#When that is due to GI disease and kidney disease
Explore tagged Tumblr posts
Text
Great news. It is 70 degrees out realfeel in the 80s with no cloud cover so I went to the Korean grocery store then got home, vomited about a pint of bile, and briefly passed out. POTS will kill me via climate change AMA
#Like I'm genuinely terrified of this summer. I Will lose my job and I will be too incapacitated to function#Cardiologist won't change my treatment and they just keep ordering EKGs every month that say I have#Heart problems due to electrolyte imbalances and dehydration#When that is due to GI disease and kidney disease#Like it is all Connected but none of my doctors will work holistically about it#I drink 2-3 liters of water and at least 12 oz of Liquid IV every day and I am so dehydrated it#Shows up on bloodwork as metabolic acidosis and renal damage#Because my body won't retain water and pisses Everything out
9 notes
·
View notes
Text
Gastro in Kanpur: Expert Gastro Surgery by Dr. Kaustubh Gupta
Gastrointestinal (GI) disorders are a common concern for many individuals, affecting the digestive system, including the stomach, intestines, liver, pancreas, and gallbladder. These conditions can range from mild issues such as indigestion to more serious ailments like gallstones, acid reflux, or cancer. If you are seeking a trusted Gastro specialist in Kanpur, Dr. Kaustubh Gupta is your ideal choice for expert diagnosis, treatment, and recovery. With his extensive qualifications and expertise, Dr. Gupta provides top-tier care for various gastrointestinal issues, including gastro surgeries, gall bladder issues, hernia surgeries, and more.
Piles doctor in kanpur
This article provides a comprehensive look into the world of gastro care in Kanpur, highlighting the services offered by Dr. Kaustubh Gupta and why he is considered one of the best surgeons in Kanpur.
What is Gastro Surgery?
Gastro surgery refers to the range of surgical treatments aimed at addressing issues related to the gastrointestinal tract. The digestive system is a complex network of organs, and when one part of the system malfunctions, it can lead to significant discomfort and health complications. Gastro surgery may involve the treatment of conditions affecting the stomach, liver, intestines, gall bladder, pancreas, and other digestive organs.
Some of the common gastro conditions that may require surgical intervention include:
Gallstones
Acid reflux and GERD (Gastroesophageal reflux disease)
Hernia
Inflammatory bowel diseases (IBD)
Colon cancer
Stomach ulcers
Diverticulitis
Pancreatitis
Dr. Kaustubh Gupta, an expert in gastro surgeries, offers a wide range of treatments that are designed to address these issues effectively, helping patients return to optimal health.
Why Gastro Issues Shouldn’t Be Ignored
The digestive system plays a vital role in maintaining overall health by breaking down food, absorbing nutrients, and eliminating waste. When this system is compromised due to illness or injury, it can significantly affect a person’s quality of life. Some conditions, if left untreated, can lead to severe complications, including:
Malnutrition from poor absorption of nutrients
Chronic pain or discomfort
Dehydration due to improper digestion
Infections resulting from untreated conditions
Increased risk of cancer in cases of delayed treatment for conditions like colon cancer
Therefore, timely intervention is essential. Dr. Kaustubh Gupta specializes in diagnosing and treating gastrointestinal issues with precision, using the latest medical technologies and surgical techniques.
Dr. Kaustubh Gupta: Best Gastro Surgeon in Kanpur
Dr. Kaustubh Gupta is one of the most trusted gastro surgeons in Kanpur. With a medical career spanning several years, Dr. Gupta has earned a reputation for providing expert care for various gastrointestinal problems. Holding multiple advanced qualifications such as MBBS, MS, DipMAS, FMIS, FIAGES, EFIAGES, and FAIS, he is equipped with both the knowledge and the skills to address even the most complex gastro conditions.
Dr. Gupta’s clinic in Kakadeo, Kanpur, offers a full range of services to diagnose, treat, and manage gastrointestinal conditions, ensuring patients receive the best possible care. His expertise extends to a wide range of surgeries, including:
Gall bladder surgery for gallstones or other issues
Hernia surgery for abdominal or groin hernias
Stomach and intestinal surgeries for diseases such as IBD, ulcers, or colon cancer
Stone treatment and surgery for kidney or bladder stones
Trauma surgery for injuries to the digestive organs
Varicose veins surgery for swollen veins in the legs, often related to gastrointestinal health
Hydrocele surgery for fluid accumulation around the scrotum
His specialization as a proctologist further allows him to provide expert care for conditions like hemorrhoids, anal fissures, and other anorectal issues. Whether you need piles treatment, a comprehensive gastro surgery, or cancer care, Dr. Kaustubh Gupta ensures that every patient receives the appropriate treatment based on their unique condition.
Services Offered by Dr. Kaustubh Gupta
Gastro Surgeries
Gastrointestinal surgeries are an essential part of Dr. Gupta’s practice. From minimally invasive techniques to more complex procedures, Dr. Gupta utilizes state-of-the-art equipment and modern surgical approaches to ensure the best outcomes for his patients.
Some common gastro surgeries performed by Dr. Gupta include:
Gall Bladder Surgery: Gallstones are a common issue that can lead to severe abdominal pain, nausea, and vomiting. Dr. Gupta performs laparoscopic gallbladder surgery to remove the gall bladder in a minimally invasive manner, ensuring faster recovery and minimal discomfort.
Hernia Surgery: Hernias, especially in the abdominal region, are another common issue that can affect the digestive system. As a renowned hernia surgeon in Kanpur, Dr. Gupta offers effective surgical treatments to correct hernias and prevent recurrence.
Appendix Surgery (Appendectomy): In cases of appendicitis, an infection in the appendix, Dr. Gupta performs appendix surgery to remove the infected appendix and prevent more severe complications like rupture or peritonitis.
Cancer Surgery: Dr. Gupta is also a well-regarded cancer doctor in Kanpur, particularly specializing in gastrointestinal cancers. Whether it’s stomach cancer, colorectal cancer, or cancer of the liver or pancreas, Dr. Gupta provides comprehensive surgical solutions.
Proctology Services
As a skilled proctologist in Kanpur, Dr. Kaustubh Gupta treats a wide range of anorectal conditions such as:
Piles (Hemorrhoids): Dr. Gupta provides both surgical and non-surgical treatments for piles, ensuring that the most appropriate approach is taken based on the severity of the condition.
Fissures and Fistulas: For patients suffering from painful anal fissures or fistulas, Dr. Gupta offers minimally invasive treatments that promote quick recovery and relief.
Anal Incontinence: Dr. Gupta’s expertise also extends to treating issues related to anal incontinence, which can occur due to nerve damage, trauma, or other underlying gastrointestinal conditions.
Stone Treatment and Surgery
Kidney stones, bladder stones, and gallstones can all disrupt the normal functioning of the digestive system. Dr. Gupta offers cutting-edge solutions, including laparoscopic stone removal and other non-invasive methods to treat and eliminate stones in the gastrointestinal and urinary systems.
Varicose Veins Surgery
Though varicose veins are often thought of as a vascular issue, they can sometimes be related to gastrointestinal health, particularly when associated with liver disease or digestive problems. Dr. Gupta’s varicose veins surgery provides relief to those suffering from swollen, painful veins in the legs.
Dr. Gupta’s Approach to Treatment
Dr. Kaustubh Gupta’s approach to gastro care is patient-centered, with a focus on precise diagnosis and effective treatment. He combines traditional surgical techniques with modern advancements in gastroenterology, ensuring that his patients receive the best care available.
Moreover, his emphasis on patient education helps individuals understand their conditions and the treatment options available to them, empowering them to make informed decisions about their health.
Why Choose Dr. Kaustubh Gupta for Gastro Care in Kanpur?
When it comes to gastro surgery in Kanpur, Dr. Kaustubh Gupta stands out for several reasons:
Expertise and Experience: With numerous qualifications and years of experience in the field, Dr. Gupta is one of the most sought-after gastro surgeons in Kanpur.
Comprehensive Care: Whether it's treating a simple digestive issue or performing complex gastrointestinal surgery, Dr. Gupta provides comprehensive care for all gastro-related conditions.
Advanced Treatment Options: Dr. Gupta uses the latest medical technologies to ensure that his patients benefit from the most effective treatments available.
Patient-Focused Approach: He takes the time to listen to his patients, diagnose their conditions accurately, and recommend the best course of treatment tailored to their needs.
See more:-
Varicose veins in kanpur
Proctologist in kanpur
Piles doctor in kanpur
Cancer doctor in kanpur
0 notes
Text
Healthy Eating for Diabetics: How to Make Smart Food Choices for Better Blood Sugar Control
Introduction:
Eating the right foods plays a crucial role in managing diabetes. Whether you're newly diagnosed or have been living with diabetes for years, the foods you choose can have a major impact on your blood sugar levels. But with so much conflicting information about what to eat, it can be overwhelming to know where to start. In this blog, we’ll explore practical strategies for making healthier food choices and creating a balanced diet that supports your diabetes management goals.
1. The Basics of Diabetes and Diet: Why It Matters
When you have diabetes, your body has difficulty regulating blood sugar levels due to either insufficient insulin production or insulin resistance. Eating foods that help stabilize blood sugar is key to maintaining good control over the condition.
Why Diet is Important:
Blood Sugar Control: Certain foods can cause blood sugar levels to spike or drop rapidly. The goal is to choose foods that provide a steady release of energy, keeping blood sugar levels within a healthy range.
Weight Management: Maintaining a healthy weight helps improve insulin sensitivity, especially for those with Type 2 diabetes.
Preventing Complications: A balanced diet helps reduce the risk of diabetes-related complications such as heart disease, nerve damage, and kidney problems.
By making smart food choices, you can reduce the risk of these complications and improve your overall health.
2. Understanding Carbohydrates: The Key to Blood Sugar Management
Carbohydrates are the primary nutrient that impacts blood sugar levels. However, not all carbs are created equal. It’s important to focus on the quality of carbohydrates you eat, rather than just the quantity.
Types of Carbohydrates:
Complex Carbs (Good Carbs): These include whole grains (like brown rice, quinoa, and oats), legumes, vegetables, and fruits. They are rich in fiber and digest more slowly, which helps prevent blood sugar spikes.
Simple Carbs (Bad Carbs): These are found in foods like sugary snacks, sodas, and refined grains (like white bread and pasta). They cause quick spikes in blood sugar levels and can lead to insulin resistance over time.
Glycemic Index (GI): The glycemic index measures how quickly a food raises blood sugar levels. Low-GI foods (like whole grains, sweet potatoes, and beans) have a slower effect on blood sugar compared to high-GI foods (like white bread and sugary cereals).
Tip: When planning your meals, focus on including complex carbs and avoid refined sugars and processed foods as much as possible.
3. The Power of Fiber: A Diabetes Superfood
Fiber is one of the most important nutrients for diabetics. It helps control blood sugar by slowing down digestion and the absorption of sugar, preventing sharp spikes in blood glucose levels.
Fiber-Rich Foods:
Whole Grains: Brown rice, quinoa, barley, and whole-wheat bread are all excellent sources of fiber.
Fruits and Vegetables: Fiber-rich options include leafy greens, apples, pears, berries, and avocados.
Legumes: Beans, lentils, chickpeas, and peas are great sources of fiber and protein.
Key Tip: Aim for at least 25–30 grams of fiber per day to help regulate blood sugar and promote digestive health.
