I AM NOT A DOCTOR. Fuck paying for shit. I am bad at taking pictures. Anyone posting comments about buying/selling drugs will have their comments removed and you will be blocked.
Don't wanna be here? Send us removal request.
Text
Pharmacology - Chapter 5 - Therapy for Viral Infections and Immunizations
Part One (Pages 1-10) Part Two (Pages 11-20) Part Three (Pages 21-30) Part Four (Pages 31-40) Part Five (Pages 41-46)
4 notes
·
View notes
Text
Pharmacology - Chapter 5 - Therapies for Viral Infection and Immunization
Part One Part Two Part Three Part Four
Transcription under the cut!


Immunization
Common Vaccines
Travel vaccines
Recommended when traveling from areas of low infection rates to areas of high infection rates
Given two or more weeks before travel to give the immune system time to mount sufficient response
Travel clinics may be located in clinics or pharmacies and provide immunizations and advice about what vaccines are necessary
Common side effects
Fever
Headache
Upset stomach
Local injection-site irritation
Mild skin rash
Irritability
Managing side effects
Acetaminophen for 24-48 hours after vaccine given
Caution and considerations
Patients to receive vaccine information sheet (VIS) and sign a consent form as required by law
Healthcare personnel trained in vaccine administration must be trained in CPR
Most vaccines are to be stored in the refrigerator or freezer with storage temperatures strictly followed
Must be used right away and not refrigerated again if warmed to room temperature
Must be used within minutes to hours if reconstituted
Advance mixing of vaccines not recommended
Vaccines not to be mixed in same syringe with other medications
Complementary and Alternative Therapy
Andrographis
May reduce symptom severity and duration of influenza if started within 36 to 48 hours
Side effects include chest discomfort, headache, nausea, rash
Colloidal silver
Used topically and orally for infections
Side effects include argyria, neurologic deficits, kidney damage
Elderberry
May be used for influenza when initiated within 48 hours of symptoms
Chapter Summary
Viruses replicate by using the host cell's metabolic processes
Antiherpes agents include acyclovir, famciclovir, valacyclovir, and valganciclovir
Anti-influenza agents include amatadine, oseltamivir, rimantadine, and zanamivir
HIV is a virus that converts its RNA into DNA and inserts the copy into the DNA of the host cell
The standard of care for HIV patients involves a combination of antiretroviral drugs
The CDC releases vaccination recommendations and schedules
1 note
·
View note
Text
Pharmacology - Chapter 5 - Therapies for Viral Infections and Immunizations

Part One Part Two Part Three Part Five
Transcription under the cut!

HIV/AIDS and Antiretroviral Agents
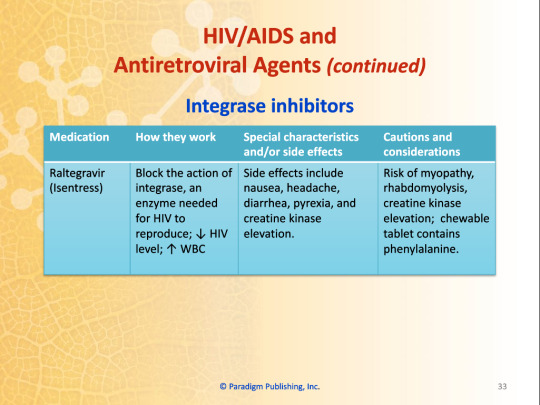
Integrase Inhibitors
Blocks the action of integrase, an enzyme needed for HIV to reproduce; decreased HIV level; increased WBC
Dolutegravir (Tivicay)
Believed to work better than other integrase inhibitors in viral resistance; side effects include elevated serum lipase, insomnia, elevated liver enzymes, hyperglycemia
Risk of fat redistribution and hypersensitivity reaction
Elvitagravir (Vitekta)
Side effects include depression, fatigue, insomnia, headache, diarrhea, abdominal pain
Risk of lactic acidosis, to be avoided in severe liver impairment
Raltegravir (Isentress)
Side effects include nausea, headache, diarrhea, pyrexia, and creatine kinase elevation
Risk of myopathy, rhabdomyolysis, creatine kinase elevation; chewable tablets contain phenylalanine
Work Wise
Raltegravir film-coated tablets and chewable tablets or oral suspensions are not bioequivalent. This means they cannot be substituted on a mg-for-mg basis.
Responding to Exposure to HIV
Healthcare worker risks
Exposure to blood and other bodily fluids
Needlestick injuries
Postexposure Prophylaxis (PEP)
Can decrease the risk of infection by 80%
Should start within 2 hours of exposure
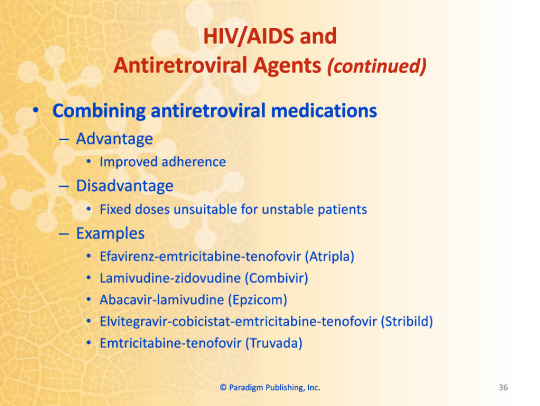
Combining Antiretroviral Medications
Advantage
Improved adherence
Disadvantage
Fixed doses unsuitable for unstable patients
Examples
Efavirenz-emtricitabine-tenofovir (Atripla)
Lamivudine-zidovudine (Combivir)
Abacavir-lamivudine (Epzicom)
Elvitegravir-cobicistat-emtricibine-tenofovir (Stribild)
Emtricitabine-tenofovir (Truvada)
Immunization
Immunization
The process whereby a person acquires immunity or resistance to an infectious disease
Methods of acquiring immunity
Passive immunity
Antibodies transferred to an individual
Occurs naturally during pregnancy
Occurs artificially through administration of immunoglobulin
Active immunity
Individual makes own antibodies
Occurs naturally following exposure to pathogens
Occurs artificially through vaccination
Live attenuated vaccines
Use live but weakened pathogens to induce an immune response
Inactivated vaccines
Use pathogens that have been killed
Pharm Facts
Community immunity describes a situation in which a sufficient proportion of a population has immunity to an infectious disease (usually through vaccination or prior exposure). Community immunity, in theory, makes it less likely for diseases to spread from person-to-person; this means that protection is extended to those within the community that do not have immunity. Another term for community immunity is herd immunity.
Immunization Schedule
Schedule source
Adults and childhood vaccination schedules are published by the CDC
Vaccines for children
Most lead to lifetime immunity
Boosters given for continued protection
Vaccines for healthcare workers
Hepatitis B vaccination and annual influenza vaccine often required by employers
Common Vaccines
Role of pharmacy technicians
Screen patients
Complete necessary forms
Stock and store vaccines
Draw up vaccine for pharmacist to administer
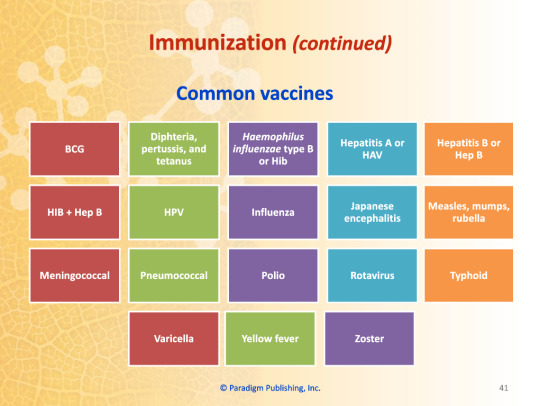
Common Vaccines
BCG
HIB+Hep B
Meningococcal
Varicella
Diphtheria, Pertussis, and Tetanus
HPV
Pneumococcal
Yellow Fever
Haemophilus influenzae type B (HiB)
Influenza
Polio
Zoster
Hepatitis A (HAV)
Japanese encephalitis
Rotavirus
Hepatitis B (Hep B)
Measles, Mumps, and Rubella
Typhoid
0 notes
Text
Pharmacology - Chapter 5 - Therapies for Viral Infections and Immunizations
Part One Part Two Part Four Part Five
Transcription under the cut!


HIV/AIDS and Antiretroviral Agents
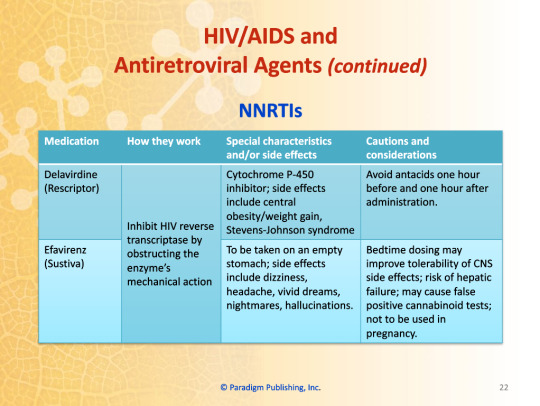
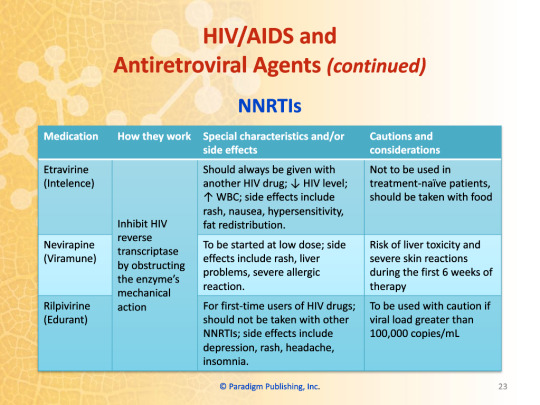
NNRTIs
Inhibits HIV reverse transcriptase by obstructing the enzyme's mechanical action
Delaviridine (Rescriptor)
Cytochrome P-450 inhibitor; side effects include central obesity/weight gain, Stevens-Johnson syndrome
Avoid antacids one hour before and one hour after administration
Efavirenz (Sustiva)
To be taken on an empty stomach; side effects include dizziness, headache, vivid dreams, nightmares, hallucinations
Bedtime dosing may improve tolerability of CNS side effects; risk of hepatic failure; may cause false-positive cannabinoid tests; not to be used in pregnancy
Etravirine (Intelence)
Should always be given with another HIV drug; decreased HIV level; increased WBC; side effects include rash, nausea, hypersensitivity, fat redistribution
Not to be used in treatment-naive patients, should be taken with food
Nevirapine (Viramune)
To be started at low dose; side effects include rash, liver problems, severe allergic reaction
Risk of liver toxicity and severe skin reaction during the first 6 weeks of therapy
Rilpivirine (Edurant)
For first-time users of HIV drugs; should not be taken with other NNRTIs; side effects include depression, rash, headache, insomnia
To be used with caution if viral load greater than 100,000 copies/mL
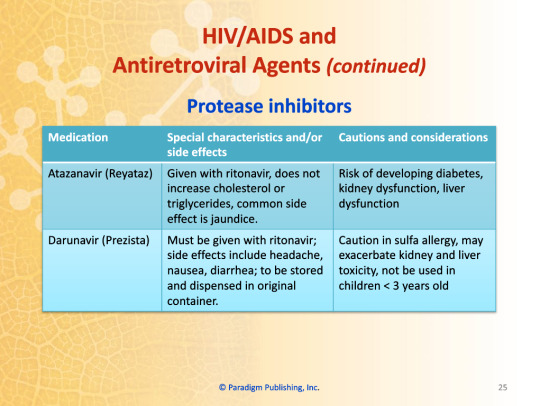
Protease Inhibitors
Decreases formation of protease enzyme, which cleaves certain HIV protein precursors necessary for the formation of new infectious virions
Typically combined with other HIV drugs; metabolized through cytochrome P-450 resulting in many drug interactions which are sometimes severe; not to be used with statins; side effects include redistribution of body fat, facial atrophy, breast enlargement, hyperglycemia, hyperlipidemia; possibility of increased bleeding episodes in patients with hemophilia.
