#Gallbladder inflammation
Explore tagged Tumblr posts
Text
Understanding Cholecystitis: Causes, Symptoms, and Treatment
Imagine this: You're enjoying your favorite meal when all of a sudden, you're hit with a sharp pain in your upper abdomen that radiates to your right shoulder, making it difficult for you to even sit up straight. You're experiencing cholecystitis!
Imagine this: You’re enjoying your favorite meal when all of a sudden, you’re hit with a sharp pain in your upper abdomen. It’s so intense that it radiates to your right shoulder, making it difficult for you to even sit up straight. You’re experiencing cholecystitis, an inflammation of the gallbladder that can cause severe abdominal pain and other complications. This article aims to provide an…

View On WordPress
#Abdominal Pain#Cholecystectomy#Cholecystitis#digestive health#Gallbladder Inflammation#Gallstones#Health and Wellness#Medical Treatment#Preventive Care#Symptoms and Diagnosis
0 notes
Text
What is Gallbladder Inflammation (Cholecystitis)? What are the symptoms?
New Post has been published on https://bankakredin.com/what-is-gallbladder-inflammation-cholecystitis-what-are-the-symptoms/
What is Gallbladder Inflammation (Cholecystitis)? What are the symptoms?
The gallbladder is an important organ that has an effect on the absorption of various minerals and vitamins in terms of homeostasis (body internal balance) and storage of digestive secretions. Located in the lower-posterior region of the liver, this structure is about 10 cm long and acts as a kind of sac. Its main task is to store the bile produced in the liver.
Bile contains liquids that are alkaline, which aid digestion and especially facilitate fat digestion. As long as the pH value of the bile fluid and the ratio of the substances it contains are within certain limits, the individual can perform a healthy digestive function. When these ratios are in abnormal changes, diseases occur. Among these, the most common diseases are inflammation of the gallbladder, i.e. cholecystitis.
What is the Role of the Gallbladder and its Secretion?
The bile produced in the liver and discharged into the bladder via the bile ducts is yellow-green in color. The gallbladder has two main functions in the body. The main task of the gallbladder is to store the bile secretion as much as its capacity. It neutralizes the acidic enzymes coming from the stomach with its alkaline structure and makes the first part of the intestine (duodenum) ready for digestion.
This secretion, which is discharged from the liver into the pouch, is necessary for the conversion of large fatty food particles into small pieces before they are absorbed. In addition, bile contains breakdown products of hemoglobin, which is responsible for carrying oxygen to the blood. Bile salts, bile acids, sodium, chlorine, calcium, bicarbonate and water constitute the content of bile, apart from bilirubin and cholesterol, which are the breakdown products of hemoglobin. This secretion, which is stored in the gallbladder,
Why Is The Gallbladder Inflamed?
Since the gallbladder acts as a depot, it must release the secretion in its contents into the duodenum at regular intervals. Bile secretion is transmitted to the duodenum through the cystic duct. The most common cause of gallbladder inflammation is the formation of stones in the gallbladder. In the case of gallstone formation, which is referred to as cholelithiasis in the literature, obstruction occurs in the cystic duct due to stones.
When the content of the bile secretion under normal conditions changes, the secretion may acquire a mud-like structure and form stones ranging in size from millimeters to centimeters. These stones, which block the duct, cause the secretion to accumulate in the bile ducts. After a while, the bile may become clogged and swollen; it may even reach the level of explosion in advanced cases.
This condition, which starts with abnormal values in the body, results in death at a rate of 3% according to studies. However, stone formation is not the only cause for inflammation. Tumors in the gallbladder and its periphery, infections caused by bacteria or viruses, immunosuppressive diseases such as HIV positivity, pathologies such as obstruction or folding in the cystic duct other than stone formation, and interruption of blood flow to the gallbladder may also cause inflammation.
Important Factors That May Cause Gallbladder Inflammation
Inflammation of the gallbladder is a condition that is more common in women, as the disease progresses, the level of pain intensifies and causes comorbid results in the body. Various risk factors can increase the likelihood of developing the disease in individuals. The main risk factors can be listed as follows:
Age: Conditions that may cause inflammation occur more frequently in advancing ages.
Gender: Cases are more common in women due to sex hormones.
Sedentary life: As in many anomalies, a sedentary life may be a risk factor in gallbladder inflammation.
Nutrition: Inflammation cases are more common especially in the diet where fatty foods are overdone.
Genetics: Since the defense cells of the person and the codes of the immune system are in the DNA structure, genetic factors can cause inflammation in the body.
Environment: According to studies, the environment and habits are important for gallbladder inflammation. The cases are more common in cold countries such as America, where fast food habits are consumed or fatty foods are consumed frequently.
What are the Symptoms of Gallbladder Inflammation?
Understanding the successive symptoms in the body is important for diagnosing cholecystitis. Because the inflammation first manifests itself in the hemogram values, and then reveals the definitive diagnosis with various pathologies. The most common symptoms that patients complain about when applying to health institutions can be listed as follows:
Widespread pain in the upper-right abdomen
Indigestion, especially after a fatty meal
Vomiting after meals
Fire
decreased appetite
dizziness
Significant stiffness in the area of pain
Significant change in stool color
Increased inflammation in blood values (sepsis), hole in the sac (perforation) caused by the inability of the gallbladder to discharge the secretion in advanced cases, peritonitis seen with the spread of inflammation around the abdomen, inflammation of the pancreas (pancreatitis), bile or cystic duct detected by imaging methods Stone formation confirms the diagnosis of acute inflammation.
These symptoms seen in patients with gallbladder inflammation are reflected in blood values as increased bilirubin (jaundice), increase in leukocytes, which are defense cells, a serious increase in inflammation value (CRP) and ALT and AST values, which are liver function tests.
