#medical psychiatric involuntary confinement
Explore tagged Tumblr posts
Text
INVADING SOMEONE'S PERSONAL HOME LIKE CRIMINALS HAVE DONE AT BRAD GEIGER'S ON WHITETAIL
#INVADING SOMEONE'S PERSONAL HOME LIKE CRIMINALS HAVE DONE AT BRAD GEIGER'S ON WHITETAIL#automatic#automatic response#response#brad geiger#medical attacks#medical#medical psychiatric involuntary confinement#continuously sustained medical attacks related to weirds apparently not leaving#unnecessary medical#medical psychiatry#medical psychiatric involuntary commitment#psychiatricmentalhealthfacility#psychiatry#psychiatric pseudoscience#mind control requests conveyed by regularly taking a pill that could not do what it claims to because of the blood brain barrier#blood brain barrier#human anatomy#definition of psychiatric medicine and all related terms and concepts
10 notes
·
View notes
Text

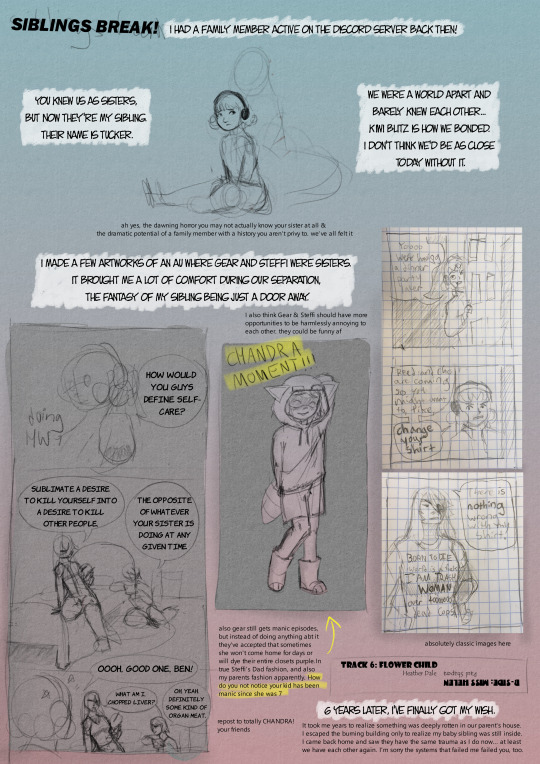

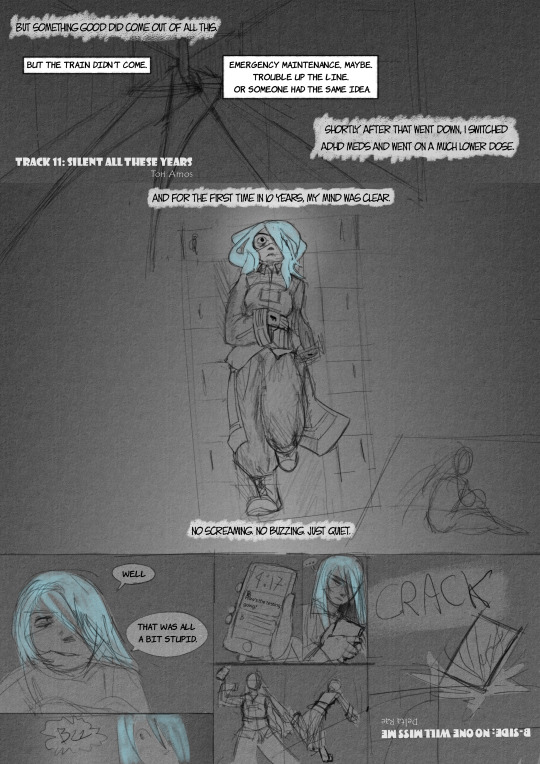
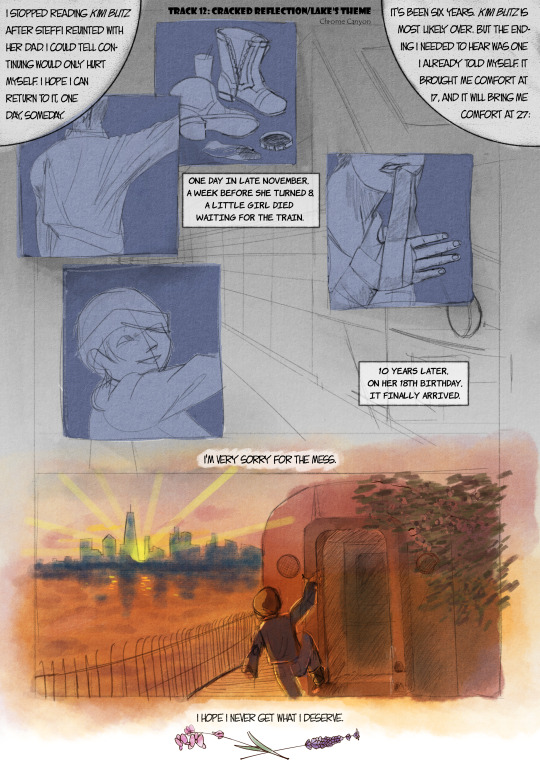
4'33'', by John Cage, is commonly remembered as 4 and a half minutes of silence. But contrary to popular belief, the song is not actually meant to be the sound of silence, but the sound of quiet. Ambient noises contribute to - and consist of - the performance. True silence does not exist. If one tilts their head right, the whole world sings. and, with that said, a playlist.
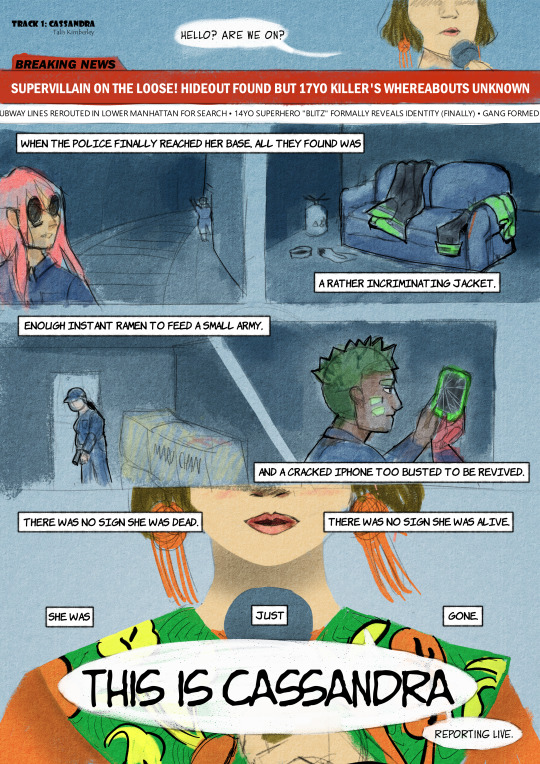
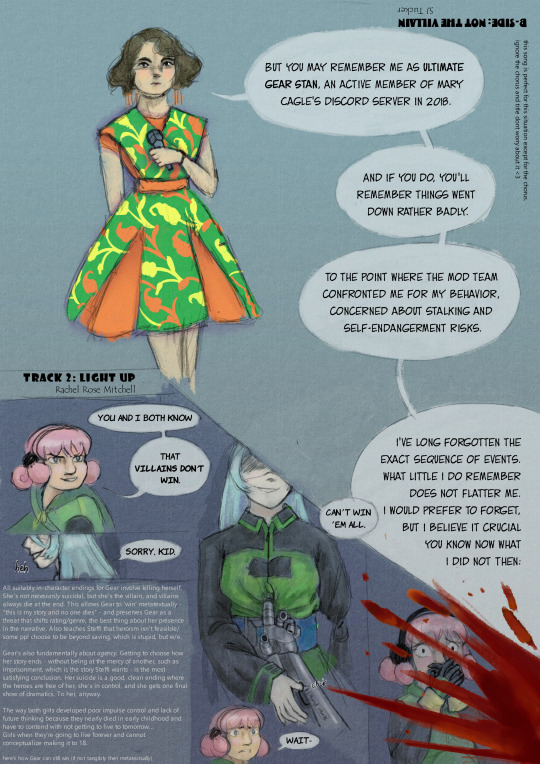
yeah, this one's a doozy. hi, cubewatermelon and co. miss me?
rhetorical question. don't answer that.
A few nitty-gritty things out of the way, first. this is specifically intended for the 2018 mod team for the sleepless domain fans discord server, primarily cubewatermelon/mary cagle. Folks who knew me are welcome to look on, but I'm not going to do much to catch people up to speed. hi, everyone! hope you're well!
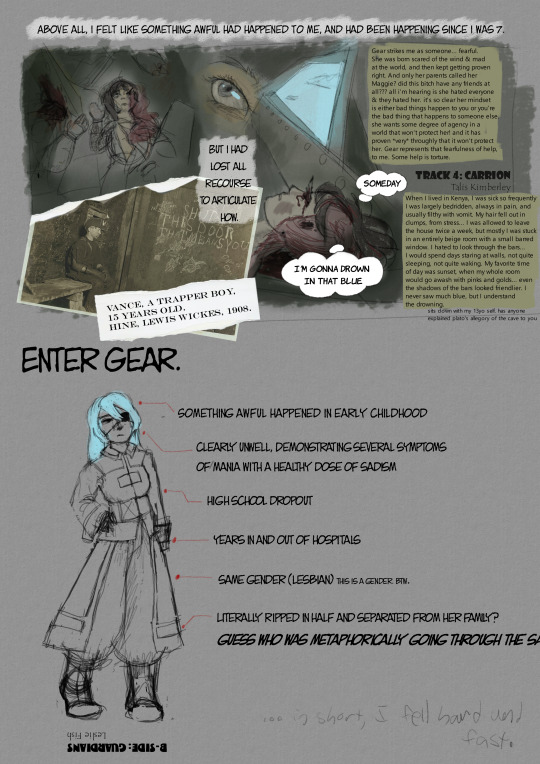
I also might be a bit disjointed or biased in my recollection. For reasons that will be made clear extremely soon, I can't put my childhood on a linear timeline. I can only express myself, and hope I don't mess it up horribly this time.
