#self diagnosed chronic fatigue syndrome is
Explore tagged Tumblr posts
Note
self diagnosed chronic fatigue syndrome is getting overly tired and napping for hours, unable to be woken up when you had a pretty good amount asleep the night before
.
12 notes
·
View notes
Text
Urgent care doc: okay so Im gonna put you on propanalol, your heart rate could be contributing to your increased migraines and why it isn't going away. Are you getting enough fluids? You know your heart rate is way high.
Me: oh Its always that high.
Doc: it is??????? (Visibly concerned)
#pots#urgent care#pots syndrome#self diagnosed pots#lupus#systemic lupus erythematosus#autoimmune disease#autoimmune#chronic disability#chronic pain#chronic migraine#chronic fatigue#chronic illness#disability#doctors#invisible disability#disabilities
41 notes
·
View notes
Text
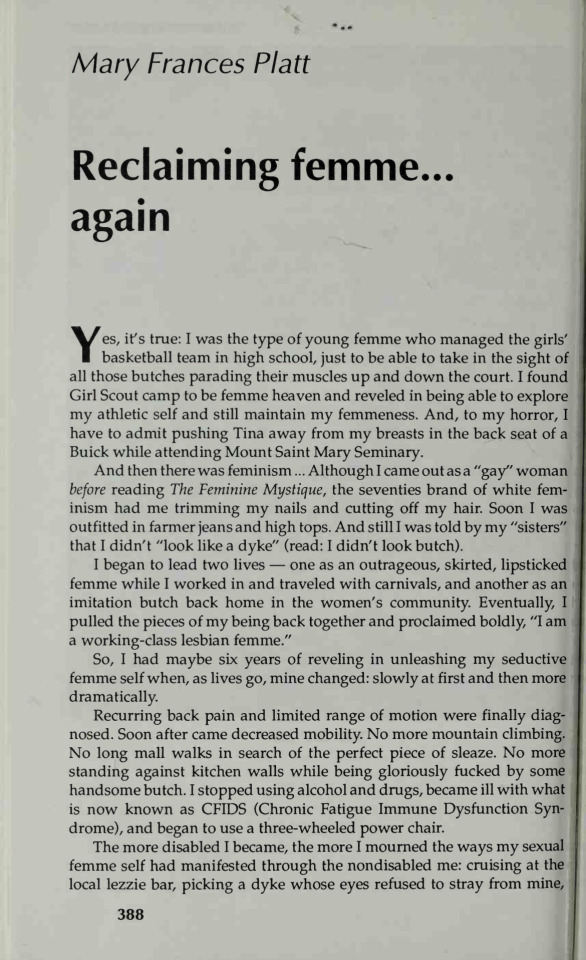

"Yes, it's true: I was the type of young femme who managed the girls basketball team in high school, just to be able to take in the sight of all those butches parading their muscles up and down the court. I found Girl Scout camp to be femme heaven and reveled in being able to explore my athletic self and still maintain my femmeness. And, to my horror, I have to admit pushing Tina away from my breasts in the back seat of a Buick while attending Mount Saint Mary Seminary. And then there was feminism... Although I came out as a "gay" woman before reading The Feminine Mystique, the seventies brand of white feminism had me trimming my nails and cutting off my hair. Soon I was outfitted in farmer jeans and high tops. And still I was told by my "sisters" that I didn't "look like a dyke" (read: I didn't look butch). I began to lead two lives- one as an outrageous, skirted, lipsticked femme while I worked in and traveled with carnivals, and another as an imitation butch back home in the women's community. Eventually, I pulled the pieces of my being back together and proclaimed boldly, "I am a working-class lesbian femme." So I had maybe six years reveling in unleashing my seductive femme self when, as lives go, mine changed: slowly at first and then more dramatically. Recurring back pain and limited range of mobility were finally diagnosed. Soon after came decreased mobility. No more mountain climbing. No long mall walks in search of the perfect piece of sleaze. No more standing against kitchen walls being gloriously fucked by some handsome butch. I stopped using alcohol and drugs, became ill with what is now known as CFIDS (Chronic Fatigue Immune Dysfunction Syndrome), and began to use a three-wheeled power chair. The more disabled I became, the more I mourned the ways my sexual femme self had manifested through the nondisabled me: cruising at the local lezzie bar, picking up a dyke whose eyes refuse to stray from mine, dancing seductively, moving all of me for all of her. Cooking: love and suggestion neatly tucked into the folds of a broccoli quiche. Serving my date in varying, sleazy clothing, removing layers as the meal and our passion progressed. And making love... feeling only pleasure as my hips rose and fell under the weight of her. Accomplishment and pride smirked across my face as her wrists finally submitted to the pressure of strong persistent hands. There are the ways I knew to be femme, to be the essence of me.
It's been five years now since I began using my wheelchair. I am just awakening to a new reclamation of femme. Yes. I still grieve the way I was, am still often unsure how this femme with disabilities will act out her seduction scenes. I still marvel when women find passion amidst the chrome and rubber that is now a part of me.
There have been numerous dates, lovers, relationships, sexual partners, and fliterations along the way. Cindy, Jenny, Ellie, Emma, Diane, Dorothy, Gail, June, Clove, Lenny, Cherry, Diana, Sarah I, and Sarah II. You have all reminded me in your own subtle or overt, quit or wild ways that I am desirable, passionate, exciting, wanted.
Yes I am an incredibly sexual being. An outrageous, loud mouthed femme who's learning to dress, dance, cook, and seduce on wheels; finding new ways to be gloriously fucked by handsome butches and aggressive femmes. I hang out with more sexual outlaws now- you know, the motorcycle lesbians who see wheels and chrome between your legs as something exciting, the leather women whose vision of passion and sexuality doesn't exclude fat, disabled me.
Ableism tells us that lesbians with disability are asexual. (When was the last time you dated a dyke who uses a wheelchair?) Fat oppression insists that thin is in and round is repulsive. At times, these voices become very loud, and my femme, she hid quietly amidts the lists.
Now my femme is rising again. The time of doubt, fear, and retreat has passed. I have found my way out of the lies and oppression and have moved into a space of loving and honoring the new femme who has emerged. This lesbian femme with disabilities is wise, wild, wet, and wanting. Watch out.
-"Reclaiming femme... Yet again" Mary Francis Platt, The Persistent Desire (Edited by Joan Nestle) (1992)
#lesbian#lesbianism#lesbian history#disabled lesbian#lgbt history#gay history#butch femme#femme lesbian#feminism#lesbian feminism#the persistent desire#intersectionality#disability history#disability rights
2K notes
·
View notes
Text
about 1 in 10 people who have had epstein-barr virus develop lifelong, clinically significant chronic fatigue. EBV is also known as mononucleosis or mumps, and is considered a common and harmless childhood disease. if you have ever had EBV and have serious problems with energy or sleep, you are probably living with CFS and don't realize it.
