#Gallbladder Inflammation
Explore tagged Tumblr posts
Text
Understanding Cholecystitis: Causes, Symptoms, and Treatment
Imagine this: You're enjoying your favorite meal when all of a sudden, you're hit with a sharp pain in your upper abdomen that radiates to your right shoulder, making it difficult for you to even sit up straight. You're experiencing cholecystitis!
Imagine this: You’re enjoying your favorite meal when all of a sudden, you’re hit with a sharp pain in your upper abdomen. It’s so intense that it radiates to your right shoulder, making it difficult for you to even sit up straight. You’re experiencing cholecystitis, an inflammation of the gallbladder that can cause severe abdominal pain and other complications. This article aims to provide an…

View On WordPress
#Abdominal Pain#Cholecystectomy#Cholecystitis#digestive health#Gallbladder Inflammation#Gallstones#Health and Wellness#Medical Treatment#Preventive Care#Symptoms and Diagnosis
0 notes
Text
tummy ache got me googling whether indica or sativa is better for nausea
#bitch i’m dying#the doctors don’t think anything is wrong ^w*#the only thing that even KIND OF helped was taking double the recommended dose of the strongest gas pill on the market every day#but that stuff is super expensive so i can’t afford to take it every day#none of my scans or bloodwork showed anything except for slightly elevated levels of inflammation according to my blood test#but all my abdominal ultrasounds and x rays are normal#i don’t even have an ulcer this time#and my gallbladder and liver look fine#so i don’t fucking know#lesley time
2 notes
·
View notes
Text
ARGHH...... i have to be up at 5:30 and its already 1:30........
we have to drive my sister to the train station in tacoma bc shes going down to portland for the weekend. the train leaves at 8 fucking am
good thing is my mom is dropping me off at the ER which is on the way to tacoma fjdkslfs and it works out bc she has to pick up stuff for her next post-cancer check in... BUT 5:30 AM.........
#yappin#my tummy hurtie and i want answers is it my gallbladder or some sort of stomach inflammation disease or both arghh#i ate a small salad with a couple vegan chicken nuggets bc i needed to eat some sort of vegetable#i cannot live on chicken and stars soup forever
5 notes
·
View notes
Text
A REGULATED NERVOUS SYSTEM = SUCCESS
This is list of some of the diseases and conditions a women can get due to chronic stress. I have said it before, messing with someone’s nervous system is a form of abuse because it not only deliberately disrupts your mental and emotional stability, it can cause long term harm to your health!!!!
Cardiovascular disease
Hypertension
Stroke
Diabetes
Obesity
Depression
Anxiety disorders
Gastrointestinal disorders (IBS, ulcers)
Autoimmune diseases (lupus, rheumatoid arthritis)
Thyroid disorders (hyperthyroidism, hypothyroidism)
Infertility
Menstrual irregularities
Osteoporosis
Chronic fatigue syndrome
Sleep disorders (insomnia)
Migraine and tension headaches
Fibromyalgia
Alzheimer’s disease and cognitive decline
Eating disorders
Chronic pain disorders
Endometriosis
Polycystic ovary syndrome (PCOS)
Heart arrhythmias
Metabolic syndrome
Adrenal fatigue
Hair loss (telogen effluvium, alopecia)
Chronic inflammation
Eczema and psoriasis
Acne and other skin disorders
Urinary incontinence
Osteoarthritis
Temporomandibular joint disorder (TMJ)
Chronic pelvic pain
Sexual dysfunction
Nonalcoholic fatty liver disease (NAFLD)
Weakened immune system (leading to frequent infections)
Vision problems (stress related blurred vision)
Hearing loss or tinnitus
Substance use disorders
Increased risk of cancer (breast, ovarian)
Hormone imbalances
Gallbladder disease
Hyperprolactinemia
Chronic kidney disease
156 notes
·
View notes
Text
A couple of the blood tests that the hospital did a week ago said that I have a little bit of inflammation in my body but that test was done before I had my gallbladder removed, which was inflamed. So, could you please pray that the inflammation they found was only because of my gallbladder and not something else? Thank you
22 notes
·
View notes
Text
Doctor said I have inflammation/infection around my gallbladder. So a general surgeon and his team are coming to talk to me. Sometimes they do antibiotics or it'll be surgery... im scared
24 notes
·
View notes
Note
Any updates? Did you have your surgery? I'm wishing you the best.
Also, I know how terrifying it is to have a major surgery for the first time. Funny enough, I wasn't much older than you when it happened either. I was 24. I've had two brain surgeries, and for the first one I was literally freaking out. Then I woke up, and everything was fine.
You got this, friend! I'm hoping for the best for you! 💝
Oooh my god I am SO SORRY for disappearing after dropping all those bombs💀💀💀
So! Imma try to give you a summary of what happened.
I had surgery the day after they admitted me into the hospital, but unfortunately it was not the surgery I was waiting for🫠
Essentially, a stone went down into my bile duct and was pretty much suffocating my gallbladder, which would've made it impossible to remove my gallbladder safely because it was getting all inflamed.
So, they instead opted to remove the stone that was obstructing the bile duct so that, you know, my blood values could start going back to normal and such.
