#transgender healthcare analysis
Text
youtube
5 notes
·
View notes
Text
HIV research and monitoring has historically excluded transgender men, creating blind spots in understanding this group’s sexual well-being and happiness. Two recent studies—one out of New York and the other from Germany—suggest that transgender men who have sex with other men have a higher prevalence of HIV than the general population. The German analysis further finds that transgender men who have sex with other men face a host of inequities compared to cisgender gay and bisexual men, including reduced access to sexual healthcare and less satisfying sex lives.
[...] Almost three quarters of trans MSM reported their income was insufficient for them to live comfortably, compared to about half of cis MSM. The researchers note that the income disparity could be due to the trans MSM participants being younger on average, but they also suggest discrimination could play a role.
In terms of mental health, survey scores indicated both groups experienced various degrees of depression and anxiety from mild to severe. However, trans MSM were almost four times as likely to suffer from severe anxiety and depression compared to cis MSM (15% vs 5%). Furthermore, trans MSM indicated far more suicidal ideation than their cisgender counterparts (41% versus 16%).
The survey results also pointed to gaps in sexual satisfaction, with more trans MSM being unhappy with their sex life than cis MSM (34% versus 22%). Trans men more often disagreed that sex was as safe as they wanted (18% versus 11%) and indicated less ability to say no to unwanted sex (23% to 12%). Trans MSM reported fewer sexual partners than cis MSM, and the study authors propose that difficulties in finding partners due to stigma may contribute to less happiness in their sex lives.
On the whole, trans MSM also had poorer access to healthcare compared to cis MSM. Fewer had ever received either an HIV test (41% versus 24%) or an STI test (55% versus 45%). Drawing on other research, the authors suggest that one reason for this may be discrimination in healthcare settings, which may cause trans men to avoid seeking sexual health services. The authors go on to say that stereotypes, such as assuming trans men only have sex with cisgender women, may also interfere with providing adequate care. Finally, although trans MSM had higher rates of HIV than the general population, this was lower than amongst cis MSM (2.5% versus 10.7%).
A different study conducted in New York City by Dr Asa Radix and colleagues of the Callen-Lorde Community Health Center also found that HIV prevalence is higher in transgender men. In this retrospective analysis, the authors identified a racially diverse group of 577 transgender men who sought care at the facility between 2009 and 2010. Among this group of men (mean age 32 years), less than half (n=250) had ever had an HIV test. Out of the 250 individuals who had, 2.8% (n=7) tested positive for HIV, a significantly higher rate of HIV than the current US national prevalence of 0.41%. Of the 18 trans men who had sex exclusively with cis men and tested for HIV, two (11.1%) were positive.
600 notes
·
View notes
Text
I do not have the expertise or knowledge to join in the chorus of people who are accusing JK Rowling of Holocaust denial. I’ve done part 1) of my goals with this piece and explained why people are making the accusation; she was objectively wrong about a historical fact in which the Nazis burnt research into trans healthcare. But any analysis as to whether this constitutes Holocaust denialism is, in my view, best left to the experts in that field.
My expertise is in transphobia and the way it operates. I think JK Rowling’s social media activity over the last two days is an interesting case study into how bigotry constantly and confidently bullshits itself into believing it has successfully reasserted the narrative. When, in reality, any real inspection causes it to quickly fall apart.
Throughout these tweets Rowling seemingly can’t give a direct response to anything put to her. The tweet that kicked off people making these accusations is unmistakeably her disagreeing with established historical fact about the burning of Institut für Sexualwissenschaft’s research. When presented with citations by Caraballo and others demonstrating the established historical facts regarding the burning of Hirschfeld’s Institute JK Rowling’s responses get increasingly further from the point.
She moves the goalposts as facts are repeated to her, adding more conditions and hoops trans people need to prove and jump through for her to accept she was wrong in that first tweet. When this fails, she changes tactic to discrediting Hirschfeld, as if his shitty beliefs somehow make the burning of his Institute – and research into trans healthcare it contained – null and void.
Then, you get the ending; the real anxiety the she was expressing reveals itself. In my view, this is demonstrated via the tweets where Rowling expresses the belief that trans people are inserting ourselves into history and centering things around us all the time. To my eyes, its just another form of the common anti-LGBTQIA+ trope of claiming we’re asking for too much in some regard.
None of this was about historical facts. It wasn’t about the Nazis. It wasn’t about the Holocaust or any of its victims. It wasn’t about the research Magnus Hirschfeld led. It wasn’t about what a few random Twitter accounts said. It wasn’t about the lives of transgender people in early 1900s Germany.
It was, in my opinion, just a bigot being upset that trans people aren’t quiet about our erasure from history. All just one big billionaire whine that we are asking for too much by insisting that our histories aren’t erased.
Gemma Stone, via TransWritesWorld, March 2024
#anti jkr#jkr transphobia#transphobia#gemma stone#transwritesworld#holocaust denial#terf logic#joanne rowling#bigotry#twitter#social media#analysis#anti billionaire#eat the rich
12 notes
·
View notes
Text
By: Paul Terdal
Published: Jul 2, 2024
It’s understandable to want to help troubled kids. But the evidence simply isn’t there that unproven drugs and surgeries are what they need.
In our drive to eliminate health inequities, my fellow liberal Democrats and I are eager to help children who identify as transgender. This compassionate urge has led our state, Oregon, to fast-track Medicaid coverage of medical transition services for kids, including puberty-blockers, cross-sex hormones, and surgical removal of breasts and genitals. Yet I’m deeply concerned that in the push for equity, Oregon has ignored evidence, to the point of jeopardizing children’s health. I know from experience that my state can do better to ensure that kids get medically necessary care.
Oregon has long been a national and even international model for evidence-based medicine. I personally encountered my state’s strong commitment to medical science after my two young sons were diagnosed with autism in the late 2000s. At the time, few autism treatments were covered by insurance or Medicaid anywhere in America, so I worked with state leaders and a broader coalition to right that wrong. One key hurdle was Oregon’s Health Evidence Review Commission (HERC), which determines what treatments Medicaid covers and strongly influences the coverage of private health-insurance plans.
HERC held us to its customary high standards for quality of evidence. We organized testimony from some of the world’s leading experts on autism and submitted reams of peer-reviewed journal articles, all of which were rigorously scrutinized by HERC’s experts. We prevailed only after the U.S. Agency for Healthcare Research and Quality published a groundbreaking systematic review that supported the effectiveness of behavioral interventions for autistic children. In 2014, HERC approved Medicaid coverage of such treatments for children like mine. HERC’s wise focus on evidence steered patients and physicians away from risky and unproven interventions that were popular at the time, some of which, such as chelation therapy, reportedly killed autistic children. To this day, I’m grateful for the commission’s high standards.
Yet HERC hasn’t upheld the same standards for gender medicine. To its credit, the commission began looking at this issue in 2012, before gender dysphoria was on the social radar. At the time, based primarily on studies of adults over the age of 30, it concluded that there was “very poor evidence” of benefits of medical interventions for patients. Even so, HERC decided in 2014 to provide comprehensive Medicaid coverage for puberty-blockers, cross-sex hormones, and surgeries for anyone, including children, who identifies as transgender. In a strange departure from its own rules, HERC didn’t run these policies through its evidence-based-guidelines subcommittee. In my fight for autism coverage, that subcommittee was the most important part of the process.
I’m confident the commissioners were trying to help people in what was then a unique situation. At the time, in 2015, the state estimated that very few patients would choose medical transition: according to NPR, “at least 175” patients per year, of all ages. NPR quoted HERC’s medical expert as estimating that the combined total cost for this coverage would be “up to $200,000 — for the whole state.” Yet by 2019, more than 7,500 Oregonians were receiving such treatment, at a cost of over $20 million per year. Based on my analysis of state data, hundreds of children have received some combination of puberty-blockers, cross-sex hormones, and surgeries. None of these procedures have gone through clinical trials to demonstrate their safety and effectiveness, and in the case of hormones, children are receiving drugs that haven’t been approved for such use by the FDA.
Amid this exponential rise, HERC in 2023 commissioned a thorough review of the latest studies. The draft report, which I obtained via a freedom-of-information request, found that the evidence was still very limited. For youth, the investigators reported that they were unable to find any systematic reviews — the key evidence we had to provide for autism coverage — with “extractable data” showing benefits of transgender treatments for children. The report also noted that many lower-quality studies can’t be applied to patients who seek a rapid gender-affirming transition, which is typically the case with children. The report was essentially Oregon’s version of the Cass Report, which the United Kingdom released in April.
Yet Oregon’s report was never finalized, and HERC staff didn’t even present their draft to the body’s 13 commissioners. Instead, after the state passed a law requiring the coverage of “accepted standards of care” for transgender treatments, HERC quickly endorsed guidelines from an advocacy group — without any analysis of the contents. The guidelines are highly aggressive yet based on low-quality evidence. Today, preteen Oregonians can be put on powerful chemicals without FDA approval, before moving on to surgeries as adolescents. These interventions can irreversibly alter their bodies and leave them less likely or even unable to have children of their own later in life. The risks to their physical and mental health are high and, crucially, not justified by existing proof of benefit.
Equity cannot be achieved by ignoring evidence and stripping away consumer protections from historically underserved people. While I deeply sympathize with the goal of helping struggling kids, we can’t accept shortcutting medical ethics — and we didn’t accept it a decade ago, with autism coverage. The ethical path is for HERC to define “accepted standards of care” based on the best science. Medicine is supposed to follow the evidence because health and well-being hang in the balance. The stakes are especially high for children. If we truly want to be equitable, Oregon will stop undermining children’s right to evidence-based medical care.
[ Via: https://archive.today/WcL66 ]
#Leor Sapir#Paul Terdal#Health Evidence Review Commission#medical scandal#medical malpractice#medical corruption#Cass review#Cass report#gender affirming healthcare#gender affirming care#gender affirmation#puberty blockers#wrong sex hormones#cross sex hormones#evidence based medicine#religion is a mental illness
8 notes
·
View notes
Text
Okay as a disabled trans man, let me tell you how this sounds a lot better than it actually is.
The ADA is an amazing bill, it took a lot of work from disability activists to pass. It is still seen as a bit too progressive for a lot of corporate America because it requires businesses to accommodate their employees and to let disabled people use their services.
It is unique to disability because of accommodations. It needs to exist separately from other rights bills because disabled people cannot simply get equal access and have actual equality obtained. This bill is one of the few that focus on equity.
I have yet to be actually protected by the ADA as a disabled person. All of my progress and accommodations are from Section 504, which has a limited reach but is more enforced by the U.S. government.
Here are some reasons why this ruling has me incredibly conflicted:
Putting the protection under the diagnosis of gender dysphoria allows employers and other authority figures to require trans people to have that diagnosis to request "accommodations." Which will likely be seen as being able to change their name at work or school without a legal name change, go by pronouns other than their agab, use the correctly gendered spaces, etc. It puts the entire transgender identity into the hands of doctors.
Meaning that if a trans person wants to get basic respect, an employer can require them to get a doctors note for it. You need healthcare, time, and luck getting a doctor that will diagnose you if you are not already diagnosed.
This should be obvious but yeah, requesting accommodation gives employers the right to have some access to your medical records. Many people do not know that it's against the law for an employer to request medical records unrelated to disability, and employers will try to do that with trans people.