Noooowww to the big stuff. re: stalking; i genuinely didn't mean to stalk anyone, and when they told me to back off, i backed off. I am not willing to discuss this further. not being able to conceptualize other people's emotions or the consequences of my actions has caused some problems for me
that's an autism thing btw. im autistic i dont think i told anyone that
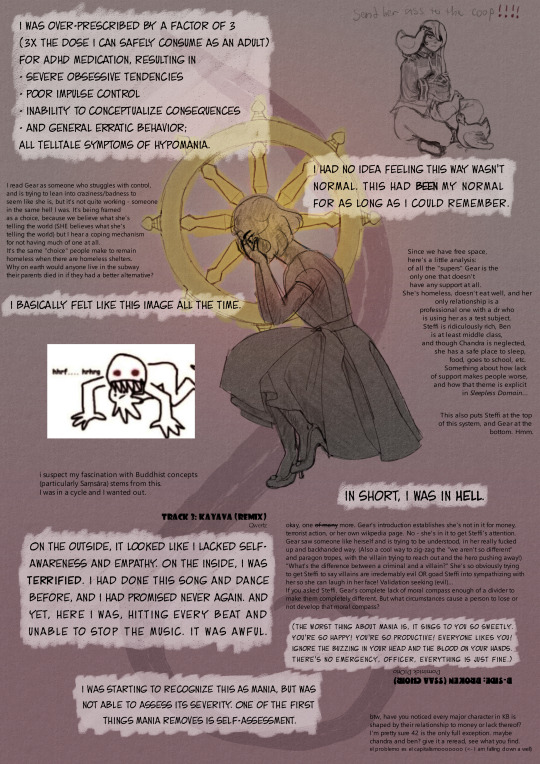
And now, the special guest you've all been waiting for: a big round of applause for the elephant in the room! In accordance with the WMA Declaration of Tokyo, the deliberate overprescription of psychotropic medication is a form of pharmacological torture. Most victims of pharmacological torture and experimentation are children, because it is nigh-impossible to sue for brain damage when there is no fully-formed adult brain for comparison prior to the abuse.
Torture is a strong word, but I don't have another word to use. psychiatric abuse usually describes mistreatment in psychiatric wards; pharmacological abuse describes a patient who takes advantage of a prescription; medical abuse is when a doctor (usually physically) abuses their patient. Being able to understand what happened to you is a form of agency, and I don't even have the words. I identify as a torture victim; this may change.
This high dose was precedented and legal, but the vaginal stretching of intersex infants is also legal. much involuntary psychiatric & psychotropic treatment (such as restraints and solitary confinement) are legal, and child marriage is legal. abuse is not abnormal: it is profoundly normal. Because something is normal, legal, and precedented does not prevent it from being torture.
and when your mother hands you a poison apple and says "here, eat this; it will be good for you; i hope someday you'll forgive me" you have to eat it, because you are eight years old and you don't get to argue with your mother. despite all this, I don't blame my aunt for refilling the high dose. when I said the dose was hurting me, she listened. (thank you, auntie. i wouldn't have gotten out without you.)
And this brings us to you. oh, you four. (five? i forget myself!)
I'd like to establish some context. I was used to things getting taken from me. friend groups in particular: I didn't expect to keep any friends, because I constantly expected to have to pack up and move on. I moved a lot in my childhood, and in Africa, i was constantly told that at some undetermined point in the near future, i'd have to go back to the states. living with my aunt was a temporary thing, i was expected to eventually move back in with my parents at some undetermined point in the future. I relied heavily on online friends because they were people I could have anywhere, so online communities were my only lifeline - not to mention, i was basically in solitary confinement while in Kenya.
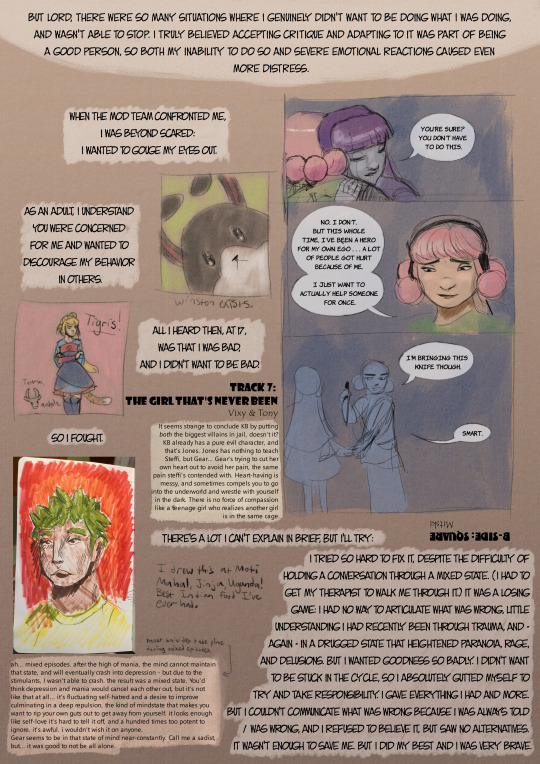
Most of all, I was terrified of my mental health/actions being exposed, examined, found lacking, and ultimately excluded. (this is why i was so afraid of psychiatric wards.) When you decided something had to be done about me - cutting me off from the server so i had to speak with you - It was either comply with your demands to communicate (which I could not, and did not understand why) or lose the community. I was so, so afraid of you i wanted to die when you all confronted me, and of course i couldn't say that, because only manipulative people would say "your attempt to solve this problem makes me want to seriously hurt myself."
But then I got called manipulative anyway <3 yay <3
Seriously: I wasn't trying to manipulate anyone, and i have no idea how you can manipulate someone without intention. (ah, that felt good to say!) Between medication spellbinding, alexithymia, and prior abuse, all my thoughts were so disordered i genuinely couldn't explain myself most of the time. Looking back, I have no childhood memory where I was fully lucid. I leaned into a manic persona because it was the only way I had any agency at all. I was something beyond both reason and self-recognition, and I willingly tried to brute-force my way through an extreme trauma response to please you. And you still hit me with my worst nightmare. that's why i was mad at you lol
I was so, so afraid, all the time, and I didn't even have the tools to understand I was afraid. How could someone as confident and impulsive as me be so fearful all the time? Was that manic persona freedom? Or was it a longer leash?
(Forgive my impulse toward rhetoric. I shouldn't ask questions you can't answer.)
I also couldn't say how badly i was hurting, because that would be venting, but you also accused me of venting when I was just talking about my day? or what was on my mind? I didn't understand that very well. autism moment, don't bother explaining it now. I also couldn't burden people with my actual mental health problems, because making strangers deal with that would be toxic! I resent you for setting up a system where it seemed safest not to speak and then punishing me for my inability to communicate. I resent every system that set me up for failure and punished me for failing, including yours.
And yet - I know that was not your intent! I can see in retrospect how hard you tried to be kind using the tools you had. The people with power over me, who genuinely did not want to do me harm and gave me multiple second chances, still upheld and facilitated the systems that tortured me; a miniature parody of the psychiatric system. (talk therapy and communication are useless if you struggle with self-awareness.) The same is true for the source: No person in my psychiatric treatment wanted me to suffer, and yet, here I am: a torture victim without a torturer. (except my parents, sort of.)
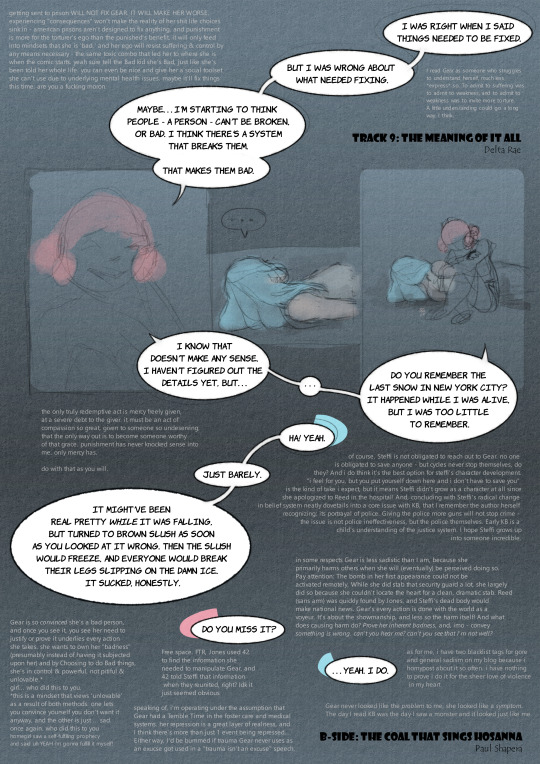
The logical conclusion, then: the system only intends to heal those who are already compliant, or prioritize compliance. The rest of us are treated to induce compliance, and if we still cannot, we are sequestered away. My medicine made me sick, and my prescribers made money off of keeping me sick - off of my torture. This is not a conspiracy: it is my lived experience.