4. Healthy Fats: Good for Your Heart and Blood Sugar
Many people with diabetes are at an increased risk of heart disease, which makes choosing healthy fats especially important. Healthy fats can help improve insulin sensitivity and lower cholesterol levels, benefiting both your heart and blood sugar.
Healthy Fat Sources:
Avocados: Packed with heart-healthy monounsaturated fats, fiber, and nutrients.
Nuts and Seeds: Almonds, walnuts, chia seeds, and flaxseeds are excellent sources of healthy fats, fiber, and protein.
Olive Oil: A great source of monounsaturated fats that can help reduce inflammation and improve heart health.
Fatty Fish: Salmon, mackerel, and sardines are rich in omega-3 fatty acids, which support heart health and improve insulin sensitivity.
Tip: Aim to replace saturated fats (like butter and full-fat dairy) with healthier options, such as olive oil or avocado.
5. Protein: Essential for Diabetes Management
Protein is an important part of a balanced diet, as it helps stabilize blood sugar levels and provides long-lasting energy. Including a variety of protein sources in your meals can help you feel full and satisfied, reducing the temptation to snack on high-carb foods.
Good Protein Sources:
Lean Meat: Chicken, turkey, and lean cuts of beef and pork provide high-quality protein without excess saturated fat.
Fish and Seafood: Fish like salmon, trout, and tuna are great sources of protein and healthy fats.
Plant-Based Protein: Tofu, tempeh, edamame, and legumes (beans, lentils, chickpeas) are excellent plant-based protein sources.
Eggs: A versatile and affordable source of protein, eggs are also rich in vitamins and minerals.
Tip: Aim to include a source of lean protein at every meal to help maintain stable blood sugar levels and prevent overeating.
6. Portion Control: How to Avoid Overeating
Portion control is crucial for managing diabetes, as overeating—even healthy foods—can cause blood sugar levels to rise. By learning to control portion sizes, you can enjoy a variety of foods without negatively impacting your health.
Tips for Portion Control:
Use Smaller Plates: Eating from a smaller plate can help trick your brain into feeling satisfied with smaller portions.
Measure Your Food: Use a food scale or measuring cups to track portions until you get a better understanding of appropriate serving sizes.
Listen to Your Body: Eat slowly and stop when you feel full. It takes time for your body to signal that it’s had enough food.
Tip: Try using the “plate method” to control portions: half of your plate should be non-starchy vegetables, a quarter should be lean protein, and a quarter should be whole grains or starchy vegetables.
7. Hydration: The Importance of Drinking Water
Staying hydrated is essential for overall health and helps regulate blood sugar levels. Sometimes, thirst can be mistaken for hunger, leading to overeating and fluctuations in blood sugar.
Healthy Hydration Tips:
Drink Water: Water is the best beverage for hydration and has no impact on blood sugar levels.
Limit Sugary Drinks: Avoid sugary sodas, juices, and sweetened teas, as they can cause blood sugar spikes.
Herbal Tea: Unsweetened herbal teas (such as green tea, peppermint, or chamomile) can be a good alternative to sugary beverages.
Tip: Aim to drink at least 8 cups (64 ounces) of water a day, or more if you're active or live in a hot climate.
8. Planning Your Meals: Easy Strategies for Success
Creating a diabetes-friendly meal plan can help you make healthier choices and stay on track with managing your blood sugar. Planning ahead also reduces the likelihood of reaching for unhealthy snacks when hunger strikes.
Meal Planning Tips:
Cook at Home: Preparing meals at home gives you control over ingredients and portion sizes.
Batch Cooking: Prepare large batches of meals and store them in portion-sized containers for easy access throughout the week.
Plan for Snacks: Choose healthy snacks like nuts, yogurt, or raw vegetables with hummus to keep blood sugar levels stable between meals.
Tip: Consider working with a registered dietitian to develop a personalized meal plan that fits your taste preferences, lifestyle, and diabetes management goals.
Conclusion: Make Every Bite Count for Better Diabetes Management
Healthy eating is one of the most important tools in managing diabetes and maintaining good overall health. By making informed food choices, focusing on balanced meals, and controlling portion sizes, you can better manage your blood sugar and enjoy a healthier life. Remember, it's not about perfection—it's about consistency and finding what works best for your body.
Share Your Tips: What are your favorite diabetes-friendly meals? How do you manage your blood sugar through diet? We'd love to hear your thoughts in the comments below!
0 notes
Text
I have this, have for years; the hemoglobin levels are always normal, but my ferritin levels are precarious. I think the problem is that iron absorption without anemia (anemia is when the hemoglobin's too low), is under-studied and can be caused by many unrelated things. I've had various tests over the years and still haven't found a cause.
Here are some articles I have found during my own search, I've copied the info they have about causes below:
Iron deficiency without anaemia: a diagnosis that matters
"Causes of iron deficiency can be grouped into the following categories: inadequate dietary intake, increased body needs, reduced absorption, chronic inflammation and chronic blood loss."
Causes of non-anaemic iron deficiency (aetiology)
Inadequate intake (nutritional iron deficiency):
Plant-based diets with little meat.
Low calorie intake in relation to iron requirement - eg, growing children, pregnant women and the elderly.
Inadequate absorption:
Malabsorption - eg, coeliac disease.
Excessive consumption of foods which reduce absorption - eg, cow's milk, tea.
Achlorhydria (gastric acid maintains ferric iron in solution, so aids absorption) - eg, from proton pump inhibitors or post-gastrectomy.
Helicobacter pylori colonisation reduces iron uptake.8
Excessive loss:
Heavy menstrual bleeding.
Gastrointestinal (GI) losses:
Peptic ulcer, erosion, oesophagitis.
GI malignancy (although this tends to cause iron deficiency with anaemia).
Inflammatory bowel disease.
Coeliac disease.
Non-steroidal anti-inflammatory drugs (NSAIDs).
Other GI losses - eg, recurrent bleeding from haemorrhoids, dental bleeding or epistaxis.
Intestinal parasites - eg, hookworms.
Haematuria.
Blood donation.
Intravascular haemolysis (rarely).
Endurance athletes may be at risk of iron depletion from increased losses.
Functional iron deficiency:
This is inadequate iron supply to the bone marrow, while storage iron is present in the reticulo-endothelial cells.
It can occur in chronic kidney disease (CKD) and many chronic inflammatory diseases (eg, rheumatoid arthritis and inflammatory bowel disease).
Iron deficiency can be either absolute or functional in patients with heart failure, and is an independent predictor of outcomes and significantly contributes to exercise intolerance, whether there is anaemia or not. It may be caused by blood loss due to medication (anti-platelets, anticoagulants), malabsorption or reduced intracellular iron uptake.9 Patients with heart failure should be screened for iron level even if they are not anaemic, as treatment of depletion can improve prognosis.10
Hey, so, guess who has hidden secret anemia that wasn’t detected by a basic iron panel? Again.
🫠
4K notes
·
View notes
Text
cw for more medical and animal death stuff under the cut about my pet but at least it's not super duper depressing this time (admittedly v dependent on your opinion of depressing)
after some back and forth with his vet + the care team at the hospital, we're pretty sure at this point of two things:
sweet likely passed away due to acute kidney failure. that's why he was so chipper and energetic in the days leading up to it, and why we had so little warning. apparently, kidney failure in rabbits can occur in hours. because they're just so freaking good at hiding it when they're ill, the only signs we had that something was off with him were that he was suddenly disinterested in his hay again, which is something we knew how to respond to due to the recurring GI stasis episodes he'd been having for about 7-8 months, and the day just before he had an accident on the couch.
that one kind of haunts me, because it literally never happens - sweet was like, perfect about peeing in his litterbox. so a part of me thinks i should've known something was going on when that happened. we were giving him a pain med, motility meds and simethicone at that point, on the recommendation of his doc. we thought we had it totally handled and his organs were shutting down.
secondly, the reason why his gut kept going into stasis was almost certainly something called rabbit megacolon syndrome. our vet was reluctant to diagnose that last year, because he wasn't really having the diarrhea that's most characteristic of it, but all of the other symptoms match up. he was struggling to process nutrients, and stressed from being sick over and over again. so his kidneys started to go.
he did not have a granuloma. it's unlikely that the diet we were feeding him caused an outgrowth of microbes. he was fully vaccinated against RHDV2, and his tests came back negative for parasites. plus, megacolon is genetic (either parent), so the fecal transfaunation his doc suggested like, the week before all of this happened might not have even helped very much to rebalance his gut flora, because recurring periods of GI stasis would've eventually caused another imbalance.
and, okay, i'm going to moralize for a second, because i'm a little mad, because my friend is dead and i love him very much. if there is anything at all that this horribly confusing experience has taught me, it's that for an animal so prized for their ease of utility in lab protocols, rabbits and the diseases that can affect them are NOT well enough researched.
if i'd known the above info sooner, i would've made different choices about how i'd spent our time together. we know now that sweet basically wasn't going to get better, but that's new. our vet gave us the strong impression that if we acted carefully and continued in a process-of-elimination strategy, we might eventually be able to heal him, and that wasn't ever going to happen. the shitty thing is, it wasn't his doc's fault for giving us hope, either! she was working off of the knowledge that she had about the disease states and conditions that are known to affect rabbits. it's just upsetting to think about how we would've done it different.
#maybe we could've spoiled him!!! or done more things to 'prepare' and make him comfortable. even chosen a day for him to go to sleep#instead of the insane midnight running red lights shit we did trying to get him to the hospital in time.#sweet tag
1 note
·
View note
Text
Veterinary rambling:
So Sophie gets to go in tomorrow for an expensive abdominal ultrasound, because due to some recent bloodwork and other symptoms, they are maybe suspecting GI cancer.
This is totally a possibility, but I’ve been doing some googling and I’m not so sure anymore it’s such a clear thing. The symptoms they think would be explained by cancer, she’s had for years now, (which I told them, and I feel like no one is listening to me) and I don’t see how she could be sick enough with cancer that it’s been causing symptoms for almost FOUR YEARS, but ALSO did not show up in the extensive diagnostics they ran one year ago when she was very sick with a bladder infection. The blood levels that can indicate cancer can ALSO apparently just be their own separate and discrete disorder not caused by anything else, and the vet didn’t tell me that.
I mean it’s totally possibly that unrelated to anything else, she has developed cancer over the last year. She is 15, something like that is going to happen sooner or later inevitably. If it’s not that, the kidney disease will eventually get her some day. I think she should still get the tests tomorrow, but I’m going to be extremely cranky if the ultrasound comes back entirely normal, and then they want to run even more expensive tests, on a cat that really isn’t… sick or in pain in any way that affects her quality of life day to day. We’ll see what happens.
At the very least, I don’t have my mom hanging over me right now reminding me constantly how silly she thinks it is to spend so much money on just a cat.
1 note
·
View note
Text
Alarm Bells in Liver Cirrhosis! When to contact the doctor urgently?
Liver cirrhosis causes nodular transformation of liver parenchyma with progressive deterioration of liver function. Liver Transplantation is a sustainable curative option for liver cirrhosis.
The patients of liver cirrhosis may live for a long time without needing liver transplantation, if they stay away from chemicals harming liver like alcohol, certain drugs and include a balanced, protein rich diet and regular exercise in their lifestyle. They must be in regular follow up with their physician with regular blood reports and imaging reports, as advised by the doctor.
There are certain alarming symptoms and signs in liver cirrhosis, which must prompt the patient to reach the doctor or the hospital immediately.
