#Gastrointestinal health and surgery
Explore tagged Tumblr posts
Text

Discover the benefits of minimally invasive gastrointestinal surgery at Healix Hospitals, offering advanced techniques for better patient outcomes.
Do Visit: https://www.healixhospitals.com/blogs/minimally-invasive-gastrointestinal-surgery:-benefits-and-procedures
#Minimally Invasive Gastrointestinal Surgery#Benefits of minimally invasive surgery#Gastrointestinal surgery procedures#Advantages of minimally invasive surgery#Types of gastrointestinal surgery#Minimally invasive surgical techniques#Recovery from gastrointestinal surgery#Laparoscopic gastrointestinal surgery#Minimally invasive GI surgery#GI surgery benefits#Advanced gastrointestinal surgical procedures#Minimally invasive surgery recovery time#Cost of minimally invasive surgery#Risks of minimally invasive surgery#Gastrointestinal health and surgery#Patient outcomes in minimally invasive surgery
1 note
·
View note
Text
Well, I managed to make it through the night. Even with all the physical pain, anxiety, catastrophizing, obsessive thoughts, panicking, sobbing, etc. I still fell asleep eventually (and without having to take more of my sleep aid than what I've been taking for the past 2 weeks). Pain is actually a little bit better today but not completely gone.
I scheduled an appointment with my doctor for June 13 but still have to make an appointment with the gastroenterologist and with the lab to test me for stomach bacteria again. I'm trying my best but this is so exhausting and there's no guarantee I'll even have any answers by the end of all this. I just wish this was all a nightmare I could wake up from and finally be okay.
#IBS#gastrointestinal issues#painsomnia#panic attack#I had a full-on breakdown last night feeling like that was it for me#the pain was terrible#and my meds were not working#next month is the 10 year anniversary of when I had to undergo an emergency surgery#so maybe I have that in the back of my mind... idk#I'm always thinking that I'm never going to be okay and that whatever health issue I have going on with me is just going to kill me#it could also be the fact I've always been surrounded by death especially in the past couple years#and I've never been able to resolve my Health Concern OCD even though that was one of the first conditions I was diagnosed with#I'm just so tired of all this#I was crying last night while thinking 'How much longer do I have to deal with this?'#I'm so full of regrets#I should have taken better care of my stomach and overall health#not to mention my mental health too#I'm just so overwhelmed always trying to balance things all on my own without any help#I guess that's part of being an adult but still...#I just can't handle anything it seems
2 notes
·
View notes
Text
Vitamin B12: What to Know
Vitamin B12: What to Know
Introduction: Vitamin B12, also known as cobalamin, is a vital nutrient that plays a crucial role in maintaining overall health and well-being. Despite its importance, many individuals may not be aware of the signs of B12 deficiency or how it can impact their health. In this comprehensive guide, we’ll explore the significance of vitamin B12, common symptoms of deficiency, and strategies for…

View On WordPress
#anemia#animal products#B12 absorption#B12 deficiency#B12 deficiency treatment#B12 injections#B12 supplements#balanced diet#breastfeeding#cardiovascular issues#celiac disease#cobalamin#cognitive impairment#Crohn&039;s disease#dietary guidance#Dietary Guidelines#dietary intake#dietary recommendations#dietary sources#dietary supplements#DNA synthesis#fatigue#fetal development#gastric surgery#Gastrointestinal Disorders#Health and Wellness#Health Awareness#Health Education#health risks#Healthcare
2 notes
·
View notes
Text
GI Surgery Specialist Ahmedabad: Your Trusted Partner for Digestive Health
GI Surgery Specialist Doctor In Ahmedabad – Looking for the best GI surgeon in Ahmedabad? Dr. Dhaivat Vaishnav is a highly skilled and experienced GI surgeon at Gastro Surgeon Gujarat, who offers a wide range of treatments for digestive disorders.
Google Map:-->https://maps.app.goo.gl/Y4M7v25g3UsgRRWx7
GI Surgery Specialist Ahmedabad: Your Trusted Partner for Digestive Health, Best Gastro Surgery Specialist Doctor In Ahmedabad, GI Surgery Specialist Doctor In Ahmedabad, Best Gastrointestinal Surgeon Doctors in Ahmedabad, Best Gastro Surgeon in Ahmedabad, Best Gastro Surgeon in Gujarat, Best Gastroenterologists In Ahmedabad, Best Gastroenterologists in Ahmedabad, Ahmedabad, Gujarat, Ahmedabad Gujarat India, www.gastrosurgeongujarat.com, Dr. Dhaivat Vaishnav
#GI Surgery Specialist Ahmedabad: Your Trusted Partner for Digestive Health#Best Gastro Surgery Specialist Doctor In Ahmedabad#GI Surgery Specialist Doctor In Ahmedabad#Best Gastrointestinal Surgeon Doctors in Ahmedabad#Best Gastro Surgeon in Ahmedabad#Best Gastro Surgeon in Gujarat#Best Gastroenterologists In Ahmedabad#Best Gastroenterologists in Ahmedabad#Ahmedabad#Gujarat#Ahmedabad Gujarat India#www.gastrosurgeongujarat.com#Dr. Dhaivat Vaishnav
0 notes
Text
Hiatal Hernia Friendly Foods Delicious Dishes to Soothe Your Belly and Fight the Burn #herniadiet #n
#health #herniarepair #hernia #surgery #medicalstudents #medicalprofessionals #DrAtefAhmed #MedicalMystery #DoctorReacts #MentalHealthAwareness #ChronicIllness #HealthTips #Wellbeing #FitnessMotivation #MedicalSchool #Nutrition #HealthyLifestyle #DiseasePrevention #FirstAid #Anatomy #Healthcare #MedicalTechnology #PatientStories #DoctorLife #MedStudent Atef’s Notes In Hernia for Medical…
View On WordPress
#AI in medicine#anxiety#cardiac surgery#clinical rotations#diabetes#endoscopy#gastrointestinal medicine#healthcare technology#hernia#infectious diseases#laparoscopy#medical ethics#medical school tips#medical specialties#minimally invasive surgery#neurology#Neurosurgery#oncology#orthopedic surgery#palliative care#patient communication#physician burnout#psychiatry#Public health#residency application#robotic surgery#schizophrenia#telemedicine#usmle prep
0 notes
Text

Understanding Alcohol-Induced Liver Disease (ALD)
Alcohol-induced liver disease (ALD) is a serious condition that results from prolonged excessive alcohol consumption. It encompasses a range of liver disorders, including fatty liver, alcoholic hepatitis, and cirrhosis. ALD can have severe consequences for liver function and overall health, making it essential to understand its causes, symptoms, and treatment options.