The surgery itself was rather quick and it went well. . . Buuuuuuuut there were some itty bitty complications🥲
The stone had descended reeeal low and was very close to my pancreas, and when that happens there can be some not very fun side effects to the surgery.
Long story short, the surgery gave me very bad pancreatitis and I have been in pain for a whole week by now lmao.
Oh, well, now I feel better, but recovery is still a bit far from reach. The first two days were absolutely excruciating and they had to give me two rounds of morphine just to get me to sleep through it and recuperate. Now I can sit up, breathe, walk, eat. VERY slowly and with A LOT of effort, but it's already so much more than I could do, say, four days ago.
Now it's mostly a matter of waiting for the inflammation to go down and the fluids to kinda fuck off from where they don't belong aaaaand while we are at it try to understand why the fuck I am always running a fever even on paracetamol.
So essentially, I am doing better! Not well, but better. And I thank you for checking in on me!❤️
Also, brain surgery sounds terrifying. And at 24?? What a trooper!
7 notes
·
View notes
Text
https://www.telegraph.co.uk/health-fitness/conditions/cancer/the-little-known-cancer-thats-linked-to-the-gut/
“The surge in cases of cancer in the under-50s has made many of us worry, with bowel, breast and lung cancers among those increasing most rapidly. But what is more surprising is that rates of aggressive gallbladder cancer have risen even more sharply, affecting many more women than men, particularly those who have had children. It’s also more likely in those who have suffered from the common problem of gallstones.
The figures are alarming, with cases having doubled in British people aged between 24 and 49 in the past three decades, according to Cancer Research UK. But the good news is that there are measures you can take to limit the risk of the disease, through changes to your diet and lifestyle.
Here, our experts explain what exactly the cancer is, the reasons it is spiking in younger people and what we can do to increase our chances of avoiding it.
What is gallbladder cancer?
The gallbladder is an apple-sized organ near the liver and is primarily responsible for storing bile, a substance produced by the liver and used by the body to break down the fats we eat.
Thousands of years ago, humans might have eaten one big meal every few days and “we might have needed that extra boost of bile to help us digest it, if the liver couldn’t produce it fast enough,” says Dr Anita Balakrishnan, a consultant hepatopancreatobiliary (HPB) surgeon at Addenbrooke’s Hospital and an associate lecturer at the University of Cambridge..
“The gallbladder is a vestigial organ, like the appendix – now we don’t really need it for normal digestion, and sometimes it causes trouble.’”
Cancer occurs when healthy cells in the gallbladder develop genetic mutations that cause them to grow and multiply out of control. Just over 1,000 cases have been diagnosed in the UK each year, equivalent to about three per day and, “sadly, it’s an aggressive cancer,” says Dr Balakrishnan.
What are the risk factors?
According to Cancer Research UK, women account for 71 per cent of cases. In women who have given birth, particularly those who have had five or more children, the risk is increased.
The reason for this is not fully known, but women are two to three times more likely to suffer from gallstones, which are a major risk factor for gallbladder cancer. Oestrogen can increase cholesterol levels in bile and decrease gallbladder contractions, which can lead crystals to form in the bile and create stones. During pregnancy, the gallbladder also grows in volume.
“Having gallstones doesn’t necessarily mean you’ll get cancer, but they cause inflammation of the gallbladder, which puts people at a higher risk,” says Mr Shahid Farid, a consultant surgeon with a specialism in gallbladder surgery at Nuffield Health Leeds Hospital.
People with a family history of gallbladder cancer are five times more likely to develop the disease, and it is more common in people of Asian descent.
Smoking and obesity also increase the risk, with the rise in obesity since the mid-1990s believed to be a major factor in the increase in cancer among younger people, in particular.
What are the main symptoms, treatment and survival rate?
Unfortunately, gallbladder cancer is often a silent disease which becomes symptomatic only in its later stages.
“Any symptoms people have are usually non-specific, such as tiredness and perhaps some abdominal discomfort,” says Mr Farid.
Eventually, symptoms can include jaundice, pain in the upper right abdomen, weight loss, nausea and vomiting. “By that stage, it has usually grown beyond the gallbladder and is at an advanced stage,” he says.
It is often detected by chance during operations, for instance to remove gallstones, and if it is contained within the gallbladder, the five-year survival rate is 60-70 per cent. If it has spread to local tissues or lymph nodes, survival rates are almost 30 per cent, while if it has spread to more distant areas, rates are under 5 per cent.
If possible, treatment involves surgery, along with chemotherapy.
What can we do to minimise our risk?
1. Maintain a healthy weight
Being overweight and obese is the second biggest cause of cancer in the UK, after smoking. Several studies have found a link between an increased risk of gallbladder cancer and a BMI of over 25, with the World Cancer Research Fund stating that the risk increases by 25 per cent per 5 kg/m2 increase in BMI.
One recent Norwegian study found a concerning 47 per cent increased risk in women per 5 kg/m2 increase in BMI, while the increased risk in men was smaller and not statistically significant. It also showed a decreased survival rate for overweight and obese women with gallbladder cancer.
“Eating a healthy diet and staying within a healthy BMI range will help avoid gallbladder cancer,” says Dr Balakrishnan. “Giving up smoking and keeping alcohol consumption under recommended limits is also vital.”