Since conditions such as obstructive jaundice, sepsis, yellowing of the skin of patients with perforation, fever, nausea, vomiting, and chills indicate acute inflammation, promptness in treatment saves time for the patient.
Gallbladder Inflammation Treatment Methods
After patients apply to health institutions, all examinations are performed in the light of the findings. After the diagnosis with blood values and imaging methods, a treatment plan is drawn according to the patient’s condition. First of all, the patient is kept under the control of a physician for a while, and during this period, his eating habits are controlled; When necessary, oral feeding is interrupted. In cases with obstruction in the canal, antibiotic treatment is started according to the size of the stone and the course of the inflammation.
Reducing the patient’s pain and relieving inflammation is a priority. The most common treatment method in patients with cholelithiasis or severely disseminated gallbladder inflammation is removal of the gallbladder by laparoscopic surgery. Physician who performs the procedure with the help of stick-like tools through the holes of 1-1.5 cm in the abdomen, monitors the operation from the screen on which the operation area is projected. This procedure, which is performed with the closed surgical method instead of deep and large incisions in the body, is more comfortable for both the physician and the patients.
Is It Possible to Prevent Gallbladder Inflammation?
In order to prevent diseases directly or indirectly related to the digestive system, the first goal should be to change the lifestyle. It is important for individuals to stay within a healthy weight target in order to maintain the internal balance of the body. Having a normal cholesterol level is essential for not being diagnosed with acute cholecystitis and maintaining a healthy life.
Therefore, in order to avoid gallbladder and other digestive problems, cholesterol level should be kept at a normal level, and if necessary, medication should be started under the control of a physician. Many of the things that should be done before the treatment of the cases are also the precautions to be taken to avoid the disease.
After Gallbladder Inflammation Treatment
After the gallbladder is removed, bile secretion is directly released into the duodenum without being stored, and the digestion process continues as before the treatment.
The patient, who is diagnosed with cholecystitis and is in the post-treatment period, should continue his life with a lower fat diet. Compliance with the diet program in which the fat ratio is minimized, prepared for the patient in the company of expert dietitians, facilitates the post-treatment process.
Exercise programs should also be included in new routines with physician control and expert guidance. As long as the person whose gallbladder is removed follows the recommendations, he can adapt to his life in a short time without any problems.
gallbladder inflammation, what are gallbladder inflammation symptoms, what foods are good for gallbladder inflammation, what are the treatments of gallbladder inflammation, inflammation of the gallbladder dangerous, can gallbladder problems cause inflammation, can your gallbladder get inflamed, can gallbladder inflammation be cured, can gallbladder inflammation come and go, can gallbladder inflammation cause weight gain, can gallbladder inflammation cause diarrhea, can gallbladder inflammation go away, can gallbladder inflammation cause chest pain, can gallbladder inflammation heal itself, can gallbladder inflammation cause indigestion, can gallbladder inflammation be seen on ultrasound, can gallbladder inflammation cause blood in stool, does gallbladder inflammation go away, does gallbladder inflammation cause bloating, does gallbladder inflammation cause diarrhea,
#can gallbladder inflammation be cured#can gallbladder inflammation be seen on ultrasound#can gallbladder inflammation cause blood in stool#can gallbladder inflammation cause chest pain#can gallbladder inflammation cause diarrhea#can gallbladder inflammation cause indigestion#can gallbladder inflammation cause weight gain#can gallbladder inflammation come and go#can gallbladder inflammation go away#can gallbladder inflammation heal itself#can gallbladder problems cause inflammation#can your gallbladder get inflamed#does gallbladder inflammation cause bloating#does gallbladder inflammation cause diarrhea#does gallbladder inflammation go away#gallbladder inflammation#inflammation of the gallbladder dangerous#what are gallbladder inflammation symptoms#what are the treatments of gallbladder inflammation#what foods are good for gallbladder inflammation
0 notes
Text
ARGHH...... i have to be up at 5:30 and its already 1:30........
we have to drive my sister to the train station in tacoma bc shes going down to portland for the weekend. the train leaves at 8 fucking am
good thing is my mom is dropping me off at the ER which is on the way to tacoma fjdkslfs and it works out bc she has to pick up stuff for her next post-cancer check in... BUT 5:30 AM.........
#yappin#my tummy hurtie and i want answers is it my gallbladder or some sort of stomach inflammation disease or both arghh#i ate a small salad with a couple vegan chicken nuggets bc i needed to eat some sort of vegetable#i cannot live on chicken and stars soup forever
5 notes
·
View notes
Text
Doctor said I have inflammation/infection around my gallbladder. So a general surgeon and his team are coming to talk to me. Sometimes they do antibiotics or it'll be surgery... im scared
24 notes
·
View notes
Text
Vet Bills and a Sick Kitty Boy
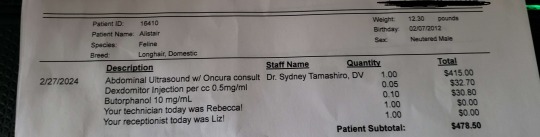
Hello all, over the past month and a half I have incurred some medical bills for my cat Alistair, that while one bill hurts but isn't world ending. Multiple have put us in a bind.
Our Total: $430/$1176.86
My Paypal: tielfingriley or paypal.me/tieflingriley
The Story:
So my sweet yet very hungry boy Alistair, had been having stomach troubles. He's 12 years old, so not uncommon for a cat his age, and he has always had a bit of a sensitive tum, but this was different. He was projectile vomiting mostly water, and I had noticed he was loosing weight. He is a long cat, and his healthy weight sits at 15-16 pounds.