EBV isn't the only virus that can trigger CFS, and it's suspected the common root is a specific, otherwise asymptomatic retrovirus frequently or constantly reactivating immune responses to other viruses. in general, CFS involves damage to the mu opioid receptors and can sometimes be treated quite effectively with naltrexone, with a handful of typically minor side effects. it can also be treated with lifestyle changes such as consistent sleep - about 8 hours every 24, no more or less - and careful management of physical energy and fatigue triggers.
(noteworthily, there is research suggesting that in at least some cases, COVID-19 exposure can produce CFS as a long viral syndrome.)
if you have ever been diagnosed with CFS, especially before the last couple of years, it was commonplace for clinicians to prescribe frequent exercise as a treatment protocol. even at the time this was known to have marginal positive results at best and severe, inescapable effects on fatigue levels. this is another thing that helps: self-advocacy. if you find that running a mile in a day means you can't brush your teeth or get out of bed in the morning, you need to put your foot down about not doing it and get any clinician you see to take alternative lifestyle changes and treatments more seriously, or else find another clinician
268 notes
·
View notes
Text
hii there ! you can call me ruru or toffuu, i am plural however generally no other will post on here apart from me, ruru. please read this through for more information about me 🤍
🎐 . about disabilities & disorders of mine
im a high-complex support needs autistic / level 3 autistic with an intelectual disability (low iq). this means i heavily struggle with expressing what i mean correctly and process language differently. also have continued late regression of skills.
i have many disabilities and disorders. please be mindful, respectful and patient with me. Moderate ADHD Combined type, Mild visual impairment, learning disabilities, on the shizophrenic spectrum and mentally ill.
hypermobile enhlers danlers syndrome, chronic fatigue syndrome, chronic joint pain, unexplained momentary paralysis of the legs, medically suspected arthritis.
semiverbal with speech impairment, late met speech milestone. generally part time aac device user.
mildly hard of hearing and future wheelchair user.
🎐 . about my identity & who i am
im an intersex nonbinary transgirl, im also transfemneu and transxenofem and cistrans. i use a lot of xenogenders and am a pansexual lesbian.
i use shi/hir, kid/kidself, pie/pieself, mew/mewself pronouns for the most part, if you struggle with abstract pronouns, you may just use my name or it/itself.
🎐 . what will be on this account?
me rambling and silly posting, talking about my interests as well as my disabilities and my day.
continue below for further information on my beliefs and interests as well as tags.
🎐 . what are my stances / beliefs on things?
i support all types of queer folk and their identities and what they are, no matter if contradictory or not.
i support all plural folk no matter of origin or what labels they use, i wont exclude anyone or try to go at them because of how they believe their brain is wired.
i support educated and informed self diagnosis, however, intelectual disability is not self diagnosable.
lastly dont involve me in any discourse, may that be queer discourse, system discourse or ship discourse, i dont care and it's odd.
the misinformation and ignorance a lot of folk put onto the topic of the puzzle piece symbolism on autism is often ableist and should be worked on in the lower needs autism community.
🎐 . what i like, interests and so on!
special interests of mine
my little pony, specifically generation four or generation three merchandise. its been my special interest for about ten years now.
i have also had a special interest in autism for about seven years now.
and a game called adopt me on roblox has been a special interest of mine for five years now!
hyperfixations of mine which i have or which come back
breaking bad, shameless us, the amazing world of gumball, tokio hotel, cookie run kingdom, heartbreak high, isopods, snails, future man, avatar the last airbender and way more.
hobbies which i have right now
watching cartoons or east asian dramas
collecting toys, rocks, notebooks, stickers, manga, sensory items, stuffed animals and more
🎐 . the tags i might use in my posts
#rurusharing : just a general type of tag of mine, might use this when im just sharing about my day or something which happened.
#rururant : not particularly venting, but could be, it'll be sharing of some sort related to negativity.
#ruruspinterest : this is me talking about my special interests in any way!
rurufixates : mentioning of hyperfixations
#actually autistic#autism#autistic adult#high support needs#aac user#multiply disabled#queer#chronically ill#heds#level 3 autism#disability#higher support needs#alterhuman#otherkin#otherhearted#intersex#pansexual lesbian#mspec lesbian#pro endo#lgbtqiia+#lgbtq community#actually adhd#adhd#chronic disability#chronicpain#chronic illness#chronic fatigue#physically disabled#physical disability#severe autism
31 notes
·
View notes
Text
Here’s some positivity for systems with chronic fatigue!
Chronic fatigue can be quite serious, and can cause great challenges in the lives of those who deal with it. However, those who live with chronic fatigue still deserve to have their voices heard and their struggles uplifted and addressed! This post is for all the systems with chronic fatigue out there!
Shoutout to systems who are diagnosed or who have self-diagnosed with chronic fatigue syndrome (CFS)!
Shoutout to headmates who are symptom holders for chronic fatigue!
Shoutout to systems who can’t work, go to school, or pursue hobbies and interests due to being fatigued all the time!
Shoutout to systems who struggle to maintain relationships due to their chronic fatigue!
Shoutout to systems who have been exhausted for as long as they can remember!
Shoutout to systems who have missed out on potentially life-changing events and opportunities due to their chronic fatigue!
Shoutout to systems who are desperately in need of a nap right now!
Shoutout to systems who cannot stand, walk, or sit upright for long periods of time!
Shoutout to systems whose processing power is often allocated to managing their system and symptoms, and are left constantly fatigued as a result!
Shoutout to systems with chronic fatigue who struggle with dissociative amnesia and/or brain fog!
Shoutout to systems whose chronic fatigue onset suddenly with little warning or explanation!
Shoutout to systems who are spoonies or have to ration their energy in order to make it through the day!
Having chronic fatigue may make it exhausting for systems to be active members of their communities. Regardless of how active you are in your life or plural spaces, please know that your productivity is not a reflection of your worth! You are a valued, cherished, and integral member of the plural community just the way you are.
We hope that you can find joy, acceptance, and lots and lots of rest in your future surrounded by loved ones who care about you. We’re wishing you plenty of lazy days, peaceful nights, and understanding from those around you. Thanks for reading, and have a great day!

(Image ID:) A pale orange userbox with a cluster of multicolored flowers for the userbox image. The border and text are both dark orange, and the text reads “all plurals can interact with this post!” (End ID.)