2. Look after your microbiome
In recent years, scientists have increasingly focused on the microbiome, the ecosystem of bacteria which populates the gut, when searching for causes of the increase in early-onset cancers.
“Research into the influence of the microbiome on cancers including gallbladder cancer is still in its early days, but it’s only logical that it plays a part,” says Mr Farid. “Our microbiome can contribute to inflammation, and that can predispose us to cancer.”
A Chinese study from 2023 investigated the microbiome of patients with biliary tract cancers, of which gallbladder cancer is one. It found patients with the disease had increased levels of the Enterobacteriacae bacteria, and decreased levels of others including Clostridia, suggesting an imbalance. Both are associated with inflammation.
We can boost the diversity and good bacteria in our microbiome with fermented foods such as kefir, sauerkraut and kimchi, and prebiotic foods like mushrooms, onions, garlic, asparagus, leeks and apples, which feed the bacteria in our gut.
Good bacteria such as Clostridia can naturally be found in food such as vegetables, while high-fibre foods such as fruit, wholegrains and nuts will also nurture the microbiome.
3. Avoid fried, fatty foods and sugary drinks
The link between different types of diet and higher rates of gallbladder cancer is still being researched, but some studies have highlighted certain principles by which it’s best to live.
Eating too many fatty and fried foods have been linked to an increased chance of getting the disease because they raise cholesterol which is linked to gallstones, which are in turn strongly linked to gallbladder cancer.
Red meat, and particularly processed meat containing nitrates, is also associated with a higher risk, so cutting down to 455g of cooked lean red meat per week is recommended.
Drinking sugar-sweetened and artificially sweetened beverages has been shown to double the risk of gallbladder cancer when individuals drank 400ml or more per day. This is thought to be because increased sugar consumption is linked to a higher BMI, and also to Type 2 diabetes, which increases the risk of cancer.
Ultra-processed foods (UPFs) are linked to a higher incidence of all cancers, and researchers believe they may be a major driver of the increase in cancers among under-50s. “Reducing the amount you consume and eating unprocessed food where possible is best,” says Mr Farid.
4. Eat the DASH diet
One Swedish study revealed that two types of healthy diet are associated with a lower risk. One is the Dietary Approach to Stop Hypertension, or DASH, which includes fruits, vegetables, whole grains, low-fat dairy, and lean protein from chicken, fish, beans and nuts. It avoids foods high in salt, saturated fat, and added sugar. The second is the Mediterranean diet, which follows very similar principles.
One Indian study reported that eating sweet potatoes was associated with a lower risk of gallbladder cancer, along with green chillis, radish, mango, orange and melon – all of which contain high levels of antioxidants.
5. Exercise regularly
Regular physical activity has been shown to be likely to reduce the risk of gallbladder cancer, and studies have shown it can increase the diversity of the gut microbiome.
“Exercise also promotes cell turnover in a different way to when you’re sedentary,” says Mr Farid. “It also reduces the amount of fat and also inflammatory cytokines in your blood. So it’s one of the most important things you can do to modify your risk of many cancers, including gallbladder.””
6 notes
·
View notes
Text
Vet Bills and a Sick Kitty Boy
Hello all, over the past month and a half I have incurred some medical bills for my cat Alistair, that while one bill hurts but isn't world ending. Multiple have put us in a bind.
Our Total: $430/$1176.86
My Paypal: tielfingriley or paypal.me/tieflingriley
The Story:
So my sweet yet very hungry boy Alistair, had been having stomach troubles. He's 12 years old, so not uncommon for a cat his age, and he has always had a bit of a sensitive tum, but this was different. He was projectile vomiting mostly water, and I had noticed he was loosing weight. He is a long cat, and his healthy weight sits at 15-16 pounds.
So we take him to the vet and the do a initial blood panel with a special panel to check a for a heart protein, it is here that I learn my asthmatic cat also has a heart murmur! But because of the special check it had to be sent to THE ONLY LAB IN THE US THAT CHECKS FOR IT, which meant it was pricey

Good news, blood came back fine. His heart and kidneys weren't failing but he was still vomiting water at this time. At this point we were moved to a different vet who noted his long term tum issues. Informing me that long term inflammation can lead to Gastrol Intestinal Cancer. (Maybe) They only DEFINITIVE way of checking was to slice him open and do biopsies, which wasn't ideal. Instead we opted for an Ultrasound, it would check for inflammation, which would say absolutely yes or no on inflammation, but would still be a maybe on the cancer (however its the same treatment either way). But could also check Liver, Pancreas, and Gallbladder. I of course chose this because it was far less invasive to the boy. Alistair did need to be sedated. He isn't a violent cat, but he is a squirmy noodle.
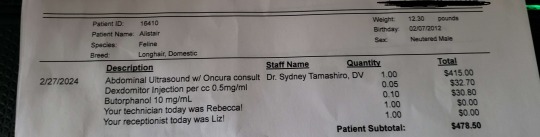
This is when things got really spicy for us financially. You see this happened RIGHT before my birthday. Like legit I found out my cat had maybe cancer the day before. And my husband a few weeks prior had bought me a rather nice gift of storage drawers? IDK what you would call it but furniture for my art supplies to be stored in. It was a bit pricey but I was having a rough time and a history of astronomically shitty birthdays. (As you can see, the universe has a sense of humor)
So the Ultrasound came back. Yes there are signs of inflammations, so cancer is still a maybe. However, what had the doctors eyes and was concerning her more was the pancreas. It was, extended and incorrect. She believed that it wasn't producing a enzyme to help break down food, particularly fat, for absorption. Essentially, on top of the inflammation, Alistair was slowly starving to death. However before just popping some pig panceas pills inside my boy, she wants to make sure. So more blood work, TO THE ONLY LAB IN THE US OF COURSE, an another bill.