So we take him to the vet and the do a initial blood panel with a special panel to check a for a heart protein, it is here that I learn my asthmatic cat also has a heart murmur! But because of the special check it had to be sent to THE ONLY LAB IN THE US THAT CHECKS FOR IT, which meant it was pricey

Good news, blood came back fine. His heart and kidneys weren't failing but he was still vomiting water at this time. At this point we were moved to a different vet who noted his long term tum issues. Informing me that long term inflammation can lead to Gastrol Intestinal Cancer. (Maybe) They only DEFINITIVE way of checking was to slice him open and do biopsies, which wasn't ideal. Instead we opted for an Ultrasound, it would check for inflammation, which would say absolutely yes or no on inflammation, but would still be a maybe on the cancer (however its the same treatment either way). But could also check Liver, Pancreas, and Gallbladder. I of course chose this because it was far less invasive to the boy. Alistair did need to be sedated. He isn't a violent cat, but he is a squirmy noodle.
This is when things got really spicy for us financially. You see this happened RIGHT before my birthday. Like legit I found out my cat had maybe cancer the day before. And my husband a few weeks prior had bought me a rather nice gift of storage drawers? IDK what you would call it but furniture for my art supplies to be stored in. It was a bit pricey but I was having a rough time and a history of astronomically shitty birthdays. (As you can see, the universe has a sense of humor)
So the Ultrasound came back. Yes there are signs of inflammations, so cancer is still a maybe. However, what had the doctors eyes and was concerning her more was the pancreas. It was, extended and incorrect. She believed that it wasn't producing a enzyme to help break down food, particularly fat, for absorption. Essentially, on top of the inflammation, Alistair was slowly starving to death. However before just popping some pig panceas pills inside my boy, she wants to make sure. So more blood work, TO THE ONLY LAB IN THE US OF COURSE, an another bill.
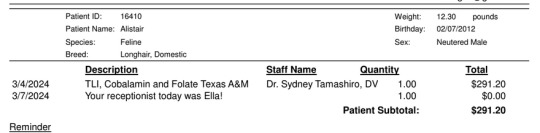
Now we are waiting on this information. He is on some pro and prebiotics that have stopped the vomiting entirely. However his weight is still quite thin. I am unsure if we will have more hefty bills. For reference a checkup at this vet is 50 bucks. So normally its not to rough on us, and check up plus vaccines is 100 which is a planned event. None of this was planned to say the least.
AND NOW THE SAPPY SHIT
Alistair saved my life. I know logically getting a cat as a means to not kill yourself isn't the best thing to do, but sometimes you gotta do what you gotta do. Ive had him since September of 2012. I love that fluffy biscuit stealing bastard with my entire heart. I have a tattoo on him on my arm, my first and currently only tattoo. Because of him, I was able to live a longer and healthier life and I want that for him.
Despite being a cat, he loves biscuits, potato chips, and the tops of muffins but only the tops. He can and will open cookie jars for cookies. I have explained he is an obligate carnivore and he has explained like a good southern he cant turn down a carb.
He will fist fight you for cheese. Love to play fetch with a hair tie. Isn't a lap cat with the exception of me. LOVES NAPS, and likes to watch Markiplier.
He's a very good boy with separation anxiety, and tummy issues who just wants to nap and eat and I think we can all relate.



Oh...and he has a little mustache
Thank you to all who donate and to everyone who spreads the word to help us get out of this debt.
#Fundraising#gofundme#Donate if you can#But absolutely reblog#Thank you so much#Alistair the cat#Cat
31 notes
·
View notes
Note
Genius of Marx to come up with a theory that required the working class to repeatedly risk their lives for his ideas while he spent the rest of his life getting blackout drunk in his rich friends many houses.
Between 1843 and 1848 he was arrested and exiled from six countries (Prussia, France, Belgium, France again, Prussia again, France a third time) and in London lived in three small rooms (his wife described them as ‘evil’ and ‘frightful’) in Soho, where two of his young children died and he constantly suffered from headaches, eye inflammation, joint pain, insomnia, liver and gallbladder problems, and boils so bad he couldn’t sit down. But most importantly, if you had suggested that the presence or absence of any of these things in his life weighed on the correctness of his theory he would have spat in your face
310 notes
·
View notes
Note
What's the most insane bit of physical diagnosis you know? (The bit with lifting the legs and moving them around to diagnose appendix inflammation made me go :000)
Honestly all of physical diagnosis is wild. There are so so many weird things that the human body does, and even weirder things that we figured out to tangentially find problems with it.
I wish physical diagnosis was more rigorously taught, or at least had more time allotted to it (currently students get about 8-20 total hours/semester for 2 years, some of which is testing) where I teach. Cause damn it would be fun to get into all the fiddly bits of abdominal signs, musculoskeletal, and neuro. You can learn so freaking much from a neuro exam that isn't just memorizing the cranial nerves. You can generally tell where in the brain a stroke occurred, and tenuously what kind of stroke it was, with a 20-minute exam (not that any doctor ever has 20 whole minutes with a patient, but still).
And not to sound like a fuddy-duddy but PD is quick n cheap compared to nearly all high tech alternatives. What you can figure out from PD is a little inferior from what you might get with a CT or ultrasound, but for a trained practitioner it's close enough.
As serious and high-stakes as we like to think medicine is, only very specific things in medicine need to be super accurate. You need to be about 85% sure what the problem is, then you're either going to do some kind of surgery about it, or give some kind of medicine. Either way, if it doesn't work, you try something else. Human bodies are weird af and don't conform to a textbook ever.