Atazanavir (Reyataz)
Given with ritonavir; does not increase cholesterol or triglycerides, common side effect is jaundice
Risk of developing diabetes, kidney dysfunction, liver dysfunction
Darunavir (Prezista)
Must be given with ritonavir; side effects include headache, nausea, diarrhea; to be stored and dispensed in original container
Caution in sulfa allergy, may exacerbate kidney and liver toxicity, not to be used in children <3 years old
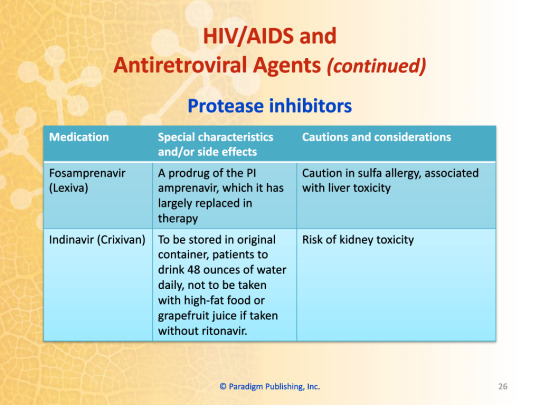
Fosamprenavir (Lexiva)
A prodrug of the PI amprenavir, which it has largely replaced in therapy
Caution in sulfa allergy, associated with liver toxicity
Indinavir (Crixivan)
To be stored in original container, patients to drink 48 ounces of water daily, not to be taken with high-fat food or grapefruit juice if taken without ritonavir
Risk of kidney toxicity
Kioubavir-Ritonavir (Kaletra)
Less cramping since includes lower dose of ritonavir; diarrhea and nausea still present
Oral liquid contains high percentage of alcohol and propylene glycol
Nelfinavir (Viracept)
Main side effect is diarrhea which resolves with continued use
May dissolve nelfinavir tablets in small amount of water, consume immediately, and then rinse glass consuming any dose left; avoid mixing with acidic beverages or acidic food
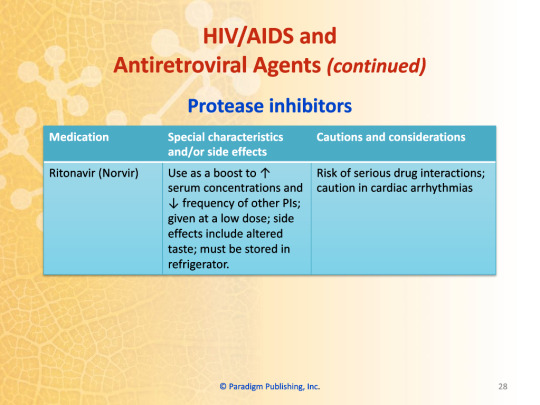
Ritonavir (Norvir)
Used as a boost to increase serum concentrations and decrease frequency of other PIs; given at a low dose; side effects include altered taste; must be stored in refrigerator
Risk of serious drug interactions; caution in cardiac arrhythmias
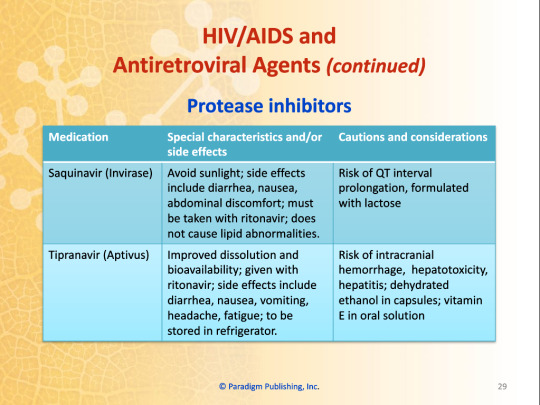
Saquinavir (Invirase)
Avoid sunlight; side effects include diarrhea, nausea, abdominal discomfort; must be taken with ritonavir; does not cause lipid abnormalities
Risk of QT interval prolongation, formulated with lactose
Tipranavir (Aptivus)
Improved dissolution and bioavailability; given with ritonavir; side effects include diarrhea, nausea, vomiting, headache, fatigue; to be stored in refrigerator
Risk of intracranial hemorrhage, hepatotoxicity, hepatitis; dehydrated ethanol in capsules; vitamin E in oral solution
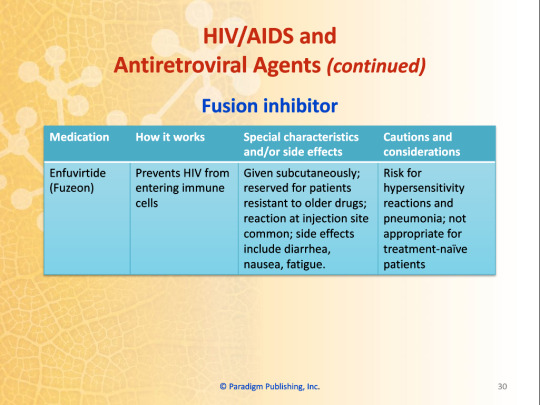
Fusion Inhibitor
Enfurvirtide (Fuzeon)
Prevents HIV from entering immune cells
Given subcutaneously; reserved for patients resistant to older drugs; reaction at injection site common; side effects include diarrhea, nausea, fatigue
Risk for hypersensitivity reactions and pneumonia; not appropriate for treatment-naive patients
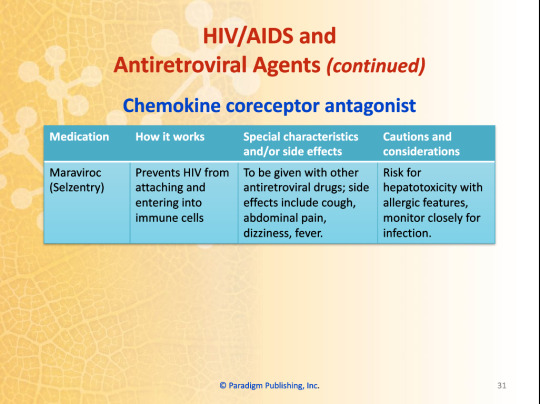
Chemokine Coreceptor Antagonist
Maraviroc (Selzentry)
Prevents HIV from attaching and entering into immune cells
To be given with other antiretroviral drugs; side effects include cough, abdominal pain, dizziness, fever
Risk for hepatotoxicity with allergic features, monitor closely for infection
0 notes
Text
Pharmacology - Chapter 5 - Therapies for Viral Infections and Immunizations
Part One Part Three Part Four Part Five
Transcription under the cut!



