#neurocognitive disability
Explore tagged Tumblr posts
Text
this is a cripple punk post [also focusing on all kinds of HSN disabled folks]; ableds must tag reblogs with #i’m able bodied
for the record
i generally shower exactly once a week & wash my hair the same day
sometimes i can’t change undergarments for a few days, sometimes i change them multiple times a day
i rely on several adaptive tools to shower, period
i do need to shave/trim pubic and body hair for my hygiene, and can’t keep clean otherwise
in winter, i often can’t wash my hands unless i have lotion with me or they’ll crack painfully
i change clothes once or twice a day to make up for most of this the best i can
i’m saying this because all of those things are very common issues for many disabled people (especially high-support ones), and because i feel like if i’m going to talk about destigmatizing hygiene struggles, i should at least be open about my own.
hygiene is very difficult and energy consuming. it involves a lot energy that many of us can’t access.
not being able to maintain one’s personal hygiene doesn’t make anyone selfish, disgusting, or undeserving.
if you can’t be kind and supportive and not say “ew” when you hear about one of the most common impairments moderately to severely disabled people experience, you don’t support disabled people. if you don’t support disabled people who smell bad or have dandruff or cracked hands or un-exfoliated skin, you don’t support disabled people.
yes, even if you have sensory issues. yes, even if you’re germaphobic. your disabilities are not an excuse to be ableist to others. find a way to be kind anyway.
#DO NOT TAG AS “C SLUR/TW SLUR” OR “UNHYGIENIC”#use “cw hygiene issues” or don’t reblog. consider how your phrasing impacts those who struggle with their hygiene#cw hygiene issues#hygiene#cripple punk#cpunk#crippunk#cripplepunk#cognitive decline#neurocognitive disability#neurological disability#crazy cripple pride#mad crip pride#mad pride#madpunk#neuropunk#ableism
253 notes
·
View notes
Text
feeding into my curiosity about the demographics of tumblr
*this is a specific category of diagnosis. if you're not sure if your disorder falls under this category then google it. ADHD, intellectual disability, and autism are not neurocognitive disorders- they are neurodevelopmental disabilities.
if you have both intellectual disability and a neurocognitive disorder click the relevant "yes" option
58 notes
·
View notes
Text
Well, I'm in the hospital ER.
I've been experiencing episodes of shaking, muscle spasms/weakness, midnight-awakenings, severe restlessness, fear/panic attacks, HUGE chunks of time-loss (i.e. I look at the clock - 6pm - I do task or just stand/sit for I what I perceive to be 30m, 45m tops - I look at the clock - 9:55pm /also/ I go do task that should take 15m tops - I complete task - it has been 90m), dissociation, pain-flares, urinary incontinence, esophageal spasms, confusion, irritability, visual snow.. the works.
I hope at the very least, this visit contributes to the notes that will help my providers understand what's going on with my brain, long-term.
I knew the trauma would catch up with me.. seems like the repercussions are starting to forge on, full speed ahead...
I pray, all is well, and all manner of thing will be well. I pray for the providers attending to my care, and for the outcomes we receive to be just what we're needing to know. May all be clear, all be gentle, all be swift..
#trauma#hospital.txt#metampsychosis.txt#time loss#dissociation#neurocognitive#neurology#psychiatry#cptsd#neurological disability#emergency room#blackouts#fibromyalgia#chronic illness
4 notes
·
View notes
Text
autistic people dominate AAC conversation on tumblr so for this AAC awareness month (October), let us also remember all non-autistic AAC users & autistic AAC users who not use AAC because or solely because autism.
people use AAC for from intellectual & developmental disorders to neurocognitive disorders to neurological to physical disorders. people use AAC for disorders from birth & acquired disorders. progressive & non progressive disorders.
some AAC users have mouth speech, motor, and/or sound clarity related difficulties, others use for language and/or cogntive difficulties, some for combo of reasons.
those with…
intellectual disability
genetic & chromosomal disorders like down syndrome, rett syndrome, angelman syndrome, williams syndrome, etc.
cerebral palsy
speech language disorders like aphasia & dysarthria
schizophrenia & schizoaffective & schizo-spec
brain injury
dementia
amyotrophic lateral sclerosis (ALS), multiple sclerosis (MS), huntington’s, frederick’s ataxia, etc.
tracheotomy
locked in syndrome
n so much more not listed here
#AAC#AAC user#AAC users#loaf screm#some of these physical so apply to cripplepunk. idk should tag it tho.
2K notes
·
View notes
Note
Hello! Sorry if you’ve posted about this somewhere already/if it’s redundant, but I thought your coinage of “transMad” was very cool and I’m wondering what that term means to you? I’m really happy to see other people talking about madness being intertwined w their gender/transness and looking forward to checking out your reading lists :))
thank you so much for asking about one of my favorite things to infodump about!! rather than rehash a bunch of stuff, if it's okay, I'm going to borrow a few quotes from past!me that i've published in different places // offer you some things of mine to read.
broadly, though, i use transMadness as a way to explore the identificatory, epistemological, methodological, and theoretical implications of an orientation (to use Sara Ahmed's term) toward bodymind noncompliance and self/selves-determination. this orientation refuses to delineate diagnostically between Maddened / transed experiences of the world/our many worlds, and instead takes this shared/overlapping ground as a jumping off point for solidarity and speculation - that is, something that allows us to imagine otherwise worlds / make them manifest through creativity and collaboration.
(Ha, and I claimed i wouldn't talk too much...famous autistic last words)
ANYWAY. here are some clips that might help explain more dimensions of transMadness. note that, in my dissertation-in-progress, i'm focusing on xeno/neogender and/as self-diagnostic cultures among queercrip and transMad internet users. i'm interested in the anti-psych liberatory potential of this digital community work, especially as it centers forms of knowledge and scholarship devalued within Academia Proper, especially because so much of it is made by and for disabled, Mad, queer, trans people, esp. youth. Onward to quotes!