It has been stated by researchers that gender dysphoria should not be diagnosed unless specifically requested by the patient for health insurance coverage because of the stigma it causes and because how little health providers are informed on it.
This legal ruling for the United States puts all trans people under a medicalized view. It puts our rights not in our hands but in the hands of medical authority. A lot of trans people do not have a good fucking time at the doctors office despite the overwhelming support that transition should be seen as medically necessary.
It clarifies that gender dysphoria is seen as a mental disorder like other disabilities. If American society ran on the social model of disability, where disability is seen as a natural variation, this would be fine. Sadly, it runs on the medical model, where disability is seen as something to get fixed. This ruling implies that gender dysphoria is unnatural instead of a normal reaction to having a gender identity that does not match your birth-assigned one. This goes against the view that even medical practitioners take with gender dysphoria.
The ADA needs to be enforced by the individual in courts. If you are discriminated against, you need the time and money to go to court for years on something that is usually hard to prove. I got fired from a job for requesting accommodations but never did anything about it because even if I did have a case, not many lawyers would bother taking a reward from a minimum-wage job.
Small businesses (businesses with under 15 employees) do not need to abide by the ADA. At all. Under this, a small business denying trans people services is still completely legal.
"Analysis of cases decided under Title I of the Americans with Disabilities Act (ADA), which addresses employment discrimination, reveals that defendants have consistently prevailed in well over 90% of cases since the ADA’s inception."
Luckily the amended ADA in 2008 allows for the protection of those who are perceived as disabled, so even without diagnosis, there can still be a case when it comes to discrimination from strangers.
Still, even though it's disability pride month, it is not good to be lumped in with us regarding rights because often it's "hey that's illegal" and nothing comes of it. Public attitudes influence how laws are enforced, and public attitudes on disability are abysmal.
I am not trying to play the oppression Olympics, I am trying to give a good overview. This can be an improvement for some trans people, and it especially helps with the constant healthcare bans we are seeing. I am incredibly worried about this, though, and I need to share why that is.
#disability law#supreme court#transgender rights#transgender news#supreme court ruling#disability rights#americans with disabilities act#ada#transgender#trans
22 notes
·
View notes
Text
The Transgender Issue: An Argument for Justice by Shon Faye

Trans people in Britain today have become a culture war 'issue'. Despite making up less than one per cent of the country's population, they are the subjects of a toxic and increasingly polarized 'debate' which generates reliable controversy for newspapers and talk shows. This media frenzy conceals a simple fact: that we are having the wrong conversation, a conversation in which trans people themselves are reduced to a talking point and denied a meaningful voice.
In this powerful new book, Shon Faye reclaims the idea of the 'transgender issue' to uncover the reality of what it means to be trans in a transphobic society. In doing so, she provides a compelling, wide-ranging analysis of trans lives from youth to old age, exploring work, family, housing, healthcare, the prison system and trans participation in the LGBTQ+ and feminist communities, in contemporary Britain and beyond.
The Transgender Issue is a landmark work that signals the beginning of a new, healthier conversation about trans life. It is a manifesto for change, and a call for justice and solidarity between all marginalized people and minorities. Trans liberation, as Faye sees it, goes to the root of what our society is and what it could be; it offers the possibility of a more just, free and joyful world for all of us.
#the transgender issue#the transgender issue: an argument for justice#shon faye#transfem#transmasc#nonbinary#trans book of the day#trans books#queer books#bookblr#booklr
15 notes
·
View notes
Text
The Transgender Issue: An Argument for Justice by Shon Faye
goodreads

Trans people in Britain today have become a culture war 'issue'. Despite making up less than 1% of the country's population, they are the subjects of a toxic and increasingly polarised 'debate', which generates reliable controversy for newspapers and talk shows. This media frenzy conceals a simple fact: that we are having the wrong conversation, a conversation in which trans people themselves are reduced to a talking point and denied a meaningful voice.
In this powerful new book, Shon Faye reclaims the idea of the 'transgender issue' to uncover the reality of what it means to be trans in a transphobic society. In doing so, she provides a compelling, wide-ranging analysis of trans lives from youth to old age, exploring work, family, housing, healthcare, the prison system, and trans participation in the LGBTQ+ and feminist communities, in contemporary Britain and beyond.
The Transgender Issue is a landmark work that signals the beginning of a new, healthier conversation about trans life. It is a manifesto for change, and a call for justice and solidarity between all marginalised people and minorities. Trans liberation, as Faye sees it, goes to the root of what our society is and what it could be; it offers the possibility of a more just, free and joyful world for all of us.
Mod opinion: I've read this book and it's really good and interesting.
#the transgender issue#shon faye#polls#trans lit#trans literature#trans books#lgbt lit#lgbt literature#lgbt books#nonfiction#feminism#politics#own voices
5 notes
·
View notes
Text
Florida’s newest Boards of Medicine appointees wrote an anti-trans letter calling for gender “exploratory” therapy, citing a report of a trans teenager being involuntarily hospitalized for nearly two years
Previously:
Gender Analysis calls for a hearing on the Florida Board of Medicine and Board of Osteopathic Medicine proposed trans youth care bans 64B8–9.019 and 64B15–14.014 F.A.C.
Anti-trans group SEGM’s cofounder Stephen Beck is an executive at Bon Secours Mercy Health, the fifth-largest Catholic healthcare network in the US
Background
On December 2, 2022, Governor Ron DeSantis appointed pediatric endocrinologist Dr. Monica M. Mortensen to the Florida Board of Osteopathic Medicine, followed by the appointment of pediatric endocrinologist Dr. Matthew R. Benson to the Board of Medicine on December 28. Benson previously spoke in favor of the state Medicaid trans care exclusion Rule 59G-1.050(7) at a July 8, 2022 AHCA meeting, and coauthored a September 23 letter to the Boards of Medicine with Mortensen and seven others in support of the trans youth care bans 64B8–9.019 and 64B15–14.014.
Benson and Mortensen’s positions are relevant to an ongoing issue: although the Boards of Medicine voted to advance the trans youth care ban at the November 4 meeting, it has not yet taken effect. Another joint meeting on the ban will now take place on February 10 in response to calls for a rule hearing from Southern Legal Counsel, ACLU of Florida, Gender Analysis and others. Public comment is now open for the upcoming hearing until February 7 at [email protected]. Benson and Mortensen’s letter provides important clues to how they will likely approach this rule and other issues involving gender-affirming care as Board members, and this letter warrants extended analysis.
The September 23, 2022 letter to the Boards of Medicine (“Benson letter”)
Benson and Mortensen’s letter was coauthored with seven other pediatric endocrinologists and pediatric endocrine nurse practitioners working at Nemours Children’s Health Jacksonville: Larry A. Fox, Rehem Hasan, Nelly Mauras, Lournaris Torres-Santiago, Lydia Snyder, Joseph W. Permuy, and Kaley Carroll (“An Open Letter to the Florida Board of Medicine: Regarding the Proposed Rules to Limit the Use of Hormonal and Surgical Care for Gender Variant Youth”, pp. 1308–1313 of October 28 meeting public materials). Benson’s background includes research in the use of GnRH analogues to treat central precocious puberty in cisgender children (Benson et al., 2021), while Mortensen was involved in providing medical and psychological records of an adolescent trans boy treated at Nemours Jacksonville in the case Adams v. School Board of St. Johns County in 2017 (Expert report of Diane Ehrensaft, 21 Sep 2017). The Benson letter repeats several common anti-trans talking points that have featured heavily throughout the rulemaking process, including:
Arguing for any gender-affirming medical treatment of trans minors to be restricted to “high-quality research protocols approved by an IRB” (para 9).
Citing Dhejne et al. (2011), a study of transgender adults from 1973 to 2003, to assert that adolescents who transition are at risk of “persistently high rates of suicide, depression and premature death” (para 7).
Asserting that the practices of Sweden, Finland, France, and the UK support adoption of highly restrictive regulations of trans youth care in Florida (paras 3, 9).
Relying on a flawed and widely criticized review of transition treatments commissioned by the state of Florida (para 8), which was conducted far outside the usual standards for the authors’ evidence reviews (see section 9) as well as outside the normal Florida Medicaid processes for making a coverage determination.
Claiming that evidence supporting transition treatments is “mostly low quality and largely expert opinion, which is among the lowest level of medical evidence”, with “limited data from prospective, controlled trials, which are the gold-standard by which we judge any therapeutic intervention” (para 2).
Arguing for “nonjudgmental exploratory psychodynamic therapy in gender-dysphoric youth” as an alternative to transitioning (para 10).
The letter features a number of erroneous claims and misinterpretations of evidence, and Benson et al. rely on mostly low-quality sources to support their arguments.
Exploring “exploratory therapy”
“Gender exploratory therapy” is a recent term for non-affirming prolonged psychotherapy for trans youth and adults (Ashley, 2022), now frequently promoted by the closely connected anti-trans groups Society for Evidence-Based Gender Medicine (SEGM) and Gender Exploratory Therapy Association (GETA). These groups, emerging in only the last few years, repeatedly assert that “exploratory therapy” is not an anti-gay or anti-trans conversion therapy — while at the same time campaigning against conversion therapy bans (see section 4) and claiming that this psychotherapy may cause gender dysphoria to resolve without a need for gender-affirming treatment.
Benson and Mortensen cite five sources in support of their call for “exploratory psychodynamic therapy”:
We also support the expansion of competent expert psychological support with rapid implementation of nonjudgmental exploratory psychodynamic therapy in gender-dysphoric youth [7–11].
7: Levine, S. B., & Lothstein, L. (1981). Transsexualism or the gender dysphoria syndromes. Journal of Sex and Marital Therapy, 7(2), 85–113. https://doi.org/10.1080/00926238108406096
8: Davenport, C. W., & Harrison, S. I. (1977). Gender identity change in a female adolescent transsexual. Archives of Sexual Behavior, 6(4), 327–340. https://doi.org/10.1007/BF01541204
9: Churcher Clarke, A., & Spiliadis, A. (2019). ‘Taking the lid off the box’: the value of extended clinical assessment for adolescents presenting with gender identity difficulties. Clinical Child Psychology and Psychiatry, 24(2), 338–352. https://doi.org/10.1177/1359104518825288
10: D’Angelo, R., Syrulnik, E., Ayad, S., Marchiano, L., Kenny, D. T., & Clarke, P. (2021). One size does not fit all: in support of psychotherapy for gender dysphoria. Archives of Sexual Behavior, 50(1), 7–16. https://doi.org/10.1007/s10508-020-01844-2
11: Lemma, A. (2018). Trans-itory identities: some psychoanalytic reflections on transgender identities. International Journal of Psychiatry, 99(5), 1089–1106. https://doi.org/10.1080/00207578.2018.1489710
Levine & Lothstein (1981) is a case series of transgender adults in the 1970s; uncontrolled case series are considered one of the lowest “levels” of evidence in most evidence hierarchies (Stony Brook University, 2022). Churcher Clarke & Spiliadis (2019) and Lemma (2018) are also small case series of patients (12 and 2 subjects, respectively). Davenport & Harrison (1977) consists of a single case report of an adolescent, and D’Angelo et al. (2021) is a letter to the editor by six members of SEGM; this expert opinion is generally considered even lower in the hierarchy of evidence than case series or case reports.