1) Blood in vomitus or stool or coffee colored vomitus or black colored stool
Blood in vomiting or vomiting of ground coffee color is suggestive of bleeding from dilated veins (varices) in food pipe (esophagus) or stomach. Black colored stool with tar-like appearance is also suggestive of bleeding in gastrointestinal tract. These bleeding episodes may often turn to be life-threatening. One must immediately reach the hospital in event of any such episode. One may require upper GI endoscopy or colonoscopy to find the source of bleeding and control it.
2) Increasing abdominal girth
Increasing abdominal girth may be suggestive of fluid accumulation in abdomen, also known as ascites in medical term. Ascites formation is indication of deteriorating liver function. One must consult the doctor as control of ascites may require some diet modification and/or addition of some medicines, known as diuretics. Ascites, which is not controlled by diuretics (refractory ascites), or intolerance to diuretics (diuretic-intolerant ascites) may warrant an early liver transplantation.
3) Altered sensorium, altered sleep cycle or loss of consciousness
Ammonia is detoxified by liver. Once liver function deteriorates, ammonia is not excreted out and starts building up in blood. High ammonia circulating in blood, may cause altered sensorium, altered sleep cycle or loss of consciousness, also known as hepatic coma. The conglomeration of these features is also known as hepatic encephalopathy, which may turn out to be a life-threatening condition. Onset of any of these symptoms warrants urgent hospitalization. Control of blood ammonia levels may require certain measures like lactulose enema and lactulose syrup.
4) Jaundice – yellowish discoloration of eyes, skin and urine
New onset of jaundice may be related to a binge of alcohol drinking or may be indicative of worsening function of liver. One must visit the doctor in such situation to get evaluated.
5) Reduced urine output
Decreasing urine output in liver cirrhosis may be due to multiple causes like infection, hepatorenal syndrome (kidney dysfunction due to liver disease) or may indicate worsening of liver function. It may warrant hospitalization in some situations especially if it is associated with deranged kidney function tests or infection.
6) Acute pain in abdomen
Acute pain in abdomen in liver cirrhosis may be because of infection in fluid in abdomen (spontaneous bacterial peritonitis). It is a serious complication of liver cirrhosis and warrants hospitalization and intravenous antibiotics with tapping of fluid (ascites).
7) Fever
Liver cirrhosis compromises the immune system of a patient. Such patients are at risk of recurrent infections which may affect any part of the body, commonly – lungs, urinary system, and biliary system. It will require antibiotics and often hospitalization if infection is serious.
8) Difficulty in breathing
Patients with liver cirrhosis, may often develop fluid accumulation in abdomen or chest. Excessive fluid collection in abdomen can cause difficulty in breathing and/or difficulty in eating. Excessive fluid collection in chest can cause difficulty in breathing. One should immediately reach the hospital in any such situation. One may need removal of fluid and modification in medicines to relieve the symptoms and prevent further complications.
9) Significant weight loss
Sudden and significant weight loss (involuntary weight loss – more than 10% of weight in last 6 months or more than 5% of weight in last one month) may be indicative of worsening of liver function or onset of a new complication like liver cancer. In event of significant weight loss, one must immediately contact the doctor and get evaluated.
10) An abnormal mass or lesion on routine ultrasound or CT scan
Liver cirrhosis is a pre-malignant (cancer predisposing) condition. This is the reason, why, regular scans in form of ultrasound are advised for the patient. If during such scan, any mass or lesion in liver is detected, it warrants further evaluation in form of blood tests and CT scan or MRI. Such patients may require liver transplant, surgical resection of tumor containing part, ablation, TACE or chemotherapy, depending on the stage of the tumor, functional status of the liver, and general health status of the patient.
Conclusion
The patients with liver cirrhosis must stay in regular follow up with their physicians. Onset of any of the above symptoms must prompt them to reach the hospital and get evaluated by their physician.
The above is the management in brief about liver cirrhosis. If you have any patient suffering from liver problems, do consult your Liver specialist. To know more, feel free to call +91 6359 602647
#liver specialist doctor in gujarat#liver transplant surgeon in ahmedabad#liver transplant in ahmedabad
0 notes
Text
What Are The Best Medicines For Treating A Bloated Stomach?
In your belly, you have bloating (stomach). It occurs when your digestive system (GI) is overflowing with gas or air. From the mouth to the anus, the GI tract is located (bottom). Your whole digestive system is a part of it. When you are bloated, it seems like you have eaten a substantial meal, and your stomach is full. Your belly feels tight and full. It could hurt or be unpleasant. You could think that your stomach is larger. After some time, it normally fades away, but for some people, it keeps happening. Hormonal changes and digestive problems can bring on cycles of bloating. You should consult a doctor to find out the source of your swollen stomach if it doesn't go away.

Gas off tablet is a homeopathic medicine for bloating from Doctor Bhargava. We'll understand more about its benefits later in this post.
Who May Have Bloating: Causes of Gas
Small Intestinal Bacterial Overgrowth (Sibo):
Numerous bacteria that aid in food digestion reside in the stomach and intestines. An increase in dangerous bacteria in the small intestine might result from disrupting the equilibrium of microorganisms. Small intestinal bacterial overgrowth, or SIBO, is what this is.
Retention Of Fluid:
Chronic bloating brought on by fluid retention may be due to a more serious condition, such as diabetes, liver disease, or kidney failure. A person should consult a doctor if the bloating persists.
Food Allergies:
Some people — such as those who have lactose intolerance, gluten allergies, or celiac disease — experience bloating after consuming particular meals. Bloating can be brought on by diarrhoea or stomach pain and will go away if the offending meal is eliminated.
Gynaecological Conditions:
Bloating can be brought on by some gynaecological issues, such as menopause or monthly menstruation. Bloating, cramping, and stomach discomfort can also be symptoms of endometriosis, a condition in which the lining of the womb connects to the stomach or intestines.
How Can The Problem of Rectal Prolapse be Prevented?
Even though homeopathic remedy for bloating is present, you shall first understand how to prevent bloating at home.
Teas made from herbs, such as peppermint, chamomile, ginger, turmeric, and fennel, can help with digestion and the elimination of gas. Dandelion tea can assist in reducing fluid retention.

Capsules containing peppermint oil work as a natural spasmodic. They, therefore, aid in the relaxation of your gut muscles. This can assist you in releasing gas and stool that has been retained, especially if your difficulties are related to your motility.
Antacids have been demonstrated to reduce digestive tract irritation and facilitate simpler gastric emptying. Simethicone, an active component of several antacids, helps pass gas by clumping together tiny gas bubbles. Simethicone can be purchased individually as well.
Magnesium supplements assist in relaxing the gut muscles and neutralizing stomach acid. Magnesium has a natural laxative effect that can be occasionally useful but can become habit-forming if used excessively.
Your gut bacteria can be augmented or rebalanced with the use of probiotics. Some will improve how you digest your food, while others could aid in the absorption of more gas. You might need to take them consistently for a few days or weeks to see an improvement.
Psyllium husks are a well-liked fibre supplement that might encourage more frequent bowel movements. Always add fibre supplements gradually and drink a lot of water when doing so. As needed, over-the-counter laxatives can also be used.
Abdominal bloating may be fought with consistent training that emphasizes core body strengthening.
Homeopathic Medicine For Flatulence:
Gas off tablet:This is one of the best homeopathic remedy for gas manufactured by Dr Bhargava. It is a helpful homeopathic remedy for gas, flatulence, indigestion, bloating, abdominal distention, agitated bowel motions, constipation, colitis, and acidity, as well as for gastritis and flatulence.
0 notes
Text
Cat Facts: Why’s this Cat Vomiting?

Like most of my posts, this is coming more from a veterinary student/pre-vet education perspective, but hopefully some owners that follow me can get some useful info from this!
Unsurprising to most vet students, there’s about as many reasons for vomiting as there are diagnoses in general. We’re going to attempt to narrow that down a bit, break them into categories which makes it more useful for diagnostics and relevant differentials.
First off, you have to differentiate vomiting from regurgitation.
Vomiting: nausea (drooling, lip licking, swallowing, depression/restlessness), abdominal muscle contraction, contains bile/digested blood/digested food
Regurgitation: no nausea, no abdominal contractions or bile, presence of undigested food in a tubular shape.
Once you’re sure it’s actually vomiting, you’ll need to differentiate it into acute or chronic, as well as emergency/non-emergency. Acute will be in the last few days or day of presentation, often multiple times in the same day, and will often present as more “sick” than the chronic vomiter.
In chronic cases, the vomiting is usually more than 2 times a month and has been going on for months to years. Chronic vomiters can be “apparently healthy” and the vomiting only brought up at a wellness check or prompted by the vet/nurses and the owner didn’t think to bring it up because “cats just vomit, and they seem fine other than that.” History can help a lot! If there’s an acute case, and the cat has access to toxic substances, a habit or likelihood of eating foreign objects (hair ties, string, q-tips, etc), or has had a recent change in diet, that could lead you immediately to the most likely cause and the most appropriate next steps. Acute vomiting generally has fewer causes or at least more obvious causes, and next steps generally include abdominal radiographs or triage/supportive care if indicated. Physical exam can locate a linear foreign body that’s anchored to the underside of the tongue.
So, what if that doesn’t help? That’s when you start your baseline diagnostics! CBC/Chem/UA can rule in or rule out a lot of potential causes for vomiting:
Diabetes: hyperglycemia, glucosuria, ketonuria, low USG
Liver disease: hyperbilirubinemia, decreased BUN, increased liver enzymes, bilirubinuria
Renal disease: increased BUN/creatinine, low USG
Hyperthyroidism: increased T4, increased liver enzymes (ALP, ALT), mild increase in PCV, low USG
Electrolyte/acid-base derangements: Na, K, Cl, Ca, pH, bicarb, tCO2
Eosinophilia: parasites, IBD, hypereosinophilic syndrome, mast cell tumors
Neutrophilia: gastroenteritis, neoplasia
Neutropenia: salmonellosis, retroviruses
Hemoconcentration: dehydration
Anemia: chronic disease, GI blood loss
Fecal may also show parasites, and FeLV/FIV positive snap test might be supportive of vomiting from a FeLV/FIV related illness
Secondary diagnostics beyond bloodwork and urinalysis would be the next step after that. Radiographs may show abnormalities in organ size/architecture (small kidneys, enlarged liver), foreign bodies, GI obstruction, or masses.
Ultrasound is the diagnostic of choice for **chronic vomiting and normal bloodwork**. It can reveal thickening of the stomach/small intestines, wall layer changes, and/or enlarged lymph nodes. It can also show or allow better examination of abdominal masses, or the presence of free fluid.
fPLI may be indicated if pancreatitis is suspected, but may be normal in chronic pancreatitis cases. Heartworm testing if the cat lives in an endemic area, after other causes have been ruled out.
Intestinal biopsy and histopathology is recommended in cases of chronic vomiting with GI thickening seen on ultrasound. This will differentiate between IBD and lymphoma, which cannot be done without the histopath! Though presumptive and empirical treatment may be considered in cases of financial concern. IBD is often in younger cats and lymphoma in older, however that’s simply a generalization and not a hard and fast rule. IBD and lymphoma are the two most common causes of chronic vomiting in cats. Exploratory surgery and full thickness biopsies is preferred over endoscopic biopsy, as you can retrieve intestinal samples from more than just the duodenum, the samples will be higher quality for your pathologist, and you can determine the staging of the lymphoma (if that’s the cause).
