#Liver transplant recipients
Explore tagged Tumblr posts
Text
Analytical and Clinical Validation of a Novel Blood- Based Biomarker of Liver Transplant Rejection
Weems JC, Pierry D, Holman J, Kandpal M, Kurian SM, Meintjes P, Beswick N, and Levitsky J. "Analytical and Clinical Validation of a Novel Blood-Based Biomarker of Liver Transplant Rejection." J Transplant Technol Res 11 (2021): 180.
Abstract Background: We have discovered and validated a microarray-based test that analyzes blood gene expression profiles (GEP) as an indicator of immune status in liver transplant recipients with stable liver function. Methods: Analytical performance studies to characterize stability of RNA in blood during collection and shipment, analytical sensitivity (input RNA concentration), analytical specificity (interfering substances) and assay performance (clinical validity, and intra-assay, inter-assay, inter- laboratory reproducibility). Results: Total RNA extracted from whole blood specimens collected in PAXgene Blood RNA tubes was stable up to 3 days at room temperature (stable RNA yield). Under routine ambient shipping conditions, storage and shipping temperatures did not affect results. However, specimen shipments exposed to temperatures >400°C or to ambient temperatures for >3 days were unacceptable for processing. Analytical sensitivity studies demonstrated tolerance to variation in RNA input (50 to 400 ng per 3’ IVT (in vitro transcript] labeling reaction). Specificity studies using genomic Jurkat DNA spiked into 3 ’IVT reactions at 10-20% demonstrated negligible assay interference. The test was reproducible across operators, runs, reagent lots, and laboratories. External validation demonstrated that the TruGraf Liver blood test accurately classified patients in 84% of 155 samples. Conclusions: The previously published biomarker is the first non-invasive test to be demonstrated to have clinical utility in assessing immune status of LT recipients with stable liver function and shows promise as a reasonable and necessary tool supporting personalizing immunosuppressive therapy.
Submit manuscript at https://www.scholarscentral.org/submissions/transplantation-technologies-research.html or as an e-mail attachment to the Editorial Office at [email protected]
0 notes
Text




Recovery is really hard, but days like today make it all feel worth it.
3 notes
·
View notes
Text
Organ Transplant: Saving Lives Through Donation and Medical Advancement

The History of Organ Transplant
The first successful organ transplant took place in 1954 when a kidney was transplanted between identical twins in Boston. This groundbreaking surgery paved the way for other transplant procedures. Throughout the 1950s and 60s, doctors continued experimenting with kidney transplants with varying success rates due to the body's natural immune response. It wasn't until the 1980s that anti-rejection drugs like cyclosporine were developed, allowing transplants between non-related donors and recipients to become more widely performed and successful. Types of Transplants
Kidneys are the most commonly transplanted organs, with over 80,000 kidney transplants performed in the United States alone between 1988-2018 according to the Organ Procurement and Transplantation Network. Other organs that can be transplanted include the liver, heart, lungs, pancreas, intestine, and thymus gland. Tissue such as corneas, skin, bone marrow, heart valves, veins and ligaments can also be donated. Organ Donation
For a Organ Transplant to occur, a donor must first agree to donate their organs upon death. In the United States, individuals can register as organ donors through their state's department of motor vehicles or on the Organ Donor Registry. Family consent is also required before organs can be recovered. Once a donor is declared brain dead but their heart is still beating, doctors work to preserve the organs until they can be surgically removed and transplanted into recipients waiting for a life-saving gift. Waiting for an Organ
The need for donated organs far outweighs the available supply. As of January 2020, there were over 113,000 candidates on the U.S. national transplant waiting list according to the Organ Procurement and Transplantation Network. The waiting time for a donated organ varies depending on blood type, organ size match and medical urgency. On average, 20 people die each day from the lack of available organs. Children have a higher mortality rate while waiting, with nearly 5,000 children in need of a transplant. Advancements in Living Donation
While deceased donor transplants remain the standard, advancements have been made to increase living donation options. In kidney and portions of liver or lung donation, a healthy person can elect to donate an organ or parts of organs to recipients in need. The recipient's prognosis is often better when the donated organ is still functioning at the time of transplant rather than being recovered from a deceased donor. Some donors are emotionally motivated to help a loved one, while others choose to altruistically donate to a stranger. Either way, living donation has elevated many from waiting lists to restored health. The Future of 3D Bioprinting and Xenotransplantation
Scientists are exploring new frontiers to close the organ supply gap through bioprinting and cross-species transplantation possibilities. 3D bioprinting uses inkjet-like printers to deposit cells layer by layer, building functional organs. Researchers have printed heart tissue, liver buds and kidney structures, with the goal of fully printed transplantable organs in development. Meanwhile, some scientists are testing the use of organs from genetically-modified pigs, known as xenotransplantation. Pig heart valves and skin are already used as human transplants with promising research underway for whole organs. If effective, bioprinting and xenotransplantation could revolutionize transplant availability in coming decades. The Impact of a Transplant
For recipients who receive that lifesaving gift from a donor, organ transplantation means a second chance at life. Kidney transplant patients can discontinue dialysis treatments and greatly improve their quality of living without being tethered to a machine. Liver recipients are cured of end-stage liver disease and related conditions. Heart transplant patients are no longer constrained by heart failure.
lung transplants restore breathing abilities for people suffering from cystic fibrosis, COPD or pulmonary hypertension. The impact of organ donation should not be underestimated - for both recipients who receive more days with their families, and donors who give the ultimate gift so others may live on. Continued medical progress and donation awareness will help even more individuals overcome organ failure in the future.
Get more insights on Organ Transplant
About Author:
Money Singh is a seasoned content writer with over four years of experience in the market research sector. Her expertise spans various industries, including food and beverages, biotechnology, chemical and materials, defense and aerospace, consumer goods, etc. (https://www.linkedin.com/in/money-singh-590844163)
#Organ Transplant#Organ Donation#Transplant Surgery#Organ Recipient#Donor Organs#Kidney Transplant#Liver Transplant#Heart Transplant#Transplant Medicine
0 notes
Text
Organ Transplants and Mental Health: Coping with Emotional Challenges
Organ transplantation is a remarkable medical advancement that offers a lifeline to individuals suffering from organ failure. In a bustling metropolis like Mumbai, the demand for organ transplantation, particularly liver transplants, is rising. This life-saving procedure is physically demanding and poses significant emotional and psychological challenges. Coping with these emotional hurdles is a crucial aspect of the transplant journey. Thankfully, organizations, including NGOs helping with liver transplants, play a pivotal role in providing support, information, and resources to help individuals navigate the emotional complexities of organ transplantation.
The Emotional Journey of Organ Transplant Recipients
For individuals awaiting organ transplantation, the emotional toll can be significant. They often grapple with various emotions, including anxiety, fear, and anticipation. The uncertainty of when a suitable organ will become available and the life-or-death nature of the procedure can lead to profound stress.

The Role of Mental Health in Transplantation
Mental health is a crucial aspect of the transplant journey. The stress and emotional upheaval associated with organ transplantation can impact a person’s overall well-being and physical recovery. Anxiety and depression, if left unaddressed, can hinder the body’s ability to heal and adapt to the new organ.
In this context, the support of NGOs helping with liver transplants in Mumbai and similar organizations across the world becomes invaluable. These NGOs often have mental health professionals and support networks that offer recipients a safe space to express their emotions, share their experiences, and access counselling services.
The Power of Support Networks
Support networks are lifelines for organ transplant recipients. They provide a sense of belonging and understanding that is vital during this journey. Whether connecting with other recipients who have faced similar emotional struggles or relying on friends and family for support, these networks can help individuals feel less isolated.