#multiplicity#pluralgang#plurality#actuallyplural#system positivity#plural positivity#plural pride#system pride#me cfs#cfs (chronic fatigue syndrome)#cfs/me#chronic fatigue
106 notes
·
View notes
Text
This is the longer of 2 trailers for the #Notjustfatigue 15-minute documentary on ME/CFS. Watch it for free here
My first impressions from watching this 15-minute video documentary:
It's the story of one person and her family rather than something involving experts talking.
She vividly describes her symptoms.
I have shared many similar experiences to her:
- missed a sibling's wedding due to the illness (in my case 3 siblings' weddings);
- had to initially self diagnose after having symptoms for a long time, before finally getting the diagnosis confirmed by some experts;
- declined into severe ME having initially been less severely affected;
- have improved a little compared to my lowest level but still remain severely affected after many years.
Watch it yourself for free here:
Elizabeth has posted this video already on her #Notjustfatigue social media accounts & has kindly given me permission to share it on some other social media platforms I'm on. Please do check out the website for her non-profit #Notjustfatigue
13 notes
·
View notes
Text

⛰️— Hello, we are the Tempest Castle entourage, more about us and / or the blog under the cut.
current layout by @roaringdrago
We are a self diagnosed, bodily 23 yro, Brazilian osdd-1b introject heavy system going by Tempest or Indigo collectively as well as they/it pronouns, we also have a mixed personality disorder with bpd and aspd symptoms as well as autism and adhd, to top of the sunday of unfortunate events we have had chronic fatigue syndrome since around 2018/2019. For a little more information about us you can go on our carrd
We do not have a dni, we just block anyone we don't want interacting with us, most of our protectors think dni's are useless because the people that actually care about them are never the ones that are in them.
We have a partner system, their blog is @reverse-moon and they are generally who we mean in the tag #tempest moon.
The emojis used in the beginnings of the tags signify which alters are posting.
This is the key for what the navigation tags mean:
#[tempestuous talks] → Random original posts
#[rainwatching] → All of our reblogs
#[observatorium visit] → Ask replies
#[thunder and lightning] → Information about our system we might want to come back to or reference
#[and the rain pours] → Writing we may post here from time to time
The last tags are for posts in that specific language, since we speak three. English will not be tagged as it is the majority in our blog, but the other two will.
Tags for posts a specific friend would like:
#posts misha would like
#reminds me of august
#this one for lia
Side blogs:
@chaoracle → Delphi's (host) side blog
@stainedmosaic → Mosaic's (host) side blog
@wrtchedhound → Thorn's (host) side blog
@fieldoflilac → Lilac's (co-host) side blog
@aphamedic → July's (co-host) side blog
@mephistokiran → Timaeus' side blog
@cresntmoon → Sindri's side blog
@hvrstmoon → Our littles' side blog
@hellshaunted → Hellaverse introjects side blog
@hauntedsymphonia → Kpop introjects side blog
Legacy tags key:
#Ω eerie whispers → Random original posts
#Ω shivers of cold rooms → All of our reblogs
#Ω creaking floorboards → Information about our system we might want to come back to or reference
#Ω candlelight halls → Writing we may post here from time to time
#Ω invited by séance → Ask replies

#[tempestuous talks]#[rainwatching]#[observatorium visit]#[thunder and lightning]#[and the rain pours]#pt br#es ar#tempest moon
8 notes
·
View notes
Text
Also preserved on our archive
By Tarun Sai Lomte
New research reveals how lingering viral activity and immune disruption contribute to long COVID, highlighting novel therapeutic strategies that could change the course of treatment for millions.

A recent study published in the journal Cell reviewed the current state of knowledge on the pathophysiology and biology of long COVID.
Coronavirus disease 2019 (COVID-19) can affect health over the long term. Although it is self-limited in most individuals, some infected individuals experience post-acute sequelae, including fatigue, cognitive dysfunction, and muscle weakness, among others. While more common after severe COVID-19, individuals with a history of mild or moderate severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection have the highest burden.
The World Health Organization (WHO) defines post-COVID-19 condition as unexplained symptoms persisting ≥ two months that manifest ≥ three months after SARS-CoV-2 infection. Further, while many countries have adopted this definition, several have formulated their own definitions. The patient community that first identified the condition prefers the term long COVID.
Overall, the definitions vary in the time scale on which the condition is defined and whether the condition is restricted to unexplained patient-reported symptoms or inclusive of incident medical diagnoses/laboratory abnormalities. The present study reviewed the epidemiology of long COVID, with emphasis on how the underlying mechanisms explain the physiology. Additionally, the study highlights how symptom clusters, identified through techniques like cluster analysis in electronic health records (EHR), could improve long COVID diagnosis by linking specific biological drivers to clinical endotypes.
Epidemiology and clinical features of long COVID There are variations in epidemiological estimates of long COVID across variants, populations, and regions. Some studies suggest a prevalence of 30% or higher but define the syndrome as new unexplained symptoms, which might lead to misclassification. Not all symptoms may be related to SARS-CoV-2; as such, other conditions must be ruled out. Determining what is new after infection and what might be unmasking of sub- or pre-clinical conditions is a significant challenge.
Further, SARS-CoV-2 is not the only virus associated with protracted symptoms. Studies have estimated that 18 million adults in the United States (US) might suffer from long COVID. The WHO and the Institute for Health Metrics and Evaluation estimated that one in 30 European individuals had long COVID in the first three years of the COVID-19 pandemic. Globally, an estimated 65 million individuals have long COVID.
Notably, the epidemiology of severe, disabling long COVID-19 is unknown. Long COVID can manifest during or weeks after the acute infection. Cognitive problems, fatigue, and post-exertional symptoms are the most common. In addition, symptom clustering based on organ systems, such as autonomic dysfunction, neurocognitive impairment, and exercise intolerance, offers a more precise understanding of long COVID phenotypes. Further, many symptoms of long COVID overlap with those of other infection-associated chronic conditions (IACCs), such as chronic Lyme disease, post-Ebola disease, post-Giardiasis, and myalgic encephalitis/chronic fatigue syndrome, among others.
Biological drivers of long COVID The biological drivers of long COVID are upstream processes, such as perturbations of the coagulation system and immunity, which do not directly cause disease but instead drive one another, leading to downstream physiological changes that manifest as symptoms. Some of these biological processes, like clotting and immune dysfunction, may interact, creating a cycle of chronic inflammation and tissue damage. Microclots, resistant to fibrinolysis, have been detected in long COVID patients and may contribute to tissue hypoxia and organ dysfunction. There are also associations between viral activity levels during infection and long COVID risk, with higher viral replication linked to more severe illness.
Long COVID risk appears to be lower with Omicron variants. The protective effect of antiviral therapy and vaccination suggests that viral replication and transmission during the acute phase is a significant determinant of long-term outcomes. Therefore, early COVID-19 interventions could mitigate long COVID and support pursuing robust preventive agenda.
