#Thymus cell lymphocyte
Explore tagged Tumblr posts
Text
Human Cell Tournament Round 2
Propaganda!


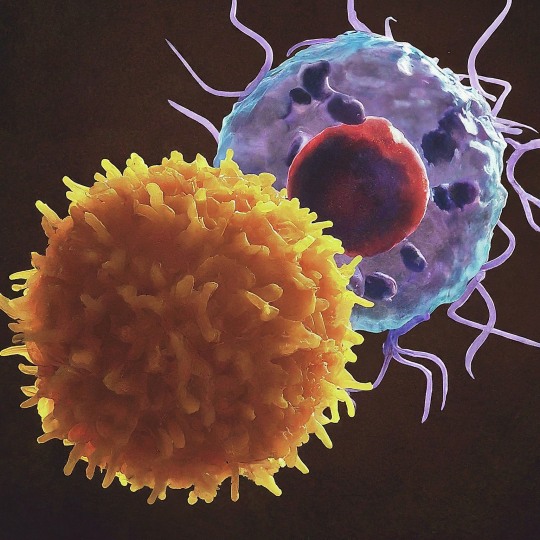
T cells are one of the important types of white blood cells of the immune system and play a central role in the adaptive immune response. Groups of specific, differentiated T cell subtypes have a variety of important functions in controlling and shaping the immune response. T cells are born from hematopoietic stem cells, found in the bone marrow. Developing T cells then migrate to the thymus gland to develop (or mature). After migration to the thymus, the precursor cells mature into several distinct types of T cells. T cell differentiation also continues after they have left the thymus. Groups of specific, differentiated T cell subtypes have a variety of important functions in controlling and shaping the immune response.
Endorphins are peptides produced in the brain that block the perception of pain and increase feelings of wellbeing. Endorphins are endogenous painkillers often produced in the brain and adrenal medulla during physical exercise or orgasm and inhibit pain, muscle cramps, and relieve stress.
#Thymus cell lymphocyte#Endorphins#poll#polls#tumblr poll#tumblr polls#vote#tournament poll#wikipedia#cells of the human body#science tournament#biochemistry
15 notes
·
View notes
Text



Leukemia and Lymphoma Awareness Flags!!
This flag was designed by us, as we currently have a family member with Leukemia and wish to bring awareness to this kind of cancer.
color meaning:
#FF2D34: Myeloma
#00DC0E: Non-Hodgkin Lymphoma
#FF8C2E: Leukemia
#D12DFF: Hodgkin Lymphoma
Below is information all about Leukemia and Lymphoma Cancers.
Leukemia and Lymphoma are both cancers that are not associated with a tumor. Lymphomas are cancers that affect the lymph system and start in cells called lymphocytes. Leukemia is a cancer of the early blood-forming tissues, including your bone marrow and lymph system.
There are many types of lymphoma. Some grow and spread slowly and some are more aggressive. There are two main types of Lymphoma:
1. Hodgkin Lymphoma is cancer that starts in the B lymphocytes (B cells) of the lymph system. Your lymph system helps you fight infection and control the fluids in your body.
2. Non-Hodgkin Lymphoma (NHL) is cancer that starts in the lymphocytes anywhere lymph tissue is found:
Lymph nodes
Spleen
Bone marrow
Thymus
Adenoids and tonsils, or
The digestive track.
Leukemia typically involves white blood cells, the cells that are your infection fighters. Leukemia can be divided into categories: fast growing (acute) and slow growing (chronic); and by which white blood cells are affected:
Acute lymphocytic leukemia (ALL)
Acute myelogenous leukemia (AML)
Chronic lymphocytic leukemia (CLL
Chronic myelogenous leukemia (CML)
A screening test is used to detect cancers in people who may be at higher risk for developing the disease. With leukemia and lymphoma, there are no early detection tests. The best way to find them is to be aware of the symptoms:
Swollen lymph nodes which can appear as a lump in the neck, armpit or groin;
Fever
Night sweats
Weight loss without trying, and
Fatigue.
Leukemia can have similar symptoms but also can include:
Easy bleeding or bruising;
Recurring nosebleeds; and
Bone pain or tenderness
Myeloma is cancer of the plasma cells. Plasma cells are white blood cells that produce disease- and infection-fighting antibodies in your body. Myeloma cells prevent the normal production of antibodies, leaving your body's immune system weakened and susceptible to infection. The multiplication of myeloma cells also interferes with the normal production and function of red and white blood cells. An abnormally high amount of these dysfunctional antibodies in the bloodstream can cause kidney damage. Additionally, the myeloma cells commonly produce substances that cause bone destruction, leading to bone pain and/or fractures.
Myeloma cells are produced in the bone marrow, the soft tissue inside your bones. Sometimes myeloma cells will travel through your blood stream and collect in other bones in your body. Because myeloma frequently occurs at many sites in the bone marrow, it is often referred to as multiple myeloma.
Signs and symptoms of myeloma include the following:
Hypercalcemia (excessive calcium in the blood)
Anemia (shortage or reduced function of red blood cells)
Renal damage (kidney failure)
Susceptibility to infection
Osteoporosis, bone pain, bone swelling, or fracture
High protein levels in the blood and/or urine
Weight loss
In 2022, more than 62,650 people are expected to be diagnosed with leukemia. In addition:
Leukemia accounts for 3.6% of all new cancer cases.
The overall 5-year survival rate for leukemia has more than quadrupled since 1960.
62.7% of leukemia patients survive 5 years or more.
The diagnosis of leukemia requires specific blood tests, including an examination of cells in the blood and marrow.