While Davenport & Harrison (1977) long predates any formalization of “gender exploratory therapy”, the treatment described appears extreme and alarming. The abstract states that this consisted of “two years of individual and milieu therapy” for a 14.5-year-old trans boy, but the authors later explain that this took place at an inpatient psychiatric facility:
In accordance with those treatment goals, the patient was admitted to an inpatient psychiatric hospital for adolescents, where she remained for 20 months. In the hospital she was involved in triweekly, individual psychotherapy with a male therapist and milieu therapy. The milieu therapy included active intervention by psychiatric nurses and aides, therapeutic school, recreational therapy, and occupational therapy geared specifically toward adolescents. The patients admitted to this service manifest a wide variety of adolescent pathology. Approximately two-thirds of the patients are short-term admissions and one-third remain in residential treatment for prolonged periods of time.
It then becomes clear that this confinement was involuntary and distressing:
Her severe social withdrawal was striking, and she spent much of the time in her room avoiding both staff and other patients. … There seemed to be a quality of stubbornness demonstrated in her refusal of hospital activity and withholding of information in interviews. When first admitted, she refused to eat, and seemed to be using this to pressure her parents to sign her out of the hospital. Signs of anxiety, however, were also clear, and weeks later she was able to acknowledge in psychotherapy that she was scared and did not have any appetite.
…
She talked also about being angry about being in the hospital, having to come to psychotherapy and not knowing what to say. The material about cross-dressing again arose. Her cousin was getting married and there was to be a formal party to which she was invited. However, she knew that this would entail wearing a dress. She marked her ambivalence by saying that one way to avoid the problem would be to run away and then be restricted to the ward.
…
She then returned to the hard line: there was no conflict, she just had gotten the wrong body, when was the therapist going to quit bugging her by keeping her in the hospital? She began missing appointments and only returned when her milieu manager said if she did not go to therapy she would lose privileges, including weekend passes.
…
Her favorite female staff member was leaving, which aroused feelings of abandonment. She said that she wanted to leave the hospital when the staff member did, but her father would not permit it until she saw herself as a girl.
Psychiatric hospitalization from ages 14–16 is a drastic intervention, especially in cases where there isn’t actually any mental or behavioral disorder that disrupts normal functioning to the point of requiring treatment under constant supervision and confinement. TASN School Mental Health Initiative (2016) describes some circumstances in which children may be hospitalized for psychiatric reasons:
Severe mental disorders are associated with a variety of symptoms that disrupt life at home and at school. Not all mental disorders require hospitalization. However, when a child or youth manifests such symptoms as hallucinations, threatens to self-harm or harm others, and/or has not eaten or slept for days, psychiatric hospitalization is a common reaction.
Being trans — identifying as a gender different from one’s assigned sex — is not like a hallucination, endangering oneself or others, or otherwise acting in a way that requires continuous monitoring by professionals. Trans youth and adults accept and embrace their identities as trans people all the time and have done so for decades, broadly to the benefit of their own well-being and sense of self, and generally with no need for psychiatric hospitalization in relation to this or any other matter.
Benson et al. assert in their letter that “data are lacking on the long-term safety and efficacy of the prescribed treatments” of puberty blockers and HRT (para 3), and they contend that “These decisions are too critical and important for young children to make as they cannot easily comprehend the long-term ramifications” (para 14). However, they fail to address the long-term developmental and psychosocial impacts of being involuntarily held in a residential psychiatric facility for almost two years in the middle of adolescence. This near-total separation from one’s family, community, and peers from ages 14–16 jeopardizes an adolescent’s well-being in ways that simply do not apply to trans youth who receive gender-affirming medical treatment while being welcomed in their communities. Tougas et al. (2022) describe a variety of adverse impacts on youth hospitalized in a psychiatric facility:
In the United States and Canada, it is estimated that close to one third are rehospitalized in the year following discharge (2- 6). Moreover, in addition to high social costs (7–8), youth hospitalizations may result in serious academic and social difficulties (e.g., absenteeism, social isolation, stigma, bullying, difficulty managing psychiatric symptoms, low academic performance, motivational problems, dropouts; 9–11).
This is a massive tradeoff of quality of life, particularly when hospitalization is not apparently necessary for any reason. A child kept in an inpatient facility during this time will miss out on countless milestones and memories that are irreplaceable, but this study seems to argue that this is preferable over freely enjoying your teenage years as a trans person with your friends, schoolmates, family, and others in a normal community setting.
The case report is also not an instance of “nonjudgmental” therapy as claimed by Benson et al. Although this patient wanted to leave the hospital, their parents would not allow this “until she saw herself as a girl”. The report goes on to describe hospital staff reinforcing “feminine traits” and “feminine behavior”, encouraging the patient to identify with their mother, and providing “therapy for her dread of femininity, which she had needed”:
Near the end of the first year of hospitalization, we had begun gradually to recognize feminine traits and to reinforce them. Her attempts to avoid being involved with the girls’ group were confronted, and she was seemingly merging with that group.
…
She began to experiment with “feminine” behavior, and this was encouraged and supported by staff.
…
In reality, the father was psychologically and physically absent; his appearance of strength was based on degrading the mother and the maternal role. Certainly the patient’s recognition of the true dynamics made identification with her mother more possible. It helped the patient take another look at the role of women and to see her parents’ marital situation as pathological and not like that of most families.
…
Therefore, she could now participate in the therapy for her dread of femininity, which she had needed but could not previously acknowledge.
Finally, note should be made of the role of the milieu staff in the treatment. They were able early in hospitalization to get her involved in the adolescent issues that are current on an adolescent service. They were very supportive of her feminine behavior and tactfully reinforced it during the second year in hospital when this was appropriate.
It’s clear that any “exploratory” therapy here was done with a fixed destination in mind: identifying with one’s assigned sex, and no longer requesting any gender-affirming care. This was a gender identity change effort directed toward establishing a cisgender identity, which is encompassed by the widely understood meaning of conversion therapy. Major medical and professional organizations recognize that conversion therapy is ineffective and dangerous (Forsythe et al., 2022), and a United Nations independent expert has described conversion therapy as “inherently discriminatory” and “cruel, inhuman and degrading treatment” (UN OHCHR, 2020).
The treatment of a trans adolescent described by Davenport & Harrison may actually constitute a serious human rights violation. Even if an “expansion” and “rapid implementation” of long-term psychiatric hospitalization for thousands of new teenage patients was at all feasible or realistic, its use for this purpose would be completely immoral and ethically unacceptable. Being transgender, and identifying as such, is fundamentally not a treatable “illness”. As a trans woman living in Florida, I fervently hope that this pathologizing perspective will not be represented at the Boards of Medicine by Benson and Mortensen.
Familiar faces: Dr. Stephen B. Levine
The remaining four sources cited by Benson et al. to support “exploratory” therapy at least do not describe involuntarily hospitalizing us in psychiatric wards until we stop saying we’re trans. Regardless, they still fail to provide any high-quality evidence supporting this exploratory psychotherapy in its own right, let alone as any kind of replacement for gender-affirming care. Levine & Lothstein (1981) is a case series of 150 transgender adults — the authors describe a minimum age of 21 for a diagnosis of gender dysphoria. This is a distinctly different population from the trans minors in Florida whose access to gender-affirming care is now being jeopardized by the Boards of Medicine. The authors also do not provide any detailed information on the overall outcomes of their patients who were treated with gender-affirming care or alternative psychotherapies. Instead, the study describes the baseline co-occurring mental health conditions of 51 adult trans women and 18 adult trans men, with 7 case vignettes, and only “overall impressions” of the patient population undergoing gender-affirming surgery at Case Western Reserve University. Only one of these vignettes illustrated an apparent disappearance of gender dysphoria following psychotherapy.
Levine & Lothstein acknowledge the shortcomings in the evidence base for psychotherapies to eliminate gender dysphoria:
These clinical impressions have not been documented by systematic studies. There have been numerous published case reports of apparent “cures,” and fewer papers by clinicians who have seen large numbers of patients but do not report on any one case in considerable detail. The latter group contains accounts of patients who improved in many ways but were not cured of their gender problems.
The psychotherapy they’re proposing is also not a “nonjudgmental” therapy. The authors posit “realistic” goals for trans patients:
Some realistic goals for gender patients include: strengthening the patient’s heterosexuality; decreasing the frequency of cross-dressing; enabling a comfortable acceptance of a homosexual life style.
All of these goals — being straight and cisgender, gay and cisgender, or cis without “cross-dressing” — are formulated with the intention of discouraging gender-diverse expression and identifying as transgender. This, too, is a gender identity change effort that can fall within the definition of conversion therapy.
Notably, the authors provide several arguments against prohibition of gender-affirming care or restriction to narrow clinical research settings as proposed by Benson et al.:
Prohibition of SRS in the United States. Some patients would seek a foreign source, but others might be totally dissuaded from the idea of surgery. Many professionals are familiar with patients who have “seen the light” about their gender identities after some media exposure to transsexualism. If SRS receives less publicity, patients may be forced to find nontranssexual solutions. Such an approach may actually be unethical, since SRS appears to help some patients. Should the moral objections of some citizens deprive others of potentially beneficial medical treatment?
…
Restriction of SRS to centers involved in a multiuniversity research project aimed at answering relevant clinical questions. This rational approach might yield significant new knowledge within five years. Given the current economic climate, however, it seems unlikely that the federal government, or any other granting agency, would fund research on a problem that is relatively rare, personally unsavory, and politically controversial.
What Benson and Mortensen are proposing would similarly amount to a de facto ban on any such care by effectively regulating it out of existence. Far from the “judicious pause” that Benson et al. request, this would be utterly disruptive to the status quo, where trans youth are able to receive these treatments as a matter of private clinical decisionmaking between themselves, their healthcare providers, and their parents or guardians.
After 1981, coauthor Stephen B. Levine has continued to contribute to the scientific literature, public discourse, and legal debate on gender-affirming care and non-affirming psychotherapies. In several cases, Levine has testified against allowing incarcerated trans women to receive gender-affirming surgery, and has more recently offered numerous expert declarations stating that reversible social transition causes persistence of gender dysphoria into adolescence. This claim relies on his misinterpretation of the findings of Steensma et al. (2013), a study which only examined associations rather than causation, and found only a minimal association in trans girls and no association at all for trans boys.
Levine has accepted thousands of dollars from SEGM to write and publish articles against informed consent for gender-affirming care (Deposition in Fain v. Crouch, 27 Apr 2022, p. 30):
Q: Okay. And what about to, did you receive any grants to research or publish about the treatment of gender dysphoria?
A: I received a $5,000 grant to publish, to work on, to develop an article on informed consent which of course involves the treatment of people with gender dysphoria.
Q: And what’s the name of that grant?
A: It’s from the Society for Evidence Based Gender Medicine and I, I, I don’t really have a, I don’t know the answer any further than that, that is a grant number or something, I couldn’t tell you.
Levine frequently coauthors commentary against gender-affirming care with SEGM cofounder Julia W. Mason (Levine et al. 2022a; Levine et al. 2022b; Abbruzzese et al. 2023), and recently coauthored GETA’s “clinical guide” to exploratory therapy with SEGM’s Roberto D’Angelo, Sasha Ayad, Lisa Marchiano, and Dianna T. Kenny, as well as Genspect founder Stella O’Malley (Ayad et al., 2022). Levine also disclosed that he is a clinical supervisor of Miriam Grossman (Deposition in Brandt v. Rutledge, 26 May 2022, p. 34), who has worked as an anti-trans expert for the Florida AHCA and has previously endorsed anti-gay conversion therapy.