Anyway, off my soapbox, here's some cool physical diagnosis things to try at parties:
Percussion: Need to find if a thing under the skin is solid (like liver), full of liquid (like acites in the abdomen), or full of air (like the gastric bubble or lung)? Look no further than this poor man's ultrasound! Take the middle finger of your non-dominant hand and find the last joint, called the DIP. Press the DIP down against the part of the body you want to hear like this:

Then, with the tip of your dominant middle finger (or a knuckle, or reflex hammer I'm not picky) tap hard directly over the DIP. Really throw your wrist into it. You want a callus to form over that DIP.
You'll hear a sound that will mean absolutely nothing to you. But try in a few different places and you'll start to be able to calibrate. Percuss in the following areas and note the difference in sound: Upper right chest (lung, gas), lower right chest (liver, solid), anywhere on abdomen (probably gas, or a mix of gas and solid), thigh (muscle, solid). Make sure you're pressing down really hard with the DIP and not percussing over bone (between ribs is okay).
As you get more and more comfortable with this, you can start "mapping out" abdominal/thoracic organs in people (or dogs. dogs love this for some reason)- particularly the spleen, liver, diaphragm, lungs, and heart. Once you get REALLY good at this, you can use percussion to find tumors and pneumonia in lung tissue (find a solid thing in the lung? Probs a tumor. Find liquid in the lung? Heart failure or pneumonia depending on where it is), and quantify liquid in the abdomen or bladder, among many other things.
Am I putting the BladderScan company out of business with this illicit knowledge? No. But that's just cause everyone likes a number, and while I can't do much more than "full" or "not full" or "really full oh sh*t really full", the bladder scanner can snarkily say ">999".
McMurphy's Sign: Think someone might have inflammation in their gallbladder (cholecystitis) due to a blockage or stones? Mash down with your hand just below the right lower edge of their rib cage. Hold your hand there pushed in and have them take a deep breath. Do they stop breathing suddenly because it hurts real bad? Cholecystitis.
Allen Test: Your hand has 2 arteries that bring blood to it. Both of them work about equally well when you're healthy. But let's say you have to do something that might endanger one of these arteries (say, an arterial line, or you need to snake a catheter from the wrist to the heart). You need to make sure that the other one works well enough that if you totally destroy the other one, the patient won't lose their hand.
So basically to do this, you have someone lay their hand palm up on a table. Put a thumb over each side of the wrist (feel a bone, a bundle of tissue, and another bone across the wrist, and your thumb should be in the divot between the tissues bundle and the bone on each side) and press down. Have your patient make a fist and then relax it. The palm should be white, because you've just squeezed all the blood out of it and aren't letting any back in because you've occluded the arteries.
Then you're going to release pressure on one side. The hand should pink up within a second or two. Then repeat with the other side. If the hand pinks up twice, you've got enough blood flow to do your thing with one of the arteries.
Bruits Over the Carotids (and other places): As people get older, they build up plaque in their arteries. This can cause narrowing of blood vessels throughout the body, and if it gets bad enough, can prevent blood from flowing to various organs. This can cause severe hypertension (if the blood isn't getting to the kidneys), angina (if the blood isn't getting to the heart muscle), or syncope (if the blood isn't getting to the brain.
If you take a stethoscope and listen over the carotid artery, you can tell about how bad this is by how much noise the blood makes moving through the artery at each beat. This sound is called a bruit (pronounced brew-ee). While you can sometimes hear bruits in the abdomen, they are usually hard to localize. The condition of the carotids makes a good proxy for other less-find-able arteries. So someone has hypertension that meds are struggling to treat and a carotid bruit? Maybe look into the condition of their renal arteries and see if a stent would solve their blood pressure issues.
172 notes
·
View notes
Text
flare day 56
i had labs done a couple of days ago and results are starting to roll in. confirmed i don’t have celiac disease, which is both relieving that i don’t have to give up my favorite foods and disappointing that i still don’t know what’s wrong with me. one result came back showing i have high CRP levels, which is indicative of inflammation in the body. this may be stomach related, but also could be due to my joint problems.
i have a HIDA scan next week to check my gallbladder. i’ve already had a CT scan with contrast as well as two ultrasounds, but this may show something that was missed. at the end of june i’ll be doing a gastric emptying study to see if it could be gastroparesis, which is the main running theory based on what the ER doctors and my GI think. yay, i get to eat radioactive eggs!
i’m really tired, to-the-bone type fatigue. sometimes it’s hard just getting from my bed to the bathroom, and the protein shakes i’m practically living on only provide so much nutrients. i’m trying to busy myself with projects, like knitting and sewing and drawing. sometimes i cook or bake, but it’s hard when i know it will all make me so sick.
one of my best friends told me yesterday that they realized what ever this is could kill me with how little i eat and how much weight i’ve lost, and while i had that realization myself early on it definitely hurts my heart hearing someone i love realize it too. i find myself wishing i could suffer quietly, away from where my loved ones can see. i don’t want them to see me wasting away.
i’m looking forward to all the things i’ll be able to do if/when i feel better, like going out to restaurants with friends and experimenting with making cocktails and even just going back to the office. i look forward to dressing up in my favorite outfits again and eating good food in even better company and enjoying not being stuck with needles in ER beds and the smell of saline.
but until then i’ll just keep working on my projects and trying my hardest to stay alive.
#actually chronically ill#gi issues#gastroparesis#tummy ache survivor#gastric emptying scan#gastric emptying study#HIDA scan#gastro issues#chronic illness#chronic pain#chronically ill#pots syndrome#potsie#postural orthostatic tachycardia syndrome#heds#hypermobile eds#hypermobile ehlers danlos#ehlers danlos syndrome#tummy ache talks
10 notes
·
View notes
Text
A list of Long Covid Symptoms
Allergy/Histamine (2)
Heightened Food Sensitivities — Worse reactions to foods I was already sensitive too
Inflammation After Eating Avocado — Seems to be histamine reaction
Arms/Hands (8)
Fingernails Brittle
Fingernails Slow Growing
Hand Coordination Off — Dropping things randomly
Hand Weakness — Trouble opening jars, etc.