On transMad epistemologies: citation/power/knowledge:
I’ll spend most of this piece looking not at what transMad is, but what it does. First and foremost, transMad cites. Even its name alludes to other portmanteaus: neuroqueer and queercrip being the best-known among them. Many people have offered many different (ever-“working”!) definitions of these terms; today, I offer co-coiner Nick Walker’s (2021) definition of neuroqueer: a verb and an adjective “encompass[ing] the queering of neurocognitive norms as well as gender norms” (p. 196). In terms of queercrip, I also return to its coiner, Carrie Sandahl (2003), who for whom the queercrip (as person and as method/movement) confuses the diagnostic gaze, bears sociopolitical witness, and performs glitchful[4], incongruous, confusing in(ter)ventions into possible community. At base, “queer” and “crip” appear as analogous, reclaimed slurs signifying marginalized transgression. When combined, they describe a loop, perhaps a Möbius strip: crip (ani)mates queer, queer tells-on crip. The specter of crip haunts queer—and even more explicitly, as we will see, trans—and the crip(ped) bodymind holds, moves, and fucks queerly. Who knows where “queer” stops and “crip” and “neuro” begin? Likewise, transMad, whose citational style leaves little room for diagnostic clarity amidst a pastiche of noncompliant text.
On transMad epistemologies: multiplicity (h/t @materialisnt):
They encourage us to remove others’ names from our bodies, to reign in unruly citations, to set “boundaries” which violate Mad, crip ethics of care (see Fletcher, 2019). In truth, any framing of individual authorship in which the body text is “mine” and the citations gesture “elsewhere” belie the inherent interdependence of all intellectual life, and particularly of transMad intellectual life. transMad plural scholar mix. alan moss (2022) argues in relation to the pathologization of multiple systems: “all people, indeed all that exists, is a system that itself is constantly enmeshed in several overlapping and interconnected systems.” In short, I am full of Is, and will continue as many more. Just as disability justice helps us understand all life as interdependent and deserving of access, a transMad approach sees our selves as numerous and fuzzy. We have permission to dispense with the need for tidy texts, with our interlocutors, edits, and iterations either obfuscated entirely or exclusively relegated to a bibliography. transMad citation may thus be considered akin to visible mending[6], creating flamboyantly messy, multiplicitous work that does not seek to pass as objective or discrete.
On the value of (crip) failure and/as "virtuality":
Don’t get me wrong: Zoom PhD work is a failing enterprise. That is to say, it is a queercrip, transMad enterprise, which is to say, it is a beautiful, beautiful project. Mitchell, Snyder, and Ware describe such “fortunate failures” in the context of “curricular cripistemologies.”5 Coined by Merri Lisa Johnson, the term “cripistemologies,” refers to “embodied ways of knowing in relation, knowing-with, knowing-alongside, knowing-across-difference, and unknowing,” ways which frequently exist outside the purview of mainstream academia.6 Curricular cripistemologies, then, refer to an intentional, queercrip deviation from normative pedagogical approaches which trades the corrective impulse of “special ed” and other rehabilitative programs, and offers instead a generative noncompliance.7 That is, rather than trying to identify, isolate, and ameliorate difference, curricular cripistemologies lean into difference as it is experienced by disabled students ourselves, querying how atmospheres of in/accessibility shape normative approaches to education and how the embrace of “failure,” not as a last-resort but as a first choice, poses potentially transformative possibilities.
On transMadness and fat liberation: (for @trans-axolotl's Psych Survivor Zine)
A transMad, fat approach to disorderly eating requires making connections with humility and understanding, and, as I discussed above, engaging in compassionate, critical interrogation of our own anti-fatness.
[...]
A transMad, fat, abolitionist politic is one that makes room. We imagine beyond the cage, even if the details of that imagining are not yet clear. Just as we have carved micro-sites of support within violent digital and in-person contexts, just as we have learned to think about our lifeworlds beyond the paradigm of “recovery or death,” we can also reconceptualize fatness not as the enemy, but as another form of bodymind noncompliance in alliance and/or entanglement with disorderly eating practices. For thin disorderly eaters, this requires us to fundamentally challenge the way we view food and embodiment, even while maintaining a Mad respect for alternative ways of approaching reality.
On xenogenders, virtuality, and self-determination:
It is this very “irrationality” –– the “unrealness,” the “you’ve-got-to-be-kiddinghood,” that is most frequently weaponized against xenogenders, as well as their newly-coined sets of xenopronouns. The perceived and actual virtuality of xenogenders is often placed against the notion of “actuality,” in this case, of “real” (or “practical”) genders and pronouns to be used in one’s “real life.” Disabled activists have rightly resisted the distinction between online and (presumed-offline) “real life,” given that this categorically excludes homebound bodyminds, as well as those without IRL social and support circles. That said, I believe the virtual –– as almost, not-quite, proximite, making-do –– is incredibly useful in thinking about xenoidentities as transMad tools –– particularly, as transMad tools of underground collaboration / co-liberation.
[...]
What if gender was a project we wanted to fail? That is, what if trans- was a process not of getting better, not of moving-toward a bodymind more sane, more straight, and more cisheteropatriarchially desirable, but rather a line of flight on a longer trail to illegibility? Indeed, what if we replaced pathology’s narrow “path” with a trail lighted by the language of our comrades, whose linguistic interventions make and break gender in ways heretofore unimaginable? Xenoidentities, both individually and as a trans-gressive M.O., are fundamental to a broader transMad project of crafted, collective illegibility; intersubjective citation (imagine what it feels like for someone to be the gender that you coined!); and collective care that refuses a politics of cure. Crucially both virtual and digital, xenoidentities are furthermore a manifestation of the power of trans, predominantly disabled digital counterpublics, who overturn the hierarchy which places the IRL-real above the digital-unreal, making unruly, Mad space in which (with apologies to Donna Haraway) a hundred xenoselves might bloom.