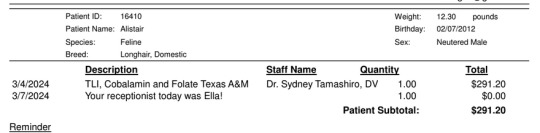
Now we are waiting on this information. He is on some pro and prebiotics that have stopped the vomiting entirely. However his weight is still quite thin. I am unsure if we will have more hefty bills. For reference a checkup at this vet is 50 bucks. So normally its not to rough on us, and check up plus vaccines is 100 which is a planned event. None of this was planned to say the least.
AND NOW THE SAPPY SHIT
Alistair saved my life. I know logically getting a cat as a means to not kill yourself isn't the best thing to do, but sometimes you gotta do what you gotta do. Ive had him since September of 2012. I love that fluffy biscuit stealing bastard with my entire heart. I have a tattoo on him on my arm, my first and currently only tattoo. Because of him, I was able to live a longer and healthier life and I want that for him.
Despite being a cat, he loves biscuits, potato chips, and the tops of muffins but only the tops. He can and will open cookie jars for cookies. I have explained he is an obligate carnivore and he has explained like a good southern he cant turn down a carb.
He will fist fight you for cheese. Love to play fetch with a hair tie. Isn't a lap cat with the exception of me. LOVES NAPS, and likes to watch Markiplier.
He's a very good boy with separation anxiety, and tummy issues who just wants to nap and eat and I think we can all relate.



Oh...and he has a little mustache
Thank you to all who donate and to everyone who spreads the word to help us get out of this debt.
#Fundraising#gofundme#Donate if you can#But absolutely reblog#Thank you so much#Alistair the cat#Cat
31 notes
·
View notes
Note
So say I’m writing a one shot series (think whumptober prompts but related) of whumpy incidents where a character keeps getting injured in different ways. Because of these incidents, they have repetitive damage to their chest/ribs/lungs over the course of a decade or so (they end up in a lot of motor vehicle-related accidents for plot reasons).
how:
1- do I keep things different enough for the audience to keep things exciting, injury-wise
2- does getting hurt/healing in this place over and over again impact their medical health as time goes on?
I'm really not sure about this one. Maybe complications? After chest trauma, you might see things like pneumonia, pneumothorax/hemothorax (air or blood in the sac that surrounds the lung that compresses the lung and restricts ventilation), cardiac tamponade (like a hemothorax but in the lining of the heart), sepsis (systemic infection characterized by bacterial infestation of the blood that can lead to rapid decompensation), mediastinitis (inflammation of the space in the chest that contains the heart, great vessels, trachea, bronchi, esophagus, phrenic nerve, vagus nerves, and thoracic duct), atelectasis (state in which a lung no long inflates), fistulas (openings between hollow body structures that don't normally connect [example: a hole between the trachea and esophagus]), thromboembolic events (blood clots that usually form in the legs or pelvis and can travel to other parts of the body [examples: deep vein thrombosis, pulmonary embolism]), disseminated intravascular coagulation (a condition in which the platelets form clots that block small vessels, depleting the body's platelet supply and causing increased bleeding), gastric or duodenal ulcers (erosions of the inner lining of the stomach or topmost portion of the small intestine that often develop after severe trauma), and cardiac dysrhythmias or heart block (irregular patterns or electrical activity in the heartbeat that can lead to a variety of issues if left untreated).