However, even if i could communicate perfectly, we still would have had massive communication issues. Like - you know that one page where ben and steffi talk about dating, and ben says he thought steffi was gay? and steffi gets super defensive and it escalates into a screaming fight? I found that offensive, because a character getting that offput by the concept of not liking men (or a man) is kind of lesbophobic! But I understood that it would be a pain to redraw/write the page so they they fight about something else, don't fight, or some other solution, so i didn't need it to be fixed - just wanted to point out that was a reasonable interpretation, and one to be aware of in the future. but somehow my concerns got interpreted as a phrasing issue…? like, Ms. Cagle rewrote the page to say "weren't into guys" instead of "gay"..? You were very polite about it, Ms! But I found this interaction so baffling I didn't even try to correct it. that… wasn't what i said…
frankly we should bring back mildly homophobic steffi. twas narratively appropriate (<- different essay for a different time)
but yeah the whole communication operation was doomed from the start. rip!
The issue was always my inability to communicate, but my meds made it nigh-impossible to understand what I was feeling, and when I did, expressing myself could get me institutionalized. My suffering was inevitable but always, somehow, my fault. Awesome! *disintegrates into a pile of sand*
I cannot deny I was a girl like a box of matches waiting to be struck. You had no choice but to do as you did. But is it really what you ought to have done? (On this, I have no answer. I hope you have one that satisfies you.)
(that was genuine, by the by. i've spent a lot of time pondering this mess, and I still haven't found the "right" answer. I don't think there is one - though action or inaction, there is no version of this story where I don't suffer. I can only hope it was worth it. wait, hold on *adds the omelas child to my Kin List*)
Nor can I deny making my previous open letter in a small attempt to 'get back' at you - i'm not above that. lord knows i'm not innocent. but i really was trying to channel that rage into something productive. unfortunately i was doomed to fail because i didn't know what i meant. if you showed me that letter now, you'd hear a lot of "what? I don't know why I said that" "i have no idea why i would complain about something so minor" etc. You can disregard all that. This is what I was trying to say. the obsession, the trauma, the projection: all of it. So much of my obsession was talking around an issue i couldn't identify.
(meguka image) I know now
I knew I would be traumatized by this whole situation. I saw it coming and i could do nothing to stop it. But Gear was crucial to deciphering all this - in fact, suddenly thinking about her last year prompted me to really dissect my medical situation and realize i was tortured. I couldn't have done it without her. cassie & maggie, against the world.
Gear scans surprisingly well as a victim of long-term torture, actually. I don't think you meant to do that but good job!
speaking of her - i still don't think she's consistently suicidal. she's a real cockroach of a character, and I love her for it! But sometimes, i want to die and i want to live mean the same thing, because they both mean i need to get out of here. Imo, her thought processes and desires frequently contradict themselves, like mine did. and making your favs kill themselves in increasingly gruesome ways is really fun catharsis!
But please don't take this to mean I consider myself - or Gear - blameless. I love her because she's not blameless, because she's cruel for fun, because she'd rather be wicked than helpless. Like knows like. What I mean to say is, as of 2018, there is a black space between little Margret and Gear, and I saw all the signs of something very, very bad happening in that space. I know because I shared that space. what I mean to say is, teenage girls don't go out of their minds over nothing. Everything I made here is just an expression of what I heard in the narrative's silences.
and thus my biggest apprehension around revisiting the comic. knowing the author and I have such fundamentally different experiences with mental health - what if the signs of torture i picked up on weren't intended, or i completely made them up? what if, in the parts i haven't read yet, there's information that uproots my entire interpretation, or berates her for refusing mental health services that hurt me profoundly? how do you reconcile that a character so crucial to deciphering yourself may not be anything like you at all? I Don't Know. Shitpost, probably
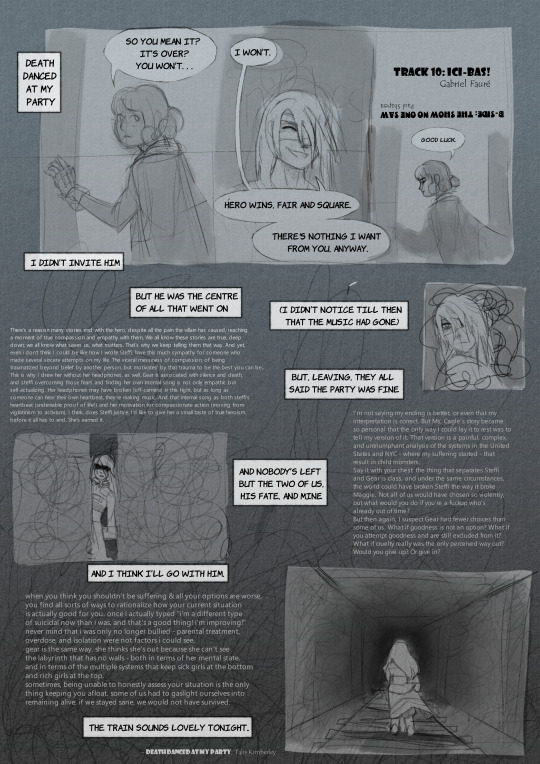
You're welcome to share those shitposts and whatnot by the way. Creating this let me put down years of hurt, and i hope it relieves you, too. I don't need to go back on the server, or forgiveness, or anything besides understanding. consider this a peace offering. the terms are yours.
Despite writing nearly 10k words, I still probably missed something or was callous or whatever. Self-expression and self-understanding are… new to me. My apology may be understated, but please take it as I meant it, with utmost sincerity. My askbox is open, and I'm more than happy to discuss antipsych resources, KB, What The Hell Is Wrong With Gear, artistic choices made in this comic, etc. I'm even down to reconnect on discord! Maybe. Uh, I'm conflicted. I reserve my right to not want to talk, be slow in responding, and so on, as should you. we've no obligations and all the time in the world. Let neither of us hurt ourselves in meeting because it's the "right" thing to do. I'm not blaming anyone or trying to start drama. If it would give you the most peace of mind to completely ignore this, please do so.
or, translated: as of right now, I'm not ready for any information about KB after steffi reunites with her dad, or difficult emotional reunions. I would really like to hear from everyone, and I'd appreciate casual well-wishes. I don't want things to be the same, I want them to be peaceful. Baby steps, cassie, baby steps. (very large and fearful prey animal tries not to run into oncoming traffic)
mostly, making this was for me. Perhaps I've said too much, but after spending so long unable to express myself freely, my art was cathartic and necessary. I'm no one's martyr or innocent, I'm just a torture victim trying to make sense of it all. I want to articulate some thoughts I couldn't figure out how to say before and make some silly things that make people laugh. Most of all, I'm happy in ways I never thought I could be, and I would like to share that joy with old acquaintances and other fans of a story I adored.
What I mean to say is: The train's about to leave the station, and there's an empty seat beside me. The train will still leave whether or not you board; but I would be honored not to go it alone!
Thank you to everyone who stuck by me even after the drama. Ethel, Felipe, Chris - even though we've fallen out of contact, your kindness and patience meant more than i can say. special thank you to @stars-in-a-jam-jar, the first person i confessed everything to after the smoke cleared, and someone i consider myself close with no matter how long we fall out of contact. My close online friends, @shafpanda, @theoandmoon, @dvanaestmrva, my honorary cousin @my-name-is-jimmy, and everyone else I confided in about my torture. and, of course, my partners @transloo and @teenyjellyfishy, and my little sibling, @aroacenezhaanddainsleif, the three people I love most in the world. Thank you, all. it is an honor to love you, and be loved by you.
#kiwi blitz#there's a lot more we could discuss. this barely scratched the surface#i didn't even MENTION barry and he's so important!#for now I'll just say: pain obfuscates everything outside of yourself#i still can't really conceptualize how yall feel about my actions other than 'probably bad?'#so i decided it was in the best taste to simply speak for myself#rather than put words in your mouth#i hope that's the right choice#it's funny. i thought i'd be angrier.#now there's just hope where my rage should be. how'd that happen?#torture tw#child torture tw#gore tw#medical abuse tw#psychiatric abuse tw#suicide tw#death tw#blood tw#abuse tw#parental abuse tw#child abuse tw#suicidal ideation tw#uhhh there's more probably. quite the laundry list here#also! you would express romantic attraction really strangely too#(as a severely undersocialized & completely manic lesbian teenager)#if you knew what happened to david kato.#not saying i was right obv. just saying.#ok back to never speaking of that again#this is cassandra
21 notes
·
View notes
Text
In the few studies that people have bothered to do, it's been found that involuntary inpatient (which I consider outright kidnapping and unlawful confinement) doesn't really help people. Outcomes are terrible, and the risk of further trauma is very high. Conditions are often terrible, abuse is rife, other medical care for other health conditions is poor to nonexistent, and patients are dehumanized and subjected to psychologically manipulative tactics. Also, they sometimes have to pay for their own incarceration.
Yet I can't usually tell my providers "I would literally kill myself when I got out, either out of immediate trauma, or as a knock-on effect of never again going for any sort of psychiatric care, leaving me unmedicated." I can't even tell them the truth.
"Oh, they won't actually section you if you just mention suicide." Why don't you talk to more people who have been sectioned and see just how much you are wrong.
I am in no way advocating for people not to get therapy and meds, to see if that helps, but psychiatry itself? Like, the system and also most of the actual medical part? It has next to no use at all, and is only there to gatekeep, pathologize, monitor, and threaten patients.
Therapy and meds have helped me immensely. Saved my life.