Heavy Arm Feeling — Felt like they were two sacks of potatoes
Vertical Ridges on Fingernails
Waterlogged Look in Fingertips — Probably neurologically related
Wrist Pain
Back (2)
Back Cracking — Feels constricted & tight
Back Pain — Lower & upper, probably due some to organ inflammation
Bladder (4)
Discolored Urine — Clear/Dull at times, probably due to dehydration
Frequent Urination — Had to urinate more often, water would run right through me
Urgency in Urination — Trouble holding it at times, would have to go suddenly and immediately
Urine Smell — When Covid was most active, sweat would smell too
Circulation/Vascular (9)
Blood Dark
Blood Thick — Hard to get out of veins at times, wet cupping showed dark/thick blood too
Bumps on Veins — Briefly had bumps, making it hard to do IVs in certain spots, went away
Cold Hands & Feet
Covid Toes — Had slightly, toes under toenails would turn a little purple
Elevated Veins — Veins were raised at times
Felt Like I Was Having a Stroke — Weird sensation in brain stem, one of the more frightening symptoms
Hypertension — Blood pressure was up 140+/80+, normally I’m at 110-120/60-70
Micro-Clotting — Seen in blood from wet cupping
Ears/Mouth/Teeth/Throat (11)
Clogged Ears
Dry Mouth — Especially when Covid most active
Ear Cracking
Ear Pain — Sharp pain would come on inside of my ears at times, like an earache almost
Gum Receding — Not often
Hoarse Voice — Especially when Covid most active
Itchy Ears
Jaw Pain
Loose Teeth — Felt like some teeth would fall out, had to be careful eating certain things for some time
Pain in Teeth — Probably nerve related
Throat Tightness — Like a constriction
Energy (2)
Fatigue — Had extreme fatigue for months, could barely do anything
Malaise
Eyes (8)
Blurry Vision
Double Vision
Dry Eyes — Especially when Covid most active
Floaters
Itchy Eyes — Histamine or Covid related
Light Sensitivity — Especially when having brain stem inflammation
Motion Sensitivity — Especially when having brain stem inflammation
Tunnel Vision
Gallbladder (2)
Gallbladder Pain
Pain & Inflammation When Eating Fatty Foods — Have not had steak in 2 years, that sent me to the hospital the one time I decided to go for Long Haul Covid
Gastrointestinal (13)
Bloating — Upper GI
Burping — Worse with active Covid
Constipation
Craving Food
Diarrhea — More common with active Covid
Gassy — Worse with active Covid
Growling/Rumbling — Worse when eating things my body doesn’t want me to
Loss of Appetite
Nausea — Can come on with reflux
Reflux — Has been a mainstay, waxes and wanes, reinfection flares it up
Stomach Pain — Abdominal pain all over
Vomiting — Sometimes blood (when I had nasty gastritis from BA.5)
Weight Loss — Lost 28 pounds at lowest, have gained 16 back now
Head/Neurological (36)
Anxiety — A chemical physical anxiety
Brain Fog/Memory Issues — Trouble remembering names, etc.
Compressed Nerve — Constant nerve pain in neck/upper back that had to be relieved by Atlas Orthogonal Chiropractor, came on after reinfection
Confusion — Felt like dementia at times, forget why came downstairs, put keys in fridge
Delirium — Totally out of it for a short period, crazy thoughts, couldn’t think straight
Difficulty Concentrating — ADHD type feeling
Dizziness — Would have to hold on to the railing vertigo was so bad
Electrical Zaps
Fainting/Blacking Out
Fleeting Nerve Sensations — Quick phantom sensations
Hair Loss — Moderate loss of hair when showering
Hair Texture Changed — Coarse for a time
Hard Finding Right Word
Headaches/Migraines
Heat Sensitivity — Too much heat would make me feel horrible, nervous system related
Higher Heart Rate at Rest — Went up to 80s at rest when should have been 60s, higher standing and moving than normal as well
Limb Weakness — Dead arms at times, brain stem/neuro related
Nerve Burning Sensation
Nerve Pain
Numbness in Face
Occipital Neuralgia — Nerve pain in head
Pain & Inflammation After Using Brain Too Much — Only have so much brain power in a day at times
Partial Paralyzation — GBS symptoms, Thanksgiving 2020 could barely move half the day, shallow breathing
PEM — At one point couldn’t walk 5 minutes without feeling horrible that rest of day and the next, now can walk many miles without an issue, but strenuous exercise still a problem
Pins and Needles — Neuropathy in arms and legs
POTS — Dizzy/Blacking out when standing
Pressure in Brain Stem
Restless Legs — Fidgety, can’t sit still, moving legs a lot when trying to go to sleep
Shaking/Tremors — I remember seeing a new doctor and thinking she would believe I’m a drug addict, as I was shaking like someone going through violent withdrawals
Slurring Speech
Sound Sensitivity
Tinnitus — Some ringing in ears at times
Trouble Breathing — This was a neurological difficulty breathing, like my body didn’t know how to do it
Trouble Controlling Arm and Leg Movements — IV C really brought on GBS symptoms, brain couldn’t control my arms and legs
Trouble Swallowing — Food, pills, water
Trouble Typing/Writing
Vibrations
Heart (5)
Pain in Heart When Laying Down — Maybe reflux related
Pounding Heart — Probably neuro, was worse when at 100mg of Fluvoxamine for months
Skipped Heart Beats
Stinging Pain — Sharp pain, not so much anymore
Tachycardia — Was racing out of control, so rushed to Cardiologist and convinced them to give me steroids
Hormones/Mood/Psychological (9)
Depression — Slight, but I’m not a depressed person, if I was it would probably be extreme
Dissociation — Out of body, not present
Emotional — Crying, when I shouldn’t have, a few times
Feeling of Doom & Gloom — Felt at times I would never get better, but it was a chemical/physical thing
Feeling Irritable — Easily angered at times
Intrusive Thoughts
Mood Change — A little colder, less jovial
PTSD — From this whole experience
Sex Drive Decreased — Probably due to testosterone lowering some
Immune System (4)
Body Temperature Changes — Hot to Cold
Chills
Fever — Never higher than 102
Night Sweats — For a period would sweat profusely at night
Joints/Muscles (7)
Bone Pain
Hurt to Lay Legs on Top of Each Other While Sleeping — Had to put comforter in between legs
Joint Pain — All over joint pain, especially hips, knees, hands, comes and goes
Loss of Muscle Mass
Muscle Constriction/Tightness — All over body, Covid has caused a tightening, could use a massage daily for a year
Muscle Pain
Muscle Spasms — All over muscle spasms, especially arms, chest, legs, head, worse when Covid active
Kidneys (1)
Kidney Pain — Bilateral at same time always it seemed
Legs (5)
Calf Pain — Circulation?