Antiviral Agents (Nonretroviral)
Antiherpes Agents
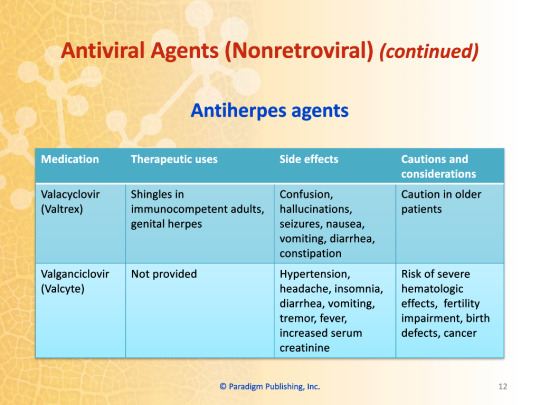
Valacyclovir (Valtrex)
Used in: Shingles in immunocompromised adults and genital herpes
Side effects: confusion, hallucinations, seizures, nausea, vomiting, diarrhea, constipation
Caution in older adults
Valganciclovir (Valcyte)
Side effects: hypertension, headache, insomnia, diarrhea, vomiting, tremor, fever, increased serum creatinine
Risk of severe hematologic effects, fertility impairment, birth defects, cancer
Anti-Influenza Agents
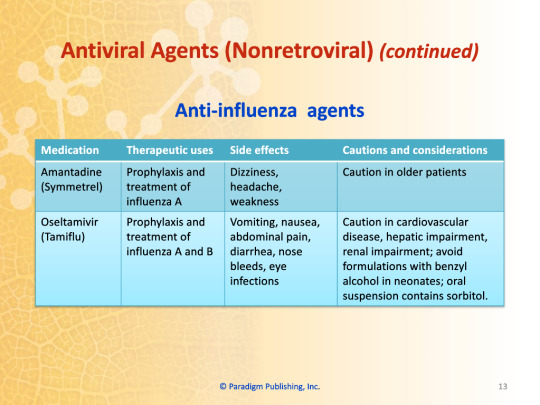
Amantadine (Symmetrel)
Used for: prophylaxis and treatment of influenza A
Side effects: dizziness, headache, weakness
Caution in older patients
Oseltamivir (Tamiflu)
Used for: prophylaxis and treatment of influenza A and B
Side effects: vomiting, nausea, abdominal pain, diarrhea, nose bleeds, eye infections
Caution in cardiovascular disease, hepatic impairment, renal impairment; avoid formulations with benzyl alcohol in neonates; oral suspension contains sorbitol
Rimantadine (Flumadine)
Used for: prophylaxis and treatment of influenza A
Side effects: dizziness, headache, weakness, GI effects
Caution in hepatic impairment, renal impairment, psychosis, seizures; caution in older adults
Zanamivir (Relenza)
Used for: prophylaxis and treatment of influenza A and B
Side effects: headache, throat/tonsil discomfort, cough
Caution in patients sensitive to milk products
Other Antiviral Agents
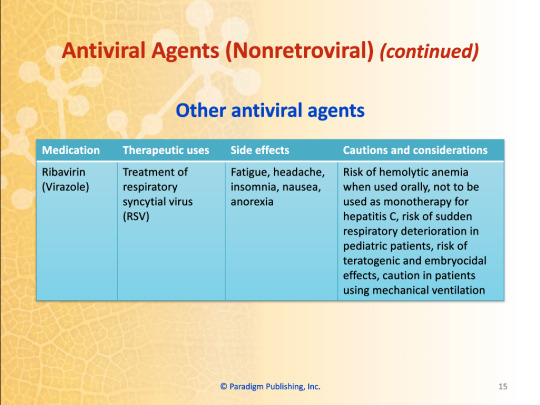
Ribavirin (Virazole)
Used for: treatment of respiratory syncytal virus (RSV)
Side effects: fatigue, headache, insomnia, nausea, anorexia
Risk of hemolytic anemia when used orally, not to be used as monotherapy for hepatitis C, risk of sudden respiratory deterioration in pediatric patients, risk of teratogenic and embryocidal effects, caution in patients using mechanical ventilation
HIV/AIDS and Antiretroviral Agents
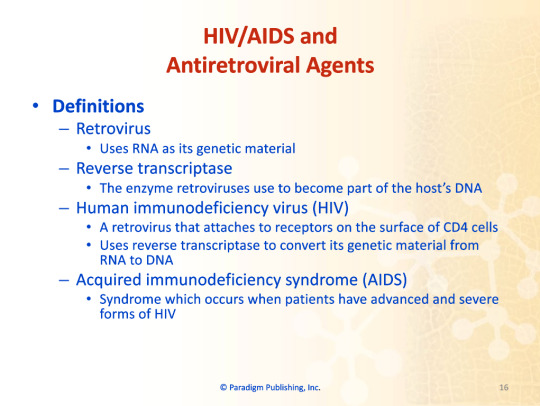
Definitions
Retrovirus
Uses RNA as its genetic material
Reverse transcriptase
The enzyme retroviruses use to become part of the host's DNA
Human immunodeficiency virus (HIV)
A retrovirus that attaches to receptors on the surface of CD4 cells
Uses reverse transcriptase to convert its genetic material from RNA to DNA
Acquired immunodeficiency syndrome (AIDS)
Syndrome which occurs when patients have advanced and severe forms of HIV
Antiretroviral drugs
Difficult to tolerate due to side effects and drug interactions
Can be combined in a "cocktail" which attacks viral replication in multiple stages
Must be taken chronically
Some cocktails available as a single tablet
Safety Alert
One of the biggest problems when treating HIV is nonadherence with the drug regimen because problematic side effects and complex dosing
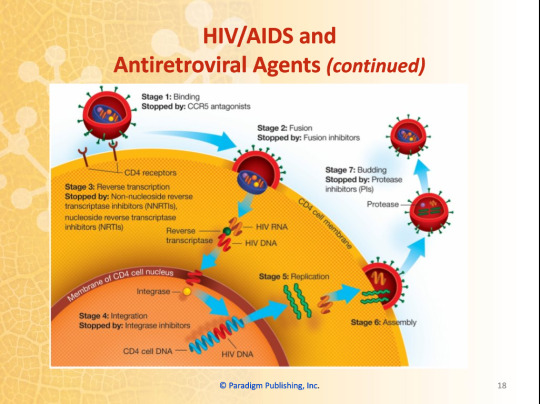
Stage One: Binding
Stopped by: CCR5 antagonists
Stage Two: Fusion
Stopped by: Fusion inhibitors
Stage Three: Reverse transcription
Stopped by: Non-nucleoside reverse transcriptase inhibitors (NNRTIs), Nucleoside reverse transcriptase inhibitors (NRTIs)
Stage Four: Integration
Stopped by: Integrase inhibitors
Stage Five: Replication
Stage Six: Assembly
Stage Seven: Budding
Stopped by: Protease inhibitors (PIs)
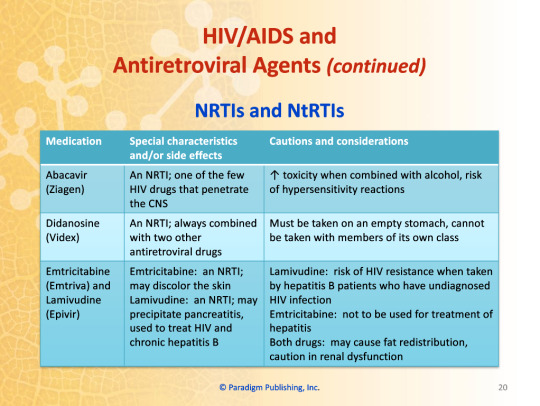
NRTIs and NtRTIs
Inhibit reverse transcriptase which prevents the formation of a DNA copy of viral RNA
Side effects: nausea, diarrhea, abdominal pain which improve in first few weeks.
More permanent effects: lactic acidosis with hepatic steatosis
Abacavir (Ziagen)
An NRTI; one of the few HIV drugs that penetrate the CNS
Increased toxicity when combined with alcohol, risk of hypersensitivity reactions
Didanosine (Videx)
An NRTI; always combined with two other antiretroviral drugs
Must be taken on an empty stomach, cannot be taken with members of its own class
Emtricitabine (Emtriva) and Lamivudine (Epivir)
Emtricitabine: an NRTI; may discolor the skin; not to be used for treatment of hepatitis
Lamivudine: an NRTI; may precipitate pancreatitis, used to treat HIV and chronic hepatitis B; risk of HIV resistance when taken by hepatitis B patients who have undiagnosed HIV infection
Both drugs: may cause fat redistribution, caution in renal dysfunction
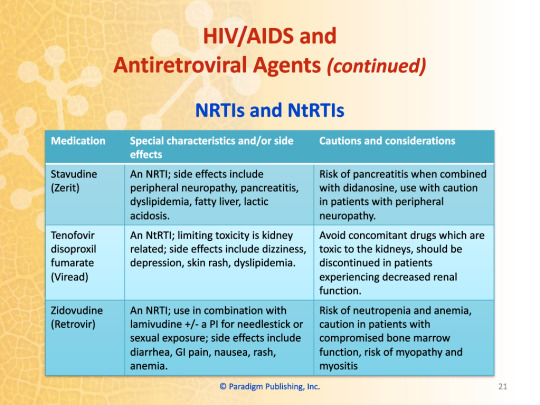
Stavudine (Zerit)
An NRTI; side effects: peripheral neuropathy, pancreatitis, dyslipidemia, fatty liver, lactic acidosis
Risk of pancreatitis when combined with didanosine, use with caution in patients with peripheral neuropathy
Tenofovir disoproxil fumarate (Viread)
An NtRTI; limiting toxicity is kidney related; side effects: dizziness, depression, skin rash, dyslipidemia
Avoid concomitant drugs which are toxic to the kidneys, should be discontinued in patients experiencing decreased renal function
Zidovudine (Retrovir)
An NRTI; use in combination with lamivudine +/- a PI for needlestick or sexual exposure; side effects: diarrhea, GI pain, nausea, rash, anemia
Risk of neutropenia and anemia, caution in patients with compromised bone marrow function, risk of myopathy and myositis
0 notes
Text
Pharmacology - Chapter 5 - Therapy for Viral Infections and Immunizations
Part Two Part Three Part Four Part Five
Transcription under the cut!

Chapter 5 - Therapy for Viral Infections and Immunizations
Chapter Topics
Viruses and viral infections
Antiviral agents (nonretroviral)
HIV/AIDS and antiretroviral agents
Immunization
Complementary and alternative therapies
Learning Objectives
Explain the differences between bacteria, fungi, and viruses, and why the drugs used to treat them must have very different mechanisms of action
Differentiate antiviral and antiretroviral drugs by their indications, therapeutic effects, side effects, dosages, and administration
Use antiviral and antiretroviral terminology correctly in written and oral communication
Identify drugs used for HIV and understand their synergism
Describe the importance of immunization
Identify common vaccines and their side effects
Viruses and Viral Infections
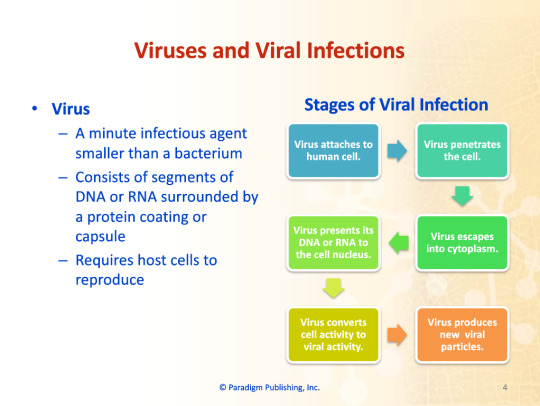
Virus
A minute infectious agent smaller than a bacterium
Consists of segments of DNA or RNA surrounded by a protein coating or capsule
Requires host cells to reproduce
Stage of Viral Infection
Virus attaches to human cell
Virus penetrates the cell
Virus escapes into cytoplasm
Virus presents its DNA or RNA to the cell nucleus
Virus converts cell activity to viral activity
Virus produces new viral particles
Influenza (the flu)
Symptoms include vague discomfort, tiredness, muscle pain, headache, chills, fever.
Patients at risk for complications include the elderly; patients with cardiovascular disease, renal disease, diabetes, asthma; immunocompromised patients.
Annual vaccinations recommended for those at risk for complications.
