#Symptoms of Mitral Valve
Explore tagged Tumblr posts
Text
Me: *gets my test in which I am supposed to give a diagnosis to a patient*
My patient: *Has ALL of the textbook symptoms of TWO DIFFERENT HEART ISSUES, a bunch of general symptoms that can be attributed to both of them, and a HEART ATTACK in history, which can cause one, but not the other, but both of them can lead to each other, and there's literally ZERO INDICATION which one is the main one*
Me: WHAT AM I SUPPOSED TO DO WITH THIS?!!?!?!!!
#HOW ARE YOU EXPECTING ME TO GIVE A FINAL DIAGNOSIS WHEN I HAVE NO INFO TO DIFFERENTIALLY DIAGNOSE WHO'S THE PROBLEM#I CAN'T DO THIS. ISCHEMIA CAUSING MITRIAL STENOSIS AND MISTRIAL STENOSIS WITH ADDITIONAL ISCHEMIA SYMPTOMS ARE TWO DIFFERENT THINGS#I CAN'T TELL YOU A DIAGNOSIS WITHOUT KNOWING WHICH PART OF THE HEART BROKE FIRST#(it was more of a question of 'who do we blame the CRVF on' and I did put stenosis as the main one but still)#also I should never listen to my groupmates because one of them threw me off even more by saying that right ventricular failure because of#Mitral valve stenosis can't happen. it CAN. it DOES.#what a total failure of a day honestly#med school diaries#med school shenanigans#med school stuff#med school#med student
2 notes
·
View notes
Text
God I swear I’m not trying to be all doom and gloom talking about my health I know it’s annoying I just really need a break and everyone irl is already done with my shit bc I’ve been too anxious to go back to the doctor bc the last one told me I’d just have to deal with it and potentially get more surgeries and I’m 23 dude. It took nearly 3 years before my doctor even agreed that that surgery was necessary and it didn’t even fully fix my shit it just lessened the pain — which I’m grateful for, don’t get me wrong! But I haven’t had full limb function in my left arm since I was 15 and they made it sound like the surgery would fix it and then acted like I was overreacting when it didn’t. And my left leg has been deeply fucked for nearly as long, and at least slightly fucked at least since I hit double digits, and has gotten progressively worse. So like I know, I get it that I need to go to a doctor, but why would it go better now? What’s going to make a doctor take me seriously now?
I want to be angry, but I’m too tired.
#chronic health#chronic pain#cpunk#cripple punk#tw surgery#I was told (in a nonprofessional capacity) that I should be screened for ehlers danlos syndrome#which matches a lot of my symptoms#and my parental units want me to get screened for pots#and a heart murmur#and mitral valve prolapse#and asthma but I’ve been tested for that within the last 5 or 6 years and seem to be fine in that regard at least#I don’t want to keep doing this man#I would really like to be healthy#I miss ballet a fuckton#and martial arts#and just being able to go places with my friends without having to plan out how to avoid fainting or pain flares#maybe hEDS#I don’t want to clutter up the actual tags with my hypothetical shit#tw vent#fever’s vibe check#feverdreamsandlucidnightmares
4 notes
·
View notes
Text
0 notes
Text
I wonder if that geneticist I saw who’s supposedly a foremost authority on EDS would diagnose me now that I’ve lost a lot of weight and the hyperextension in my joints (particularly my knees) is a lot more obvious.
All of that plus the ‘tism, the GI problems, the hiatal hernia, the mitral valve regurgitation, the POTS symptoms, etc. etc. like what else could it be lmao. Genuinely what the fuck else could it be.
12 notes
·
View notes
Note
Hey Joy, this isn't a question so much as a way for me to convince myself I'm not a hypochondriac, lol. Lately, I've been experiencing symptoms of fatigue, brain fog or memory issues, light-headedness, etc, that are uncommon for my age (30). I have related disorders such as anemia, anxiety, & ADHD that may be contributing to these symptoms, although they seem to have gotten worse or appear more frequently now than when I was initially diagnosed with those disorders. My work allows me to read & interact with disabled people with rare diseases, so I often find similarities with their medical issues. At first, I thought this was all just burnout or something related to the lockdown during COVID. I just saw my doctor and had blood work done to check my levels, and I may have a heart condition (tachycardia, mitral valve prolapse). I've fallen asleep at work before because I can't keep my eyes open, even after a full 8 hours of sleep. I can get dizzy from standing up too fast & can't seem to be on my feet for very long without discomfort & pain (I used to work retail, how did I ever do it?). I've researched some of my symptoms and found ME/CFS and POTS as possible conditions. Do you think it's a possibility I have these, or is it just my anxiety? Thank you! (P.s. Hunger Pangs is on my tbr!)
I obviously cannot tell you with any certainty what is wrong--and I am glad you are seeing doctors about it already and may have possible answers wrt tachycardia and the mitral valve.
What I will say is that there are many types of dysautonomia, of which POTS is one, and that what you are describing sounds very familiar to me as someone with two known types of dysautonomia.
The fact that this is hampering your quality of life to the point where you fall asleep at work, are unable to stand without getting dizzy, and are experiencing chronic pain, is enough of a reason to pursue further testing for things like dysautonomia and, yes, possibly even ME/CFS though given your history of anemia, I'm inclined more toward dysautonomia because the two often go hand in hand.
Also, it is normal to feel anxiety experiencing these types of symptoms. Even if it turns out to be a symptom of your anxiety, doesn't make the experiences any less real and debilitating, and you deserve treatment that will help improve your quality and comfort of life. And there is treatment and things you can do that will make you feel better. Getting your anemia under control should be a top priority if it isn't already. Mines was allowed to go untreated for years until we found out my iron anemia was being caused by pernicious anemia (b12 deficiency), and the iron anemia I'd been plagued with since birth suddenly cleared up.