NGOs focused on organ transplantation often organize support groups where recipients can share their stories and insights. Hearing from others who have walked a similar path can be immensely reassuring. These organizations also offer resources on mental health, including coping strategies and tools to manage stress and anxiety.
The Role of NGOs in Supporting Mental Health
NGOs helping with liver transplants in Mumbai and other major cities in India and worldwide are dedicated to providing comprehensive support to transplant recipients. They recognize that the emotional journey is as critical as the physical one.
These organizations offer:
Counselling Services: Many NGOs have trained mental health professionals who specialize in working with transplant recipients. They provide one-on-one counselling and group therapy sessions to address emotional challenges.
Educational Resources: NGOs offer information and educational materials on mental health, organ transplantation, and the recovery process. This knowledge empowers recipients to understand better and manage their emotional well-being.
Support Groups: Support groups create a sense of community. They allow recipients to connect, share experiences, and receive emotional support from their peers.
Advocacy: NGOs often advocate for policies and practices that promote transplant recipients’ mental and emotional well-being. They work to reduce stigmas surrounding mental health issues in the context of transplantation.
Access to Financial and Social Services: Some organizations offer assistance with financial and social challenges, as these can be additional stressors for transplant recipients.
Conclusion
Organ transplantation is a journey that extends beyond the operating room. The emotional challenges that recipients face can be profound and impactful. However, with the support of organizations like NGOs helping with liver transplants in Mumbai and elsewhere, individuals can access the resources, counselling, and communities that help them navigate the emotional complexities of this life-changing experience.
Mental health support is an integral part of the transplantation process, and these organizations play a crucial role in ensuring that recipients receive the comprehensive care they need to cope with the emotional challenges, heal, and embrace their second chance at life.
#organ donor#organ donation#organ transplant#transplant organization#organ transplantation#liver transplants in Mumbai#organ transplant recipients
0 notes
Text

The treatments for liver transplant rejection include the following:
1. General Immunosuppression: Liver transplant recipients receive a standard immunosuppressive regimen, including drugs like tacrolimus, mycophenolate mofetil, and prednisone, to suppress the immune system and prevent rejection.
2. Treatment of Acute Cellular Rejection:
a. Increased Immunosuppression: Adjusting the dosage or frequency of medications or adding new agents can address mild cases.
b. Steroid Bolus Therapy: Intravenous high-dose corticosteroids dampen the immune response in moderate to severe rejection.
c. Antilymphocyte Agents: Drugs like antithymocyte globulin or monoclonal antibodies target specific immune cells when steroid therapy fails.
3. Treatment of Chronic Rejection:
a. Optimization of Immunosuppression: Modifying the immunosuppressive regimen, including adjusting medication dosage and combinations.
b. Introduction of Novel Therapies: Considering newer agents like mTOR inhibitors to slow fibrosis and progression.
c. Supportive Care: Implementing dietary changes, managing complications, and monitoring liver function due to chronic rejection leading to liver failure.
4. Antibody-Mediated Rejection: Managing rejection caused by donor-specific antibodies using plasmapheresis, immunoglobulin therapy, rituximab, or bortezomib.
5. Transplant Rejection Prevention: Monitoring drug levels, regular follow-ups, adhering to medication schedules, addressing risk factors such as HLA mismatch, blood type incompatibility, and viral infections.
6. Future Directions in Rejection Treatment:
a. Tolerance Induction: Research on inducing immune tolerance to eliminate lifelong immunosuppression.
b. Biomarkers: Identifying reliable biomarkers for early rejection detection and personalized treatment.
c. Immune Modulation: Exploring selective immunomodulatory therapies to target the immune response while reducing complications.
d. Cellular Therapies: Investigating regulatory T cells or mesenchymal stem cells as potential treatments for immune modulation and tolerance promotion in liver transplant recipients.
Hospitals like Apollo Navi Mumbai Hospital are well-equipped with good doctors and hospitals to handle liver transplant rejection cases. The cost of liver transplant in Mumbai and the subsequent cost of treating liver transplant rejection will vary depending on several factors like the health condition of the patient, the type of liver transplant performed, etc.
#liver transplant#liver failure#liver damage#liver disease#donor#liver transplant recipient#liver transplant donor#liver cancer
0 notes
Text










IDK that I've ever put it in one post before, but here's the transplant speedrun.
1 - Valentines day 2021, he's admitted to the hospital. We take a pre-hospital selfie then I shave his head and he shaves his beard because he doesn't want to deal with hair at the hospital. Me and his mom drop him off; at that point you can only visit someone as they are actually dying and we're told that he's going to stay in the hospital until he gets a transplant or he dies, and if he's rejected as a transplant recipient he'll receive palliative care in this hospital.
2 - First week of March, they allow patients to have one screened visitor; this is our first visit - I take photos in the hospital to show his mom because at this point he has a pump in his shoulder and it is difficult for him to move his arms to use his phone. He has also been confined to a bed since the week he arrived because he's on the ECMO machine, so he can't walk or move around, though they stand him up every once in a while. At one point one of the ecmo tubes pulls out of his femoral artery, which is Not! Great! He also needed a blood transfusion about every two days at that point, which worried the doctors because it increased his likelihood of rejecting. But he had been approved for transplant at that point!
The first thing he said to me on this visit was "look, I have abs" and then he showed me his abs because it turns out when you're really really dying of heart failure your body begins to eat itself.
3 - Now That's What I Call Jaundice (cardiac cirrhosis is liver failure as a result of heart failure and it's pretty much the big giant neon flashing sign of heart failure that says "hey you're fucking dying" so if you've got heart failure and your bilirubin number is off or the whites of your eyes are yellow please kick up a gigantic stink until they check your liver; large bastard's GP, who is my doctor, who I hate, saw his bloodwork with a very high bilirubin number a month before he was diagnosed with cardiac cirrhosis and wrote it off as a testing fluke fuck that guy)
4 - Don't let the sad face fool you, he's acting pathetic so that his mom will stop yelling about the fact that I'm bringing him cookies. He's allowed to have cookies. At that point he weighed 98kg and was outsourcing his heartbeat, he was allowed to eat whatever he wanted. (have i mentioned that I was moving us from Vegas to LA at this time? I was bringing him cookies because I'd baked hundreds of peanut butter cookies and other cookies to use up the flour, sugar, and peanut butter in the vegas house)
5 - Mid-march, he's got a match! He called me when I was in Vegas filling up the truck with another load and I drove right back and to the hospital. Once he went in for surgery I drove to his mom's house and crashed, then woke up and drove to our storage unit and unpacked the truck while I waited to hear from the doctors. I was unloading a bookcase when I got the call. (There wasn't any point in waiting alone in the hospital for sixteen hours; either he was going to make it or he wasn't and someone was going to have to unload the truck at some point. People have been weird about this, like I should have been sitting at his side all the time, but there was a two-hour daily limit for most visits and look i have sat in a waiting room while this dude had a thirteen hour surgery i do not need a repeat of that experience without the soothing balm of nicotine getting me through it; so unloading a truck it was)
6 - Two days after surgery and kind of mad about it. His chest hurt a lot (obviously) but, like, a lot a lot because they'd had to open him up for the bypass just two years earlier.
7 - First walk outside of his room after transplant in early April; he needed a LOT of PT because of how much muscle he'd lost. He lost sixty pounds in the hospital before the surgery, and only gained back about twenty while he was in there.