Psychiatry? Hasn't done shit besides diagnose me (which I found helpful). This constant micromanagement from the psych? The constant intrusive questions from even my GP because my file is flagged for regular mental illness "screenings" that actually do me more harm than good? The patronizing suspicion with which I am regarded for being on the meds I'm on? Fuck that.
The idea is to be able to go to someone who understands your conditions and is better able to manage medications for those conditions because those can be tricky. It's unfortunate that you can't be sure they can do the former, and that they actively seem not to want to do the latter, or do it poorly on purpose.
Extremely unpopular opinion but the concept of bodily autonomy needs to FULLY extend to extremely depressed people who are at risk of self-harm. Like, essentially arresting people for it doesn't fucking help, and violates their right to determine their own care. Get people some peer support, therapy, material assistance with daily tasks, get them help that helps. Don't make them walk on eggshells around twitchy medpros who will call the cops on them and throw them in crazy bitch jail for wanting a fucking break.
I'm sick of having to walk on my tiptoes while simultaneously disclosing my trauma to people who could send me off to be further traumatized. Either let me talk or YOU shut the fuck up and don't ASK me about it.
Especially if you aren't my psych or therapist! Sorry, GP's nurse, you don't have my trust. You are some random person I have never seen before. Let it fucking go.
6K notes
·
View notes
Text
5150

5150 is a term used to refer to the California Welfare and Institutions Code, Section. This section allows for the temporary, involuntary psychiatric confinement of individuals who present a danger to themselves or others due to signs of mental illness. The confinement can last up to 72 hours and is usually initiated by a family member, police officer, or another medical professional. During this period, the individual will receive an evaluation from a mental health professional to determine if he or she needs further treatment. If the individual is deemed to be a danger to himself or others, they may be admitted to a psychiatric hospital or another treatment facility for further care. It is an important tool in protecting the safety of individuals who are at risk of harming themselves or others.
0 notes
Note
are you against psychiatric medication universally or just as part of the system? or just as a matter of personal taste i guess?
I don’t think either?
I mean I certainly think using some psychoactive substances can be good and right for some ppl and I think it’s reasonable to go to doctors to get them prescribed. I’m not like, a scientologist
But. For one I think there are psychiatric drugs that essentially nobody should use and that I would recommend almost anyone I met to quit either openly or in secret if they are currently taking them—most antipsychotics fall under this heading
There is a more systemic critique here though than just some bad apple drugs. I think patients should in general approach their doctors adversarially, the way I would recytyem approaching a boss, or a landlord, or a high school teacher. You can derive benefits from that relationship, but you can’t trust them to be working in your best interests, and correspondingly you can’t treat your relationship as a cooperative partnership. Your prescriber is not your friend, and this goes double for an area of medicine like psychiatry where our medical understanding is so comparatively immature and that can so easily serve as a nexus of control and disenfranchisement
As an extension of this point: I think a lot of ppl taking psychiatric medication do so under coercion. Sometimes ofc this is so openly and unambiguously—with children, or under court orders, or for those under involuntary confinement—but sometimes more subtly. When ppl take it for fear of reprisal by family members, or school/employers, or informal support groups, for example. And again in such situations it is important to recognise that as a patient you are acting—whether compliantly or defiantly—under a condition of duress
And finally I am opposed to the metaphysic of Getting Treatment that is the moral expression of this relation of power and coercion. That for those suffering from Mental Illness there must exist somewhere out there the “right” medicine or therapy and that you should, even if not actively, always be pursuing it. There is nothing in the nature of the pharmaceutical industry or human psychology to guarantee there is out there always some drug or therapy such that taking it is better for a patient than taking nothing. And even if there is this is no guarantee the associated costs of seeking it out don’t outweigh the benefits
Sorry this is a bit rambly and doesn’t neatly answer yr question maybe? But it’s as close as I can give offhand
26 notes
·
View notes
Text
series of poor life decisions: a narrative
“oh gosh I should really sleep”
“well okay I’ll read one more link”
“oh, another interesting link, let me just read that and then I’ll sleep”
“huh, this mentions the Judge Rotenberg Center. I wonder what that is.”
*googles*
*reads*
*reads*
*should stop reading*
*can’t*
*reads*
*reads*
*reads*
5:15 AM: *is curled up in tiny ball of distress*
#aaaaaaa#this was so foreseeable#the mention even had a trigger warning#but did i listen#noooooo#speaking of which#psychiatric abuse cw#medical abuse cw#involuntary confinement cw#mental institutions cw#institutional abuse cw#psychiatry cw#medical cw#seriously do not google that#be smarter than me#sleep is for people who make good life decisions unlike me
19 notes
·
View notes
Text


https://disabilityvisibilityproject.com/2020/07/22/abolition-must-include-psychiatry/
There is a dangerous tale in the United States, one based on a myth of the deinstitutionalization of psychiatric asylums. Through this story, we are told that the asylum died and is a thing of the past. We are told that, now, “patients” have rights, are treated with human dignity, and are not criminalized for their neurodivergence. We’re told that restraints and forcible medication only happen in “extreme” cases. We’re told that the mental health care system is here to help us, support us, and “treat” us. And now, when abolition has entered mainstream discourse, we’re told that this very system should be considered an alternative to incarceration in jails and prisons. But those of us who have survived psychiatric incarceration know that not only did the asylum never die — it is, and always was, another prison. Knowing the truth of these myths, we work towards writing a new story.
...
As we talk about prison Abolition, discourse that was largely founded and remains spearheaded by revolutionary Black Women, we must reckon with the history of psychiatry, and better understand how the mental health system perpetuates processes of criminalization, policing, and surveillance. When we look deeper, we can see striking similarities between prisons and psychiatric institutions. As Leah Ida Harris described, both prisons and psychiatric institutions: have an overrepresentation of BIPOC (Black, Indigenous, and people of color), disregard the rights and safety of TGNC (trans and gender non-conforming) folks, use law enforcement transport/response, use solitary confinement and seclusion in cells/“rooms,” forcibly medicate folks (also known as chemical restraints), use physical restraints, offer extremely limited access to sunlight, fresh air, cell phones, news/media, and the outside world. In addition, sexual violence is routine, there is limited power to appeal legal/medical decisions, and the overwhelming majority of inmates are survivors of previous traumatic experiences. This year, the UN Special Rapporteur on Torture presented a report asserting that involuntary psychiatric interventions “may well amount to torture.”
Prison culture is not solvable by “funding the mental health system” more robustly. The mental “health” system is fundamentally carceral, meaning that it is one of the many kindred systems that function to contain and surveil people, take away their locus of control, isolate them from their communities, and limit their freedom. As it functions in America and in all places touched by colonialism, psychiatry is rooted in torture, white supremacy, and a culture of shame and punishment. Yes, the asylum lives on — and the police love the asylum.
Abolition means that all the cages come down, including those that function under the guise of psychiatric “care.”
The abolition of psychiatry does not mean that no one is allowed to identify with psychiatric diagnoses that they feel serve them, or that no one is allowed to continue taking psychiatric medications they find effective.
...
It means, too, that psychiatry was built with a core desire to dehumanize, drug, and discard those whose behavior and ways of being diverged from the status quo. This status quo was and is white, patriarchal, and absolutely enamored with respectability and compliance with the state’s self-serving notions of “normalcy.”
Many Psychiatric Survivors have made incredible strides in pursuit of justice, reform, and sometimes abolition. But the current nature of psych wards, which, for the most part, have remained violent, degrading prisons at which a majority of ex-inmates assert that they were not helped and were further traumatized, arguably indicates that the asylum never died. Why? Because it was never supposed to. Psychiatry IS the ethic of the asylum, and it will not fall until Psychiatry falls.
Our discussions of psychiatric abolition are deepened when we look to the history of prison culture in its many forms — policing, the death penalty, disposal of the divergent, and underneath it all, an allegiance to the binary notion that there are good people, and there are bad people. The punishment and disposal of the “bad” and divergent is not just an American problem, but its manifestations in this country are unique and inextricably rooted in the enslavement and genocide of Black and Indigenous folks. In Amerikkka, those who are “good” adhere to (or fit naturally into) the state’s status quo, and are useful cogs in the twin machines of white supremacy and capitalism. Within the state’s “bad” category are those whose utility to the state is questionable, which disproportionately includes BIPOC, TGNC folks, LGBTQIA2S+ folks, Disabled and Neurodivergent folks, poor folks, and those who attempt to hold the state accountable for its violence.
...
We would also like to validate that some folks have had good experiences in psych institutions. From an abolitionist lens, we believe that the good parts of those experiences could be replicated and improved upon within respite centers and other innovations in non-carceral healing spaces. Also, saying you had a good experience on a psych ward and therefore psychiatry shouldn’t be abolished is like saying the police have helped you and therefore shouldn’t be abolished—the point being that you are in the minority, and the wisdom of those who have suffered at the hands of these institutionally-backed harm-doers needs to be centered.
.
and here is the thing. all psych wards are bad. every single one. I don’t think there is such a thing as a good psych ward—I’m willing to believe that there are some good people who work in psych wards, who have good intentions, and who might end up helping some people. but the psych ward as a whole? There are no good psych wards. The structure of a psych ward inherently prevents it from being good. Even if you personally think you had a good experience in a psych ward, most likely what that means is that the abusive practices weren’t used on you. But those things are still there. even if you weren’t put into solitary confinement, it is extremely likely that your psych ward still had a room for that. even if you weren’t drugged without your consent, it is very likely other people were being drugged without consent!! even if you weren’t strip searched, or tied to your bed, or starved…it is VERY likely that your psych ward has protocols for all these things and regularly does them to many people who come through the ward! And it is vital to think about how your race, class, and other identities affected your experience before making broad claims about things “never happening” in psych wards.