Cramps — Would get wicked, painful cramps in legs
Heavy Leg Feeling — Dead legs
Thigh Pain, Weakness — Would get weird thigh pain, and weakness, as if they wanted to give out
Tight Hamstrings
Liver (1)
Pain in Liver — Mid-upper right side abdominal pain
Lungs/Respiratory (13)
Chest Pain — Especially with acute/active Covid
Coughing — Not too often
Coughing Up Phlegm — Still doing this, still nebulizing sometimes, cough up when I walk a lot
O2 Drop — Never measured below 93, would hoover 95-99 most of the time
Rapid Breathing — Scary, almost what I assume a panic attack is like
Rattling Of Lungs
Runny Nose — Usually more so with acute/active Covid
Shortness of Breath — Comes & goes
Sneezing — Usually more so with acute/active Covid
Throat Sore — Usually more so with acute/active Covid
Tightness in Chest — Chest was super tight after BA.5, wanted to stretch constantly, starting to use The Gun now
Trouble Breathing — Mostly beginning of Long Haul Covid, acute/active Covid
Wheezing
Lymphatic System (2)
Edema — Some fluid noticed around chest by Lymphatic Massage Therapist
Swollen Lymph Nodes — Noticed this especially under arms at times
Neck (2)
Cracking Neck — Worse with inflammation in area, acute/active Covid
Stiff Neck — Much worse with acute/active Covid, makes neuro symptoms worse
Pancreas (1)
Craving Food — Felt like a blood sugar problem, which was slightly higher than normal for me
Skin (7)
Acne/Cystic Acne — Would break out at times, maybe because I’m overloaded with toxins?
Bruising Skin — Would bruise after getting a line in vein, not anymore
Itchy Skin — Inflammation
Peeling Skin — Skin would peel around mustache when head inflammation was at its worst
Rash — Around nose, could be allergy/histamine reaction
Shiny Skin — Old baseball mitt looking skin for a period of time
Sensitivity To Touch
Sleep (7)
Awakened Suddenly — Wake up trying to catch my breath
Insomnia — Not for a very long period of time thankfully
Jolted Awake After Asleep For A While — Adrenaline dumping?
Trouble Falling Asleep — Tossing and turning
Trouble Sleeping Until Alarm — Would wake up way before alarm went off, that would never happen before Covid
Vivid Dreams — Nightmares, crazy dreams, remembering dreams (would not before Covid)
Woke Up Due to Dream Movements — Once swung my arms and knocked everything off my nightstand, woke myself up
Smell/Taste (2)
Burning/Phantom Smells — Not often
Metallic Taste — Not often
Other (7)
Craving Bananas — Was craving bananas for months, body wanted potassium?
Dehydrated — Covid commonly makes you dehydrated, still need to drink a lot of water and take electrolytes
Rib Pain — Cartilage/Rib inflammation, Costochondritis
Sudden Jerks
Sweat Smelled — Sweat & Urine smelled due to Covid
Thirst for Water — Likely due to dehydration
Trouble Walking
#chronic pain#chronically ill#covid#covid isn't over#covid19#long covid#chronic illness#long haul#covid long hauler#post covid syndrome#post covid#covid is airborne#covid pandemic#covid vaccine#symptoms#still sick#i feel sick#sick#sickness
3 notes
·
View notes
Text
i have my gallbladder scan tomorrow. i want it to either be clean and i don't know it was just an inflammation crisis or whatever, or i want it to be filled with stones and ready to explode
#My doctor said because my bloodwork was ok and it seems like my other organs haven't been affected from my horrible crisis from august#we wouldn't be able to ask for surgery if it's just a couple of stones in there#and that would mean possibly having recurring crises until my other organs actually do suffer from it#Well that's a shitty rule#personal
4 notes
·
View notes
Text
Soooo Sansa has a tumor on her gallbladder -_-
But all signs point to it being benign (her white blood cells are looking normal) and at her age, the vet advised just taking supplements to keep the inflammation down. It's a domino effect on her liver and pancreas, so sweeping out the gunk that's built up with antibiotics this month should clear her organ stress up.
Then it'll just be supplements for the rest of her life, my poor jellyroll. But hey, could always be much worse.