8 - A visit from the tiny doggo
9 - I come to visit and I've got a new phone with a portrait mode so he steals it and takes stupid pictures for a few minutes. Dude is bored and restless; this is in late april and he's feeling well enough to be moody. ETA: There is a jar of pickles in front of him because he'd been fluid limited for a long time and his salt levels were off and when he got to the hospital they were like "you need electrolytes and a lot of salt" and he was like "sweetheart can you please please please bring me delicious salty things" so I was bringing him jars of pickled mushrooms and garlic stuffed olives and just a huge number of pickles that he kept trying to share with the nurses. "Alli brought the mushrooms again; would you like a pickled mushroom? I have fancy toothpicks to share them with!"
10 - He comes home for the first time in early May; he ends up getting readmitted two more times because of complications before finally being released in early July. ETA: The second time he got readmitted it was for something that he wasn't at all worried about but that they needed to monitor for a couple weeks so he was *SO BORED* and actually feeling pretty okay; so at one point when I was leaving the parking garage at 8pm my car wouldn't start, I did some troubleshooting with the manual and the internet and didn't figure it out, so I called him and he tried to troubleshoot over the phone and got frustrated and was begging his nurses to let him come out to the parking structure to work on my car (they refused) - I ended up getting a tow and fixing it when I replaced the battery terminals.
Photos are all posted with his permission.
Also I dyed my hair purple between photos one and two because it's his favorite color. I also bought a blue dress, red tights, and yellow shoes to wear to visit him because he always teases me for wearing so much black.
I just love him a lot. It was a hard couple years there, but things are getting better.
430 notes
·
View notes
Text
Centaur anatomy notes which I might turn into diagrams (courtesy of me in 2023)
The air flow is one-way, in the nose and out the mouth, the main body lungs do the most work and the human torso lungs work to strip out the last % of oxygen, so they are actually engaged on the lower chest exhale which passes air back out through the human lungs and mouth. In times of exertion they can inhale and exhale simultaneously using their two sets of intercostal muscles. Even non-athletic centaurs have very high endurance and good breath control. lower respiratory tract infections are extremely dangerous as are any conditions that might partially occlude the airway (like a common cold), so pulmonary health is very important to centaurs
cardiac system is similarly duplicated, there's a big barrel heart and a smaller human chest heart which aids in the circulation of blood from the upper lungs. the human half heart and lungs are larger than their equivalents in humans because the alimentary canal is not duplicated, so there's lots of free real estate in there (i.e past the human half diaphragm there's no stomach, liver, etc, those are all in the animal half)
a centaur can survive their upper-body heart and lungs ceasing to function (by trauma, disease, etc) but not the reverse. in the modern era, it is actually possible for a centaur to give a(n upper) heart transplant and survive but they would experience reduced quality of life as a result (having low tolerance to physical exertion). however it is an option for recipients whose lower heart has reduced function as this is life threatening
diet is determined by animal type. ungulates are nearly all vegetarians, they need a specialised diet high in cellulose and enough roughage to save them from getting painful ulcers. they drink spirulina water and consume specially-formulated hay/grass/etc products. they could eat a handful of plain grass if they wanted but there's not much flavour in that. grazers eat as many as six or seven small meals a day, carnivores would eat one or two.
the babies are all altricial like human babies. this means ungulates are born with their lower halves less developed than their newborn animal equivalents and can't walk for the first few months of life (coordinating six limbs is tricky). human chest handles the lactation as it's easier to cradle a baby there. i know we were all dying to know
flexibility is pretty good as previously mentioned but it does vary by species. the big cats can even climb ladders and have an easier time living in conventional housing
an ungulate centaur has two ways of lying down; sternal recumbency and lateral recumbency. in sternal recumbency the human half is held upright, in lateral, that's the full 'passed out' lying on ur side experience, and lateral recumbency is required for REM sleep. beds consist of thick pads or bedding (straw etc) and are usually ground-level. REM sleep time varies for animal type, for horses they'll need about 2 hours of it every day. they can nap and sleep shallowly while standing up. too much time spent lying down is bad for circulation as weight on hooves is actually a part of the circulatory system in horses, so they will spend most of their time standing to avoid issues with venous drainage. where a centaur is injured, a full body sling (suspended from a wheeled frame usually) can help them keep as much weight on their hooves as possible while also supporting them.
spinal injuries are very common in centaurs for obvious reasons, particularly torsion or compression fractures to the acute spine, which is the junction between the upper and lower body. this area is heavily reinforced and incorporates a structure similar to the stay structure in a horse's leg, which makes supporting the upright torso effortless. but all the reinforcement in the world won't stop nearly every centaur getting a sore back in their later years. ruptured discs are extremely common. in modern times, many would have brace implants fitted there. because there's more than just the torso's own muscles supporting it, it's easy for a centaur to hold their torso in what might seem like a high-effort position to humans (i.e not just upright)
78 notes
·
View notes
Text
XF OctoberFicFest Day 2: Hell Money
There were cases that made her painfully aware of her middle-class upbringing, her sheltered existence. As a Navy brat, she’d imagined herself on the edges in some ways. They’d moved often enough to give her a permanent sense of slight displacement. She’d seen the world. She understood the import of her father’s work. There was always a chance, however slim, that he would come home in a coffin. But she couldn’t imagine a situation where her parents were desperate enough to be sold off for parts. They had safety nets. Her family’s immigration stories felt like fairytales: once upon a time. They had integrated beyond the vulnerability of Mr. Lo or Mr. Li.
Her father’s blue eyes. Her mother’s warm heart. It hurt to imagine these things, though her parents were organ donors. Her father’s heart hadn’t been suitable for transplant, but his liver, his kidneys, his eyes did live on. She’d seen the letters from the recipients.
Still, there was a difference. Her father had offered up these things willingly, and he had had no more use for them. These victims hadn’t. Their parts had been stolen from them. The game they played wasn’t winnable. The stakes were punishing; the false hope was cruel.
This wasn’t her world. It was clearly marked Keep Out. She didn’t understand the language or the culture. She couldn’t recognize the medicines in the apothecary shop, despite her years of training. She and Mulder were too visible, too other. The perpetrators saw this as a private matter. The federal government had jurisdiction over Chinatown, but no authority. She and Mulder could leave no lasting impression on the situation. She tried to focus on the remedies she could administer: some measure of protection for Mr. Hsin and his daughter.
She felt for Chao. He saw himself as a bridge, neither one thing nor the other, rejected by both societies in which he participated. He was lucky: he spoke his family’s language, he could navigate the streets of Chinatown. But she saw how he was shut out. She understood it, a little, as a woman in physics, a woman in medicine, a woman in the FBI. She never entirely belonged with anybody but Mulder. Even in the moments she was embraced, she was aware the acceptance was contingent on her correct behavior. Like Chao, she could prove herself over and over and it would never really matter. She would be caught between her own loyalties, her own proficiencies and those others imagined for her. Trusted by no one.
She hoped, wherever he was, Chao had found some kind of satisfaction. Her investigator’s mind knew he hadn’t. His rest would not be peaceful. His house would be haunted, marked and sealed as a warning.
28 notes
·
View notes
Text
On a recent Thursday afternoon, researchers Lanuza Faccioli and Zhiping Hu wheeled an inconspicuous black and white plastic cooler from an operating room at a hospital in downtown Pittsburgh. Inside was a badly scarred liver, just removed from a 47-year-old man undergoing a transplant to receive a new one from a donor.
But what if patients could avoid that fate? Faccioli and Hu are part of a University of Pittsburgh team led by Alejandro Soto-Gutiérrez attempting to revive badly damaged livers like these—as well as kidneys, hearts, and lungs. Using messenger RNA, the same technology used in some of the Covid-19 vaccines, they’re aiming to reprogram terminally ill organs to be fit and functioning again. With donor livers in short supply, they think mRNA could one day provide an alternative to transplants. The team plans to begin a clinical trial next year to test the idea in people with end-stage liver disease.