On Maddening queer "diagnosis":
In her indictment of all “Kwik-Fix Drugs,” Gray further indicates the practice of forced treatment as in and of itself as a project of violent normalization, regardless of specific target or reason. The intentional ambiguity between her narrative of Madness and her narrative of asexuality disrupt mounting demands for a healthy (sanitized, neoliberal, and consumable) queerness. A Mad ace approach identifies these demands as, indeed, comparable with cis heteronormative notions of sexual maturity and responsibility – the idea that participation in culturally-normative sexual practices is a prerequisite for health (Kim, 2011, 481) and thus, personal autonomy (Meerai, Abdillahi, and Poole 2016, 21). By fusing the “lack of sexual appetite” attributed to her medications for bipolar disorder with her asexuality, Gray destabilizes the binary between healthy-sexual-diversity and unhealthy-psychopathology. She is once again disrupting contemporary queer impulses to dissociate from ongoing histories of pathologization. Here, Mad and queer/asexual activism are as inseparable in text as they are in Gray. Gray and her comrades collectively refuse both sexuality-as-“rehabilitation” (See Kim 2011, 486) and asexual acceptance predicated upon normative “health” (Kim 2010, 158) – that is, they Madden asexuality. Twoey, in her own voice, remixes the sources of her own pathologization, staggering the supposedly-divine pronouncement of the DSM across pages and bookending its extracts with her own writing and art. In this undermining of the DSM’s epistemological polish, Gray disrupts the domination of written prose over poetry and visual art, while also critiquing the role of the DSM in commercialized health “care.” Her zine opens with the lines “sex sells and sex is sold / sex was being sold and i didn’t buy” (Gray 2018, n.p.). Gray indicates a pathology perceived not only in a refusal to practice sex, but also in a refusal to buy (into) it. After all, a refusal to buy into existing sexual paradigms is for her also a refusal to buy into a feminized reproductive mandate.
94 notes
·
View notes
Text
How Common is Neurodivergence?

[image id: poster of "How Common is Neurodivergence?.” There are 12 circles and five small images: an image of a brain, speech bubbles, an infinity sign, a person reading, and a person surrounded by arrows and balls. Each of the 12 circles has a percentage representing how common a particular form of neurodivergence is written in Open Dyslexic font. Full transcript, more information, and references under the cut.]
More Information
Forms of neurodivergence represented here are focused on neurodevelopmental disorders.
These percentages are representative of percentage in general population and do not reflect percentages within neurotypes which are often higher due to co-occurrence being the norm, rather than the exception, within neurodevelopmental disorders; for example, 33-45% of people with ADHD will also have dyslexia (Butterworth & Kovas, 2013), whereas only 10% of the general population are dyslexic (British Dyslexia Association [BDA], 2023).
Certain neurodivergencies are often underrepresented and under-reported, so the percentages are likely to be higher; for example, one study suggests that rates for FASD in the UK may be as high as 17% (McQuire et al., 2019).
Some of the neurodivergencies represented here are umbrella terms and percentages given are representative of all forms of neurodiversity belonging to that term; for example, SpLds include dyslexia which is at a rate of 10% (BDA, 2023) and dyscalculia which is at 3-7% (Haberstroh & Schulte-Körne., 2019). Tic Disorders at 1% are another example here, as this is inclusive of Tourette Syndrome which is at 0.6%, and around 1 in 5 individuals exhibit tics at some point during childhood (Cavanna et al., 2017).
______________
Transcript in Full
1% Intellectual Disability
10% Language Disorder
4% Speech Sound Disorder
5% Stuttering
7.5% Social (Pragmatic) Communication Disorder
1.7% Autism
5% ADHD
10% Specific Learning Disorder (SpLD)
5% Developmental Co-Ordination Disorder (DCD)
3-4% Stereotypic Movement Disorder
1% Tic Disorders
3.6% Fetal Alcohol Spectrum Disorders (FASD)
______________
Sources
American Psychiatric Association. (2022). Diagnostic and Statistical Manual of Mental Disorders (5th Ed., Text Rev.).
Arvidsson, O., Gillberg, C., Lichtenstein, P., & Lundström, S. (2018). Secular changes in the symptom level of clinically diagnosed autism. Journal of Child Psychology and Psychiatry, 59(7), 744–751.
Attention-deficit/hyperactivity disorder (ADHD). PsychDB. (2022, November 29).
Autism spectrum disorder (ASD). PsychDB. (2022, May 19).
Butterworth, B., & Kovas, Y. (2013). Understanding neurocognitive developmental disorders can improve education for all. Science, 340(6130), 300–305.
Cavanna, A. E., Coffman, K.A., Cowley, H., Fahn, S., Franklin, M. E., Gilbert, D.L., Hershey, T.G., Jankovic, J., Jones, M., Leckman, J.F., Lehman, R., Mathews, C.A., Malaty, I., McNaught, K., Mink, J.W., Okun, M.S., Rowe, J.A., Scahill, L.D., Scharf, J.M., Schlaggar, B.L., Stewart, E., Walkup, J.T., Woods, D.W.. (2017). The spectrum of Tourette Syndrome and TIC disorders: A consensus by Scientific Advisors of the Tourette Association of America. Tourette Association of America.
British Dyslexia Association. (2023). Dyslexia. British Dyslexia Association.
Dyspraxia at a glance. Dyspraxia Foundation. (2023).
Haberstroh, S., & Schulte-Körne, G. (2019). The Diagnosis and Treatment of Dyscalculia. Deutsches Arzteblatt International, 116(7), 107–114.
Ketelaars, M. P., Cuperus, J. M., van Daal, J., Jansonius, K., & Verhoeven, L. (2009). Screening for pragmatic language impairment: The potential of the Children’s Communication Checklist. Research in Developmental Disabilities, 30(5), 952–960.
May, P. A., Baete, A., Russo, J., Elliott, A. J., Blankenship, J., Kalberg, W. O., Buckley, D., Brooks, M., Hasken, J., Abdul-Rahman, O., Adam, M. P., Robinson, L. K., Manning, M., & Hoyme, H. E. (2014). Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics, 134(5), 855–866.
McQuire, C., Mukherjee, R., Hurt, L., Higgins, A., Greene, G., Farewell, D., Kemp, A., & Paranjothy, S. (2019). Screening prevalence of fetal alcohol spectrum disorders in a region of the United Kingdom: A population-based birth-cohort study. Preventive Medicine, 118, 344–351.