What should I tell owners to keep a look out for? 2x a month or more vomiting, INCLUDING HAIRBALLS, is abnormal and justifies an ultrasound study. Cats should in theory be able to process hair since they evolved to groom their fur (a bit more leeway is given to long-haired cats since that’s a genetic mutation we’ve selected for), and vomiting hairballs regularly is suggestive of hypomotility of the GI tract.
The only exception to this is eating grass and vomiting, as grass is irritating to the stomach and can cause vomiting, but is more or less harmless on its own.
Due to this being a very wide topic I didn’t go much into specifics, but I can if you all are interested in any specific parts of this!
232 notes
·
View notes
Text
Zinc: How Much Do You Need?
Zinc is an essential mineral naturally present in some foods and should be consumed every day in order to maintain the overall health and support of hundreds of important bodily functions. Zinc is naturally present in high protein foods such as red meat, poultry, other meats, nuts, and beans. Zinc is involved in numerous functions including hormone production, cell division, cell growth, wound healing, digestion, and the body’s defence system (immunity).
Unfortunately, zinc levels decrease with diarrhea, kidney disease, liver disease, alcoholism, and diabetes. In such instances, zinc supplementation may be recommended.
Zinc Supplements
Zinc supplements are available in various formats like, oral lozenges, syrups, gels, tablets, and capsules. It’s also found in most multivitamin and mineral supplements. When it comes to dosing, zinc supplements are sold in a wide range of potencies between 15 and 50 mg – with 40 mg being considered the upper tolerable limit. However in instances of zinc deficiency, supplements in the 45 to 50 mg daily are often warranted. So how do you determine the appropriate dose for you? Let’s explore.
Zinc Potencies According to Needs
15 to 20 mg –
Healthy adult women need at least 8 mg of zinc daily, while men typically need 11 mg. Daily zinc requirements increase to 11-12 milligrams during pregnancy and lactation respectively. Individuals suffering from generalized dietary insufficiency, those with genetically-based zinc malabsorption, or dietary interference of zinc absorption (i.e. those consuming a high fibre, high phytate diet – grains, nuts, and legumes) may benefit from a daily zinc top-up in the 15-20 mg range.
25 to 30 mg –
A zinc supplement in the 25 to 30 mg range may be ideal for those who consume an adequate amount of high zinc foods; but are living with conditions such as chronic diarrhea, kidney disease, liver disease, alcoholism, or diabetes. A mid-range zinc supplement may also be ideal for athletes and the gym crowd in general since zinc is lost through perspiration. Those who live in hot climates and those who regularly use saunas or steam rooms could also benefit from a good 25-30 mg of zinc daily. This dose of zinc may also be ideal for those on oral contraceptives, diuretics, ulcer medications, and antibiotics since they deplete zinc in the body.
45 to 50 mg –
Zinc supports the growth and normal functioning of immune cells, so those that do not obtain an adequate amount of zinc through their diet may especially benefit from a clinical dose zinc supplement to protect them from viruses and bacteria. A higher dose zinc supplement may also be ideal for the elderly who often have low zinc intakes due to poor appetite, existing diseases (most notably GI conditions that hinder the absorption of zinc), and multiple medication use.
Final Thoughts
Zinc is an essential mineral for the body; it’s important to ensure you are getting the correct amount daily for your needs and lifestyle. If you are unsure if you are zinc deficient, get your levels checked by your doctor and speak to them or another health care practitioner to determine which dose would be appropriate for you.
2 notes
·
View notes
Text
everyday is Friday the 13th when you're studying
100 days of productivity
day 13
RS/CVS
NIPPV has best effect between pH 7.25-7.35; but generally trial NIPPV before tubing unless imminent or current respiratory collapse (or other indications such as failure to protect airway)
constrictive pericarditis vs tamponade: differentiate with y-descent of JVP; this is *absent* in tamponade, but otherwise they are clinically very similar
in the absence of thromboembolic events, pts with bioprosthetic valve replacements *do not need* warfarin (low dose aspirin sufficient)
asthma ICS dose: budesonide: low dose < 400 mcg; mod dose 400-800 mcq; high dose >800 mcg
ICS dose conversion: budesonide = beclomethasone, multiply budesonide dose x2 to get fluticasone dose
Rheum/Derm
pseudoxanthoma elasticum: AR mutation in ABCC6 (ATP-binding cassette transporter) skin: cutaneous laxity + yellow papules in flexural regions; eyes: blue sclerae + peau d'orange of Bruch's membrane + retinal angioid streaks; GIT: upper GI bleed!; CVS: accelerated atherosclerosis w/ consequent IHD/CVA/PAD; rheum: demineralisation w/ reduced circulating pyrophosphate
microscopic polyangiitis and GPA cause kidney involvement with equal frequency; HSP causes IgA nephropathy with much less frequency (and much less severity)
tinea incognita = tinea corporis that has had topical steroid tx; may show florid fungal growth without characteristic tinea lesions (skin scraping w/ KOH stain is sufficient to dx)
inclusion body myositis (not to be confused with hereditary inclusion body myopathies): most common inflammatory muscle disease in adults! → sporadic, nonheritable progressive asymmetric weakening and wasting of both proximal and distal muscle groups (may mimic ALS but is a myopathy rather than a neuropathy and NCS/bloods will reflect that, eg, ↑CPK in IBM)
CNS
floaters + flashes of light = vitreous detachment
important ddx for Wernicke encephalopathy: cerebellar stroke. Do NOT forget the CT brain!
neuromyelitis optica: differentiate from MS w/ anti-NMO IgGs (such as anti-aquaporin 4 (AQP4) and anti-myelin oligodendrocyte glycoprotein (MOG))
pons = horiPONStal gaze palsy
SCD: T2-weighted hyperintensity of affected areas (dorsal column, lat corticospinal tracts, spinocerebellar tracts)
Haem/Onc
Stauffer syndrome: renal cell ca associated nonmetastatic hepatobiliary dysfunction (cholestatic enzyme pattern, elevated platelets/PT, hepatosplenomegaly, NORMAL bilirubin, NO jaundice)
GIT
FAP: the second most common cause of death after colorectal cancer is duodenal cancer
Whipple's disease: tx with 1-1.5 yrs of ampicillin or cotrimoxazole or doxy+HCQS, then assess, then continue tx if necessary
Psych/Toxo
sertraline specifically is used for agoraphobia due to best cost-effect ratio; other SSRIs are second line
long-term lithium side effects: LITHIUM: Leukocytosis, Intracranial hypertension, Tremor/Teratogen, Hair loss/Hypothyroid/Hyperparathyroid, Increased Urine (N-DI), Metabolic syndrome
other than hypokalaemia, other precipitating factors for digitoxicity include hypernatraemia, hypomagnesaemia and hypothermia
Misc
bezlotoxumab → C. diff toxin B
suvratoxumab → S. aureus alpha toxin
6 notes
·
View notes
Text
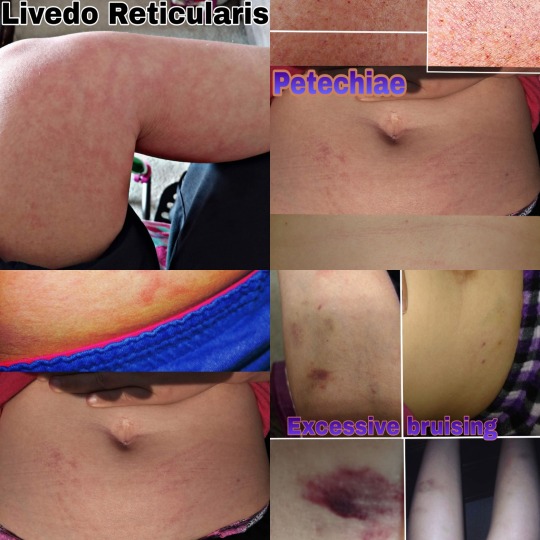
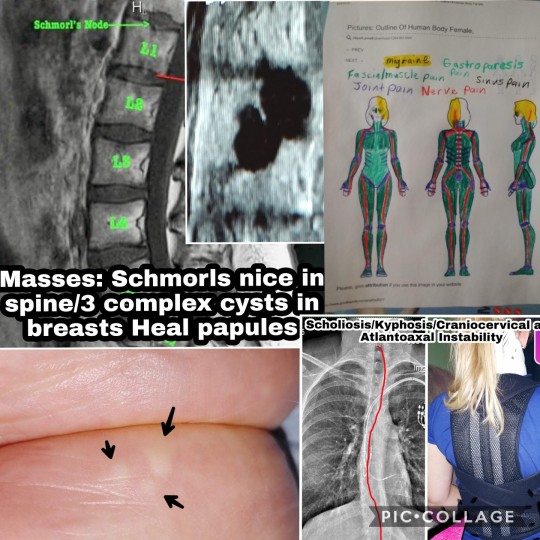
2021 Ehlers Danlos Society Awareness Month (Day 3 Prompt: Symptoms)
Unbeknownst to most people in the community and even many in the medical community as most medical personnel never learned about EDS in school or if they have were only taught the very most basic information about it but Ehlers Danlos Syndrome is a systemic condition and predisposes those with it to over 250 other conditions so it's not unusual for someone with EDS to have 20, 30 or even more other conditions caused by it which are called comorbid conditions or comorbidities.

EDS is a genetic condition that affects the structure of connective tissue. There are multiple types of connective tissue but there are also multiple types of EDS so one or more types of connective tissue can be impacted. Connective tissue also makes up at least part of every part of the body so when your connective tissue is faulty and prone to damage that also means so is everywhere connective tissue is located including but not limited to the skin, cartilage, the brain, heart, lungs, GI system, liver, kidneys, bladder, Mesentery system which is the stringy organ that is around your abdominal organs that eases then and holds them in place, lymph nodes, lymph ducts, nerves, blood vessels, blood cells, nerves, bones, bone marrow, joints, tendons, ligaments, muscle sheathing, eyes, ears, nails, hair follicles, spinal cord, sweat glands, respiratory system etc. You name it, it contains connective tissue so anything can go wrong with any part of the body leaving many patients diagnosed with conditions such as conversion disorder, meaning that all of your symptoms are in your head and you're fine for years and more often, decades because we usually get diagnosed with a lot of these comorbidities before we finally find that one doctor who can put the pieces together and say, this isn't in your head, you have Ehlers Danlos Syndrome and those other conditions are very real because EDS is what caused all of them.

Now that we have discussed comorbidities I have dealt with countless symptoms over my life. As a kid it started with chronic pain, migraine headaches, and issues resulting from a compromised immune system because I caught everything going around and usually more than once. I don't remember a holiday as a kid where I wasn't sick or hurt. I was extremely clumsy, unable to run correctly until high-school with the very extensive help of my gym teacher. I was always falling, rolling my ankle, and just in general looking awkward with my body movements. I had multiple gym teachers who would agree that there was something physically wrong with me long before I could get any doctors to listen to my mom or as an adult, myself. I had to take special reading and writing classes because even to this day I cannot hold a pencil well or write with control because my fingers are too hypermobile to control a pencil so my writing is often illegible. I had a very severe failure to thrive, also called juvenile dwarfism, not even growing an inch between the ages of 2 and 12. My parents were told when I was 2 years old that I would be 6’4’’because I was so tall as at one and two years old that people would criticize my mom for carrying me out in public thinking I was 4 or 5 years old when I was only a year or two years old. I was 3’2” from the age of 2 to the age of 12 and of course when I was 12 I was extremely short and was bullied for my size as well as my weight which increased due to inflammation from undiagnosed celiac disease. There were multiple incidences with medical personnel and social workers as a kid because I always had such severe bruising all over my body and they believed I was abused. I didn't lose my teeth, losing only one on my own and at the age of 8 my dentist began pulling out my teeth which left me with dental crowding and requiring braces which were removed prematurely. I dealt with Learning disabilities and have been in glasses since age 4. I would pass out all the time as a kid, starting at 8 years old.