Psych wards are inherently violent, oppressive, and unethical based solely on the fact that they are a form of incarceration, but even beyond that? If a psych ward is committed to enforcing compliance and incarceration, it is going to have some of those abusive measures that I listed above, and that is going to be standard protocol. Even if there are good people working in a psych ward, their reach is going to be limited—the power of the institution means that they constantly have to weigh the decision to break the rules and help someone, or to follow violent protocols. Most clinicians and staff will choose not to lose their job and even if they find it personally distasteful, will still choose to enable these types of violence. Good people on the inside are not able to fundamentally change the reality of what psych wards are and what they can do.
I strongly believe that people who say they have good experiences are the outlier and also are likely to be white and rich. Even if people don’t think that their experience was abusive, a lot of people generally find it boring, unhelpful, and mediocre. And so, so many people are experiencing abuse in a daily fucking basis in these places. Even if there are individuals who manage to escape the worst of a psych ward, the fact that the psych ward has the power, structure, and protocol to do these things to anyone is a problem.
9K notes
·
View notes
Text
A Brief Overview of Kinds of Mental Health Treatments and Terms
There is a wide variety of mental health treatments available to anyone seeking them. It would be nearly impossible to list all of them in one place. However, for the sake of better navigating healthcare spaces, here is an overview of the more common forms of treatment and other helpful terms to know:
Professionals:
Psychologist, counselor, and therapist - These are all titles of professionals that may provide therapy. There are slight differences between them in terms of the specific education they have. Those differences might come up in certain settings, but for most situations it's negligible. Each is able to be licensed to practice therapy and for the patient’s purposes that’s the only qualification they really need to check for. Each form of therapy requires a different license so any given professional may possess one or multiple.
Psychiatrist - A psychiatrist is a doctor that can prescribe medication for someone’s mental health (psychiatric medications). A professional has to have a doctorate to do this, so if you’re interested in medication, you want one of these, not anyone else. You can also get your medication from other doctors like a physician, but I strongly recommend you don’t. A physician isn't likely to be as diligent or knowledgeable on mental health medications, which is a shame because they can be very finicky to work with. A psychiatrist is probably going to be a better experience.
Psychiatrists do not typically provide talk therapy. If you want to do both (and you should since psychiatric medication is best used as a supplement to talk therapy) you’ll probably have to find a second provider
Social Worker - A social worker is a distinct kind of professional different from any of the ones listed above. A psychologist, counselor, therapist, and psychiatrist are all medical professionals. They’re main duties include serving as healthcare providers and providing treatment services. A social worker, on the other hand, is more of a case manager. They are educated in the mental health field and may be licensed to provide some limited treatment services. However, they’re main duties include looking over a client’s overall wellbeing and helping them manage their resources. A social worker may recognize a mental health issue in a client and diagnose it. However, they’re more likely to refer that client out to another provider than treat them themselves. Social workers may also help their clients with their living situation, employment, legal cases, and other aspects of life unrelated to mental health. For that reason, there aren’t really private practices for social workers. You are more likely to see them in larger facilities like a hospital or legal settings like those involved with health and family services.
Settings/Formats:
Remote/Virtual/Telehealth therapy - These are treatment services that are provided remotely through the internet, over the phone, through chat, or other messaging systems. Most forms of treatment like psychiatric appointments and therapy sessions can be done this way. Treatment services that require physical participation like exercise or animal therapy may not be available remotely. Also keep in mind that there may be instances in which you are asked to come in person, like if you need to take a medical test of some kind. That being said, it can be a great resource to those who do not have more local service providers, who have trouble with transportation, or who simply prefer to communicate digitally.
Outpatient - An outpatient program is one in which you come and go as opposed to living at a facility. Most forms of treatment are outpatient save for more intensive programs.
Partial Hospitalization Program (PHP) - This is a program that involves attending treatment multiple times per week for several hours a day. It typically includes both group therapy and individual therapy, but may offer other forms of therapy as well. Most of the time, this is provided on an outpatient basis without requiring overnight stay. However, some PHP programs may offer boarding services for convenience or require it outright.
Inpatient - An inpatient program is one in which you stay within a facility for a period of time. Despite being associated with involuntary confinements, inpatient programs are usually voluntary. Typically they are intended to last for longer periods of time: several days, multiple weeks, a month, or sometimes more. The inpatient component of treatment may be optional or may be required to participate in the other parts of treatment. Inpatient programs are pretty intensive and will probably involve several hours of multiple forms of treatment. Staying in a facility usually means you are required to stay on campus, but not necessarily inside. Most inpatient facilities have outdoor amenities and they may have instances in which you are allowed off campus potentially with supervision.
Services:
Psychiatric evaluation/assessment - This is a medical test that can be given by a licensed mental health professional. It is used to diagnose mental health disorders and recommend treatments. Most of the time this will be administered verbally but there may be written components as well. Your first appointment will usually be this as it allows the professional to get a good overview of what’s going on. That being said, don’t read too far into it. When done as a part of therapy, your evaluation will be more brief. The results aren’t intended to act as definitive statements. They’re more like jumping off points to identify what the main problems are and what might help them.
Outside of therapy, a psychiatric evaluation might be sought out to obtain documented proof of a disorder that can be used to qualify for disability benefits, accommodations in school, and other resources. When done for this purpose, the evaluations tend to be a bit longer and more involved since they are actually trying to find out without a doubt what’s going on.
There are other kinds of evaluations that might be given in different circumstances like a substance abuse evaluation for example. They are similar, but require different licenses, so any given professional may be able to do one or multiple kinds.
Individual Therapy - This is therapy conducted between only a therapist and the individual seeking treatment. It is the main form of therapy used to treat mental health disorders as well as less pathologic problems the individual is struggling with like grief, stress, trauma, and so on. It allows the therapist to focus almost entirely on the individual, their thoughts and feelings, the factors contributing to their problems, and the resources available to assist them. Although this form of therapy will always revolve around one individual, loved ones can be involved in it. Just keep in mind that it will be in the context of supporting the person seeking treatment, as opposed to the relationship between you. That is more appropriate for relationship therapy.
If you haven’t tried mental health treatment before or you don’t know what form of therapy you’re interested in, you should start here. Often an individual therapist serves a similar role as a primary care physician. They’re the first person you bring a problem to, they do a majority of treatment planning and case managing, and may provide referrals to other forms of treatment if necessary.
As such individual therapists can be found in almost any setting: hospitals, legal/correctional departments, treatment centers, and so on. If you find yourself in one of these settings, you’ll probably be assigned an individual therapist that works there. If you’re on your own, the easiest place to find one is a private practice that may be operated solely by the therapist or a medical group with multiple providers.
CBT, DBT, Mindfulness, and other forms of talk therapy - You might know a bit about different kinds of talk therapy such as Cognitive Behavioral Therapy, Dialectical Behavioral Therapy, Mindfulness, and so on. While the differences between these models is certainly fascinating and you may naturally come to learn about them during the course of treatment, you absolutely do not need to be familiar with them at all. That being said, there are some people who have a preference for or found success with one specific model or another and want to seek it out specifically. Thankfully, you don’t have to search too hard for them. Pretty much any form of talk therapy can be provided by anyone licensed to practice individual therapy. I said before that each kind of therapy requires a specific licence, but that doesn’t include these. Inversely, it is required to know multiple models of talk therapy in order to get a license to begin with. Moreover, talk therapy will usually incorporate elements from multiple models in different percentages depending on the client. If you’re interested in one in specific, you need only to inform your therapist and they can accommodate that request. No other additional steps need to be taken to find it.
Group Therapy - Group therapy is conducted between one therapist and a group of patients seeking treatment for the same, or closely similar, problems. The forms of talk therapy provided in group therapy will be largely the same as in individual therapy. The difference is just that you are being treated alongside others as well. It is intended to foster a community of social support, which can be a pivotal part of recovery, especially for those who may not have other supportive relationships. Patients in group therapy support one another and receive support in return in a mutual exchange, allowing them to feel like they are both contributing to a relationship and being cared for. They get the benefit of seeing their groupmates progress in their recovery, allowing them to learn from their success and ideally, believe success is possible for them as well. Sometimes the bonds created in group therapy can even persist after treatment.
Group therapy is usually provided by a larger facility like a hospital, a treatment center, a practice with multiple providers, and so on. A private practice owned and operated by a single person isn’t likely to have the resources to operate it, but may refer out to a specific facility.
Relationship/Family Therapy - This form of therapy focuses on a relationship between two or more people as opposed to one person in specific. Most commonly this is associated with marriage partners or parents and children, but it can be applied to any relationship between any number of people. This is usually found at a private practice or medical group.
Art, Music, Dance, Animal, Exercise, and other Non-traditional forms of Therapy - This encompasses a wide variety of forms of therapy. Truthfully, they deserve to be distinguished from one another as uniquely beneficial treatments, but in most contexts they’re lumped together under “miscellaneous.” To add to the disrespect, they may not always be acknowledged by health insurance companies. If they are, they might require a referral from another provider proving that you need that service in specific before they are willing to cover it. Ideally, anyone would be freely able to pursue these forms of treatment like they can others. Unfortunately they are not valued as highly so there may be additional obstacles in pursuing them. That being said, many of the individuals and facilities who offer these services may provide additional assistance outside of insurance to aid those interested in them. Since these forms of therapy are less common, they are usually provided by a private practice. However, that practice may also visit or contract with other facilities to provide their services to patients there.