Years and years of blood transfusions and infusion treatments, and the whole time I needed b12. Who knew? Certainly not my old doctors.
Anyway. If your symptoms are at the point where you are recognizing yourself in things like POTS? It's time to pursue that with your doctor. Don't put it off because you think it's not that bad or others have it worse. Everyone deserves to feel well.
Good luck.
200 notes
·
View notes
Text
mom looked up ehlers-danlos symptoms and said "mitral valve prolapse.... that's exactly what your dad had" so um. checking it off the list 👍
5 notes
·
View notes
Text
Entry #012
Hypermobility
A problem many autistic fellows of mine, including me, are suffering from is hypermobility. It's a underdiagnosed, underrecognized part of autism.
I personally deal with Ehlers-Danlos Syndrome (EDS), which runs in my family. My great-grandmother, grandmother, and mother all have it, and so do I. It comes with a host of symptoms: atrophic scars, mitral valve insufficiency, postural / orthostatic tachycardia syndrome, gastric motility disorder, pelvic and bladder dysfunction, extremely soft and stretchy skin, and, of course, extreme hypermobility. I can bend my joints in ways that I only learned in medical school was abnormal, and I’ve often felt like a bit of a freak during skills practices. I remember asking an orthopaedic surgeon during training why people couldn’t do 90 degrees flexion and extension with their forefeet, only to be met with confusion. When I demonstrated what I meant, the look on his face was one of pure astonishment. This highlights how different our experiences can be and how misunderstood they often are.
One of the most frustrating parts is not being taken seriously by some doctors. I’m lucky to have a medical degree and trusted colleagues I can consult, but many autistic individuals don’t have this luxury. Too often, our symptoms are dismissed or attributed to our mental health, leading us to delay seeking help until things get really bad. Please, don’t wait. The longer you put off seeing a doctor, the harder it becomes to treat your symptoms. Find a physician who listens and takes you seriously. Hypermobility doesn't necessarily mean you have EDS, but hypermobile or not, moving and living isn’t easy. Chronic exhaustion is real and debilitating. I touched on managing energy levels in entry #003 with routines based on my modified spoon theory, which I call the cutlery theory. I’ll dive deeper into this in a future post.
Living with hypermobility means constant joint pain, frequent dislocations, and early arthritis. I’ve never known a pain-free day, and overdoing it physically just makes things worse. Recovery takes time, and I’m still figuring out if physical and mental fatigue recover together or separately. Overstraining definitely not only impacts physical, but also my mental state. Not everyone can access rehabilitation programs, but there are steps you can take on your own to make it a little easier or better. Start by tracking your symptoms to identify patterns. This can help you find ways to support yourself. Working with a physiotherapist or occupational therapist is ideal, but you can also use trial and error to find what works for you. I’m always here to brainstorm and offer support.
I’m a big believer in creative therapy. One exercise is to color in a body image to show where you feel comfortable, uncomfortable, or in pain. This helps you and your healthcare providers understand your condition better and develop a personalised treatment plan.
Also, braces can be a lifesaver for dislocated or overstretched joints, even though I hate wearing them. They help prevent further injury and aid in recovery. Despite the awkward looks and comments, they’re definitely worth it.
In conclusion, hypermobility is often a comorbidity of autism. It can cause mental fatigue and chronic pain, among other symptoms. Don’t suffer in silence, but find ways to accommodate yourself and make life easier. Medication and surgery aren’t always the answers, although they can help. Awareness and lifestyle adjustments can make a big difference too. Talk to your physician, physiotherapist, occupational therapist, and fellow patients to find what works for you.
#autism#autistic#high functioning autism#autistic spectrum#autism spectrum disorder#autistic adult#autistic community#actually autistic#autistic things#being autistic#autistic experiences#unmasking autism#high masking autism#hypermobility#hypermobile ehlers danlos#hypermobile eds#hypermobile spectrum disorder#chronic fatigue#mental fatigue#chronically fatigued
16 notes
·
View notes
Text
i kind of scared the new hire today (oops)
we were swapping medical lore, and i mentioned my scarlet fever and lack of antibiotics growing up, etc. her healthcare background is even more extensive than mine, so she immediately recognized the potential complications and asked me if i had a heart murmur (she specifically mentioned the mitral valve, hell yeah). i explained yes, and that it's gotten worse per my last physical 2 years ago, but no cardiologists that i've talked to thus far take our insurance. so i can't get in for an echocardiogram to see if i actually need surgery, but everything i read about rheumatic fever/rheumatic heart disease matches my symptoms.
