#diagnosis and treatment of sleep disorders
Explore tagged Tumblr posts
Text
The Science of Sleep: Understanding the Importance of a Good Night's Rest
We all know how it feels to wake up after a restless night, groggy and exhausted. But did you know that lack of sleep can have serious consequences on our physical and mental health? In this blog post, we will be diving into the science of sleep, exploring what happens in our bodies when we sleep and providing practical tips for getting a better night’s rest. Sleep is essential for our overall…

View On WordPress
#bedtime routine for better sleep#creating the perfect sleep environment#diagnosis and treatment of sleep disorders#establishing a regular sleep schedule#how to improve sleep quality#how to sleep#natural remedies for restless leg syndrome#sleep and aging#sleep and athletic performance#sleep and mental health#sleep and productivity#sleep and weight loss#sleep and your immune system#sleep apnea treatment options#sleep tips for insomnia#sleeping problems#the importance of sleep for overall health and well-being
0 notes
Text
I hate how people view autistic people and sex. I've seen a lot of people say that autistic people can't enjoy sexual things which is completely not true. Autistic people are people who can enjoy sex and masurbation the same as neurotypicals. We are capable of it, and thinking overwise is incredibly infantilising. I've been masterbating since I was 4 years old, and when I say that people either don't believe me or are disgusted. But what is there not to enjoy?? Like yes, I want to move my body in a way that makes me feel good. Let me enjoy stimming in this way 🙏🙏
#actually autistic#autism#autistic experiences#autism spectrum disorder#autistic adult#autistic things#autism and sleep#autistic culture#being autistic#neurodivergent#asd#autism spectrum condition#autism struggles#autism diagnosis#autism experiences#autism rant#autism thoughts#autism treatment#autism traits#autism is autisming#autism infantilising is not cool
8 notes
·
View notes
Text
Sleep Disorders Doctor | Dr. Lakshmi Kolli, MD | Sleep Apnea Help | Spring Hill, FL
Sleep is essential to living a healthy, happy life. However, for many people, sleep disorders like sleep apnea can significantly disrupt their health and quality of life. If you or a loved one is struggling with sleep issues, Dr. Lakshmi Kolli, MD, is here to help. As a leading sleep disorders doctor in Spring Hill, FL, Dr. Kolli offers compassionate, expert care to diagnose and treat a wide range of sleep problems, helping patients regain restorative sleep and improve their overall well-being.

Why Sleep Is Crucial to Your Health
Sleep plays a critical role in maintaining physical, mental, and emotional health. Poor sleep can lead to a range of health issues, including:
Heart disease and high blood pressure
Obesity and weight gain
Cognitive impairment, memory loss, and poor concentration
Mood disorders like anxiety and depression
Chronic fatigue and decreased productivity
If you frequently wake up feeling tired, snore loudly, or experience interruptions in your breathing while sleeping, you may be suffering from a sleep disorder like sleep apnea.
What Is Sleep Apnea?
Sleep apnea is one of the most common sleep disorders, affecting millions of Americans. It occurs when your breathing stops repeatedly during sleep due to blocked airways or improper signals from your brain.
Types of Sleep Apnea
Obstructive Sleep Apnea (OSA): Caused by physical airway blockage, often due to relaxed throat muscles.
Central Sleep Apnea (CSA): Occurs when the brain fails to send proper signals to control breathing.
Complex Sleep Apnea Syndrome: A combination of OSA and CSA.
Symptoms of Sleep Apnea
Loud snoring
Gasping or choking during sleep
Excessive daytime sleepiness
Morning headaches
Insomnia or frequent nighttime awakenings
Difficulty concentrating during the day
If you or someone you know experiences these symptoms, seeking a sleep disorders doctor like Dr. Lakshmi Kolli in Spring Hill, FL, is essential.
Meet Dr. Lakshmi Kolli, MD: Sleep Disorders Specialist
Dr. Lakshmi Kolli, MD, is a board-certified physician specializing in the diagnosis and treatment of sleep disorders, including sleep apnea. With years of experience and a patient-focused approach, Dr. Kolli has earned a reputation for providing personalized care to individuals struggling with sleep issues.
Why Choose Dr. Kolli?
Expertise in Sleep Medicine: Specialized knowledge to diagnose and manage sleep apnea and other disorders.
Comprehensive Care: Thorough evaluations, advanced testing, and customized treatment plans.
Compassionate Approach: Dr. Kolli listens to your concerns, explains your diagnosis, and works with you to find the best solutions.
Advanced Diagnostic Tools: Use of modern sleep studies and testing for accurate diagnosis.
Dr. Kolli is committed to helping her patients in Spring Hill, FL, achieve healthy, restorative sleep and live a better quality of life.
Comprehensive Sleep Disorder Services Offered in Spring Hill, FL
Dr. Lakshmi Kolli provides a full range of diagnostic and treatment options to address various sleep disorders, including:
1. Sleep Apnea Diagnosis and Treatment
In-Clinic and At-Home Sleep Studies: To monitor your breathing, heart rate, and brain activity during sleep.
CPAP Therapy: Continuous Positive Airway Pressure (CPAP) machines to keep your airway open during sleep.
Oral Appliance Therapy: Customized oral devices for mild to moderate sleep apnea.
Lifestyle Modifications: Guidance on weight loss, sleeping positions, and habits to improve sleep.
2. Insomnia Management
Dr. Kolli offers therapies and solutions to address chronic insomnia, helping patients fall asleep faster and stay asleep longer.
3. Restless Leg Syndrome (RLS) Treatment
Tailored therapies to reduce the uncomfortable sensations and urge to move the legs that disrupt sleep.
4. Narcolepsy Diagnosis and Treatment
Evaluation and treatment options to manage excessive daytime sleepiness and sudden sleep attacks.
5. Parasomnias and Circadian Rhythm Disorders
Care for conditions like sleepwalking, night terrors, and misaligned sleep schedules.
What to Expect During Your Visit
When you visit Dr. Lakshmi Kolli, MD, for sleep disorder care, you can expect a thorough and supportive process:
Comprehensive Evaluation: Dr. Kolli will discuss your symptoms, medical history, and sleep habits.
Advanced Testing: You may undergo a sleep study, either at home or in a sleep center, to monitor your sleep patterns.
Personalized Treatment Plan: Based on your diagnosis, Dr. Kolli will create a treatment plan tailored to your specific needs.
Ongoing Support and Follow-Up: Dr. Kolli will track your progress and make necessary adjustments to ensure effective treatment.
Sleep Better, Live Better: Benefits of Treating Sleep Disorders
Proper treatment for sleep disorders can transform your life. Benefits include:
Improved energy and daytime alertness
Better heart health and blood pressure control
Enhanced mental clarity and focus
Reduced risk of accidents due to fatigue
A happier, healthier lifestyle
Dr. Lakshmi Kolli has helped countless patients in Spring Hill, FL, overcome their sleep challenges and enjoy better health. Don’t let sleep apnea or other disorders hold you back from living your best life.
