#cowden syndrome
Explore tagged Tumblr posts
Text
shout out to those of us chronically ill people who have stacks of rare diagnoses that took years or decades to dx. Shout out. to those of us in those categories who had earlier diagnoses questioned because of our other, at this point undiagnosed, rare illnesses.
To have a doctor look at something very concrete and telling of a certain diagnosis (for me, it was a muscle biopsy that showed a very obvious mitochondrial cytopathy) and go 'nah i don't think its actually this thing we have evidence of' because you also have another completely unrelated rare illness is gross and inexcusable.
If you are in this situation, i pray that things prevail for you. Remember that you know your body far better than any medical professional ever will, and that no matter what they say, you're not crazy for having inexplicable symptoms.
to deny the idea that someone can be doubly sick with three or more different rare illnesses when we know so little about genetics and all the different ways the human body can screw itself over is extremely and without a doubt idiotic. we all deserve better.
#chronic illness things#chronic illness#chronically ill#cripple punk#queer cripple#cripple posting#crip punk#mitochondrial cytopathy#mitochondrial disease#mast cell activation syndrome#MCAS#cowden syndrome
313 notes
·
View notes
Text

I'm not saying DID isn't bad or downplaying the severity, but stop calling it a rare disease.
#plural#syscourse#i guess#did#osdd#system#anti misinformation#plurality#rare diseases#pten hamartoma tumor syndrome#cowden syndrome#Bannayan–Riley–Ruvalcaba syndrome#Lhermitte–Duclos#look at me with my medically recognized large head and my 80% risk of breast cancer#and my lack of thyroid
15 notes
·
View notes
Text
An estimated 11,000 Ontarians have died while waiting for surgeries, MRIs and CT scans in the past year.
Jordanna Bialo, a 38-year old patient who became sick in October 2020, is one of many patients who are fearfully navigating the current healthcare system desperately searching for an answer.
“I’m medically burnt out. It’s a fight. I have a little son, he’s five years old, and I promised him I would be at his wedding,” said Bialo. “That’s why I fight – for my family. It’s a full time job. It’s a full time job to be a patient right now.”
It took three years for doctors to diagnose Bialo with a rare genetic tumour syndrome called Cowden syndrome.
Bialo is also waiting to receive a double mastectomy, which is minimum a year wait.
“I am full of these tumours that can turn any minute – it’s like Russian roulette and I just have to continue to keep pushing.” [...]
Continue Reading.
Tagging: @politicsofcanada, @vague-humanoid
65 notes
·
View notes
Text
Welcome
Hello! You can call me Jester or Shin. I'm the soulbonder/host of the Daydream Soulbond Group.
Since I've been seeing a bit more people discovering or considering that they might be a soulbonder (and since I am one myself), I decided to set this up.
You can send in asks about being a soulbonder or soulbond (soulbonding/soulbonder/soulbond culture is:)
We're always open for questions about soulbonding.
(DNI and details about mod below)
No sexism, racism, lgbt+phobia, or any other form of bigotry.
No pro-contact harmful paraphiles.
I'm uncomfortable with transids that are radqueer, and radqueers in general. You can still interact, but you're on thin ice.
Don't involve this account in endo/trauma discourse, or shipcourse. Or any discourse not related to soulbonding. There's intersection between plurality and soulbonding, but some soulbonders don't consider themselves plural. More rules will be added if needed.
I am a bodily minor, and have a diagnosis of ADHD and ASD (autism spectrum disorder). I fit the criteria for CPTSD. I have PTEN Hamartoma Tumor Syndrome, also known as cowden syndrome.
The two soulbonds who have expressed interest this blog are West Virginia, who will sign of as -WV, and Victor, who will sign off with his name. I will specify if anyone else wants to comment.
#soulbond#soulbonding#soulbonder#soulbonding culture is#pinned post#rules#intro#not soulbonding culture is
2 notes
·
View notes
Text
The more research I do into Wilson's cancer (stage II thymoma) the more confused I am
According to the national cancer institute the treatment for stages 1 and 2 are surgery .. then maybe radiation therapy after depending on the situation.
According to cancernet the 5 year survival rate when the cancer is located only in the thymus is 93%. If it's spread to surrounding tissue and organ the survival rate is still 79%. And if it's found only after spreading to distant parts of the body the survival rate is still 40%, on average much higher than say lung cancer that's still localized (which is 56%) while lung cancer that's spread to other organs has a 5 year rate of only 5(five!) %. (This is from the American lung association)
I just find it frustrating that of all the cancers they picked, they picked one that ... Won't kill him? At stage 2? And he didn't need to do chemotherapy he needed to just have surgery???