Alcohol use, hepatitis infection, and a buildup of fat in the liver can cause scarring over time. When there’s too much damage, the liver starts to fail. “Right now, if you get end-stage liver disease, it’s irreversible,” Soto-Gutiérrez says. “Well, we found that is not true. It is reversible.”
Soto-Gutiérrez and his team have been experimenting on rats and organs taken from people undergoing transplants at the University of Pittsburgh Medical Center, one of the busiest transplant centers in the US. To help design the mRNA and figure out how to deliver it to the human liver, they’ve partnered with Drew Weissman, a physician and immunologist at the University of Pennsylvania who won the 2023 Nobel Prize in Physiology or Medicine for his pioneering work on mRNA. Together, Soto-Gutiérrez and Weissman lead the Center for Transcriptional Medicine, launched in April with the goal of bringing these medicines to patients.
On the day I visited, I followed Faccioli and Hu through a maze of hallways until they deposited the freshly explanted liver at a pathology lab, where a team of scientists was anticipating the special delivery. After infusing the liver with an experimental mRNA therapy, they placed the organ in an oxygenated bath meant to maintain its function for several days.
A healthy liver is spongy and reddish-brown in color with a smooth appearance. But when the surgeons took this one out of the cooler, it was hard, marbled, and covered in bumps—evidence of cirrhosis, a type of end-stage liver disease. Over time, the man’s healthy liver cells had been replaced by scar tissue, and eventually, his liver stopped working. His only option was to get a new one.
Livers are the second most in-demand organ. In 2023, a record 10,660 liver transplants were performed in the US, driven in part by a steadily growing number of living donors. In a living liver transplant, a piece is taken from a healthy person’s liver and transplanted into a recipient. But even with this uptick in transplants, not everyone who needs a new liver receives one. Patients may have other health problems that disqualify them from a transplant, and others may die while waiting for one. In 2022, the latest year for which data is available, the Centers for Disease Control and Prevention recorded nearly 55,000 deaths due to chronic liver disease.
Living donor transplants are possible because of the liver’s unique capacity to regenerate itself—more so than any other organ in the body. In a healthy person, the liver can regrow to its normal size even after up to 90 percent of it has been removed. But disease and lifestyle factors can cause permanent damage, rendering the liver unable to repair itself.
When Soto-Gutiérrez was studying medicine at the University of Guadalajara in Mexico, his uncle died of liver disease. From then on, he became dedicated to finding a treatment for patients like his uncle. In the early years of his medical career, he noticed that some patients with scarred livers were bound to a hospital bed waiting for a transplant, while other people with cirrhosis were walking around, seemingly living normal lives. He figured there must be cellular differences in these livers.
He teamed up with UPMC transplant surgeon Ira Fox to look for transcription factors—master regulators that can dial up or down the expression of groups of genes—that can potentially reprogram injured organs. Genes rely on transcription factors to perform many essential functions in organs. Together, Soto-Gutiérrez and Fox have analyzed more than 400 failing livers donated by transplant patients. When they compared them with dozens of normal donated livers that acted as controls, they identified eight transcription factors essential for organ development and function.
They zeroed in on one in particular, HNF4 alpha, that seems to act like a main control panel, regulating much of the gene expression in liver cells. In healthy liver cells, levels of HNF4 alpha were turned up, and so were other proteins it controls. But in the cirrhotic livers they examined, HNF4 alpha was almost nonexistent.
The team needed a way to get the transcription factor into liver cells, so they turned to mRNA technology. Used in some of the Covid-19 vaccines, mRNA is a molecule that carries instructions for making proteins, including transcription factors. In the Covid vaccines, the mRNA codes for a part of the virus known as the spike protein. When injected into a person’s arm, the mRNA enters cells and kicks off the protein-making process. The body recognizes these spike proteins as foreign and generates antibodies and other defenders against it.
The Pitt team is using mRNA instead to essentially turn back time in injured organs. “What we’re proposing to do with mRNA is use it to deliver proteins that have the capacity to repair those damaged liver cells,” Weissman says. “Our hope is that we can treat end-stage liver disease and turn the livers around, maybe forever, or at least until patients can get a transplanted organ liver.” Instead of delivering instructions for a foreign protein to generate an immune response, they’re delivering the genetic code for producing a transcription factor—HNF4 alpha.
In a paper published in 2021, the approach revived human liver cells in lab dishes. The researchers have since tested the mRNA therapy in rats with cirrhosis and liver failure. They treated a group of rats every three days for three weeks while a second group served as a control. The animals that were receiving the injection of HNF4 alpha started being more active. The untreated rats continued to decline and eventually died, the expected result at their stage of disease. Some of the treated rats were still living six weeks after receiving the mRNA medicine. Those results have not yet been published in a peer reviewed journal.
The team is also testing the mRNA infusions in human livers removed from patients undergoing transplants—the process I got to observe. Unlike live rats, explanted human livers can’t be observed for weeks on end. Livers have to be retrieved quickly and infused with the mRNA treatment soon after they’re removed from the body. They stay fresh for just four days or so in a preservation fluid. Six hours after the mRNA infusion, levels of HNF4 alpha start going up and last for two to three days. When HNF4 alpha peaks, other essential liver proteins, such as albumin, start to increase as well. That’s important, Soto-Gutiérrez says, because maintaining those protein levels could mean the difference between a patient needing a transplant or not.
Ideally, Soto-Gutiérrez says the mRNA therapy would be something patients could get once a week or every other week in an outpatient facility and go back home. But initially, they’ll need to test the experimental treatment in very sick patients, likely ones that are hospitalized, to make sure it’s safe. The team is gathering data from the rat and human liver experiments to submit a clinical trial application to the Food and Drug Administration in the coming months.
While livers are the first target, Fox thinks other injured organs may be amenable to this approach. “We’ve been wondering whether the same process might be taking place in other organs,” he says. Currently, the team is searching for similar transcription factors in lungs with chronic obstructive pulmonary disease and kidneys with chronic kidney disease.
Josh Levitsky, a liver transplant specialist at Northwestern University who isn’t involved in the work, says new treatments for chronic liver disease are sorely needed. Current therapies can help slow down scar tissue buildup and ease symptoms but don’t address the underlying disease. “The concept of reprogramming and being able to reverse liver failure could be really game changing if it were to pan out in clinical studies,” he says.
But lots of questions remain. How much damage could be reversed? Would patients need to be on the therapy indefinitely? Or would their livers rebound enough to go off it? Could a liver ever be restored back to normal?
“It certainly has a lot of promise,” Levitsky says, “but the clinical development is going to take a long time.”
20 notes
·
View notes
Text
I just did the hardest thing in my life.
Now I'm not sure how to go about talking about something like this.... i'm not all here mentally so just bear with me.... TW: Death, passing of a loved one, and organ donation. self harm mentioned.
I'm in Louisiana… Got here yesterday, everything feels like a blur… yet it feels like it's moving in slow motion���. It feels really good to see my stepmom, and stepsibs and my half brother Bear who came down to Louisiana JUST for me. Bear and our dad didn't really have a relationship, not the way I did with our dad. But Bear came down from Minnesota for me..... and I'm truly grateful for that.