Schedule Your Appointment with Dr. Lakshmi Kolli in Spring Hill, FL
If you’re experiencing symptoms of sleep apnea or any other sleep disorder, don’t wait. Early diagnosis and treatment are key to preventing serious health complications.
Contact Dr. Lakshmi Kolli, MD, Today!
Address: 10500 Spring Hill Dr, Spring Hill, FL 34608
Phone: (352) 835–7155
Website: https://springhillprimarycare.com
Dr. Kolli and her dedicated team are ready to help you achieve restful, quality sleep and improve your overall well-being.
FAQs About Sleep Disorders and Sleep Apnea
Q: How do I know if I have sleep apnea?
A: Common signs include loud snoring, daytime fatigue, and pauses in breathing during sleep. A sleep study can confirm the diagnosis.
Q: Is sleep apnea dangerous?
A: Yes, untreated sleep apnea can increase the risk of heart disease, stroke, diabetes, and accidents.
Q: What is a sleep study?
A: A sleep study monitors your breathing, heart rate, and brain activity to diagnose sleep disorders like sleep apnea.
Q: Do I need a CPAP machine for sleep apnea?
A: CPAP is a common treatment for moderate to severe sleep apnea. Dr. Kolli can help determine if it’s right for you.
Take the First Step Toward Better Sleep
Sleep disorders like sleep apnea don’t have to control your life. With expert care from Dr. Lakshmi Kolli, MD, in Spring Hill, FL, you can take the first step toward better sleep and better health.
Call today to schedule your consultation and start your journey to restful, rejuvenating sleep.
#SpringHill#SleepApnea#SleepDisorders#SleepMedicine#Doctor#Healthcare#MedicalClinic#Spring Hill sleep doctor#Spring Hill sleep clinic#Spring Hill sleep apnea treatment#sleep apnea treatment#sleep study#sleep disorder diagnosis#sleep medicine
0 notes
Text
Lewy body disease: a complex dementia
Lewy body disease is a complex neurodegenerative disease that progressively affects cognitive function, movement and sleep. It is characterised by the presence of abnormal deposits of proteins called Lewy bodies in certain brain cells. These deposits disrupt the normal function of these cells, leading to a variety of symptoms.

What are the main symptoms of Lewy body disease?
The symptoms of Lewy body disease are varied and can change over time. Among the most common are
- Cognitive fluctuations: Intellectual abilities can vary considerably from one moment to the next, with periods of lucidity alternating with episodes of confusion or disorientation.
- Visual hallucinations: These hallucinations are often very realistic and can be frightening for the person experiencing them. They may take the form of people, animals or objects.
- Movement disorders: Similar to Parkinson's disease, movement disorders include tremors, muscle rigidity, slowness of movement (bradykinesia) and difficulty maintaining balance.
- Sleep disorders: People with Lewy body disease often suffer from REM (rapid eye movement) sleep disorders, manifested by agitated sleep behaviour, intense nightmares or nocturnal visual hallucinations.
- Behavioural problems: Mood swings, agitation, attention problems and conduct disorders may also occur.
How is Lewy body disease diagnosed?
Diagnosing Lewy body disease can be complex, as the symptoms overlap with those of other neurodegenerative diseases such as Alzheimer's and Parkinson's disease. Diagnosis is based on a combination of :
- The patient's medical history and symptoms.
- A detailed neurological clinical examination.
- Complementary examinations such as :
o Magnetic resonance imaging (MRI): to assess the structure of the brain and rule out other possible causes.
o Positron emission tomography (PET): to visualise protein deposits in the brain.
o Biological tests: to rule out other possible causes.
What is the treatment for Lewy body disease?
There is currently no cure for Lewy body disease. However, treatments can help to relieve certain symptoms and improve the patient's quality of life. Treatments are often tailored to each individual and may include:
- Medication to treat motor symptoms (such as levodopa for movement disorders) or cognitive problems (such as cholinesterase inhibitors).
- Psychological treatment to help patients and their families cope with the disease.
- Non-drug therapies such as physiotherapy, occupational therapy and speech therapy to maintain functional abilities.
Go further and contact
#dementia#neurodegenerative disease#alpha-synuclein#Lewy bodies#hallucinations#movement disorders#sleep disorders#diagnosis#treatment#quality of life
0 notes
Text
It's so frustrating that multiple of my majorly pressing physical issues in life no longer meet diagnostic criteria due to preventative drug use (thanks to years of trial and error and finally having one decent doctor) and lifestyle changes. Like yeah I have regained "use" of my right hand so long as I don't use it too much. This is not indicative of an underlying and disabling neuropathy or impingement of the nerve. Yes I can breathe and "only" break out in rashes when I'm overheated or touching something I shouldnt or angry due to being on 4 separate allergy medications, singulair, and having a rescue inhaler I take throughout the day. As opposed to all the time for no reason. This is not indicative of mast cell activation disorder. Yes I can fall asleep at a reasonable time if I drug myself hard enough and force myself out of bed the next day but this results in fatigue that only goes away when I get 10+ hours of sleep during or partially during the daytime. This is surely not indicative of a sleep cycle disorder.
#it drives me CRAZYYY bc yes my symptoms are partially managed so its like is it worth pursuing when pursuit would mean reverting to a state#wherein they are not managed in order to undergo diagnostic testing#how could i ever know if thats worth it? is there anything more doctors could be doing for me than im already doing? is the documentation#worth it?#for pots it absolutely was... but it was a years long fight i just dont know if i have it in me#its also fucking infuriating bc my pots doctor told me i have mcas but she cant make the diagnosis. my psychiatrist told me i have a#circadian rhythm disorder. but cant make the diagnosis#and finally my pcp told me i have a nerve impingement. but again. cant diagnose it#and with the exception of maybe my hand no doctor will see me bc my symptoms are no longer clinically significant despite causing daily pain#and disrupting my day#AFTER i do all the treatments and lifestyle changes#bc it reduces it all just enough to not show up in diagnostic testing#losing it at 1am over this shit once again#i need to sleep but im all drugged up and not the least bit tired#and also everything hurts and im having asthma symptoms#what the fuck else is new
1 note
·
View note
Text

Solve Your Sleep Problems with the help of meditation
Good sleep is essential for our overall well-being. Poor sleep habits, such as irregular sleep schedules and excessive caffeine or alcohol consumption, can lead to sleep disorders. Discover effective sleep problem solutions to improve your sleep quality and overall health.
#sleep problems solutions#sleep disorders treatment#sleep disorders types#sleep disorders symptoms#sleep disorders test#sleep insomnia meditation#sleep problems during pregnancy#sleep disorders diagnosis#causes of sleep disorders
0 notes
Text
common myths about migraines (AKA if you get headaches regularly, please seek treatment for migraines)
"i don't have migraines because while i get them several times a week, it's only when i am hungry or dehydrated."
those are probably migraines. thirst, hunger, sleep disturbances, or any disruption to routine are common migraine triggers.
"my headaches are specifically barometric related, i get them when the weather/altitude changes."
those are probably migraines. barometric pressure is a common migraine trigger.