This one is tough, and I'll answer it with the unofficial motto of nursing: it depends. How fast was the car going when the accident occurred? Was the chest trauma blunt or penetrating? Did the patient sustain other injuries (e.g., head injuries, spinal injuries, abdominal injuries)? How old is the patient? Does the patient have other health problems (e.g., diabetes, asthma, hypertension, etc.)? How well were the injuries managed initially? Did the patient comply with the treatment regimen? That being said, injuries often sustained in chest trauma include fractured ribs, fractured sternum, fractured clavicles (collar bones), pneumothorax or hemothorax, cardiac tamponade, flail chest (a condition in which a part of the lung inflates out of sync with the rest of the lungs after three or more ribs have been fractured), bruising to the chest muscles, bruising to the lungs, bruising to the heart, injury to the great vessels (laceration or rupture of the aorta or vena cava), injury to the airways (crushing, laceration, or rupture of the trachea or bronchi), injury to the esophagus (laceration or rupture), diaphragmatic rupture, and internal or external hemorrhage. Abdominal injuries are also common in motor vehicle accidents, so you may also see bruising or laceration of the liver (VERY bad; the liver bleeds a lot), pancreatic injury, gallbladder injury, splenic rupture (very VERY bad, also bleeds a lot), stomach bruising and perforation, intestinal perforation (also very bad, gastrointestinal bleeds can kill in hours), bladder bruising or perforation, kidney injury (bruising, laceration or rupture), and uterine or testicular injury. You may also see vertebral fracture and spinal cord injury, pelvic fracture, and head injuries. Some of the invasive treatments you might see for these are multiple surgeries, some of which may be reconstructive; ventilator use, placement of plates, screws and wires to fix serious fractures; placement of a gastrostomy/duodenostomy/jejunostomy/ileostomy feeding tube (a tube tunneled through the abdominal wall into the stomach, or small intestine); and removal or the spleen, pancreas, gallbladder, stomach, portions of the intestines, bladder, or uterus or teste(s). Since everyone is different and heals from injuries differently, I can't tell you for sure what some of the long-term sequelae of these injuries would be, but I can make some educated guesses. The great vessels, particularly the aorta, may become weakened after injury and repair and may rupture down the road. The lungs may also be weakened following injury, leading to decreased ability to breath effectively. A damaged heart may weaken or hypertrophy (the muscle thickens), leading to heart failure. Removal of the spleen can predispose someone to infections. Removal of the pancreas creates lifelong need for insulin, glucagon, and pancreatic enzymes. Removal of the gallbladder requires a low-fat diet. Removal of the stomach requires lifelong vitamin B12 injections. Removal of parts of the intestines causes reduced absorption of nutrients and water, and the removal of a significant amount of the intestines may require an ostomy. Removal of the bladder can require construction of a neobladder or ostomies to drain urine externally. The patient may receive a kidney, liver, pancreas, lung, or heart transplant if theirs are damaged enough, which would require them to be on immunosuppressive medications for the rest of their life. Vertebral fracture and spinal cord injury may cause reduction or loss of motor or sensory function below the injury, which can lead to mobility issues, bowel and bladder control issues, and increased potential for injury due to decreased sensation. Head injuries may lead to vision and hearing problems, speech problems, amnesia, cognitive issues, and seizures. Repeated head injuries can cause dementia-like cognitive decline.
For more information on any of the above, check out the National Library of Medicine.
Happy whumping!
3 notes
·
View notes
Text
Maomao no Hitorigoto Episode 19 : Ox Bezoar / 猫猫のひとりごと 第19話 『牛黄(ごおう/Go-o)』
Please note that the English lines are just my translations.
猫猫「うーん…塩の過剰摂取(かじょうせっしゅ)による死…海藻の食中毒…爆発…。どれも仕組まれた出来事だとしたら…やはり、あの官女が?」
Maomao “Uuun… Shiono kajo-sesshuni-yoru shi… Kaisono shoku-chudoku… Bakuhatsu… Doremo shiku-mareta deki-goto-dato-shitara… yahari, ano kanjoga?”
Maomao “Hmm… The death from salt overdose… Seaweed food poisoning… The explosion… If all of them were staged events… As I thought, was that court lady the one?”
壬氏「薬屋。随分(ずいぶん)熱心だな」
Jinshi “Kusuriya. Zuibun nesshin-dana.”
Jinshi “Apothecary. You’re very enthusiastic, aren’t you?”
猫猫「はい!これから書庫で調べ物をして参ります!」
Maomao “Hai! Korekara shokode shirabe-mono’o shite-mairi-masu!”
Maomao “Yes! Now I’m going to the court library to do some research!”
壬氏「あ…そ、そうか。ところで、あの牛黄という品は、そんなに貴重な物なのか?」
Jinshi “A…So, Soka. Tokorode, ano Goo-to-iu shinawa, sonnani kichona mono nanoka?”
Jinshi “I-I see. By the way, is that item called ox bezoar really that valuable?”
猫猫「よくぞ聞いて下さいました!」
Maomao “Yokuzo kiite-kudasai-mashita!”
Maomao “That’s nice of you to ask!”
猫猫「猫猫の豆知識。牛黄は、牛の胆嚢(たんのう)にできた胆石(たんせき)。希少性(きしょうせい)が高いことや、効能(こうのう)あらたかな生薬(しょうやく)として、ひときわ価値のある特別な存在。金と同額で取引されることもある」
Maomao “Maomaono mame-chishiki. Goowa, ushino tannoni dekita tanseki. Kisho-seiga takai-kotoya, kono-aratakana shoyaku-to-shite, hitokiwa kachino aru tokubetsuna sonzai. Kinto dogakude torihiki-sareru-kotomo aru.”
Maomao “Here’s Maomao’s bits of knowledge. Ox bezoar is a gallstone that forms in the gallbladder of a cow. It is a very valuable and special entity as a very rare and highly effective herbal medicine. It’s sometimes traded for the same price as gold.”
猫猫「不老長寿(ふろうちょうじゅ)の薬、命を養う薬とも言われ、高熱や炎症を抑えるのはもちろん、心臓の働きを高めて、健忘予防(けんぼう・よぼう)にも使われるとか。おまけに死人の邪気を払う効果が…」
Maomao “Furo-Chozuno kusuri, inochi’o yashinau kusuri-tomo iware, konetsuya ensho’o osaeru-nowa mochiron, shinzono hataraki’o takamete, kenbo-yobo-nimo tsuka-wareru-toka. Omakeni shinin’no jaki’o harau kokaga…”
Maomao “It’s said to be a medicine for eternal youth and longevity, and a medicine that nourishes life. It not only suppresses high fevers and inflammation, but also enhances heart functions and prevents amnesia. In addition to that, it’s said to ward off evil spirits of the dead…
壬氏「おっ…おお、おおお。も、もう十分だ!」
Jinshi “O…Oo, ooo. Mo, Mo jubunda!”