she looked aghast and asked me how i'm not worried all the time and desperately trying to figure out how to pay for an echo. i told her i decided not to stress too much because even if an echo shows i need surgery, i couldn't afford it anyway, not with our current coverage. all it would do is confirm death is coming for me young, which i've always known and been fine with. she was mildly appalled by this, but thankfully, still thinks i am cool and a good teacher. so that's a relief lol
#listen my mom's anti vax phase resulted in more than one brush with death#just for me my other 3 siblings alive for that phase were fine#but that and to going to funerals nonstop when i was little bc the alcoholism was catching up with my dad's side#means that i feel very comfortable with the thought of death and always have#typical southern experience#probably a typical white trash experience regardless of region#blog#medical cw
11 notes
·
View notes
Text
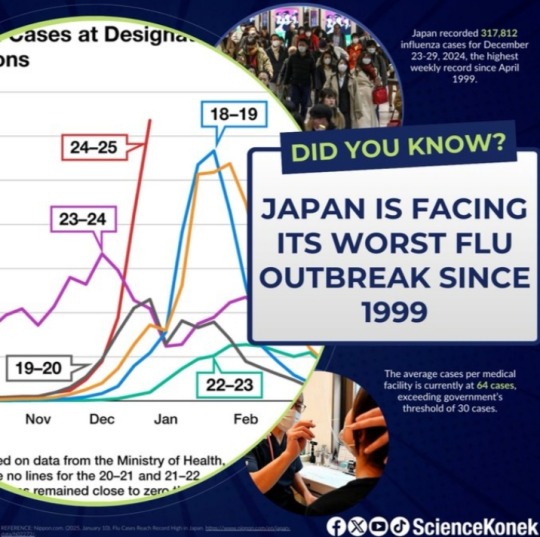
𝗝𝗮𝗽𝗮𝗻 𝗶𝘀 𝗲𝘅𝗽𝗲𝗿𝗶𝗲𝗻𝗰𝗶𝗻𝗴 𝗶𝘁𝘀 𝘄𝗼𝗿𝘀𝘁 𝗳𝗹𝘂 𝗼𝘂𝘁𝗯𝗿𝗲𝗮𝗸 𝘀𝗶𝗻𝗰𝗲 𝟭𝟵𝟵𝟵 😷
At the end of 2024, Japan recorded an unprecedented 𝟯𝟭𝟳,𝟴𝟭𝟮 𝗶𝗻𝗳𝗹𝘂𝗲𝗻𝘇𝗮 𝗰𝗮𝘀𝗲𝘀, as reported by the country’s Ministry of Health, Labor and Welfare, its highest number of cases since 1999.
In terms of average cases per medical institution, it now reached 𝟲𝟰.𝟯𝟵 𝗰𝗮𝘀𝗲𝘀, exceeding both the government's warning threshold of 30 cases and previous high of 57.09 cases in January 2019.
The 𝘄𝗼𝗿𝘀𝘁 𝗵𝗶𝘁 𝗶𝘀 𝘁𝗵𝗲 𝗢𝗶𝘁𝗮 𝗣𝗿𝗲𝗳𝗲𝗰𝘁𝘂𝗿𝗲 𝗶𝗻 𝘄𝗲𝘀𝘁𝗲𝗿𝗻 𝗝𝗮𝗽𝗮𝗻, recording 104.84 average cases, followed by the other prefectures in the Kyushu region.
There are several factors that led to this massive influenza outbreak in Japan.
According to Osaka University’s Satoshi Kutsuna, a professor of epidemiology, the 𝗳𝗹𝘂 𝘀𝗲𝗮𝘀𝗼𝗻 𝘀𝘁𝗮𝗿𝘁𝗲𝗱 𝗲𝗮𝗿𝗹𝘆 𝗶𝗻 𝗡𝗼𝘃𝗲𝗺𝗯𝗲𝗿 𝟮𝟬𝟮𝟰 and has been in increasing trend ever since.
There are also signs of decreasing herd immunity. During the pandemic, widespread mask-wearing and rigorous hand hygiene significantly reduced influenza transmission.
However, 𝗮𝘀 𝘁𝗵𝗲𝘀𝗲 𝗺𝗲𝗮𝘀𝘂𝗿𝗲𝘀 𝘄𝗲𝗿𝗲 𝗿𝗲𝗹𝗮𝘅𝗲𝗱 𝗮𝗻𝗱 𝗶𝗻𝘁𝗲𝗿𝗻𝗮𝘁𝗶𝗼𝗻𝗮𝗹 𝘁𝗿𝗮𝘃𝗲𝗹 𝗿𝗲𝘀𝘂𝗺𝗲𝗱, 𝘀𝘂𝘀𝗰𝗲𝗽𝘁𝗶𝗯𝗶𝗹𝗶𝘁𝘆 𝘁𝗼 𝗶𝗻𝗳𝗹𝘂𝗲𝗻𝘇𝗮 𝗶𝗻𝗰𝗿𝗲𝗮𝘀𝗲𝗱.
Influenza can lead to severe complications such as viral pneumonia and secondary bacterial infections, most especially in 𝘆𝗼𝘂𝗻𝗴 𝗰𝗵𝗶𝗹𝗱𝗿𝗲𝗻, 𝘁𝗵𝗲 𝗲𝗹𝗱𝗲𝗿𝗹𝘆, 𝗮𝗻𝗱 𝗶𝗺𝗺𝘂𝗻𝗼𝗰𝗼𝗺𝗽𝗿𝗼𝗺𝗶𝘀𝗲𝗱 𝗶𝗻𝗱𝗶𝘃𝗶𝗱𝘂𝗮𝗹𝘀.
To prevent complications due to influenza, it’s important to always 𝗽𝗿𝗮𝗰𝘁𝗶𝗰𝗲 𝗴𝗼𝗼𝗱 𝗵𝘆𝗴𝗶𝗲𝗻𝗲, 𝘄𝗲𝗮𝗿 𝗺𝗮𝘀𝗸𝘀 especially while in crowded places, 𝗴𝗲𝘁 𝘃𝗮𝗰𝗰𝗶𝗻𝗮𝘁𝗲𝗱, and 𝘀𝗲𝗲𝗸 𝗲𝗮𝗿𝗹𝘆 𝘁𝗿𝗲𝗮𝘁𝗺𝗲𝗻𝘁 once experiencing influenza-like symptoms.
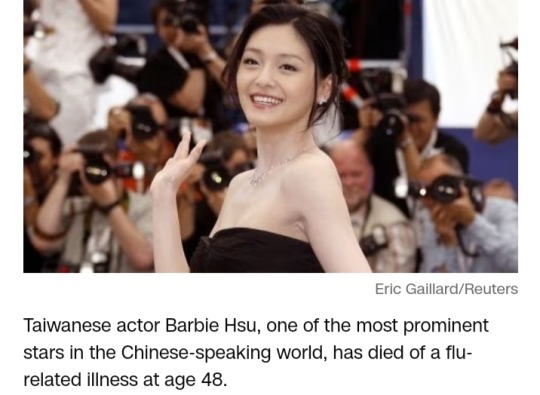
Yesterday, the world was shocked after learning the news about the unfortunate death of Taiwanese star Barbie Hsu due to influenza-induced pneumonia.