Early in the pandemic, it was commonly assumed that SARS-CoV-2 infection would be transient; however, this was challenged by reports that viral proteins and nucleic acids could be detected months after infection. Although the precise anatomic site of viral persistence is unclear, there is consensus that persistence is tissue-backed. Various studies have linked immune dysfunction and inflammation with long COVID.
Many studies have focused on the role of inflammatory macrophages and monocytes in long COVID. Mast cell activation might also contribute to long COVID. Although not infected by SARS-CoV-2, external triggers can activate mast cells. Severe COVID-19 is also associated with autoimmunity. COVID-19 is also associated with a higher incidence of autoimmune conditions, such as lupus, Sjogren’s syndrome, inflammatory bowel disease, and rheumatoid arthritis.
Acute SARS-CoV-2 infection can lead to a hypercoagulable state and elevate the risk of thromboembolic events. Interactions between the spike protein and fibrinogen may result in abnormal clots that can trigger microglia activation in the brain, potentially contributing to neurocognitive symptoms of long COVID. Clotting has been implicated as a long COVID mechanism, with aggregates of platelets and clotting proteins detected in affected individuals.
Clinical physiology of long COVID The most efficient explanation for long COVID is tissue damage mediated by SARS-CoV-2 that was initiated during (initial) infection. Pancreatic infection by SARS-CoV-2 has been implicated in post-COVID-19 diabetes, another form of the post-acute sequelae, offering proof of principle. Endothelial dysfunction has been suggested to be involved in long COVID.
Various mechanisms might lead to endothelitis and macrovascular diseases, and their end-organ consequences could result in long COVID. Additionally, the study suggests that microclots and endothelial dysfunction could impair tissue perfusion, leading to organ damage and contributing to persistent symptoms such as fatigue and cognitive issues. Disruption of the gut-brain axis enables a direct connection between post-COVID-19 processes and disruption of normal physiology, including brain fog, autonomic dysfunction, and abnormal stress responses.
Brain fog, i.e., problems with memory, concentration, and attention, is among the most debilitating manifestations of long COVID. It has been a prominent symptom among non-hospitalized patients since the early pandemic. Some people, especially those with diabetes, learning and attention disorders, and substance, have a predisposition for developing brain fog. Individuals with brain fog are more likely to have abnormal cerebrospinal fluid measures.
Concluding remarks The COVID-19 pandemic has been described as a once-in-a-century challenge, with long COVID representing a challenge of similar scale. Although long COVID is not the first known IACC, it is the first time that such a condition has manifested in a substantially large number of people following a shared, known exposure. Emerging therapies, including antivirals like nirmatrelvir/ritonavir and immunomodulators targeting inflammatory pathways, are currently being explored in clinical trials as potential treatments for long COVID. As such, there is an urgent need for all types of research (basic, epidemiological, translational, and clinical and implementation sciences) into the natural history, biology, and treatment for long COVID.
Journal reference: Peluso MJ, Deeks SG. Mechanisms of long COVID and the path toward therapeutics. Cell, 2024, DOI: 10.1016/j.cell.2024.07.054, www.sciencedirect.com/science/article/pii/S0092867424008869
#long covid#covid conscious#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#still coviding#sars cov 2#wear a respirator#covid is airborne
5 notes
·
View notes
Note
Your blog is so awesome. I'm ABDL and am also Incontinent too. How do you deal with being in diapers and Autism
Thank! I am glad you like my blog.😊
I always been wearing diapers and always loved them. When I discovered the abdl community at the age of 14, it was awesome to see that my love for my diapers, my special needs, special gears and my comfortable age was very close to abdl.
Growing as an autistic kid got harder as I got more aware of my differences at teenage, and hardly understanding what and why ppls, teachers and special ed therapists were expecting to change, endure, and try to “hide” the real me. Today, I am still struggling with changes, sensory overload, non-sense and lies I hear everyday from everywhere.
I am glad the autism awareness evolved in the general population, and Better understandings from more doctors. However I am concerned to hear that many persons do self-diagnosis without being evaluated by a good autism specialist. The criteria list on quick evaluation tests online is too vague, not precise enough, and does not replace a professional evaluation where several “sisters-conditions/ disorders” can be diagnosed and rule out ASD.
For me, wearing diapers is normal. To like them is a plus. To fit in abdl lifestyle and such an awesome and huge community like that is a blessing!
As an adult today, being autistic is still a challenge on a daily basis. What makes me happy is to be able to stim when I need it, not hide, not be ashamed, live my life the way I want it to be, not what traditional society expects from me.
At the end, my weaknesses can be supported with specialists, and my strengths are very helpful in society. Just a different way of thinking and functioning. Not stupid, not an idiot. I have an exceptional memory that works in millions of images, and I am not hiding facts. I’m anxious, autistic, incontinent guy who likes diapers, safety gears, and like being little for so many reasons! I deal well with all this. 😊 Dealing less well with mystery challenges like chronic fatigue syndrome sadly. Ups and downs that I can’t explain well, neither doctors can, and there’s no known cure.
19 notes
·
View notes
Text
Happy Disability Pride Month!
In honor of the shift from LGBTQ Pride Month to Disability Pride Month, I’m going to bring awareness to some underrepresented and underinformed disabilities as a queer and disabled artist/writer. These are all disorders that I have come across among friends and acquaintances. Every disorder I discuss must have a clinical diagnosis in order to be treated. You should only be self-diagnosing if you plan on going to a doctor to confirm your speculations. Do not self-diagnose if you are not willing to confirm with a medical professional. This post is not to diagnose you.
Big Trigger Warning: Discussions of psychological disorders like E/Ds, depression, and personality disorders.
Dysautonomia
Any disorder relating to the autonomic (involuntary) nervous system
POTS
I have this! It is a nervous system disorder that affects heart rate and blood pressure because your nervous system does not allow your muscles to properly circulate blood, especially through the legs. Some symptoms include elevated heart rate, chest pain, low or high blood pressure, fatigue, changes in body temperature, and dizziness or fainting. POTS is more common in AFAB people than AMAB.
Amyloidosis
Amyloidosis is a disorder that occurs when a protein known as amyloid builds up in the organs. Amyloidosis is closely related to dysautonomia and chronic pain syndromes such as Ehlers-Danlos Syndrome because of the comorbid symptoms. These symptoms include edema, purpura around the eyes, skin that bruises easily, and fatigue.
Frey’s Syndrome
A neurological disorder closely related to dysautonomia that causes excessive sweating while eating. There are very few solutions to this disorder and even fewer of them are known to work.