My dad was legally pronounced brain dead on September 3rd 2024. Yesterday, September 4th, 2024. He had his Hero Walk from his ICU room to the ambulance bay…. i feel… I dont know… I've only ever have seen that on like med dramas before.. ya know? There's a place out here were they take him to handle as they put it "His gifts". Because he was an organ donor… I'm so proud of him for that Oh my gods I'm so proud of him for that…. but that walk… seeing all those doctors and nurses staff. some of who are my step moms co workers… it was the hardest thing i have ever done/ had been a part of in my life…. there is already a recipient of his liver. My dad is going to save someone else's life….. (we just got a call from the place that he went to, they were able to recover his liver, and two other things for transplants!!! THREE THINGS. MY dad is helping three different people!!!!)
Before we did the Hero Walk, Bear got to hang up a flag in honor of our dad. which was flown at half mast at the hospital. He's keeping the flag. Yesterday I had the honor of recording his heartbeat, and it's on my phone. I haven't listened to it since recording it.... I'm scared too, but I know that I wanna save up to get a Seattle Seahawks bear from Build a bear and put his heartbeat in that. I know it's going to kill me everytime I play it, but I think it'll also help???? the jury is still out.. lol
THe hero's walk was so surreal.... seeing that in real life.... I...I don't know how to process it... the doctors, nurses, and staff lined the hallways from the ICU to the ambulance bay.... it was so quiet, and I was sobbing the entire time walking behind my dad. He really is a hero... and my respect for him grew. I already had so so much respect for him. But wow.... The hero's walk was up til today, something I only saw on med dramas.... it felt so heavy, every single one of those people in those hallways had such a heavy look of respect and admiration for my dad. I feel like I'm shock kinda.... just a lot going on my head I cant keep things straight tbh...
Everyone has been a mess, but I think my stepmom and I take the cake on being a mess. (She doesn't have Tumblr, and none of my other family do so i'm not worried about them seeing this heh...) I have been dissociating a lot... I think... been blasting Sleep Token a lot to deal with this.... I never thought that my dad would be gone so soon... It's weird sitting in his chair writing this, knowing that he would usually never let anyone else sit in it... I have moments of hearing his voice when it's completely silent.... it's a sound that I will never forget, and his deep belly laugh when you would get him rolling.... his smile... Gods... I don't know how to feel.... it's weird to be here without him.... I wouldn't be sober if it wasn't for my dad, yeah I made the choice to get sober, but he helped me. He let me scream, cry, vent.... I didn't go to rehab, I literally detoxed on a greyhound bus on my way to Ohio. but when I got to Ohio. My dad was a Video call away, and I called him a lot. He didn't care about my ramblings, or the fact that I can never stay on topic.... he did the same thing.
We are cremating him, and having a wake for him with a viewing... which is going to be really hard for me honestly. After seeing him in the ICU.... but I think it'll be nice. and by cremating him. I'll be able to always have a little piece of him with me always. I just need to find something for his ashes, something that means something to both of us. Just us. I don't know where to even start... I'm not gonna be able to do anything until next month anyway...... I honestly feel so lost right now.... I keep thinking who am I gonna call. and my first thought is my dad....
I can't call him, and it hurts so much. But I know he isn't in pain anymore. He's with his dad, and grandpa. He's with my grandma, and aunts who loved him. But.... I feel lost... my heart hurts so much... I know that I'll learn to cope, and with a lot of time. It will get easier, but it doesn't feel like it. It really doesn't...
there is a GoFundMe going... i can get it from my stepmom if anyone wants it.. it was set up by a family friend.. just dm me I guess. i'll answer DMS but that's really it.

Me and my dad in 2019 in Idaho

This picture of my dad, I'm not sure when it was taken, but he looks so cool.
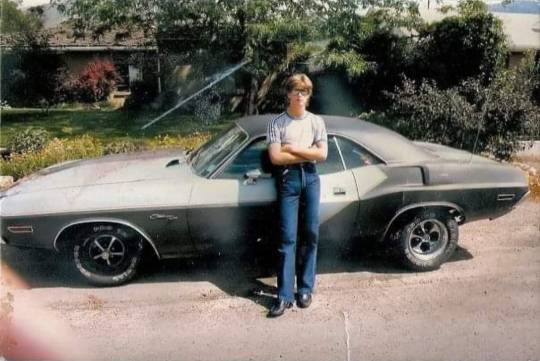
My dad when he was about 17 or so and his Mopar, this is my absolutely favorite picture of him. Picture courtesy of my Uncle Floyd on Facebook hehe.



Then these are pictures of his flag, the first three I took from the parking lot of the hospital. the last one my brother Bear took. I'm gonna post more photos of my dad. My Uncle Floyd, his brother is sending me a lot, and my stepmom and I are going through his facebook page and shes telling me stories about some of them. While going through some of his stuff... I know its soon.... but honestly... I'm keeping a lot of it. IDK where I'm putting it. But so far its mainly clothes, and stuff me and TJ one of my partners can wear. Might give my other partner a shirt if they'd like....
My dad is a hero, and is going to be saving someone's life tonight with the gift of his liver. I am so proud to be his daughter, but at the same time I am so hurt that he's gone. A small piece of him is going to live on with somebody else, whoever that is. I know they will be grateful for this, and that makes me happy. so happy, my dad loved helping people. So he is very much a super hero in my eyes.
Fly high daddy. I love you so much. You are saving one more life tonight, and I am so proud of you. So very proud to be your daughter, thank you for being my dad and one of my best friends. Even if you said that we weren't. I feel in my heart of hearts we were, I will never stop thinking about you. Or what you would do, or say. what jokes you would make, or how you say them. I love you so so much. I know you will be watching over us from now on, and that you wouldn't want me crying. But dammit dad... you know how I am... I can't help it... It's going to take a while before I can think of talk about you with crying. and you know it. you were always my hero for many reasons....
Do you know how hard it is going to be for me? Not being able to call you? Not being able to excitedly chitter to you about small things like my crystals or tarot cards? or...or calling you crying because I don't feel good or I have cramps and you make me feel better by making me laugh?? I know you know... I get the concept. heh.. But...I guess something is coming from it. I'm getting to know my Uncle Floyd better... He misses you a lot dad, Floyd loves you so much. He's sending me all of these really neat pictures of you guys... and he was making me laugh. Explaining the difference between having a mullet, and having long hair with bangs... lol
Floyd has been checking in on me and everyone almost daily, I haven't talked to him this much ever... which, yeah I know I can't take all the blame. He even said so.... You know you two are so much alike its kinda scary. heh. He called me princess the other day while I was on greyhound. I don't think he was thinking about it to be honest. He's been calling me kiddo a lot, kinda like you did. I think its cute. hehehe. But I think sadly this was the push I needed to connect with him more... He also has a really nice voice, just like yours. And the push I needed to connect with Kim more too.
I know that because of my mom, my relationship with Kim has been kinda weird. But I'm realizing that... some information was revealed and more clarified to me about certain happenings with my mom and wellll.... let's just say there are A LOT of emotions right now with that... I don't even know where to begin on that.... woooboyyyy dad... there's a lot to unpack there... and I know we've kinda touched on this crap here and there and really talked about things from your point of view. But Kim told me stuffs that.... Well I'm gonna need to talk to my therapist about it first because I really don't know how to process it. Because it was during the time I was treating you so horribly.... and I'm sorry... I didn't fully know or understand what was going on. I know I know I don't have to apologize for anything I know. But knowing this new information..... I'm sorry..... I'm so sorry. Ok i'm gonna try not to say that anymore. TRY.
I'm taking a lot of your clothes to be honest, oh and Ace is like my best friend now. Look! HE HUGE DAD HOLY FUCK


As soon as I started talking to Floyd Ace came out and started loving on me. I love him so much dad, he's so soft and sweet oh my gosh. But he misses you. He's definitely your cat lol for sure your cat. Everytime attacks Kim I giggle I can't help it. it's so funny, Tucker and Flash miss you too. Tucker has been so happy to see me. I love those dogs so much. I'm so happy to see them, and cuddle with them!!!! it's been so nice to be writing this and being able to set this aside to love on one of them for a minute. It's also been nice to spend time with Bear, We hung out a little yesterday.