Bullying was a huge issue for me as a kid because I was socially awkward showing signs of OCD as well as being more mature than my peers due to my medical experiences and history with my siblings that forced me to grow up more quickly. That combined with issues such as my clumsiness and height made me the perfect target for bullying. I got what I believe was my first Traumatic Brain Injury when I was 9 years old while hanging upside down on the monkey bars. My bully had another student who had Down Syndrome, climb to the top of the monkey bars and lift my legs so I fell off onto my head.
My second was in the 6th grade. The same bully would bully other kids to help her bully a bigger target of hers which was me. One day I was at my locker between classes. Our lockers were assigned in alphabetical order by last name, of course my bully's last name came right before mine so her locker was directly to the left of mine. My mom tried to get it changed but the school refused. She shoved me down between classes while I was exchanging my books and the two kids with the locker to the right of mine she had help her roll me onto my stomach on the ground, one sat on my butt and held my feet down, the other sat on my back and held my arms down under her feet. my bully yanked my head up so my forehead was on the floor of my locker and I was trying to get out so she had the girl on my back use one of her hands to hold my head down. My bully then kicked my locker door shut on my head over and over again and I went unconscious. There were two teachers in the hall at the time but they just waked into the classroom when it started. I woke up and the hall was empty. I went to the office and told them I needed them to call my mom, I needed to go home and explained what happened. They called my mom and instead of telling her the truth they told her she needed to pick me up because I was acting strange. She came and got me and found out what happened getting me treatment.

She then took me to the school a few days later since the doctor didn't want me to return for so long (I apologize I don't remember a lot from the two weeks following this so I'm going off what I was told so the exact time I was out of school, I believe was around two weeks but I'm not sure. Anyhow at the school, we met with the principal and office staff who denied any teachers were in the hall or that any of this happened. My mom demanded to see the recordings on the cameras as a hall came in at a T right behind my locker so that camera faced my locker as well as one at each end of the hall my locker was in. They tried to tell her all three cameras were broken. My mom wasn't buying it so they tried then saying the recordings were gone. they went round and round and the school flat out refused to show her the video. My mom demanded that the girl who did this be punished because she has been asking for the school to help me since I was in the first grade and this girl started bullying me but they always fail to do anything.
They tried to then give me an in school suspension which my mom refused to let them do. They still went behind her back when I returned and made me take peanut butter sandwiches to the kids in detention during my lunch as punishment because they were mad my mom came in to question the incident. They refused to punish my bully in any way and when my mom demanded to know why, they said her mom and grandmother graduated from the school so she has a lot of history with the school which years later we found out after me and 9 other kids that I know of and who knows how many others, ended up being pulled out of the same school because of her bullying that having history at the school actually turned out to mean, she was black and they would not punish her because of her color. At the end of the school year my mom pulled me out of the school not sure what to do since back then they didn't have any kind of free online schooling so pretty much everything costed money which is when my grandma stepped up and told my mom she would help because there was no way I would be going back to deal with more bullying.
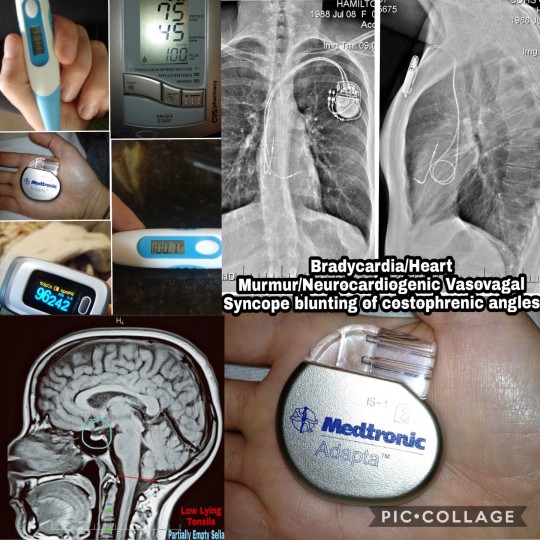
I had a ton of intestinal issues having to start colonics at around 10 years old and get my first colonoscopy around the same time. As a teen I really went down hill, struggling to eat because I had very severe nausea and cramping pain upon eating which made many of my friends believe I was anorexic but I went years without being diagnosed with gastroparesis. I started having thyroid issues and finally diagnosed with food allergies at age 14, Chest pain, palpitations, arrhythmias and trouble breathing around age 15 and seizures and cardiac arrest events at age 17.
At age 19, right before starting college I lost the ability to walk with no reason why and was sent to physical therapy to learn to walk again. The hospital visits continued in college from the seizures, emergencies from my thyroid levels going sky high or bottoming out, I started having issues with low sugar, rectal bleeding and more GI and Muscular Skeletal issues that again came to the attention of a physical education professor I had in college. The cardiac arrests continued to happen and I got an emergency pacemaker put in at age 23. Also lost the ability to walk a second time and re learned during this time.

After graduating and starting working I really went down hill. My nerve pain got so bad I could hardly tolerate it and had a lot of issues with muscle spasticity. Passing out and dizzy spells got worse, seizure meds aren't working muscle weakness got again worse in my legs and I started literally wondering if I was dying, I had such severe fatigue that I slept every moment I wasn't working, bleed very badly during my period or with just mild trauma worrying my dentist so badly that he sent a letter to my doctor suggesting a possible bleeding disorder. I was going into shakes from low sugar and low sodium frequently but at the time had no idea why I would start shaking multiple times a day. Myoclonic epilepsy started and has progressively gotten worse, Dystonia started up, I started getting intestinal obstructions more often and more gastroparesis symptoms with the nausea and vomiting, sometimes cyclic vomiting. I developed a limp and went onto forearm crutches which eventually progressed to paralysis.
I have always had issues with dislocations of joints and spinal manifestations like scoliosis, Craniocervical and Atlantoaxial instability. I’m prone to non cancerous masses that could be cancerous one day including masses in my breasts, heals and between the vertebrates in my spine. My memory has deteriorated and I now have issues which I call temporary blindness when I turn my head a certain way which pinches my already compressed brainstem kinking it off so my vision is interrupted. With Systemic Mastocitosis I deal with allergic reaction type symptoms such as anaphylaxis, overproduction of mucus, coughing, hives, swelling, rashes, itching, hot flashes, flushing and more. I overheat and have hyperhidrosis. I have muscle spasms from the paralysis, dry mouth from the meds, in addition to the heart arrhythmias and trouble controlling my body temperature from the damage to my autonomic nervous system failure I have swelling of my abdomen, extreme thirst, bladder retention, abdominal cramping and more.

There are endless symptoms associated with EDS and it’s comorbidities which has a huge impact on your social life. You can't do the things you used to do and may come up with new hobbies and later deal with the grief associated with losing the ability to do those hobbies, in turn having to find new hobbies. You lose all or almost all of your friends because they don't like what you have become, the things you used to be able to do with them and no longer can, they don't understand if you need to cancel plans, when you lose the ability to drive they drop you cold because they don't want to pick you up many of us deal with the realization of how badly we wanted friends growing up due to our social awkwardness that resulted from our illness, time spent in the hospital, maturing more quickly, as well as the result of decades of medical abuse and neglect which in most of us has resulted in complex PTSD.
Almost all EDS patients are either on the Autism Spectrum, diagnosed with Obsessive Compulsive Disorder which some associate with social awkwardness and also the intense need for us to please people meaning many EDS patients were known as extremely hard and dedicated workers when working or in school as well as very dedicated to friends and families. We basically give our friends the clothes off of our backs meaning that most of us unknowingly befriend people who use us and are in take take take relationships where we give everything we have into a friendship or relationship while the other person gives little back resulting in most of us losing all or almost every friend we had when we get sick and no longer have anything to give. When we are no longer able to do for others those people quickly jump ship leaving us with no friends. Most of us have this very similar personality type due to our history of growing up quickly along with the shared comorbidity of Autism, OCD, and Complex PTSD.

There are countless symptoms associated with EDS and they are different for each individual. Even in my case alone these are only the tip of the iceberg when it comes to symptoms I have experienced alone so EDS isn't an easy condition to live with physically or emotionally and the diagnosis can be quite the pill to swallow with little understanding from friends, sometimes family or even the medical community.
2 notes
·
View notes
Text
Health Benefits of Date Palms.
Dates have an excellent nutrition profile, High in Fiber. They are high in several nutrients, fiber and antioxidants, all of which may provide health benefits ranging from improved digestion to a reduced risk of disease. There are several ways to add dates to your diet. One popular way to eat them is as a natural sweetener in various dishes. They also make a great snack.
You can eat dates at any time of the day without any digestive issues. They also make for an energy-rich snack that will keep you full and satisfied but you should eat 4-6 dates daily if you're trying to lose weight. You can have them along with a cup of black coffee in the morning and then again in the evening with a cup of milk tea or green tea.

Benefits of Dates:
1. Dates are Highly Nutritious.
2. Aids Healthy Bowel Movements.
3. High Concentration of Anti-oxidants.
4. Improves Brain Functionality.
5. Facilitates Natural Labour.
6. Reduces Risk of Cancer.
7. Prevents Microbial Infections.
8. Helps Fight Diabetes.
Avoid or refrain from having water after eating fruits because it hinders the absorption and digestion process in the stomach leading to acidity. This is why some people experience uneasiness after consuming fruit. It is recommended that you have water at least an hour after you eat fruits.
Dates are rich in iron and dietary fiber, but eating a lot of them will lead to weight gain as 70 per cent of their weight comes from sugar, reports sfgate.com. CalorieKing suggests that there are 66 calories in a single date, so avoid eating a bunch of them if you're trying to lose weight.
Dates are a naturally sweet snack that packs seven grams of fiber. Not only can their high fiber level help you poop, but it can also keep your blood sugar under control. Dates can be used in desserts to replace some of the recipe's sugar or enjoyed on their own.
A study in the support of dates as anti-inflammatory showed that the leaves of dates can be considered as a good source of natural antioxidant and anti-inflammation drugs.
Dates have a low GI, which means they're less likely to spike your blood sugar levels, making them a safe choice for people with diabetes. Moreover, dates have a medium GL, which means that 1 or 2 fruits at a time are a good choice.
Dates are an excellent source of vitamin C and D which helps to maintain your skin elasticity and keeps your skin smooth. Dates also come with anti-ageing properties and prevent the accumulation of melanin.
The side effects of consuming dates include: Weight gain: Dates, when consumed in excess, can lead to weight gain due to high caloric content. So, it is essential to consume dates in moderation. Kidney disease: Individuals with kidney disease should follow caution while having dates.
When you have high blood pressure, make sure you eat sufficient fruits and vegetables as they are rich in potassium. For vegetables, you could choose peas, greens, tomatoes, spinach and potatoes. Fruits such as bananas and oranges and dried fruits such as raisins, apricots, prunes and dates are also high in potassium.