Treatment and prognosis depend on the type of blood cell affected and whether the leukemia is acute or chronic. Chemotherapy and blood and marrow transplant are often used to treat leukemia.
If you wish to read more about Leukemia and Lymphoma cancer, please visit this website!
#leukemia#lymphoma#blood cancer#leukemia and lymphoma society#leukemia awareness#lymphoma awareness#blood cancer awareness#pro endo#pro endogenic#endo friendly
7 notes
·
View notes
Text


LORE💥💥💥
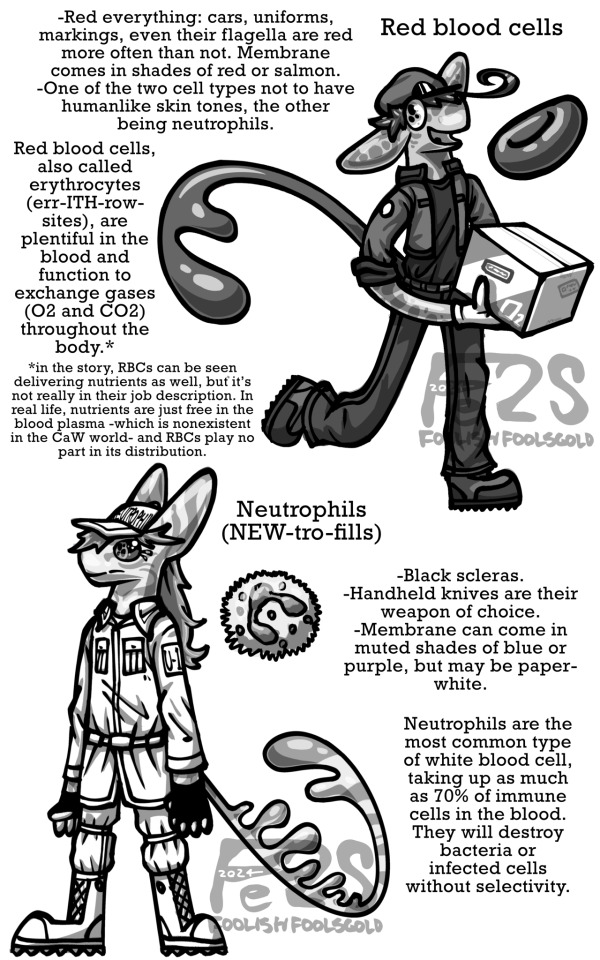
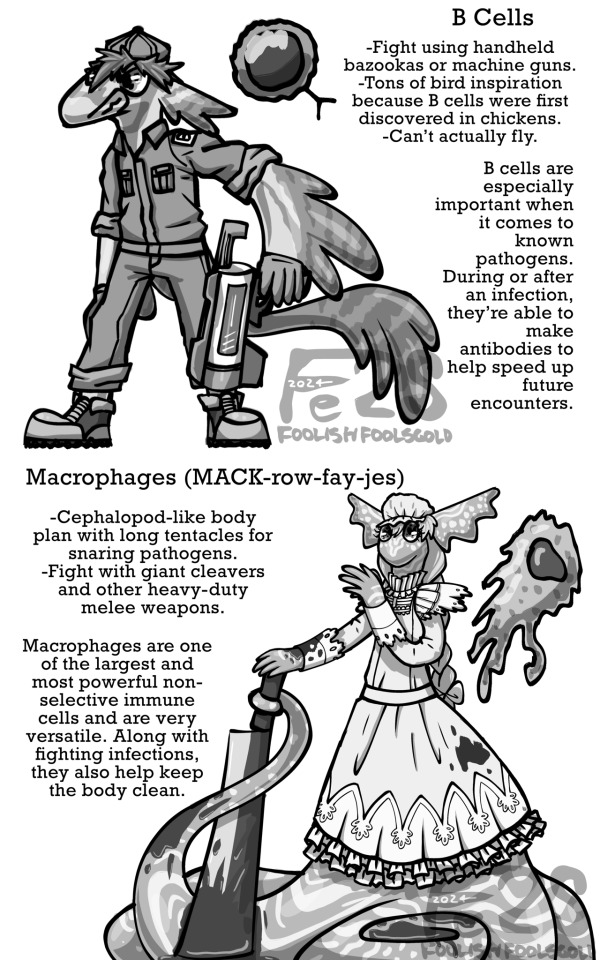
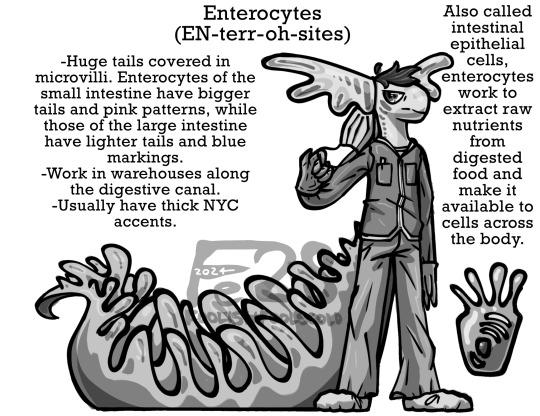
So I’m looking to get my fic printed when its done (and maybe but on a site too but we’ll see) and I have a big ass world building guide in there because I can’t be normal about anything! Here’s the section about common cell types that show up, all in black and white bc ooo official fancy. ID, mostly copy-pasted image text, below
[Start ID: first image showcases red blood cells and neutrophils alongside their real-life counterparts, reading “Red everything: cars, uniforms, markings, even their flagella are red more often than not. Membrane comes in shades of red or salmon. One of the two cell types not to have humanlike skin tones, the other being neutrophils. Red blood cells, also called erythrocytes (err-ITH-row-sites), are plentiful in the blood and function to exchange gases (02 and CO2) throughout the body. Then there’s an asterisk leading to: in the story, RBCs can be seen delivering nutrients as well, but it's not really in their job description. In real life, nutrients are just free in the blood plasma -which is nonexistent in the CaW world- and RBCs play no part in its distribution.” Reb blood cells have tails with two lobes at the end, long non frilled ears and their usual uniforms. For neutrophils, it says: “Black scleras. Handheld knives are their weapon of choice. Membrane can come in muted shades of blue or purple, but may be paper-white. Neutrophils are the most common type of white blood cell, taking up as much as 70% of immune cells in the blood. They will destroy bacteria or infected cells without selectivity.” Neutrophils also have their usual white uniforms and basic ears, but have skinnier tails with dorsal lobes.