She was on vacation to celebrate the holidays in Tokyo.
According to Kyodo News, Hsu previously revealed that she had a history of mitral valve prolapse and epilepsy. She was 48.
𝗥𝗲𝘀𝘁 𝗶𝗻 𝗽𝗮𝗿𝗮𝗱𝗶𝘀𝗲, 𝗕𝗮𝗿𝗯𝗶𝗲 𝗛𝘀𝘂 (1976-2025), 𝗼𝘂𝗿 𝗱𝗲𝗮𝗿 𝗦𝗵𝗮𝗻 𝗖𝗮𝗶 𝗳𝗿𝗼𝗺 𝗠𝗲𝘁𝗲𝗼𝗿 𝗚𝗮𝗿𝗱𝗲𝗻. 🕊️
4 February 2025
✍️ Jan Luis Antoc
#japan#flu#influenza#pneumonia#oita prefecture#influenza outbreak#flu season#herd immunity#viral pneumonia#secondary bacterial infections#good hygiene#wear face masks#𝗲𝗮𝗿𝗹𝘆 𝘁𝗿𝗲𝗮𝘁𝗺𝗲𝗻𝘁#get vaccinated#flu shot#barbie hsu#shan cai#meteor garden#taiwan#taiwanese actress#health news#medical update
2 notes
·
View notes
Note
Hi, I saw ur EDS post and was wondering what your symptoms are? I also have rather severe EDS, and I was just curious. You don’t have to tell me! No pressure :) /gen
- 🦓
Honestly it'd be easier to list the symptoms I don't have LMAOOOO but I am more than happy to share!
Head to Toe, Internal and External, here we go!
(in no specific order)
-hearing loss
-joint hypermobility and instability (both major and minor joints), limb bowing, and slipping ribs
-atrophic scarring, poor healing, and generally fragile skin (easy bruising, bandaids irritate my skin and medical tape can tear it; its also velvety to touch)
-kyphoscoliosis (i think i may also have craniocervical instability which causes its own symptoms, similar to POTS if not POTS), also i'm super short. Before scoliosis I would've been about 5'0", but it stole my height in highschool so I'm 4'8" on a good day.
-Mitral Valve Prolapse
-muscle weakness and hypotonia (also atrophy as I've been out of PT)
Now for dysautonomia, things that are indirectly caused/directly affected by my EDS
-Digestive issues like IBS-A and Gastroparesis, also GERD (fun fact: my esophagus curves with my spine 😭)
-POTS (postural orthostatic tachycardia syndrome)
-Migraines and Tension headaches in my neck (my head is quite literally too heavy sometimes)
-Osteoarthritis from severe/frequent dislocations
I usually hate trying to list everything bc it's so much that it seems fake, like I WISH I were making up the amount of stuff constantly going on with my body, it is so much some days it gets overwhelming.
I do however think it's funny to say the forces that be in the universe had to nerf me or I would have been to powerful bc I am one anarchy lovin motherfucker, but no chance I can do anything about it tho 💀
#ehlers danlos syndrome#chronically ill#chronic illness#EDS is a full time job#BLESS my mom who lets me talk about it to her (she is the person who makes my doc appts and is usually the one to help me around the house)
12 notes
·
View notes
Text

TYPES OF HEART DISEASE
Heart disease encompasses a wide range of cardiovascular problems. Various conditions fall under the heart disease umbrella, each affecting the heart or blood vessels in distinct ways. Understanding these types can help in recognizing symptoms early and seeking appropriate treatment. This article explores the primary types of heart disease, their causes, and potential treatments.
1. Coronary Artery Disease (CAD)
Overview:
Coronary Artery Disease is the most common type of heart disease. CAD occurs when the coronary arteries, responsible for supplying blood to the heart muscle, become hardened and narrowed due to the buildup of cholesterol and other materials, known as plaque, on their inner walls. This process is called atherosclerosis.
Symptoms:
Chest pain (angina)
Shortness of breath
Fatigue
Treatment:
Treatments include lifestyle changes, medication, and possibly procedures like angioplasty or coronary artery bypass grafting (CABG).
2. Heart Arrhythmias
Overview:
Arrhythmias are irregular heartbeats. The heart can beat too fast (tachycardia), too slow (bradycardia), or irregularly. This can be due to a fault in the heart’s electrical system.
Symptoms:
Palpitations
Dizziness
Fainting
Treatment:
Treatment might involve medications, lifestyle adjustments, and in some cases, implantable devices like pacemakers or procedures like catheter ablation.
3. Heart Valve Disease
Overview:
The heart contains four valves: the tricuspid, pulmonary, mitral, and aortic valves. These valves open and close to direct blood flow through the heart. Valve disease occurs when one or more of these valves do not function properly.
Symptoms:
Fatigue
Swollen ankles or feet
Shortness of breath
Treatment:
Treatment may include medication, surgical repair, or valve replacement depending on the severity and specific type of valve disease.
4. Congestive Heart Failure (CHF)
Overview:
Heart failure, sometimes known as congestive heart failure, occurs when the heart can’t pump blood as well as it should. This can result from any condition that damages the heart muscle, including CAD, high blood pressure, and heart valve disease.
Symptoms:
Shortness of breath
Persistent coughing or wheezing
Swelling in legs, ankles, and feet
Treatment:
Managing heart failure involves a combination of lifestyle changes, medications, and possibly surgery or devices like ventricular assist devices (VADs) or implantable cardioverter-defibrillators (ICDs).