From helping in killing intestinal worms, to cleansing the vital organs and improving heart and liver health, dates should best be eaten early in the morning to benefit from their much needed boost of energy.
Dried fruits, such as dates, figs, prunes, apricots, and raisins, are another great source of dietary fiber that acts as constipation relief. Prunes, in particular, are great because they not only are high in fiber, they also contain sorbitol, which is a natural laxative.
2 notes
·
View notes
Text
Spirulina

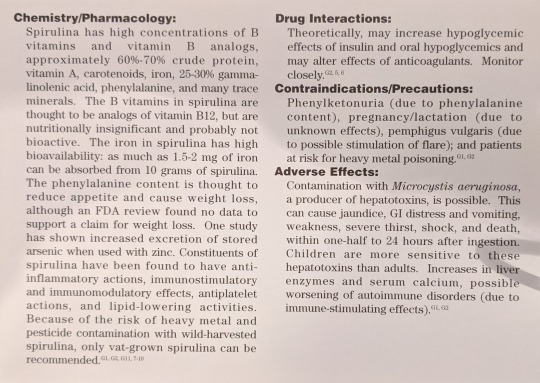
Scientific Names: Microcystis aeruginosa, M. wesenbergii, and other Microcystis species, Spirulina maxima, S. platensis, and other Spirulina species; Anabaena species; Lyngbya wollei; Aphanizomenon flos-aquae Other Common Names: AFA, BGA, blue green algae, cyanobacteria, Klamath blue/green algae Overall Safety: 😐
Therapeutic Efficacy and Considerations:
Bronchial Asthma: 🙁 The one small trial conducted demonstrated no difference from placebo. Spirulina is not recommended for this indication.
Oral Leukoplakia: 😊 Due to spirulina’s high carotenoids (found to have benefit in healing precancerous lesions) content, a trial examined efficacy of S. fusiformis for treatment of leukopenia and demonstrated complete regression of homogenous lesions in 57% of patients. Because this precancerous condition requires close monitoring and treatment, it is recommended that spirulina not be used as monotherapy, but only as an adjunct to conventional treatments under a healthcare provider’s supervision. Dose: no more than 1 gm/day.
Kidney Disease-Associated Hyperlipidemia: 😐 Although preliminary evidence demonstrates that spirulina may have effects to lower cholesterol in patients with patients with kidney disease, at this time evidence is not sufficient to recommend use for this indication. Dose: 1-5 gm per day.
Hyperlipidemia and Hyperglycemia Associated with Type II Diabetes: 😐 Small, preliminary trials demonstrate that spirulina may have benefit in lowering cholesterol and fasting blood sugar. At this time, evidence is not sufficient to recommend use. Dose: no more than 1 gm BID.
Note: In general, although in vitro and preliminary tests have found many beneficial activities, spirulina can, with the possible exception of prevention of leukopenia progression, be considered to be a very expensive source of trace minerals. Patients who wish to take spirulina because of its gamma-linolenic acid (GLA) content, should be directed toward less expensive sources, such as evening primrose oil.
Chemistry/Pharmacology: Spirulina has high concentrations of B vitamins and vitamin B analogs, approximately 60-70% crude protein, vitamin A, carotenoids, iron, 25-30% gamma-linolenic acid, phenylalanine, and many trace minerals. The B vitamins in spirulina are thought to be analogs of vitamin B12, but are nutritionally insignificant and probably not bioactive. The iron in spirulina has high bioavailability: as much as 1.5-2 mg of iron can be absorbed from 10 grams of spirulina. The phenylalanine content is thought to reduce appetite and cause weight loss, although an FDA review found no data to support a claim for weight loss. One study has shown increased excretion of stored arsenic when used with zinc. Constituents of spirulina have been found to have anti-inflammatory actions, immunostimulatory and immunomodulatory effects, antiplatelet actions, and lipid-lowering activities. Because of the risk of heavy metal and pesticide contamination with wild-harvested spirulina, only vat-grown spirulina can be recommended.
Drug Interactions: Theoretically, may increase hypoglycemic effects of insulin and oral hypoglycemics and may alter effects of anticoagulants. Monitor closely.
Contraindications/Precautions: Phenylketonuria (due to phenylalanine content), pregnancy/lactation (due to unknown effects), pemphigus vulgaris (due to possible stimulation of flare); and patients at risk of heavy metal poisoning.
Adverse Effects: Contamination with Microcystis aeruginosa, a producer of hepatotoxins, is possible. This can cause jaundice, GI distress and vomiting, weakness, severe thirst, shock, and death, within one-half-24 hours after ingestion. Children are more sensitive to these hepatotoxins than adults. Increases in lever enzymes and serum calcium, possible worsening of autoimmune disorders (due to immune-stimulating effects).
#sigler dietary supplement drug cards#2nd edition#spirulina#microcystis aeruginosa#microcystis wesenbergii#spirulina maxima#spirulina platensis#anabaena species#lynbya wollei#aphanizomenon flos-aquae#afa#bga#blue green algea#cyanobacteria#klamath blue/green algea#drug facts
2 notes
·
View notes
Text
Anion gap, alk/acidosis, lipase, A1C, UUN, labs, specialized labs, clinical presentation, BUN, Creatinine
Anion gap (will cover this in more depth with diabetes) is calculated from sodium level – (chloride + bicarbonate). You could do (sodium + potassium) – (chloride + bicarbonate). Potassium contributes so little that it’s often omitted, however. Anion gap means something else is contributing to the acid-base balance, not just the exchange of chloride for bicarbonate, for example.
Metabolic acidosis: Low pH, a low HCO3- concentration. Compensatory hyperventilation that contributes to a decreased pCO2. Most common causes: Inability of kidneys to excrete dietary hydrogen ion load, increase in hydrogen ion generation due to an addition of hydrogen ions or a loss of bicarbonate
Metabolic alkalosis: High pH, a high bicarbonate- concentration, and compensatory hypoventilation that contributes to an increased pCO2. Most common causes: loss of gastric acid from vomiting or nasogastric suction, loss of intravascular volume and chloride from diuretic use. Overtreatment of metabolic acidosis with bicarbonate. Excess of acetate in PN (parenteral nutrition), which becomes metabolized to bicarbonate
A1C distinguishes between diabetes and hyperglycemia associated with metabolic stress
Protein: Again:
First start by converting the protein intake of the patient (94g in this example) to grams of nitrogen. Second, calculate their nitrogen balance. We find that the patient is in negative nitrogen balance. Nitrogen balance should be the same amount of nitrogen coming into the body as is coming out in the urine. Third: Correct the deficit to get into nitrogen balance. Take that -2g of deficit that they are at (take the minus sign away), and multiply that by 6.25g of protein (1g of nitrogen = 6.25g of protein). Correcting the deficit of nitrogen finds that the patient will require 12.5 more grams of protein just to get into nitrogen balance. Fourth, we still need the patient to be in positive nitrogen balance, so, we increase protein and shoot for 2g more protein to promote anabolism (goal for anabolism is +2-4g of nitrogen a day more). So, that low end we are aiming for is 2g of nitrogen: 2N (6.25g of protein/1g of nitrogen) = 12.5g of protein needed to put the patient in positive nitrogen balance. Fifth, we want to try to promote anabolism, so we have to add the amount of protein that puts the patient at nitrogen balance to the amount of protein that puts the patient in positive nitrogen balance, and add the sum of those two to the amount of protein the patient is taking in (the 94g). Hence the new protein goal is 94g + 12.5g + 12.5g = 119g of protein/day or approximately 120g of protein per day.
Remember: even though you prescribed 100g of protein a day, the patient only actually got 94g. So, that’s why you use 94g in these calculations.
A valid 24-hour urine collection can be difficult to collect
Conversion factor of UUN to total nitrogen excretion may not be accurate in certain conditions: burns, major wounds, diarrhea, vomiting
Factor of 0.85 converts UUN to TUN
Assumes that 85% of urinary nitrogen is from urea
Other nitrogen sources in urine= ammonia, proteins
Conditions that alter or increase ammonia excretion will lead to underestimation
Ex if Adam had liver disease and ammonia excretion was higher/ UUN only 75%
◦ UUN = 13 (13/0.75) = 17 (vs 15)
Diminished renal function alters results
For the most part you are addressing whether the patient is renal insufficient or dehydrated. BUN:Cre ratio, if high BUN and Cre is normal, then it's usually dehydration. If the BUN and Cre are high, it's often renal failure.
LABS:
K+, Cr, and Phosphate are often looked at when assessing kidney function. K+, Mg2+, phosphate are often looked at together as well
Refeeding syndrome (hemodilution, hemodynamics) is indicated by labs. Lab error (e.g. blood that has been sitting out too long, things degrade), stress impacts labs, components of the blood (e.g. serum iron) need to be looked at with other portions of bloodwork. Disease states affect labs. High blood glucose can begin to displace sodium, causing sodium to appear low (false low result), like in diabetic ketoacidosis.
• Think about which labs are affected by which organ system
• Lungs: chloride, acetate
• Kidneys: BUN, creatinine, potassium, phosphorus, albumin, calcium
• Heart: Sodium, BUN (volume status)
• Pancreas: Blood glucose, serum lipase
• Liver: Liver function tests
• Liver disease: colloidal pressure AKA oncotic pressure. With liver disease, you’re not going to make as much visceral proteins (like albumin), which hang onto the water portion of the blood. If albumin is not hanging on, it will start to seep out and accumulate in different places (third spacing).
• Pleural effusions are seen commonly in malignancy. Ascites from cancer, for example. Just because patient doesn't have liver disease doesn't mean they won't have issues with fluid. Extra fluid creates a dilution efffect (causing sodium and albumin, calcium, etc. appear low. If you take those labs at face value, you can be thrown off.
Liver disease: colloidal pressure AKA oncotic pressure. With liver disease, you’re not going to make as much visceral proteins (like albumin), which hang onto the water portion of the blood. If albumin is not hanging on, it will start to seep out and accumulate in different places (third spacing).
Pleural effusions are seen commonly in malignancy. Ascites from cancer, for example. Just because patient doesn't have liver disease doesn't mean they won't have issues with fluid. Extra fluid creates a dilution effect (causing sodium and albumin, calcium, etc. appear low. If you take those labs at face value, you can be thrown off.
Serum sodium doesn't really relate to dietary sodium. Serum sodium is a marker of fluid status, because salt is like a sponge and pulls in a lot of fluid. So, if sodium is really low, often times there’s a fluid issue going on. High sodium indicates a fluid deficit.
• Potassium: 3.4– 5.1 mmol/L
• Magnesium: 1.7 – 2.6 mg/dL
• Low magnesium can make it difficult to successfully replete potassium and phosphorus (SO YOU WANT TO MAKE SURE MAGNESIUM IS NORMAL)
• Phosphorus: 2.4 – 4.3 mg/dL
Story: Patient with a phosphorus of 7 starting nutrition at a slow rate, but then his team gave him a bunch of dextrose-containing fluids to correct a sodium issue, and his phosphorus then dipped to a 2! This results from massive refeeding. The trends in your potassium, magnesium, phosphorus are important. What essentially happened was that the glucose (dextrose) activated insulin, and insulin activation caused a massive shift intracellularly of phosphorus, leading to lower levels of phosphorus in the blood. When not eating much, your cells aren’t taking in magnesium and phosphorus, etc. So, again, sugar stimulates intracellular shift because insulin will activate when sugar is reintroduced, leading to even lower blood levels of minerals. Your heart won’t have enough potassium to beat properly, your lungs won’t have enough phosphorus to breathe well. Certain diuretics can lead to potassium deficiency, E.g. thiamin follows potassium (Wernicke's Encephalopathy), certain diuretics that are potassium wasting come with a risk of thiamin deficiency. Can fix this by prophylactically give thiamin in anticipation of potassium drop.