The next image has killer T cells and neutrophils. Killer ts are anatomically similar to neutrophils but lack dorsal tail lobes. Text reads: “-Skinny tails with a pair of retractable stingers that can inject deadly perforin into victims. Markings are brown, black, or dark navy blue. Generally don't fight with weapons, prefer to use their tails or knee-jerk punches. Take their orders from helper T cells, who act as commanders. "Pack hunters" who form close bonds with their squadrons of about 6-10 cells, each led by an experienced squad leader. Killer Ts are lymphocytes born in the bone marrow and matured in the Thymus, where they face a rigorous selection process that primes them for targeted destruction of infected cells, cancer cells, and sometimes bacteria.” Eosinophils are also similar to neutrophils: “Wield two-pronged spears, the heads of which grow as proteins on the tips of their tails until they're ready to be changed out, keeping the weapon sharp and shiny. Pink uniforms and purple markings. Eyes have no scleras- the eye color, usually shades of purple, takes up the whole eye minus the pupils. Eosinophils aren't as swift as other non-selective WBCs with bacteria or viruses. They do, however, come into play during inflammation, allergic responses and parasitic infections.” The third image has B cells and macrophages. For B cells: “Fight using handheld bazookas or machine guns. Tons of bird inspiration because B cells were first discovered in chickens. Can't actually fly. B cells are especially important when it comes to known pathogens. During or after an infection, they're able to make antibodies to help speed up future encounters.” For macrophages, which have no legs and look a bit like Ursula body-plan wise, “Cephalopod-like body plan with long tentacles for snaring pathogens. Fight with giant cleavers and other heavy-duty melee weapons. Macrophages are one of the largest and most powerful non-selective immune cells and are very versatile. Along with nghting infections, they also help keep the body clean.” Next up are natural killer cells and dendritic cells. For NKs: “Four legs in a centauroid body plan. Green camo-style patterns. Have the most freedom of any immune cell when it comes to weapon choice. NK cells are "lone wolf" hunters who, like killer Ts, also use perforin stingers to take down all sorts of pathogens. They're not as supervised as killer Ts and act on their own judgement.” The bottom half of NK cells are clothed unlike traditional centaurs, and the top piece covers both the chest and front legs. For dendritic cells, “Also sport green markings. Generally calm and collected in the face of crisis. Often described as treelike, hence the plant features. Dendritic cells act as coordinators on the front lines of an infection. They also manage antigens (basically tangible memories of an attack that can set off a planned response in the future).” Lastly are enterocytes. Unlike in canon, they wear a scrub-like uniform with gloves and shoe bags. Also unlike previous cells, they have big frilled ears. Text reads: “Huge tails covered in microvilli. Enterocytes of the small intestine have bigger tails and pink patterns, while those of the large intestine have lighter tails and blue markings. Work in warehouses along the digestive canal. Usually have thick NYC accents. Also called intestinal epithelial cells, enterocytes work to extract raw nutrients from digested food and make it available to cells across the body.” End ID.]
#so much reused art I’m sorry#I’m working on more OC stuff#cells at work#hataraku saibou#my art#au#spec evo#speculative biology#speculative evolution
9 notes
·
View notes
Text
The T Cell Landscape
T cells, a critical component of the adaptive immune system, stand as the body's elite force in combatting infections and diseases. These specialized lymphocytes boast remarkable diversity, each type playing a distinct role in orchestrating a targeted and effective immune response.
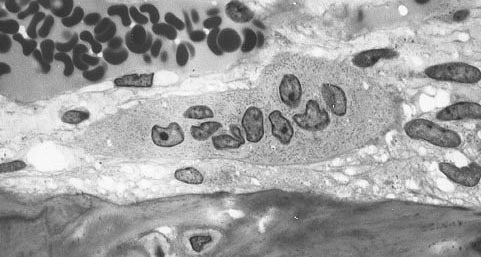
T cells, like all blood cells, originate from hematopoietic stem cells residing in the bone marrow. However, their training ground lies within the thymus, a specialized organ located in the chest. Here, they undergo a rigorous selection process known as thymocyte education. During this process, immature T cells, called thymocytes, are presented with self-antigens (molecules unique to the body) by special cells. Thymocytes that bind too strongly to these self-antigens are eliminated, preventing them from attacking healthy tissues later. Only thymocytes that demonstrate the ability to recognize foreign invaders while exhibiting tolerance to self are released into the bloodstream as mature T cells.