What's even more interesting is I was looking into this cancer trying to find a way to make it believable .. give them the benefit of the doubt. And I found a disorder called Cowden Syndrome which is very rare and causes the patient to have an increased risk of both benign and cancerous tumors in their life.
While the most common tumors are in the skin, mouth, and gastrointestinal tract, the patient has an increased risk for cancerous tumors in the thyroid, colorectum, breast, etc.
Now these growths would be noticed on any number of scans so I can only assume a whole body scan was the only way they got a diagnosis of such a rare (indeed very rare cancer for Wilson. A statistic I read on cancer net said that for every 1 million people in the US only 1.5 people will be diagnosed with this disease. Naturally the complete picture can never be known but that's an insanely specific cancer for Wilson to get !)
Anyway the only way I can justify him having such a small and specific cancer is to have him highly susceptible to tumors and therefore one grew there. By that logic maybe he got another one elsewhere and that was the real reason he was dying.
Not a doctor so if anythings inaccurate I apologize but I just spent a lot of time reading differential diagnoses for both thymomas and Cowden Syndrome and can honestly say as far as rare interesting disorders go, that would have been my choice. Fits very well with House's zebras not horses mentality that the cancer doctor would get a disorder specifically generating tumors throughout his whole life and maybe one just went somewhere deadly.
#hey look im posting another essay#this one is actually interesting...kinda ..it is to me#james wilson#house md#house season 8
18 notes
·
View notes
Text
6 notes
·
View notes
Text
“Cowden Syndrome”, Victor McKusick, Mendelian Inheritance in Man, 1966. 考登綜合症。(PIK3CA).
Here I present: “Cowden Syndrome”, Victor McKusick, Mendelian Inheritance in Man’, 1966. 考登綜合症。(PIK3CA). INTRODUCTION. Cowden syndrome is a hamartomatous disorder characterized by macrocephaly, facial trichilemmomas, acral keratoses, papillomatous papules, and an increased risk for the development of breast, thyroid, and endometrial carcinoma. While there is association with mutation in the…
0 notes
Text
Lipoma Causes, Symptoms, And Effective Prevention Methods
Lipoma is a common benign tumor that forms under the skin. It is composed of fat cells and can occur in any part of the body, but is most commonly found on the neck, shoulders, arms, and torso. Lipomas are non-cancerous and do not usually cause any harm, but they can be concerning due to their appearance and potential growth. There are different types of lipomas, such as superficial and deep-seated, which may vary in size and location. Lipomas are prevalent in the population, with about 1 in 100 people having them. Despite being harmless, addressing lipoma is important for overall health and wellness. In this article, we will provide a comprehensive understanding of lipoma, covering its causes, symptoms, diagnosis, treatment, and effective prevention methods.

There is no definitive answer to what causes lipoma, but research suggests that there may be a combination of genetic and environmental factors at play. Lipoma is more commonly seen in people with a family history of the condition. Hormonal imbalances and advancing age have also been linked to the development of lipoma.
Furthermore, certain underlying conditions such as adiposis dolorosa, Gardner syndrome, and Cowden syndrome have been associated with an increased risk of developing lipoma. It is important to note that these conditions are rare and not all individuals with lipoma will have an underlying condition.
While the exact cause of lipoma may not be known, it is important to monitor any suspicious lumps on the body and seek medical attention for proper Diagnosis and Treatment. Early detection and management can help prevent further growth and potential complications of lipoma.