Mitochondrial Syndrome
Mitochondrial diseases occur when there are genetic mutations and deformations to the mitochondria in cells that directly influence how the organelle produces energy. People with mitochondrial diseases can have poor growth, muscle weakness, seizures, visual and / or hearing problems, learning disabilities, and may develop kidney, liver, or heart disease.
Autonomic Dysreflexia
Autonomic dysreflexia is a disorder that causes abnormal overreactions of the autonomic nervous system. Symptoms include elevated heart rate, excessive sweating, and high blood pressure.
Chronic Pain
Any disorder relating to long-lasting pain surrounding any part of the body.
Patellofemoral Pain Syndrome
I have this one too! Patellofemoral pain syndrome is a chronic pain syndrome in which muscles in the lower extremities are too weak to support patellar (kneecap) movement. Thus, the patella (kneecap) will not track right. this causes lots of issues with walking.
Scoliosis
I also have this one! Scoliosis is defined as a physical disorder in which the spine is not a straight vertical line. There is either an “S” or “J” curve in the spine, compressing it and causing sharp or aching back pain.
Temporomandibular Joint Dysfunction
TMJ causes pain and tenderness in jaw joints and surrounding muscles and ligaments. Symptoms of TMJ include jaw stiffness, limited movement and locking of the jaw, ringing in ears, and dizziness.
Myofascial Pain Syndrome
This is a chronic muscular pain disorder. Typically, this pain is confined to one specific area, such as the neck or shoulders.
Fibromyalgia
A chronic disorder that causes pain and tenderness throughout the body, as well as fatigue. People with fibromyalgia can also have depression, anxiety, and trouble with memory and concentration.
Ehlers-Danlos Syndrome
EDS is a group of disorders that affect connective tissues that support the skin, bones, blood vessels, organs, and other tissues. Symptoms of EDS include stretchy, translucent skin, loose joints, and chronic pain.
Arthritis
Arthritis is defined as inflammation in one or more joints causing stiffness and pain. There are many different kinds of arthritis, each with different causes. These causes can include wear over time, infections, and underlying diseases.
Neurological Disorders
Any disorder relating to the brain and how it functions.
Seizure Disorders
Epilepsy
Epilepsy is a disorder of the brain characterized by repeated seizures. People with epilepsy can experience multiple kinds of seizures and can experience symptoms such as confusion, staring spells, stiff muscles, and loss of consciousness.
Cerebrovascular Diseases
Functional Neurological Disorder
Functional Neurological Disorder is essentially a stroke mimic. It can replicate the symptoms of a stroke, such as limb weakness, numbness, and speech disturbance.
Migraines
Lots of people have migraines and I am no exception. Migraines are caused by excessive blood flow to the brain. Migraines affect more than 10% of people worldwide and are 3 times more likely to affect AFAB people than AMAB people.
Psychological Disorders
Any disorders affecting mood, thinking, and behavior. I will not be discussing my mental disorders on the internet. Most people are familiar with what these are and what they look like, so I will instead be providing statistics for each one.
Anxiety Disorders
Generalized Anxiety Disorder (GAD) affects 6.8 million adults. Only 43.2% of those adults are receiving treatment. AFAB are twice as likely to be affected (Anxiety Disorders Association of America).
Panic disorder (PD) affects 6 million adults. AFAB are twice as likely to be affected (Anxiety Disorders Association of America) .
Obsessive-Compulsive Disorder (OCD) affects 2.5 million adults. AFAB are 3x more likely to be affected (Anxiety Disorders Association of America) .
Post-Traumatic Stress Disorder (PTSD) affects 7.7 million adults. AFAB are 5x more likely to be affected (Anxiety Disorders Association of America) .
Depression
Approximately 280 million people in the world have depression. AFAB are twice as likely to develop depression (World Health Organization).
Bipolar Disorder
4.4% of US adults experience bipolar disorder in their lives (National Institute of Health).
Personality Disorders
It is estimated that 9% of US adults have at least one personality disorder (American Psychiatric Association).
Eating Disorders (TW)
Eating Disorders affect 9% of the population worldwide (National Association of Anorexia Nervosa and Associated Disorders).
BIPOC are significantly less likely than white people to be asked by a doctor about eating disorder symptoms (National Association of Anorexia Nervosa and Associated Disorders).
Black teenagers are 50% more likely than white teenagers to exhibit bulimic behaviors (National Association of Anorexia Nervosa and Associated Disorders).
Rates of body dissatisfaction were higher among transgender and nonbinary youth (90%) compared to cisgender youth (80%) (National Association of Anorexia Nervosa and Associated Disorders).
#disability pride month#disability awareness#disability#dysautonomia#pots#chronic pain#neurological disorder#psychological disorders
15 notes
·
View notes
Text
I don't think I've ever posted on here about my disabilities but I'm having thoughts today and ironically my disability has made my world very small in terms of able bodied people to talk to so going to rant into the void here
Having lots of fraudulent feelings today. Even writing this, I felt like I should put disability in quotes. By legal and medical definition I have a disability. I have diagnoses. I still don't believe they're the right diagnoses but there ya go. I have the medically approved labels of hypermobility, chronic pain and chronic fatigue (plus anxiety and depression but everyone has that lbr). I have the prescribed meds plus the extra meds to treat the symptoms of the first lot. I've been to so many appointments, seen some specialists, had my blood taken so many damn times, use aids in my day to day life and get government support.
However. I only exist in my body. And being in online spaces for chronic illnesses everyone always seems worse off then me. So I have days like today. Where I wonder if I really am in more pain then anyone else. If maybe this is just getting older. If I'm not fatigued I'm just lazy. If it's not insomnia, it's me being self destructive. It's days like today where I want to survey a bunch of able bodied people - are you in pain right now? I'm sure you're tired but what kind of tired? Could you do housework or take a shower right now? Does it feel impossible? Does your body feel heavy? How often do you have a headache or feel nauseous? Does socialising, even theoretically, exhaust you? Maybe I'm just burned out, depressed, maybe this is just how it feels to exist in this shitty world. Maybe I'm just weaker then everyone else. Maybe we all feel the same I just can't cope like everyone else. Maybe all these labels are just excuses for me to not try. If I just got over myself maybe my world would be bigger.
But I'm only in my body and I don't have people to ask. If I did ask anyone it would probably just make them sad or think I was fucking weird - I am but yknow, a different brand of weird.
Being alive in itself can be really fucking isolating and I guess I'm just feeling that today. So I post on my tumblr I've had since I was 14 like that's gonna do a damn thing. We hear about imposter syndrome in the positive parts of life but it exists here too.