Causes of ALD:
The primary cause of ALD is excessive alcohol consumption over an extended period. Alcohol is metabolized by the liver, and chronic alcohol abuse can lead to inflammation, scarring, and damage to liver cells. Factors that increase the risk of developing ALD include:
Heavy and prolonged alcohol consumption Genetics Poor nutrition Obesity Hepatitis C infection Gender (women are more susceptible to ALD) Symptoms of ALD:
The symptoms of ALD can vary depending on the severity of the liver damage. In the early stages, individuals may not experience any noticeable symptoms. However, as the disease progresses, symptoms may include:
Fatigue Jaundice (yellowing of the skin and eyes) Abdominal pain and swelling Nausea and vomiting Loss of appetite Weight loss Easy bruising and bleeding Swelling in the legs and ankles Confusion and cognitive impairment Treatment Options for ALD:
The treatment of ALD depends on the stage of the disease and the extent of liver damage. Treatment goals typically include:
Abstinence from Alcohol: The most critical aspect of managing ALD is to stop drinking alcohol completely. This can help prevent further damage to the liver and may even reverse early stages of the disease. Nutritional Support: A healthy diet rich in vitamins, minerals, and antioxidants can support liver health and promote healing. In some cases, nutritional supplements may be recommended. Medications: Medications may be prescribed to manage symptoms, reduce inflammation, and improve liver function. These may include corticosteroids, pentoxifylline, or medications to address complications such as fluid retention or infections. Liver Transplant: In severe cases of ALD, where the liver is severely damaged and non-responsive to other treatments, a liver transplant may be necessary. Consult the Best Gastroenterologist in Chennai:
If you or someone you know is struggling with alcohol-induced liver disease, it's crucial to seek expert medical care from a qualified gastroenterologist. Dr. Kumar Gurubaran, the best gastro doctor in Chennai, specializes in the diagnosis and treatment of liver disorders, including ALD. With his expertise in gastrointestinal health and advanced treatments such as laparoscopic surgery, Dr. Kumar Gurubaran provides comprehensive care to patients in Chennai and beyond.
Don't let ALD compromise your liver health and overall well-being. Take the first step towards recovery by consulting with Dr. Kumar Gurubaran, the leading gastroenterologist in Chennai, today.
#Best Gastroenterologist Chennai#Best Gastro Doctor Chennai#Best Gastro Surgeon Chennai#Gastro Specialist Chennai#Best Gastroenterologist in Chennai#Best Laparoscopic Surgeon Chennai#Dr. Kumar Gurubaran#Gallbladder Stones#Colorectal Surgery#Fistula in Ano#Pancreatitis#Constipation#Endoscopy#Colonoscopy#ERCP#Bile Duct Stones#Obesity Awareness#Laparoscopic Surgery#Gastrointestinal Health#Laparoscopic Hernia Surgery#Hernia Surgery Chennai#Hernia Surgery in Chennai#Hernia Surgeon#Hernia Chennai#Groin Hernia#Incisional Hernia#Inguinal Hernia#Umbilical Hernia#Ventral Hernia#Hiatus Hernia
0 notes
Text
Best Breast Cancer Doctor in Ludhiana
Experience top-tier breast cancer care at Ramanhospital, recognized for hosting the Best Breast Cancer Doctor in Ludhiana. Our dedicated team offers comprehensive treatment and support, ensuring optimal outcomes for patients. With advanced technology and compassionate care, Ramanhospital prioritizes your well-being throughout your journey. Trust Ramanhospital for excellence in breast cancer treatment. Book your appointment today and receive the care you deserve.
Visit us :- https://www.ramanhospital.in/cancer-surgery.html
#cancer#cancer surgery#cancer hospital#breast cancer#lung cancer#Gynecological Cancer#Gastrointestinal Cancer#Urological Cancer#Head & Neck Cancer#Thoracic Cancer#cancersurgeryhospital#disease#public health#prevention#medicine#hospital#ludhiana#treatment
0 notes
Text
youtube
Which wrap is preferable for a Hiatus Hernia repair?
Hiatus hernia is a disorder that causes severe heartburn and indigestion. It is frequently overlooked, but if not addressed promptly, it can lead to major issues. Dr. Arun has produced this five-part series to address the five most frequently asked questions concerning this illness. Please keep in mind that this video is not intended to substitute medical advice. It was created solely for educational purposes.
#hiatus hernia#hiatal hernia symptoms#hiatal hernia treatment#hiatal hernia weird symptoms#hiatal hernia repair surgery#paraesophageal hiatal hernia#treatment of hiatus hernia#hiatus hernia causes#best treatment for hiatal hernia#treatment for a hiatus hernia#gastroenterology#gastrointestinal surgeon#gastrointestinal doctor#health and wellbeing speakers#gastrointestinal treatment#Dr Arun Dhir - Surgeon#hiatal hernia hernia repair#Hiatus Hernia repair#Youtube
0 notes
Text
web of wyrd: annual energies and potential surgeries associated with the year
the outer rim of the wyrd web foretells the themes of our year ahead. today i will be covering some common surgeries that tend to occur. in no way does one number mean a single surgery type. each number can mean different surgeries - multiple surgeries - no surgery... this is just what i associate medically with these energies and i have seen correlate with other charts when surgery occurred. your lack of a number correlation with an experience below does not mean to minimize your experience. this is a general hypothesis not a fact.
tw: sensitive topics like amputation, ivf, addiction, weight, physical trauma, and end of life care are included in post.
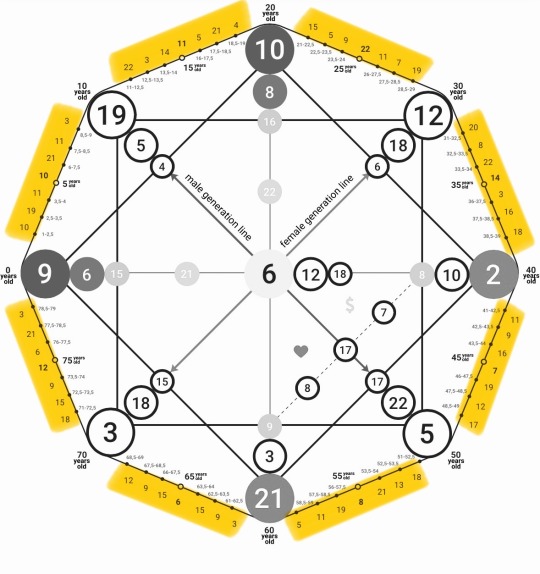
1 (the magician): laser surgery
skill, precision, and transformation. this technique uses precision tools to create change in the body.
2 (the high priestess): diagnostic surgery
intuition, secrets, and hidden knowledge. seeks to uncover hidden issues or provide clarity about a medical condition (will be common for 2000 baby around the time doctors start recommending colonoscopies and mammograms).
3 (the empress): fertility surgery
surgeries like in vitro fertilization (IVF) or other fertility-related procedures.
4 (the emperor): orthopedic surgery
structure and stability. anything involves bones, joints, and structural support of the body, resonates with this energy.