5. Cardiomyopathy
Overview:
Cardiomyopathy refers to diseases of the heart muscle. These diseases enlarge or make the heart muscle rigid and more prone to arrhythmias.
Symptoms:
Breathlessness
Swelling of the legs
Fatigue
Treatment:
Treatment focuses on controlling symptoms and may include medications, lifestyle modifications, or devices to help the heart pump more effectively.
6. Congenital Heart Defects
Overview:
Congenital heart defects are structural problems with the heart present from birth. They can involve the walls of the heart, the valves of the heart, and the arteries and veins near the heart.
Symptoms:
Symptoms vary widely and can include cyanosis (a bluish tint to the skin, lips, and fingernails), breathing difficulties, and fatigue.
Treatment:
Treatment depends on the type and severity of the defect and may involve medication, catheter procedures, or surgery.
Conclusion
Heart disease is a broad term that covers various conditions affecting the heart’s structure and function. Recognizing the signs and symptoms of these different types can lead to early diagnosis and treatment, significantly improving quality of life and outcomes for those affected. Regular check-ups and conversations with healthcare providers about heart health can help individuals understand their risks and take proactive steps towards heart disease prevention.
#usascriphelpersofficial#heart failure#heart disease#heart disease prevention#heart disease risk#health care#medical care#public health
2 notes
·
View notes
Text
Turning in the cardiac monitor today. The report from the echo showed mild mitral valve and trace tricuspid regurgitation- which isn’t a huge deal in the present, but can worsen over time and lead to heart failure…which runs in my family. I had to press the button on the holter monitor several times for noticeable arrhythmias when I lay down at night. Waiting to speak with the cardiologist. Man I hope I’m ok. I’ve always been physically healthy. It’s the mental health I struggle with- although the heart stuff could explain the intense physical symptoms I get during anxiety. On the other hand, life sometimes surprises us with shit- I can’t be mad at my body for something I was probably born with. It has weathered me through a lot, and seeing my heart on the screen during the echo- with the tenacious little valves opening for the streams of blood, something it has done since before I was born- gave me a new appreciation for my body. All I can do is continue to take good care of it. For about a month I’ve been working with a health coach that is provided by insurance and my physical health has improved. I’m going to keep chipping away at it. I’ll be ok.
#mitral and tricuspid regurgitation#echocardiogram#holter monitor#generalized anxiety disorder#writeblr
2 notes
·
View notes
Text
Uh, I know I’m not a doctor and I’m not trying to self diagnose. I was directed to the HEDS diagnostic criteria, and I decided to fill it out as best I could with my limited knowledge. An actual doctor can tell me if I’m right/wrong on these but… ? This at least gives me somewhere to start?
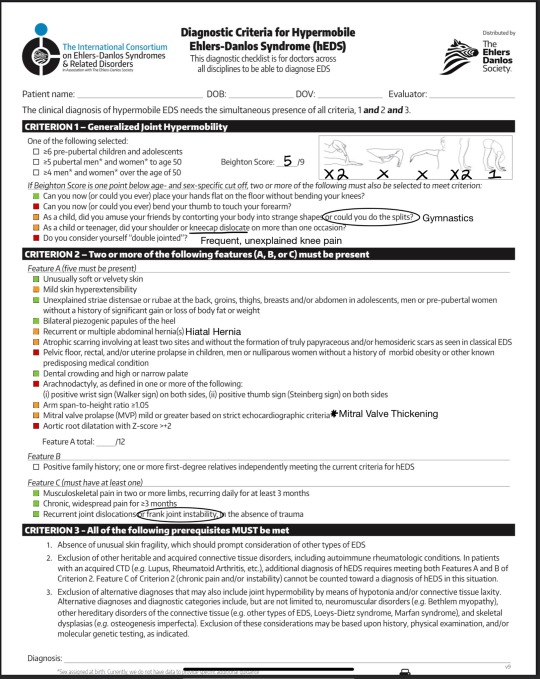
Green = Yes; Orange = Unsure; Red = Definitely No
I definitely don’t have classical EDS, and I never thought I would fit into the category of hyper-mobile… but maybe that last part isn’t true. I was tested for POTS. Didn’t quite fit that criteria, but I was told I had “mitral valve thickening” and that I was “dehydrated.” I also have the majority of the symptoms for MCAS, but I know that’s difficult to diagnose.
I’ll ask my primary about it once I go. I still want to rule out MS because of my muscle spasms and paresthesia. I do have b12 deficiency and vitamin D deficiency, but these problems only slightly improve when I take vitamins.
I have doubts that I will fit the criteria for a HEDS diagnosis when evaluated by a doctor, but I might just be on the cusp of these things. I’ve been told things like hyper mobility, dysautonomia, and mast cell activation can be on a spectrum. Having a diagnosis or a direction to go in would be nice, because I’m having far too many flare ups to manage without any answers.