CONSEQUENCES OF REPLETING TOO QUICKLY
• Low potassium: cardiac arrhythmia, cardiac arrest
• Low magnesium: seizure, coma
• Low phosphorus: respiratory distress, difficulty breathing/getting off mechanical ventilation
Patients who are at risk for refeeding syndrome can have a number of different conditions to begin with:
• Anorexia nervosa
• Chronic alcoholism
• Cancer
• Post-surgery (NPO for many days pre- and post-op)
• Elderly (poor dentition, reduced thirst/taste sensation)
• Uncontrolled diabetes mellitus (electrolyte abnormalities, polyuria)
• Critically ill and unfed for >7 days
• Inflammatory bowel disease, chronic pancreatitis, short bowel syndrome
• Cystic fibrosis
• Long-term antacid use (phosphorus levels are often low 2/2 magnesium and aluminum salts in the medications)
• Long term diuretic use (potassium-wasting) such as with CHF
• Patients who are vomiting frequently
Patients with poor blood levels at baseline (K/Mg/P) will be at risk of intracellular shifts and thus lower blood lab values. Patients with SBD have reduced absorptive capacity, for example, and are at risk for refeeding syndrome.
• When a patient is experiencing hyperkalemia (K+ > 5.1 mmol/L), there are a number of treatments a Team may utilize
• 50% Dextrose ampule + Insulin
• Calcium Gluconate
• Kayexalate or Lokelma
• Why would we use these medications? (insulin will stimulate intracellular K+ shift, Lokelma and Kayexalate bind potassium)
Giving dextrose and insulin mimics refeeding. So, you are pulling potassium out of the blood and giving it to the cells.
Giving dextrose and insulin mimics refeeding. So, you are pulling potassium out of the blood and giving it to the cells. With renal patients who are often in a hyperkalemic state, kayexalate and lokelma will stop potassium absorption in GI tract. When someone’s potassium hits the ceiling, arrhythmia can occur. Calcium is given to offset that. If a pt is hyperkalemic and EKG changes are seen, patient is given 2g of calcium. Calcium gluconate is the preferred IV administration for hypocalcemia (Severe symptomatic hypocalcemia should be corrected promptly with IV administration of calcium gluconate over 10 minutes to control symptoms. Calcium gluconate is the preferred salt for peripheral venous administration to avoid extravasation—leakage of liquid into surrounding tissue.)
Specialized labs: Liver function tests give you enzymes (alanine aminotransferase and aspartate aminotransferase, ALT and AST) and you are also given bilirubin as s measure of liver function, as bilirubin is a waste product of heme metabolism. When liver is not functioning well, bilirubin won't be cleared well. At that point, liver is also not good at clearing minerals such as copper and manganese.
Liver function tests give you enzymes (alanine aminotransferase and aspartate aminotransferase, ALT and AST) and you are also given bilirubin as s measure of liver function, as bilirubin is a waste product of heme metabolism. When liver is not functioning well, bilirubin won't be cleared well. At that point, liver is also not good at clearing minerals such as copper and manganese.
When T. bili is >5 mg/dL, give PO multivitamin without minerals, or remove copper and manganese from your TPN (total parenteral nutrition) solution
If patient is eating, give them a multivitamin without minerals. If patient is on TPN, remove copper and manganese, as toxicity of these can risk brain damage.
Blood and iron studies: Hemoglobin is the last thing to change. Look at ferritin as an earlier sign. Hematocrit can respond to anemia, but also to an overflow of other blood cells. Professor Trussler works with blood in the heme oncology setting. White blood cells in certain type of malignancies (e.g. leukemia) are elevated. Blood smear can count white blood cells and immature white blood cells (blasts). High blasts signals that something is wrong in bone marrow and they’re pumping a lot of immature white blood cells out. Also, immature blasts are a measure of whether someone’s chemotherapy has been effective. Treatment decisions can be made on this.
Absolute number of neutrophils can be used to determine treatment decisions. Low neutrophil count can be used as a guideline for a neutropenic (low bacteria) diet.
A1C: 3-month average blood glucose. When someone is acutely ill, you can see high glucose in the blood, but this is not diabetes, it’s “stress hyperglycemia” (due to injury). But if this is prolonged, an A1C can help you see if they have undiagnosed prediabetes. A1C is useful for newly diagnosed diabetic patients.
Lipase: You shouldn't be seeing a lot of lipase in the bloodstream, as this indicates pancreatic damage (e.g. pancreatitis)
Vitamin and mineral labs get expensive, so you don't want to be checking EVERYTHING for every situation. There are some vitamins and minerals where a serum lab isn't going to be helpful. E.g. pyridoxine (B6), Per the American Society of Parenteral and Enteral Nutrition (A.S.P.E.N.), you need serum B6, 24-urinary B6, erythrocyte AST, and erythrocyte ALT to assess sufficiency of B6.
Common vitamin labs:
· Someone who is having trouble absorbing fat will be at risk for vitamin A deficiency. Vitamin A is key to skin integrity and building (a pressure injury/injuries not healing well may indicate vitamin A deficiency), with substance use disorder deficiency comes up because you’re generating a lot of free radical damage from substance use disorders and the vitamin A is getting used up for that. Vitamin A is protein bound (RBP), so you can look at C-reactive protein in combination with this, because vitamin A may look low when it's not (falsely low result).
· B12 is worth looking at, esp. for vegans, vegetarians, elderly, heavy alcohol or substance users, and patients with IBD.
· Vitamin C builds collagen matrix for skin, thus wounds could cause a vitamin C deficiency in wound patients. Dialysis causes water loss, so you can lose vitamin C. COVID-19 may cause a vitamin C deficiency (the antioxidant vitamin is getting used up).
· Check vitamin D, after it's activated by the kidneys a second time, that active form doesn't last very long, so it may not give you a good result. Vitamin D labs are good to check for elderly patients who don’t synthesize enough vitamin D, and for kidney injury patients because their kidneys aren’t activating as much vitamin D. Checking vitamin D for oncology patients is also great, because they may have some complications in certain cancer treatments. COVID-19 appears to be affecting vitamin D levels.
· Vitamin E is good to check in a patient who is malabsorbing fat. If you think someone is malabsorbing, the team can do more work up.
Less common vitamin labs:
If the vitamin is water soluble, there’s less risk of toxicity, so you can give it prophylactically. For example, folate costs about $1, so it can be given for 3 days prophylactically.
B1 (thiamin) is given prophylactically if you think the patient is deficient. At Brigham and Women’s, if you anticipate that someone might refeed, you give them thiamin for the first few days that they’re getting nutrition support to anticipate that shift with potassium.
Professor T doesn’t usually check vitamin K often, because gut microbiota make vitamin K. Prothrombin (PT-INR, a marker of blood clotting) is a better indicator of vitamin K sufficiency because the clotting factors in your blood need vitamin K to work. If you were truly functionally deficient, you would have trouble clotting.
Common mineral labs
Both copper and ceruloplasmin must be low in order to diagnose a true copper deficiency. Bariatric patients tend to be low, esp. in Roux-en-Y gastric bypass patients, as the surgery is bypassing some of the areas where copper is absorbed. Wouldn't normally suspect a copper deficiency unless there's some sort of malabsorptive process occurring.
Zinc deficiency is caused by (and can also cause) diarrhea. If you have someone with diarrhea that isn’t resolving, it could be due to zinc deficiency, and also zinc could be causing the diarrhea. Zinc is lower in stressed state. If a patient is borderline deficient and their CRP is very high, you may want to hold off on repleting zinc, and then check zinc levels again.
Selenium, like zinc, decreases when someone has diarrhea, but can also cause diarrhea as a side effect of deficiency. Selenium will be low in substance use disorder patients, as it participates in antioxidant functioning (where antioxidants get used up).
Less common mineral labs:
Manganese: No good lab test to measure for this. If worried patient is getting too much, try to just remove it. E.g. taking manganese out of total parenteral nutrition, or giving a supplement that doesn’t have manganese. Manganese toxicity can cause brain damage
Chromium: No real lab measure for chromium, either, but people on long term TPN might develop this deficiency. Sometimes chromium is given prophylactically. People who are diabetic can be low in chromium, but it is difficult to figure out because you can’t check this mineral.
Specialty Lab
• Fecal Calprotectin
• Marker of inflammatory bowel disease
• Protein released by immune cells (neutrophils) at sites of inflammation in the GI tract, which is then excreted in the stool
• Low level (10-50 mcg/mg): likely IBS or viral infection
• Moderate level (>50 mcg/mg): potential IBD flare or worsening inflammatory condition such as parasitic infection
#anion gap#alkalosis#acidosis#lipase#A1C#UUN#labs#specialized labs#clinical#BUN#creatinine#dietetics#Medical Nutrition Therapy
2 notes
·
View notes
Text
Going through questions:
The most common pediatric leukemia is acute lymphoblastic leukemia (ALL). T cell or B cell ALL can occur. In T cell ALL, mediastinal masses occur.
Non-Hodgkin lymphoma causes B symptoms (weight loss, night sweats). Epstein Barr virus infects B cells and is associated with NHL. HIV infection is associated with NHL.
Multiple myeloma - plasma cell cancer-> monoclonal immunoglobulin (M-spike); presents with osteolytic lesions. Radiolucent bone lesions will be seen. Metastatic prostate cancer causes blastic bone lesions.
Bleeding time tells you about platelet defects. Von Willebrand disease-> prolonged bleeding time and PTT. vWF is needed for platelet adhesion and it is needed to stabilize factor 8. So No vWF-> no platelet adhesion (causing increased bleeding time) and unstable factor 8 (which is part of the intrinsic pathway, so increased PTT). I remembered that Von Willebrand's disease is the most common heritable bleeding disorder, which is why I got the question right. But now the increased bleeding time and PTT going with it make sense. It's AD.
Blood loss, not decreased nutritional intake, is the cause of iron deficiency anemia to rule out first in post-menopausal women. It could be an occult GI bleed.
LMWH binds to factor Xa and prevents it from converting prothrombin to thrombin. Unfractionated heparin can bind to factor Xa and to thrombin. So LMWH (e.g. enoxaparin) doesn't bind thrombin like unfractionated heparin does. LMWH is like heparin, but has fewer molecules than heparin.
Pyruvate kinase converts PEP to pyruvate in glycolysis. Pyruvate kinase deficiency-> hemolysis. Pts with pyruvate kinase deficiency have splenomegaly because cells in red pulp have more damaged RBCs to filter out.
I didn't know what a minor red blood cell antigen was. It's an antigen on the RBC that may not be screened for, thus a week later, pts have a reaction to it in delayed hemolytic transfusion reactions. He didn't mention this one in OnlineMedEd. The pt was initally exposed to the minor RBC antigen and developed memory B cells. The next time the pt is exposed, the B cells release antibodies (anamnestic response). Delayed hemolytic transfusion reaction occurs more than 24 hours after transfusion. Anamnestic response = delayed response
G6PD deficiency is X-linked recessive. I knew that's what the pt had in a question, but I forgot it's inheritance pattern. D: Heinz bodies are the hemoglobin that got damaged by oxidative stress because G6PD wasn't around to help regenerate the NADPH that is needed to make reduced glutathione, which prevents oxidative damage.