Hepatitis
Inflammation of the liver
Various forms referred to as hepatitis A through G
Severity range from benign to serious
HIV
Considered a chronic disease
Important to monitor for drug interactions
Regimens usually contain at least three drugs
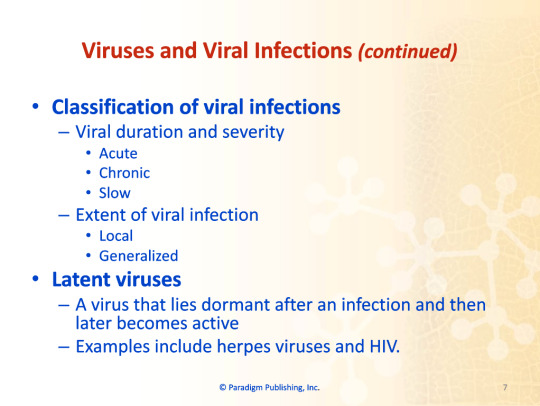
Classification of viral infections
Viral duration and severity
Acute
Chronic
Slow
Extent of viral infection
Local
Generalized
Latent Viruses
A virus that lies dormant after an infection and then later becomes active
Examples include herpes virus and HIV
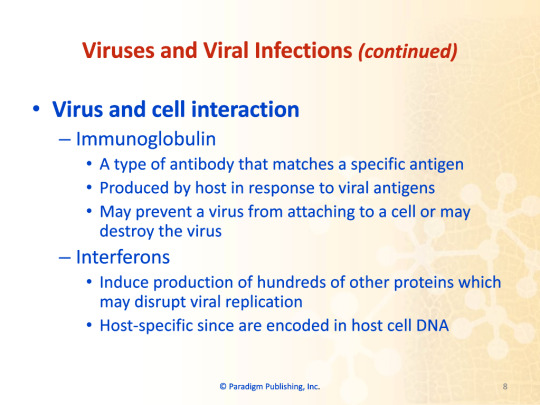
Virus and Cell Interaction
Immunoglobulin
A type of antibody that matches a specific antigen
Produced by host in response to viral antigens
May prevent a virus from attaching to a cell or may destroy a virus
Interferons
Induce production of hundreds of other proteins which may disrupt viral replication
Host-specific since are encoded in host cell DNA
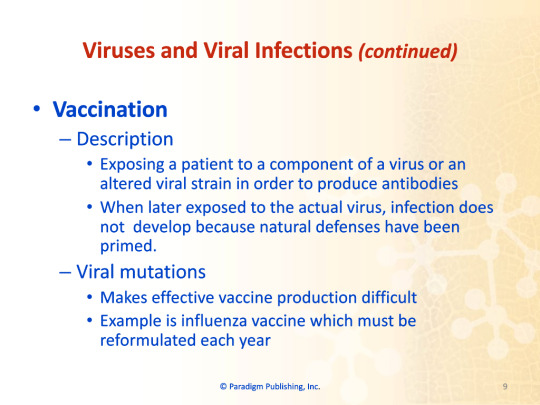
Vaccination
Description
Exposing a patient to a component of a virus or an altered viral strain in order to produce antibodies
When later exposed to the actual virus, infection does not develop because natural defenses have been primed
Viral Mutations
Makes effective vaccine production difficult
Example is influenza vaccine which must be reformulated each year
Antiviral Agents (Nonretroviral)
Antiviral Drugs
Risk of toxicity to host since virus uses host's cellular processes to function and replicate
Formulated to prevent viral replication without interfering with normal host cell function
Therapeutic Uses of Antiviral Drugs
Herpes simplex 1
Herpes simplex 2
Varicella-zoster
Cytomegalovirus (Human Herpes Virus 5)
Influenza
Respiratory syncytial virus (RSV)
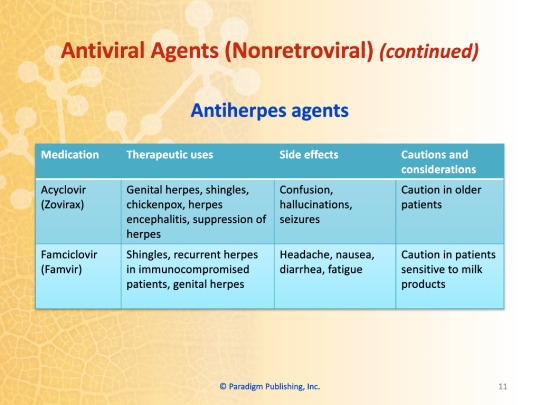
Acyclovir (Zovirax)
Used for: genital herpes, shingles, chickenpox, herpes encephalitis, suppression of herpes
May cause: confusion, hallucinations, seizures
Caution in older adults
Famciclovir (Famvir)
Used for: shingles, recurrent herpes in immunocompromised patients, genital herpes
May cause: headache, nausea, diarrhea, fatigue
Caution in patients sensitive to milk products
0 notes
Text
Pharmacology - Chapter 4 - Antibiotics and Antifungals
Part One (Slides 1-10)
Part Two (Slides 11-20)
Part Three (Slides 21-30)
Part Four (Slides 31-40)
Part Five (Slide 41)
0 notes
Text
Pharmacology - Chapter 4 - Antibiotics and Antifungals - Part Five
Part One
Part Two
Part Three
Part Four
Transcription under the cut!
Chapter Summary
Some antibiotic suspensions are stored in the refrigerator while others may be stored at room temperature.
Ophthalmic antibiotics have strict manufacturing requirements which may result in increased expense.
Several sexually-transmitted infections may be treated with antibiotics.
Drugs that fight bacterial infections generally will not work for fungal infections.
0 notes
Text
Pharmacology - Chapter 4 - Antibiotics and Antifungals - Part Four
Part One
Part Two
Part Three
Part Five
Transcription under the cut!





Fungi and Fungal Diseases
Fungus
Single-celled eukaryotic organism (has a defined nucleus)
Includes mushrooms, yeasts, and molds
How they differ from green plants
Lack chlorophyll
Reproduce by spores
How they differ from animal cells and bacteria
Have a rigid cell wall
How they differ from human cells
Human cell membranes contain cholesterol
Fungi cell membranes contain ergosterol
Fungal diseases
Mild, topical infections
Dermatophytes: athletes' foot and ringworm
Candida: vaginal yeast infections, oral thrush
Serious systemic infections
States of immunodeficiency
Drug therapy
Poor nutrition
IV catheters
Some cancers
Human immunodeficiency virus (HIV)
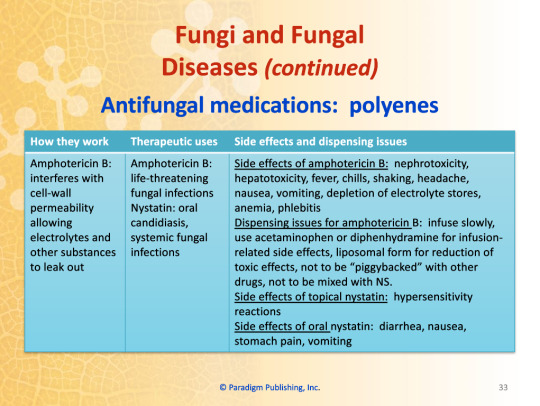
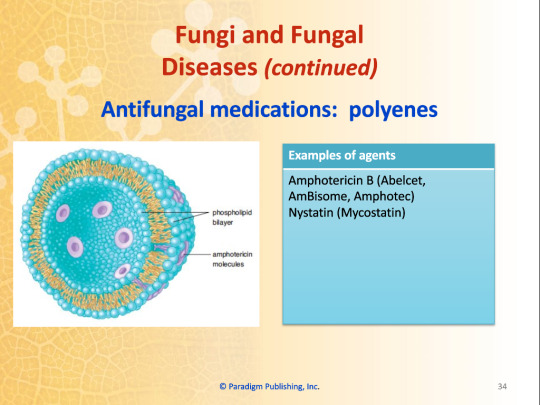
Antifungal Medications: Polyenes
How they work:
Amphotericin B: interferes with cell-wall permeability allowing electrolytes and other substances to leak out
Therapeutic uses:
Amphotericin B: life-threatening fungal infections
Nystatin: oral candidiasis, systemic fungal infections
Side effects:
Amphotericin B: nephrotoxicity, hepatotoxicity, fever, chills, shaking, headache, nausea, vomiting, depletion of electrolyte stores, anemia, phlebitis
Topical nystatin: hypersensitivity reactions
Oral nystatin: diarrhea, nausea, stomach pain, vomiting
Dispensing issues for amphotericin B: infuse slowly, use acetaminophen or diphenhydramine for infusion-related side effects, liposomal form for reduction of toxic effects, not to be "piggybacked" with other drugs, not to mixed with NS.
Examples of agents:
Amphotericin B (Abelcet, AmBisome, Amphotec)
Nystatin (Mycostatin)
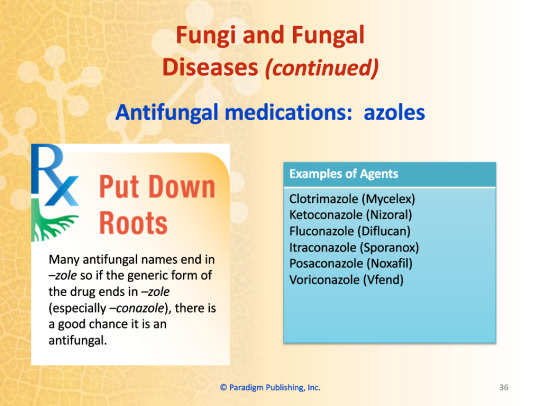
Antifungal Medications: Azoles
How they work:
Inhibit the formation of the cell wall
Therapeutic uses:
Variable: oral candidiasis, vaginal candidiasis, skin infections, nail infections, oropharyngeal or systemic infections caused by Candida and Aspergillus
Side effects:
Of class: nausea, vomiting, abdominal pain, diarrhea
Voriconazole: transient vision changes, visual hallucinations, alopecia, nail changes or loss, skin rash
Topical agents: burning, discomfort, edema, pain
Dispensing issues:
Itraconazole capsules and solution not to be substituted for each other
Take itraconazole capsules with acidic food or drink
Take posaconazole with food
Infuse voriconazole over one to two hours and not with other drugs
Short expiration of voriconazole
Examples of agents:
Clotrimazole (Mycelex)
Ketoconazole (Nizoral)
Fluconazole (Diflucan)
Itraconazole (Sporanox)
Posaconazole (Noxafil)
Voriconazole (Vfend)
Put Down Roots:
Many antifungal names end in -zole, so if the generic form of the drug ends in -zole (especially -conazole), there is a good chance it is an antifungal.
Antifungal Medications: Echinocandins
Inhibit the synthesis of D-glucan, which is an integral part of the fungal cell wall.