"i get headaches all the time but ibuprofen gets rid of them so they can't be migraines."
that's not true. ibuprofen works great at relieving migraine pain for many people.
"my consistent headaches are tension headaches. i feel them originate in my neck/shoulders."
those are probably migraines. muscle tension is a common migraine trigger.
if you are regularly getting headaches (once a week or more), you are likely getting migraines. in fact, a good rule of thumb if you're consistently getting headaches is to treat them as migraines until you can rule out migraines. that's how common "chronic headache = migraine" actually is.
migraines are a neurological disorder wherein pain is one symptom. pain is often the MAIN symptom, and the most noticeable symptom, which can make diagnosis tricky. other symptoms of migraine include:
fatigue
nausea/vomiting
digestive issues
visual disturbances (auras)
sensitivity to light and/or sound
mood changes
brain fog/cognitive changes
ringing in the ears
dizziness/vertigo
numbness/weakness on one side of the body
this list is NOT complete, but is a starting point. i really like the comparison to a hangover. if you generally feel hungover when you get a headache (without having consumed alcohol), that's a classic migraine presentation.
so many people suffer from migraine and don't even know it, so they aren't able to advocate for themselves to get treatment. there are great new migraine treatments on the market! if you're able, please seek treatment for your migraines. a better quality of life is possible.
19K notes
·
View notes
Text
MİDHEALT - PLATİN (2)

Unlocking Wellness: Explore a World of Health Tips, Vegan Meal Prep Ideas, and Insights on Medical Treatments at Midhealth
In the quest for optimal health and well-being, access to reliable information and resources is paramount. At Midhealth, we strive to be your trusted companion on your journey to wellness, offering a wealth of knowledge on health tips, vegan meal prep, medical treatments like ketamine therapy, and even insights into specific health conditions such as Cushing's disease in cats.
Health Tips:
Midhealth is your go-to source for valuable health tips to help you lead a balanced and fulfilling life. From nutrition advice to exercise recommendations, stress management techniques to sleep optimization strategies, our platform provides practical insights to support your overall well-being. Whether you're looking to boost your immune system, improve your mental health, or enhance your energy levels, Midhealth has you covered with evidence-based tips and guidance.
Vegan Meal Prep Meals:
For those embracing a plant-based lifestyle, Midhealth offers a treasure trove of vegan meal prep meals ideas to inspire your culinary journey. Discover delicious and nutritious recipes crafted by our team of experts, designed to nourish your body and tantalize your taste buds. From vibrant salads to hearty stews, wholesome bowls to decadent desserts, our vegan meals prep meals make it easy to enjoy flavorful and satisfying dishes while prioritizing your health and the planet.
Ketamine Treatment Cost:
Exploring innovative medical treatments? Midhealth provides insights into the cost of ketamine therapy cost, a promising option for individuals struggling with treatment-resistant depression, chronic pain, PTSD, and other mental health conditions. Our comprehensive information helps you understand the potential benefits, risks, and financial considerations associated with ketamine treatment, empowering you to make informed decisions about your health care journey.
Cushing's Disease in Cats:
Pet owners seeking information on specific health conditions will find valuable resources at Midhealth, including insights into Cushing's disease in cats. Learn about the causes, symptoms, diagnosis, and treatment options for this hormonal disorder, enabling you to provide the best possible care for your feline companion.
In essence, Midhealth is your virtual wellness hub, offering a diverse array of health tips, vegan meal prep inspiration, insights into medical treatments, and resources on various health conditions. Whether you're embarking on a journey to better health for yourself or seeking guidance for your furry friend, Midhealth is here to support you every step of the way. Explore our platform today and unlock a world of wellness possibilities!
556 notes
·
View notes
Text
One Day At A Time (Part 6/?)
Jake "Hangman" Seresin x reader
Summary: Hangman's fiancée is hospitalised and Jake waits for her to wake up
T/W: Anxiety, panic disorder, PTSD, POW, hints to torture, SA, abortion, pregnancy references, death
A/N: Sorry this got so much darker than I was expecting... Also as per I haven't proof read so ignore the grammar
Part 5 in case you missed it

Jake POV -
Jake wakes up stomach rumbling with a dead arm from clutching your hand as he sleeps. He momentarily breaks your hand hold to move his arm a bit, hoping to regain some feeling.
A consultant walks in smiling slightly at Jake as they make eye contact through the glass of the door.
"Morning." the doctor says walking in.
"Any news today?" Jake responds hopeful that you'll be coherent enough to talk to him soon.
The man proceeds to walk Jake through all of your bigger injuries - you arm and several ribs are broken; your ankle is sprained; they've operated on your shoulder to make sure it heals correctly. No haemorrhage from hitting your head but you might have a mild concussion.
"There's one other thing as well." The doctor says meeting Jake's gaze.
"I don't like that look doc, what is it?" Jake's nerves skyrocket from the doctor's obvious hesitation.
All of the colour in Jake's face drains as the doctor starts explaining to him what an ectopic pregnancy is. He shudders in repulsion as the doctor says the same thing in a slightly different way in an effort to fully express that it's not viable.
He cuts the doctor off when they start talking about treatment options. "I-I-I just need a minute." Jake says tears filling his eyes. "It's not about the abortion. I just need a minute to process that someone's done that too my Y/N." Jake tries to explain that this isn't a pro-life meltdown.
He doesn't see the doctor nod but he hears the man leave.
The second the door shuts Jake lets out a loud sob at the glimpse of what the last few years have looked like for you. He hunches over stomach clenching from worry - he knows that the minute you find that out that particular diagnosis, you're going to freak out.
Jake continues to cry he thinks back to the only other time you've been pregnant. The time that it was his kid and there were complications. Whatever bastard did this to you is going to unknowingly force you to relive that day.
Jake fruitlessly wipes his eyes on the sleeve of his hoodie then turns back to you face still wet from the tears silently falling down his cheeks. "This changes nothing with you and me sweets. I will be here every step of the way if you want me to." Jake says kissing your hand.
Having gone through a million emotions in the span of a few minutes Jake needs to step out of the room to try and let go of his rage.
*
Reader POV -
Every muscle In your body is tense in the knowledge that someone was nearby when you were trying to wake up earlier.
Wires and tubing press uncomfortably against your back. Why would they lie you over them that seems stupid?
You lie there controlling your breathing, eyes shut tightly just listening for signs of someone else.
I really don't want to open my eyes in case I'm not alone.
It's eerily quiet. All you can hear is the faint buzzing of tinnitus in your ears and a machine steadily beeping.
Okay, no one else is here, you tell yourself before gently opening your eyes. You scan the otherwise empty hospital room frowning in confusion. You're not sure whether someone was next to you or whether you dreamt that someone was in the vacant chair by your side?
There's fresh flowers and a card on the windowsill, so someone has been here.
A male nurse walks in as you try to disconnect from the machines behind you.
"Please don't do that! You're in the hospital." He says to you.
God my head is pounding.
"I got out?" you murmur in response, so drained that even talking is more of an effort than it has been recently.
"Yes you got out. You're okay." He confirms.