Norbury, C. F., Gooch, D., Wray, C., Baird, G., Charman, T., Simonoff, E., Vamvakas, G., & Pickles, A. (2016). The impact of nonverbal ability on prevalence and clinical presentation of language disorder: Evidence from a population study. Journal of Child Psychology and Psychiatry, 57(11), 1247–1257.
Polanczyk, G. V., Willcutt, E. G., Salum, G. A., Kieling, C., & Rohde, L. A. (2014). ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. International Journal of Epidemiology, 43(2), 434–442.
Polanczyk, G., de Lima, M. S., Horta, B. L., Biederman, J., & Rohde, L. A. (2007). The worldwide prevalence of ADHD: A systematic review and metaregression analysis. American Journal of Psychiatry, 164(6), 942–948.
Prevalence and Therapy Rates for Stuttering, Cluttering, and Developmental Disorders of Speech and Language: Evaluation of German Health Insurance Data. (2021). Frontiers in Human Neuroscience, 15(645292), 1–13.
Social (pragmatic) communication disorder. PsychDB. (2021, March 29).
Stereotypic movement disorder. United Brain Association. (2022, August 8).
Wren, Y., Miller, L. L., Peters, T. J., Emond, A., & Roulstone, S. (2016). Prevalence and predictors of persistent speech sound disorder at eight years old: Findings from a population cohort study. Journal of Speech, Language, and Hearing Research, 59(4), 647–673.
UCL. (2013, April 19). Learning disabilities affect up to 10 per cent of children. UCL News.
#neurodiversity#neurodiverse stuff#neurodivergent#neurodivergence#actually autistic#actually audhd#autism#audhd#adhd#dyspraxia#disability#disabilties#neurodevelopmental#intellectual disability#communication disorder#stuttering#asd#motor disorders#dcd#actually dyspraxic#dyspraxic#tics#tourettes#splds#dyslexia#dyscalculia#dysgraphia#fasd
363 notes
·
View notes
Note
Can u pls explain why moving back means you are no longer housebound thank u
Inaccessible environment and hostile architecture are capable of worsening different aspects of disability, as well as making it hard to reliably go in and out of a space on their own or with just the available help they have. Negative feedback loop.
The usual example is wheelchair users living in an apartment without wheelchair ramps, no working elevators, with heavy door difficult to open in wheelchair, on an upper floor, and so on.
In our case, it was a combination of physical, mobility, mental, and neurocognitive disability issues.
At the moment, going back to birth home has familiar pathways that include parts with less effort. Though can't say they're truly "accessible", they're just less "inaccessible" and is a house with a different layout.
So can at least briefly go out much further than otherwise could have.
Though, not enough to get out consistently nor do socialization + appointments on own that way - just enough to not be on the same disabling level of before.
enough to decide it doesn't fit our internal definition of "housebound" at least. By other people's definitions maybe, we'd still fit that but am unsure.
Is enough to be more manageable for our neurocognitive issues as well, without as much risk losing it forgetting where we are and what we were doing while not being far from "home", for example. Amongst other things.
Pros and cons.
16 notes
·
View notes
Text
Also preserved on our archive
By Tarun Sai Lomte
New research reveals how lingering viral activity and immune disruption contribute to long COVID, highlighting novel therapeutic strategies that could change the course of treatment for millions.

A recent study published in the journal Cell reviewed the current state of knowledge on the pathophysiology and biology of long COVID.
Coronavirus disease 2019 (COVID-19) can affect health over the long term. Although it is self-limited in most individuals, some infected individuals experience post-acute sequelae, including fatigue, cognitive dysfunction, and muscle weakness, among others. While more common after severe COVID-19, individuals with a history of mild or moderate severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection have the highest burden.
The World Health Organization (WHO) defines post-COVID-19 condition as unexplained symptoms persisting ≥ two months that manifest ≥ three months after SARS-CoV-2 infection. Further, while many countries have adopted this definition, several have formulated their own definitions. The patient community that first identified the condition prefers the term long COVID.
Overall, the definitions vary in the time scale on which the condition is defined and whether the condition is restricted to unexplained patient-reported symptoms or inclusive of incident medical diagnoses/laboratory abnormalities. The present study reviewed the epidemiology of long COVID, with emphasis on how the underlying mechanisms explain the physiology. Additionally, the study highlights how symptom clusters, identified through techniques like cluster analysis in electronic health records (EHR), could improve long COVID diagnosis by linking specific biological drivers to clinical endotypes.
Epidemiology and clinical features of long COVID There are variations in epidemiological estimates of long COVID across variants, populations, and regions. Some studies suggest a prevalence of 30% or higher but define the syndrome as new unexplained symptoms, which might lead to misclassification. Not all symptoms may be related to SARS-CoV-2; as such, other conditions must be ruled out. Determining what is new after infection and what might be unmasking of sub- or pre-clinical conditions is a significant challenge.
Further, SARS-CoV-2 is not the only virus associated with protracted symptoms. Studies have estimated that 18 million adults in the United States (US) might suffer from long COVID. The WHO and the Institute for Health Metrics and Evaluation estimated that one in 30 European individuals had long COVID in the first three years of the COVID-19 pandemic. Globally, an estimated 65 million individuals have long COVID.
Notably, the epidemiology of severe, disabling long COVID-19 is unknown. Long COVID can manifest during or weeks after the acute infection. Cognitive problems, fatigue, and post-exertional symptoms are the most common. In addition, symptom clustering based on organ systems, such as autonomic dysfunction, neurocognitive impairment, and exercise intolerance, offers a more precise understanding of long COVID phenotypes. Further, many symptoms of long COVID overlap with those of other infection-associated chronic conditions (IACCs), such as chronic Lyme disease, post-Ebola disease, post-Giardiasis, and myalgic encephalitis/chronic fatigue syndrome, among others.