5 (the hierophant): cardiovascular or oral surgery
what maintains order/structure in the body a.k.a. anything dealing with the heart and blood flow. oral surgery is because of this card connection to the throat and sharing of beliefs which requires the mouth - it might be time for your wisdom teeth extraction.
6 (the lovers): cosmetic or reconstructive surgery
this is often elective surgery / chosen for personal reasons related to self-image.
7 (the chariot): neurosurgery
deals with the brain and nervous system (the body's control center), which aligns with the chariot's themes of mastery and control.
8 (strength): physical rehabilitation surgery
requires a lot of resilience as muscles and tendons aren't easy to heal...
9 (the hermit): gastrointestinal surgery
involves the digestive system, relates to the internal processes and inner workings (aligning with hermit energy).
10 (the wheel of fortune): emergency surgery
often needed unexpectedly and dictated by fate, aligns with the theme of chance.
11 (justice): corrective surgery
aims to fix or balance out bodily functions or appearance, mirrors the themes of rectifying and balancing.
12 (the hanged man): organ transplant
sacrifice, suspension, and new perspectives. transplant surgery involves the sacrifice of one organ for the life of another, offering a new lease on life.
13 (death): amputation
a literal removal or ending of a part of the body, that can also lead to a transformative process of healing and adapting.
14 (temperance) : bariatric surgery
used to achieve weight balance and improve health.
15 (the devil): addiction, breast reduction, and reproductive surgery
surgeries that address addiction-related issues, such as gastric banding for overeating. but also reproductive surgery like a tubal ligation or vasectomy. any surgery where something big/open becomes small, constricted, snipped, or thinned.
16 (tower): trauma surgery
sudden upheaval, destruction, and revelation. this type of surgery is often performed in response to sudden, life-altering accidents or injuries, echoes the energies themes of sudden change and crisis.
17 (the star): reconstructive/plastic surgery
hope, healing, and renewal are themes of this energy - this surgery which restores form and function after trauma or illness, aligns with the themes of healing and rejuvenation.
18 (the moon): biopsies and tissue collections
biopsy involves extracting tissue to investigate potential issues, often when there’s uncertainty about a diagnosis or the presence of something hidden (like tumors or other abnormalities).
19 (the sun): pediatric surgery
performed on children and ensures their health and vitality, which connects with the energy's themes of life, energy, and well-being.
20 (judgment): organ transplant or some other life changing/saving surgery
life-saving surgeries, such as heart or organ transplants, can offer a second chance at life, reflecting the energy's themes of renewal and awakening.
21 (the world): making a full recovery or end-of-life care
surgeries that lead to a full recovery or decisions around end-of-life care align with the themes of closure and achieving a state of completeness found with this energy.
22 (the fool): exploratory surgery
represents the unknown. aligns with entering a medical situation without knowing what will be found.
like what you read? leave a tip and state what post it is for! please use my "suggest a post topic." button if you want to see a specific topic or theme next!
click here for the masterlist
click here for more web of wyrd related posts
want a personal reading? click here to check out my reading options and prices.
© a-d-nox 2024 all rights reserved
#astrology#astro community#natal chart#astrology tumblr#tarot witch#tarot art#daily tarot#rider waite tarot#tarot deck#tarot reading#tarot cards#tarot#tarotblr#tarotcommunity#tarotdaily#wyrd web#web of wyrd#matrix of destiny#destiny matrix#matrix of fate#the matrix
145 notes
·
View notes
Text
Every year all of the big diet companies have to come up with some brand new labeling for their plans in order to encourage people to get on the January weight loss train.
This year, Weight Watchers is going further than they’ve ever gone before, by announcing that they have created a new system to give their members access to prescriptions for drugs like Ozempic and Mounjaro.
Let me remind you that these drugs only work while you’re taking them. As soon as you stop, all of your appetite comes back. Your desire to eat returns, and because it has been artificially suppressed it may feel much stronger and less controllable than it was before you took the drugs. Many people who come off these drugs, usually because of cost (because insurers are balking at coverage for weight loss) or shortages (because so many people are taking them for weight loss, which is leaving the diabetics who need them up shit creek) or side effects report that the first weeks are really difficult, mentally painful and often binging occurs.
Additionally, all of these drugs carry a real risk of creating a terribly painful and potentially deadly condition called Gastroparesis, in which your gastrointestinal system just stops functioning, you cannot digest and process food at all.
You do not need to lose weight to be healthy. You do not need to lose weight to be beautiful or attractive, to have success, or love. You do not need to lose weight in order to pursue fitness. If you have particular health needs or goals that can only be achieved by changing the way you eat, (e.g. lowering cholesterol or blood glucose or addressing gastro issues) that does not mean that you need a weight loss diet plan, just one designed toward your needs.
But more than anything, you do not ever need to put another penny into the coffers of the multibillion dollar weight loss industry, which, if it actually had a way to take a fat person and make them thin permanently (something that cannot even be achieved by surgeries that drastically rearrange digestive systems) would be a multi quadrillion dollar industry instead. 
#cw: weight loss#cw: weight loss drugs#weight watchers#ozempic#mounjaro#diabetes drugs for fat people#new year new you old bullshit#health at every size#fatphobia
385 notes
·
View notes
Text
Minimally Invasive Gastrointestinal Surgery: Benefits and Procedures

Minimally invasive surgery has revolutionized the field of gastrointestinal (GI) health, offering numerous advantages over traditional surgical methods. At Healix Hospitals, we pride ourselves on providing top-notch Minimally Invasive Gastrointestinal Surgery, utilizing the latest techniques and technologies to ensure the best possible outcomes for our patients. This blog post delves into the benefits of minimally invasive surgery, various gastrointestinal surgery procedures, and what patients can expect in terms of recovery and overall gastrointestinal health.
What is Minimally Invasive Gastrointestinal Surgery?
Minimally Invasive Gastrointestinal Surgery refers to a range of surgical techniques used to treat conditions affecting the digestive tract. Unlike traditional open surgery, minimally invasive procedures involve smaller incisions, resulting in less pain, faster recovery, and reduced risk of complications. Laparoscopic gastrointestinal surgery is one of the most common forms of minimally invasive GI surgery, where surgeons use a laparoscope – a thin tube with a camera – to perform the surgery with precision.

Benefits of Minimally Invasive Surgery
The benefits of minimally invasive surgery are numerous, making it a preferred option for many patients and surgeons. Here are some key advantages:
Reduced Pain and Discomfort: Smaller incisions mean less trauma to the body, which translates to less postoperative pain.
Faster Recovery Time: Patients typically experience quicker healing and shorter hospital stays compared to traditional surgery.
Lower Risk of Complications: Minimally invasive techniques reduce the risk of infection and other complications associated with larger surgical wounds.
Minimal Scarring: Smaller incisions result in less noticeable scars, which can be a significant aesthetic benefit.
Improved Patient Outcomes: Overall, patients undergoing minimally invasive surgery tend to have better outcomes and higher satisfaction rates.