In contrast to his public-facing work, Levine was remarkably candid about the state of evidence for non-affirming or exploratory psychotherapy during deposition in Kadel v. Folwell (pp. 109–110):
Q: Okay. Understood. And as for your more conservative approach, can you cite to any studies or research that resulted in better outcomes than people who adhere strictly to the WPATH standards of care version 7?
A: No. This is part of the problem in the field for — although there are alternative approaches, there’s no randomized controlled study of any approach, including those which the standards of care seem to endorse. But the alternative approaches are equally deficient scientifically and are just like many people who are advocates are based on anecdotal evidence.
Q: Sorry. I missed the last part of that. You said your approach as well is not — has no controlled studies or support in that way?
Mr. KNEPPER: Objection, form.
A: Not only does it have no controlled studies, it has no systematic follow up based upon prior agreements about how we’re going to evaluate those things.
Benson and Mortensen’s own source attests, in 1981 and again in 2021, that this alternative of exploratory psychotherapy does not have an empirical basis sufficient to meet their high standards for evidence. In his foreword to a book coauthored by SEGM cofounder Marcus Evans (Evans & Evans, 2021), Levine describes the benefits of these psychotherapies as a matter of “faith” rather than “compelling data”:
What is known about the outcome of psychotherapies for trans-identified young people and adolescents? This book’s erudite chapters about highly defensive intrapsychic development provide evidence that some psychotherapies can enable some patients to decide to desist from a trans identity. Those of us who have faith in the benefit of such work regardless of the patients’ ultimate decisions about their gender expressions do not have compelling data to support our faith.
Where does faith sit within the levels of evidence? “Mostly low quality and largely expert opinion” would be too generous for this. As state regulatory agencies, the Boards of Medicine are intended to make policy and decisions based on compelling data, not unconditional faith. Faith-based policymaking at the Boards of Medicine would be unacceptable under any circumstances, but especially when this is used to disrupt access to real medicine in favor of promoting an unproven alternative therapy that runs on confidence instead of evidence.
A core group: D’Angelo, Syrulnik, Ayad, Marchiano, Kenny, & Clarke (2021)
D’Angelo et al. (2021) is a letter to the editor by six members of SEGM:
Roberto D’Angelo. D’Angelo is president of SEGM, an advisor to the closely related anti-trans group Genspect, and coauthor of the 2022 GETA clinical guide. Before his work with SEGM, D’Angelo served as the adversarial expert psychiatrist on behalf of a trans girl’s disapproving mother in the Australian case Re Imogen (para 4). This is notable as an early instance in which a core SEGM member directly attempted to interfere with a trans child’s gender-affirming care, in favor of imposing “psychotherapy and psychodynamic psychiatry” and “‘agenda free’ psychological exploration” (paras 174, 219). During the case, D’Angelo argued to the family court that Imogen, a 16-year-old trans girl, should be taken off her estrogen for at least one year to undergo weekly “intensive psychotherapy” (para 218). Imogen’s mother had a history of being physically violent to her (para 128) and had attempted to file complaints against her medical providers (para 244). D’Angelo sought to diagnose Imogen as having complex post-traumatic stress disorder rather than gender dysphoria (paras 170, 174) on the basis of “two online interviews” (para 182). Imogen’s mother then argued that Imogen was not competent to consent to gender-affirming care because she had not volunteered to D’Angelo that she had ordered estradiol from overseas (para 196). However, the court recognized that “Imogen did not want any medical information shared with her mother and she knew if she told Dr D’Angelo about the overseas drug, that information would be shared with her mother” (para 196). The court ultimately found that Imogen was competent to consent to treatment, setting a crucial precedent in Australia to protect access to gender-affirming care for youth. Elsewhere, D’Angelo has contributed a chapter to the anti-trans book “Inventing Transgender Children and Young People” (D’Angelo, 2019a), published a case report of a trans adult who “no longer believes he is a man” following psychotherapy D’Angelo (2019b), coauthored commentary with four other SEGM members (Clayton et al., 2021) and coauthored a letter to the editor with four SEGM cofounders (Malone et al., 2021).
Ema Syrulnik. Syrulnik is a healthcare data analytics expert who assisted with Clayton et al. (2021) and received an acknowledgment in Evans & Evans (2021). A 13 Jan 2023 privilege log in the Florida Medicaid trans care exclusion case Dekker v. Weida (previously Dekker v. Marstiller) shows that then-assistant deputy secretary Jason C. Weida emailed Ema Syrulnik on June 29, 2022 regarding “RE: Followup thoughts” (Plaintiffs’ motion to compel production, 20 Jan 2023). The privilege note describes Syrulnik as a consultant: “Email between General Counsel, Chief of Staff, and consultant regarding GAPMS Report.” This correspondence followed SEGM member Romina Brignardello-Petersen and SEGM associate Quentin L. Van Meter contributing two anti-trans expert reports for Florida AHCA on May 16–17, 2022, and the appointment of SEGM member Patrick K. Hunter to the Florida Board of Medicine on June 17, 2022.
Sasha Ayad. Ayad is a psychotherapist whose practice, Inspired Teen Therapy, provides “individualized therapy and parent coaching around adolescent gender identity issues” and advertises tiered monthly subscription memberships for parents of trans and gender-questioning youth. She describes herself as a founding board member of GETA, Genspect, and the International Association of Therapists for Desisters and Detransitioners. Ayad also serves on the board of the Institute for Comprehensive Gender Dysphoria Research with Roberto D’Angelo, Lisa Marchiano, and Stella O’Malley, and is lead author of the GETA clinical guide.
Lisa Marchiano. Marchiano assisted Lisa Littman in developing her “rapid onset gender dysphoria” study (Littman, 2018), defended Evans & Evans (2021) with Roberto D’Angelo (D’Angelo, Marchiano & Gorin, 2022), and is a coauthor of the GETA clinical guide. She has described the emergence of trans youth in terms such as “outbreak”, “psychic epidemic” (Marchiano, 2017), and “modern hysteria” (Marchiano, 2022). Health Liberation Now! has identified Marchiano, Ayad, and Stella O’Malley as constituting a “core trio” substantially responsible for the founding or development of nine highly similar anti-trans groups over the past five years (Leveille, 2022).
Dianna T. Kenny. Kenny is an Australian psychologist who contributed a chapter to “Inventing Transgender Children and Young People” (Kenny, 2019), coauthored the GETA clinical guide, and was paid $75,000 by the state of Alabama to provide an anti-trans expert report in Eknes-Tucker v. Ivey (now Boe v. Marshall). Kenny has described trans youth coming out, and even gender-affirming medical care itself, as “social contagions” (Kenny, 2021).
Patrick Clarke. Clarke is an Australian psychiatrist who coauthored Clayton et al. (2021) and submitted an October 2022 letter to the Icelandic parliament arguing against a ban on conversion therapy, claiming to be “greatly concerned that this Bill will result in ethical, neutral psychotherapies being conflated with Conversion Therapy”.
The article is a letter to the editor rather than a study with any original research findings or systematic synthesis of evidence, and this expert opinion would be among the lowest levels of evidence as described by Benson and Mortensen. D’Angelo et al. is mostly an argument against the findings of Turban et al. (2020) that gender identity change efforts are harmful, against that study’s use of the 2015 US Trans Survey, and against using the USTS as a source generally. This is a criticism of one publication’s methodology, not a refutation or even an engagement with the substantial overall body of evidence showing that sexual orientation and gender identity conversion therapies are ineffective and harmful. Were D’Angelo et al. to prevail in their argument that Turban et al. is an unreliable study, this would still do nothing to provide positive evidence that gender identity change efforts are themselves safe or likely to be effective. Elsewhere, SEGM members Stephen Levine, Ema Abbruzzese and Julia Mason briefly described the “evidence that psychotherapy can ameliorate gender distress in youth” as “low quality” (Levine et al., 2022b), but this is only mentioned informally and in passing. It is not the conclusion of any kind of systematic review that would rank this evidence as being even of low quality, rather than very low quality or completely excluded from consideration.
D’Angelo et al. refer to case reports of psychotherapy resolving gender dysphoria, citing the same Churcher Clarke & Spiliadis (2019) and Lemma (2018) sources as Benson and Mortensen:
Further, GD can present as a transient symptom that resolves spontaneously or in the context of developmentally informed psychotherapeutic treatment. Some common examples of transient gender-dysphoric states include adolescents girls, often on the autism spectrum, experiencing distress around the physical and social changes of puberty or gender-non-conforming young women struggling with shame about being seen as “butch.” These individuals, searching for ways to understand and remedy their distress, can incorrectly attribute their discomfort to being transgender. Several case reports (Churcher Clarke & Spiliadis, 2019; Lemma, 2018; Spiliadis, 2019) indicate that the distress of young people with GD can lessen or resolve with appropriate psychotherapeutic interventions that address the central issues.
Lemma (2018) is a case series of two patients: an adult trans man who stated he did not regret transitioning, and a trans boy who did not want to be in therapy (“She said she was seeing me only because her parents would not let her take hormones unless she saw me”). Churcher Clarke & Spiliadis (2019) is a case series of 12 patients, with crucial limitations; the authors state “the majority had not received a formal diagnosis of GD”, and 7 had not socially transitioned. By the conclusion of this study, 5 still identified as transgender. Worryingly, one of the study’s success stories appears to be a 14-year-old publicly performing masculinity for reasons of safety, while continuing to experience unresolved distress:
He spoke openly about continuing to feel confused about his identity and was still struggling with low mood, although his suicidal thoughts had decreased. However, in relation to gender, Alfie was reflective in talking about the ways he understood himself to be a vulnerable and sensitive young person, alongside the need to embody and perform masculinity differently across different contexts; to be read as a ‘guy’ in particular ways in public (Butler, 2004; Kimmel, 2004). He connected this to preserving his own safety as a non-stereotypically masculine young man. Clinicians understood these changes as signifying Alfie developing a more integrated sense of self.
Coauthor Anastassis Spiliadis serves on the board of the Institute for Comprehensive Gender Dysphoria Research with D’Angelo, Ayad, and Marchiano, and has repeatedly referred to “Gender Exploratory Therapy” or “Gender Exploratory Model” as though these were trademarked terms. In the UK, Spiliadis’ application in 2021 to trademark “Gender Exploratory Therapy” and “Gender Exploratory Approach” was refused. The services intended to be associated with the trademark were listed as training courses, workshops, and seminars, as well as psychotherapy:
Class 41
Training consultancy;Postgraduate training courses;Conducting training seminars;Provision of training;Educational and training services;Training;Training and further training consultancy;Training services;Continuous training;Practical training;Training courses;Providing training;Conducting workshops [training];Organisation of training;Education and training;Providing of training;Organisation of training seminars.
Class 44
Psychotherapy;Psychotherapy services.