Herditary spherocytosis has AD inheritance pattern.
Schistocytes = hemlet cells. Thes occur in microangiopathic hemolytic anemia and in pts who have had heart valve surgery, which damages the RBCs. Artificial heart valves can damages RBCs-> schistocytes on blood smear. HUS, TTP, and DIC cause fibrin stands in small blood vessels-> schistocytes.
LMWH (e.g. enoxaparin) can be given for DVT in pregnant women. I remembered that heparin doesn't cross the placenta. But it is renally cleared, so if you have renal insufficiency (creatinine clearance less than 30 mL/min), then LMWH is contraindicated and you can give unfractionated heparin instead.
Azathioprine is a prodrug of 6-mercaptopurine. It gets metabolized by HGPRT into active 6-thioguanine, which is a purine analogue that disrupts DNA synthesis and thus prevents cell proliferation. 6MP is inactivated by xanthine oxidase and TPMT. Xanthine oxidase is inhibited by allopurinol and febuxostat. Some people have genetic deficiency of TPMT. If neither xanthine oxidase nor TPMT can inactivate 6MP, more of the 6MP gets converted to active 6-TG-> toxicity and increased immunosuppression. So some pts get genetic testing for TPMT before starting azathioprine and some pts need to avoid being on 6MP and allopurinol or febuxostat simultaneously.
Sickle cell is autosomal recessive, so you need 2 bad alleles to have it. If each parent is a carrier, then 1/4 kids will have it and 24 kids will be carriers. 1/4 kids will be normal. Glutamic acid (polar) is replaced by valine (non-polar) in sickle cell anemia. A point mutation in one of the codons for beta globin causes this substitution. This causes HbS.
One of my classmates mentioned rasburicase to me last year and I know it was between two answers in this question, but I chose the wrong one. D: It makes uric acid more soluble. In tumor lysis syndrome, more cells are being lysed by the chemotherapy. Since cells have high levels of K+ and phosphate, this can lead to hyperkalemia and hyperphosphatemia. Also, more protein needs to be broken down. Therefore, there's more purine catabolism. And purines end up as uric acid, which can precipitate in the kidneys and cause kidney injury. Rasburicase turns uric acid into allantoin, which is more soluble than uric acid and can be eliminated in the urine. Yeah, I remember my friend telling me that rasburicase is in certain animals. Rasburicase is recombinant urate oxidase. Animals have urate oxidase, but humans don't. So rasburicase turns uric acid into soluble allantoin, which is eliminated in urine. Allopurinol prevents formation of uric acid; it looks like purine and prevents xanthine oxidase from breaking down hypoxanthine. Febuxostat inhibits xanthine oxidase and has fewer adverse effects than allopurinol.
I didn't know heat stroke causes increased procoagulants. But it does and that leads to DIC due to increased coagulation factors; then you get increased fibrinolysis to get rid of the clots that form. Because the platelets and clotting factors all get used up, pts will bleed.
Multiple Myeloma = B cells become plasma cells that make a ton of useless immunoglobulin light chains. Treated with bortezomib, which causes increased apoptosis of plasma cells. Multiple myeloma causes lytic bone lesions, anemia, AKI, fatigue, constipation, weight loss. Myeloma kidney = light chain casts. Tons of kappa and lambda light chains being filtered by the kidney combine with Tam-Horsfall proteins (pretty sure I never heard of that) and cause casts that damage the tubules-> AKI. 24 hour rine protein is elevated.
Myeloma cells makes RANKL and destroy osteoprotegerin, which cause more activation of osteoclasts, hence the lytic bone lestions. I already reviewed RANK and RANKL and I know it pretty well. Glad I posted about it before. Multiple myeloma cells also release IL-3, IL-7, and Wnt pathway inhibitors, which inhibit osteoblasts.
I knew that this baby in this question had dactylitis, which occurs in sickle cell anemia, but I didn't understand what they were asking. If you have sickle cell, the sickled RBCs get destroyed, releasing hemoglobin. Hemoglobin is toxic and needs to be bound to haptoglobin. So the haptoglobin leven in the baby would be abnormal (decreased) because it would be all bound up by the Hgb coming from the hemolysis of the sickled RBCs. It had mentioned the baby's brother dying from an infection and I wasn't sure how that was related. It was because the brother also had sickle cell and therefore he probably had autosplenectomy due to the sickle cell. No spleen leaves you susceptible to encapsulated bugs like strep pneumo and the brother died from strep pneumo sepsis.
Hepcidin is an inflammatory mediator and it also decreases absorption of iron. So in anemia of chronic disease, hepcidin plays a role.
I knew this pt had beta thalassemia minor, I just didn't know what initiates it. It's a problem with mRNA. You see target cells and hypchromic, microcytic RBCs on blood smear. Pts have increased HbA2 (2 alpha chains and 2 delta chains; an alternate form of adult Hgb because they lack beta globin chains) and sometimes increased fetal Hgb (2 alpha chains and 2 gamma chains). If you try to treat these pts with iron, it doesn't do anything because they aren't iron deficient. Beta thalassemia is due to mutations that affect the transcription of mRNA for beta globin. Usually, there's messed up splicing of pre-mRNA or premature translation termination.
In obstructive sleep apnea, the kidney doesn't get enough oxygen, so it releases erythropoitein-> polycythemia (increased hematocrit).
Chemotherapy Induced Nausea and Vomiting (CINV) can be treated with 5HT3 receptor antagonists (ondansetron) and neurokinin-1 receptor antagonists (aprepitant). Early CINV is due to release of serotonin from enterochromaffin cells in the intestine that are damaged by the chemo. This leads to stimulation of 5HT3 vagal fibers-> vomiting reflex. Delayed CINV is due to substance P in the blood and CSF-> substance P binds neurokinin-1 receptor in the nucleus tractus solitarius and area postrema-> vomiting. Aprepitant can block the neurokinin-1 receptors and is therefore used for delayed CINV.
Low oxygen level leads to sickling of HgbS. High acid or dehydration also trigger the cycling. 2,3-BPG stabilizes the taut form of Hgb, which also would cause sickling. Low 2,3-BPG would increase Hgb's affinity for oxygen and thus decrease sickling. So high oxygen, high pH, and low levels of 2,3-BPG would prevent sickling. The opposite causes sickling. That's why pts with sickle cell anemia can't do as much strenuous activity--their HgbS starts sickling when they have less oxygen, more acid (from working muscles), and more need to unload oxygen to tissues (facilitated by 2,3-BPG) during exercise.
Fetal Hgb has replacement of histidine (positively charged amino acid) for serine, which is less positively charged. This prevents 2,3-BPG from binding for fetal hemoglobin, thus fetal hemoglobin has higher affinity for oxygen than adult hemoglobin. This helps baby take O2 from mom's hemoglobin in utero.
AML = Acute Myloid Leukemia = blasts (large nuclei, little cytoplasm) with Auer rods (rods seen in the blasts; not present in acute lymphoblastic leukemia, so look closeley to see if there are Auer rods--if there are, it's AML). Pts have pancytopenia. More than 20% myeloblasts in bone marrow. Chronic myelogenous leukemia = more mature cells.
Fluorescence In-Situ Hybridization (FISH) = cytogenetic test; finds deletions, translocations, and chromosome duplications in cells. FISH probes = ssDNA; they're added to the cell and combind with complementary DNA. FISH is more sensitive than karyotype.
Abixaban is a direct factor Xa inhibitor. It prevents conversion of factor II (prothrombin) to factor IIa (thrombin). I got the question wrong and so did 58% of respondents. It doesn't prevent conversion of factor X to Xa--it prevents factor Xa from converting prothrombin to thrombin. Wow. -_-
You need mitochondria to make heme. The precursors for RBCs have nuclei and mitochondria. After a certain division, they lose their nuclei, then they lose the mitochondria. So if they're at the point where they lack mitochondria, they can't make heme. Heme is made in the liver and in the erythrocyte precursors in the bone marrow.
Polycythemia can be relative (due to dehydration or diuresis), in which case plasma volume is decreased, but RBC mass, SaO2, and EPO levels are normal. Primary polycythemia = polycythemia vera; increased plasma volume, increased RBC mass, normal SaO2, and decreased EPO level. Secondary polycythemia can be physiologic or inappropriate. Physiologic = due to hypoxia; normal plasma volume, increased RBC mass, decreased SaO2, increased EPO level. Inappropriate = tumor that make EPO; normal plasma volume; increased RBC mass, normal SaO2, and increased EPO level.
Polycythemia vera = myeloproliferative disease of hematopoietic stem cells (HSC); mutation of JAK2 wherein valine is replaced with phenylalanine-> HSC are more sensitive to growth factor (EPO and thrombopoeitin, growth factors that stimulate erythrocyte and thrombocyte production). Pts can have itching after they shower due to release of histamine from basophils; plethora (red face), splenomegaly. Dx with low serum EPO and bone marrow study that shows the JAK2 mutation. Tx: phlebotomy.
I got confused about hepcidin. I know how it works and made a post about it before. I thought it came from the intestinal cells, but it doesn't. It comes from the liver and it can affect intestinal cells by preventing the absorption of iron from the gut. Hepatic parenchymal cells secrete hepcidin, which controls the storage and release of iron from other cells. Hepcidin is high when there's already enough serum iron. Hepcidin is also an acute phase reactant and is elevated during inflammation. Increased erythropoiesis and low oxygen lower hepcidin levels. Ferroportin-1 allows iron to come in on the basolateral side (the side of the intestinal cell that faces the blood) of intestinal cells. Ferroportin-1 is also located on macrophages. High serum iron or inflammation causes hepcidin to increase and hepcidin causes breakdown of ferroportin-1, preventing iron from coming into the blood. On the apical surface of intestinal cells (the side facing the gut lumen) is Divalent Metal Transporter-1 (DMT-1), which allows Fe2+ to be absorbed from the small intestine into the intestinal cell. Inside the enterocyte, the iron is either maintained inside ferritin, or it goes through ferroportin-1 into the blood, where transferrin binds to it and carries it to whatever cells have transferrin receptors, which allow the iron to be taken into said cell.
Nephrotic syndrome = loss of protein in urine; can lose anticoagulation factors, like antithrombin III in the urine-> hypercoagulable state-> renal vein thrombosis. Renal vein thrombosis-> hematuria, flank pain, increased LDH. So nephrotic syndrome is a hypercoagulable state.
Heparin is found in mast cells. LMWH enhances the effect of antithrombin III and inhibits factor Xa. Unfractionated heparin not only inhibits factor Xa, it also inhibits thrombin.
Ugh! There was a question about cancer and I knew breast cancer was more common in women but also knew that lung cancer has higher mortality. Most common cancers (by incidence) in women are breast, lung, and colorectal cancer. Breast cancer is more common in women, but not as deadly as lung cancer.
#B symptoms#oncology#ALL#non Hodgkin lymphoma#von willebrand disease#heparin#LMWH#anamnestic#anamnestic response#G6PD#hereditary spherocytosis#schistocytes#helmet cells#rasburicase#allantoin#multiple myeoloma#polycythemia#polycythemia vera#hepcidin#ferritin#transferrin#ferroportin#iron#cancer
5 notes
·
View notes