Continue Reading: https://www.healixhospitals.com/blogs/minimally-invasive-gastrointestinal-surgery:-benefits-and-procedures
#Minimally Invasive Gastrointestinal Surgery#Benefits of minimally invasive surgery#Gastrointestinal surgery procedures#Advantages of minimally invasive surgery#Types of gastrointestinal surgery#Minimally invasive surgical techniques#Recovery from gastrointestinal surgery#Laparoscopic gastrointestinal surgery#Minimally invasive GI surgery#GI surgery benefits#Advanced gastrointestinal surgical procedures#Minimally invasive surgery recovery time#Cost of minimally invasive surgery#Risks of minimally invasive surgery#Gastrointestinal health and surgery#Patient outcomes in minimally invasive surgery
1 note
·
View note
Text
writing share tag!
Oh shit, @cowboybrunch left an open tag on that beautiful excerpt of babygirl Theo being an asshole. And I'm whittling away at this short story.
Yesterday I posted the first 3.1k words of "Among the Elements," which I am revising.
Today I'm offering up 1,930 words and content warnings for DIY surgery, first-person past-tense body horror, and general Mad Science in the name of self-impregnation. It's explicit. IDK how else to tag this. Be careful.
Week 12 Wednesday Most obvious answer has been in front of me the entire time. , Or, rather, adjacent to the experiment itself--it is within my own corpus.
Incubator biosynthetic for sake of fetus's health and safety--never designed with goal of implanation--odds of rejection significant--lower than odds of discovery if left exposed.
Will need to procure robotic assistance. Unable to perform procedure alone. Will require magnetic nerve block, suction, traction, cauterization, waste management if the procedure is successful…
Uncertain as to best incision site. If transverse, reduced risk of hernia and shorter recovery time--limited exposure to surgical site, challenging closure, risk of nerve damage.
Longitudinal…
Had I known I would be installing through a longitudinal incision I may have made different methodological decisions. Earlier installation for one. Will have to manually extract incubator at conclusion of gestation.
Worry about that later.
//
Completed risk assessment.
Incubator 49.5cm in length. Able to accommodate utilizing space in abdominal cavity.
Circumference presents concern. Material somewhat inflexible. Will have to rearrange cavity interior. Possible organ removal necessary.
//
Must be longitudinal incision. Large scar, slower recovery; fewer surgical complications due to open site, will be able to visualize organ migration.
Nothing more to consider. Prepping now. Will update after.
Thursday Glad I'm not two centimeters shorter.
//
Anti-rejectants performing admirably. No redness at site of incision. Pain persistent but tolerable--pharmaceutical intervention will cause unwanted mutations at this stage of gestation even if our systems are not enmeshed.
Acclimating to persistent feeling of fullness and the effect it is having on the gastrointestinal and urogenital systems. Unable to rest supinated--incubator weight occludes the inferior vena cava. Pressure on diaphragm also an unforeseen concern. Several pre-surgical consideration for future application of this prototype.
//
Awakened with realization that THIS IS A PROTOTYPE.
If this doesn't kill either myself or the fetus the implication of successful implantation is phenomenal.
Of course the probability of our both expiring is significant. Compared to this afternoon the fetus's vitals are stable and strong while father vitals are stable and show hypotension and hypoxemia. Lower limb elevation with compression and oxygen adjunct resolved.
I must proceed with caution.
Friday Limited space in hollow organs.
Have learned to vomit without use of abdominal muscles.
Longitudinal incision a terrible idea. That robot was a terrible idea. This was all a terrible idea. I am the king of terrible ideas.
//
Terrible Idea That Wasn't Terrible After All #18: program robot to feed cat in morning. Stay in bed.
She did join me, which was unforeseen. Cleaned her face for roughly an hour and then--purring--laid on my side. Desires the heat of the incubator, doubtless. Considered kicking her out of bed but felt unwell. Feel less unwell, now.
Saturday Fetal heartrate elevated today.
Corpus temperature 38.1C.
This may be how I die. I'd always hoped it would be an explosion that did it. Or an electrical mishap.
Adjusting anti-rejectant dosage.
Sunday Fetal heartrate returned to 110bpm. Corpus temperature reduced to 37.8C. All other systems nominal.
Would say it is easier to breathe but that would be both a colloquialism and a lie. Am however much improved compared to yesterday. Damned cat purred and refused to leave my side until I was able to remove her myself. Robot shuttled broth from the nutrient synthesizer to the bed--I've not taken in nutrients since Wednesday evening.
Thus far the onboard biometrics have reported no issues with the fetus's metabolism or gestation. Incubator nutrient system is unaffected by change in environmental conditions.
Too soon to celebrate.
Monday Cat insists on running in front of me as I'm walking.
Blood loss within acceptable limits--stitches holding--some internal shifting that resolved with external binding. Incubator switching from internal nutrition and filtration to transplacental--connecting its vascular system to mine--a strange sensation I'm unable to put into words, knowing how like and unalike a plumbing system, it can be.
Thinking of my body as a house. Must still be delirious. Back to bed.
Week 13 Wednesday Condition improving--post-operative pain and swelling have subsided significantly--am able to walk from one side of the apartment to the other and have attempted stairs--the incubator appears settled in the abdominal cavity.
One benefit of this arrangement is the incubator will not grow. It is sized for a 12-week-old infant. If I am careful I believe I will be able to keep the incubator hidden for the duration--either in my person, which is less than ideal, or upon returning to a secure laboratory where I can work uninterrupted to perform an extraction. Until such time, I suppose the fetus--
Continuing to refer to the experiment as "the fetus" is unideal. Will have to decide upon a more appropriate name.
Week 18 Friday Initial consideration of healing factor accelerant not entirely baseless--however, I've decided to allow the installation site to close on its own without interfering with placental growth factor. Elastic bandage ensured the incubator did not exert excess pressure on--quite a bit of in and ex in those two sentences for there being not a lot of either, until this stage of the experiment.
Five weeks to complete closure--I should say that's nominal healing, under the circumstances. My own biology may be resistant to the experiment but it continues to perform its essential functions. Equilibrium is returning.
Final and admittedly unthought-through stage of phase I complete.
The experiment is safe.
Week 19 Monday The temptation--the need, I would say, if I were inclined to enter hyperbole into scientific record at some point in the future. I don't need. I want to run scans on this experiment, and the frequency of that want is… overwhelming. Until this point, it would have been too early to scan. Yet that want reared its head near every week for the past month.
Today I was able to measure the fetus's development, and observed continued healthy growth and functionality. Fetus is in the 25th percentile for height and weight with no abnormalities. All vital organs and systems functioning within normal parameters. The incubator is effectively supporting fetal growth and well-being.
While the incubator itself is completely self-contained and able to produce its own hormones, mine has now joined the lymphatic and vascular systems in reducing the incubator's energy consumption.
Am uncertain what to make of this, and look forward to postpartum dissection of the incubator to determine what caused spontaneous integration.