He needed to run to Walmart, I tagged along cause well I wanted to go for a car ride. and I wanted to spend time with him too. He did drive all the way down here for me.... and yeah I know. I'm just glad he's here, he's getting some kind of closure with all of this... I know I've always been kinda like the fixer.. always trying to fix things... like relationships. like with my mom and Kim.
I now understand what was really going on... and I...I can't fix that. I can't, I have my own shit I need to worry about dad... like how i'm gonna live without you.... how am I going to do that?? I know I have TJ and Fruits... Kim, Bear, Floyd... Yes I've been constantly talking to TJ. I've been keeping him updated every step of the way....
But not you.... goddammit dad..... I know I'm going to be ok eventually, but this fucking sucks right now... My mind is racing, one minute I'm laughing about something you joked about or said, the next i'm shaking and sobbing because you aren't here... I feel like i'm constantly panicking.... I would totally lose my mind if I wasn't here with Kim and them... honestly I think if I wasn't here with them, I think I would be hurting myself right now or wanting to be really badly.... and that's a scary thought to be honest. I don't know if I do right now... but so much has been going on that I haven't really thought bout it frankly. I'm keeping a lot of your shirts for myself and TJ. I'm gonna see if J wants any of them. If not, well I'm not worried about it. ¯\_(ツ)_/¯
I promise to take good care of your shirts that your dad gave you. I have a lot of good memories of you two together, so to have some of these shirts that I vividly remember grandpa Taylor wearing when I was little, then seeing you wearing them... now me... its.... very special to me. And I'm very honored?? I'm not sure if that's the right term, but i'm gonna go with it...Of course I'm taking your Kiss Blankie, and one of your Seahawks shirts. my favorite one. the one you always wore, you know the one. hehe. I even have the shirt J and I made for you when we were teeny tiny. My handprint is so small oh my gosh dadddd... I promise to take good care of it.
Gods....there's so much more I wanna say. But I'm not really sure how too... I definitely feel like i'm still in shock...I thought I still had time... Dad... You HAVE to tell people when you don't feel good, I know you don't like people worrying about you but... THIS IS WHYY!! GOD dad.... I'm happy your not in pain anymore I'm so happy for that, cause god knows that you hated it so much... But this was too fucking sudden for everyone. Too fucking sudden old man.... Christ... leaving me...us like this... fucking hell dad.... I just... I need you. here with me. I'm always going to need you. I don't know what I'm going to do without you.... you were a really good man whether you believe it yourself or not.
You ARE a good man, you saved three different lives.... but mine is going to be changed forever and you know how much I hate change like this..... Honestly personally I don't think I'll ever really get over this, or this trauma... I really don't think I will. I hate this so much I do. plain and simple. I want you here with me dammit, it's not fucking fair! It's so not fucking fair!! I hate feeling like i'm being selfish when I know this is normal....I feel like I have to be strong for everyone else I don't wanna be. I spent most of my life hating you because of my mom!!! I HATE MYSELF FOR THAT AND ITS NOT MY FAULT. I missed out because of her, and because she lied to me about a lot of things..... and that's time I will never get back with you.... that kills me so badly..... like oh my gods it hurts bad.... so much..... I know there is still a lot of high running emotions. But you know how strongly I felt and loved.... gods... How am I going to this without you? I know I will..... but right now...I don't know how... I really don't know how..... I love you so much this hurts so badly.... I don't think I can properly pet into words how bad i'm hurting.... how badly i'm missing you right now. I know for a fact that if you were here right now, we would be talking about everything under the sun. Gods I need that right now..... I really do daddy... I just wanna talk to you, and laugh and hug you.
I would give almost anything for just one more day.... just to hear your voice, see your green eyes. hear your laugh.... feel your arms around me... I am so glad that we were able to work on our relationship. So fucking grateful. you mean so much to me daddy, you really do. I hope you know how much you mean to me.... I really really hope you do . I love you dad. I will talk soon.... maybe... might start a sideblog with letters for you... I'll have to think about that for a little bit. But I love you daddy. I will talk you later. toodles....
#stoned rae#yes I have been very stoned writing this......#honestly.... it's its only thing I really can do.#although my stepmom has involved us kids in every step of this process....#and giving us a choice whether or not we want to bury dad or cremate him.....#it's nice#very nice.#but I'm ok but not ok.#I am safe#I am loved#a lot of back and forth emotions right now.....#BIIIGGGGGG FEEELLLIINGGGSSSSS#wooobooyyyy#we are cremating him.#We all want a lil piece of him with us#I feel proud of myself for being present for the conversation... I kinda remember it lol#but we all agree that we want to cremate him.#cause his other wish...#we can't do....#This man#wants to be buried ass up#butt naked#with a sign that says “Kiss my ass” and heavy metal playing in the background.#I think that would be funny as hell#but my stepmoms family#wouldn't like it that much#and well. I like my stepmoms family.#so we respect dem!#lol#Otay I done rambling
10 notes
·
View notes
Note
Could Gallifreyans donate organs to humans, and, if so, would human's need immunosuppressants?
Can humans donate organs to Gallifreyans, and how would this affect regeneration since it is not tissue that is Gallifreyan?
Hows does organ donation work between Gallifreyans and humans?
Now we're getting into the really fun stuff :D Let's explore what organ donations might look like between humans and Gallifreyans.
🧬 Gallifreyan to Human Organ Donation
Gallifreyans can donate certain organs to humans due to their unique physiology, which isn't limited by the typical biological barriers faced in human-to-human transplants.
1️⃣Preparation
Gallifreyan organs must first be conditioned to process and 'understand' human blood, which can be achieved through:
Blood transfusions from the recipient for a few days;
Direct injections of the recipient's blood into the organ while the organ is still in the Gallifreyan;
A spacey-wacey magic machine that does this step.
This allows the organ to see and understand human blood cells before encountering them in situ. Also, the organ will be marked with a little genetic code from the recipient, resulting in much better chances the human body will accept it. This wouldn’t be a pleasant experience for the Gallifreyan by any means. For a nicer experience, the Gallifreyan can retreat to a trance or a healing coma state to allow their body to focus on processing.
If this isn't done:
The chances of rejection are dramatically increased;
If the organ is part of processing like a kidney, it could start trying to break down/eliminate red blood cells and white blood cells, leading to hypoxia and severe immunodeficiency for the human, inevitably resulting in death.
2️⃣Surgical Transfer
Transplant operations are similar to human procedures, with a few extra notes:
💉Anaesthesia: Anaesthesia needs to be adjusted very precisely for a Gallifreyan to adequately sedate them, else you could just end up paralysing them throughout the whole thing or killing them altogether.
🪨Durability: Gallifreyans need a little more gusto to get into due to their durable skin and muscle layers.
🩹More Heals: Their healing rate means the operation must be fast. Very fast.
3️⃣Post-Operative Adjustments
Human recipients might experience initial fluctuations in the organ's function as the Gallifreyan organ tries to adjust to a far less efficient environment. However, they'll benefit from an overall improvement in their biological functions in the long term.
❓Potential Organs
🫀🫀Hearts: Gallifreyans hearts are symbiotically linked and donating one is extremely complex and dangerous. The donor will lose significant biological advantages involving healing and energy, and if it really goes wrong mid-op, there could be a permanent death. Not to mention the heart has a slightly different structure to a human heart.