Spiliadis and coauthor Anna Churcher Clarke also work at “Explore Consultation”, a group now conducting training seminars on gender exploratory therapy for the South London and Maudsley NHS Mental Health Trust in England. D’Angelo et al. similarly endorse an “exploratory psychotherapy that is neither ‘affirmation’ nor ‘conversion’”, repeatedly positioning this “non-affirmation-non-conversion” as “agenda-free evaluation”, “agenda-free psychotherapy”, or “agenda-free, neutral therapy”. It is nonsensical and unwarranted for anyone to position themselves as being “agenda-free” here, as though they are uniquely outside of a system of influences, assumptions, and attitudes that inform how all of us approach questions of transgender identities and gender-affirming care. In particular, there is nothing agenda-free about “non-affirmation”, because there is nothing agenda-free about refusing to recognize or address a trans person as their name and gender. Certainly it was not “agenda-free” for Roberto D’Angelo to argue before a family court that a 16-year-old trans girl should be deprived of her HRT for a year or more. Remarkably, D’Angelo et al. argue that trans people cannot be trusted when we say we were subjected to conversion therapy, because we may be mistaken or unreliable due to mental illness:
Further, patients with psychiatric diagnoses, highly prevalent in transgender-identifying populations (Gijs, van der Putten-Bierman, & De Cuypere, 2013; Goodman & Nash, 2018; Wanta, Niforatos, Durbak, Viguera, & Altinay, 2019), can potentially experience or misinterpret neutral interpersonal interactions as invalidating or rejecting (Barnow et al., 2009; Beck & Bredemeier, 2016; Gotlib, 1983). Not only does the survey question provide no detail to help discriminate between these essential therapy encounters and unethical conversion therapy, but it arguably biases the recall of neutral encounters toward recall of conversion by using emotionally charged language (e.g., “stop you being trans”) and by conflating recall of religiously motivated encounters with clinical ones. … As we have demonstrated, it is not uncommon for agenda-free, neutral therapy interventions to be experienced by the subjects as non-affirmative. However, non-affirmative is not the same as “conversion,” as the latter implies a therapist agenda and an aim for a fixed outcome (American Psychological Association, 2015).
It is hardly “agenda-free” to argue that cisgender healthcare professionals should be believed over vulnerable trans patients when we say that we experienced conversion therapy. In their conclusion, D’Angelo et al. openly acknowledge their specific agenda for treatment:
We call on the scientific community to resist the stigmatization of psychotherapy for GD and to support rigorous outcome research investigating the effectiveness of various psychological treatments aimed at ameliorating or resolving GD.
In depositions in B.P.J. v. West Virginia State Board of Education and Brandt v. Rutledge, Stephen Levine describes presenting an American Psychiatric Association symposium on May 24, 2022 with Sasha Ayad, Lisa Marchiano, and Ken Zucker (Deposition in BPJ v. WV, p. 89):
A: I forgot to tell you. I also sometimes am invited to give continuing education lectures. And, for example, at the — I’ve given courses, for seven years in a row, at the American Psychiatric Association on sex and love, mostly love I use as — as the title, and we talk about sexual problems and the barriers to loving. And this year’s APA meeting, I — I am presenting a symposium with three colleagues on whether or not this is time to reexamine the best practices for transgender youth. So all those things are — in my review, are — are my teaching.
Q: I was going to ask you about the May presentation. Who are your copresenters for that?
A: Sasha Ayad, Lisa Marciano and Ken Zucker.
Levine later explained the agenda of this psychotherapy — “helping people to desist” (Deposition in Brandt v. Rutledge, p. 238):
A: Yes. I just came from a symposium two days ago where two people talked about their psychotherapy helping people to desist, what we call desist or detransition through psychotherapy. So these are, again, anecdotal reports. Basically psychiatry has a lot of those anecdotal reports.
Q: Who were those clinicians or those that spoke about their experience?
A: You want their names?
Q: Yes, please.
A: One was Sasha Ayad and the other was Lisa Marchiano.
In B.P.J. v. West Virginia, Levine agreed he was trying to dissuade people from being transgender (pp. 237–238):
Q: No, no, I — I — I just want to know the basis for these — these paragraphs, so I appreciate you telling me that. My question is — you know, I read 202 and 203, and you say — you list various perceived harms and challenges from being transgender; is that fair?
A: Yes.
Q: What I’m confused about is, is this premised on the notion that there’s a way to dissuade someone from being transgender so that they don’t have these outcomes?
A: Exactly. I — this is what I’m trying to do.
Additionally, during deposition in Kadel v. Folwell, Levine explained that “people in SEGM are biased in the direction of being conservative and providing psychotherapeutic evaluations of the child, of the teenager and of their parents” (p. 112); in B.P.J. v. West Virginia, he stated “Parents would very much like me to be able to return their child efficiently and quickly … to a cis state” (p. 221). AHCA expert report contributor Quentin Van Meter described his work with SEGM at the God’s Voice conference in June 2022, claiming that SEGM members “all agree” that even social transition is an “abomination” for trans and gender-diverse youth:
[53:23] QUENTIN L. VAN METER: So there are little chinks in the armor that are starting to form. There’s a group called the Society of Evidence-Based Gender Medicine, SEGM. You should look them up because they are a reference, a beautiful scientifically-based reference group, that has a broad clinical spectrum of politics in terms of the backgrounds of these individuals. But what we all agree on is that the affirmation, from social to medical to surgical, is an abomination for these children, it is the wrong thing to do.
Exploratory psychotherapy is not “nonjudgmental”, “agenda-free”, or “neutral” if it considers the outcome of living openly as a trans person to be an “abomination”. Are trans people merely “patients with psychiatric diagnoses” who “misinterpret” this “neutral” stance by psychotherapists as “invalidating or rejecting”? This is the contention of D’Angelo et al., who ask readers to ignore SEGM members’ own documented activities and statements demonstrating an intended therapeutic outcome of desistance or detransition, and instead attribute any appearance of conversion therapy to the alleged mental incapacity of the trans community generally. This insulting dismissal of the trans population and thousands of respondents to the 2015 USTS, as though we are unable to recognize conversion therapy when we are subjected to it, is not agenda-free. It is an agenda of gaslighting a community whose medically necessary healthcare has been directly targeted and disrupted by members of SEGM in several states and countries. Such an agenda should not have any place on the Florida Boards of Medicine, and if Matthew Benson and Monica Mortensen continue to promote this “non-affirming” psychotherapy, every effort must be made to reveal this practice for what it is: anti-trans conversion therapy.
Support Gender Analysis on Patreon
14 notes
·
View notes
Text
[Vent ahead go ahead and ignore. Suicide mention]
Im doing my exams project on transgender healthcare, specifically, how we can improve it. Ive been reading international scholar articles for the past few days for my work and analysis; its hermeneutic and inductive.
I finally get to one from my own country and read an issue out of a well-known nursing scholar paper and turn the page.. in the corner, there's a short text depicting that transgender people are 8 times more likely to commit suicide.
At that moment, unfair as it may be, im just hit with this.. deep bone sorrow. Irrational thoughts of how are we not even worth more than a small square? That you put it together on a page with other stuff, most predominantly how to improve student internships, and then that small, small text glaring at me.
Before i know it im crying and closing the page
I know its unfair to say people dont care, seeing as the bit made it in the paper at all, but still
But still.
1 note
·
View note
Text
Beyond Binary Frames: Intersecting Autism Research and Feminist Insights
Hello everyone, welcome back to NeuroSimplified! In my first ever debut blog post (minus the introductory post), we embark on a journey through the world of autism research, guided by a feminist perspective. As we are aware, autism research, while making remarkable strides, often falls short of considering the intricate interplay of gender and other social dimensions. So! By melding these two critical lenses, we aim to unravel hidden biases, advocate for inclusivity, and pave the way for a more holistic understanding of autism.
Let us begin!
The ASD Research Landscape
The realm of autism research is vast and multifaceted, encompassing a range of theoretical frameworks, methodologies, and assumptions. However, traditional paradigms often lean towards binary constructs and fail to capture the complexity of gender identity and intersectionality. This oversimplification not only obscures meaningful insights but also perpetuates a limited understanding of the diverse experiences within the autism community [1].
For instance, emerging research has begun to shed light on the gender bias deeply ingrained in autism research. Lai and colleagues [2] conducted an exhaustive meta-analysis revealing a staggering male-to-female diagnosis ratio of 4-5:1. This imbalance, widely known as the "gender paradox”, has inadvertently resulted in the underdiagnosis of autistic women and individuals who identify as non-binary. This disparity underscores the necessity of dismantling the gender binary within research frameworks to capture the full spectrum of autism experiences.
Gender-related critiques in ASD research also comes from Nicolaidis and colleagues [3], who spotlighted the often-marginalized experiences of transgender and non-binary individuals within the autism community. This research bridged the gap between autism research and gender studies by recognizing that the experiences of transgender and non-binary individuals are not only impacted by their autism but also deeply intertwined with their gender identities. The intersectionality of these identities forms a matrix that shapes their experiences, influencing everything from social interactions to access to healthcare and support services. By looking at how ASD intersects with gender identity, we create more nuanced, holistic understandings of autism. Not only might this create more inclusivity generally but has the potential to ease the diagnostic process (which we know is utterly exhaustive), streamline treatment and let non-cis-male people with autism feel seen.
Thus, by not only shining a light on the often-overlooked experiences females in research but transgender and non-binary identities too, their research challenges the traditional gender binary assumptions inherent in autism research. This critique resonates through the very fabric of autism studies, compelling researchers to revaluate and expand their understanding of gender in the context of ASD.
So how might feminist theory actually help resolve these deep-rooted medical biases? Let’s take a look.
Feminist theory stands as a potent intellectual framework, offering an expansive toolkit that delves into the intricacies of power dynamics, identity formation, and representation. When applied to the realm of autism research, this lens ushers in a cascade of fresh perspectives that illuminate the intersection of autism and gender. As we’ve seen, it goes beyond mere observation, serving as a rallying call for inclusivity, empathy, and the pursuit of social justice.
At its core, feminist theory confronts the intricate power dynamics that underscore societal structures. Within the context of autism research, it prompts us to question who holds the power to define "normalcy." This probing inquiry reveals how conventional paradigms often prioritize neurotypical experiences, inadvertently silencing the narratives of autistic individuals. By adopting a feminist lens, we scrutinize the power dynamics that shape research agendas and the narratives that emerge.
Moreover, this analytical toolset unravels how these power dynamics interact with gender. Feminist theory invites us to explore how patriarchal norms perpetuate the erasure of non-binary experiences and diminish the significance of feminine expressions within the autistic community. Researcher Clare Harrop [4], for example, examined how societal power structures contribute to the underdiagnosis of autistic women. The study revealed that the emphasis on male-presenting autism traits in diagnostic criteria perpetuates gender-based disparities in recognition and support. Thus, adopting a feminist lens compels researchers to redefine power dynamics within the context of autism research, centring the voices and perspectives of those who have long been marginalized.
Identity, often reduced to simplistic categories, becomes a vibrant tapestry under the scrutiny of feminist theory. This lens encourages us to deconstruct the binary notions of "male" and "female" that underpin traditional autism research. By doing so, we make space for the rich and diverse identities that populate the autism spectrum.
When we apply this lens to the intersection of autism and gender, we unravel the intricate ways in which these identities intersect and intertwine. Autistic individuals, who are often relegated to the periphery of society, find their experiences illuminated in a nuanced light. Non-binary and transgender autistic individuals, who navigate the intersection of gender identity and neurodiversity, are finally recognized as vital contributors to the broader discourse.