2 notes
·
View notes
Text
one of the worst symptoms of anxiety (also mitral valve prolapse bc i think that’s what causes mine) are heart palpitations cuz i just woke up and immediately my heart started skipping beats and it’s sooo uncomfortable and scary i fucking hate them
4 notes
·
View notes
Text
Marfan Syndrome In 1896, the pediatrician Dr. Antoine Bernard-Jean Marfan described the exceptionally long, slender limbs and physique of a 5-year-old girl, Gabrielle P., in front of the Medical Society of the Hospital of Paris (Enersen). It is unknown whether Gabrielle P. actually suffered from what is now known to be Marfan syndrome, but Dr. Henricus Jacubus Marie Weve was recognized as the first person to use the term 'Marfan syndrome' to describe this common genetic disorder. In the decades leading up to Dr. Weve's use of Marfan syndrome to describe a patient's symptoms in 1931, other physicians had begun to document their encounters with this disease with the benefit of radiological images (Enersen). Drs. Henri Mery and Leon Baonneix studied Gabrielle P. anew using this new technology in 1902 and noted a misaligned spine, thoracic asymmetry, long digits, cardiovascular abnormalities, and dislocation of the ocular lens. During the same year, Dr. Achard described a patient with similar characteristics, including joint hypermobility and a pattern of family inheritance. Epidemiology The estimated prevalence of Marfan syndrome can range between 1:3,000 (Lavall, Schafers, Bohm, and Laufs 228), 1:5,000 (NAIMS "What is Marfan Syndrome?"), and 1:10,000 (Dean 724). The lowest estimate by Lavall and colleagues assumes a significant number of people with Marfan syndrome remain undiagnosed (228). The prevalence of this disorder dies not seem be influenced by gender or ethnicity (NAIMS "What is Marfan Syndrome?"). Clinical Features Marfan syndrome is an autosomal dominant genetic disorder, and in most cases transmitted from parent to offspring (NIAMS, "What causes Marfan Syndrome"). Therefore, one of the cardinal features of the disorder is a family history. The common physical features include exceptionally long limbs and digits, exceptional height, high palate, eye lens dislocation, thoracic asymmetry, hyper-flexible joints, and susceptibility to cardiac deformities (Beighton 403-404). However, a definitive diagnosis is not always straightforward, since manifestation of the disease can vary considerably between individuals. For example, only 50% of patients are predicted to suffer from a lateral curvature of the spine (scoliosis). Other symptoms can include poor muscle development, little fat tissue, hernias, and lung disease (Thurmon 243). Adding to the difficulty of diagnosing this disorder is that many of these symptoms can appear as part of other genetically-distinct syndromes (Thurmon 242). These other syndromes include contractural arachnodactyly, Marfan-like connective tissue disorder, and several diseases resulting from collagen abnormalities. Marfan-like symptoms can also emerge due to acquired medical conditions and simply by chance. For example, extreme tallness and the heart defect mitral prolapse occur in the general population at rates of 3% and 6%, respectively, so physicians will eventually encounter both occurring in the same individual, but in the absence of Marfan syndrome. One of the most common features of Marfan syndrome is ectopia lentis, which occurs when the lens of the eye becomes detached at one or more locations (Thurmon 243). This results in the lens tilting into the vitreous humor and causing vision problems. This can be easily observed in approximately 50% of adult patients and is detectable in close to 80% of adults with the proper vision test. Another common symptom is cardiovascular defects (Missimini 633). Those of primary concern are mitral valve prolapse and aortic aneurysms. The mitral valve is important for controlling blood flow into the aorta, and if it does not function properly then the blood will flow in the wrong direction. Mitral valve prolapse can be identified in some Marfan syndrome patients at birth, but in most by age 10 (Thurmon 243). Aortic aneurysms develop when the aortic vessel expands, leading to a weakening of the vessel wall and eventual rupture (dissection). Aortic aneurysms tend to develop adjacent to the heart first and then expand towards the periphery. Some patients will experience chest pain (angina) as an early sign. Aortic insufficiency is common by the time patients reach puberty and tears can develop in women who become pregnant. Approximately 75% of Marfan syndrome patients will develop cardiac problems and this has a significant impact on life expectancy (Lavall, Schafers, Bohm, and Laufs 228-229). Most deaths due to an aortic rupture occur after the age of 20, with an average of 32 years (Thurmon 243); however, these statistics are for patients not being treated (Lavall, Schafers, Bohm, and Laufs 229). With proper treatment, patients can live as long as 60 years. Etiology Marfan syndrome is caused by genetic mutations in the fibrillin-1 gene, a gene that produces a protein important for proper functioning of connective tissue (NIAMS, "What causes Marfan Syndrome"). Approximately 75% of all cases are inherited from a parent who carries the mutated gene. The parent would also show signs of Marfan syndrome. The other 25% of cases are caused by spontaneous mutations in the fibrillin-1 gene during the formation of sperm or eggs in the parents, therefore the parents of these children do not have Marfan syndrome. The fibrillin-1 gene produces a 350 kD glycoprotein that becomes an essential component of the extracellular matrix, where it polymerizes to form microfibrils (Dean 728-729). In addition to providing structural support to tissue, these microfibrils sequester proteins of the transforming growth factor ? (TGF?) -- family. This process of sequestration prevents this growth factor family from being released and exerting its effects on the neighboring cells. Due to the mutations in the fibrillin-1 gene though, this TGF? 'sink' is often compromised, resulting in excess TGF? affecting cellular function in detrimental ways. Although a defective fibrillin-1 protein may cause some structural problems, it is now believed that this excess TGF? is primarily to blame for Marfan symptoms. How this occurs remains unknown. Diagnosis Diagnosis remains difficult in some cases, because of the considerable variability in symptoms (NMF "About Marfan Syndrome: Diagnosis."). Diagnosis in most cases still depends on a taking a family history, performing a physical examination of the patient, and administering the following tests: echocardiogram, electrocardiogram, eye exam, and imaging of the lower back. The intense diagnostic focus on cardiovascular problems represents how threatening these defects are to the patient's health and the need for immediate intervention. Imaging of the lower back is diagnostically useful because many Marfan patients develop dural ectasias, which are an expansion of the membrane encasing the spinal cord (England). In Marfan patients, this membrane commonly expands, causing lower back pain, and can sometimes herniate into the area around the spinal column. The genetic disorder Loeys-Dietz has been recently discovered and its symptoms overlap considerably with Marfan syndrome (NAIMS "How is Marfan Syndrome Diagnosed). For this reason, it is important to distinguish between the two because