This is a very familiar feeling for me. I was never traumatised enough to call my childhood bad. Was never thin enough to call it an eating disorder. Not fucked up enough but not functional enough. Not queer enough. Not sick enough. Not independent enough. Not open. Not brave. Not disliked but no ones favourite. Not Not Not. I'm tired. But the same tired as everyone else? Who fucking knows.
2 notes
·
View notes
Text







— ☆ you can call me . . . Soleil / Hazard / Rewind!
☆ 23 years old. it & he pronouns only.
☆ xenogender effeminate T4T gay thing.
☆ white, norwegian, bilingual.
☆ physically disabled, neurodivergent, and autistic.
— ☆ welcome to my disability-focused sideblog, made by your local hypermobile rivethead latex-slugthing!







I'm an ambulatory wheelchair user. I am on full disability benefit, and have been since I turned 18.
due to the nature of this blog, I'm comfortable sharing certain health issues, since I'll occasionally talk about them & it recontextualizes my posts in a way I feel is important. yes, these are all either professionally diagnosed or acknowledged, though I am pro informed self-dx.
— hypermobile ehlers-danlos syndrome accompanied by myalgic encephalomyelitis / chronic fatigue syndrome.
— severe bilateral nasal valve collapse with a deviated septum, inferior turbinate hypertrophy, and chronic rhinitis with chronic sinus headaches.
— non-allergic asthma.
— multiple kinds of chronic skin issues.
— fibromyalgia.
— avoidant personality disorder, autism, dyscalculia, & ocd.
— light sensitivity & myopia (nearsightedness).
I will be getting surgery for the severe structural issues with my nose sometime in 2025, despite my anxiety regarding it all. I plan to document my experiences with this eventually, but I am a little shy!
as for other major surgeries important to me, I had a problematic femur osteochondroma removed in 2017. I also had an inguinal hernia repair done in around 2007-2008.
you may see me space out my punctuation in my posts. this is not a typing quirk; this is to make my posts a little more accessible to those with difficulty following sentences.

1 note
·
View note
Text
okay I have some thoughts about the cripplepunk movement, specifically on mind body dualism.
to be simple, I think it's bullshit.
people with anxiety and autistics suffer digestive issues to the extent of chronic pain. are they disabled yet? are they allowed to be cripplepunk?
people with severe mental health issues that result in life changing self injury. are they disabled yet? are they allowed to be cripplepunk?
autistic people who become catatonic or lose control of their bowels or bladder. are they disabled yet? are they allowed to be cripplepunk?
a trans guy with bowel incontinence/ severe urgency, debilitating chronic pain and chronic fatigue. he's diagnosed with anxiety. is he disabled? is he cripplepunk?
a doctor looks at him and decides he's sick enough to test. it's a common but poorly understood and recently discovered syndrome that has nothing to do with mental illness and everything to do with a non functioning migrating motor complex and stomach acid levels. same symptoms. am i disabled? can i be cripplepunk?
8 notes
·
View notes
Text
Females And Autism / Aspergers: A Checklist
Lynda Lim Abstract Multiple FemalesLynda Lim "Multiple Females"
This list is meant as a springboard for discussion and more awareness into the female experience with autism.
By Samantha Craft
Females with Autism: An Unofficial List
Section A: Deep Thinkers
A deep thinker
A prolific writer drawn to poetry
*Highly intelligent
Sees things at multiple levels, including her own thinking processes
Analyzes existence, the meaning of life, and everything, continually
Serious and matter-of-fact in nature
Doesn’t take things for granted
Doesn’t simplify
Everything is complex
Often gets lost in own thoughts and “checks out” (blank stare)
Section B: Innocent
Naïve
Honest
Experiences trouble with lying
Finds it difficult to understand manipulation and disloyalty
Finds it difficult to understand vindictive behavior and retaliation
Easily fooled and conned
Feelings of confusion and being overwhelmed
Feelings of being misplaced and/or from another planet
Feelings of isolation
Abused or taken advantage of as a child but didn’t think to tell anyone
Section C: Escape and Friendship
Survives overwhelming emotions and senses by escaping in thought or action
Escapes regularly through fixations, obsessions, and over-interest in subjects
Escapes routinely through imagination, fantasy, and daydreaming
Escapes through mental processing
Escapes through the rhythm of words
Philosophizes, continually
Had imaginary friends in youth
Imitates people on television or in movies
Treated friends as “pawns” in youth; e.g., friends were “students” “consumers” “members”
Makes friends with older or younger females more so than friends her age (often in young adulthood)
Imitates friends or peers in style, dress, attitude, interests, and manner (sometimes speech)
Obsessively collects and organizes objects
Mastered imitation
Escapes by playing the same music over and over
Escapes through a relationship (imagined or real)
Numbers bring ease (could be numbers associated with patterns, calculations, lists, time and/or personification)
Escapes through counting, categorizing, organizing, rearranging
Escapes into other rooms at parties
Cannot relax or rest without many thoughts
Everything has a purpose
Section D: Comorbid Attributes
OCD (Obsessive Compulsive Disorder)
Sensory Issues (sight, sound, texture, smells, taste) (might have Synthesia)
Generalized Anxiety
Sense of pending danger or doom
Feelings of polar extremes (depressed/over-joyed; inconsiderate/over-sensitive)
Poor muscle tone, double-jointed, and/or lack in coordination (may have Ehlers Danlos Syndrome and/or Hypotonia and/or POTS syndrome)
Eating disorders, food obsessions, and/or worry about what is eaten
Irritable bowel and/or intestinal issues
Chronic fatigue and/or immune challenges
Misdiagnosed or diagnosed with a mental illness
Experiences multiple physical symptoms, perhaps labeled “hypochondriac”
Questions place in the world
Often drops small objects
Wonders who she is and what is expected of her
Searches for right and wrong
Since puberty has had bouts of depression (may have PMDD)
Flicks/rubs fingernails, picks scalp/skin, flaps hands, rubs hands together, tucks hands under or between legs, keeps closed fists, paces in circles, and/or clears throat often
Section E: Social Interaction
Friends have ended friendship suddenly (without female with AS understanding why) and/or difficult time making friends
Tendency to overshare
Spills intimate details to strangers
Raised hand too much in class or didn’t participate in class
Little impulse control with speaking when younger
Monopolizes conversation at times
Brings subject back to self
Comes across at times as narcissistic and controlling (is not narcissistic)
Shares in order to reach out
Often sounds eager and over-zealous or apathetic and disinterested
Holds a lot of thoughts, ideas, and feelings inside
Feels as if she is attempting to communicate “correctly”
Obsesses about the potentiality of a relationship with someone, particularly a love interest or feasible new friendship
Confused by the rules of accurate eye contact, tone of voice, proximity of body, body stance, and posture in conversation
Conversation are often exhausting
Questions the actions and behaviors of self and others, continually
Feels as if missing a conversation “gene” or thought-filter
Trained self in social interactions through readings and studying of other people
Visualizes and practices how she will act around others
Practices/rehearses in mind what she will say to another before entering the room
Difficulty filtering out background noise when talking to others
Has a continuous dialogue in mind that tells her what to say and how to act when in a social situation
Sense of humor sometimes seems quirky, odd, inappropriate, or different from others
As a child it was hard to know when it was her turn to talk
Finds norms of conversation confusing
Finds unwritten and unspoken rules difficult to grasp, remember, and apply
Section F: Finds Refuge when Alone
Feels extreme relief when she doesn’t have to go anywhere, talk to anyone, answer calls, or leave the house but at the same time will often harbor guilt for “hibernating” and not doing “what everyone else is doing”
One visitor at the home may be perceived as a threat (this can even be a familiar family member)
Knowing logically a house visitor is not a threat, but that doesn’t relieve the anxiety
Feelings of dread about upcoming events and appointments on the calendar
Knowing she has to leave the house causes anxiety from the moment she wakes up
All the steps involved in leaving the house are overwhelming and exhausting to think about
She prepares herself mentally for outings, excursions, meetings, and appointments, often days before a scheduled event
OCD tendencies when it comes to concepts of time, being on time, tracking time, recording time, and managing time (could be carried over to money, as well)
Questions next steps and movements, continually
Sometimes feels as if she is on stage being watched and/or a sense of always having to act out the “right” steps, even when she is home alone
Telling self the “right” words and/or positive self-talk (CBT) doesn’t typically alleviate anxiety. CBT may cause increased feelings of inadequacy.