Remember that this list is not exhaustive. Each form of treatment has its benefits, but not every kind will be a good fit for everyone. You might need to try more than one or a combination to address everything you’re struggling with, but try to stay hopeful. One of the most useful things you can do is understand your treatment and be an active part in the decision making process, so feel free to ask your provider questions if you don’t understand anything fully. Best of luck
For more information on mental health topics, check out our Index
#PSA#mental health#treatment#therapy#psychology#abnormal#depression#anxiety#PTSD#bipolar#OCD#psychosis#borderline#personality#selfharm#self harm#suicide#dissociation#ADHD#ADD#autism#disorder#selfcare#self care#wellness#positivity
1 note
·
View note
Text
i see my friends and professors sharing this number so please understand that when sharing the suicide hotline (including 988), if you are viewed as a danger to yourself, rather than being trained in de-escalation techniques, your location will be tracked and the police will be sent to you. mental health checks like these, esp for BIPOC, can mean life or death. and at best, you end up at a psychiatric facility which has treatment comparable to prison, exceedingly high rates of abuse & assault, and little to no autonomy this does NOT mean don't reach out for help, but rather look into non-carceral (and often times free) alternatives like warmlines, peer support specialists, and peer respites, PLEASE. you deserve compassionate, patient-led support, not incarceration.
As we talk about prison Abolition, discourse that was largely founded and remains spearheaded by revolutionary Black Women, we must reckon with the history of psychiatry, and better understand how the mental health system perpetuates processes of criminalization, policing, and surveillance. When we look deeper, we can see striking similarities between prisons and psychiatric institutions. As Leah Ida Harris described, both prisons and psychiatric institutions: have an overrepresentation of BIPOC (Black, Indigenous, and people of color), disregard the rights and safety of TGNC (trans and gender non-conforming) folks, use law enforcement transport/response, use solitary confinement and seclusion in cells/"rooms", forcibly medicate folks (also known as chemical restraints), use physical restraints, offer extremely limited access to sunlight, fresh air, cell phones, news/media, and the outside world. In addition, sexual violence is routine, there is limited power to appeal legal/medical decisions, and the overwhelming majority of inmates are survivors of previous traumatic experiences. This year, the UN Special Rapporteur on Torture presented a report asserting that involuntary psychiatric interventions "may well amount to torture."

i see this going around instagram yet again and in all my syllabi for school, so quick alert!
61 notes
·
View notes
Text
Sensory Deprivation
There’s a lot of confusion in the press, fiction and occasionally research about sensory deprivation. So as with solitary confinement I’ll start off with some definitions.
Sensory deprivation set ups reduce or mask at least the following senses: sight, hearing, smell and touch.
Additionally some equipment reduces the sensation of gravity.
I try to avoid describing tortures as ‘extreme’. I feel this can imply that some tortures are ‘less damaging’ or ‘safer’ and this is not true.
However the way that sensory deprivation damages human beings demands the term.
This is extreme.
It is almost uniquely damaging and the speed and extent of the damage inflicted is frankly terrifying.
Thankfully sensory deprivation has never ‘caught on’ as a torture.
I accept that as writers we often depict things that aren’t true to life. My advice regarding sensory deprivation is usually to avoid it. It has only been used to torture in isolated cases (a small number of mental health facilities in America) and the damage to characters is so severe that functioning in a basic way is unlikely.
I’m going to cover methods of sensory deprivation and then go on to the effects seen in volunteers and victims. So if you do decide to use it in your story you can do it as accurately as possible.
Baldwin’s Box
Confusingly not developed by Baldwin (it was developed by Donald Hebb who used it in ethical experiments), ‘Baldwin’s box’ is actually a small room. It’s padded and equipped with a ventilation system that masks smells from outside.
It is sometimes soundproof and sometimes the occupants wear ear muffs to mask sounds. It can be dark or under a constant, low lighting level. The interior is uniform and undecorated.
Occupants occasionally wear oven gloves, dark glasses or padded clothing to further mask their senses.
Baldwin’s box has been used in ethical and consensual experiments but it has also been used on unconsenting mental health patients and members of the American armed forces.
This is a structure that has to be specially built and quite sizeable. That means it both costs money and is relatively easy to detect. This is something that you’d need planning permission for.
So if you decide to use Baldwin’s Box sensory deprivation in your story consider how the structure was built or adjusted and how it might be disguised. Does your villain have the resources to build it from scratch? Do they have the space for this kind of structure? If they build it themselves where do they get the materials and are the materials flimsy enough that the occupant could break out (something that happened in at least one real life case).
Lilly’s Tank
Lilly’s tank is a sealed structure that’s significantly smaller than Baldwin’s box but significantly larger than a coffin. They might be around the size of a double bed (although Lilly’s original was significantly larger).
The tanks either has an air regulation system that masks smells from outside or a breathing mask that goes over the occupant’s head. It’s sound proof and it closes over the occupant cutting out light sources. Then tank is filled with a saline solution, kept at body temperature. This masks the sense of touch generally and also reduces the ability to feel temperature and creates a feeling of weightlessness.
Lilly’s tank affects more senses than Baldwin’s box. It’s significantly more complicated to make but smaller and commercially available. They’re currently used in some spas as a relaxation treatment, usually for an hour at a time.
Lilly, to his very great credit, halted his research and left his institution shortly after receiving questions on the use of his tank against ‘involuntary subjects’. His tank was never used on anyone unwilling and the vast majority of his research was done by experimenting on himself.
They’re expensive, the spa varieties are somewhere between $3,500-6,500 (via Rejali). They’re also cumbersome, difficult to maintain and full of water. This means that an unconsenting occupant would have ample opportunity to drown themselves, making their use as a torture device extremely unlikely.
Time frames for sensory deprivation experiments
As with solitary confinement the amount of time a volunteer will stay in one of these devices is a really important measurement.
During Hebb’s work using ‘Baldwin’s Box’ half of his volunteers left at around 24 hours. The extreme outlier in the group stayed in the ‘box’ for six days. Most of the others had left after two days.
In contrast the longest a volunteer has stayed in Lilly’s tank is 10 hours with the average duration a little under 4 hours.
Effects of Sensory Deprivation
Sensory deprivation produces extreme disorientation, insomnia, confusion, loss of ‘disciplinary control over the thinking process’ and hallucinations in willing volunteers.
Let me give you an example of what that means.
Hebb’s volunteers were so disorientated that they sometimes got lost inside the bathroom they went to for breaks and couldn’t leave it without assistance. One of them started hallucinating after 20 minutes. Hallucinations in Lilly’s tank occur in under three hours.
So far as I can tell willing volunteers who were confined for short periods (24 hours or less) didn’t suffer any lasting effects.
Beyond that the situation begins to get somewhat murky due to unclear records and poor research practices.
Baldwin, after whom the box is named, locked a US Army ‘volunteer’ in a sensory deprivation chamber for 40 hours during which Baldwin’s notes describe the man breaking down, crying and begging to be released. The ordeal ended when the man kicked his way out of the box.
Ewen Cameron subjected around 100 patients to sensory deprivation along with forced ECT keeping one woman ‘Mary C’ confined for 35 days.
A follow up study of 79 of Cameron’s patients ten years later noted unspecified ‘physical complications’ in 23% of the group. 85% were either hospitalised or ‘maintain psychiatric contact’.
60% had lost large chunks of their memory surrounding their time as a research subject, lost memories ranged from six months to ten years. 75% were judged as ‘unsatisfactory or impoverished’ when it came to interacting with other people and forming social bonds. Of the patients who had been working before they went into Cameron’s hospital around half could no longer work full time.
All of these people had received treatment in the intervening time.
In 1980, around thirty years after the experiments, a group of Cameron’s former subjects sued the CIA and Canadian government. Two of these people were unable, thirty years later, to recognise faces or everyday objects.
Some of the sources I’ve read recently that followed up Cameron’s patients suggest that a small number of them were able to leave hospital, find employment and live a relatively normal life. Which goes against my previous statements that all of them were permanently hospitalised or otherwise in care.
It’s not clear whether these victims were subjected to shorter periods of sensory deprivation.
Further factors to keep in mind
Sensory deprivation is, by definition, also solitary confinement. So victims subjected to sensory deprivation will also be suffering from the negative effects of solitary confinement and the effects of solitary confinement are likely to be exacerbated by the effects of sensory deprivation.
A lot of the asks I’ve had referring to sensory deprivation seem particularly interested in the effect this would have on children. Thankfully no one has ever done that experiment. My best guess is that the effects would be much much worse and would affect the child’s development and ability to interact with others profoundly.
The confusion and disorientation caused by sensory deprivation is also extreme enough that a character confined in this way might not be able to reliably eat, drink or take medication they’re provided with. Remember the long term is one day.
This is not as detailed as I’d like it to be; I’m struggling to find better sources. Hopefully this helps put sensory deprivation in perspective and clears up some of the questions people have had.
Sources
For clarity I’m breaking these into the ones I’ve actually read in full (which come first) and the original source or research material with some further reading.