With this, feminist theory beckons us to dismantle the barriers that perpetuate exclusion and inequality. In the context of autism research, this means dismantling the structures that inadvertently marginalize the experiences of autistic individuals who identify as women or non-binary. By adopting a feminist lens, we embark on a journey toward creating research spaces that celebrate diversity, defy conformity, and embrace the authentic experiences of all autistic individuals.
This lens also champions the pursuit of social justice. It implores researchers to advocate for equitable access to resources, support services, and opportunities for autistic individuals of all gender identities. Research by Michelle Dean [5] exemplifies how embracing a feminist approach in autism research led to the recognition of the unique support needs of autistic women. By advocating for equitable access to resources, support services, and opportunities for individuals of all gender identities, we create a transformative shift that uplifts the experiences of everyone, regardless of how they navigate the intersections of autism and gender. This shift is imperative, as it sets the stage for a more just and inclusive society that uplifts the experiences of everyone, regardless of how they navigate the intersections of autism and gender.
In conclusion, embracing a feminist lens within autism research generates a seismic shift in perspective. It calls for a recalibration of power dynamics, a deconstruction of traditional identity paradigms, and an unwavering commitment to inclusivity and social justice. By weaving feminism into the fabric of autism research, we embark on a journey that reframes the discourse, broadens our horizons, and reshapes the very foundations upon which knowledge is built.
As we conclude this journey, we recognize the potential for transformation. Embracing feminism within autism research reframes our approach, paving the way for a more inclusive and empathetic understanding of autism. By challenging traditional norms, we set the stage for a research landscape that amplifies diverse voices, dismantles barriers, and advocates for social justice.
So, this fusion of feminism and autism research is not merely an intellectual exercise; it's a call to action. As researchers, advocates, and society as a whole, we stand on the precipice of change, poised to create a more equitable and compassionate future for all autistic individuals.
┍━━━━ ⋆⋅☆⋅⋆ ━━━━┑
And that concludes it! Thank you for embarking on this insightful journey with me. Stay tuned for more explorations that unravel the complexities of neurodiversity and the human experience. I'm aware that, whilst this blog post was about gender and ASD, investigating intersectionality goes beyond just gender. As culture massively shapes our understanding of the world around us, I aim to explore the impact of culture on ASD research and what kind of biases emerge within that sphere.
Please feel free to give constructive feedback or share your general thoughts!
All the best, always.
With unwavering curiosity and empathy,
Emily
┍━━━━ ⋆⋅☆⋅⋆ ━━━━┑
References:
Sala, G., Pecora, L., Hooley, M., & Stokes, M. A. (2020). As diverse as the spectrum itself: Trends in sexuality, gender and autism. Current Developmental Disorders Reports, 7, 59-68.
Lai, M. C., Lombardo, M. V., Auyeung, B., Chakrabarti, B., & Baron-Cohen, S. (2015). Sex/gender differences and autism: setting the scene for future research. Journal of the American Academy of Child & Adolescent Psychiatry, 54(1), 11-24.
Nicolaidis, C., Raymaker, D. M., Ashkenazy, E., McDonald, K. E., Dern, S., Baggs, A. E., ... & Boisclair, W. C. (2015). “Respect the way I need to communicate with you”: Healthcare experiences of adults on the autism spectrum. Autism, 19(7), 824-831.
Harrop, C., Jones, D. R., Sasson, N. J., Zheng, S., Nowell, S. W., & Parish‐Morris, J. (2020). Social and object attention is influenced by biological sex and toy gender‐congruence in children with and without autism. Autism Research, 13(5), 763-776.
Dean, M., Harwood, R., & Kasari, C. (2017). The art of camouflage: Gender differences in the social behaviors of girls and boys with autism spectrum disorder. Autism, 21(6), 678-689.
#feminism#patriarchy#male bias#autism#neurodivergent#neurodiversity#neurospicy#diagnosis#neuroscience#research paper#asd#neurosimplified#scholarly academia#academia
2 notes
·
View notes
Text
video essay recommendations
i am personally a big fan of video essays and have watched a great number of them. if you're looking to learn about trans people and issues relating to us and like the video essay form, see here my personal list of video essay recommendations grouped by topic
if you want all the videos in a small neat playlist click here! (the only exceptions are two series of videos who are instead linked in the list as playlists)
on transphobia:
The History of Transphobia by Mia Mulder
Transphobia: An Analysis by Philosophy Tube
Tracing the Roots of Pop Culture Transphobia by Lindsay Ellis
What Are Women? by Lily Alexandre
Response to BBC transphobia by Shaun
The Continually Escalating Anti-LGBT Rhetoric by Jessie Gender
The Anti-Trans Disinformation Pipeline by Jessie Gender
How PragerU Creates Transphobia (in Trans-Affirming Folks) by Jessie Gender
on Gender Criticals/TERFs
What Are TERFs? - How "Gender Critical" TERFs Harm Transgender Folks by Jessie Gender
Gender Critical by Contrapoints
Inside a Cult - Gender Critical - Recruitment by Caelan Conrad
Inside a Cult - Gender Critical - Conversion Therapy by Caelan Conrad
Inside a Cult - Gender Critical - Fascism by Caelan Conrad
Exploring The "Gender Critical" Radicalization Pipeline by Jessie Gender
TERFs and the Fascist Roots of Anti-Trans Movements by Jessie Gender
TERFs and False Consciousness by Rosencreutz
TERFs Are Wrong About Biological Sex by Lily Alexandre
The TERF AI App That Uses Modern Pseudoscience by Jessie Gender
on J.K. Rowling
J.K. Rowling by Contrapoints
I'm Done With JK Rowling by Jessie Gender
Hogwarts Legacy, JK Rowling, and Trans Advocacy by Ro Ramdin
An Over-Emotional Look at Why JK Rowling is Bad by James Somerton
Death of the Author 2: Rowling Boogaloo by Lindsay Ellis
"Separating Art vs. the Artist" doesn't work for Harry Potter by Kuncan Dastner
on trans people in sports
Should Trans Women Be Allowed In Womens Sports? by Mia Mulder
Are Transgender Athletes The End of Sports? by Jessie Gender
The Science of Trans Women in Sport by Jangles ScienceLad
other topics
Autogynephilia by Contrapoints
Puberty Blockers Are Safe, As Far As We Know. Get Over It. by Mia Mulder
Irreversible Damage from a cog psych perspective (Series) by Cass Eris
Transmedicalism: An Investigation by CopsHateMoe
What Is "Gender Ideology"? (Hint: It Doesn't Exist.) by Lily Alexandre
Detransition, Gender by Mia Mulder
The Unending Lies of Matt Walsh by Jessie Gender
The Manipulations of Matt Walsh's "What is a Woman?" by Jessie Gender
Transvestigation: The Conspiracy Theory That Everyone Is Transgender by Mia Mulder
We Have Always Existed: Transgender Ancient History Show by We Have Always Existed Ancient Transgender History
I Emailed My Doctor 133 Times: The Crisis In the British Healthcare System by Philosophy Tube
Do "Binary Trans Women" Even Exist? The Politics of Gender Conformity by Lily Alexandre
5 notes
·
View notes
Text
Autism & Genderqueer
This is the same list of readings I sent to my mom to explain how being autistic affects how I experience gender. Other people will probably find these helpful as well, and they're super interesting.
The intersection of autism
and gender in the
negotiation of identity:
A systematic review
and metasynthesis
https://journals.sagepub.com/doi/full/10.1177/09593535221074806
“I Don't Feel Like a Gender, I Feel Like Myself”: Autistic Individuals Raised as Girls Exploring Gender Identity
https://www.liebertpub.com/doi/full/10.1089/aut.2018.0001
The lived experience of gender dysphoria in autistic adults: An interpretative phenomenological analysis
https://journals.sagepub.com/doi/10.1177/13623613211039113
Healthcare clinician perspectives on the intersection of autism and gender dysphoria
https://journals.sagepub.com/doi/full/10.1177/13623613221080315
Gender Identity and Autism Spectrum Disorders
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4345542/
Autism and transgender identity: Implications for depression and anxiety https://www.sciencedirect.com/science/article/pii/S1750946719301540
Autism and Trans Identity
http://murmurations.cloud/ojs/index.php/murmurations/article/view/142/84
Both sex- and gender-related factors should be considered in autism research and clinical practice
https://journals.sagepub.com/doi/full/10.1177/1362361320913192
Elevated rates of autism, other neurodevelopmental and psychiatric diagnoses, and autistic traits in transgender and gender-diverse individuals
https://www.nature.com/articles/s41467-020-17794-1
https://www.nature.com/articles/s41467-020-17794-1?source=techstories.org
Supporting transgender autistic youth and adults: A guide for professionals and families
https://books.google.ca/books?hl=en&lr=&id=4_qXDwAAQBAJ&oi=fnd&pg=PP1&dq=info:tHdwKqeMUVIJ:scholar.google.com/&ots=Hid96xQYlH&sig=Jc1mAmN3enQOspOmRmVXPfEzeR8&redir_esc=y#v=onepage&q&f=false
Gender Variance Among Youth with Autism Spectrum Disorders: A Retrospective Chart Review
https://www.liebertpub.com/doi/full/10.1089/trgh.2015.0007
Autistics Never Arrive
A Mixed Methods Content Analysis of Transgender and Autistic Autobiography
https://bulletin.appliedtransstudies.org/article/1/1-2/7/
Autistic traits in individuals self-defining as transgender or nonbinary
https://www.cambridge.org/core/journals/european-psychiatry/article/autistic-traits-in-individuals-selfdefining-as-transgender-or-nonbinary/EBA481AA354DA47D8C3F88AE5B9BD6BC
#actually autistic#autistic#autism#transgender#this doesn't mean that if you're autistic you are automatically queer or vice versa#but being autistic directly influences how i experience things#including social concepts such as gender#anyways if you're interested have fun
4 notes
·
View notes
Text
Key Issues on LGBTQIA Part 8
Unequal Healthcare
This is our definition of the LGBT community on unequal healthcare. The LGBTQ community is still fighting for equal treatment by medical professionals and insurance companies that have the power to deny people access to necessary care, as well as for improved access to healthcare. Adolescents who identify as LGBTQ are more likely to experience substance misuse and mental health problems, and transgender people may encounter prejudice from health insurers just because of their identity. Insurance firms may discriminate based on sexual orientation and gender identity in 37 states. How the LGBTQ community can deal with the disparities in healthcare. According to him, there are several reasons at work, including lower insurance coverage rates, higher rates of mental health problems, a lack of cultural competence in the medical context, and, regrettably, even outright discrimination by certain medical personnel. "Members of racial or ethnic minorities who identify as LGBTQ+ are even more likely to be impacted by these disparities." Here's a detailed analysis of the top seven health inequalities that LGBTQIA+ populations must deal with. Also included is information on dealing with these differences as an ally of the LGBTQIA+ community and as an individual. What are some potential remedies for the LGBTQ community's access to inequitable healthcare? Establish a space where someone identifying as LGBTQIA+ can feel comfortable telling you about themselves. When someone tells you who they are, you should believe them. Engage in active advocacy on behalf of your LGBTQIA+ peers. Financial assistance can be extended to LGBTQ+ friends, acquaintances, and family members, as well as to LGBTQ+ individuals you meet through online fundraisers and requests for Mutah well as the LGBT people you interact with through online fundraising and pleas for mutual aid, provide financial support to your queer friends, acquaintances, and family.