Knowing she is staying home all day brings great peace of mind
Requires a large amount of down time or alone time
Feels guilty after spending a lot of time on a special interest
Uncomfortable in public locker rooms, bathrooms, and/or dressing rooms
Dislikes being in a crowded mall, crowded gym, and/or crowded theater
Section G: Sensitive
Sensitive to sounds, textures, temperature, and/or smells when trying to sleep
Adjusts bedclothes, bedding, and/or environment in an attempt to find comfort
Dreams are anxiety-ridden, vivid, complex, and/or precognitive in nature
Highly intuitive to others’ feelings
Highly empathetic, sometimes to the point of confusion
Takes criticism to heart
Longs to be seen, heard, and understood
Questions if she is a “normal” person
Highly susceptible to outsiders’ viewpoints and opinions
At times adapts her view of life or actions based on others’ opinions or words
Recognizes own limitations in many areas daily, if not hourly
Becomes hurt when others question or doubt her work
Views many things as an extension of self
Fears others opinions, criticism, and judgment
Dislikes words and events that hurt animals and people
Collects or rescues animals (often in childhood)
Huge compassion for suffering (sometimes for inanimate objects/personification)
Sensitive to substances (environmental toxins, foods, alcohol, medication, hormones, etc.)
Tries to help, offers unsolicited advice, or formalizes plans of action
Questions life purpose and how to be a “better” person
Seeks to understand abilities, skills, and/or gifts
Section H: Sense of Self
Feels trapped between wanting to be herself and wanting to fit in
Imitates others without realizing it
Suppresses true wishes (often in young adulthood)
Exhibits codependent behaviors (often in young adulthood)
Adapts self in order to avoid ridicule
Rejects social norms and/or questions social norms
Feelings of extreme isolation
Feeling good about self takes a lot of effort and work
Switches preferences based on environment and other people
Switches behavior based on environment and other people
Didn’t care about her hygiene, clothes, and appearance before teenage years and/or before someone else pointed these out to her
“Freaks out” but doesn’t know why until later
Young sounding voice
Trouble recognizing what she looks like and/or has occurrences of slight prosopagnosia (difficulty recognizing or remembering faces)
Feels significantly younger on the inside than on the outside (perpetually twelve)
Section I: Confusion
Had a hard time learning that others are not always honest
Feelings seem confusing, illogical, and unpredictable (self’s and others’)
Confuses appointment times, numbers, and/or dates
Expects that by acting a certain way certain results can be achieved, but realizes in dealing with emotions, those results don’t always manifest
Spoke frankly and literally in youth
Jokes go over the head
Confused when others ostracize, shun, belittle, trick, and betray
Trouble identifying feelings unless they are extreme
Trouble with emotions of hate and dislike
Feels sorry for someone who has persecuted or hurt her
Personal feelings of anger, outrage, deep love, fear, giddiness, and anticipation seem to be easier to identify than emotions of joy, satisfaction, calmness, and serenity
Difficulty recognizing how extreme emotions (outrage, deep love) will affect her and challenges transferring what has been learned about emotions from one situation to the next
Situations and conversations sometimes perceived as black or white
The middle spectrum of outcomes, events, and emotions is sometimes overlooked or misunderstood (all or nothing mentality)
A small fight might signal the end of a relationship or collapse of world
A small compliment might boost her into a state of bliss
Section J: Words, Numbers, and Patterns
Likes to know word origins and/or origin of historical facts/root cause and foundation
Confused when there is more than one meaning (or spelling) to a word
High interest in songs and song lyrics
Notices patterns frequently
Remembers things in visual pictures
Remembers exact details about someone’s life
Has a remarkable memory for certain details
Writes or creates to relieve anxiety
Has certain “feelings” or emotions towards words and/or numbers
Words and/or numbers bring a sense of comfort and peace, akin to a friendship
(Optional) Executive Functioning & Motor Skills This area isn’t always as evident as other areas
Simple tasks can cause extreme hardship
Learning to drive a car or rounding the corner in a hallway can be troublesome
New places offer their own set of challenges
Anything that requires a reasonable amount of steps, dexterity, or know-how can rouse a sense of panic
The thought of repairing, fixing, or locating something can cause anxiety
Mundane tasks are avoided
Cleaning self and home may seem insurmountable
Many questions come to mind when setting about to do a task
Might leave the house with mismatched socks, shirt buttoned incorrectly, and/or have dyslexia and/or dysgraphia
A trip to the grocery store can be overwhelming
Trouble copying dance steps, aerobic moves, or direction in a sports gym class
Has a hard time finding certain objects in the house but remembers with exact clarity where other objects are; not being able to locate something or thinking about locating something can cause feelings of intense anxiety (object permanence challenges), even with something as simple as opening an envelope
This unofficial checklist can be copied for therapists, counselors, psychiatrists, psychologists, professors, teachers, and relatives, if Samantha Craft’s name and contact information remain on the print out. This list was created in 2012 and updated in May, 2016.