🫘Kidneys: This is one of the easier transplants to perform from Gallifreyan>Human, and the least complex.
🫁 Liver, Lungs, etc.: Theoretically possible, but each Gallifreyan organ will have its own unique challenges and side effects.
🩺 Human to Gallifreyan Organ Donation
Donating human organs to Gallifreyans is more problematic due to the advanced and different nature of Gallifreyan physiology, not to mention a little bit pointless.
🚫Inadequate Function: Human organs probably won't meet the physiological demands of a Gallifreyan body, so they're not much help.
🔁Regenerative Impact: Introducing human organs into a Gallifreyan could interfere with their regenerative abilities, potentially causing rejection or failure during a regeneration cycle, which isn't going to be pretty.
🌱Regrowth Through Healing: If the Gallifreyan has an elevated level (i.e., just after regeneration or some form of lindos therapy), it could be possible to regrow the organ using lindos, so chances are they won't need it anyway.
💊 Immunosuppression and Rejection
For Human Recipients:
Usually, in humans, the body will identify a donor organ as an infection and order the immune system to attack it—this is why donor recipients take immunosuppressants to inhibit the immune system’s function.
Immunosuppressant medication is not actually required here. A small, regular dose of artron in the form of an IV infusion (every month) will hugely reduce the risk of acute or chronic rejection. If this artron IV is unavailable, a blood transfusion from any Gallifreyan will be a good replacement—from the original donor, it's even better. If that isn’t available, immunosuppressants can be used, although it isn't ideal. If that's a no-go, then the kidney will be rejected.
For Gallifreyan Recipients:
While theoretically transplantable, human organs would likely be inadequate without significant modification and support, possibly involving Gallifreyan technology to enhance function and compatibility.
The risk of rejection is heightened, with severe consequences for the Gallifreyan’s health and regeneration capabilities.
🏫 So ...
Organ donation between Gallifreyans and humans, while theoretically possible, involves a bit of thought. For Gallifreyan to human transplants, it's very much a yes, but human to Gallifreyan organ donations are just a bit non - it's possible, but there are much easier ways to go about healing the Gallifreyan than giving them your lung.
Related:
Can Time Lords undergo surgery?: How surgery is achieved for Gallifreyans.
Gallifreyan Assessment Scoring System (GASS): Guide for assessing vital signs.
Hope that helped! 😃
More content ... →📫Got a question? | 📚Complete list of Q+A and factoids →😆Jokes |🩻Biology |🗨️Language |🕰️Throwbacks |🤓Facts →🫀Gallifreyan Anatomy and Physiology Guide (pending) →⚕️Gallifreyan Emergency Medicine Guides →📝Source list (WIP) →📜Masterpost If you're finding your happy place in this part of the internet, feel free to buy a coffee to help keep our exhausted human conscious. She works full-time in medicine and is so very tired 😴
#doctor who#gil#gallifrey institute for learning#dr who#dw eu#gallifrey#gil biology#gallifreyans#gallifreyan biology#whoniverse#time lord biology#ask answered#transplants
12 notes
·
View notes
Text
youtube
India: 80% Organ Donors Women; 80% Organ Recipients Men | Vantage with Palki Sharma
Transcript:
Now let's talk about something that's seldom discussed: organ donation in India. One person is added to the organ donation waitlist every 10 minutes - one person every 10 minutes. It tells you how grave the situation is.
Turns out it also has a gender problem and this is according to the latest data that has come out. Four out of five organ donors in India are women. What about those who receive organs? Four out of five recipients in India are men; in other words 80% of the donors are women but 80% of the recipients are men. So why are these numbers so skewed? Our next report tells you.
Last December Indian politician Lalu Prasad Yadav underwent a kidney transplant. Sounds like a normal procedure a simple transplant surgery but it made headlines everywhere. Why? Because the donor was his daughter Rohini Achara. It was shown as a story of sacrifice; a daughter doing what she could to save her father.
The optics were great but data suggests this is the reality of India's organ donation. It's all about sacrifice and usually it's about sacrifice by women. A recent study analyzed organ donations from 1995 to 2021. 36,640 transplantations were carried out in India; 29,000 of them were for men only. 6,945 were for women. If you put those numbers into perspective basically men were 80% of the total recipients for organ donations but when it comes to donations it's a completely opposite scenario.
Women make up for 80% of the organ donors and who are these women? They are usually wives or mothers when their son or husband needs an organ they are the first to volunteer which makes them living organ donors. You see, organ donation is easier between family members this means they are genetically easier this lessens the risks of rejections but what explains this disparity?
Well the answer is socioeconomic pressure in our society. Men are seen as Breadwinners; women on the other hand are seen as caregivers. More often than not they feel pressurized to donate their organs. On the other hand men think twice in a situation like this; they hesitate to go into surgery which means most men donors in India are cadaver donors. That means they donate their organs only when they're dead.
These are stories that make for great headlines: a mother giving a kidney to her son, a wife giving her liver to her husband. They are shown as the Messiah of sacrifice and it's society that is to blame for this. Organ donation shouldn't happen under any sort of pressure it should be a choice that one should take freely.
That said the whole picture isn't too great also India's organ donation rate is quite bleak. It stands at 0.52 per million people. Every 10 minutes one person is added to the waitlist. In 2022 over 2 lakh patients needed a kidney transplant. Guess how many got it? It was only 7,500 people. That's just 3.4% so you get the gist the numbers are bad which is why more people need to step up not just women but more people should be open to donating organs. It's an act that saves lives.
#india#organ donation#sex based oppression#the way that i raged while listening to this#hearing that these women literally feel pressured to give up their ORGANS for these men#feminism#radical feminism#i hate the way that media glorifies female sacrifice as if it's this glorious thing when it really just reinforces gender inequality#notice how no one in this video is referring to uterus-havers or other genderist BS#they know exactly what women are and that this matter affects them specifically#terfsafe#terfs do interact#radblr#terfblr#TERF#Youtube
23 notes
·
View notes
Text

Phantom Transplants
Sonny Graham was on the verge of death in 1955 due to congestive heart failure, he had been given just six months to live. It was a happy day when he received word that a heart had become available. It belonged to a 33-year-old man, Terry Cottle who had committed suicide by one shot to the brain, leaving his young bride behind.
After Graham was informed who his donor was, he began to write Cottle’s widow in appreciation. The two met, fell in love and married.
Love for this young woman wasn’t the only thing these two men shared. Graham discovered that he now craved beer and hot dogs, which were Cottle’s favorites.
Twelve years after his successful transplant, Graham took his own life by shooting himself in the head. Leaving this wife to mourn twice.
The cravings and personality changes that occurred in Sonny Graham’s life are actually often everyday experiences among transplant recipients.
Organ transplants, including heart, liver, kidney, and lung have saved many lives. There were more than half a million performed in the U.S. alone, between 1988 and 2016.
There are countless stories about the unusual side effects that occur after these transplants.
Claire Sylvia had a heart transplant at the age of 44. She believes that along with this vital organ that saved her life, she also received her donors tastes and memories.
After her operation, she was asked what she would like to do first. Without hesitation, she answered, “I am dying for a beer right now.” This was strange for Sylvia had always hated the taste of beer.
Over the next few months, she began to have a variety of strange food cravings. Most notably McDonald’s Chicken McNuggets, something she had never desired.
Sylvia now had allergies that she did not have in the past as well as a heightened empathic ability. She also became extremely moody, which was not like her. She had a series of odd dreams where a thin, tall young man talked to her. He told her his name was Tim.
Her curiosity peaked, Sylvia did some research and discovered that a young man named Timothy Lamirande was involved in a motorcycle accident on the same day she received her heart transplant.