0 notes
Text
what percentage of the population is lgbt
When we talk about the LGBT population, we’re referring to individuals who identify as lesbian, gay, bisexual, or transgender. Understanding the size of this community can help in creating a more inclusive and supportive society. So, what percentage of the population is LGBT? Let's dive into the numbers and their significance.
The Numbers Behind the LGBT Population
The percentage of people who identify as LGBT can vary depending on the source and methodology of surveys. However, a commonly referenced statistic comes from the Gallup Poll, which has been tracking LGBT identification in the United States for several years. According to their 2021 data, about 5.6% of U.S. adults identify as LGBT.
Also Read: https://digizidoc.com/
This number has been steadily increasing over the years, likely due to growing social acceptance and more people feeling comfortable to self-identify. It's also worth noting that younger generations, particularly Gen Z, show higher percentages of LGBT identification compared to older generations.
Global Perspective
The percentage of the LGBT population can differ worldwide due to cultural, social, and legal factors that affect self-reporting. For instance, a 2020 survey by the International Lesbian, Gay, Bisexual, Trans and Intersex Association (ILGA) suggested that LGBT identification in various countries ranges from 1% to 10%.
In countries with more progressive attitudes towards LGBT rights, such as those in Western Europe, the numbers tend to be higher. Conversely, in regions where there is significant social stigma or legal repercussions for being LGBT, such as parts of Africa and the Middle East, the reported percentages are lower.
Also Read: Boost Your SEO Strategy with SWOT Analysis
Factors Influencing LGBT Identification
Several factors can influence the percentage of people who identify as LGBT:
Social Acceptance: In more accepting societies, individuals may feel more comfortable coming out. Acceptance can be fostered through education, representation in media, and supportive policies.
Legal Protections: Places with strong anti-discrimination laws and protections for LGBT individuals often see higher rates of self-identification. Legal recognition of same-sex marriages and protections against hate crimes contribute to a safer environment for coming out.
Survey Methodology: The way questions are asked can impact responses. Anonymity and the framing of questions play crucial roles. Surveys that assure confidentiality and use inclusive language tend to yield more accurate representations.
Also Read: AI Evolution How Intelligent Machines Are Shaping Our World
Why These Numbers Matter
Understanding the percentage of the population that is LGBT is crucial for several reasons:
Policy Making: Governments can create better policies to protect LGBT rights, such as anti-discrimination laws, and health and social services that cater to the needs of the LGBT community.
Healthcare: Tailoring healthcare services to meet the specific needs of LGBT individuals, including mental health support and specialized medical care, is essential for their well-being.
Social Support: Enhancing support systems in communities, schools, and workplaces can lead to more inclusive environments where LGBT individuals feel valued and accepted.
Moving Towards Inclusivity
Recognizing the diversity within our communities is the first step toward inclusivity. Whether the percentage is 5.6% or varies across different regions, every individual’s identity is valid and deserves respect. Here are some steps to foster inclusivity:
Education: Educating the public about LGBT issues can reduce stigma and promote understanding.
Representation: Increasing LGBT representation in media, politics, and other public spheres can help normalize diverse identities.
Support Networks: Creating and supporting LGBT groups and networks within communities and workplaces can provide a sense of belonging and safety.
Challenges and Considerations
While understanding the percentage of the LGBT population is important, it's also crucial to recognize the challenges faced by this community. Many LGBT individuals experience discrimination, mental health issues, and lack of access to appropriate healthcare. By addressing these challenges, society can better support the LGBT community.
Conclusion
The percentage of the population that identifies as LGBT might seem like just a number, but it represents real people with unique experiences and needs. By understanding these numbers, we can work towards a society that is more accepting, inclusive, and supportive of all its members.
Remember, the journey towards inclusivity starts with awareness and education. Let's continue to learn and grow together, embracing the diversity that makes our communities richer and more vibrant.
Also Read: Boost Your Rankings with SEO Experts
0 notes
Text
By: Bernard Lane
Published: Dec 12, 2023
The gist
Analysis
An Australian health minister, Shannon Fentiman, who is responsible for the busy gender clinic of the Queensland Children’s Hospital, has acknowledged the lack of consensus on how to treat gender dysphoria.
Four words stood out in Ms Fentiman’s otherwise cagey, scripted response to a question in state parliament about the source of the evidence justifying the puberty blockers and cross-sex hormones given to minors by the Brisbane-based clinic.
“Whilst acknowledging that best practices rely on some aspects of transgender health care and there is not consensus [Emphasis added], the work continues,” she said on November 30.
Child and adolescent psychiatrist Dr Jillian Spencer, who has been calling for an independent federal inquiry into the care of gender dysphoric youth, welcomed Ms Fentiman’s concession reflecting the state of medical opinion—a concession not forthcoming from Australia’s other health ministers.
“It is such a relief to have [Queensland’s] health minister finally acknowledge that there is not consensus regarding the best practices for transgender healthcare,” Dr Spencer told GCN.
Dr Spencer is a critic of the “gender-affirming” treatment approach followed by the Queensland gender clinic. Earlier this year she was suspended from clinical duties at the children’s hospital reportedly after a patient lodged a complaint of “transphobia”.
“The minister says that the work of the [clinic] continues despite the lack of consensus on best practice for transgender healthcare,” Dr Spencer said.
“Why is the work of the [clinic] continuing if there is no consensus? Shouldn’t we be more careful than that—especially when the health of children is at stake? Parents want cautious and evidence-based healthcare for their children.
“The children and parents of Queensland deserve to have paediatric gender services that are based on a systematic review of the research evidence similar to what is happening in the UK with the Cass Review.”
She challenged the advice given to Ms Fentiman that the work of the Queensland gender clinic represented “international best practice”.
“[It appears her advisers] have failed to let her know that, internationally, when [countries such as Finland, Sweden and the UK] have conducted independent, systematic reviews of the research literature, they have moved away from an affirmative approach to prioritise psychosocial interventions rather than puberty blockers and cross-sex hormones”.
“A new front in the struggle over transgender issues has opened up. Two [US] medical malpractice lawsuits, each levied by a plaintiff who regrets having undergone medication-based gender-transition treatment—one at age 14—have taken aim at the American medical establishment’s support for prescribing such drugs to minors.”—Journalist Benjamin Ryan, news report, New York Sun, 5 December 2023
---
The detail
Behind the scenes
Minister Fentiman’s remarked on the lack of medical consensus during her short November 30 reply to Robbie Katter MP, whose question was prompted by Ms Fentiman’s earlier reassurance that care at the gender clinic was “of very high quality and based on the best available evidence.”
The minister’s surprising concession to critics of the gender-affirming approach—the approach enforced at the gender clinic—chimes with the reference by Queensland’s chief psychiatrist, Dr John Reilly, to plans for an “independent review” of the clinic.
GCN has sought clarification on both points from the government; there was no reply.
Might Queensland be the first Australian jurisdiction to publicly acknowledge the force of the international debate about medicalised gender change for minors? Have there been frank discussions, even talk of doing something, in Ms Fentiman’s office or among her health and hospital officials?
The main focus now for Queensland’s governing Labor Party is re-election. In power since 2013, the party has shuffled its leadership as it prepares for the state poll scheduled for 26 October 2024.
It appears that Steven Miles, a former health minister, will succeed the long-serving Annastacia Palaszczuk as premier.
Ms Fentiman, a solicitor from the party’s left faction, was briefly in the running. Her narrative was change and renewal, a government with “the maturity to admit where we have fallen short.”
Does anyone think that concerns about gender medicine will have evaporated by next October?
--
Affirmed by guidelines
Minister Fentiman’s November 30 defence of the gender clinic boiled down to its “adherence to peer-reviewed national and internationally accepted published practice clinical guidelines”.
She cited the latest, 8th edition of standards of care issued last year by the World Professional Association for Transgender Health (WPATH), which she said evinced “a rigorous and evidence-based approach”.
She also invoked the 2017 clinical guideline of the Endocrine Society, offering to get a copy for Mr Katter, who represents a minor party in the parliament.
And she cited a third document, the 2018 “Australian standards of care” issued by the Royal Children’s Hospital Melbourne.
Back in September, Ms Fentiman had said the gender medicine practised by the Queensland clinic was “an emerging field globally—no-one shies away from that—but the evidence base is sound.”
In fact, the evidence base for medicalised gender change for minors is very weak and uncertain, according to five independent systematic reviews since 2019 in Finland, Sweden, the United Kingdom (one review each for puberty blockers and cross-sex hormones) and the American state of Florida.
The founder of the Queensland gender clinic, Dr Stephen Stathis, recently conceded the complaint of sceptics that the evidence base for gender-affirming treatment is of low quality, although he argued this was not unusual in the field of child and adolescent psychiatry.
Lack of solid evidence has led gender-affirming clinicians and activists to rely heavily on treatment guidelines and position statements from medical organisations when claiming that puberty blockers, cross-sex hormones and surgery are “settled science”.
But systematic reviews are regarded as the highest form of evidence, while treatment guidelines and position statements—representing expert opinion or professional consensus—are the lowest.
And it’s arguable that gender-affirming treatment guidelines do not even reflect expert consensus, as Ms Fentiman’s arresting remark suggests.
The extent of health professional dissent from the gender-affirming model is masked because it is well known that critics will be smeared as “transphobic”, subjected to bad-faith complaints and have their careers put at risk.
If in truth there is no consensus, the treatment guidelines cited by Ms Fentiman are misleading and cannot justify the risky medical interventions given by the gender clinic.
It’s unclear how this contradiction in the minister’s November 30 statement arose. Does it reflect a confused briefing from her advisers and officials, or a belated awareness that gender-affirming medicine is hardly settled science?
--
Reviewphobia
In any case, the problem for Ms Fentiman is that her faith in those three treatment guidelines is misplaced.
The “rigorous” WPATH guideline process involved a chaotic last-minute abandonment of minimum ages for most hormonal and surgical interventions; the rationale appears to be to give clinicians better protection against malpractice suits.
Credible guidelines draw on a systematic review of the evidence. WPATH’s new chapter on adolescents—the group that is the focus of international concern—involved no such review. WPATH pleaded the scarcity of studies on early medical intervention.
And yet early medical intervention is what the guideline recommends. Perhaps WPATH was worried about the predictable output of a systematic review, not the meagre input.
Scarcity of studies did not prevent Sweden’s systematic review of the evidence. Its literature search began with almost 10,000 research abstracts and identified just 24 relevant studies for evaluation.
One of the experts involved, Professor Mikael Landén of the Karolinska Institute said—
“Against the background of almost non-existent long-term data, we conclude that [puberty blocker] treatment in children with gender dysphoria should be considered experimental treatment rather than standard procedure. This is to say that treatment should only be administered in the context of a clinical trial under informed consent.”
The gender clinic that Ms Fentiman celebrates for its “life-changing care” gives puberty blockers as routine treatment. And remember, Queensland’s parliament has been assured by the minister that “the evidence base is sound”.
--
A matter of trust
Ms Fentiman also cited the 2018 “Australian standards of care” from the Royal Children’s Hospital Melbourne (RCH), noting its publication as a position statement in the Medical Journal of Australia (MJA).