You nod slightly in recognition of what he just said, but mentally you completely disagree that you're okay right now.
"How's the pain on a scale from one to ten?" He questions.
Groaning in pain you shift slightly, you don't verbalise the feeling that you can only imagine is similar to being hit by a bus. Instead you ask "Can I self discharge?"
"It would be strongly against our medical advice if you were to self discharge right now. I would recommend that you stay here under observation and on the IV for a few more days." He grimaces at the prospect of you leaving this room.
"I'm not staying here." You exclaim, wincing slightly as you rip out a needle from your arm.
"Let me just go get a consultant to talk everything through with you and if you still want to leave after that, then you can." The nurse says hesitantly before jogging out of the room. I think he must be new to the role.
The door to your room opens and you suddenly understand the nurse's hesitancy as two police officers walk in.
You try to dart into an upright position to be more alert but whimper at your body's reluctance to move. The agony radiating from your left arm is unbearable. I can't imagine what sitting up would've felt like if that hadn't put my arm in this sling.
"Oh great you're awake!" The young police lady says standing pencil straight by the side of your bed ready to start questioning you.
"You're in the hospital, do you know what happened?" The guy questions you.
"What happened to Ghost?" You begin your own interrogation for answers.
"High on painkillers?" The female officer turns to the man who shakes his head.
"Was that your back seaters callsign?" He queries.
"Yeah. Is h-h-" You nod but you're cut off by the officer.
"It was instant. He wouldn't have felt anything." He answers without making you ask.
You cover your eyes with the palms of your hands fighting to regain a semblance of composure at how abysmal that news makes you feel.
The anxious ringing in your head eventually subsides and you remove your hands from your face. You're somehow still surprised to see that the officers stayed for however long it took for you to be able to fake okay.
"I need to go home." you admit quietly more to yourself than to them. You don't articulate that you just want to blanket cocoon on your sofa while Jake silently assures you that everything is going to be fine.
Your hands quiver slightly at the reality that he might not have waited for you; your home might not even be your home anymore.
Thoughts torrent your mind before you finally muster the courage to ask the room what date it is.
"April the 8th" The police lady answers.
"W-w-what year is it?" You speak up. The police man standing silently in the doorway looks horrified at the prospect that you might not know that but he interjects and answers you anyway.
"Shit." You respond in momentary disbelief that it's been that long.
I mean it felt like forever but I had convinced myself it had been a couple of months and i'll go home to everything the same.
"Jake thinks I've been dead for four years?" tears flood your eyes and your voice breaks, for the first time in years it's not from disuse.
How the fuck am I meant to go home after that amount of time?
If he hasn't moved onto someone else, surely he would've at least mourned you. If he's said goodbye to you like that how is it fair to suddenly reappear?
None of this is fucking fair.
Ghost should be here too.
*
Jake POV
Jake's heart drops to the floor as he carefully opens your room door to reveal an empty bed. From the haphazard sheets and wires flung across the room, he knows that no one has taken you into surgery without consulting him.
You're still in fight or flight mode.
He discards his unopened sandwich on the table and runs to the nurse's station.
"Room 26 - where is she?" Jake asks the guy behind the desk.
"She asked to self discharge; she's gone." he shrugs.
"She's gone?" Jake clarifies.
"Yep. If you can convince her to come back to hospital I think that would be in her best interest." He responds.
Five minutes - I was gone for five fucking minutes. Jake flings himself down the stairs, running at full speed to the exit.
He forces himself to stop when he's out of the hospital. He glances over everyone in the immediate vicinity.
You have to be here somewhere. And yet you're not here.
Where on earth would you go?
After all this time would you go home?
Home is fucking miles away - how would you get there with no phone and no money?
Jake's heart pounds in his chest as he walks to his car. He walks at a snail's pace so that he can check everyone that crosses his path isn't you.
I'll find you. I promise I'll find you.
Part 7
Masterlist
Tags:
@inthestars-underthesun
@rainy-darling
@emma8895eb
@tgmreader
@ems-alexandra
@djs8891
@els-marvelvsp
@lets-turn-and-burn
#jake seresin#tgm#top gun#jake hangman seresin#jake hangman fic#hangman imagine#hangman x reader#hangman angst#top gun au#top gun x reader#top gun hangman#hangman#top gun fic#top gun maverick#tgm fic#tgm x reader#tgm au#jake x reader#top gun imagine#tgm imagine#hangman fanfiction#hangman seresin
184 notes
·
View notes
Text

My PMDD hell: why I went abroad to have my ovaries removed (Sarah Gillespie, The Times, Nov 27 2024)
"For six years, from my late twenties, I have lived with a condition called premenstrual dysphoric disorder, or PMDD.
Due to a genetic quirk, I have a brain sensitivity that makes my body intolerant to its own hormonal changes.
Instead of becoming moody and irritable, as with PMS, I become catatonic and racked with pain.
Dysphoria blooms in my brain, making me depressed and paranoid. I binge on carbohydrates, needing 3,000 calories a day just to function.
This happens for 7-14 days every month, during the latter half of my menstrual cycle, as hormone levels plummet.
On the third day of my period, the fog lifts and I feel normal again. But relief is soon replaced by dread as I survey the destruction.
There are relationships to repair, overdue bills to pay and excess pounds to lose.
It is the life of Sisyphus: every month, I roll the boulder up the mountain only for it to roll down again. (…)
PMDD is surprisingly common and, according to World Health Organisation data, affects 5.5 per cent of women of child-bearing age — about 824,000 women in the UK.
Of these, more than a third have attempted suicide. Yet hardly anyone’s heard of it.
No one knows the cause, either, though scientists generally agree that it’s genetic — hence why psychological therapies can’t fully fix it.
It was only in 2019 that the WHO added PMDD to its international classification of diseases and related health problems (ICD-11), legitimising it as a medical diagnosis (though there are still medical professionals who dispute its existence). (…)
After diagnosis, women with PMDD are put onto a ladder of treatments ranked from least to most invasive.
But as the body ages and hormones become more erratic, PMDD gets progressively worse.
So even when I found a rung on the ladder that worked, I never got to rest there for long.
First, there were lifestyle changes: diet, weight training, high-intensity interval training (HIIT).
Then supplements: chasteberry, evening primrose, magnesium, calcium, L-tryptophan, vitamin B6. Then antidepressants: fluoxetine, sertraline, citalopram.
Then contraceptives: Evra, Yasmin, Eloine. Finally, there was HRT: Utrogestan, Estradot, Estraderm.
I climbed that ladder for five years. Only HIIT and fluoxetine worked, for about nine months each; the rest worked for two months, if at all. (…)
After all this, only one rung was left on the ladder — one with a 96 per cent satisfaction rate, the closest thing to a cure.
This last-resort treatment is a bilateral salpingo oophorectomy: the surgical removal of both ovaries and fallopian tubes.
Upon their removal, all hormone fluctuations would stop, my hormone levels would drop to almost zero and I would enter menopause.