Jinshi “Oh… Oh, oh. That’s enough!”
猫猫「そうですか」
Maomao “Sodesuka.”
Maomao “Is that so?”
壬氏「お前の牛黄に対する情熱は分かった」
Jinshi “Omaeno gooni taisuru jonetsuwa wakatta.”
Jinshi “I understood your passion for the ox bezoar.”
猫猫「私だけでなく、世界中の薬師にとって、垂涎(すいぜん)の一品(いっ���ん)でございます」
Maomao “Watashi-dakede-naku, Sekai-juno kusushini totte, suizen’no ippinde gozai-masu.”
Maomao “This is a coveted item not only for me, but for pharmacists of all over the world.”
猫猫(きっとおやじも喜ぶはずだ…!もし牛黄が手に入ったら…ぐふ~!)
Maomao (Kitto oyajimo yorokobu-hazuda…! Moshi googa teni haittara… Gufuuu!)
Maomao (I’m sure my dad will be happy…! If I can get that ox bezoar…!)
壬氏「…はぁ…」
Jinshi “…Haa…”
Jinshi (sigh)
猫猫「次回、『曼荼羅華』。ついに、この騒動の真犯人が…。お楽しみに」
Maomao “Jikai, ‘Mandarage.’ Tsuini, kono sodono shin-hanninga… Otanoshimini.”
Maomao “Next episode, ‘Thornapple.’ Finally, the real culprit of this commotion will be… See you next time.”
―――――――――――――――――――――――――――――――
「やはり(Yahari)」「やっぱり(Yappari)」: as I thought, I knew it.
「熱心な(ねっしんな/Nesshin-na)」: enthusiastic, eager
「よくぞ聞いて下さいました!」; That’s nice of you to ask! Thanks for asking that!
「ついに(遂に/Tsuini)」: finally, at last, eventually
「垂涎の一品/逸品(すいぜんのいっぴん)」: coveted item, a mouth-watering dish
「垂(すい/Sui)」「垂れる(たれる/Tareru)」: droop
「涎(ぜん/Zen, よだれ/Yodare)」: drool
#apothecary english#apothecary romaji#the apothecary diaries#apothecary diaries#learning japanese#japanese#薬屋のひとりごと#薬屋のひとりごと 英語#薬屋 英語 学習#japan#KNH
3 notes
·
View notes
Text
The issues that might plauge Vomiting Vera.
Based off the posts made by @/2astralightthestoryteller1 & @/yupthatsoundsright. (because credit baby!)
This is basically going to be a run-down of estimates of conditions that she may potentially dealing with.
Why am I writing this out? Because I feel like answering the question everybody’s been asking. To my dismay /hj.
First, what is up with her? … There’s not much to go off. She just vomits a lot. It seems that there is no triggers or actual reason why she might be vomiting quite a bit.
Another thing we can look at is the color or her vomit. Sounds gross but trust me.. it matters? For the most part. At first it was green but then it turned beige.
What does this tell us? When it was green it was most likely bile. Which is a fluid that helps your body digest fats from foods. It’s made in your liver and stored in your gallbladder.
What causes somebody to throw up bile? Vomiting on an empty stomach, food poisoning, or a blockage in the intestines. It also says binge drinking but I don’t think a baby is doing that lol.
Based off how frequent she IS vomiting, it could also be bile reflux. Which happens when bile backs up from your liver into your stomach and esophagus.
So if she DID have a blockage to her intestines; there’s some reasons why it could be happening. Certain cancers and tumors, Diverticulitis (small pouches to form in the intestinal wall.) Hernia (A weakening in part of the intestine that causes it to bulge out into the abdomen or another part of the body.) IBD (Inflammation in the intestine.) and Volvulus which is a twisting of the intestine.
Though what if it ISN’T a blockage to her intestines? Then it could also be liver failure & Gastroenteritis.
But whatever it was, it wasn’t permanent. Because at some point the color of her puke turned stopped being green and turned beige.
Beige? Is that even a real color of vomit you ask? Not exactly. There’s clear and white vomit. No beige. But for this sake I’m calling it white for realism.
What could cause white vomit? The most common cause is excess gas. It also says that drinking a lot of milk could cause it. You may think that’s a dumb reason to include but she is a infant and is drinking breast milk so I imagine.. that COULD be a reason.
But back to the idea of excess gas. What causes that? Acid reflux, Gastritis, and Gastroenteritis.
Let’s cut to the chase. Based off the facts. It might be Gastroenteritis. Why? Because it showed up as reasons for both green and white vomit. The stomach flu.. That does sound a bit stupid doesn’t it? I mean come on.. how many times can a infant catch a stomach flu?
Eh… There could be reasons why she could get it a lot. She could be somebody who catches virues easily, she could have parasites, or you know… she’s being poisoned.