Biological drivers of long COVID The biological drivers of long COVID are upstream processes, such as perturbations of the coagulation system and immunity, which do not directly cause disease but instead drive one another, leading to downstream physiological changes that manifest as symptoms. Some of these biological processes, like clotting and immune dysfunction, may interact, creating a cycle of chronic inflammation and tissue damage. Microclots, resistant to fibrinolysis, have been detected in long COVID patients and may contribute to tissue hypoxia and organ dysfunction. There are also associations between viral activity levels during infection and long COVID risk, with higher viral replication linked to more severe illness.
Long COVID risk appears to be lower with Omicron variants. The protective effect of antiviral therapy and vaccination suggests that viral replication and transmission during the acute phase is a significant determinant of long-term outcomes. Therefore, early COVID-19 interventions could mitigate long COVID and support pursuing robust preventive agenda.
Early in the pandemic, it was commonly assumed that SARS-CoV-2 infection would be transient; however, this was challenged by reports that viral proteins and nucleic acids could be detected months after infection. Although the precise anatomic site of viral persistence is unclear, there is consensus that persistence is tissue-backed. Various studies have linked immune dysfunction and inflammation with long COVID.
Many studies have focused on the role of inflammatory macrophages and monocytes in long COVID. Mast cell activation might also contribute to long COVID. Although not infected by SARS-CoV-2, external triggers can activate mast cells. Severe COVID-19 is also associated with autoimmunity. COVID-19 is also associated with a higher incidence of autoimmune conditions, such as lupus, Sjogren’s syndrome, inflammatory bowel disease, and rheumatoid arthritis.
Acute SARS-CoV-2 infection can lead to a hypercoagulable state and elevate the risk of thromboembolic events. Interactions between the spike protein and fibrinogen may result in abnormal clots that can trigger microglia activation in the brain, potentially contributing to neurocognitive symptoms of long COVID. Clotting has been implicated as a long COVID mechanism, with aggregates of platelets and clotting proteins detected in affected individuals.
Clinical physiology of long COVID The most efficient explanation for long COVID is tissue damage mediated by SARS-CoV-2 that was initiated during (initial) infection. Pancreatic infection by SARS-CoV-2 has been implicated in post-COVID-19 diabetes, another form of the post-acute sequelae, offering proof of principle. Endothelial dysfunction has been suggested to be involved in long COVID.
Various mechanisms might lead to endothelitis and macrovascular diseases, and their end-organ consequences could result in long COVID. Additionally, the study suggests that microclots and endothelial dysfunction could impair tissue perfusion, leading to organ damage and contributing to persistent symptoms such as fatigue and cognitive issues. Disruption of the gut-brain axis enables a direct connection between post-COVID-19 processes and disruption of normal physiology, including brain fog, autonomic dysfunction, and abnormal stress responses.
Brain fog, i.e., problems with memory, concentration, and attention, is among the most debilitating manifestations of long COVID. It has been a prominent symptom among non-hospitalized patients since the early pandemic. Some people, especially those with diabetes, learning and attention disorders, and substance, have a predisposition for developing brain fog. Individuals with brain fog are more likely to have abnormal cerebrospinal fluid measures.
Concluding remarks The COVID-19 pandemic has been described as a once-in-a-century challenge, with long COVID representing a challenge of similar scale. Although long COVID is not the first known IACC, it is the first time that such a condition has manifested in a substantially large number of people following a shared, known exposure. Emerging therapies, including antivirals like nirmatrelvir/ritonavir and immunomodulators targeting inflammatory pathways, are currently being explored in clinical trials as potential treatments for long COVID. As such, there is an urgent need for all types of research (basic, epidemiological, translational, and clinical and implementation sciences) into the natural history, biology, and treatment for long COVID.
Journal reference: Peluso MJ, Deeks SG. Mechanisms of long COVID and the path toward therapeutics. Cell, 2024, DOI: 10.1016/j.cell.2024.07.054, www.sciencedirect.com/science/article/pii/S0092867424008869
#long covid#covid conscious#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#still coviding#sars cov 2#wear a respirator#covid is airborne
5 notes
·
View notes
Text
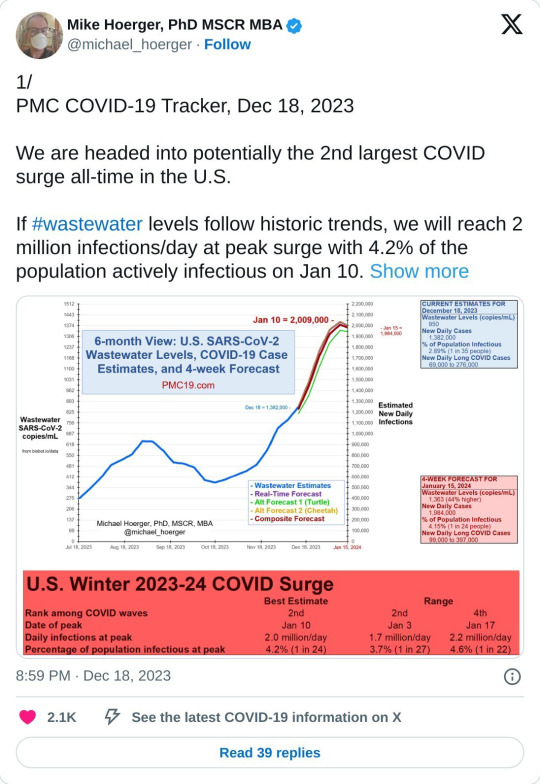
COVID-19
We are currently in the largest COVID surge of all-time in the US.
There is also a new variant that is not protected by the previous vaccine.
Please start back masking and please get the COVID-19 booster (schedule with your local pharmacy).
Wastewater counts are obscenely high right now, belying the official case numbers. Considering that we've stopped collecting or reporting most COVID data, wastewater is the best way we have to judge the actual infection rate now. Wastewater is collected from washing our hands, going the bathroom, etc. We shed COVID into the water system and based on the concentration of COVID in waste water, we can get very accurate estimates of how many people are infected at one time.
We are currently seeing ten million new infections a week, and can expect that to greatly increase within the next three weeks.
* If you've stopped masking, please start again, for your own safety and the safety of your community. Many hospital systems are already trending toward being overwhelmed right now; wear a mask when in crowded, enclosed, or poorly ventilated areas, and keep a safe distance from others, as feasible.