I would need to take hormone replacement therapy (HRT) until my fifties or risk the early onset of osteoporosis, heart disease and dementia. It would also make me infertile. (…)
Getting approved for surgery on the NHS requires a trial period in a reversible “chemical” menopause: monthly injections that would shut down my ovaries, end my suffering and “prove” that I had PMDD.
That was the idea, anyway. Instead, the injections threw my hormones into chaos, resulting in a PMDD episode that lasted for 11 months.
Deprived of even the monthly breaks in my symptoms, I languished in bed.
My attention shattered; I spent countless days scrolling my phone. I gulped down painkillers and sleeping pills like Skittles.
My finances were collapsing. I gained more than two stone in weight.
“It should be working by now,” the gynaecologist said after three months. “Have you tried eating more vegetables?”
The next gynaecologist was no better. “If it hasn’t worked, that suggests it’s not PMDD,” she said. “I should probably refer you to a psychiatrist.”
After months of my pleading, she agreed to write to the surgeon. But her letter was an act of sabotage.
“Sarah has diagnosed herself with PMDD,” she wrote, ignoring my GP’s diagnosis.
“She is on many help groups and accessing a lot of support from other PMDD sufferers online.” In other words: “This hypochondriac is spending too much time on the internet.”
Yes, I was on the internet, but I wasn’t talking to help groups any more.
Instead I’d been digging into scientific papers to find studies on chemical menopause.
Eventually, I found one — a meta-analysis of five clinical trials published in the Journal of Clinical Psychiatry.
It stated that chemical menopause treats PMDD in “upwards of 70 per cent” of cases — but not 100 per cent, as the NHS doctors had said.
The International Association for Premenstrual Disorders (IAPMD) backs this up.
On its page on chemical menopause it says, “In rare cases [chemical menopause] does not fully suppress the cycle and there are breakthrough symptoms… If this was the case, you may still respond well to surgical menopause.”
Two months later, I was in Lithuania. Feeling desperate and unable to afford the £10,000 it would cost for private surgery in the UK, I had googled “gynaecology surgery Europe”.
This led me to Nordclinic in Kaunas, which treats about 2,000 British patients annually.
I sent my medical records to the surgeon, who agreed to perform the surgery. (…)
Though it’s early days, I still can’t believe how well I feel. My future unfurls before me without interruption.
I have so much time: time to write, to see friends and family, to travel, go on dates, paint and sing and read and run.
Time to cook, as I can now handle knives without fear. Time to sit and do nothing and burst out laughing from sheer wonder — for life without PMDD is so, so wonderful and I will forever be grateful for it.
That said, I still need to reckon with all the time taken from me over the past six years.
My trust in our healthcare system is broken and will probably never be restored.
I need to kick away the crutches — food, phone, pills, alcohol — that have held me up and rediscover better ways to cope.
But this time, I don’t need to keep starting again and again and again every month.
Yes, the scars are still red and raw. But by next summer, they’ll be gone."
35 notes
·
View notes
Text
Distinguishing between bipolar disorder (BD) and borderline personality disorder (BPD) can be challenging, as there is some overlap in symptoms, but they are distinct conditions. Here are some key differences and similarities that can help:
Bipolar Disorder (BD)
• Core Features: The primary feature of bipolar disorder is extreme mood swings, including mania or hypomania (elevated or irritable mood, impulsivity, energy, and grandiosity) and depression (low mood, fatigue, loss of interest, feelings of hopelessness).
• Mood Episodes: In bipolar disorder, the manic or hypomanic episodes can last for days, weeks, or longer, while depressive episodes also last for a significant period. The mood swings typically occur in discrete episodes (e.g., you may feel normal between them).
• Mania Symptoms: During a manic episode, people may experience a drastically elevated mood, excessive energy, rapid speech, impulsive behavior (e.g., spending sprees, risky sexual behavior), and decreased need for sleep.
• Depression Symptoms: In depressive episodes, people may experience feelings of deep sadness, hopelessness, fatigue, changes in appetite or sleep patterns, and suicidal thoughts.
• Mood Shifts: The mood shifts in BD tend to follow a more cyclical pattern and can last for extended periods (weeks to months).
Borderline Personality Disorder (BPD)
• Core Features: BPD is primarily characterized by instability in relationships, self-image, and emotions. People with BPD often experience intense emotional reactions, fear of abandonment, and difficulty managing interpersonal relationships.
• Emotional Instability: In BPD, emotional reactions are often intense and short-lived (hours to a few days) rather than the prolonged episodes seen in bipolar disorder. This may manifest as sudden mood swings based on external events (e.g., feeling elated one moment, deeply rejected the next).
• Fear of Abandonment: One of the hallmark features of BPD is a fear of abandonment, which can lead to frantic efforts to avoid real or imagined abandonment.
• Self-image Issues: People with BPD often have a fluctuating or unstable sense of self, and may experience sudden shifts in how they view themselves.
• Impulsivity and Risky Behaviors: Like bipolar disorder, BPD can involve impulsive behavior, but these impulsive acts are often driven by emotional distress, such as self-harming, substance abuse, or risky sexual behaviors.
• Chronic Feelings of Emptiness: People with BPD often report feeling empty or like something is missing.
Key Differences
• Mood Swings: BD involves more distinct mood episodes (mania and depression), while BPD involves rapid, intense mood swings often triggered by external events.
• Duration of Symptoms: In BD, mood swings (mania or depression) last for a longer period (days to weeks), whereas in BPD, emotional reactions are more transient and may shift within hours.
• Focus of Emotional Reactions: In BPD, emotional reactions are typically more tied to interpersonal issues (e.g., abandonment fears), whereas in BD, mood swings are more related to the underlying mood state (mania or depression).
Overlap
• Both disorders can involve impulsivity, irritability, and risky behaviors.
• Both may have periods of depression, although the depressive symptoms tend to be more persistent in BD and more reactive in BPD.
Diagnosis
A mental health professional (psychiatrist or psychologist) is essential for a proper diagnosis, as these conditions can look similar. The assessment will include:
• Clinical Interview: Discussing your personal history, symptoms, and patterns of mood.
• Assessment Tools: Questionnaires or structured interviews to assess the symptoms more thoroughly.
• Duration and Impact: Understanding how long the symptoms have been occurring and how they impact your daily life.
Treatment
Both conditions are treatable, but the approaches differ:
• Bipolar Disorder: Treatment often includes mood stabilizers, antidepressants (carefully managed), and sometimes antipsychotic medications. Psychotherapy, such as cognitive-behavioral therapy (CBT) or interpersonal therapy (IPT), can help manage symptoms.
• Borderline Personality Disorder: Dialectical behavior therapy (DBT) is a specialized form of therapy that is particularly effective for BPD, focusing on skills for emotional regulation, interpersonal effectiveness, and distress tolerance.
If you’re concerned about your symptoms, it’s crucial to seek professional help. Proper diagnosis and treatment can significantly improve quality of life.
#bipolar disorder#borderline personality disorder#actually bpd#mental illness#mentally exhausted#bpd thoughts#bpd blog#bpd problems#bpd stuff#bpd#bipolor#bipolar 2#bipolar 1
35 notes
·
View notes
Text
Well, this is awkward.