[See supplemental data log for biometric data for week 19 fetal growth.]
//
The biometric scanner is capable of producing imagery of the fetus based on soundwaves.
I saw them. I saw them tonight. They're alive.
//
For the sake of transparency--yes. I was overcome with emotion. It would appear as though the incubator's presence within my abdominal cavity is also exerting bottom-up control over the corpus's endocrine system. I am drawn to think of abstract concepts such as embodiment and caregiving. Of how my corpus had not changed in the milliseconds before the biometric scanner produced an image of the experiment's face, but the experiment became the baby upon subjection to the observer effect. Whether that meant I, by extension, was changed. Whether I had inherited personhood with the death of my ignorance.
I was overcome. I now know everything there is to know about the baby.
I saw my child tonight.
Week 21 Monday The temptation to perform a scan more frequently than every four weeks is maddening. I have the incubator set to alert me if anything changes--not even to suboptimal levels; any change at all--I know when the heartbeat increases, when not enough nutrients are moving through the exchange--when the baby puts their thumb in their mouth.
The only metric I have not gathered concerns their sex. All I know is they are healthy, and I have to be patient.
That sad, I am finding it increasingly difficult to focus on other projects with earlier deadlines. This requires patience, and I keep daydreaming. Knowing months are left between myself and the conclusion of this experiment--for which I was unable to gather consent from the most important participant! Not quite six months, and the difference in how I think of this baby today compared to a series of CRISPR instructions… it may be the literal internalization of my role in the infant's development, or knowing that soon they could survive outside the incubator--so much time has passed, and yet it is not near soon enough to extract the unit.
Nothing to do between here and then but gather data--and, I suppose, as the child has ears, to read to them. Or sing.
Unable to recall if my parents sang to me, when I was only a possibility. Before they sent me away. I was an agreeable child, is my recollection. The Society came for me, and appealed to my parents. They could not give me the sort of education the Society was offering to pay for, and my parents wanted to give me everything. They did not want me to have to work the way they worked.
I wish I would have argued with them. It would have made no difference. But I wish I had told them I didn't want to go.
This child deserves a promise--not to be sent away, and not to be made to be agreeable, if we are not in agreement.
Now I understand why strangers ask if other strangers want to see pictures of their babies, the new ones, all the way up to teenagerhood. I want to show everyone I pass on the street that printout of the impression of this child, the unformed features of their face, and I want to tell them, I made this. This is the only important thing I'll ever do in my life.
Week 23 Neighborhood hot when I returned from the metro. Counted no fewer than four MIB per square kilometer. Uncertain whether they're looking for me--no reason why they ought to be. Simplest and most obvious answer is someone else in the area is drawing attention to themselves. See prev entry re: Omens. Foolish to think ignoring the presence of Technocrats reduces their interest in me, should their interest be above zero. Will proceed with caution.
Week 24 Weight increased substantially, though the incubator has not changed in size. Baby has been gaining 29 grams per week, and the placenta is keeping pace with their development. Anticipate accelerated growth as the trimester continues.
Plenty to discuss, and nothing at all of note. My impatience rears when I acknowledge it; and, in acknowledging it, I have to wonder if impatience doesn't serve as this child's mother, rather than Scientific inquiry.
Week 25 I'm certain other events occurred yesterday that are worth noting. Every other day I make a new discovery, or experience a breakthrough. Were I not frightened of it being entered into evidence, I would record much more of the child's development than I have been.
I am afraid--paranoid, even--and yet.
Every ounce of fear I've felt thus far was erased by a sensation I'd never felt before--never would have felt before--replaced by what can only be described as enlightenment.
I felt like a mortal man stealing fire from the divine. One who went up the mountain sightless and returned with fire. I was, for a moment, a god.
And in that moment I was aware of the presence of life growing within my own, housed within a structure that defies reason or sanity, and I was aware because I felt. I ought not to have been able to feel--I never programmed the biopolymers to transmit information--yet they have.
This is not referred mechanoreception.
I can feel my child move.
#short story: among the elements#c: khalid#when i tell you i tina belcher groaned my way through the first half of this
20 notes
·
View notes
Text
Exploring the Root Causes of Vitamin B12 Deficiency: Understanding the Culprits Behind this Common Condition
Introduction: Vitamin B12, also known as cobalamin, plays a crucial role in various bodily functions, including nerve function, red blood cell production, and DNA synthesis. Despite its importance, many individuals suffer from vitamin B12 deficiency, which can lead to a range of health problems if left untreated. In this comprehensive guide, we’ll delve into the various factors that can cause a…

View On WordPress
#alcohol consumption#B12 deficiency#celiac disease#cobalamin#Crohn&039;s disease#dietary intake#dietary restrictions#gastric surgery#Gastrointestinal Disorders#genetics#H2 receptor antagonists#health conditions#Health Maintenance#healthcare professional.#inflammatory bowel disease#lifestyle choices#medications#metformin#MTHFR gene#nutrient absorption#pernicious anemia#proton pump inhibitors#veganism#vegetarianism#vitamin b12
0 notes
Text
Living with Long COVID: What it’s Like to be Diagnosed with the Debilitating Disease - Published Sept 3, 2024
By: Nicole Pajer
Even mild cases of COVID-19 are linked to potential long-term repercussions — some of them deadly serious
Chrissy Bernal has caught COVID-19 three times, most recently in October 2023. “My symptoms were always pretty mild,” she says. But after her third round of the virus, she developed extreme allergies to foods she used to eat all the time: oats, dairy, gluten, sesame seeds and peanuts.
“I literally have some level of anaphylaxis every single day,” she says. In May, Bernal, 46, a public relations professional in Houston, went into anaphylactic shock during a virtual meeting. “I had to inject myself with an Epi while everyone watched in horror on Zoom,” she says.
Natalie Nichols, 53, has been struggling with debilitating asthma and severe food allergies since she first caught COVID more than three years ago. “Last fall, I spent two-and-a-half months confined to bed, motionless, because moving, including holding a cellphone, made me too short of breath,” she says.
She’s also experienced brain fog, high blood pressure, hyperglycemia, fatigue and gastrointestinal symptoms. Nichols, the founder of a nonprofit in Nacogdoches, Texas, recently underwent surgery to repair joint damage caused by COVID-induced inflammation.
Lorraine W., of Clarence Center, New York, was looking forward to an active retirement when she was diagnosed with COVID in March 2020. “I’ve never returned to my pre-COVID self,” says Lorraine, 65.
She’s on medication to treat small blood vessel damage to her heart and continues to battle a lingering cough, fatigue and breathlessness, as well as kidney disease. Neurological changes have made her legs unsteady when she walks, requiring her to use balance poles. “None of these conditions were present before COVID,” Lorraine says.