Following this rigorous training, mature T cells exit the thymus and embark on their patrol, circulating throughout the bloodstream and lymphatic system. They remain vigilant, constantly scanning for their specific targets – antigens. Antigens are foreign molecules, such as fragments of viruses, bacteria, or even cancerous cells, that trigger the immune response.
The hallmark of a T cell is its T cell receptor (TCR), a highly specialized protein complex embedded on its surface. This receptor acts like a lock, uniquely shaped to fit a specific antigen, the "key." Each T cell develops a unique TCR capable of recognizing only a single antigen, enabling a highly specific immune response.
But how do T cells encounter these hidden antigens lurking within infected or cancerous cells? This critical role is played by antigen-presenting cells (APCs). APCs, such as macrophages and dendritic cells, engulf pathogens or abnormal cells, break them down into smaller fragments (peptides), and present them on their surface complexed with major histocompatibility complex (MHC) molecules. MHC molecules act as identification tags, allowing T cells to distinguish between "self" and "non-self." When a T cell's TCR encounters its specific antigen bound to an MHC molecule on an APC, a dance of activation begins. The T cell becomes stimulated, and a cascade of signaling events is triggered. This leads to the T cell's proliferation, producing an army of clones specifically tailored to combat the recognized threat.
T cells are not a single, monolithic entity. They comprise a diverse population, each type with a specialized function:
Helper T Cells (Th Cells):
Helper T cells, often abbreviated as Th cells, play a central role in coordinating immune responses. They express the CD4 surface marker and can recognize antigens presented by major histocompatibility complex class II (MHC-II) molecules. Subtypes of helper T cells include Th1, Th2, Th17, and regulatory T cells (Tregs), each with distinct functions and cytokine profiles.
Th1 cells mediate cellular immunity by activating macrophages and cytotoxic T cells, crucial for defense against intracellular pathogens.
Th2 cells are involved in humoral immunity, promoting B cell activation and antibody production, thus aiding in defense against extracellular parasites.
Th17 cells contribute to the immune response against extracellular bacteria and fungi, producing pro-inflammatory cytokines. Regulatory T cells (Tregs) maintain immune tolerance and prevent autoimmunity by suppressing excessive immune responses.
Cytotoxic T Cells (Tc Cells):
Cytotoxic T cells, also known as Tc cells or CD8+ T cells, are effector cells responsible for directly killing infected or aberrant cells. They recognize antigens presented by MHC class I molecules on the surface of target cells. Upon activation, cytotoxic T cells release perforin and granzymes, inducing apoptosis in target cells and eliminating the threat.
Memory T Cells:
Memory T cells are a long-lived subset of T cells that persist after the clearance of an infection. They provide rapid and enhanced immune responses upon re-exposure to the same antigen, conferring immunological memory. Memory T cells can be either central memory T cells (TCM), residing in lymphoid organs, or effector memory T cells (TEM), circulating in peripheral tissues.
γδ T Cells:
Unlike conventional αβ T cells, γδ T cells express a distinct T cell receptor (TCR) composed of γ and δ chains. They recognize non-peptide antigens, such as lipids and metabolites, and are involved in immune surveillance at epithelial barriers and responses to stress signals.
Beyond the Battlefield: The Expanding Roles of T Cells: The remarkable capabilities of T cells have opened doors for several groundbreaking applications in medicine:
Vaccines: By presenting weakened or inactivated forms of pathogens, vaccines "train" the immune system to generate memory T cells. This prepares the body to recognize and rapidly eliminate the real pathogen upon future exposure, preventing disease.
Cancer immunotherapy: CAR T-cell therapy, a revolutionary approach, genetically engineers a patient's own T cells to express chimeric antigen receptors (CARs) that recognize and target specific cancer cells. These "supercharged" T cells are then reintroduced into the patient, unleashing a potent attack against the tumor.
Autoimmune disease treatment: Researchers are exploring ways to manipulate T cells to suppress harmful immune responses that underlie autoimmune diseases like rheumatoid arthritis and multiple sclerosis.
The diverse array of T cells underscores the immune system's complexity and adaptability in mounting tailored responses against a myriad of threats. From orchestrating immune reactions to maintaining tolerance and establishing long-term immunity, T cells play multifaceted roles in safeguarding the body's health. Understanding the intricacies of T cell biology not only sheds light on immune-mediated diseases but also paves the way for developing novel therapeutic strategies harnessing the power of the immune system.
T cells represent a fascinating aspect of immunology, with their diversity and specificity driving the complexity of immune responses. As research advances, further insights into T cell biology promise to revolutionize immunotherapy and enhance our ability to combat diseases ranging from infections to cancer. By understanding and harnessing their power, we can unlock new avenues for protecting and improving human health.
#science sculpt#life science#science#molecular biology#biology#biotechnology#artists on tumblr#t cells#T helper cells#autoimmune#autoimmunity#helathcare#immunology#immunotherapy#medical care#cancer#human health#research#scientific research#the glass scientists#scientific illustration#research scientist
11 notes
·
View notes
Text


On April 8th 1973 Glasgow University appointed Delphine Parrot as head of the Department of Bacteriology its first female professor in its 522 year history.
Born in London, Parrott graduated in 1949 with an honours BSc degree in Physiology from Bedford College, University of London. She undertook her PhD at King's College Hospital Medical School and graduated in 1952.
From 1952 to 1954 Parrott worked at the MRC Clinical Endocrinology Research Unit in Edinburgh, before returning to London to join the staff of the National Institute for Medical Research in Mill Hill. In 1960, she moved to the Imperial Cancer Research Fund in Mill Hill. She worked on the problems of immune (rejection) reactions to transplants and of the movement of blood cells, especially lymphocytes, involved in inflammation reactions. She also studied the immunology of leukaemia and the effects of the removal of the thymus on immune reactions.