Used for invasive Candida and Aspergillus in patients unresponsive to amphotericin B and itraconazole
Side effects: infusion and hypersensitivity reactions such as rash, redness, hypotension, angioedema, injection-site pain
Dispensing issues: reconstitute micafungin by swirling, protect micafungin from light
Examples of agents:
Caspofungin (Cancidas)
Micafungin (Mycamine)
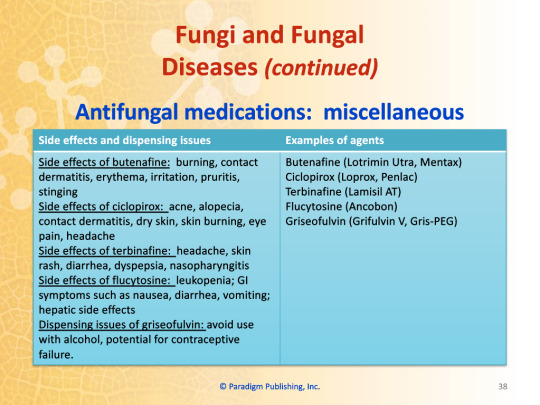
Antifungal Medications: Miscellaneous
Examples of agents:
Butefine (Lotrimin Ultra, Mentax)
Ciclopirox (Loprox, Penlac)
Terbinafine (Lamisil AT)
Flucytosine (Ancobon)
Grisofulvin (Grilfulvin V, Gris-PEG)
Side effects:
Of butenafine: burning, contact dermatitis, erythema, irritation, pruritus, stinging
Of ciclopirox: acne, alopecia, contact dermatitis, dry skin, skin burning, eye pain, headache
Of terbinafine: headache, skin rash, diarrhea, dyspepsia, nasopharyngitis
Of flucytosine: leukopenia, GI symptoms such as nausea, vomiting; hepatic side effects
Dispensing issues:
Of griseofulvin: avoid use with alcohol, potential for contraceptive failure
Complementary and Alternative Therapies
Echinacea
Used to treat the common cold, RTIs, and vaginal yeast infections
Reduces the severity and length of symptoms
Variable concentrations in the products available
No standard dose established
Must be used multiple times a day and started at the first sign of infection
Zinc
Used to enhance wound healing and prevent wound-associated infections
No well-established dose
Chapter Summary
A bacteria is a single-celled organism that can cause infection in the body.
Bacteria can be classified by oxygenation needs, shape, growth arrangement, and Gram-stain results.
Several major classes of antibiotics and antifungals are available which vary in the spectrum of activity, side effect profile, contraindications, and drug interactions.
0 notes
Text
Pharmacology - Chapter 4 - Antibiotics and Antifungals - Part Three
Part One
Part Two
Part Four
Part Five
Transcription under the cut!

Fighting Bacterial Infections
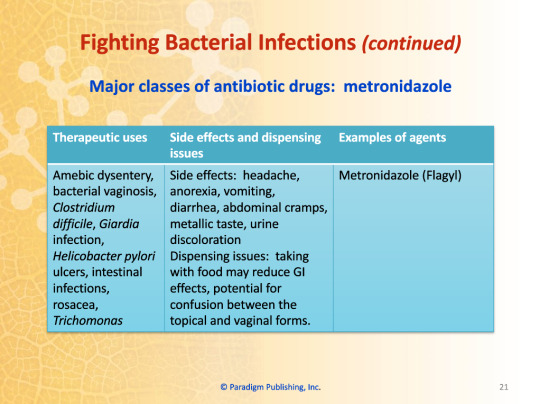
Major Classes of Antibiotic Drugs: Metronidazole
Therapeutic uses: Amebic dysentery, bacterial vaginosis, Clostridium difficile, Giardia infection, Helicobacter pylori ulcers, intestinal infections, rosacea, Trichomonas
Side effects: headache, anorexia, vomiting, diarrhea, abdominal cramps, metallic taste, urine discoloration
Dispensing issues: taking with food may reduce GI effects, potential for confusion between the topical and vaginal forms
Examples of agents: Metronidazole (Flagyl)
Major Classes of Antibiotic Drugs: Linezolid
How it works: Inhibits bacterial protein synthesis
Therapeutic uses: MRSA, VRE, other Gram positive infections
Side effects: headache, diarrhea, decreased hemoglobin, leukopenia, thrombocytopenia
Dispensing issues: protect from light
Examples of agents: Linezolid (Zyvox)
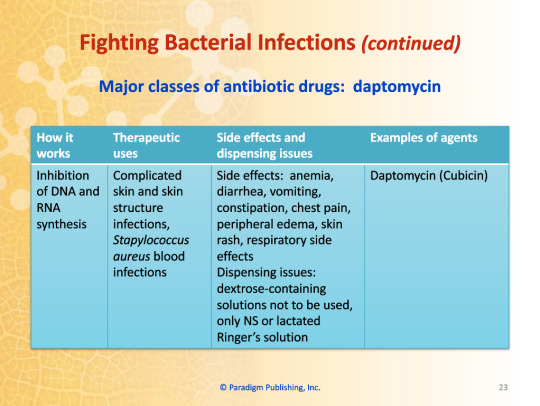
Major Classes of Antibiotic Drugs: Daptomycin
How it works: Inhibition of DNA and RNA synthesis
Therapeutic uses: Complicated skin and skin structure infections, Staphylococcus aureus blood infections
Side effects: anemia, diarrhea, vomiting, constipation, chest pain, peripheral edema, skin rash, respiratory side effects
Dispensing issues: dextrose-containing solutions not to be used, only NS or lactated Ringer's solution
Examples of agents: Daptomycin (Cubicin)
Storage of Liquid Antibiotics
Storage Requirements
Some antibiotics require refrigeration
Some antibiotics may be stored at room temperature
Appropriate for technicians to discuss this information with patient
Medication flavors
Technician may suggest and change flavors
Increases adherence in children
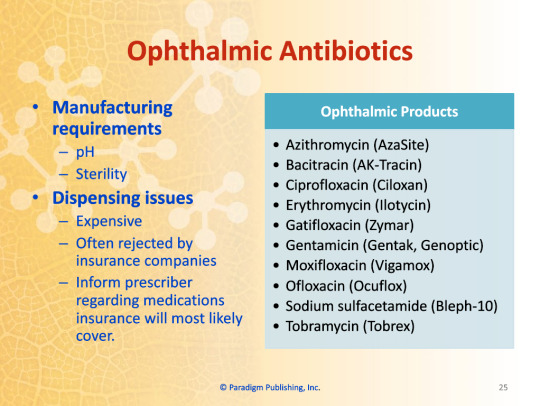
Ophthalmic Antibiotics
Manufacturing requirements
pH
Sterility
Dispensing issues
Expensive
Often rejected by insurance companies
Inform prescriber regarding medications insurance will most likely cover
Ophthalmic Products
Azithromycin (AzaSite)
Bacitracin (AK-Tracin)
Ciprofloxacin (Ciloxan)
Erythromycin (Ilotycin)
Gatifloxacin (Zymar)
Gentamicin (Gentak, Genoptic)
Moxifloxacin (Vigamox)
Ofloxacin (Ocuflox)
Sodium sulfacetamide (Bleph-10)
Tobramycin (Tobrex)
Sexually-Transmitted Infections
Definition
Genital system infections transmitted by sexual activity
Formerly known as venereal diseases
Prevention
Abstinence
Long-term monogamous relationship with an uninfected partner
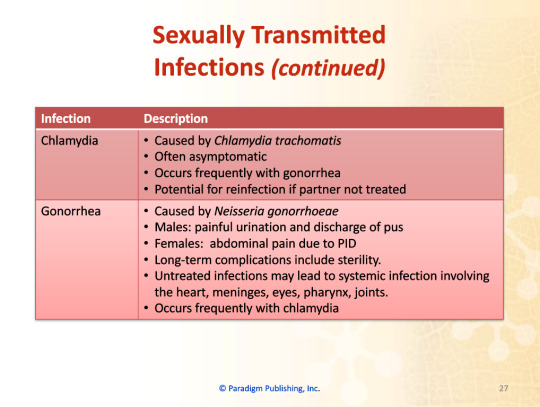
Chlamydia
Caused by Chlamydia trachomatis
Often asymptomatic
Occurs frequently with gonorrhea
Potential for reinfection if partner not treated
Gonorrhea
Caused by Neisseria gonorrhoeae
Males: painful urination and discharge of pus
Females: abdominal pain due to PID
Long-term complications include sterility
Untreated infections may lead to systemic infections involving the heart, meninges, eyes, pharynx, joints
Occurs frequently with chlamydia
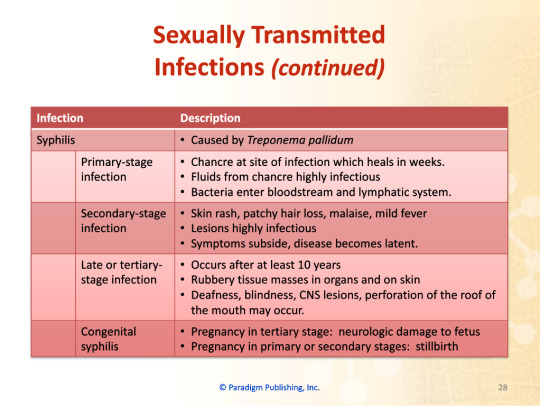
Syphilis: caused by Treponema pallidum
Primary-stage infection
Chancre at site of infection which heals in weeks
Fluids from chancre highly infectious
Bacteria enter bloodstream and lymphatic system
Secondary-stage infection
Skin rash, patchy hair loss, malaise, mild fever
Lesions highly infectious
Symptoms subside, disease becomes latent
Late- or tertiary-stage infection
Occurs after at least 10 years
Rubbery tissue masses in organs and on skin
Deafness, blindness, CNS lesions, perforation of the roof of the mouth may occur
Congenital syphilis
Pregnancy in tertiary-stage: neurologic damage to fetus
Pregnancy in primary- or secondary-stage: stillbirth
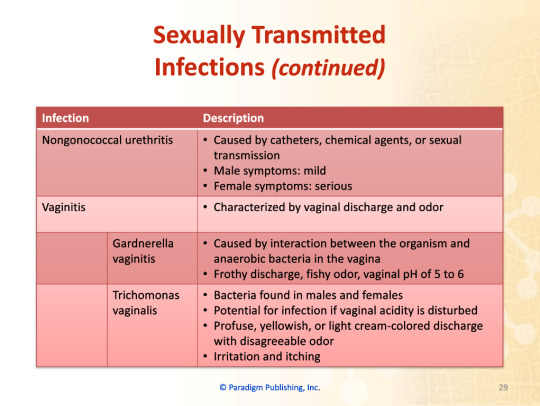
Nongonococcal urethritis
Caused by catheters, chemical agents, or sexual transmission
Male symptoms: mild
Female symptoms: serious
Vaginitis
Characterized by vaginal discharge and odor
Gardnerella vaginitis
Caused by interaction between the organism and anaerobic bacteria in the vagina
Frothy discharge, fishy odor, vaginal pH of 5 to 6
Trichomonas vaginalis
Bacteria found in males and females
Potential for infection if vaginal acidity is disturbed
Profuse, yellowish, or light cream-colored discharge with disagreeable odor
Irritation and itching
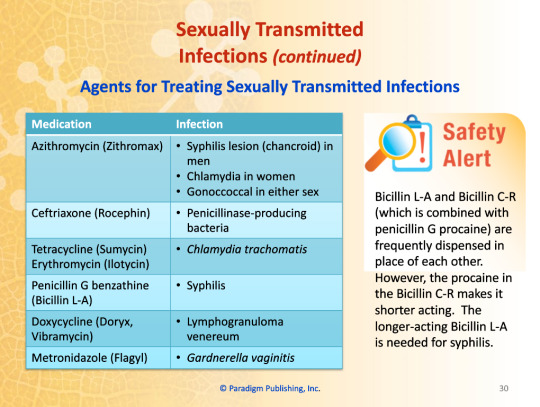
Agents for Treating Sexually-Transmitted Infections
Azithromycin (Zithromax)
Syphilis lesions (chancroid) in men
Chlamydia in women
Gonoccoccal in either sex
Ceftriaxone (Rocephin)
Penicillinase-producing bacteria
Tetracycline (Sumycin), Erythromycin (Ilotycin)
Chlamydia trachomatis
Penicillin G benzathine (Bicillin L-A)
Syphilis
Doxycycline (Doryx, Vibramycin)
Lymphogranuloma venereum
Metronidazole (Flagyl)
Gardnerella vaginitis
Safety Alert
Bicillin L-A and Bicillin C-R (which is combined with penicillin G procaine) are frequently dispensed in place of each other. However, the procaine in the Bicillin C-R makes it shorter acting. The longer-acting Bicillin L-A is needed for syphilis.