Results
TGD [transgender and gender diverse] adolescents and 6,603 cisgender siblings were included. TGD adolescents were more likely to have a mental health diagnosis (OR 5.45, 95% CI [4.77–6.24]), use more mental healthcare services (IRR 2.22; 95% CI [2.00–2.46]), and be prescribed more psychotropic medications (IRR = 2.57; 95% CI [2.36–2.80]) compared to siblings. The most pronounced increases in mental healthcare were for adjustment, anxiety, mood, personality, psychotic disorders, and suicidal ideation/attempted suicide. The most pronounced increased in psychotropic medication were in SNRIs, sleep medications, anti-psychotics and lithium. Among 963 TGD youth (Mage: 18.2) using gender-affirming pharmaceuticals, mental healthcare did not significantly change (IRR = 1.09, 95% CI [0.95–1.25]) and psychotropic medications increased (IRR = 1.67, 95% CI [1.46–1.91]) following gender-affirming pharmaceutical initiation; older age was associated with decreased care and prescriptions."
#gender identity#transgender#lgbtq#lgbt#trans#protect trans kids#nonbinary#enby#nb#trans research#gender affirming care
29 notes
·
View notes
Text
Drs. Ziyad Al-Aly, Akiko Iwasaki and Eric Topol, along with other acclaimed researchers, have issued a position statement on Long COVID published yesterday in the journal Nature Medicine. This document provides a much-needed perspective on the continued dangers posed by the “forever COVID” policy enshrined in official public health policies.
This important review comes on the heels of the recent publication in the New England Journal of Medicine (NEJM) of a reference frame for the chronic disease. It was developed by the National Academies of Sciences, Engineering, and Medicine (NASEM) Committee on Examining the Working Definition for Long COVID.
The 2024 NASEM Long COVID definition is: “Long COVID is an infection-associated chronic condition that occurs after SARS-CoV-2 infection and is present for at least 3 months as a continuous, relapsing and remitting, or progressive disease state that affects one or more organ systems.”
Most importantly, previous documentation of a COVID infection is not required for the diagnosis. The NASEM report explains: “By now, most persons worldwide have had at least one episode of acute SARS-CoV-2 infection. A requirement for proof of diagnosis could wrongly exclude many patients …”
This closer approximation to a scientific definition of long COVID is an important step towards educating the public and issuing a call for action to address the viral assault on the global population.
The authors of the study, published in Nature Medicine, should be commended for giving urgency to an issue that Dr. Al-Aly has rightly called “the elephant in the room.” Yet as sincere as these appeals may be to take Long COVID seriously, they will not convince the bourgeois authorities who have already dismissed warnings about the acute stage of COVID-19.
The complex multisystem disorder that can affect nearly every organ system after a COVID infection spares no one across the age spectrum. It appears that even fetuses in utero are at increased risk of respiratory ailments if the mother was infected during pregnancy.
Considering our rapidly developing comprehension of the long-term health consequences of COVID, thanks to the exemplary work being done by these scientists, the policy of mass infection demanded by the financial oligarchy assumes an even more sinister and deranged character.
The “cardinal” symptoms of Long COVID include brain fog and memory changes, fatigue, rapid sudden onset of heart rate, significant sleep disturbances, and immense sense of discomfort and illness after exerting oneself. There are no cures and, worse, no diagnostic tools that can tell someone they have Long COVID. Only recently have healthcare workers and researchers begun to identify treatments for Long COVID, but there is an absence of randomized trials to guide these decisions.
The authors note, “Care for people with Long COVID varies widely across settings and practitioners. It is often challenged by lack of widespread recognition and understanding of Long COVID among medical professionals, constrained resources and competing demands on healthcare systems still recovering from the shock of the pandemic, lack of standardized care pathways, lack of definitive diagnostic and treatment tools, and a general pervasive pandemic fatigue with an urge to ‘move on.’” The last point is a byproduct of the impact of forcing the population to accept COVID as a permanent fixture of society.
On top of the horrific impact it has on an individual person, on a social scale, mass Long COVID leads to loss of productivity, disruption in the workplace and increased risk of occupational-related injury or fatalities. Cognitive impairment, even after mild infections, is common, and there can be dire consequences for workers in occupations where the slightest error or inattention can be devastating: truck drivers, electricians, airline pilots, first responders and more. To say nothing of the impact on the wider community.
The report makes reference to the 2022 US Brookings Institute estimates on the figure of 2 million to 4 million US adults who were out of work because of Long COVID. Add to this the Minneapolis US Federal Reserve Bank report from July 2022, finding that people with Long COVID had a 10 percent poorer chance of being employed, and when they were, worked 25 to 50 percent less than uninfected individuals.
On a global scale, the authors wrote, “On the basis of all the available data, a conservative estimate of the annual global economic toll of Long COVID could be around $1 trillion, amounting to 1% of the 2024 global GDP.” Other estimates are even higher: An economic study from 2022 placed the cost of Long COVID at $3.7 trillion, or $11,000 per capita for the US alone, amounting to 17 percent of the gross domestic product (GDP).
Most compelling in the Al-Aly et al. review was their assessment of the global cumulative incidence of Long COVID, which until now had been opaque.
Basing their estimates on meta-regression studies that pooled all the available evidence, they estimated that figure for the first four years of the pandemic at 409 million cases of Long COVID. The authors remarked, “It is crucial to emphasize that these estimates only represent cases arising from symptomatic infections and are likely to be conservative. The actual incidence of Long COVID, including cases from asymptomatic infections or those with a broader range of symptoms, is expected to be higher.”
By comparison, among the most common ailments afflicting the world’s population, heart and circulatory issues, affect around 620 million. This means that in only four years, Long COVID, as a disease, has risen nearly to the top of the global list. Furthermore, Long COVID, as a multi-organ disease process, will only exacerbate noncommunicable and communicable diseases that arise in the future.
Placing these figures into context, this week, based on wastewater data, infection modelers estimate that COVID infections have once again climbed above 1 million cases per day, a staggering figure, to which the CDC is completely indifferent. COVID modeler Dr. Mike Hoerger of the Pandemic Mitigation Collaborative, in a social media discussion with this writer, said that presently, on average, every American has been infected between three or four times.
In a rare show of concern, the World Health Organization (WHO) announced that COVID-19 was spreading across the globe, with positivity rates in Europe above 20 percent. In opening their August 6, 2024, news report on COVID, they warned, “The UN health agency is also concerned that more severe variants of the coronavirus may soon be on the horizon.”
The European continent is swimming in a river of infection, like the unfortunate Olympic athletes sickened by swimming in the polluted Seine. And as we have already noted, the Olympics themselves have been a superspreader event.
Knowing that reinfections, more severe disease, and remaining unvaccinated, all raise the risk of Long COVID, one can only watch the current wave of infections with alarm. These will be given further fuel as schools and universities begin to open their doors later this month. Furthermore, global COVID vaccinations have essentially come to a halt. Long COVID is the long tail of the ongoing pandemic that has no end.