Torture and Democracy by D Rejali, Princeton University Press, 2007
Cruel Britannia: A Secret History of Torture by I Cobain, Portobelo 2012
‘Effects of Decreased Variation in the Sensory Environment’ by W H Bexton, W Heron, T H Scott, Canadian Journal of Psychology 1954, 70-76
‘Production of Differential Amnesia as a Factor in the Treatment of Schizophrenia’ by D E Cameron, Comprehensive Psychiatry 1960
Intensive Electroconvulsive Therapy: A follow-up study by A E Schwartzman, P E Termansen, Canadian Psychiatric Association Journal 1967
The Search for the Manchurian Candidate, by J Marks, Norton Co 1991
The Mind Manipulators, by A Scheflin E Opton, 1978
A Textbook of Psychology, by D Hebb 1966, 2nd ed
‘Effects of Repetition of Verbal Signals upon the Behaviour of Chronic Psychoneurotic Patients’ by D E Cameron, L Levy, L Rubenstein, Journal of Mental Science 1960
Edit: Spending a short amount of time in one of Lilly’s tanks on a consensual basis does not make you better able to describe the hallucinations, terror and psychotic breaks they can cause when someone is locked in one for a prolonged period (over an hour) against their will.
Disclaimer
#tw torture#sensory deprivation#masterpost#unethical experimentation#tw ableism#Baldwin's box#Lilly's tank#effects of sensory deprivation
342 notes
·
View notes
Text
Huntington’s Disease
What is Huntington’s Disease?
Huntington’s Disease (sometimes referred to as Huntington’s Chorea) is a hereditary disease marked by degeneration of the brain cells causing chorea, progressive dementia, and other psychiatric disorders.
Chorea is a neurological disorder characterized by jerky involuntary movements affecting especially the shoulders, hips, and face.
Who is at risk?
Symptoms of Huntington’s Disease can develop at any time; however, it is most common for symptoms to appear when people are in their 30s and 40s.
Juvenile Huntington’s Disease is when symptoms occur before the age of 20, usually if the symptoms appear this early they are a little different and often progress faster.
Progression and duration varies. Time from the beginning of the disease to death is anywhere from 10 to 30 years. If the person has juvenile Huntington’s, life expectancy is about 10 years. Eventually, Huntington’s disease will cause a person to need help with all activities involved in living. Even further progression of the disease will lead to the person being confined to bed and not able to speak.
What causes Huntington’s Disease?
This neurological disease is caused by a single defective gene on chromosome 4. The defective gene is dominant, which means that people who inherit it from a parent that has Huntington’s will eventually develop the disease (only one parent has to have it). The gene is supposed to code for the Huntington protein; however, it is not yet known what this protein is supposed to do because scientists have only been able to identify its defective form.
What are the symptoms of Huntington’s Disease?
For Huntington’s Disease:
Movement issues like:
* chorea
* muscle rigidity or dystonia
* slow or abnormal eye movements
* impaired posture & balance
* issues with speech or swallowing
Cognitive issues like:
* problems organizing, focusing, & prioritizing tasks
* issues with getting stuck on thoughts, behaviors, or actions
* lack of impulse control, outbursts, acting without thinking, sexual promiscuity
* not being aware of their own behaviors
* trouble finding words or show processing of thoughts
* trouble learning new information
Psychiatric issues like:
* feeling sad or irritable
* withdrawing socially
* loss of energy & fatigue
* insomnia
* thoughts of death or suicide
* bipolar disorder
* mania
* obsessive-compulsive disorder (OCD)
Juvenile Symptoms:
Behavioral changes:
* trouble paying attention
* a drop (a rapid one) in school performance
* behavioral issues
Physical changes:
* rigidity in muscles that affects gait
* tremors & involuntary movements
* falls & clumsiness
* seizures
What are the treatment options for Huntington’s Disease?
As of now, there is no cure and no way to slow the progression of Huntington’s.
* Olansapine (an antipsychotic drug) used to help with chorea.
* Antipsychotic drugs are recommended for severe anger or threatening behavior
* For symptoms that are experienced by those who have Huntington’s, like anxiety, depression, and insomnia, it is recommended that regularly prescribed medications that are often used to treat these disorders be used.
Sources:
Definitions from Oxford Dictionary
https://www.mayoclinic.org/diseases-conditions/huntingtons-disease/symptoms-causes/syc-20356117
https://www.alz.org/alzheimers-dementia/what-is-dementia/types-of-dementia/huntington-s-disease#:~:text=Huntington's%20disease%20is%20a%20progressive,will%20eventually%20develop%20the%20disease.
#huntingtons disease#huntingtons#neuroscience#neurological#neurological disorder#neurological disorders#neurological diseases#diseases and disorders#diseases#huntingtons awareness
0 notes
Link
Expanding Involuntary Confinement is Not the Answer to Solve Gun Violence Institutionalizing People Against Their Will is Usually a Mistake
In the wake of last weekend’s tragic shootings, President Trump did what he does best: stoked fear and cast blame. He proclaimed that “we must reform our mental health laws to better identify mentally disturbed individuals who may commit acts of violence and make sure those people, not only get treatment, but when necessary, involuntary confinement.”
There are two things wrong with the idea of involuntary commitment as a solution to gun violence. First, focusing on people with identifiable mental disabilities won’t help. The data is clear: mental disability is not the primary cause of gun violence. Second, making it easier to commit people against their will would repeat one of the great wrongs of the last 150 years. It will rob innocent people of their most basic civil liberty: the day-to-day freedom to live on your own and make your own decisions about whether and what kind of medical treatment to receive.
In its modern form, the institutionalization of people with disabilities first emerged in the nineteenth century. Initially, the goal for mental institutions was to provide treatment, and quickly return patients to the community. However, facilities soon became warehouses for the same people for years and sometimes decades as they failed to deliver the quick cures they had once promised.
These problems were further exacerbated by the eugenics movement, which dramatically expanded the institutionalization of people with mental disabilities. Eugenics held that humanity should be improved by “removing” “inferior” stock from the country including, Jews, all people of color, Catholics, southern and Eastern Europeans, and people with mental and physical disabilities. The movement’s great victories were immigration laws largely based on racism and the involuntary sterilization and forced institutionalization of people with disabilities. These measures disproportionately targeted low-income Americans and, in the case of sterilization, women.
Proponents of eugenics promoted the idea that people with mental disabilities were violent, sexually promiscuous, and dangerous to society. None of it true. They succeeded in shifting the goal of institutionalization from helping the individual patient — an objective institutions were already failing to achieve — to protect society from perceived risks based on stereotypes. To eugenicists, the solution was lifelong institutionalization.
By the 1970s, thousands of people with mental disabilities were languishing in institutions — many of them living under shocking conditions of abuse and neglect. Senator Robert Kennedy and journalist Geraldo Rivera were among the first to expose these abuses at Willowbrook State School, a massive institution in New York.
In response, the New York Civil Liberties Union filed a class-action lawsuit representing the 5,400 people with mental disabilities living at Willowbrook. After three years the case forced reforms that would lead to Willowbrook’s closure, and give those within it the opportunity to live free.
NYCLU and the ACLU continued to fight for people with mental disabilities, setting up a Mental Health Law Project (now the independent Bazelon Center for Mental Health law). The tide really began to turn after the ACLU won Kenneth Donaldson’s case in the Supreme Court. Donaldson appeared to have a mental illness but had never posed a danger to himself or anyone else. He was nonetheless involuntarily confined in a mental hospital for fifteen years because other people found him disturbing. The Supreme Court ruled: “Mere public intolerance or animosity cannot constitutionally justify the deprivation of a person's physical liberty. In short, a State cannot constitutionally confine without more a non-dangerous individual who is capable of surviving safely in freedom by himself or with the help of willing and responsible family members or friends.”
People with psychiatric and intellectual disabilities have had a long and difficult path to basic freedom in the United States. This is not the moment to turn back, and most especially not in the name of safety.
The right to keep and bear arms is subject to regulation. Just like the right to privacy, the right to be free from government searches, even the right to speech. While the Constitution allows guns to protect one’s home, it does not stop the state from regulating or banning assault weapons or high capacity clips.
Nevertheless, targeting a group of Americans for incarceration is not the answer. The demographic with the highest rates of gun violence are men between the ages of 16 and 35. No one would propose as a solution forcibly institutionalizing all young men.
If the Eugenics movement sounds familiar, it should. It is largely being recycled by today’s white supremacists. Solutions to the epidemic of gun violence should be based on data, not a return to a shameful episode from our past.
Published August 13, 2019 at 09:30PM via ACLU https://ift.tt/2Z3KrOu
0 notes
Text
Yale Psychiatrist Calls On Pelosi To Put “A Mental Health Hold” On Trump
I have previously criticized psychiatrists who have regularly appeared on the air to identify a variety of mental illness that they have observed in President Donald Trump from afar. As I discussed in a prior column on the demise of the Goldwater rule, this is diagnosis without examination and often seems mixed with strong political judgments about Trump’s political positions. Bandy X. Lee, a professor of psychiatry at the Yale University School of Medicine, has been one of the most outspoken and last week urged House Speaker Nancy Pelosi to demand some ill-defined “hold” on the president pending psychiatric examination. Her position latest position is utterly bizarre but has been treated as a serious discussion point by some media like Salon magazine.
Lee previously served as the editor of the book “The Dangerous Case of Donald Trump: 27 Psychiatrists and Mental Health Experts Assess a President” and has continually argued for removal on the basis for mental illness. I previously discussed the difficulties in pursuing such loose analysis as the basis for removal under the 25th Amendment.
Lee’s most recent call for some form of intervention by Pelosi seems utterly disconnected from the constitutional process. She bizarrely treated this as an office intervention. Lee told Salon that “As a co-worker, she has the right to have him submit to an involuntary evaluation, but she has not. I am beginning to believe that a mental health hold, which we have tried to avoid, will become inevitable.”