But also, it could be way better :P
Buuuut either way, she's 12 years old, of course she has maladies. After this month, grabbing big ol' jars of meds for her arthritis and mushroom chews for her gallbladder won't be terribly expensive. As long as her lil body is less stressed.
4 notes
·
View notes
Text
well at least it's something to go to the doctor sometimes. they ran some tests and i do not have an inflammation. the doctor didnt seem to think im as yellow as i look to myself. so probably im just "seeing" it. he said that this will probably pass again as it did last time. and that i should take those painkillers regularly instead of just during an attack. (tho im a bit scared of that bc those painkillers have gnarly side effects... like the short term usage of them can increase your risk of getting heart diseases down the line so umm idk). so idk even if my pain doesnt magically disappear it is calming to know that im not dying nd dont have anything rlly seriously bad going on (like an inflammation in my gallbladder).
8 notes
·
View notes
Text
ladies can you please pray for my sister in law? she's had severe pain for a couple days and was told by her doctor that it's related to her gallbladder, though nothing is showing in tests that would indicate inflammation or malfunction thereof. the baby is fine, active and healthy! just my SIL is in quite a bit of pain. so prayers for healing and that everything will be alright would be appreciated
#she's supposed to run a worship night tomorrow and it's WAY too late to reschedule now#so my dad and our regular worship leader are getting together to try and rework it#and like yeah worship team whatever I don't care I just know that my SIL is hurting and also that she has a MASSIVELY#overdeveloped sense of responsibility and is gonna feel so bad if she can't do the worship stuff tomorrow#and I wish I could help but I. cannot. :( pray for her and my brother and baby please#they're having a girl btw. idk if I mentioned that yet. :)#Lu rambles#prayer request
20 notes
·
View notes
Text
I know why hospitals are cold but got damn it's cold in here
Dad just went for a CAT scan for potential respiratory distress (judging by the nurse's(?) >:O reaction to dad saying he doesn't wear his oxygen when he goes to the bathroom, that might be related). The nurse confirmed that they're waiting for inflammation to go down before they remove the gallbladder.
But his bowels are unblocked, so that's one less thing to worry about
He's tired of being in the hospital though. He starts calling it "The Pain Palace" after a few days sdfghjkl Partly because he's a hard stick with a needle
2 notes
·
View notes
Text
Choosing the Right Gastrointestinal Tract Drug – Factors to Consider
The gastrointestinal (GI) tract is a complex system responsible for digestion and absorption of nutrients. Given its critical function, disorders affecting the GI tract can significantly impact overall health and quality of life. Selecting the right medication to treat these conditions is essential for effective management and recovery. Centurion HealthCare, a leading gastrointestinal tract drugs supplier in India, offers a range of high-quality medications designed to address various GI disorders. In this article, we will explore the factors to consider when choosing the right gastrointestinal tract drug, and why Centurion HealthCare stands out in the best pharmaceutical industry in India.

Understanding Gastrointestinal Tract Disorders
GI tract disorders encompass a wide range of conditions affecting different parts of the digestive system, including the esophagus, stomach, intestines, liver, pancreas, and gallbladder. Common GI disorders include:
Gastroesophageal Reflux Disease (GERD)
Peptic Ulcer Disease
Irritable Bowel Syndrome (IBS)
Inflammatory Bowel Disease (IBD)
Hepatitis
Pancreatitis
Each condition requires specific treatment strategies and medications to manage symptoms, promote healing, and prevent complications.
Factors to Consider When Choosing a Gastrointestinal Tract Drug
Choosing the right drug for treating GI disorders involves multiple factors, including the specific condition, the patient’s medical history, and potential side effects. Here are key considerations:
1. Accurate Diagnosis
An accurate diagnosis is the first step in selecting the appropriate medication. Physicians use various diagnostic tools such as endoscopy, colonoscopy, imaging studies, and laboratory tests to identify the specific GI disorder. Understanding the underlying cause and severity of the condition is crucial for effective treatment.
2. Mechanism of Action
Different gastrointestinal tract drugs work through various mechanisms to achieve therapeutic effects. Understanding how a drug works helps in selecting the most suitable option. Common mechanisms include:
Antacids: Neutralize stomach acid, providing quick relief from heartburn and indigestion.
Proton Pump Inhibitors (PPIs): Reduce the production of stomach acid, effective in treating GERD and peptic ulcers.
H2 Receptor Antagonists: Decrease acid production by blocking histamine receptors in the stomach lining.
Prokinetics: Enhance gut motility, useful in conditions like gastroparesis.
Antispasmodics: Relieve intestinal cramps and spasms, often used in IBS treatment.
Anti-inflammatory Drugs: Reduce inflammation in the GI tract, essential for managing IBD.
3. Efficacy and Safety
The efficacy and safety profile of a drug are critical factors in the decision-making process. Clinical trials and real-world studies provide valuable information on a drug’s effectiveness and potential side effects. Physicians must weigh the benefits against the risks to ensure the chosen medication offers the best possible outcome for the patient.
4. Patient-Specific Factors
Each patient is unique, and various individual factors can influence drug selection. These include:
Age: Certain drugs may be more suitable for children, adults, or the elderly.
Medical History: Pre-existing conditions, such as kidney or liver disease, can affect drug metabolism and tolerance.
Allergies: Patients with known drug allergies must avoid medications that could trigger adverse reactions.
Concurrent Medications: Drug interactions can impact efficacy and safety, requiring careful consideration of all medications the patient is currently taking.
5. Route of Administration
The route of administration can affect the drug’s efficacy and patient compliance. Common routes for GI drugs include:
Oral: Tablets, capsules, and liquids are convenient for most patients.