Wow that’s a bold claim! I know. Either her parents are stupid (ie; not cooking food well enough or keeping chemicals easily accessible) or she’s being poisoned on purporse. Who can really know? I know the conclusion is very.. bare-boned. And I just went for an accusatory claim but either she has some chronic illness or she’s being poisoned by her parents.
So the answer the question of “What the fuck is wrong with this child (Vera)?”; It’s either something up with her guts or she’s being poisoned. Pick your choice.
3 notes
·
View notes
Text
i have my gallbladder scan tomorrow. i want it to either be clean and i don't know it was just an inflammation crisis or whatever, or i want it to be filled with stones and ready to explode
#My doctor said because my bloodwork was ok and it seems like my other organs haven't been affected from my horrible crisis from august#we wouldn't be able to ask for surgery if it's just a couple of stones in there#and that would mean possibly having recurring crises until my other organs actually do suffer from it#Well that's a shitty rule#personal
4 notes
·
View notes
Text
I know why hospitals are cold but got damn it's cold in here
Dad just went for a CAT scan for potential respiratory distress (judging by the nurse's(?) >:O reaction to dad saying he doesn't wear his oxygen when he goes to the bathroom, that might be related). The nurse confirmed that they're waiting for inflammation to go down before they remove the gallbladder.
But his bowels are unblocked, so that's one less thing to worry about
He's tired of being in the hospital though. He starts calling it "The Pain Palace" after a few days sdfghjkl Partly because he's a hard stick with a needle
2 notes
·
View notes
Note
I'm writing a story where a male character has gallstones. It happened to me a long time ago so I don't remember how they ran tests at the hospital to get to that diagnosis. I just remember the chest/back pain was terrible. How would they rule out a heart attack in the emergency room? What else would they test for? Are gall bladder stones common enough that a nurse or doctor thinks to check before an x-ray?
If the hospital is busy, how long is a patient allowed to be in severe pain until it warrants more meds (I've heard of morphine being used).
Cholecystitis (inflammation of the gallbladder, often related to gallstones) is a very common reason for abdominal pain. In fact, about 10-20% of Americans have gallstones, and about 1/3 of those will at some point have cholecystitis because of them.
Cholecystitis is very similar to appendicitis, just instead of the opening of the appendix getting blocked, the opening of the gallbladder does. About 90% of cholecystitis cases occur when a stone gets lodged in the tube that carries bile from the gallbladder to the small intestine.
While the pain is described as being abdominal, there is a lot of referred pain associated with the gallbladder, often in the shoulders, back, and chest. This can make it so that the person coming into the emergency room initially complains of pain in one of these areas.
If someone comes in and says their chest hurts, the hospital has to rule out something serious- like a heart attack or PE- before they can move on. Usually this involves taking bloodwork, doing an EKG, taking an X-ray or CT of the chest, and if anything comes of that, giving morphine and/or a beta blocker to reduce workload on the heart while setting up to go to the cath lab to remove the clot or place a chest tube.
If it's gallbladder pain, nothing is going to come of this- it's all going to come up normal, so they'll start working on other things. Usually this involves more bloodwork and more physical exam, as well as a CT of the abdomen.
The quickest and cheapest physical exam way to tell if someone's pain is caused by their gallbladder is to press straight down under the patient's ribcage on the right side, then tell the patient to take a deep breath. As the person breathes in, the diaphragm pushes down on the liver, which sandwiches the gallbladder between the liver and the examiner's hand, which hurts so much the person usually can't take the whole breath. This is called Murphy's sign.
As for how often the person might get pain meds- on a floor 2-6 hours depending on the med is standard- and they'll have to ask for them each time because of how they're ordered. In an emergency room, they're probably going to be lucky if they get them once, since in the ED, med doses are typically ordered individually.
Since cholecystitis isn't usually immediately life threatening, they'll either admit the person to a floor where they can get pain medicine until an OR opens up for a non-emergent slot, or they'll send the person home with some oral pain meds and schedule the surgery outpatient.
27 notes
·
View notes
Text
Choosing the Right Gastrointestinal Tract Drug – Factors to Consider
The gastrointestinal (GI) tract is a complex system responsible for digestion and absorption of nutrients. Given its critical function, disorders affecting the GI tract can significantly impact overall health and quality of life. Selecting the right medication to treat these conditions is essential for effective management and recovery. Centurion HealthCare, a leading gastrointestinal tract drugs supplier in India, offers a range of high-quality medications designed to address various GI disorders. In this article, we will explore the factors to consider when choosing the right gastrointestinal tract drug, and why Centurion HealthCare stands out in the best pharmaceutical industry in India.

Understanding Gastrointestinal Tract Disorders
GI tract disorders encompass a wide range of conditions affecting different parts of the digestive system, including the esophagus, stomach, intestines, liver, pancreas, and gallbladder. Common GI disorders include:
Gastroesophageal Reflux Disease (GERD)
Peptic Ulcer Disease
Irritable Bowel Syndrome (IBS)
Inflammatory Bowel Disease (IBD)
Hepatitis
Pancreatitis
Each condition requires specific treatment strategies and medications to manage symptoms, promote healing, and prevent complications.