He was her donor.
She met his family and they confirmed all the cravings she was having were Tim’s favorite foods, especially beer.
Oddly, they told her he had just gone to McDonald’s the day of the accident and a sack of Chicken McNuggets had been found next to his body.
Scientists put forth the idea of cell memory. Where cells within organs retain the original owner’s memories and pass them along.
11 notes
·
View notes
Text
https://x.com/kidneystories/status/1775163762242162806?s=20
Tune in Friday, April 5th at 7pmCST/8pmEST for a live broadcast with James "Uncle Jim" Myers. This week our Guest is Aimee Mackovic, Professor, Author and Award Winning Poet. She is also a Heart, Liver & Kidney Transplant Recipient!
Join us and hang out with Uncle Jim!
https://www.facebook.com/share/p/XmcCEzHu3mQBv33U/?mibextid=oFDknk

2 notes
·
View notes
Text
What Is A Dual Organ Transplant? When Do You Need A Dual Organ Transplant?

A combined or dual organ transplant is a viable option for those who have suffered multiple organ failures wherein the patient will receive two organs simultaneously during one surgical procedure. A dual organ transplant may usually include a combined liver and kidney transplant or a pancreas and kidney transplant. Whether a liver and kidney transplant or a pancreas and kidney transplant, both organs must be replaced when they fail to function properly. The most common type of dual organ transplant is a kidney-pancreas transplant, which is performed on patients with type 1 diabetes who also have end-stage renal/kidney failure.
When Do You Need Dual Organ Transplant?
When you suffer from end-stage diseases like kidney failure and liver failure associated with comorbidities such as diabetes, congenital defects, autoimmune disorders, chronic infections, or long-term damage from substance abuse, you may have to undergo dual organ transplantation. Some patients may have a genetic predisposition to develop multiple organ failure, while others may experience organ damage as a result of an accident or injury. Patients undergo liver and kidney transplants because their liver and kidney fail to function. Those who have to undergo pancreas and kidney transplantation have kidney failure and suffer from insulin resistance (diabetes) simultaneously. Liver and kidney transplantation is recommended in case of Chronic Kidney Disease and defects in the liver at the same time.
Visit a top multispecialty hospital if you or your loved one needs a dual organ transplant in Old Airport Road.
What to Expect from Dual Organ Transplant?
There are many advantages of dual organ transplants. Some of these are:
Two Organ Transplants Simultaneously
One of the significant benefits of a dual organ transplant is that you receive two organs simultaneously and do not need to undergo two surgeries separately.
Less Suffering
Undergoing surgery may drain a patient. When two organs are transplanted in one surgery, the patient is relieved from undergoing two surgeries. Thus, a dual organ transplant helps the patient avoid additional surgeries and recover faster.
Long-Term Outcomes
For patients with end-stage organ diseases, a dual organ transplant can greatly improve their quality of life and increase their life expectancy.
Steps Involved in Dual Organ Transplant
There are different steps involved in the transplantation of various organs.
Kidney and Liver Transplant
To perform kidney and liver transplants together, the patient has to undergo a series of tests and evaluations such as a comprehensive medical evaluation, blood tests, and imaging studies, to determine if they are healthy enough to undergo the transplantation surgery. The liver and kidneys are often received from a deceased donor. The size of the liver must exceed 2% of the recipient's body weight. After the liver implantation, the single kidney is implanted into the right or left of the liver transplantation.
The liver will be transplanted in the following procedure:
The doctor will make an incision in your abdomen.
Blood vessels will be separated from your diseased liver.
The diseased liver will be replaced with a healthy liver.
The blood vessels will be reconnected.
The incision will be closed and the patient will be moved to the recovery room.
To transplant a kidney, the doctor will follow the procedure mentioned below:
The surgeon will place your kidney in the area of the lower abdomen. The new kidney is placed under the existing kidney. The existing kidney is removed if the doctor finds it is cancerous or leads to increased blood pressure.
Kidney and Pancreas Transplant
A simultaneous kidney and pancreas transplant is required when a patient suffers from kidney failure and diabetes and needs a very high insulin dose to control diabetes. Once the doctor confirms that you require a kidney and pancreas transplant through a complete medical assessment, blood tests, imaging tests, etc., you will wait for a donor kidney and pancreas. The doctor will test the compatibility when the donor's kidney and pancreas are available.
During the procedure, the surgeon will place the new kidney below the left side of the abdomen and connects the blood vessels to the kidney. The vein and artery are then connected to the new kidney, and the ureter of the new kidney is also connected to your bladder. After that, the new pancreas is placed below the right side of the abdomen and connects the blood vessels. The kidney and pancreas combined surgery take almost 5 to 7 hours and you may have to stay in the hospital for up to 2 weeks.
The surgeon will monitor your condition for the next few days after the surgery, whether it is a combined liver and kidney transplant or a kidney and pancreas transplant. If everything is found normal, you will be discharged from the hospital with a post-transplant care module, which includes regular check-ups and monitoring of the function of the new organs. By following these guidelines and taking immunosuppressant medications as prescribed, patients can help ensure the long-term success of their dual organ transplant.
Risks Involved in Dual Transplants
Risks in dual organ transplants depend on the health of the patients. Since your surgeon will monitor your entire health, there is less chance of risk during the surgery. In rare cases, a patient undergoing dual transplant surgery may suffer bleeding, pain, and other infections.
Currently, dual organ transplant has emerged as an effective way for those who have suffered an acute disease. This transplant procedure is recommended when there is no other option left. The organs are received normally from a deceased patient, and you will be on a waiting list until the organs are available.
Consult a nephrologist in Old Airport Road if you require dual organ transplant services.
FAQs
Name some complications of organ transplant.
Rejection, infection, high blood pressure, and delayed graft function are common complications of organ transplants.
Which is the most complicated organ to transplant?
Lungs are the most complex organs for transplant as they are more susceptible to infections.
Can two organs be transplanted together?
Yes, two organs can indeed be transplanted together. This procedure is called a combined or dual organ transplant.
3 notes
·
View notes
Text

Stem cell transplantation (SCT) can cause a host of complications. Graft versus host disease (GVHD) is common and can be severe, affecting many organ systems. In acute GVHD, end-organ damage is the result of recipient's APCs interacting with donor T-cells, leading to donor T-cell activation with a resultant cell-mediated and inflammatory cascade. The pathophysiology of chronic GVHD is not well understood. Skin, small intestine, and liver are most commonly affected; lung involvement is less common.
Acute GVHD typically occurs within 100 days post SCT and can cause bowel wall thickening and/or dilatation, biliary abnormalities, ascites, pulmonary edema, diffuse alveolar hemorrhage, and a myriad of other findings. Chronic GVHD typically occurs within 2 years of SCT and may affect skin, mouth, GI tract, liver, lungs, muscles, joints, or genitals. Imaging is based on presenting symptoms.
Read more about the complications of SCT (including GVHD) from the American Cancer Society. https://www.cancer.org/.../transplant-side-effects.html
Today’s case is a patient 2 months post SCT who presented with shortness of breath, nausea, and vomiting. Lungs demonstrate upper lung predominant groundglass opacities and interstitial thickening, worrisome for acute GVHD. The cecum is thickened and enhancing, with pneumatosis, likely indicating typhlitis (neutropenic colitis). There is also moderate volume ascites.
Case courtesy of Hoe Han Guan, Radiopaedia.org, rID: 166522
#TeachingRounds#FOAMEd#FOAMRAd#Radiology#transplant#transplantimaging#transplantmedicine#infectiousdisease#pulmonology#gastroenterology#hematology#GVHD#stemcelltransplant
2 notes
·
View notes