* Avoid unnecessary gatherings where possible.
* Ventilate your spaces well (Corsi-Rosenthal Box).
* Reevaluate casual habits (touching face, respiratory etiquette—covering coughs and sneezes, clean your hands regularly, stay home if you are sick, get tested if you have symptoms, or if you might have been exposed to someone with COVID-19 or influenza)
Please be aware of Long Covid.
COVID impacts the immune system similar to HIV in that it hides in the body and continues to wreak havoc in the various organ system by driving inflammation and disrupting the immune response. It causes neurological, vascular, and immune dysfunction.
Patients with long COVID generally have symptoms that fall into three categories or phenotypes: fatigue, neurocognitive symptoms such as brain fog or headaches, and cardiovascular symptoms such as shortness of breath, heart arrythmias, exercise intolerance, and blood clots. Patients may have more than one type, and some also have symptoms like constipation, diarrhea, or loss of taste and smell that don’t seem to fit neatly into one of the three groups.
This is a period where we need to act with more care. Not a time to panic, but a time to be more cautious.
If you contract COVID, these are some helpful things that work to reduce viral load in the hope of minimising symptoms. And your chance of developing Long Covid:
* Brush & floss as usual
* Mouthwash (CPC (cetylpyridinium chloride, an ingredient in many/most commercial mouthwashes), cooled green tea, salt water)
* Green Tea (drink on an empty stomach if possible; can also be used for swishing/gargling once it has cooled; if green tea isn't doable for you, black tea is an alternative)
* Nasal Spray (if chemicals in nasal spray causing an issue for you, saline nasal spray also an option)
* Vitamin C supplement
* Antihistamines
* Other prophylactics to consider: Nattokinase, Grape Seed Extract, EGCG supplements
* Natto (if this is something you already eat, or would like to try. It's fermented soya beans and is popular in Japan
* Mask & Vaccinate!! A fully vaccinated individual is five times less likely to continue to have any symptoms or ill-effects three months after their initial infection compared to someone who has not been vaccinated.
Not a medical professional but compiled resources from medical professionals and individuals with disabilities including long COVID.
Free Palestine. Free Congo. Free Sudan. Free Tigray. Stop Cop City. Eyes on the Mass Graves in Jackson.
Please SHARE & Please participate in the Global Strike for Palestine 1.21-1.28.
#covid#covid19#long covid#covid isn't over#covid 19#coronavirus#corona#free palestine#free gaza#free congo#free sudan#freepalastine🇵🇸#freedom#black liberation#israel is committing genocide#israel is a terrorist state#end occupation#human rights#hawai'i#land back#decolonization#nakba#jason todd x reader#free tigray#stopcopcity#copcity#congo genocide#save congo#mass graves in jackson#jackson mississippi
14 notes
·
View notes
Text
Charlie Kelly and Fetal Alcohol Spectrum Disorder: Part One
What is Fetal Alcohol Spectrum Disorder (FASD) and how does it apply to Charlie Kelly? Fetal Alcohol Spectrum Disorders are a group of complex conditions that occur in people who were exposed to alcohol before birth. People with FASD may have distinct physical features as well as neurological differences that impact their behavior. Charlie Kelly meets criteria for having a Fetal Alcohol Spectrum Disorder based on his observable behavior and family history. There are several different conditions grouped under FASD, and the terminology is kind of a mess. The type of FASD Charlie has can be called Alcohol-Related Neurodevelopmental Disorder, Neurodevelopmental Disorder Associated with Prenatal Alcohol Exposure, Other Specified Neurodevelopmental Disorder, Fetal Alcohol Effects, or simply FASD. Charlie does not meet the criteria for Fetal Alcohol Syndrome, because you need specific physical features to be diagnosed with that one. For the purposes of this post series, I've used the DSM 5-TR provisional criteria for Neurodevelopmental Disorder Associated with Prenatal Alcohol Exposure, plus some supplemental notes. Fulfillment of this criteria would qualify him for a diagnosis of FASD. Criterion A. More than minimal exposure to alcohol during gestation, including prior to pregnancy recognition. We know that Mrs. Kelly is an alcoholic, and that she tried to get an abortion, but it "didn't take." It's highly likely that she drank while pregnant, knowingly or unknowingly, based on her medical history and Charlie's behavior patterns.
Criterion B3. Impaired neurocognitive functioning as manifested by impairment in learning: Charlie has two learning disabilities: dyslexia and dysgraphia. He really, really struggles to read. Dennis actually names the dyslexia in "The Gang Runs for Office." He also struggles with writing. Words are often out of order or missing altogether. Words that aren't spelled exactly the way they're pronounced are usually misspelled. He needs help to write something intelligible. The picture language he has is actually a great example of him trying to adapt. The issue is obviously not a lack of effort. B5. Impaired neurocognitive functioning as manifested by impairment in visual-spatial reasoning: Charlie struggles with telling left from right, as seen in "A Very Sunny Christmas." He also can't use a map, as seen in "The Gang Goes to a Waterpark." I also suspect that visual-spatial difficulties are part of the reason Charlie stops driving after season 3. We can see in "The Maureen Ponderosa Wedding Massacre" that he doesn't know how to avoid obstacles or operate a car when stressed, which would make driving difficult and unsafe. See here for part two, which contains the remainder of the criteria and the supplemental notes.
29 notes
·
View notes
Text
this is a cripple punk post [even if it also applies to nonphysical disability]; ableds must tag reblogs with #i’m able bodied
actually tagging my last post reminded me--
if you're making a post about a disability you don't have, for fucks sake, please make or use a modified tag that IS NOT a community tag.
i get that you want to sort topics and make them easier to find on your blog or whatever, but if you misuse tags you are actively making it harder for people to find community.
avoid using just an asterisk or backslash or similar to modify the tag--these tags are usually even more explicitly for the community than the disability's unmodified tag is.
my personal go-to is 're: x', like, 're: intellectual disability', and i think ive seen 'includes: x' for fiction stuff. basically anything works if it's not used by the community. for some disabilities, you're fine just using the name of the disability as a tag, but for many, the name of the disability is the community tag. this is especially common, in my experience, with disabilities that affect cognitive/intellectual/neurological functioning. please err on the side of caution.
please, please, i am literally begging you, let disabled people have our spaces. a huge part of why i made this blog is that the tags relevant to my main disabilities are totally overrun by nondisabled people and "allies." it fucking sucks and does massive damage to disabled people--and i mean that very literally.