Read more
1 note
·
View note
Text
Multiple Hamartoma Syndrome_Sound therapy session_Sounds of nature

Multiple Hamartoma Syndrome (MHS), also known as Cowden syndrome, is a rare genetic disorder characterized by the development of hamartomas in various parts of the body, including the skin, mucous membranes, and internal organs. As a complex condition with diverse manifestations, the management of MHS often involves a multidisciplinary approach, incorporating both conventional medical treatments and complementary therapies. In recent years, resonant frequency sound therapy has emerged as a promising adjunctive treatment for individuals with MHS, offering a unique approach to holistic wellness and symptom management. Resonant frequency sound therapy is based on the concept that every organ, tissue, and cell in the human body has a natural vibrational frequency. When these frequencies are in a state of harmony, the body is believed to be in a balanced and healthy condition. However, illness or disease is thought to manifest when these frequencies become disrupted. Resonant frequency sound therapy aims to restore the body's natural equilibrium by using specific sound frequencies to resonate with the affected areas, potentially promoting healing and overall well-being. When utilized as an adjunctive treatment for Multiple Hamartoma Syndrome in combination with conventional medicine, resonant frequency sound therapy offers several potential benefits: 1. Pain Management: Individuals with MHS may experience pain and discomfort due to the presence of hamartomas in various tissues. Resonant frequency sound therapy has been suggested to provide relief from pain by promoting relaxation and reducing muscle tension, potentially improving the overall quality of life for individuals living with MHS. 2. Stress Reduction: Living with a chronic condition such as MHS can be emotionally and mentally challenging. Resonant frequency sound therapy may help alleviate stress and anxiety, providing a sense of calm and mental clarity, which can be beneficial for individuals managing the complexities of their condition. 3. Immune System Support: Some proponents of resonant frequency sound therapy suggest that specific frequencies may stimulate the body's natural healing processes and support immune system function. For individuals with MHS, whose immune system may be impacted by the condition, this supportive effect could be particularly valuable. 4. Enhanced Well-being: Integrating resonant frequency sound therapy with conventional medical treatments for MHS can contribute to a more comprehensive approach to holistic well-being. By addressing the physical, emotional, and energetic aspects of health, individuals may experience an improved sense of overall wellness. It is important to note that while resonant frequency sound therapy shows promise as an adjunctive treatment for MHS, it is not intended to replace conventional medical interventions. Rather, it should be viewed as a complementary approach that can work in conjunction with traditional medical care to support the individual's health and well-being. In conclusion, resonant frequency sound therapy holds potential as an adjunctive treatment for Multiple Hamartoma Syndrome, offering a unique and holistic approach to managing the diverse symptoms associated with the condition. By integrating this complementary therapy with conventional medical care, individuals with MHS may have the opportunity to explore additional avenues for symptom relief, stress reduction, and overall well-being. TO ACHIEVE A POSITIVE RESULT, DAILY LISTENING TO VIDEOS IS REQUIRED. I wish you health and prosperity!
#ResonantFrequencySoundTherapy#MultipleHamartomaSyndrome#AdjunctiveTreatment#TraditionalMedicine#HealingFrequencies#HealthBenefits#IntegrativeMedicine#WellnessTherapy#HolisticHealing#MedicalSoundTherapy
0 notes
Text

The common types of hereditary cancer syndromes include:
1. Inherited Breast and Ovarian Cancer Syndrome (HBOC): HBOC primarily stems from mutations within the BRCA1 and BRCA2 genes. Females carrying these genetic alterations face notably heightened risks of breast and ovarian malignancies. Furthermore, BRCA mutations correlate with elevated susceptibilities to other cancers, such as prostate, pancreatic, and male breast cancer.
2. Lynch Syndrome (Hereditary Nonpolyposis Colorectal Cancer, HNPCC): Lynch syndrome arises from mutations affecting genes responsible for DNA mismatch repair, notably MLH1, MSH2, MSH6, and PMS2. Those with Lynch syndrome exhibit increased predispositions to colorectal cancer, alongside risks of endometrial, ovarian, gastric, and urinary tract cancers.
3. Familial Adenomatous Polyposis (FAP): FAP manifests with the proliferation of numerous polyps within the colon and rectum, which pose a cancer risk if untreated. Primarily linked to mutations in the APC gene, FAP substantially heightens the likelihood of early-onset colorectal cancer.
4. Li-Fraumeni Syndrome (LFS): LFS, a rare hereditary cancer syndrome, arises from mutations in the TP53 tumor suppressor gene. Individuals with LFS confront elevated lifetime risks of various cancers, including breast cancer, sarcomas, brain tumors, and adrenal gland tumors, often occurring at a young age.
5. Hereditary Diffuse Gastric Cancer (HDGC): HDGC entails an escalated susceptibility to diffuse gastric cancer, characterized by infiltration of the stomach wall. This predisposition predominantly results from mutations in the CDH1 gene, which encodes a protein crucial for cell adhesion.
6. Cowden Syndrome (CS): CS stems from mutations in the PTEN gene and is typified by multiple noncancerous hamartomas, alongside heightened risks of developing diverse cancers, such as breast, thyroid, and endometrial cancers.
7. Hereditary Retinoblastoma (RB1): Hereditary retinoblastoma arises from mutations in the RB1 gene, leading to the formation of cancerous tumors in the retina, typically emerging in early childhood.
