are involved in emotional regulation, aggression, and impulsivity; as well as certain brain chemicals that assist in mood regulation, like serotonin, may not function correctly. Researchers believe that many people with Borderline Personality Disorder have an issue with the neurotransmitters in their brain, especially serotonin. Altered serotonin levels have been linked to aggression, depression, and make it harder to control destructive urges.
Researchers are working on ways to help prevent this.. Early and intense intervention is key!
MRI scans use magnetic fields along with radio waves to produce detailed images of the inside of the body. When MRIs were done on patients with BPD, they found 3 parts of the brain that had unusual levels of activity or were smaller altogether than someone without the disorder.
The 3 parts were:
the amygdala – plays an important role in regulating emotions, especially more "negative" ones, like fear, anxiety, and aggression
the hippocampus – helps regulate self-control and behavior
the orbitofrontal cortex – used in planning and decision making
Early upbringing affects the development of these parts of the brain. They are responsible for mood regulation and might account for some of the issues those with BPD often have in personal relationships. One's relationship with their family has a huge influence on how they end up seeing the world and determines how they view others.

Environmental Factors
Many people with Borderline Personality Disorder report a history of physical and or sexual abuse as a child as well as neglect. Others lost a parent or were separated from them at a young age. Some were exposed to hostile home lives or unstable family relationships.
Unresolved emotions from childhood can lead to multiple distorted thinking patterns as an adult. For example, idealization, feeling like a child around other adults, expecting others to parent, or even bully you.
Most people experience some sort of "inconveniences" throughout life. But prolonged exposure to these things is what can lead to the development of Borderline Personality Disorder. Traumatic life events, abandonment, adversity, instability, invalidation, fear, distress, .. Whatever it may be, it has to last long enough to create a subconscious thought pattern.
The upside is, thought patterns can be corrected!

-Borderline Brooke
#borderline#borderline blog#borderline life#borderline personality disorder#borderline things#borderline personality traits#bpd risk factors#borderline personality problems#borderline feels#risk factors#mental health#borderline splitting#mental illness
1 note
·
View note