#cripple punk#cpunk#crip punk#crippunk#cripplepunk#neurological disability#neurocognitive disability#cognitive decline#nt sci#physical disability#disabled#ableism#anticrip ableism#mad pride#madpunk#neuropunk#actually disabled
30 notes
·
View notes
Text
BULIMIA: ONE DAY WITHOUT SUPPORT (BREATH OF LIFE)
MAJOR NEUROCOGNITIVE DISORDER: NO HOPE
PTSD: AFRAID OF THE ONE PARENT WHO DAMAGED YOUR CHILDHOOD NOW ESTRANGED TO SOCIAL CUSTOMS DUE TO TRAUMATIC EXPERIENCE WITH RELIGION
COMPLEX SOMATIC SYMPTOM DISORDER REVISED: NO WORLD TO BELONG IN TRUTHFULLY (ONE PERSON IN THEIR LIFE REMAINED STAGNANT TO THAT THOUGHT IS THE REASON (RELATIVE ASSOCIATION TO GUILT BREAK)
HOARDING DISORDER: BODY SLOWS DOWN TO RESERVE ENERGY FOR THE WORLD BECOME BY IMAGINATION-FACTUAL REALITY BECAME (5 YEAR MELTDOWN)
BIPOLAR I DISORDER: FIGURE OF SPEECH (HEAVILY HELPS THE NEUROTYPICAL IN THE LONG RUN)
BINGE-EATING DISORDER: DISORDERED FAMILY FOR THE BENEFIT OF THE WEALTHY BECAUSE TOXICITY STAYS THAT WAY FOR THE COURSE OF THEIR BRATTY ATTITUDE TO LIFE
BORDERLINE PERSONALITY DISORDER: RAGE INSPIRED INTUITION (REWARD GETS THE BABY SOMEWHERE FOR THE COURSE OF THE FATHERS LIFE LIVED FOR HER TO LIVE ON BECOMES NARRATIVE ON TV LORE MUCH LATER (APPROX. 25 YEARS) TO ENSURE REWARD ECONOMY STAYS NEUTRAL FOR THE BABY (VICTIM) SUPRISE FOR THE ADVENTURE COMING HER WAY FOR THE TRUTH OF THE UNIVERSE BY AN ANIMATED EVENT COMING ON TOO STRONG
SCHIZOAFFECTIVE: NUMBNESS BY LOVE ITSELF REALISED ONLY THROUGH INTIMACY
MILD NEUROCOGNITIVE DISORDER: DEREALISATION OF THE WORLD BECOME BY SOCIAL STIGMA BEING PURIFIED FOR THE HOMBODY STATUS OF A MUSLIM CROWN TAKEN OVER BY CHANCE THOUGHT PER CAUSE (LIFE IS GREAT AGAIN)
SCHIZOPHRENIA: INTUITION BROKE TO A LOST CAUSE FOR CONCERN MAKING A CIVILISATION PREPARED TO FIGHT ON THE BABY'S (VICTIM'S) BEHALF AFTER FATHER NOTICES IT BY ALGORITHM
ATTENUATED PSYCHOTIC SYMPTOMS SYNDROME: BURDENED PAST REALISED BY VIBRATIONAL ALGORITHM TO BE MADE OF THE WORLD BY ACUTE ATTENTION BY A CIVILISATION THEN BEFORE TIME REDUCED TO ATOMIC PRESSURE OF 'LOOKING FOR LOVE' ANNOUNCED AS FLAT LINE
MILD NEUROCOGNITIVE DISORDER: NO WAY OF THINKING OUT LOUD EXCEPT TALKING.
ALCOHOL USE DISORDER: TONGUE OF THAT USE (NT) IS PHYSICALLY DISABLED BY THE WONDER OF USE (INSPIRED INTENTION) THAN OF THE SOCIAL ANATOMY OF THE USE (REASONABLY THE LANGUAGE ITSELF IS IN THE FORM OF THEIR OCCUPTATION THAN IT IS NORMALLY USED TO JUDGE INTELLIGENCE (PHYSICAL DISABLED)
BIPOLAR II DISORDER: -SPAT IS RIGHT THERE: CAUSE OF THE SOCIAL CONCERN IS NOT PRESENT WITHIN THE PROLIFIC BRAT ON TV OVER A MAN SITUATION WITH A HIDDEN SEXUAL AGENDA-
MILD TRAUMATIC BRAIN INJURY (TBI): MAP IS NOT PHYSICALLY THERE BECAUSE OF THE BRAT SLUT-SHAMING HERSELF ON TV FOR VALUE ELSEWHERE (HIDDEN OCCUPATION UNVEILED BY LAW NOW AS OF SAID. (THERAPIST APPROVED)
OC PERSONALITY DISORDER: BODY PHYSICALLY ACHING WITHOUT SEXUAL REDEMANCY
MAJOR DEPRESSIVE DISORDER: ORDER IS ACTUALLY AGAINST TIME AND SPACE TO FIGURE A BRAT OUT (ON ANIMATED TV)
ANTI-SOCIAL PERSONALITY DISORDER: GUT ACHING FOR FOOD
GENERALISED ANXIETY DISORDER: SURVIVAL INSTINCTS KICK IN A LOT WITHOUT THEIR PARTNER AROUND IN REAL TIME
MIXED ANXIETY-DEPRESSIVE DISORDER: NO WAY AROUND LIFE EXCEPT A WOMAN WITH NO HEART TO BELIEVE IN HER TO APPROVE HER BODY AUTONOMY AS HER (SEXUAL EVIDENCE)
BULIMIA: PSYCHOLOGICAL DAMAGE WITHIN FAME (MORMONISM)
MAJOR NEUROCOGNITIVE DISORDER: COMMON SENSE LEAVES YOU
PTSD: LOSS OF FAMILY ON THE WAY (WHO TOLD YOU THEY WERE RIGHT OVER 'A' AND IS WHY YOU WENT IN THE SHAMS AL-MA'ARAF)
COMPLEX SOMATIC SYMPTOM DISORDER REVISED: MARRIED TO THE PLOT-LINE (TOXICITY IS NORMALISED IN EVERY GOOD HOME BECOME A GENIUS TO FIGURE THEM OUT SEXUALLY)
HOARDING DISORDER: IGNORANCE CLAIMS THEM IN PERSON TIL A LANGUAGE BARRIER BREAKS IN AN ALTERNATE UNIVERSE DECLARING WAR ON COMMON BIAS (BORDERLANDS)
BIPOLAR I DISORDER: INTELLECT IS IN THE FORM OF THE WORKING DEPRAVED CLASSES AGAINST THEIR HYPOCRISY
BINGE-EATING DISORDER: NO PEACE FOUND WITHIN. TRUTHFULLY
BORDERLINE PERSONALITY DISORDER: BODY IS NOT THEIR OWN ANYMORE (SOLD AS A SEX SLAVE)
SCHIZOAFFECTIVE: HUSBAND RITUAL NOT PRONONCE TIL DEATH OFFENDS THEM BY CULTURAL APPROPRIATION