8. Von Hippel-Lindau Syndrome (VHL): VHL arises from mutations in the VHL gene and is characterized by the development of tumors and cysts in various organs, including the kidneys, adrenal glands, pancreas, and central nervous system.
If you have a family history of cancer, you should undergo regular cancer screenings for the early detection and management of cancer. You can undergo a regular full body health checkup at Jaslok Hospital Mumbai, which is one of the best hospitals in Mumbai for cancer screening and treatment.
#cancer#hereditary cancer#hereditary cancer syndrome#Lynch syndrome#inherited breast and ovarian cancer syndrome#familial adenomatous polyposis#full body health checkup#regular health checkups#cancer screening#health checkup packages
0 notes
Text
PTEN Mutation and Breast Cancer
Phosphatase and Tensin Homolog (PTEN): Is a tumor suppressor gene, and inherited mutations in this gene can be associated with Cowden’s syndrome Cowden’s syndrome: Is associated with increased risk of multiple types of cancer including: Breast Endometrial Thyroid Colorectal Melanoma PTEN mutations carriers: Tend to develop cancers at younger ages than individuals with sporadic…

View On WordPress
0 notes
Text
maybe a hot take, maybe not? (i'm still new to the community i don't know where people stand.) but we in the chronic illness community need to remember that cancers are a group of (really fucking scary) chronic diseases, and people who are dealing with cancer are a part of our community who deserve a space.
i say this as someone who grew up angry at the way that cancer patients were treated (supposedly better than i was) until i took a step back and remembered seeing a friend of mine when i was little go through leukemia. she was very very sick, and although i did everything to stay clean and germ free for my own health, it was not enough to regularly visit her in a safe manner. the isolation i often felt, i know she felt too.
at fifteen i was diagnosed with cowden syndrome, a rare genetic disorder that not only makes me at higher risk for certain cancers but also makes it harder to combat those cancers. as of 2020 it took my left thyroid gland. but that's not the point here. i ended up going to the local childrens hospital, the cancer center my friend went to, and i saw lots of kids on some of their worst days. it breaks my heart just like it breaks my heart to know that there are kids growing up with other chronic illnesses.
i'm not mad at them anymore. i mean, for fucks sake why should i ever have been mad at them? no one chooses to have cancer. no one chooses have any chronic illness. there's so many other things, more awful things that need to be addressed, that anger should go towards. its a scary world for sick people, no matter the illness. all in all these are just my thoughts.
2 notes
·
View notes
Text
Zebrapunk

Zebrapunk: A punk term made by and for people with rare diseases and disabilities.
If you didn't know, the zebra is the mascot for people with rare diseases.
Doctors were told "When you hear hoofbeats, think horses, not zebras." To look for the more common answer.
Well, sometimes that's not the answer at all.
Zebras are here, and they're more common than you might think.
6 notes
·
View notes
Text
Is colorectal cancer hereditary?

Yes, colorectal cancer can have a hereditary component. Here's more information:
Colorectal cancer can be influenced by both genetic and environmental factors. While the majority of cases are sporadic, meaning they occur without a strong family history, about 5-10% of colorectal cancer cases are linked to inherited genetic mutations.
There are several hereditary syndromes that can increase the risk of developing colorectal cancer:
1. Lynch Syndrome (Hereditary Nonpolyposis Colorectal Cancer or HNPCC):
Lynch syndrome is the most common inherited cause of colorectal cancer. It is caused by mutations in certain genes that are responsible for DNA repair. People with Lynch syndrome have a significantly higher risk of developing colorectal cancer, as well as other types of cancer such as endometrial, ovarian, and stomach cancers.
2. Familial Adenomatous Polyposis (FAP):
FAP is characterized by the development of hundreds to thousands of polyps in the colon and rectum. If left untreated, these polyps can turn into cancer. FAP is caused by mutations in the APC gene. Individuals with FAP usually develop colorectal cancer at a younger age.
3. MYH-Associated Polyposis (MAP):
MAP is caused by mutations in the MYH gene. Similar to FAP, it leads to the development of multiple polyps in the colon and an increased risk of colorectal cancer.
4. Peutz-Jeghers Syndrome:
This syndrome is characterized by the development of polyps in the digestive tract and pigmented spots on the skin and mucous membranes. People with this syndrome have an increased risk of various cancers, including colorectal cancer.
5. Juvenile Polyposis Syndrome:
This rare syndrome causes the development of polyps in the digestive tract during childhood. While the risk of colorectal cancer is increased, it also elevates the risk of other types of cancer.