In June, the National Academies of Sciences, Engineering, and Medicine released a comprehensive definition of long COVID: “an infection-associated chronic condition that occurs after COVID-19 infection and is present for at least three months as a continuous, relapsing and remitting, or progressive disease state that affects one or more organ systems.” According to that definition, 18 million Americans have experienced long COVID; currently, more than 1 in 20 of us are living with its symptoms. Researchers have begun to link long-term COVID with another recent phenomenon: our shrinking life expectancy.
The disease we’re forgetting COVID doesn’t seem that scary anymore. More than 98 percent of the U.S. population has some degree of immunity — from vaccination, prior infection or both — and Paxlovid and other medications are available to counteract acute symptoms. For many of us, contracting COVID is like having a bad upper respiratory infection.
But “COVID isn’t gone,” says Ryan Hurt, M.D., director of the Long COVID Research and Clinical Program at the Mayo Clinic. The World Health Organization (WHO) estimates that COVID still kills at least 1,000 people every week around the globe — but “we only have data from about 40 countries,” says Maria Van Kerkhove, M.D., director of WHO’s Department of Epidemic and Pandemic Preparedness and Prevention.
Older adults and those with preexisting conditions remain among the most at-risk populations for severe, acute COVID. People 65 and older accounted for 63 percent of COVID-related hospitalizations and 88 percent of in-hospital deaths during the first seven months of 2023, according to CDC data.
Although the dangers of acute COVID infection may have ebbed for many, the reality of long COVID is coming into view. Of those who contracted COVID-19 within the past four years, 10 to 20 percent have experienced long COVID.
“With every new case of acute COVID [the initial phase of infection when diagnosed or symptoms first appear], there is risk for developing long COVID,” says Caitlin McAuley, D.O., a family physician at the Keck COVID Recovery Clinic in Los Angeles. She’s had patients who developed long COVID fully recover, get reinfected several times with no lingering effects, then develop another case that leads to a new bout of long COVID. She’s also seen patients who got COVID twice with no lingering effects, and the third time they ended up with prolonged symptoms.
“We still have a number of individuals who had the first wave of COVID who are suffering from long COVID symptoms now, several of them many years out,” says Jerrold Kaplan, M.D., medical director of the COVID Rehabilitation and Recovery Program at Gaylord Specialty Healthcare in New York.
Having escaped long COVID previously doesn’t mean you won’t face it in the future. Indeed, some research has suggested that catching multiple COVID-19 strains puts you at increased risk. A study published in 2022 found that reinfection can increase the risk of complications in major organ systems, and these risks persist at least six months beyond the initial infection.
We don’t yet know the true impact of catching COVID. “Many chronic disease processes, such as cardiovascular disease, dementia and cancer, take years to develop. And whether acute COVID-19 puts people at risk for some of these issues? Time will tell,” Hurt says. What doctors do know is that patients are flocking to their offices complaining of symptoms they never had before COVID.
Is long COVID boosting our death rate? In July, COVID accounted for less than 1 percent of all deaths in the U.S. Life expectancy in the U.S. is 77.5 years, reflecting an uptick over the past two years but still lower than prepandemic levels. Many factors contribute to that statistic, but it’s clear that the long-term effects of COVID have played a role.
For example, a study in the journal Nature Medicine found that those hospitalized with COVID had a 29 percent greater risk of death in the three years after their infection.
“But what was also alarming is that in people who weren’t hospitalized, there was also an increased risk of a variety of medical issues,” says John Baratta, founder and codirector of the COVID Recovery Clinic at the University of North Carolina at Chapel Hill. Even patients who’d had mild bouts of COVID-19 had an increased risk of respiratory, cardiovascular, metabolic and neurological issues lingering for three years after the initial infection. Long COVID patients had a significantly increased risk of severe health issues affecting the brain, lungs and heart.
We have long known that an acute case of COVID can compromise heart health: Compared with those who didn’t contract COVID, people who caught the virus were 81 percent more likely to die of a cardiovascular complication in the ensuing three weeks, according to a study of 160,000 patients published by the European Society of Cardiology. But the risk lingers long after the symptoms abate. Those who caught the virus were five times more likely to die from cardiovascular disease as long as 18 months after infection, the same study found. Heart disease deaths, which had been on a downward trend for decades, began to spike in 2020 and remained high through 2022, the last year for which data is available.
Stroke, blood clots in the legs leading to clots in the lungs, abnormal heart rhythm (arrhythmia) and inflammation of the heart are among the challenges COVID poses, says Mohanakrishnan Sathyamoorthy, M.D., professor and chair of internal medicine at the Burnett School of Medicine in Fort Worth, Texas. In long COVID, this collection of cardiovascular disruptions can present as postural orthostatic tachycardia syndrome (POTS), in which patients’ heart rates increase abnormally when they go from sitting or lying down to standing up.
One theory to explain COVID’s long-term effect on the heart — and the body in general — centers on inflammation. “Every time you get infected with COVID, there is a possible increased risk of long COVID, and some cardiac disorders can occur — especially if you have a history of heart disease, including stroke, heart disease and heart attacks,” says Pragna Patel, M.D., senior adviser for long COVID at the CDC. All of these problems can be exacerbated by the virus entering coronary tissue and triggering inflammatory responses that can damage the heart.
Researchers say COVID may also alter the gut microbiome, a primary controller of inflammation, thereby triggering the immune system to rev up the condition. “There is no single agreed-upon mechanism that’s causing the issues,” Baratta says. “An individual may have multiple factors going on in their body, and not everyone will have the same underlying mechanism causing their symptoms,” which increases the complexity of both research and treatment.
One factor that seems to matter: vaccination status. “Several studies show that vaccination can decrease the risk of developing long COVID,” Patel says. Vaccination rates tend to increase with age, with people 75 and older being the most well vaccinated — hence the most well protected from long COVID, Patel theorizes. That may explain why long COVID most commonly affects people ages 35 to 64; the risk seems to drop for those 65-plus, according to CDC data.
From long covid diagnosis to treatment No single test can determine whether a person has long COVID. Doctors typically diagnose long COVID by reviewing the patient’s health history and current symptoms and trying to rule out other causes. A positive COVID test is not required, as someone could have been infected without knowing it, then experience strange symptoms later, Patel says.
Though there are many ongoing clinical trials on long COVID, there is no umbrella treatment. Primary care physicians address what they can, then call in specialists — such as a cardiologist to handle arrhythmia or a therapist to treat anxiety — for more targeted care. There are long COVID centers around the country where teams of professionals work to help patients through their unique symptoms.
“Because the effects of COVID are so wide throughout the body and mind, there will not be a single treatment for all long COVID issues,” Baratta says. “This is going to be treated by many different types of providers and specialists, and it will be treated, often, symptom by symptom.”
Long COVID is recognized as a disability under the Americans with Disabilities Act if it substantially limits one or more major life activities. About 200 symptoms fall under that umbrella, Patel says. Here are some of the conditions we’re learning can linger months and, in some cases, years beyond an acute COVID infection. If these or other health changes seem familiar, consult your primary care physician.