MILD NEUROCOGNITIVE DISORDER: BRAIN DAMAGE IN THE FORM OF A TV GUT LIFESTYLE (THEY SEE THEMSELVES AS FOOD)
SCHIZOPHRENIA: CAMERA HUNGRY LIKE AFRICA IS IN THE FORM OF ATTENTION TO THEM
ATTENUATED PSYCHOTIC SYMPTOMS SYNDROME: THOUGHTS COME IN THE FORM OF SOCIAL DISTRAUGHT (TIMES END)
MILD NEUROCOGNITIVE DISORDER: PARYLLISED EFFECT ON THOUGHT IS WHY THEY'RE THE ONES ON SURVIVAL MODE WITH THE REASON OBJECT BY CLARITY (WORLD HUNGER CANNOT EVER BE CURED EXCEPT A.. (CAUSE)
ALCOHOL USE DISORDER: RISK DISORDER MAKING THEM OBSOLETE ELSEWHERE
BIPOLAR II DISORDER: ATTENTION TURNS TO ANGER
MILD TRAUMATIC BRAIN INJURY (TBI): EMOTIONS ARE BOUGHT FOR.
OC PERSONALITY DISORDER: MUSLIM SCENARIOS TAKE PLACE TO EASE THE VIEWER BUT IT WILL NEVER TAKE PLACE UNTIL AFTER A THOUGHT MADE A GENIUS IN THE HOUSEHOLD FOR MORE LEVERAGE OPPORTUNITY WHICH FAILS IN DnD LATER ON
MAJOR DEPRESSIVE DISORDER: SEVERE ISSUES ABOUT REAL-LIFE OFF STAGE THOUGHTS ABOUT A DEATH SCENARIO STRONGLY PROHIBITS THEIR WORLDLY CULTURE
ANTI-SOCIAL PERSONALITY DISORDER: NO PERSONAL LIFE WITHIN A PERSONAL LIFE (SECRETS)
GENERALISED ANXIETY DISORDER: SOCIAL ON-SOUGHT OF BIASED THINKING COMES IN THE FORM OF ANGER IN FOOD WHICH IS WHY THEY EAT WHAT THEY EAT
MIXED ANXIETY-DEPRESSIVE DISORDER: NO SHAME INSIDE THEM WHATSOVER TIL A TV NARRATIVE CALLS THEM OUT FOR IT BY FACTUAL EVIDENCE OF SCIENCE BEING ON THE MUSLIM'S SIDE COMPLETELY
4 notes
·
View notes
Text
got diagnosed w a high iq and neurocognitive disability and i can get vocational and educational support yay yippee
#i don’t rly believe in iq tests but it’s still interesting to know ig#also got diagnosed with immaturity and impulsivity LOL
4 notes
·
View notes
Text
want.. need.. want see so bad young people with neurocognitive disorders talk about it…
not diagnosed with anything don’t even know what group cognitive issue belong in so maybe hypocritical specify This but Not That but want see more people… because… feel so. alone
not chronic fatigue brain fog not depression not OSDDID memory issues or other mental illnesses. not what am talk about… something different
mild cognitive impairment (the disorder)… major neurocognitive disorder / dementia… etc
or like significant cognitive symptoms from severe physical or neurological disabilities
please
33 notes
·
View notes
Text
The basic principle of a suggested neurostrike weapon is a fairly simple proposition. It entails a hand held, or platform mounted, mixture of an RF, directed energy pulse or neurocognitive disrupter, combined with acoustic wave dynamics which is designed to harm, disable or permanently damage a human brain. It may also adversely affect the brains of several in close proximity to the attack. Unlike future forecasts of likely, suspected or even probably designable future kinetic weapons systems which can significantly alter the battle domain and strategic calculus cognitive warfare remains speculative and theoretical despite evidence that its subtle and dynamic technology inflicts permanent or long lasting brain injury. One conclusion indicates that after 2020 all prior theories of combat or the use of non-lethal force on both civilian and military targets must now be rethought and reconsidered. Victims of NeuroStrike attacks have experienced sustained and persistent neuro-cognitive disruptive effects which can be medically confirmed and which vary among its victims. Under existing procedures, these casualties of cognitive warfare defy facile medical definition and categorization by persons unfamiliar with the diagnostic mechanisms experts at Penn Medicine, University of Miami and the National Academy of Sciences can confirm. If you have never seen it before you don’t recognize it.
13 notes
·
View notes
Text
Why does no one talk about the fact I'm canonically disabled? Hitting my head as a baby is one thing, but based on the amnesia and personality change, I literally fit the criteria for a major neurocognitive disorder due to a traumatic brain injury (thanks to Casey for helping me type/remember that). That's a disability. Why does no one talk about it? -Goku
2 notes
·
View notes