6. Other Syndromes:
There are several other rare hereditary syndromes that can increase the risk of colorectal cancer, such as MUTYH-associated polyposis (MAP), Cowden syndrome, and Gardner syndrome.
It's important to note that having a family history of colorectal cancer doesn't necessarily mean you will develop the disease, but it does increase your risk. If you have a family history of colorectal cancer or suspect a hereditary syndrome, it's advisable to consult a genetic counselor and discuss appropriate screening and prevention strategies. Regular screenings and early detection are crucial in managing the risk associated with hereditary forms of colorectal cancer.
For more information, Consult Dr. Chintamani Godbole as he provides the Best Colorectal Surgeon in Mumbai
#drchintamanigodbole
#colorectal surgeon in mumbai.
#colon cancer treatment in mumbai
0 notes
Text
Duodenal polyp a rare cause of repeated vomiting by Lahfidi Amal in Journal of Clinical and Medical Images, Case Reports

Clinical Image Description
A 50-year-old man without ATCD who suffers from dyspepsia and frequent vomiting, prompting him to seek medical help. There were no abnormalities found during the clinical evaluation. A CT scan of the abdomen was ordered to identify a duodenal polyp that was limiting the digestive light (Figure 1).
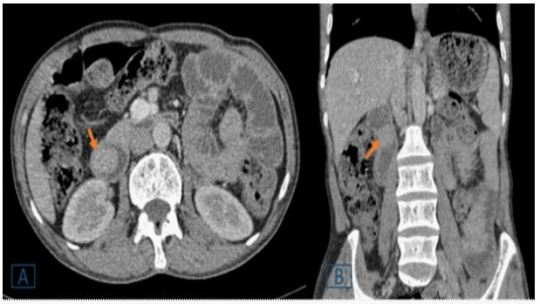
Figure 1: A duodenal endoluminal polyploid tissue process of 21 x 23 mm is shown on a transverse (A) and coronal (B) abdominal CT following contrast injection (orange arrow).
Peutz-Jeghers syndrome (PJS), juvenile polyposis, Cowden's disease, familial adenomatous polyposis, and Gardner's syndrome are polyposis syndromes that affect the duodenum [1]. Duodenal polyps are more common in children with polyposis syndromes, the majority of which are asymptomatic, according to a retrospective research in a pediatric population (aged 21 years) [2]. In the pediatric age group, duodenal polyps are seldom seen during standard high endoscopy (EGD) and radiographic investigations. In contrast, a recent study of adults using EGD and autopsy found a prevalence of up to 4.6 % [2]. Abdominal pain, vomiting, gastrointestinal bleeding, anemia, and intussusception or obstruction are among the symptoms [1, 2]. In comparison to the jejunum and ileum, duodenal disorders have received little attention in the imaging literature [1]. The exploration of the duodenum, which is still mostly examined by video endoscopy, has changed dramatically as a result of recent breakthroughs in imaging. However, advances in computed tomography (CT) and magnetic resonance imaging (MR) have made it easier to detect and characterize anomalies in the genesis of duodenal masses [1]. They are used to assess intraluminal content, the duodenum wall, and the extraduodenal area. The scanner, in combination with optimum intestinal distension and intravenous iodine contrast, provides for a thorough examination of the duodenum. Similarly, MRI has been demonstrated to be useful in diagnosing a wide spectrum of duodenal disorders when combined with duodenal distension and intravenous administration of a gadolinium-based contrast agent [1]. For the detection and characterization of a wide spectrum of duodenal lesions generating masses, CT remains the preferred imaging modality [1]. Large polyps (> 15 mm) might cause small intestinal blockage, thus it's important to keep an eye on them to see which ones need to be removed [1]. Protocols for monitoring are still being debated. Important polyps (big polyps with a proclivity for intussusception or blockage) are detected by endoscopy [1].
Surveillance in patients with polyposis syndromes was the most common reason for EGD; most of these patients were asymptomatic at the time of their EGD. In patients without polyposis syndrome, the most prevalent reason for EGD was stomach pain and vomiting [2]. CT and MRI can theoretically be used to monitor patients with many polyps and determine the best treatment, which could include endoscopic, enteroscopic, or surgical ablation, or a combination of these methods [1].
Competing Interests: The authors declare that they have no links of interest.