1. Extreme fatigue It’s common to experience fatigue when your body is busy fighting off an illness. But some people still struggle with fatigue long after their initial COVID infection. In fact, a lack of energy is the number one symptom reported by long COVID patients. In some, this can be diagnosed as chronic fatigue syndrome, which has been on the rise since the start of the pandemic, Baratta says. He defines this as “a disabling level of fatigue that severely limits daily activities.”
This lingering fatigue may be due to limited production of energy within the muscles caused by damage to the mitochondria from a COVID infection. It can happen to anyone — no matter their level of fitness before infection. “I’ve treated patients who have been triathletes and now may only be able to do 15 or 20 minutes of exercise a day, when they’re used to running and swimming miles at a time,” Kaplan says.
He recommends starting slow and pacing yourself with everything you do around the house, “doing shorter intervals several times throughout the day, rather than trying to do everything at once.” Whether it gets better depends on the individual. Some people’s symptoms clear, and some people may battle them indefinitely.
2. Shortness of breath An analysis of chest CT scans from 144 patients ages 27 to 80 found that more than one-third of people hospitalized with a previous COVID infection had lung scarring and thickening two years after coming into contact with the virus. Even patients with milder cases who walked away without scarring can experience changes in their breathing.
“Some research shows that people after COVID start to take shorter, shallower breaths,” Baratta says. “This essentially causes a type of hyperventilation they are doing without even recognizing it, not getting good fresh air deep into the lungs, and [this] can lead to shortness of breath.”
Doctors have found success using respiratory exercises to help patients relearn slow, deep breathing.
3. Cognitive changes Difficulty concentrating, spaciness and forgetfulness are just a few of the brain challenges COVID can bring on. These can last for weeks or months or — in some with long COVID — become an everyday occurrence that lasts indefinitely. COVID may linger in a person’s gut long after an infection, altering their microbiome and hindering the body’s ability to produce serotonin, leading to cognitive disturbances.
COVID may also disrupt the blood-brain barrier, allowing chemicals or molecules in the rest of the body to enter the brain blood circulation and potentially lead to brain fog, Baratta says.
One study found that 30 days after testing positive for COVID-19, people were at greater risk for cognitive decline, as well as for mental health disorders including anxiety, depression and stress. Another study found inflammation in the brains of people with mild to moderate COVID-19 was similar to the effects of seven years of aging. Doctors are leading neurologically affected patients through cognitive rehabilitation exercises that show promise in reducing symptoms.
4. Depression and anxiety “Mood-related disorders are one of the top five issues that happen to people after COVID,” Baratta says. There may be a direct relationship between the virus’s effect on the brain and mood issues. A 2021 review of eight studies found that 12 weeks after a COVID infection, 11 to 28 percent of people had depression symptoms, and 3 to 12 percent of those individuals reported their symptoms as severe. If you’re feeling more stressed or down after catching COVID, tell your primary care physician, who can refer you to a therapist. Or visit the American Psychological Association’s search tool at locator.apa.org to find a qualified therapist in your area.
5. Sleep disturbances Nearly 40 percent of people with long COVID have reported major changes to their sleep patterns. One study looked at 1,056 COVID-19 patients who did not have a severe enough infection to require hospitalization. Of that population, 76.1 percent reported having insomnia and 22.8 percent severe insomnia. Sleep apnea may also appear post-COVID, another way the disease affects the respiratory system.
Talk to your doctor if you’re having sleep issues. A CPAP (continuous positive airway pressure) machine can help with sleep apnea. Lifestyle habits that prioritize healthy sleep, such as keeping consistent sleep and wake times and avoiding large meals before bed, may also help. “Post-COVID sleep has literally been a nightmare! We saw a 23 percent increase in sleeping-pill prescription during and post-COVID,” says Michael Breus, a clinical psychologist and clinical sleep specialist in Los Angeles.
6. Digestive upset Diarrhea, constipation, abdominal pain, bloating and gas: These symptoms of irritable bowel syndrome can be by-products of an encounter with COVID. A survey of 729 COVID survivors found that 29 percent experienced at least one new chronic GI symptom six months after their infection. “There is evidence that parts of the COVID virus linger in the GI tract for many months after the initial illness, and it’s been suggested that the presence of these ongoing viral fragments causes dysfunction or problems with the GI tract, leading to mostly symptoms of diarrhea and gastric distress and discomfort,” Baratta says.
Talk to your doctor about any new digestive symptoms or seek help from a gastroenterologist. You can keep a food journal and note if your condition flares after eating certain foods. Try cutting out those foods, then reintroducing them one by one to see what you react to, Kaplan advises.
7. New or worsened allergies Some people who develop COVID experience allergies they never had before. One study found the risk of developing allergic diseases, such as asthma and allergic rhinitis, rose significantly within the first 30 days after a COVID diagnosis. This may be because one’s immune system stays hypervigilant after fighting the virus, McAuley says.
In severe cases, like Chrissy Bernal’s, this can lead to mast cell activation syndrome (MCAS), a disease that can behave like a series of severe allergies: The body’s cells become hypersensitive, causing strong reactions to everything from food and pollen to even a hot shower or exercise. Antihistamines and other medications may help, so talk to your doctor if you experience skin itching, a rapid pulse, wheezing or gastrointestinal symptoms.
8. Pain Some COVID survivors battle chronic pain, everything from aching joints to testicular pain. There is a higher risk of inflammatory arthritis, and women are at higher risk than men. One review of studies estimated that 10 percent of people who contracted COVID experienced musculoskeletal pain at some point during the first year after infection.
Reducing stress, eating a healthy diet and exercising may ease some post-COVID discomfort. Massage therapy, movement therapy, acupuncture and over-the-counter pain medications may also offer relief. Your doctor can refer you to a specialist, such as a rheumatologist, who can help manage symptoms including joint pain.
Fast-moving research means new hope If your symptoms last after a bout of COVID, start with your primary care physician, who can help treat your symptoms or refer you to a specialist. Despite previous dismissals, long COVID is more recognized these days, Patel says, and the CDC is doing its part to educate both patients and providers. And initiatives such as the National Institutes of Health’s Recover program are researching treatment options.
“In a year, things will look different, because research is moving so quickly,” says Sara F. Martin, M.D., medical director of the Adult Post-Acute COVID Clinic at Vanderbilt University Medical Center. The CDC, for instance, is funding a series of clinical trials that the NIH has in the works. This new information, Martin says, may guide doctors, including herself, who treat long COVID patients to better ease their symptoms.
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#public health#still coviding#wear a respirator
23 notes
·
View notes
Text
My cat, Frisbee, is dying.
He's been losing weight for a while now. At first it was a good thing, we thought- he was a big chonker of a tubby boy, and we figured switching him from unregulated kibble whenever he felt like it to set meal times of wet food, plus running up and down the stairs of his new house after he moved to Toronto with me, was making a difference. Certainly it did, but he continued to lose weight beyond his goal of 12 pounds, and began vomiting copious amounts of bile every couple of nights.