On this day in 1973 Parrott was made Head of Department and later Gardiner Professor of Bacteriology (later known as the Gardiner Chair of Immunology).
Delphine Parrott retired in 1990. She died on 17th January 2016.
7 notes
·
View notes
Text

Anatomy and Physiology MCQ Question 361:- Question Link- https://examobjective.com/anatomy-and-physiology-mcq-set-44/ Maturation of T-cell lymphocytes takes place at…
(a) Thyroid (b) Thymus (c) Trachea (d) Liver
0 notes
Text
How Blood Cancer Affects the Immune System

Blood cancer, also known as hematologic cancer, is a group of diseases that originate in the blood-forming tissues of the body. These cancers can have profound effects on the immune system, compromising its ability to protect the body from infections and other threats. In this blog post, we’ll explore the intricate relationship between blood cancer and the immune system, from our expert blood cancer specialist in Surat at BCI- Blood and Cancer Institute about how these diseases disrupt our body’s natural defenses.
Understanding Blood Cancer
Before delving into the effects on the immune system, it’s crucial to understand what blood cancer is. Blood cancers primarily affect the production and function of blood cells. The three main types of blood cancer are:
Leukemia: Cancer of the blood and bone marrow
Lymphoma: Cancer of the lymphatic system
Myeloma: Cancer of the plasma cells
These cancers interfere with the normal production of blood cells, including white blood cells, red blood cells, and platelets. Each type of blood cancer affects the immune system differently, but all have significant impacts on the body’s ability to fight infections and maintain overall health.
The Immune System: Our Body’s Defense Mechanism
The immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful pathogens. Hemato oncologists from BCI, one of the best blood cancer hospital in Surat, explain the key components of the immune system:
● White blood cells (leukocytes)
● Lymph nodes and lymphatic vessels
● Bone marrow
● Spleen
● Thymus gland
White blood cells, particularly lymphocytes (T-cells and B-cells), play a crucial role in identifying and destroying foreign invaders like bacteria, viruses, and cancer cells.
How Blood Cancer Compromises the Immune System
According to the cancer specialists in Surat, blood cancers can severely impact the immune system in several ways:
Disruption of normal blood cell production: Blood cancers often start in the bone marrow, where blood cells are produced. This disruption leads to a decrease in the production of healthy white blood cells, red blood cells, and platelets. With fewer functional white blood cells, the body’s ability to fight infections is significantly reduced.
Overproduction of abnormal cells: In many blood cancers, the body produces an excess of abnormal blood cells. These cells don’t function properly and can crowd out healthy cells in the bone marrow and bloodstream. This overcrowding further weakens the immune system by reducing the space for healthy, functional immune cells.
Impaired lymphocyte function: Lymphomas and some leukemias directly affect lymphocytes, key players in the immune response. When these cells become cancerous, they can’t perform their normal functions of recognizing and attacking pathogens or abnormal cells.
Weakened barrier defenses: Some blood cancers can affect the skin and mucous membranes, which are the body’s first line of defense against pathogens. This can make it easier for harmful microorganisms to enter the body.
Treatment-related immunosuppression: The treatments used to combat blood cancers, such as chemotherapy and radiation therapy, can further weaken the immune system. These treatments often destroy both cancerous and healthy cells, including those of the immune system.
Specific Effects on Immune Function
Let’s look at how different types of blood cancer affect specific aspects of immune function:
Leukemia
Leukemia affects the production of white blood cells in the bone marrow. In acute leukemias, immature white blood cells (blasts) multiply rapidly, crowding out healthy cells. This leads to:
● Decreased production of normal, functional white blood cells
● Reduced ability to fight bacterial and fungal infections
● Increased risk of severe infections that can be life-threatening
Lymphoma
Lymphomas affect the lymphatic system, a crucial part of the immune system. This can result in:
● Impaired T-cell and B-cell function
● Reduced ability to produce antibodies
● Weakened defense against viruses and other intracellular pathogens
Multiple Myeloma
Multiple myeloma affects plasma cells, which are responsible for producing antibodies. This leads to:
● Decreased production of normal antibodies
● Increased susceptibility to bacterial infections
● Impaired ability to respond to vaccinations
Consequences of a Weakened Immune System
The compromised immune system while undergoing leukemia treatment in Surat can lead to various complications:
Increased risk of infections: Patients become more susceptible to common and opportunistic infections.
Prolonged recovery time: Even minor illnesses can take longer to resolve.
Reactivation of latent infections: Dormant viruses like herpes zoster (shingles) may resurface.
Increased risk of secondary cancers: The weakened immune system may be less effective at identifying and destroying other cancer cells.
Managing Immune System Challenges in Blood Cancer
Managing the impact of blood cancer on the immune system is a crucial part of blood cancer treatment in Surat. Strategies include:
● Prophylactic antibiotics to prevent infections
● Growth factors to stimulate blood cell production
● Immunoglobulin replacement therapy
● Vaccinations (when appropriate and safe)
● Careful monitoring and prompt treatment of infections
Conclusion
Blood cancer’s impact on the immune system is profound and multifaceted. By disrupting the normal production and function of blood cells, these cancers compromise the body’s ability to defend itself against a wide range of threats. Blood cancer specialists in Surat emphasize on understanding this relationship since it is crucial for developing effective treatments and supportive care strategies for blood cancer patients.