Intravenous: Used in severe cases or when oral administration is not feasible.
Topical: Suppositories and enemas are used for localized treatment in the lower GI tract.
6. Cost and Availability
Cost can be a significant factor, especially for long-term treatments. Generic versions of drugs often offer the same efficacy as brand-name medications at a lower cost. Availability of the drug in the local market is also crucial to ensure uninterrupted treatment.
Centurion HealthCare: Leading the Way in GI Tract Drug Supply
Centurion HealthCare has established itself as a premier gastrointestinal tract drugs supplier in India, renowned for its commitment to quality, innovation, and patient care. Here’s why Centurion HealthCare is a trusted name in the best pharmaceutical industry in India:
1. Comprehensive Product Range
Centurion HealthCare offers a wide range of gastrointestinal tract drugs, catering to various GI disorders. Their product portfolio includes antacids, PPIs, H2 receptor antagonists, prokinetics, antispasmodics, and anti-inflammatory medications, ensuring comprehensive treatment options for healthcare providers.
2. Quality Assurance
Quality is at the heart of Centurion HealthCare’s operations. The company adheres to stringent quality control measures, from raw material sourcing to final product testing, ensuring that every medication meets international standards for safety and efficacy.
3. Research and Development
Centurion HealthCare invests heavily in research and development to stay at the forefront of pharmaceutical innovation. Their R&D team continuously works on developing new formulations and improving existing products to address emerging healthcare needs.
4. Patient-Centric Approach
Understanding that each patient is unique, Centurion HealthCare adopts a patient-centric approach in drug development and supply. Their medications are designed to provide maximum therapeutic benefit with minimal side effects, enhancing patient outcomes and quality of life.
5. Global Reach
As a leading gastrointestinal tract drugs supplier, Centurion HealthCare has a robust distribution network that ensures their products are available not only across India but also in international markets. Their commitment to excellence has earned them a reputation as a reliable partner for healthcare providers worldwide.
6. Affordability
Centurion HealthCare is dedicated to making high-quality medications accessible to all. Their cost-effective solutions, including generic versions of popular GI drugs, help reduce the financial burden on patients while maintaining high standards of care.
Conclusion
Choosing the right gastrointestinal tract drug involves careful consideration of various factors, including accurate diagnosis, mechanism of action, efficacy, safety, patient-specific factors, route of administration, and cost. Centurion HealthCare, as a leading gastrointestinal tract drugs supplier in India, excels in providing high-quality, effective medications that cater to the diverse needs of patients with GI disorders.
With a commitment to quality, innovation, and patient-centric care, Centurion HealthCare stands out in the best pharmaceutical industry in India. Their comprehensive product range, stringent quality assurance, advanced R&D, global reach, and affordability make them a trusted partner for healthcare providers seeking reliable solutions for GI tract disorders.
By choosing Centurion HealthCare, you can be confident in the quality and efficacy of the medications you are prescribing or consuming, ensuring the best possible outcomes for gastrointestinal health.
#Best Indian pharma industry 2024#Best pharmaceutical industry in India#Gastrointestinal tract drugs supplier#Gastrointestinal tract drugs supplier in India
3 notes
·
View notes
Note
I'm writing a story where a male character has gallstones. It happened to me a long time ago so I don't remember how they ran tests at the hospital to get to that diagnosis. I just remember the chest/back pain was terrible. How would they rule out a heart attack in the emergency room? What else would they test for? Are gall bladder stones common enough that a nurse or doctor thinks to check before an x-ray?
If the hospital is busy, how long is a patient allowed to be in severe pain until it warrants more meds (I've heard of morphine being used).
Cholecystitis (inflammation of the gallbladder, often related to gallstones) is a very common reason for abdominal pain. In fact, about 10-20% of Americans have gallstones, and about 1/3 of those will at some point have cholecystitis because of them.
Cholecystitis is very similar to appendicitis, just instead of the opening of the appendix getting blocked, the opening of the gallbladder does. About 90% of cholecystitis cases occur when a stone gets lodged in the tube that carries bile from the gallbladder to the small intestine.
While the pain is described as being abdominal, there is a lot of referred pain associated with the gallbladder, often in the shoulders, back, and chest. This can make it so that the person coming into the emergency room initially complains of pain in one of these areas.
If someone comes in and says their chest hurts, the hospital has to rule out something serious- like a heart attack or PE- before they can move on. Usually this involves taking bloodwork, doing an EKG, taking an X-ray or CT of the chest, and if anything comes of that, giving morphine and/or a beta blocker to reduce workload on the heart while setting up to go to the cath lab to remove the clot or place a chest tube.
If it's gallbladder pain, nothing is going to come of this- it's all going to come up normal, so they'll start working on other things. Usually this involves more bloodwork and more physical exam, as well as a CT of the abdomen.
The quickest and cheapest physical exam way to tell if someone's pain is caused by their gallbladder is to press straight down under the patient's ribcage on the right side, then tell the patient to take a deep breath. As the person breathes in, the diaphragm pushes down on the liver, which sandwiches the gallbladder between the liver and the examiner's hand, which hurts so much the person usually can't take the whole breath. This is called Murphy's sign.
As for how often the person might get pain meds- on a floor 2-6 hours depending on the med is standard- and they'll have to ask for them each time because of how they're ordered. In an emergency room, they're probably going to be lucky if they get them once, since in the ED, med doses are typically ordered individually.
Since cholecystitis isn't usually immediately life threatening, they'll either admit the person to a floor where they can get pain medicine until an OR opens up for a non-emergent slot, or they'll send the person home with some oral pain meds and schedule the surgery outpatient.
27 notes
·
View notes