Samantha Craft
Disclaimer: This is my opinion and based on my experience after 12 years of researching about autism and being officially diagnosed with Asperger’s Syndrome. It is not meant to replace the DSM-V Autism Spectrum Disorder definition nor is this list meant to serve as an official diagnostic tool. Hundreds of women have used this list in conjunction with the DSM-IV or DSM-V and a professional mental health professional’s guidance. It is also based on 4.5 years of communicating almost daily with those that are diagnosed with autism and some that believe themselves to be on the spectrum. It is not all inclusive. Some will fit into categories and not be autistic/Asperian. This is meant as a springboard for discussion and more awareness into the female experience with autism.
This is an unofficial checklist created by an adult female with Asperger’s Syndrome (AS) who has a son with Asperger’s Syndrome. Samantha Craft has a Masters Degree in Education. Samantha Craft does not hold a doctorate in Psychiatry or Psychology. She has a life-credential as a result of being a female with Asperger’s Syndrome and being a parent of a child with Asperger’s Syndrome. She has created this list in an effort to assist health professionals in recognizing Asperger’s Syndrome in females—for in-depth information regarding females with AS refer to Craft’s book Everyday Aspergers.
#personal#autismo en mujeres#asperger femenino#autismo femenino#autistic girl#espectro autista#autista#samantha craft#mi maldita existencia entera
35 notes
·
View notes
Text
Physical Toll of Depression: Aches and Pains

Depression is often discussed in the context of mental health, but the physical toll it takes on the body is less frequently addressed. This post will explore how depression can manifest as aches and pains, and the implications it holds for those who suffer from it. We will also share strategies to cope with these symptoms and promote holistic well-being.
Understanding the Relationship
The way depression intertwines with physical pain can be complex and deeply impactful. It's not simply a matter of being down in the dumps. The pain associated with depression is real and can be one of the most debilitating aspects of the condition.
When we experience a low mood, our bodies tend to tense up, as if bracing for an impact. Over time, this physical reaction can lead to chronic aches, most commonly in the back, shoulders, and neck. Studies have shown that individuals with depression are more likely to report ongoing, severe physical discomfort. This is especially troubling given the already steep climb those with depression face when it comes to managing their mental state.
The intensity of physical pain peaks during depressive episodes and can significantly impair an individual's quality of life. It may also create a feedback loop, whereby the pain exacerbates the depression, and the depression likewise worsens the perception of pain—a challenging cycle to break. Understanding this dynamic is the first step in addressing the issue for those who grapple with it.
Impact on Daily Life and Well-being
The physical symptoms of depression are not simply inconvenient—they can be downright life-altering. Those suffering from depression-related pain often find it difficult to engage in activities they once enjoyed. Everyday tasks can become onerous, and sleep, which is profoundly affected by the condition, is commonly disrupted.
The toll on one's well-being extends beyond discomfort. It can disrupt social relationships, harm professional pursuits, and generally undermine a person's sense of self-efficacy. The daily struggle with pain can also contribute to a feeling of isolation, as it's not always evident to those around the affected individual.
Health Implications
The link between depression and chronic physical conditions is well-documented. Disorders such as fibromyalgia, irritable bowel syndrome, and chronic fatigue syndrome are more prevalent among those diagnosed with depression. Furthermore, the risk of cardiovascular and autoimmune diseases increases in tandem with the severity of depressive symptoms.
Increased Risk of Chronic Conditions
The immune system is notably weakened in individuals with depression, which leaves them susceptible to a range of ailments that manifest physically. Chronic inflammation, which often underpins conditions like heart disease and diabetes, is also elevated in depressed individuals. This paints a sobering picture of the health landscape for those with long-term depression.
Chronic conditions are also more challenging to manage alongside depression. The mental and physical components can create a maelstrom of symptoms that resist conventional treatment, necessitating a more nuanced approach to healthcare.
Challenges in Diagnosis and Treatment
Diagnosing and treating the physical symptoms of depression requires a level of awareness that isn't always present in clinical settings. Physicians may initially focus on the psychological aspect of depression, overlooking or downplaying the physical signs. This oversight can lead to a delayed diagnosis or inappropriate treatment plans.
However, for those who endure the physical pain of depression, a clear understanding of how these symptoms manifest is crucial. It is a two-way street; alleviating the physical discomfort can contribute to an improved mental state, just as treating the underlying depression can lessen the perception of pain.
Coping Strategies
Acknowledging the reality of depression-related physical pain is only the beginning. Here, we share strategies and approaches that can help individuals cope with these challenging symptoms.
Mind-Body Techniques
Mindfulness, meditation, and yoga are just a few examples of mind-body techniques that have been shown to reduce the severity of physical pain. By training the mind to focus on the present moment and the body's sensations, these practices can offer a respite from the discomfort, however brief. They also hold the potential to interrupt the downward spiral between pain and depression, creating a path towards healing.
Professional Support and Therapy Options
Seeking professional support is a critical step for anyone contending with the physical toll of depression. Therapists who specialize in pain management or those who offer cognitive-behavioral therapy (CBT) can be invaluable resources. Techniques such as setting achievable goals, identifying unhealthy thought patterns, and establishing routines can significantly improve one's ability to manage both the pain and depression.
Medication and other therapies may also be recommended, depending on the severity of the symptoms. It is important for individuals to work closely with their healthcare providers to find a treatment plan that is both effective and sustainable.
Community Support and Resources
No one should have to manage the physical symptoms of depression alone. There are numerous support groups and online communities that provide a space for individuals to share their experiences and seek advice. Organizations focused on mental health and chronic pain often offer resources, hotlines, and educational materials that can guide individuals towards effective support.
Organizations and Platforms for Mental Health and Chronic Pain Awareness
Connecting with organizations and platforms dedicated to mental health and chronic pain awareness can be a source of empowerment. Information on the latest research, community events, and inspiring stories from others who have overcome similar challenges can foster a sense of belonging and hope.
Conclusion
The physical toll of depression is a stark reminder of the complex interplay between mind and body. By understanding the ways in which depression can manifest as physical pain, we become better equipped to address this critical aspect of the condition.
Encouraging individuals to seek help, use coping strategies, and engage with supportive communities is paramount. By approaching the treatment of depression holistically, we can aspire to a future where those who suffer from the condition need not endure its painful side effects in silence.
If you or someone you know is experiencing these challenges, reaching out for help is the first and most important step on the path to recovery. Depression need not be a life sentence to chronic pain; with the right approach, the future can be a healthier and more comfortable one.
For a comprehensive treatment plan that embraces a holistic approach, consider the services at Renewed Mental Health Group. We offer personalized care that acknowledges the full spectrum of mental and physical well-being. Contact us today to take the first step towards relief.
2 notes
·
View notes