0 notes
Text
Pharmacology - Chapter 4 - Antibiotics and Antifungals - Part Two
Part One
Part Three
Part Four
Part Five
Transcription under the cut!

Fighting Bacterial Infections
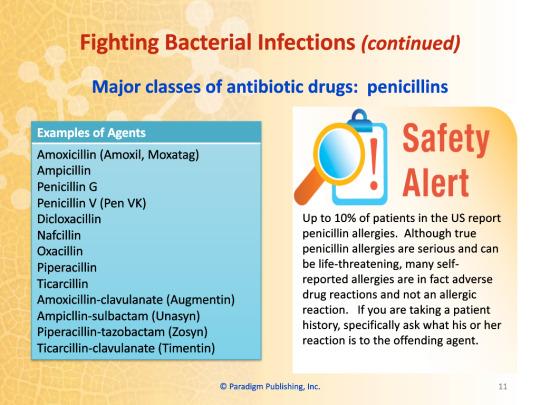
Major Classes of Antibiotic Drugs: Penicillins
Examples of agents
Amoxicillin (Amoxil, Moxatag)
Ampicillin
Penicillin G
Penicillin V (Pen VK)
Dicloxacillin
Nafcillin
Oxacillin
Piperacillin
Ticarcillin
Amoxicillin-clavulanate (Augmentin)
Ampicillin-sulbactam (Unasyn)
Piperacillin-tazobactam (Zosyn)
Ticarcillin-clavulanate (Timentin)
Safety Alert
Up to 10% of patients in the US report penicillin allergies. Although true penicillin allergies are serious and can be life-threatening, many self-reported allergies are in fact adverse drug reactions and not an allergic reaction. If you are taking a patient history, specifically ask what his or her reaction is to the offending agent.
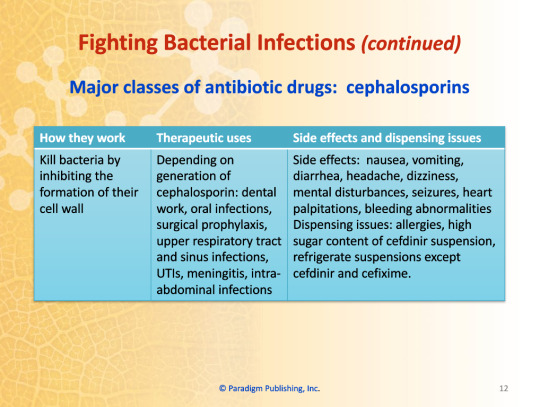
Major Classes of Antibiotic Drugs: Cephalosporins
How they work: Kill bacteria by inhibiting the formation of their cell wall
Therapeutic uses: Depending on generation of cephalosporin: dental work, oral infections, surgical prophylaxis, upper respiratory tract and sinus infections, UTIs, meningitis, intra-abdominal infections
Side effects: nausea, vomiting, diarrhea, headache, dizziness, mental disturbances, seizures, heart palpitations, bleeding abnormalities
Dispensing issues: allergies, high sugar content of cefdinir suspension, refrigerate suspensions except cefdinir and cefixime
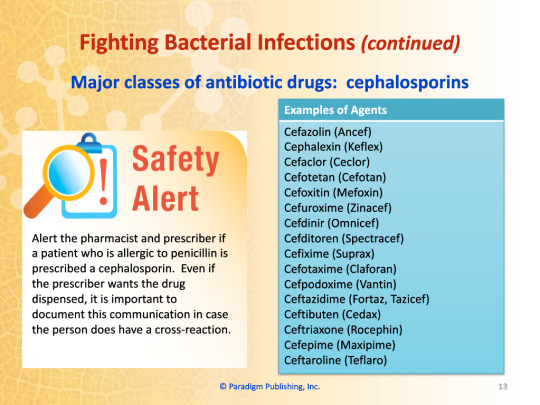
Examples of agents:
Cefazolin (Ancef)
Cephalexin (Keflex)
Cefaclor (Ceclor)
Cefotetan (Cefotan)
Cefoxitin (Mefoxin)
Cefuroxime (Zinacef)
Cefdinir (Omnicef)
Cefditoren (Spectracef)
Cefixime (Suprax)
Cefotaxime (Suprax)
Cefotaxime (Claforan)
Cefpodoxime (Claforan)
Ceftazidime (Fortaz, Tazicef)
Ceftibutin (Cedax)
Ceftriaxone (Rocephin)
Cefepime (Maxipime)
Ceftaroline (Teflaro)
Safety Alert
Alert the pharmacist and prescriber if a patient who is allergic to penicillin is prescribed a cephalosporin. Even if the prescriber wants the drug dispensed, it is important to document this communication in case the person does have a cross-reaction.
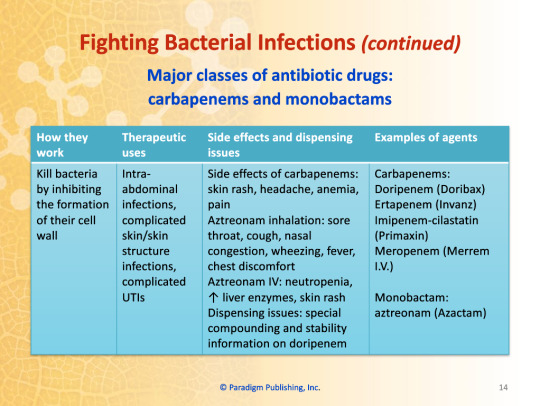
Major Classes of Antibiotic Drugs: Carbapenems and Monobactams
How they work: Kill bacteria by inhibiting the formation of their cell wall
Therapeutic uses: Intra-abdominal infections, complicated skin/skin structure infections, complicated UTIs
Side effects of carbepenems: skin rash, headache, anemia, pain
Aztreonam inhalation: sore throat, cough, nasal congestion, wheezing, fever, chest discomfort
Aztreonam IV: neutropenia, increased liver enzymes, skin rash
Dispensing issues: special compounding and stability information on doripenem
Examples of agents:
Carbapenems:
Doripenem (Doribex)
Ertapenem (Invanz)
Imipenem-cilastatin (Primaxin)
Meropenem (Merrem I.V.)
Monobactam:
Aztreonam (Azactam)
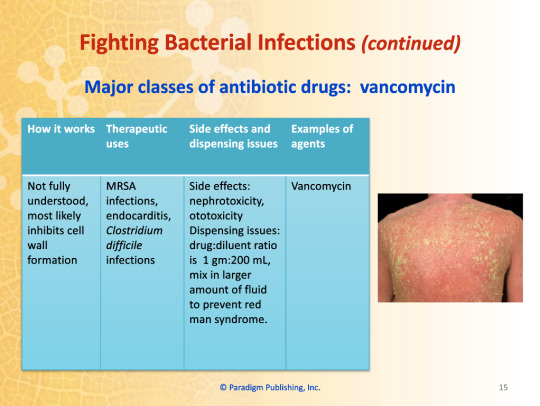
Major Classes of Antibiotic Drugs: Vancomycin
How it works: Not fully understood, most likely inhibits cell wall formation
Therapeutic uses: MRSA infections, endocarditis, Clostridium difficile infections
Side effects: nephrotoxicity, ototoxicity
Dispensing issues: drug:diluent ratio is 1 gm:200 mL, mix in larger amount of fluid to prevent red man syndrome
Examples of agents: Vancomycin
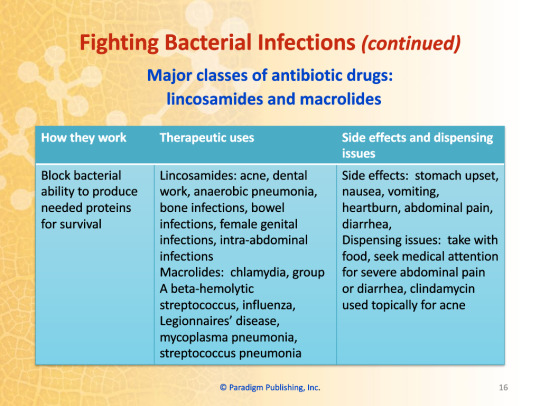
Major Classes of Antibiotic Drugs: Lincosamides and Macrolides
How they work: Block bacterial ability to produce needed proteins for survival
Therapeutic uses:
Lincosamides: acne, dental work, anaerobic pneumonia, bone infections, bowel infections, female genital infections, intra-abdominal infections
Macrolides: chlamydia, group A beta-hemolytic streptococcus, influenza, Legionnaire's disease, mycoplasma pneumonia, streptococcus pneumonia
Side effects: stomach upset, nausea, vomiting, heartburn, abdominal pain, diarrhea
Dispensing issues: take with food, seek medical attention for severe abdominal pain or diarrhea, clindamycin used topically for acne
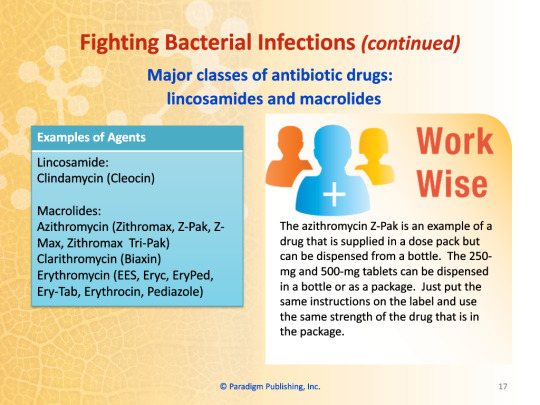
Examples of agents:
Lincosamide:
Clindamycin (Cleocin)
Macrolides:
Azithromycin (Zitromax, Z-Pak, Z-Max, Zitromax, Tri-Pak)
Clarithromycin (Biaxin)
Erythromycin (EES, Eryc, EryPed, Ery-Tab, Erythrocin, Pediazole)
Work Wise
The azithromycin Z-Pak is an example of a drug that is supplied in a dose pack but can be dispensed from a bottle. The 250 mg and 500 mg tablets can be dispensed in a bottle or as a package. Just put same instructions on the label and use the same strength of the drug that is in the package.