For more details : https://jcmimagescasereports.org/author-guidelines/
#ATCD#frequent vomiting#dyspepsia#abnormalities#Peutz-Jeghers syndrome#polyposis syndromes#gastrointestinal#EGD#Lahfidi Amal#JCMICR
0 notes
Text
What Is Thyroid Cancer? Symptoms, Diagnosis, And Treatment Options

Thyroid cancer isn’t that common, but it can still leave some traumatic imprints in the lives of those diagnosed with it. It is considered to be one of the ‘good cancers’ due to the fact that it responds well to therapy. Visit a top oncology hospital in Malleshwaram if you require treatment and care for thyroid cancer.
What Is Thyroid Cancer?
The butterfly-like gland right below Adam's apple is known as the thyroid, which produces hormones that is responsible for regulating a person’s metabolism, temperature, heart rate, and blood pressure. Thyroid cancer begins at the stage when the cells in the gland forget apoptosis (programmed cell death) and proliferate uncontrollably. It then leads to the development of a solid tumour, often pointed out as a nodule (mass/lump) at the base of one’s throat.
The formation of nodules or lumps in the thyroid is pretty common, especially in middle & old age. About 50% of the population above the age of 60 years can be diagnosed with a thyroid nodule. But, more than 90% of these nodules never turn into cancer. Children and young adults rarely develop thyroid nodules. However, when they do develop the nodules, there is a high probability of it turning out to be cancerous. Thyroid cancer is more commonly diagnosed in females than in males.
Different Types of Thyroid Cancer
Thyroid cancer is classified into four different types.
Papillary Thyroid Cancer
About 80-85% of all cases of thyroid cancer are of this type. This is also one of the most curable forms of cancer.
Follicular Thyroid Cancer
About 10-15% of all thyroid cancer cases can be diagnosed with follicular thyroid cancer. It is slightly more aggressive than papillary thyroid cancer. This type of thyroid cancer takes the help of the bloodstream to reach other body parts. A rare type of follicular thyroid cancer, called Hurthle cell cancer, is infamous for being very aggressive. Medullary thyroid cancer: less than 3% of the total population with thyroid cancer suffers from this type of thyroid cancer. Anaplastic thyroid cancer: This is the most dreadful type of thyroid cancer. Not only does it have a poor prognosis, but it also tends to resist chemotherapy with time. About 2% of all cases account for this type of cancer. It is the most aggressive type and invades the other body parts pretty quickly.
Causes and Symptoms of Thyroid Cancer
Thyroid cancer is rarely present with any symptoms. However, if the patient reports a symptom, it is mostly a swollen neck which is caused by the nodules. Although one may not point it out themselves, others might. As the nodule grows, the lump can be felt as a slight bump in front of the neck. When swelling becomes very large, the nodules become large enough to cause complications like shortness of breath, hoarseness, problems while swallowing and moving the head or neck, as well as a persistent cough. Pain is rarely present in patients with thyroid cancer.
Other Risk Factors of Thyroid Cancer
Exposure to radiation, especially during childhood, is one of the common causes that induce genetic mutations in people which can cause thyroid cancer.
People with a family history of thyroid cancer or other thyroid problems may also be at an increased risk.
Certain medical conditions, such as thyroiditis, multiple endocrine neoplasia syndrome, Cowden syndrome, and familial adenomatous polyposis, can increase the risk of developing thyroid cancer.
Common conditions like obesity or deficiency diseases like goitre can also cause thyroid cancer.
People undergoing radiation treatment for other medical conditions are also at an increased risk of developing thyroid cancer.
Diagnosis & Treatment Options for Thyroid Cancer
A fine-needle biopsy is often prescribed to confirm the presence of cancerous cells after an initial observation of thyroid glands by an oncologist. If the cells are indeed cancerous, planning for surgery will be done. Imaging techniques like CT scans or ultrasounds can help the surgeon to localize cancer and plan the surgery. Blood tests for TSH and calcitonin levels may also be required.
Surgery is usually preferred to cure small, isolated papillary, and follicular cancers. Radioactive iodine therapy and thyroid hormone replacement therapy are the treatment options commonly followed after surgery. If cancer is advanced or metastasized, radioactive iodine treatment is necessary.
Although thyroid cancer is considered one of the ‘good cancers’, proper care has to be taken for a quicker recovery. Many times people delay consulting an oncologist because they don’t develop any symptoms. Sadly, when the symptoms do manifest, it could be too late. Nevertheless, with early diagnosis, the prognosis for the patient with thyroid cancer could be greatly improved.
Consult a surgical oncologist in Malleshwaram for diagnosis and treatment of thyroid cancer.
0 notes