Unique in the report by Dr. Al-Aly and colleagues is the raising of social issues affecting the global impact of Long COVID. In support of the UN Foundation’s Sustainable Development Goals (SDG), they raise the need to end poverty and hunger, improve access to health, provide quality education, improve working conditions and reduce inequalities. They also call for funding to support coordinated interdisciplinary research on Long COVID on a global footing.
The recognition of the social issues that need to be addressed is an important insight. However, the appeal to existing public health institutions and political processes to heed their warnings will not bear any fruit.
First and foremost, the “forever COVID” policy is not a misguided public health construct. It is a calculated and coordinated approach to ensure pandemic threats would not impede the unfettered accumulation of surplus value off the backs of the working class. If the sick and infirm fall by the wayside, these social losses are seen as financial gains by the class that seeks to extract from the working class every minute of their potential labor power and avoid the cost of their “lingering on.”
In this regard, Senator Bernie Sanders’ introduction of legislation titled the “Long COVID Research Moonshot Act of 2024” is simply political theater, aimed at deluding the public into thinking that the capitalist system is capable of reform. The bill would provide a paltry $1 billion in mandatory funding per year for 10 years to the National Institutes of Health (NIH) to support Long COVID research.
To think this legislation will see the light of day while social spending is being slashed to fund the forever wars is to look at the world through very thick rose-colored glasses. Those researchers and public health advocates who wish to promote the application of the scientific principles that guide their own work must recognize the necessity for a broader social perspective.
To address Long COVID, as the world Trotskyist movement has demanded, one must begin by eliminating COVID across the world. Despite the dismissal of such a perspective by capitalist governments and the corporate media, zero COVID is and remains the only viable solution.
Only one social class is capable of taking up and fighting for such a policy: the international working class. The fight against COVID and future pandemics, like the looming H5N1, must be integrated into the revolutionary mobilization of the working class against the capitalist system and the establishment of a socialist society, in which human needs, including the most basic concerns of healthy life, will be the basis of social policy, not private profit.
#long covid#covid#mask up#pandemic#covid 19#wear a mask#sars cov 2#coronavirus#still coviding#public health#wear a respirator
32 notes
·
View notes
Note
is it ever explained anywhere in the kagepro media what is Haruka's condition? tried to look into the kagepro fanwiki what it was but it just says "[...] implied to be cardiovascular". You got any clue?
SORRY FOR THE SUPER LATE ANSWER i have been Crazy busy and Crazy going through it. hope it's still helpful!
anyway!!! neither haruka or takane's conditions are outright stated, and are only mentioned as a heart disease and a sleeping disorder. even haruka and takane themselves don't know much about each other's diagnosis, and seem to know the basics of it. i always liked this detail because it's like they didn't want to ask each other too much about it, since they know what it's like to be constantly interrogated about it.
yaaay ill talk about takane even if u didnt ask but i promise its to make a point
with takane, the general consensus is that she's got specifically narcolepsy, because her symptoms are described with enough details that narrow it down to what it could be. she randomly falls asleep, and is extremely tired/sleepy all the time. when she dies... supposedly kenjirou had... poisoned her? but that's not stated anywhere im pretty sure it was just a popular headcanon (im so lazy to go check gang sorry. but i am pretty sure it's not mentioned also when tf would he have done that) however takane was extremely accelerated from running and her epiphany, and as soon as she falls she says "no way im having an episode rn" like she immediately knew what was happening, so it seems like cataplexy is also something she experiences. basically narcolepsy is... like spot on described and shown.
instead, for haruka its much less clear. like you said, he's only described to have a heart disease that's very serious and sends him into cardiac arrest erm kind of often, and it's also genetic because his mom had it and died from it. that's... it! there's never been popular headcanons on what it could be. unlike a sleeping disorder, a heart disease can be caused by a million different things and still have the same result (heart attacks). meanwhile sleeping disorders are a little bit more specific so takane's is easier to deduce.
haruka's illness could be many things, but my personal headcanon has always been arrhythmia. to be honest i decided on this hc as a teen bc it was the only heart disease i knew at the time so i kinda ran with it LOL but ive done some more reading later on (not extensive studies of it... just random google searches) and ive still landed on arrhythmia being my headcanon because it's also genetic, and there are different types of arrythmia, some being really really scary... not that arrhythmia in itself isnt scary tbh. its the irregular beating of the heart, so a heart attack can literally happen any moment!! scary as hell. but that's also why i think it's fitting, like even a sneeze could make haruka jumpcut scene to an ambulance.
these are some old hcs of mine but a more recent one is haruka getting treatments and surgeries post str. despite awakening eyes keeps haruka alive, it doesn't Cure him, but makes him strong enough to stand these treatments he wasnt suitable for before, increasing his lifespan. so even if awakening eyes doesnt cure him, it definitely helps him live.
so post str haruka is still very much a regular patient to the hospital and both him and takane continue to be medicated for life
21 notes
·
View notes
Note
Cracks open an oyster shell to reveal a slimy half baked fetus esque Dutch van def linde inside
Do you think this sick little freak of nature is neurodivergent… or has any other disorders.. npd… bpd… etc… (no pressure to like. Actually diagnose or anything I’m assuming you aren’t a licensed psychologist, more for character analysis. Thank you so much, love your work!)
Oh he definately has something but yes I am not a psychologist and my experience with ND is limited to autism, ADHD, OCD and dyslexia because those are my family heirlooms, thus I would not feel comfortable diagnosing him but what I can do is present what fits and what does not fit about the most common diagnosises that people put on him as well as pointing out things others with more experience with these diagnosises says.
NPD- Narcissism
Dutch believes himself to be superior to others, which is very visible in many different ways, like his tent being the most luxurious to not allowing Molly, his girl to work. Which is also a big part of his entitlement, he expects others to look up to him, he expects people to treat him well, to cater his every need, and he gets angry when people doesn't.
He lives on admiration, which can be why he leans so heavily over to Micah late game when everyone else pulls their attention away from him, causing him to get angry. This time he is also very unable to handle any critisism thrown his way, reacting aggressively to it rather than listening.
One of the most obvious signs that makes people think narcissism is his willingness to exploit other, from the gang memebers to the native americans, using everything to his own advandage. He even says it himself, he is helping the natives because it helps him.
He created that friendship with Eagle Flies beacuse it boosted his confidence and his image, he lived in Micah's friendship because it fed his confidence and his image.
Narcissists tend to lack empathy and he does state in a camp event with Susan and Arthur "did you hear that Arthur? I am meant to consider feelings now!" and he is also quite arrogant, talking down to Arthur when he tries to come up with a plan in chapter 6.
Now, that said, narcissists cannot form meaning bonds which Dutch has done several times, for example with Hosea and with The Count. They are actually known for being terrible animal owners and are known for being able to fake friendships for a short amount of time while using others, not for thirty years.
Narcissits are also prone to bragging, which we do not hear Dutch nor does he belittle other people's achievements, and while he can seem like he doesn't show feelings and empathy, he does. He is genuiently sorry when Arthur gets kidnapped by O'Driscolls, he is sad when Hosea dies, he listens to John when Jack is kidnapped.