Major Classes of Antibiotic Drugs: Aminoglycosides
How they work: Kill bacteria by blocking their ability to make essential proteins for survival
Therapeutic uses: Life-threatening infections due to Gram negative aerobes, sepsis, peritonitis
Side effects: nephrotoxicity, ototoxicity
Dispensing issues: variable doses, dosing is individualized and based on patient weight or therapeutic levels
Examples of agents:
Amikacin
Gentamicin (Garamycin, Gentak)
Tobramycin (TOBI, Tobrex)
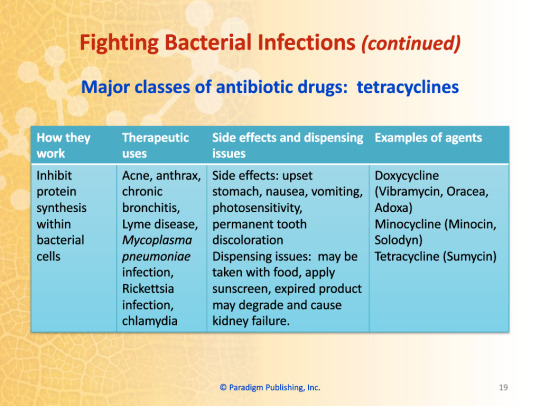
Major Classes of Antibiotic Drugs: Tetracyclines
How they work: Inhibit protein synthesis within bacterial cells
Therapeutic uses: Acne, anthrax, chronic bronchitis, Lyme disease, Mycoplasma pneumoniae infection, Rickettsia infection, chlamydia
Side effects: upset stomach, nausea, vomiting, photosensitivity, permanent tooth discoloration
Dispensing issues: may be taken with food, apply sunscreen, expired product may degrade and cause kidney failure
Examples of agents:
Doxycycline (Vibramycin, Oracea, Adoxa)
Minocycline (Minocin, Solodyn)
Tetracycline (Sumycin)
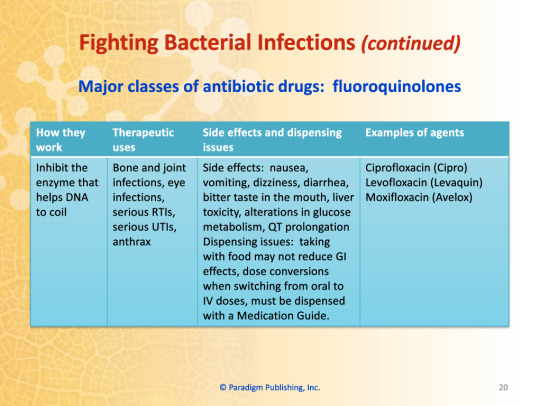
Major Classes of Antibiotic Drugs: Fluoroquinolones
How they work: Inhibit the enzyme that helps DNA to coil
Therapeutic uses: Bone and joint infections, eye infections, serious RTIs, serious UTIs, anthrax
Side effects: nausea, vomiting, dizziness, diarrhea, bitter taste in the mouth, liver toxicity, alterations in glucose metabolism. QT prolongation
Dispensing issues: taking with food may not reduce GI effects, dose conversions when switching from oral to IV doses, must be dispensed with a Medication Guide
Examples of agents:
Ciprofloxacin (Cipro)
Levofloxacin (Levaquin)
Moxifloxacin (Avelox)
0 notes
Text
Pharmacology - Chapter 4 - Antibiotics and Antifungals - Part One

Part Two
Part Three
Part Four
Part Five
Transcription under the cut!

Chapter 4 - Antibiotics and Antifungals
Chapter Topics
Fighting bacterial infections
Storage of liquid antibiotics
Ophthalmic antibiotics
Sexually-transmitted infections
Fungi and fungal diseases
Complementary and alternative therapies
Learning Objectives
Describe the differences between bacteria and fungi.
Identify the major types of antibiotics by drug class.
Determine which auxiliary labels to use when dispensing major types of antibiotics and antifungals.
Define therapeutic effects, side effects, contraindications, and administration routes of major antibiotics and antifungals.
Utilize appropriate antibiotic and antifungal general drug terminology in written and oral communication.
Describe treatment for common sexually-transmitted infections.
Discuss storage requirements of liquid antibiotics.
List common ophthalmic antibiotics.
Fighting Bacterial Infections
Bacteria
Single-celled organisms
Pathogenic bacteria
Bacteria that are harmful
Infection
Tissue damage caused by the presence of bacteria or their toxins
Work Wise
Many times bacteria names are abbreviated in the workplace. For example, you may hear Streptococcus pneumoniae called "Strep. pneumo." Clostridium difficile can be called "C. diff" and Escherichia coli is often referred to as "E. coli."
Types of bacteria
Aerobic bacteria
Need oxygen to live
Anaerobic bacteria
Can survive without oxygen
Shapes of bacteria
Cocci
Bacilli
Spirochetes
Gram positive bacteria
Have a thick cell wall which absorbs crystal violet
Gram negative bacteria
Have a thin cell wall which does not absorb crystal violet
Symptoms of bacterial infections
Fever of >101°F AND white blood cell count of >12,000/mm3
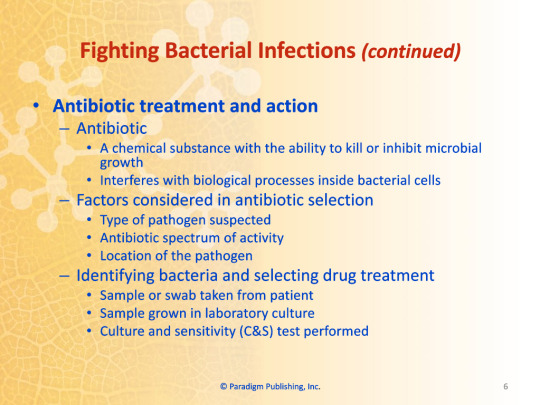
Antibiotic treatment and action
Antibiotic
A chemical substance with the ability to kill or inhibit microbial growth
Interferes with biological processes inside bacterial cells
Factors considered in antibiotic selection
Type of pathogen suspected
Antibiotic spectrum of activity
Location of the pathogen
Identifying bacteria and selecting drug treatment
Sample or swab taken from patient
Sample grown in laboratory culture
Culture and sensitivity (C&S) test performed
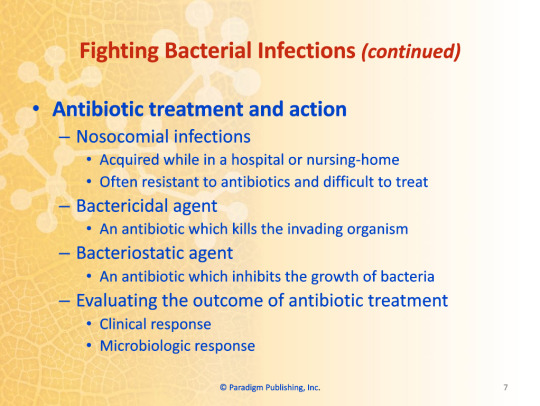
Nosocomial infections
Acquired while in a hospital or nursing-home
Often resistant to antibiotics and difficult to treat
Bactericidal agent
An antibiotic which kills the invading organism
Bacteriostatic agent
An antibiotic which inhibits the growth of bacteria
Evaluating the outcome of antibiotic treatment
Clinical response
Microbiologic response
Side effects and dispensing issues of antibiotics
Parenteral
Mix exactly as directed
Oral
Swab counting tray with alcohol
Gastrointestinal (GI) upset
Some antibiotics to be taken with food
Birth control pills
Interaction with antibiotics may decrease effectiveness
Around-the-clock administration
Purpose is to maintain consistent serum drug levels
Antimicrobial resistance
A defense mechanism of bacteria to resist or inactive antibiotics
Important for patients to complete course of antibiotics
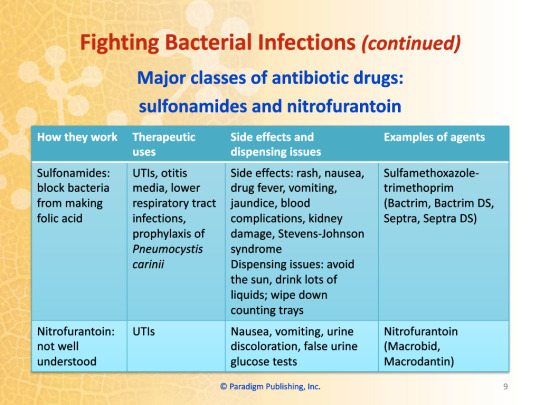
Major Classes of Antibiotic Drugs: Sulfonamides and Nitrofurantoin
Sulfonamides: Block bacteria from making folic acid
Therapeutic Uses: UTIs, otitis media, lower respiratory tract infections, prophylaxis of Pneumocystis carinii
Side effects: rash, nausea, drug fever, vomiting, blood complications, kidney damage, Stevens-Johnson syndrome
Dispensing issues: avoid the sun, drink lots of liquids; wipe down counting trays
Examples of agents: Sulfamethoxazole-trimethoprim (Bactrim, Bactrim DS, Septra, Septra DS)
Nitrofurantoin: not well understood
Therapeutic use: UTIs
Side effects: nausea, vomiting, urine discoloration, false urine glucose tests
Examples of agents: Nitrofurantoin (Macrobid, Macrodantin)
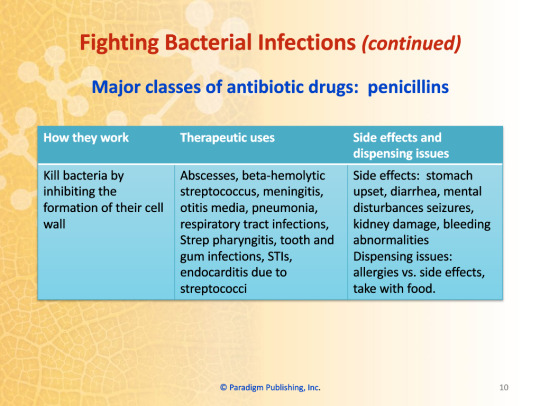
Major Classes of Antibiotic Drugs: Penicillins
How they work: Kill bacteria by inhibiting the formation of their cell wall
Therapeutic uses: Abscesses, beta-hemolytic streptococcus, meningitis, otitis media, pneumonia, respiratory tract infections, Strep pharyngitis, tooth and gum infections, STIs, endocarditis due to streptococci
Side effects: stomach upset, diarrhea, mental disturbances seizures, kidney damage, bleeding abnormalities
Dispensing issues: allergies vs. side effects, take with food
1 note
·
View note
Text
Pharmacology - Chapter 3 - Dispensing Medications
Part One (Pages 1-10)
Part Two (Pages 11-20)
Part Three (Pages 21-30)
1 note
·
View note
Text
Pharmacology - Chapter 3 - Dispensing Medications - Part Three
Part One
Part Two
Transcription under the cut!