As research in this field progresses, new therapies are emerging that aim not only to combat the cancer itself but also to bolster and restore immune function. These advancements offer hope for improved outcomes and quality of life for those affected by blood cancers.
0 notes
Text
The Master Thymus Gland
The human body is an amazing complex deal! Did you know that the thymus gland is considered to be the “master of the immune system”? This gland is so important and is essential to the maturation and maintenance of the cells of the immune system. This great master is a pinkish-gray organ that lies below the thyroid gland and in the upper chest area (thorax) behind the breast bone (sternum). This little pinkish gland can do important work for a cancer patient or someone who is trying to recover from an illness.
Science has proven that as we age the thymus degenerates and doesn’t do the job it needs to do to help the immune system to fight off troubles. The thymus is most active during a child’s early life but as we reach puberty the gland starts to shrink and degenerate and is eventually replaced by connective tissue and fat. Since the thymus gland is such a large part of the immune system, this may explain why children bounce back so quickly from illnesses such as colds and we adults have to fight a cold with everything we have.
What Are The Functions Of The Thymus Gland?
Our immune system’s job is to protect the body against outside invasions such as parasites, viruses, bacteria, good cells that turn abnormal and much more. The master thymus gland produces mature lymphocytes to help maintain the surveillance of the army that circulates in the body and helps the army to stay alert and pay attention in order to quickly defend the body from harm. I would like to encourage you to investigate and learn more about your wonderful thymus gland because I believe that one day it will be fully understood how important this gland is to the human body.
Not too long ago doctors and scientist believed that after puberty, the function of the thymus gland was so decreased there was nothing one could do but suffer through what life gave you. It was just a normal process of aging. However, new science breakthroughs have proven the thymus gland can be regenerated to work like it was created too.
Be Careful When Buying Healthfood Store Thymus
There are many products on the market today that are said to rebuild the thymus gland. Beware! If you take a thymus extract be sure you know it is a good reputable company that manufactures it and that it comes from clean, non diseased animals. This is a glandular and you can not get glandular from plants.
Our doctors at New Hope Unlimited try to rebuild our patients thymus gland since it helps create and puts out such important immune system fighters. Remember, the thymus gland is the Master of the immune system and the immune system is our first and last defense system.
Dr Fredda Branyon.
0 notes
Text
TY Devices
-
The TY Devices are designed to release a frequency that stimulates the function of the thymus gland, the main organ of the lymphatic system and a crucial player in the immune system.
➡️These are used to optimize the thymus function, thus supporting and promoting the development of T-lymphocytes (T-cells - white blood cells that protect the body against foreign organisms such as bacteria and viruses).
Note: ANF Devices cannot be purchased individually, only through trained practitioners. Find the nearest one here: www.findANF.com.
#inflammation#wellness#physical therapy#pain therapy#anf therapy#injury#chronic pain#health#doctors#education#immune system#thymus gland#organs#lymphatic system#lymphatic drainage massage
0 notes
Text
Lymphoma Treatment cost in India
Lymphoma is a type of blood cancer that affects the lymphatic system. The disease develops in the lymphocytes, which are a kind of white blood cells. These blood cells play a key role in boosting the immune defence of the body and fighting against diseases. It is about 54 per cent of the total blood cancer cases found to be lymphoma.
Lymphatic System
A web of thin lymphatic channels, organs including the thymus and spleen and lymph nodes make up the lymphatic system.
Besides, it forms a vital part of the body’s immune system. Lymph, along with the lymph nodes, comprises white blood cells known as lymphocytes that help to defend against diseases. Most importantly, lymphocytes develop in the bone marrow that is discharged into the bloodstream after maturity. These cells go into the lymphatic system.
Types of Lymphoma/ Hodgkins Lymphoma (Hl)/ Non-Hodgkin’s Lymphoma (Nhl)
There are basically two types of lymphoma – Hodgkins Lymphoma (Hl) and Non-Hodgkin’s Lymphoma (Nhl).
Hodgkin Lymphoma: Hodgkin lymphoma, also known as Hodgkin’s disease, is a rare category of lymphoma. In simple words, it is a cancerous disease that develops in the lymphatic system. This type of lymphoma usually develops in the B-lymphocytes of the bone marrow. It begins when there is a drastic change in the lymphatic cells of the lymph system and leads to uncontrollable swells. Consequently, it turns into a tumour.
The Reed-Sternberg cells’ existence interprets Hodgkin’s lymphoma. The RS cells are abnormally bigger cells diagnosed in the blood samples of patients dealing with Hodgkin’s lymphoma.
Non-Hodgkin Lymphoma: The most common lymphoma type found, especially among older people, is Non-Hodgkin lymphoma (NHL), which refers to several types of lymph system cancer different from Hodgkin’s lymphoma. This cancerous disease indicates the absence of the Reed-Sternberg cells.
<<<Read More>>>
0 notes
Text
The effects of mycotoxin risk on poultry management
Effects of mycotoxins on poultry gut health
Aflatoxins
The disruption of intestinal barrier function
Poor intestinal cell proliferation and cell death
Compromised intestinal immunity.
Ochratoxins
Altered intestinal nutrient absorption.
Increased intestinal permeability.
Intestinal cell death
Decreased villi height.
T-2 toxin / DON
Poor intestinal water and glucose absorption (diarrhea)
Necrotic lesions in GIT
Shortening of intestinal villi (poor nutrient absorption)
Increased intestinal permeability (lowered tight junction proteins)
Decreased IL-8* cytokine (responsible for pathogen removal)
Decreased mucin production.
Fumonisins
Decreased cell viability and proliferation.
Altered intestinal barrier integrity by suppressing tight junction protein.