I also would not say he is fishing for compliments, which they are known for, there are also requirements for narcisissm which we don't have enough information on, such as fragile ego and requent self-doubt.
Bipolar
Dutch in the beginning of rdr2 is a very regular dude, he has signs but he seems okay, but as time goes on, especially in chapter 4-6 we see him go up into something that can look like mania.
He does not sleep, he can work without rest. He is easily irritated, his self-esteem is through the roog and he is impulsive. He constantly obesses, he leans over to people who feeds his ego, he is paranoid and he has a lot of grandiosity.
In the first couple of chapters it does also seem like we have some episodes. After settling in Horseshoe Dutch says sorry to Hosea about Blackwater, that he made a fool of himself and doesn't know what happened, similarly with after Arthurs kidnapping.
But then we come to chapter 5-6. What does not fit here however is the fact we don't see a crash, mania cannot go on forever and yet through the months of chap 5-6 there is no crash, he does not return to his regular state. We also see the same things in rdr1, again, no crash and it has been years.
"That said, I've yet to see his crash. The mania, which separates bipolar from major depression, can't just go on forever." which was wisely said by a player diagnosed with bipolar.
Borderline personality disorder
Dutch has a very strong fear of being abanonded, he does not like others leaving him, thus he is willing to leave them first, such as leaving John in jail before allowing him to get out and leave him.
He has a lot of paranoia and looses touch with reality, such as the situation in which he is standing, but also randomly yelling out or talking to himself in chapter 6, similarly he is prone to impulsiveness, doing things that aren't exactly thought through which ends people being harmed.
While he doesn't make threats of self-harm, he did die by suicide, though I would say it was more a powerplay than a fear of abandonment.
He is quickly angered, especially in the later chapters and acts out violently throughout the story
Now we have some other "critiria" like wide moodwings and "Quick changes in how you see yourself," I saw a redditor say this: "Although Dutch sees himself as an anarchistic Robin Hood-type hero during RDR2, he's clearly conflicted by RDR1, presenting himself as both a freedom fighter and a savage who can't fight his own violent nature." And while that is true, it does not fit the critira. It is not a quick change going back and forth but rather a steady but stable decline to that. A lot of people forget that it isn't just a change, but a back and forth we need for this diagnosis, and to me it is more that he is, as said, steadily moving, when he has reached one level of "madness" he doesn't go back.
Then we have a few critera I don't think fits, like unstable relationships, he has a lot of longer, fairly stable relationships such as with Hosea and Arthur and John, those were stable for 30 years before falling apart at the end. Again we are missing the movement back and forth.
End Note
As said, I am not a psycologist and if anything is worded wrongly in a way that may seem offensive, I appologice and please let me know.
#rdr2#rdr2 community#red dead redemption 2#arthur morgan#rdr2 arthur#red dead redemption community#red dead redemption two#john marston#red dead fandom#rdr john#dutch rdr2#rdr2 dutch#dutch van der linde#dutch#rdr2 eagle flies#eagle flies#nthspecialll#i love asks sm#answered asks#ask me stuff#nthspecialll asks
26 notes
·
View notes
Text
On Nesta and Alcoholism
I’ve seen a couple takes recently saying essentially “Nesta is not an alcoholic bc xyz”. The spirit it’s said in is usually supportive of her and based in countering the way the IC dehumanizes and stigmatizes her, which is great AND there are some common stereotypes about alcoholism that can deter people from seeking treatment or realizing their alcohol use is hurting them. Alcohol is the 4th leading cause of preventable death in the United States, and ~11% of people over 18 qualify for an alcohol use disorder every year.
Creds: am a currently practicing counselor with specialization in addiction treatment
So a few basic points on problematic alcohol use:
Risk exists on a spectrum from no risk to imminent fatality. Most users fall in the middle. We have a very narrow portrait of what alcoholism looks like in popular media, especially in women, and it’s almost always the most severe end of the spectrum.
Use does not have to be 24/7 to be risky. Binge drinking, as defined by 4+ drinks for afab people and 5+ drinks for amab people in one drinking episode, has just as much potential for chemical dependency and damage.
A person does not have to be chemically dependent (“addicted”) or have cravings to have an alcohol use disorder, nor does everyone with an AUD go through withdrawal.
Using alcohol as a tool for emotional regulation, sleep, social anxiety, etc outside of rare occasions qualifies as problematic use. This kind of drinking is, unfortunately, very socially acceptable.
Problem drinking is progressive, and tends to get worse without conscious choice or effort to change
You can have a dysfunctional relationship with alcohol without having an AUD. You can have an AUD while still being a fully functioning person on the outside.
Risky or problematic use is often a symptom of a deeper emotional wound, which should be treated with care and seriousness even if someone doesn’t meet the criteria for an AUD.
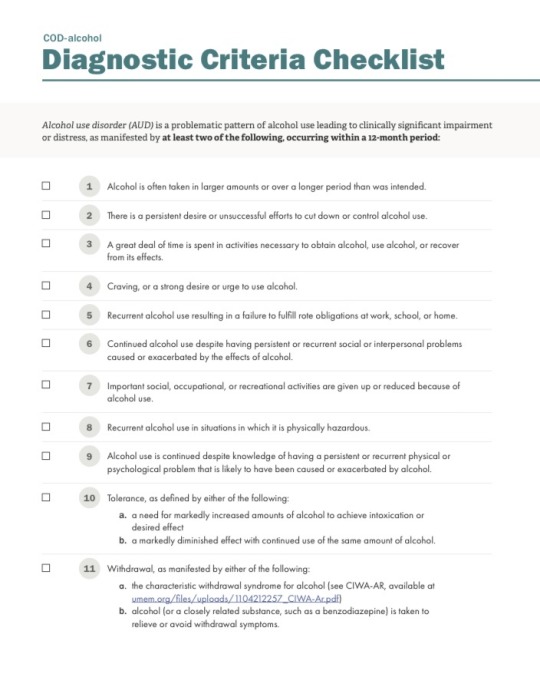
They don’t have the DSM in Prythian obviously, but for us mere mortals here are the criteria. A person only needs TWO to qualify for a diagnosis:
As a clinician, I usually look for a few hallmarks.
Alcohol is one of or is the primary strategy a person uses to regulate emotion and stress, or is a common way someone rewards or incentivizes themselves
Alcohol is an important “character” in at least one sphere of someone’s life and they feel the absence when it’s not there, eg. social activities all center around drinking, essential part of dinner/sleep routine etc
The client has feelings of shame or guilt around drinking, choices they make while drinking, or the consequences it’s had in their life. oR they feel a defensiveness about their drinking and distress at the idea of stopping.
Anyway, that’s my PSA. I would diagnose Nesta with an AUD, but I would also diagnose her with PTSD, and also diagnosis is a horribly flawed system that allows people to access their insurance benefits. I guess I just want to say that you don’t have to look like the media version of alcoholism to be concerned about your drinking or to deserve quality treatment. If you’re concerned, help is available.
36 notes
·
View notes