Factors to Consider When Choosing a Gastrointestinal Tract Drug
Choosing the right drug for treating GI disorders involves multiple factors, including the specific condition, the patient’s medical history, and potential side effects. Here are key considerations:
1. Accurate Diagnosis
An accurate diagnosis is the first step in selecting the appropriate medication. Physicians use various diagnostic tools such as endoscopy, colonoscopy, imaging studies, and laboratory tests to identify the specific GI disorder. Understanding the underlying cause and severity of the condition is crucial for effective treatment.
2. Mechanism of Action
Different gastrointestinal tract drugs work through various mechanisms to achieve therapeutic effects. Understanding how a drug works helps in selecting the most suitable option. Common mechanisms include:
Antacids: Neutralize stomach acid, providing quick relief from heartburn and indigestion.
Proton Pump Inhibitors (PPIs): Reduce the production of stomach acid, effective in treating GERD and peptic ulcers.
H2 Receptor Antagonists: Decrease acid production by blocking histamine receptors in the stomach lining.
Prokinetics: Enhance gut motility, useful in conditions like gastroparesis.
Antispasmodics: Relieve intestinal cramps and spasms, often used in IBS treatment.
Anti-inflammatory Drugs: Reduce inflammation in the GI tract, essential for managing IBD.
3. Efficacy and Safety
The efficacy and safety profile of a drug are critical factors in the decision-making process. Clinical trials and real-world studies provide valuable information on a drug’s effectiveness and potential side effects. Physicians must weigh the benefits against the risks to ensure the chosen medication offers the best possible outcome for the patient.
4. Patient-Specific Factors
Each patient is unique, and various individual factors can influence drug selection. These include:
Age: Certain drugs may be more suitable for children, adults, or the elderly.
Medical History: Pre-existing conditions, such as kidney or liver disease, can affect drug metabolism and tolerance.
Allergies: Patients with known drug allergies must avoid medications that could trigger adverse reactions.
Concurrent Medications: Drug interactions can impact efficacy and safety, requiring careful consideration of all medications the patient is currently taking.
5. Route of Administration
The route of administration can affect the drug’s efficacy and patient compliance. Common routes for GI drugs include:
Oral: Tablets, capsules, and liquids are convenient for most patients.
Intravenous: Used in severe cases or when oral administration is not feasible.
Topical: Suppositories and enemas are used for localized treatment in the lower GI tract.
6. Cost and Availability
Cost can be a significant factor, especially for long-term treatments. Generic versions of drugs often offer the same efficacy as brand-name medications at a lower cost. Availability of the drug in the local market is also crucial to ensure uninterrupted treatment.
Centurion HealthCare: Leading the Way in GI Tract Drug Supply
Centurion HealthCare has established itself as a premier gastrointestinal tract drugs supplier in India, renowned for its commitment to quality, innovation, and patient care. Here’s why Centurion HealthCare is a trusted name in the best pharmaceutical industry in India:
1. Comprehensive Product Range
Centurion HealthCare offers a wide range of gastrointestinal tract drugs, catering to various GI disorders. Their product portfolio includes antacids, PPIs, H2 receptor antagonists, prokinetics, antispasmodics, and anti-inflammatory medications, ensuring comprehensive treatment options for healthcare providers.
2. Quality Assurance
Quality is at the heart of Centurion HealthCare’s operations. The company adheres to stringent quality control measures, from raw material sourcing to final product testing, ensuring that every medication meets international standards for safety and efficacy.
3. Research and Development
Centurion HealthCare invests heavily in research and development to stay at the forefront of pharmaceutical innovation. Their R&D team continuously works on developing new formulations and improving existing products to address emerging healthcare needs.
4. Patient-Centric Approach
Understanding that each patient is unique, Centurion HealthCare adopts a patient-centric approach in drug development and supply. Their medications are designed to provide maximum therapeutic benefit with minimal side effects, enhancing patient outcomes and quality of life.
5. Global Reach
As a leading gastrointestinal tract drugs supplier, Centurion HealthCare has a robust distribution network that ensures their products are available not only across India but also in international markets. Their commitment to excellence has earned them a reputation as a reliable partner for healthcare providers worldwide.
6. Affordability
Centurion HealthCare is dedicated to making high-quality medications accessible to all. Their cost-effective solutions, including generic versions of popular GI drugs, help reduce the financial burden on patients while maintaining high standards of care.
Conclusion
Choosing the right gastrointestinal tract drug involves careful consideration of various factors, including accurate diagnosis, mechanism of action, efficacy, safety, patient-specific factors, route of administration, and cost. Centurion HealthCare, as a leading gastrointestinal tract drugs supplier in India, excels in providing high-quality, effective medications that cater to the diverse needs of patients with GI disorders.
With a commitment to quality, innovation, and patient-centric care, Centurion HealthCare stands out in the best pharmaceutical industry in India. Their comprehensive product range, stringent quality assurance, advanced R&D, global reach, and affordability make them a trusted partner for healthcare providers seeking reliable solutions for GI tract disorders.
By choosing Centurion HealthCare, you can be confident in the quality and efficacy of the medications you are prescribing or consuming, ensuring the best possible outcomes for gastrointestinal health.
#Best Indian pharma industry 2024#Best pharmaceutical industry in India#Gastrointestinal tract drugs supplier#Gastrointestinal tract drugs supplier in India
3 notes
·
View notes