Increased intestinal permeability.
Increased mucin secretion/depletion of goblet cells
Altered gut immunity.
Effects of mycotoxins on poultry immune system
Aflatoxins
Increased gene expression of IL-6*, reduced complement and interferon, suppressed macrophagic phagocytosis, suppressed DTH, reduced weight of thymus and bursa, poor antibody titers, vaccination failures.
Ochratoxins
Regression of lymphoid organs, lymphocyte depletion, poor DTH*, and antibody response is affected to a lesser extent.
T-2 toxin
Regression of bursa of Farbricius, leucopenia, proteinemia, immunosuppression, increased disease incidences
DON
Interferes with DNA, RNA and protein synthesis, immunosuppression, poor antibody titers, increased disease incidences.
Fumonisins
Thymus atrophy, decreased spleen weight, increased susceptibility to E. coli and other bacteria.
Interleukin-6, DHT - Delayed-type hypersensitivity
For More Details : https://www.trouwnutritionasiapacific.com/en-in/
0 notes
Text
Propaganda!

An osteoclast is a type of bone cell that breaks down bone tissue. This function is critical in the maintenance, repair, and remodeling of bones of the vertebral skeleton.
T cells are one of the important types of white blood cells of the immune system and play a central role in the adaptive immune response. Groups of specific, differentiated T cell subtypes have a variety of important functions in controlling and shaping the immune response.
#tournament poll#polls#wikipedia#cells of the human body#science tournament#image description in alt#T cell#osteoclast
16 notes
·
View notes
Text
Understanding Blood Cancer: Symptoms, Diagnosis, And Management - Manipal Hospitals

Blood cancer is a broad term encompassing various malignancies that affect blood and bone marrow, casting a long shadow across the globe. This condition occurs when abnormal blood cells disrupt normal blood function and require prompt diagnosis and treatment. The incidence of blood cancer in India is on the rise necessitating awareness and proactive measures. While its presence can evoke fear and uncertainty, knowledge empowers both the patients and healthcare professionals to combat this complex disease with the required diagnosis approaches and timely interventions.
Synopsis
An Overview: Blood Cancer
Types of Blood Cancer
Causes of Blood Cancer
Early symptoms of blood cancer may include
Diagnosis and Tests
Management and Treatments
An Overview: Blood Cancer
Blood cancer arises from the uncontrolled growth of abnormal blood cells, affecting bone marrow, lymphatic system and blood cells that compromise immunity and vital functions. This disrupts the production of healthy red blood cells, white blood cells and platelets, leading to a cascade of health issues.
In India, the prevalence of blood cancer is significant, with thousands of new cases diagnosed annually. Despite the challenges, medical institutions like Manipal Hospitals are equipped with state-of-the-art facilities and expertise to address blood cancer effectively, enhancing the chances of recovery and quality of life for patients.
Types of Blood Cancer
Blood cancer encompasses several types, including many subtypes. They are
Leukaemia- This is the most common cancer among young adults and also children. It usually affects the white blood cells and it can be acute and chronic.
Lymphoma-This type of cancer originates in the lymphatic system, which is part of the body's germ-fighting network.
The lymphatic system includes the lymph nodes (lymph glands), spleen, thymus gland and bone marrow. Lymphoma can affect all those areas as well as other organs throughout the body.
Myeloma- Myeloma poses a detrimental impact on plasma cells in the bone marrow, leading to severe bone damage and critical kidney problems.
Each type of cancer presents district characteristics and requires treatment approaches.
Causes of Blood Cancer
Blood cancer stems from mutated DNA in blood cells, causing abnormal growth and crowding out healthy cells. While the exact cause remains unclear, several factors are suspected:
Leukaemia: Genetic and environmental triggers, potentially involving chromosomal aberrations, may lead to uncontrolled cell growth.
Lymphoma: Gene mutations in lymphocytes cause them to multiply excessively and evade natural cell death. Infections or weakened immunity might play a role. Certain Virus Infections also cause Lymphoma.
Myeloma: Plasma cell mutations cause uncontrolled reproduction, with potential links to chromosomal changes affecting growth control genes.
Early Blood Cancer Symptoms may include:
Persistent fatigue
Unexplained weight loss
Frequent infections
Easy bruising or bleeding
Swollen lymph nodes
Bone pain or tenderness

Diagnosis and Tests
Diagnosing blood cancer involves a series of tests and evaluations to confirm the presence of abnormal blood cells and determine the specific type and severity of the disease. Key diagnostic approaches include:
0 notes
Text
Non-Hodgkin's lymphoma (NHL) is a type of cancer that originates in the lymphatic system, which is a part of the body's immune system. It involves the abnormal growth of lymphocytes, a type of white blood cell, and it can occur in various parts of the body where lymph tissue is found, such as lymph nodes, spleen, bone marrow, and other organs.
Non-Hodgkin's lymphoma encompasses a diverse group of cancers, with many different subtypes, each with its own characteristics, behaviors, and treatments. Symptoms of NHL can include swollen lymph nodes, fever, night sweats, weight loss, fatigue, and other nonspecific symptoms.
Treatment options depend on the subtype, stage, and individual factors of the patient, and may include chemotherapy, radiation therapy, immunotherapy, targeted therapy, or stem cell transplantation. Early diagnosis and appropriate treatment can improve the prognosis for many patients with NHL.
Symptoms of Non-Hodgkin's lymphoma (NHL) can vary depending on the subtype of the disease and the organs involved.
However, common symptoms may include:
Swollen lymph nodes, which may or may not be painful, typically in the neck, armpits, or groin.