I am at a loss on this one. Does Lee think that Pelosi can “as a co-worker” force the President into an involuntary evaluation? The only provision from incapacity of a president is found in the 25th Amendment and it omits such a workplace evaluation process. As I previously discussed, Section 4 has, essentially, two avenues for dragging a president from the Oval Office. First, there is the mutiny option. A vice president and a majority of the Cabinet can agree that the president is “unable to discharge the powers and duties of his office” and notify Congress that the vice president intends to take over. If Vice President Pence could get eight Cabinet officers to sign a letter to that effect, he would immediately become the “Acting President.” But if the president then declares to Congress that “no inability exists,” Trump could resume his powers.
Pence and the rebellious Cabinet would then have to send another declaration within four days to the President pro tempore of the Senate and the Speaker of the House that says, more or less, don’t believe a word, he’s unfit. Once Congress had the second declaration, if not already in session, it would have 48 hours to assemble to debate the issue. It would then have 21 days to vote on the president’s fitness. To remove the president, two-thirds of both houses would have to agree. If Congress did not vote within 21 days, the president would get his power back.
Notably, Lee again seems triggered by policies or actions with which she disagrees. This latest call for co-worker intervention was due to the killing of Iranian Maj. Gen. Qassem Soleimani. I also raised concerns over this action as a possible assassination in violation of U.S. law and an act of war under international law. However, Trump is not the first president to attack individuals on foreign soil whether it was Osama Bin Laden or the attempt on former Libyan President Muammar el-Qaddafi.
Lee’s medical diagnosis is hard to untangle from her political judgment. She insists that this is “exactly what someone who lacks mental capacity would do.”:
“This is exactly the kind of dangerous event we foresaw as Donald Trump’s response to the impeachment proceedings, just as his pulling troops from northern Syria was a direct response to the announcement of an impeachment inquiry . . . In other words, he is extremely drawn to actions that would help him appear as if he has mental capacity, such as a ‘presidential strike’ against an enemy, while avoiding the proper procedures, such as briefing with Congress, that might expose his lack of capacity . . . What we do not expect from someone who lacks mental capacity is rational, reality-based decision making that is non-impulsive, non-reckless, and cognizant of consequences.”
She adds that his attacks on President Obama must also be treated as a reflection of his mental illness: “Since he is incapable of putting himself in another person’s shoes, he projects his own thoughts entirely onto others. Hence, we can deduce that what he has said about Mr. Obama has nothing to do with the former president but has only to do with the way he himself thinks.”
At points, Lee seems herself a bit adrift. When asked about the widespread criticism of her claims of mental illness, Lee responded “My critics do not have an argument. There are many situations where I hoped that my formulation would be wrong — but now that my hypotheses have been tested so many times to 100 percent precision.”
Really? She is 100 percent right without ever actually personally examining the subject.
Then the interview gets downright batty when the 25th Amendment is raised:
“Yes. In this country, no one is above the law, and as far as mental health laws and the president are concerned, there is no Office of Legal Counsel memo, no exceptions and at this time not even confidentiality, since he has yet to be a patient. Before it is a political matter involving impeachment or the 25th Amendment, it is a medical matter. The physical danger due to psychological impairment needs to be removed, and we are bound by our own professional code not to abandon persons or the public in danger. We are even legally bound to take steps to protect potential victims if warning is insufficient and security staff will not act. If the personal physician is unavailable or too conflicted to do so, any physician can.
A 72-hour hold does not require court intervention and is enough for a solid evaluation. There is no shortage of mental health professionals willing to put their names to commitment papers, and multiple legal groups have offered to file for a court order for security staff to cooperate. All we need are auspices so as to show it is not a coup or something nefarious — although, at this point, we may need to proceed anyway because the populace is growing too sick to see any intervention as legitimate unless it is illegitimate. This is common in mental health settings, and we apply the proper treatment according to standard anyway with the hope that patients will improve enough to see that you have helped them — which happens most of the time. It is this nature of mental disease that has allowed for civil commitment laws to be possible in a country that protects civil liberties.”
Could you imagine the future of our system if a Speaker of the House could have a president civilly committed for involuntary examination? Some Republicans would no doubt have asked Pelosi’s GOP predecessor for the same civil confinement of President Obama. We would need a regular presidential suite at St. Elizabeth’s. Lee herself shows the potential for securing favorable rulings from doctors who believe no sane person could hold certain political views or take certain actions.
It would be, in a word, madness.
Yale Psychiatrist Calls On Pelosi To Put “A Mental Health Hold” On Trump published first on https://immigrationlawyerto.tumblr.com/
0 notes
Text
Expanding Involuntary Confinement is Not the Answer to Solve Gun Violence
Institutionalizing People Against Their Will is Usually a Mistake
In the wake of last weekend’s tragic shootings, President Trump did what he does best: stoked fear and cast blame. He proclaimed that “we must reform our mental health laws to better identify mentally disturbed individuals who may commit acts of violence and make sure those people, not only get treatment, but when necessary, involuntary confinement.”
There are two things wrong with the idea of involuntary commitment as a solution to gun violence. First, focusing on people with identifiable mental disabilities won’t help. The data is clear: mental disability is not the primary cause of gun violence. Second, making it easier to commit people against their will would repeat one of the great wrongs of the last 150 years. It will rob innocent people of their most basic civil liberty: the day-to-day freedom to live on your own and make your own decisions about whether and what kind of medical treatment to receive.
In its modern form, the institutionalization of people with disabilities first emerged in the nineteenth century. Initially, the goal for mental institutions was to provide treatment, and quickly return patients to the community. However, facilities soon became warehouses for the same people for years and sometimes decades as they failed to deliver the quick cures they had once promised.
These problems were further exacerbated by the eugenics movement, which dramatically expanded the institutionalization of people with mental disabilities. Eugenics held that humanity should be improved by “removing” “inferior” stock from the country including, Jews, all people of color, Catholics, southern and Eastern Europeans, and people with mental and physical disabilities. The movement’s great victories were immigration laws largely based on racism and the involuntary sterilization and forced institutionalization of people with disabilities. These measures disproportionately targeted low-income Americans and, in the case of sterilization, women.
Proponents of eugenics promoted the idea that people with mental disabilities were violent, sexually promiscuous, and dangerous to society. None of it true. They succeeded in shifting the goal of institutionalization from helping the individual patient — an objective institutions were already failing to achieve — to protect society from perceived risks based on stereotypes. To eugenicists, the solution was lifelong institutionalization.
By the 1970s, thousands of people with mental disabilities were languishing in institutions — many of them living under shocking conditions of abuse and neglect. Senator Robert Kennedy and journalist Geraldo Rivera were among the first to expose these abuses at Willowbrook State School, a massive institution in New York.
In response, the New York Civil Liberties Union filed a class-action lawsuit representing the 5,400 people with mental disabilities living at Willowbrook. After three years the case forced reforms that would lead to Willowbrook’s closure, and give those within it the opportunity to live free.
NYCLU and the ACLU continued to fight for people with mental disabilities, setting up a Mental Health Law Project (now the independent Bazelon Center for Mental Health law). The tide really began to turn after the ACLU won Kenneth Donaldson’s case in the Supreme Court. Donaldson appeared to have a mental illness but had never posed a danger to himself or anyone else. He was nonetheless involuntarily confined in a mental hospital for fifteen years because other people found him disturbing. The Supreme Court ruled: “Mere public intolerance or animosity cannot constitutionally justify the deprivation of a person's physical liberty. In short, a State cannot constitutionally confine without more a non-dangerous individual who is capable of surviving safely in freedom by himself or with the help of willing and responsible family members or friends.”
People with psychiatric and intellectual disabilities have had a long and difficult path to basic freedom in the United States. This is not the moment to turn back, and most especially not in the name of safety.
The right to keep and bear arms is subject to regulation. Just like the right to privacy, the right to be free from government searches, even the right to speech. While the Constitution allows guns to protect one’s home, it does not stop the state from regulating or banning assault weapons or high capacity clips.
Nevertheless, targeting a group of Americans for incarceration is not the answer. The demographic with the highest rates of gun violence are men between the ages of 16 and 35. No one would propose as a solution forcibly institutionalizing all young men.
If the Eugenics movement sounds familiar, it should. It is largely being recycled by today’s white supremacists. Solutions to the epidemic of gun violence should be based on data, not a return to a shameful episode from our past.
from RSSMix.com Mix ID 8247012 https://www.aclu.org/blog/disability-rights/integration-and-autonomy-people-disabilities/expanding-involuntary via http://www.rssmix.com/
0 notes
Photo

“5150: A Comission” • A 5150 is an involuntary 72-hour hold in a psychiatric facility, for evaluation. A peace officer, registered nurse, medical doctor, or certain other categories of people may place the hold. Three criteria apply to this section: a danger to themselves, a danger to others, or gravely disabled. A qualified officer, which includes any California peace officer, as well as any specifically-designated county clinician, can request the confinement after signing a written declaration stating the psychiatric diagnosis that the diagnosing medical professional believes to be the cause or reason why they believe the patient to be "a danger to themselves or others" or the psychiatric disorder that has rendered the patient incapable of making their own medical treatment decisions. #JustFriends #AvantGarments #5150 #Locomias #MentalHealth #Embroidery #Logo #Screenprinting #Longsleeves #BuyLocal #MadeInColombia // #KidsSeeGhosts (at 5150 Productions) https://www.instagram.com/p/BmedK9Jhdel/?utm_source=ig_tumblr_share&igshid=kqjf2a2wuwds
#justfriends#avantgarments#5150#locomias#mentalhealth#embroidery#logo#screenprinting#longsleeves#buylocal#madeincolombia#kidsseeghosts
0 notes