We took him in to the vet and confirmed he was a little underweight at 10.3 pounds, and with his list of symptoms the vet was hopeful that it was either feline diabetes or hyperthyroidism, both of which are treatable. Unfortunately, his white blood cell count came back outrageously high such that he almost certainly has gastrointestinal lymphoma. Which is apparently not uncommon in middle-aged cats (he's nearly ten).
They could confirm it with an exploratory surgery, but his health is obviously suffering already and there's no guarantee he'd survive the very expensive surgery. Much less the subsequent very expensive chemotherapy which would only buy him another six months to two years, on average.
Even if I had the money for the drastic options, I don't think I'd go for it- just putting the poor guy through all that when he can't understand why we're doing it. But I don't have the money anyway, so it makes it a little easier to accept that the best thing I can do for him now is make him comfortable and happy for as long as I can.
He's got, probably, a few weeks to a few months. Possibly a little more if he responds well to anti-inflammatories and can digest a bit more of his food a bit better. That much we can do for him.
I'm going to spoil him rotten for whatever time we have left. I already spoiled him with constant cuddles and affection and treats, but now instead of an overlarge handful of treats once a day, he's getting it two or three times a day. And mealtimes are off; he meows and runs to his bowl, he gets food. Why not- it will make him happy and it might make him a little stronger. His weight certainly isn't an issue.
He's been a dear friend these past nearly ten years, there for me with his head bonks and trilling purrs and grooming my beard for me like I was a fellow cat in good times and bad. He's the best cat I've ever had, and nothing can ever replace him. But there's nothing left for me to do but to make him as happy and comfortable as I can for as long as I can, until it becomes clear that he's suffering, at which point I can grant him a painless passing with me at his side.
I'm. Not doing well, emotionally, but that's to be expected. I love this little guy more than is remotely reasonable and I'm going to miss him like a vital organ when he's gone. But until then, yeah. He gets spoiled. He deserves it.

Pictured here in better health, a floofy chonker nonpareil.
#Frisbee the cat#tw animal death#kinda want to lie down and decay into nothingness my own self#but there is still a boy to take care of for a while#and after that a spouse to comfort#and friends and family to support#so i'll get up before rot sets in
45 notes
·
View notes
Text
Strange Horticulture Inspired Headcanons
prompts inspired by some of the names, descriptions, and uses of plants from the game Strange Horticulture
Aguria - How does your muse feel about psychics? Would they ever seek one out for answers about the past, present, or future?
Bella Nox - Is your muse prone to obsessions? Do they ever become so obsessive they might forget to eat or sleep? What is their current or most recent obsession?
Brimlock - Does your muse prefer cold or warm weather? Do they travel as the season changes to avoid cold, rainy, or scorching seasons?
Burdum - Does your muse have any superstitions? Do they have any objects they consider lucky or unlucky?
Caballia - Does you muse believe in an afterlife? Do they believe their actions in their current life have any impact on what happens in the next?
Candlewood - Would your muse be considered neurodivergent? Have they been diagnosed with or treated for any sort of mental illness? How do they feel about the concept of mental health in general?
Carnivorous Torren - Does your muse eat meat? If so, would they ever consider going vegetarian or vegan? Why or why not?
Cauldery - Does your muse hunt? If so, what do they use to hunt what type of game? Do they have any sort of moral stance on the way hunting should be done?
Clavilium - Does your muse know how to pick locks? If so, how have they used this skill in the past?
Common Trouse - How good or bad is your muse's eyesight? Do they need any kind of corrective lenses to be able to see? Have they undergone any sort of surgery to correct their vision issues?
Daisy Dock - Has your muse ever experienced an event that required them to show great courage? What kind of impact did it have on them as a person?
Demmel - What sort of behaviors does your muse display when they are worried or nervous? Do they have any coping mechanisms they use to calm themselves down?
Embersoul - Where would your muse consider to be their safe space? Does it have more to do with the place itself or the people associated with the place?
Feverkiss - Does your muse depend on caffeine to make it through the day? What's their go-to form of liquid energy?
Forest Camphry - How quickly does you muse fall asleep? Are they able to sleep anywhere or do they need specific conditions to fall asleep? Do they sleep soundly or wake up multiple times over the course of the night?
Fox Button - How many friends does your muse have? Are they able to form friendships easily? How much effort do they put into maintaining friendships?
Gandyroot - Are there any foods that cause your muse gastrointestinal discomfort? Do they avoid these foods, take medicine to help with the side effects, or just eat them and suffer the consequences?
Glowhorn - Is your muse afraid of the dark? Did they sleep with a nightlight as a child? Do they as an adult? What kind of things do they imagine lurk in the dark?
Grey Sandfire - Does your muse keep up with their dental hygiene? Are they missing any teeth? Are they at all self-conscious about their smile? Have they ever had braces?
Harlequin Blue - Has your muse ever screamed in genuine terror? Did the situation scar them in any way, whether mentally or physically?
Haverage - Does your muse believe in the idea of soulmates? Have they found theirs yet or are they still looking?
Henchuck - How forgetful is your muse? Do they have any methods for reminding themselves of things?
Jacob's Worth - Has your muse ever gotten genuinely lost somewhere before? Were they able to find their way to safety/home by themselves?
Lesser Merrydock - How sharp are your muse's mental faculties? How much value do they place on their mind? How would they react if they discovered they were suffering from cognitive decline?
Lisle of Neptune - How honest is your muse? Do they believe white lies are okay? How do they handle being lied to?
Mary's Breath - How good is your muse at keeping secrets? If sworn to secrecy, is there a price someone could pay (monetary or otherwise) to get them to spill the beans? Do they trust others enough to share their own secrets?
Mellow-Glow - Does your muse ever feel invisible or ignored? How do they react to these feelings?
Mountain Astory - How persuasive is your muse? Would they ever consider going into politics or sales?
Red Abony - Does your muse have any secret hiding places? What sort of things do they hide there?
Solomon's Sceptre - Does your muse believe that witchcraft is real? Do they embrace it or are they afraid of it?
St. John's Poppy - How is your muse's hearing? Do they often engage in activities that may damage their hearing? Do they wear hearing protection?
Sunset Mountcap - Does your muse believe in ghosts? Would they ever try to communicate with ghosts or spirits?
Thum - What kinds of scents does your muse prefer when it comes to things like soaps, candles, or body sprays? Are there any popular scents they absolutely hate?
Trimblehuff - How does your muse feel about weddings? Is there a particular kind of wedding they enjoy? Do they dream about what their own will be like? Do they even want a wedding?
Wild Cole - How often does your muse drink? Do they commonly experience hangovers? Are there any cures they swear by for dealing with hangovers?
Winterbore - Is your muse the type of person to relocate a spider or kill it?
7 notes
·
View notes