Fever without an obvious cause.
Night sweats, often severe enough to soak through clothing and bedding.
Unexplained weight loss.
Fatigue and weakness.
Persistent itching.
Enlargement of the spleen or liver, which may cause abdominal discomfort or fullness.
Chest pain, coughing, or difficulty breathing if the lymphoma affects the thymus or lymph nodes in the chest.
Bone pain or fractures if the lymphoma affects the bones.
Yes, lymphomas, including Non-Hodgkin's lymphoma (NHL), can recur after treatment. Recurrence refers to the return of cancer cells after a period of remission or apparent absence of the disease.
The risk of recurrence varies depending on several factors, including the specific subtype of lymphoma, the stage of the disease at diagnosis, the type of treatment received, and individual patient characteristics.
Some lymphoma subtypes have a higher likelihood of recurrence than others. Factors that may increase the risk of recurrence include:
Inadequate initial treatment: If the lymphoma is not fully eliminated during initial treatment, residual cancer cells may remain and lead to recurrence.
Aggressive or refractory lymphoma: Certain types of NHL, particularly those with aggressive features or resistance to treatment, have a higher risk of recurrence.
Stage of the disease: Lymphomas diagnosed at advanced stages (stages III and IV) generally have a higher risk of recurrence compared to those diagnosed at earlier stages.
High-risk features: Specific genetic mutations, abnormal protein expression, or other high-risk features identified during diagnosis may increase the likelihood of recurrence.
Immune system status: Patients with weakened immune systems, such as those undergoing immunosuppressive therapy or with certain medical conditions, may be more susceptible to lymphoma recurrence.
Time since remission: Recurrence can occur months or years after achieving remission, although the risk generally decreases over time.
Regular follow-up appointments with healthcare providers are important for monitoring for signs of recurrence, such as the return of symptoms or abnormal findings on imaging tests. Early detection of recurrence allows for timely intervention and appropriate treatment adjustments to manage the disease effectively.
In some cases, additional treatment modalities, such as salvage chemotherapy, radiation therapy, immunotherapy, or stem cell transplantation, may be recommended to address recurrent lymphoma.
Get best treatments for cancer at best hospitals in India, also get a full body health checkup at best hospitals.
#health#health checkup#full body health checkup#cancer#chemotherapy#radiation#adaptive radiation#non hodgkin lymphoma#hodgkin lymphoma
0 notes
Text
Peripheral T cell activation, not thymic selection, expands the T follicular helper repertoire in a lupus-prone murine model
Many autoimmune diseases are characterized by the activation of autoreactive T cells. The T cell repertoire is established in the thymus; it remains uncertain whether the presence of disease-associated autoreactive T cells reflects abnormal T cell selection in the thymus or aberrant T cell activation in the periphery. Here, we describe T cell selection, activation, and T cell repertoire diversity in female mice deficient for B lymphocyte-induced maturation protein (BLIMP)-1 in dendritic cells... http://dlvr.it/Sz5XXD
0 notes
Text
Lymphatic System
2. COMPONENTS OF THE LYMPHATIC SYSTEM
The lymphatic system consists of a fluid (lymph), vessels that transport the lymph, and organs that contain lymphoid tissue.
LYMPH
Lymph is a fluid similar in composition to blood plasma. It is derived from blood plasma as fluids pass through capillary walls at the arterial end. As the interstitial fluid begins to accumulate, it is picked up and removed by tiny lymphatic vessels and returned to the blood. As soon as the interstitial fluid enters the lymph capillaries, it is called lymph. Returning the fluid to the blood prevents edema and helps to maintain normal blood volume and pressure.
LYMPHATIC VESSELS
Lymphatic vessels, unlike blood vessels, only carry fluid away from the tissues. The smallest lymphatic vessels are the lymph capillaries, which begin in the tissue spaces as blind-ended sacs. Lymph capillaries are found in all regions of the body except the bone marrow, central nervous system, and tissues, such as the epidermis, that lack blood vessels. The wall of the lymph capillary is composed of endothelium in which the simple squamous cells overlap to form a simple one-way valve. This arrangement permits fluid to enter the capillary but prevents lymph from leaving the vessel.
ILLUSTRATION OF LYMPHATIC CAPILLARIES IN THE TISSUE SPACES

The microscopic lymph capillaries merge to form lymphatic vessels. Small lymphatic vessels join to form larger tributaries, called lymphatic trunks, which drain large regions. Lymphatic trunks merge until the lymph enters the two lymphatic ducts. The right lymphatic duct drains lymph from the upper right quadrant of the body. The thoracic duct drains all the rest.
Like veins, the lymphatic tributaries have thin walls and have valves to prevent backflow of blood. There is no pump in the lymphatic system like the heart in the cardiovascular system. The pressure gradients to move lymph through the vessels come from the skeletal muscle action, respiratory movement, and contraction of smooth muscle in vessel walls.
LYMPHATIC ORGANS
Lymphatic organs are characterized by clusters of lymphocytes and other cells, such as macrophages, enmeshed in a framework of short, branching connective tissue fibers. The lymphocytes originate in the red bone marrow with other types of blood cells and are carried in the blood from the bone marrow to the lymphatic organs. When the body is exposed to microorganisms and other foreign substances, the lymphocytes proliferate within the lymphatic organs and are sent in the blood to the site of the invasion. This is part of the immune response that attempts to destroy the invading agent.
THE LYMPHATIC ORGANS INCLUDE:
Lymph Nodes
Tonsils
Spleen
Thymus
0 notes