the risk of dying from heart defects is greater for Loeys-Dietz patients and the treatment differs significantly. However, in contrast to Marfan syndrome, a diagnostic test is available for Loeys-Dietz syndrome. Although genetic testing can be done to detect mutations in the fibrillin-1 gene, it may not provide any additional information (NAIMS "How is Marfan Syndrome Diagnosed). In addition, between 9% and 34% of Marfan patients have fibrillin-1 mutations that have not been characterized yet and therefore cannot be tested for (Dean 725). Given the large number of fibrillin-1 mutations that can cause Marfan syndrome and an unknown number that have yet to be identified, the development of a definitive diagnostic test for Marfan syndrome may occur for some time. Treatment Marfan syndrome patients can live longer and enjoy a healthier lifestyle with treatment by a specialist (Massimini 634-635). The function and size of the heart and aorta should be checked annually by echocardiogram. A comprehensive eye exam should be performed, followed by regular checkups at a qualified ophthalmologist. The development of the skeletal system should be monitored during childhood and checked regularly during adulthood. The control of blood pressure is important to reduce the stress on the heart and aorta and antibiotics may be prescribed in advance of dental or genitor-urinary procedures to prevent infections in patients with a prolapsed mitral valve or a history of heart surgeries. Blood-thinning medications will likely be prescribed for patients who have had aortic surgery, such as the repair of a rupture. Marfan patients also need to pay attention to how they cope with everyday life (Massimini 635-638). It is important to avoid strenuous exercise, contact sports, or lifting heavy objects. Any exercise regimen should be discussed with a physician in advance to avoid overexertion and to become familiar how heart medications can impact physical activity. For example, the anticoagulant Coumadin is often prescribed for patients who have had a heart valve replacement, which can increase the possibility of internal bleeding and bruising. Recommended activities include walking briskly, bicycling or jogging at a slow pace, shooting baskets, a relaxed tennis game, and 1-3 pound hand weights. The amount of activity should be limited to less than 30 minutes, 3 to 4 times per week. Famous People with Marfan Syndrome Having Marfan syndrome has not impeded the lives and careers of a large number of people around the world (NMF "About Marfan Syndrome: Notable Individuals & #8230;"). The actor Vincent Schiavelli was diagnosed with Marfan syndrome and yet he appeared in over 150 movies and TV shows. Some of the more famous films included "One Flew Over the Cuckoo's Nest," "Fast Times at Ridgewood High," and "Ghost." The lead singer of Deerhunter, Bradford Cox (aka Atlas Sound), has been diagnosed with Marfan syndrome. The British composer, John Taverner, was diagnosed with Marfan syndrome along with his brother. Abraham Lincoln, due to his appearance, is suspected of having Marfan's syndrome, as is the Italian violinist Nicolo Paganini, the Russian Composer Sergei Rachmaninoff, Mary Queen of Scots, and the father of King Tut, Akhenaten. Unfortunately, a number of successful individuals failed to be diagnosed in time to prevent an untimely death due to a ruptured aortic aneurysm (NMF "About Marfan Syndrome: Notable Individuals & #8230;"). These individuals included the captain of the 1984 U.S. Olympic volleyball team, Flo Hyman, the playwright who penned the highly successful Tony Award-winning play "Rent," Jonathan Larson, the Florida State freshman basketball player, Ronalda Pierce, the natural food advocate, author, and Grape Nuts cereal pitchman, Euell Gibbons, and the University of Maryland basketball player, Chris Patton. Summary With nearly 200,000 Americans estimated to be suffering from Marfan syndrome (Heart & Vascular Institute), this disease cannot be considered rare or exotic. This disorder also ignores cultural, ethnic, and socioeconomic boundaries and therefore all societies must confront the needs of these patients. Detection and diagnosis seem to represent the greatest barriers to these patients living a full and fruitful life, with diagnosis still limited to taking a family history, conducting a physical examination, and conducting a few non-invasive laboratory tests. Although advances have been made towards developing a definitive genetic test, the percentage of individuals who would be missed by the current tests is still unacceptably high. This leaves physicians faced with detecting and diagnosing a disorder that manifests in a variety of ways, although there are a number of classic symptoms that can be used to screen most individuals suspected of having this disorder. For example, approximately 75% of patients will have a family history, close to 80% of adults will have a detached eye lens, and 75% will have cardiac problems. For all individuals who may have Marfan syndrome to have a chance at a fulfilling life, improvements in early screening and diagnosis seem essential. Who knows, the next president of the United States may be among the countless individuals who unknowingly have Marfan syndrome and run the risk of an untimely death. Works Cited Beighton, Peter. Inherited Disorders of the Skeleton. New York, NY: Churchill Livingstone, 1978. Print. Dean, John C.S. "Marfan Syndrome: Clinical Diagnosis and Management." European Journal of Human Genetics, 15.7 (2007): 724-733. Web. 5 Aug. 2012. https://www.paperdue.com/customer/paper/marfan-syndrome-109682#:~:text=Logout-,MarfanSyndrome,-Length7pages Enersen, Ole Daniel. Antoine Bernard-Jean Marfan. WhoNamedIt.com. n.p., 1994-2012. Web. 5 Aug. 2012. England, Ellen. "What is Dural Ectasia?" MarfanLife.org. n.p., n.d. Web. 5 Aug. 2012. Heart & Vascular Institute, Johns Hopkins University. "Marfan Syndrome: What is the Marfan Syndrome?" HopinsMedicine.org. Johns Hopkins University, n.d. Web. 5 Aug. 2012. Lavall, Daniel, Schafers, Hans-Joachim, Bohm, Michael, and Laufs, Ulrich. "Aneurysms of the Ascending Aorta." Deutsches Arzteblatt International 109.13 (2012): 227-233. Web. 5 Aug. 2012. Massimini, Kathy, ed. Genetics Disorders Sourcebook. 2nd ed. Detroit, MI: Onigraphics, 2000. Print. NIAMS (National Institute of Arthritis and Musculoskeletal and Skin Diseases). (2011). Marfan Syndrome: Questions and answers about Marfan Syndrome. NIAMS. National Institutes of Health, 2012. Web. 5 Aug. 2012. NMF (National Marfan Foundation). "About Marfan Syndrome: Diagnosis." Marfan.org. National Marfan Foundation, 2012. Web. 5 Aug. 2012. NMF (National Marfan Foundation). "About Marfan Syndrome: Notable Individuals & Celebrities with Marfan Syndrome." Marfan.org. National Marfan Foundation, 2012. Web. 5 Aug. 2012. Thurmon, Theodore F. A Comprehensive Primer on Medical Genetics. New York, NY: Parthenon Publishing Group, 1999. Print. Read the full article
0 notes
Text
Mitral Valve Replacement Surgery in Pune – at HeartMate Clinic
The heart is the engine of the human body, and its proper functioning is vital for a healthy life. Among the many components of this intricate organ, the mitral valve plays a key role in ensuring efficient blood flow. When this valve becomes damaged or diseased, it can lead to serious health complications. Mitral valve replacement surgery is a proven and effective treatment for restoring normal heart function.