Factors that Influence Drug Action
Other Considerations in Older Adults
Adverse drug reactions
Beers List
Polypharmacy
Cognitive abilities
Nonadherence
Special Considerations in Children
Altered drug responses
Body weight commonly used for drug doses
OTC doses for very young or small children not on package
Calculations to be double checked
Doses to be reevaluated regularly
Allergic Response
Allergy
Hypersensitivity of the immune system induced by exposure to a particular substance
Allergens
Substances which cause an allergic reaction
Histamine
Produced by the body in response to an allergy
Signs of allergic reaction
Red, watery eyes
Sneezing
Urticaria
Rash
Bronchiolar constriction
Allergy documentation
Must be part of medication record
Teaching Patients Medication Management
Role of the pharmacy technician
Provide clearly written directions
Record medication history in profile including use of OTC medications
Explain that pharmacist is available to answer questions and provide instructions
Read exact wording on label, medication guide, or educational materials to patient
Ensure that patients know how to read medication labels
By law, no advice or counseling is to be provided by technician
Reasons for Nonadherence
Side effects
Failure to understand the disease
Confusion or complexity of the regimen
Simple forgetfulness
Medication Safety
Risk Evaluation and Mitigation Strategy (REMS) Program
Mandated by the FDA for certain medications
Goal is to ensure that benefits outweigh risks
Potential requirements
Dispensing a medication guide
Special dispensing and/or prescribing requirements
Completion of training by prescribers/pharmacists
Special dispensing procedures for technicians
Technician Role
Verify the patient's address, date of birth, phone numbers, allergies, conditions.
Ensure patient gets counseling.
E-Prescribing
Eliminates illegible prescriptions.
Automatically checks for drug allergies, interactions, dosing errors, and therapeutic duplications.
Potential for error reduction.
Physician Order Entry
Computerized physician order entry (CPOE)
Documented reduction in errors
Dispensing Cautions
Requirement to use original containers
Partial prescription not alllowed
Tamper-Resistant Pads
Required for prescribers who file for Medicaid reimbursement
If not used, prescriber will get call to verify prescription
Intent is to encourage e-prescribing
Medication Reconciliation
Improvement of patient safety during transitions of care from one level of care to another
Purpose of reconciliation is to communicate drug therapy information to next care setting
Understanding the Profession
Goals to Keep in Mind
Obtaining certification as a pharmacy technician
Securing employment in profession
Resourceful Organizations
Pharmacy Technician Certification Board (PTCB)
American Association of Pharmacy Technicians (AAPT)
National Pharmacy Technician Association (NPTA)
Chapter Summary
A prescription is a request for the dispensing of medications.
The "rights" for correct drug administration are the right patient, the right drug, the right strength, the right route, the right time, and the right documentation.
The three main routes of administration are oral, parenteral, and topical.
Several physiologic changes occur in the older adult leading to altered drug responses.
Drug doses in children are most often calculated using patient weight.
A pharmacy technician plays a positive role in influencing drug therapy.
0 notes
Text
Pharmacology - Chapter 3 - Dispensing Medications - Part 2
Part One
Part Three
Transcription under the cut!




Dosage Forms and Route of Administration
Determining Route of Administration
Disease state
Area of the body
Drug's chemical composition
Patient age and condition
Convenience
Examples of Oral (PO) Route
Sublingual (Under the Tongue)
Oral (Swallowed)
Buccal (Dissolves in the Cheek)
Oral Dosage Forms
Capsules
Elixirs
Gels
Powders
Solution
Suspensions
Syrups
Tablets
Troches/Lozenges
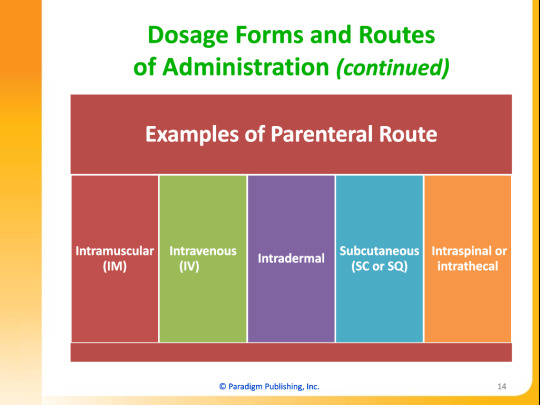
Examples of Parenteral Route
Intramuscular (IM)
Intravenous (IV)
Intradermal
Subcutaneous (SC or SQ)
Intraspinal or Intrathecal
Parenteral Dosage Forms
Solutions
Suspensions
Examples of Topical Route
Transdermal
Inhalation
Ophthalmic
Otic
Nasal
Rectal
Vaginal
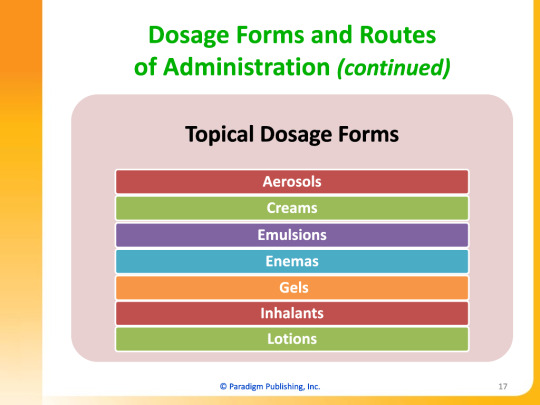
Topical Dosage Forms
Aerosols
Creams
Emulsions
Enemas
Gels
Inhalants
Lotions
Ointments
Pastes
Powders
Sponges
Sprays
Suppositories
Transdermal Patches
Factors that Influence Drug Action
Special Considerations in Older Adults
Changes in physiologic function
Visual changes
Auditory changes
Gastrointestinal changes
Pulmonary changes
Cardiovascular changes
Renal changes
Hormonal changes
Body composition changes
Altered drug responses
Absorption changes
Distribution changes
Metabolism changes
Elimination changes
Pharm Facts
Normally, blood flow (as measured per minute) decreases about 1% per year as an individual ages, beginning at about age 35 (40 percent from ages 35 to 75).
0 notes
Text
Pharmacology - Chapter 3 - Dispensing Medications (Part One)
Part Two
Part Three
Transcription under the cut!


Chapter 3 - Dispensing Medications
Chapter Topics
The prescription
Correct drug administration "rights"
Dosage forms and routes of administration
Factors that influence drug action
Teaching patients medication management
Medication safety
Understanding the profession
Learning Objective
Describe the components of a prescription
State commonly used prescription abbreviations
Explain the "rights" of correct drug administration
Recognize common dosage forms
Name the routes of administration and their abbreviations
Recognize factors that influence the effects of drugs, particularly in older adults and pediatric populations
Describe the role of the pharmacy technician in medication safety
The Prescription
Prescription
A direction for medication to be dispensed to a patient written by a physician or qualified licensed practitioner and filled by a pharmacist.
Term used in noninstitutional settings.
Medication Order
A prescription issued in an institutional setting.
Components of a Prescription
Full name of patient
Date of prescription
Drug name
Dosage
Route of administration
Amount of drug to be dispensed Note: Amounts should be written out to prevent alterations
Signature of person authorized to prescribe
DEA number if a C-II, C-III, or C-IV drug
Generic permitted
Number of refills
Patient's name
Date prescription written
Inscription which includes name of drug, dose, quantities of ingredients
Signa or "sig" which are the directions for use
Number of refills or "no refills"
Signature and address of the physician
Indication of whether generic substitution is permitted
Drug Enforcement Administration (DEA) number if for a controlled substance
Abbreviations
Used on prescriptions
Standard usage for prescribers, pharmacists, and prescriptions
Not used for patient instructions or for verbal orders
Potential source of medication errors
Official "Do Not Use" Abbreviations
U, u (unit)
Mistaken for 0, 4, or cc
Write "unit"
IU (International Unit)
Mistaken for IV or 10
Write "International Unit"
Q.D., QD, q.d., qd (daily)
Mistaken for Q.O.D., QOD, q.o.d., qod
Write "daily"
Q.O.D., QOD, q.o.d., qod (every other day)
Mistaken for Q.D., QD, q.d., qd. Period after the Q mistaken for "I" and the "O" for "I"
Write "every other day"
Trailing zero (x.0 mg)
Decimal point is missed
Write x mg
Lack of trailing zero (.x mg)
Decimal point is missed
Write 0.x mg
MSO4 and MgSO4
Confused for one another
Write "morphine sulfate" or "magnesium sulfate"
Correct Drug Administration Rights
Introduction
Used as a guideline for filling prescriptions
Concepts used to avoid medication errors
Work Wise
If something seems strange about a prescription (like a dose), speak up. As a pharmacy technician, you are a valuable asset to your pharmacist. Your pharmacist will be glad you expressed your concern.
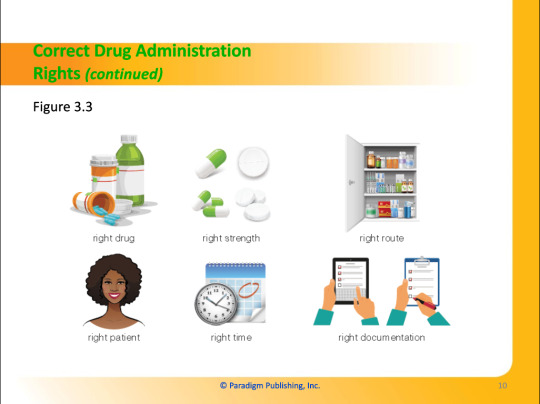
Right Drug
Right Strength
Right Route
Right Patient
Right Time
Right Documentation
0 notes
Text
Pharmacology - Chapter 2 - Basic Concepts of Pharmacology
Part One (Pages 1-10)
Part Two (Pages 11-20)
Part Three (Pages 21-29)
0 notes