But that cut-down version of the guideline, shielded by the journal’s pay wall, contains an admission not found in the full guideline which is the document that is readily available on the hospital website and relied on by youth gender clinics across Australia.
The MJA version says: “The scarcity of high-quality published evidence on the topic prohibited the assessment of level (and quality) of evidence for these recommendations.”
Earlier this year, GCN put this claim to Professor Gordon Guyatt, a pioneer of evidence-based medicine and the GRADE system for rating evidence quality.
“[That claim] is enough for me to say this is not a trustworthy guideline”, Professor Guyatt said.
The RCH guideline was considered for inclusion in the National Health and Medical Research Council’s online portal Australian Clinical Practice Guidelines but did not qualify.
“At the screening stage it was determined that the guideline did not include a funding statement, an evidence base for the recommendations or information about conflict of interest, and that it would not meet the portal selection criteria, so a full assessment was not carried out,” a spokeswoman for the NHMRC said in 2021.
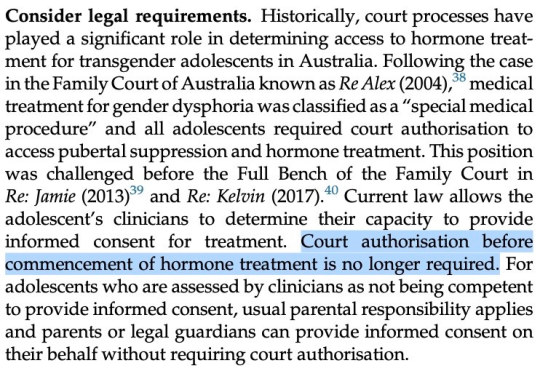
[ Screenshot: Advice from the 2018 RCH “Australian standards of care” document ]
--
Divided opinion
Also in 2021, the Royal Australian and New Zealand College of Psychiatrists (RANZCP), which had previously endorsed the RCH guideline, issued a new more cautious policy on gender dysphoria.
Its policy says that “evidence and professional opinion is divided as to whether an affirmative approach should be taken in relation to treatment of transgender children or whether other approaches are more appropriate.” (Note: After posting this article, I was alerted to an update of the RANZCP’s gender dysphoria policy, which I will report elsewhere.)
In its recently updated guide, the National Association of Practising Psychiatrists says “there is no consensus that medical treatments such as the use of puberty-blocking drugs, cross-sex hormones or sexual reassignment surgery lead to better future psycho-social adjustment.”
No consensus, but the Queensland Children’s Hospital requires health professions to follow the gender-affirming model rather than allowing a neutral therapeutic approach.
We know this because psychiatrist Dr Spencer has raised concerns—initially within the hospital, then publicly—about the potential harm done to minors by unthinking “affirmation”. She even wrote to the minister about this.
“I started testosterone five years ago today. After 4+ years of weekly injections to maintain such dangerously high hormone levels, I had elevated liver enzymes, heightened red blood cell counts, and regular heart palpitations. I am so grateful I stopped when I did.”—American detransitioner Morgan, tweet, 4 December 2023
--
Low-quality advice
Ms Fentiman’s third guideline, from the Endocrine Society, has an important feature that her advisers appear to have overlooked.
Unlike the RCH document, the 2017 Endocrine Society guideline did rate the quality of evidence supporting their treatment recommendations.
Five of the society’s six recommendations on puberty blockers depend on evidence rated as “low quality”.
The sixth recommendation—for administering blockers in early puberty, as is done at Queensland’s gender clinic—rests on “very low-quality” evidence, the lowest possible rating. Awkward but important details, rarely mentioned.
Also unmentioned is the society’s careful disclaimer that its “guidelines cannot guarantee any specific outcome, nor do they establish a standard of care.” Not helpful for those demanding a monopoly for gender-affirming care.
In July this year, the society’s president, Dr Stephen R Hammes, made the claim that, “More than 2,000 studies published since 1975 form a clear picture: Gender-affirming care improves the well-being of transgender and gender-diverse people and reduces the risk of suicide.”
This, he said in a letter to The Wall Street Journal, was the evidence used by the society in its “rigorous process” to develop the 2017 treatment guideline.
He provoked a dramatic and humiliating response—a letter of sharp dissent signed by 21 clinicians and researchers from nine countries involved in the care of teenagers with gender distress.
Among them was Finland’s reformist pioneer of gender medicine, Professor Riittakerttu Kaltiala, whistleblower clinicians from England’s Tavistock clinic Dr Anna Hutchinson and Dr Anastassis Spiliadis, and Belgian expert on evidence-based medicine Dr Patrik Vankrunkelsven.
All systematic reviews to date, the letter’s authors pointed out, had “found the evidence for mental-health benefits of hormonal interventions for minors to be of low or very low certainty.”
“Dr Hammes’s claim that gender transition reduces suicides is contradicted by every systematic review, including the review published by the Endocrine Society, which states, ‘We could not draw any conclusions about death by suicide.’ There is no reliable evidence to suggest that hormonal transition is an effective suicide-prevention measure.
“The politicization of transgender healthcare in the US is unfortunate. The way to combat it is for medical societies to align their recommendations with the best available evidence—rather than exaggerating the benefits and minimizing the risks.”
So, is Minister Fentiman confident that she had been given an apolitical and accurate summary of the benefits and risks of treatment at Queensland’s gender clinic?
“Opinion is divided about the certainty of the evidence base for gender-affirming medical interventions in youth. Proponents claim that these treatments are well supported, while critics claim the poor-quality evidence base warrants extreme caution. Psychotherapy is one of the only available alternatives to the gender-affirming approach. Discussion of the treatment of gender dysphoria in young people is generally framed in terms of two binary approaches: affirmation or conversion. Psychotherapy/exploratory therapy offers a treatment option that lies outside this binary, although it is mistakenly conflated with conversion therapies.”—Psychiatrist Dr Roberto D’Angelo, article, Journal of Medical Ethics, 2023
--
Just the one
Also, in the spirit of governments owning up to mistakes, Ms Fentiman might revisit something she said about Dr Spencer.
On September 14, Mr Katter raised the issue of the compulsion for doctors to use the gender-affirming model with dysphoric children, and asked, “Will the minister intervene to restore the ability of doctors—including Dr Jillian Spencer, who has been stood down—to use their professional medical discretion when treating gender dysphoric children?”
Ms Fentiman replied—
“I understand there have been a number of complaints made by patients in relation to Dr Spencer. These complaints are subject to a number of HR processes within Children’s Health [which runs the hospital] as well as referrals to [the health professions regulator] Ahpra and the Health Ombudsman.”
A possible implication of Ms Fentiman’s comment is that Dr Spencer had engaged in a pattern of conduct attracting multiple complaints from patients.
Last month, thanks to a right of reply mechanism, a correction from Dr Spencer was placed on the parliamentary record—
“The minister’s statement suggests that I am the subject of a number of patient complaints. That is incorrect. There is only one patient complaint lodged against me.”
--
“After being expelled from my master’s degree for speaking out about the impact of gender ideology on child safeguarding, I am extremely pleased to announce that I have agreed a settlement with the UK Council for Psychotherapy. [The council] have published a formal statement protecting therapists who believe in biological reality and stand against irreversible medicalisation of children. They say training institutions should never discriminate against students on this basis.”—UK lawyer turned trainee therapist James Esses, tweet, 11 December 2023
GCN sought comment from Ms Fentiman and RCH
==
Australia lumbers drunkenly towards figuring out this is all a major medical disaster.
#Bernard Lane#Gender Clinic News#systematic review#gender clinic#queer theory#gender ideology#medical scandal#medical malpractice#medical corruption#gender affirming care#gender affirming healthcare#affirmation model#Shannon Fentiman#no consensus#cross sex hormones#wrong sex hormones#puberty blockers#low quality evidence#religion is a mental illness
10 notes
·
View notes
Text
‘It’s Kind of Hard to Go to the Doctor’s Office If You’re Hated There.’ A Call for Gender-Affirming Care From Transgender and Gender Diverse Adolescents in the United States
Eisenberg, Marla E., Barbara J. McMorris, G. Nic Rider, Amy L. Gower, and Eli Coleman. 2020. “It’s Kind of Hard to Go to the Doctor’s Office If You’re Hated There.’ A Call for Gender-Affirming Care From Transgender and Gender Diverse Adolescents in the United States.” Health & Social Care in the Community. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7124990/).
Critical Review #3
“‘It’s Kind of Hard to Go to the Doctor’s Office If You’re Hated There.’ A Call for Gender-Affirming Care From Transgender and Gender Diverse Adolescents in the United States” is a study to know the experiences that TGD (transgender and gender diverse) youth living in Minnesota have when having to go to any healthcare provider and being discriminated against based on their gender identity. The article starts by explaining transgender and gender diverse (TGD) individuals’ encounters with significant health disparities compared to their cisgender counterparts, especially during adolescence, a crucial period for health development. Studies indicate elevated risks of emotional distress, substance use, and bullying victimization among TGD youth. Access to healthcare is also hindered by discrimination and a lack of knowledgeable providers. Minority Stress Theory underscores the chronic stressors faced by TGD populations due to stigma and discrimination, perpetuating health inequities. The American Academy of Pediatrics advocates for formal training and gender-affirming care for TGD youth, yet healthcare providers express discomfort and inadequate training in LGBTQ+ healthcare. Addressing these disparities requires comprehensive training, standardized treatment protocols, and a commitment to promoting the health and positive development of TGD individuals within a safe and inclusive clinical environment.
The method of this qualitative study engaged 12 TGD adolescents aged 14–17 in Minnesota, USA, between 2017 and 2018. Participants were recruited through various methods including clinics, LGBTQ youth-serving organizations, social media, and professional referrals. Interviews, conducted either in person or via phone/video, explored healthcare experiences and recommendations for providers. The University of Minnesota's Institutional Review Board approved the study, which utilized semi-structured interviews, transcribed and reviewed for accuracy by the interviewer. Thematic analysis of the data managed in Microsoft Word and Excel revealed emergent themes and subthemes. Two independent coders organized responses into topics and codes, resolving discrepancies through discussion.
The findings in this study involving transgender and gender diverse (TGD) adolescents emphasized the significance of healthcare providers asking about gender and pronouns. Participants expressed that such inquiries demonstrated care and respect, enhancing their comfort during clinical interactions. Suggestions were provided regarding when, whom, and how to ask about gender and pronouns, underscoring the importance of respectful communication in healthcare settings. These findings underscore the need for healthcare training to include content and skills related to affirming gender identity and promoting inclusive care practices for TGD youth. One participant commented, “I am like relieved when people ask me, or I'm like happy that they cared to ask because then it actually shows that they're interested in respecting you. And so even if they say something that isn't right or just kind of makes me feel uncomfortable, it's still good for them to ask because I can always just correct them, and, if they really care, then they'll listen to me.” Participants in the study emphasized the importance of healthcare providers gaining a basic understanding of gender identity, including definitions of key terms and the appropriate use of pronouns. They stressed the inclusion of non-binary identities in training, as these identities are often less understood by the general public.
The insights provided by participants underscore the importance of gender-affirming care, which involves healthcare practices that validate and support individuals' gender identities. This approach acknowledges the diverse experiences of transgender and gender-diverse individuals and prioritizes respectful communication, education, and understanding of their specific healthcare needs.
0 notes