If you or a loved one has been advised to undergo mitral valve replacement, HeartMate Clinic in Pune is your trusted destination for expert cardiac care. Our team of highly skilled cardiothoracic surgeons and specialists is dedicated to providing compassionate and world-class treatment using the latest surgical techniques.

What is the Mitral Valve and Why is It Important?
The mitral valve is one of the four valves in the heart. It lies between the left atrium and left ventricle, ensuring that blood flows in the correct direction—from the lungs into the heart and then out to the rest of the body.
When the mitral valve becomes narrowed (mitral stenosis) or starts leaking (mitral regurgitation), the heart has to work harder to pump blood. This can lead to symptoms such as:
Shortness of breath
Fatigue
Chest discomfort
Irregular heartbeats
Swelling in the legs or feet
If not treated on time, these conditions can lead to heart failure or other life-threatening complications.
What is Mitral Valve Replacement Surgery?
Mitral valve replacement surgery is a procedure in which a damaged or diseased mitral valve is removed and replaced with a new artificial valve. Depending on the patient’s condition, the replacement valve can be either:
Mechanical Valve: Made of durable materials like metal or carbon. These last a lifetime but require the patient to take blood-thinning medications long-term.
Biological Valve: Made from animal tissue or donated human tissue. These don’t require lifelong blood thinners but may need to be replaced after 10–20 years.
When is Mitral Valve Replacement Recommended?
Your cardiologist may recommend valve replacement if:
The valve damage is too severe to be repaired.
Symptoms are interfering with daily life.
There’s a risk of heart failure, stroke, or other complications.
Medications and other treatments are no longer effective.
HeartMate Clinic offers thorough diagnostic evaluations to determine the right time and approach for surgery. We consider your overall health, age, lifestyle, and preferences when recommending the best treatment option.
Mitral Valve Replacement Surgery at HeartMate Clinic, Pune
At HeartMate Clinic, we specialize in advanced mitral valve replacement surgery in Pune, using both open-heart and minimally invasive techniques. Our goal is to ensure optimal outcomes with minimal risk and faster recovery.
Why Choose HeartMate Clinic?
Expert Cardiac Surgeons: Our team is led by experienced heart surgeons with a successful track record of complex valve surgeries.
Modern Infrastructure: We use state-of-the-art operating theatres, diagnostic labs, and cardiac ICUs for the best possible care.
Minimally Invasive Techniques: Wherever possible, we use small incisions for quicker healing and reduced complications.
Holistic Patient Care: From pre-surgery consultation to post-operative rehabilitation, we provide end-to-end support.
Affordable & Transparent: We offer competitive pricing and clear communication regarding treatment plans and costs.
What to Expect: The Surgical Process
Pre-surgery Evaluation: Blood tests, ECG, echocardiography, chest X-rays, and angiography (if required).
During Surgery: The patient is under general anesthesia. The surgeon removes the damaged valve and implants a new one.
Post-operative Care: ICU monitoring for 1–2 days followed by a hospital stay of around 5–7 days.
Recovery: Most patients resume light activities within 4–6 weeks. Full recovery typically takes 8–12 weeks.
Our rehabilitation team at HeartMate Clinic provides personalized recovery plans, dietary advice, physiotherapy, and ongoing checkups.
Risks and Complications
While mitral valve replacement is a commonly performed and safe procedure, like any major surgery, it does carry some risks:
Bleeding or infection
Blood clots
Irregular heart rhythms
Reaction to anesthesia
Need for another surgery in rare cases
At HeartMate Clinic, we follow strict protocols to minimize these risks and ensure patient safety throughout the process.
Life After Mitral Valve Replacement
With proper care, most patients live a full and active life after mitral valve replacement. Regular follow-ups, healthy lifestyle choices, and adherence to prescribed medications are essential. If you have a mechanical valve, your doctor will guide you on managing blood thinners and regular INR checks.
Our team at HeartMate Clinic remains with you every step of the way—before, during, and after your surgery.
Book Your Consultation Today
If you or a loved one is dealing with mitral valve issues, don’t delay seeking expert care. HeartMate Clinic is here to provide you with the best possible treatment for mitral valve replacement surgery in Pune. Our compassionate team is ready to help you return to a healthier, more fulfilling life.
📍 Visit us at: https://heartmateclinic.com/department/mitral-valve-replacement-surgery/ 📞 Call now: +917028648300 📅 Book an appointment online and take the first step toward a stronger heart.
0 notes