#millionsmissing
Explore tagged Tumblr posts
Text

I've just changed my Twitter profile: I have now spent 30 years severely affected/housebound with Myalgic Encephalomyelitis / Chronic Fatigue Syndrome since age 22 (i.e. more than half my life). [I first became ill at age 16, 35.5 years ago, but was initially less severely affected but was undiagnosed].
I'm one of millions around the world.
We need more public and private money to make research progress soon, the quicker the better: my life and the lives of others are passing by.
For anyone interested, here's a list of ME/CFS research funds:
Here's my story as told in the Irish Independent in 2015: 'No one chooses to have ME - everything changed when I became ill'
16 notes
·
View notes
Text
Ren - Troubles
youtube
I can't stop listening to his new song about his battle with chronic illness and mental health. Sadness and hope, anger and determination and so much texture in the music, I keep hearing new things!
Please listen and reblog to help Ren spread awareness and conversation about the #MillionsMissing due to chronic illnesses like Lyme Disease, MCAS, POTS, EDS, ME/CFS, fibromyalgia, and long Covid, as well as chronic pain, anxiety and other issues that lead to people (and their caretakers) going #MISSING from the rest of society.
#renmakesmusic#ren gill#ren#new music#lyme disease#chronic lyme#myalgic encephalomyelitis#millionsmissing#Youtube
22 notes
·
View notes
Text
instagram
Frühe Warnsignale bei ME/CFS: Selbstfürsorge und rechtzeitige Reaktionen
Myalgische Enzephalomyelitis/Chronisches Fatigue Syndrom (#mecfs) ist eine komplexe Erkrankung, bei der die frühzeitige Erkennung von Warnsignalen entscheidend ist. Ein proaktiver Umgang mit diesen Signalen kann helfen, eine Verschlechterung der Symptome zu vermeiden.
Körperliche Warnsignale:
1. Erhöhte Erschöpfung: Ein unerwartetes, tiefes Müdigkeitsgefühl ist oft ein Hinweis auf aufgebrauchte Energiereserven.
2. Muskelschwäche:
Wenn alltägliche Aufgaben schwerfallen oder Muskelzittern auftritt, könnte eine Pause nötig sein.
3. Schmerz: Ungewohnte Schmerzen in Muskeln und Gelenken sind Warnsignale, die nicht ignoriert werden sollten.
4. Schwindel:
Schwindel beim Aufstehen oder Aktivität zeigt, dass der Körper Ruhe benötigt.
5. Herzrasen: Ein erhöhter Puls in Ruhe kann auf Überanstrengung hinweisen.
Geistige Warnsignale:
1. Konzentrationsprobleme: Schwierigkeiten bei der Konzentration deuten oft auf Ermüdung hin.
2. Gedächtnisprobleme:
„Gehirnnebel“ und Vergesslichkeit sind häufige Anzeichen mentaler Überlastung.
3. Reizbarkeit: Häufige Stimmungsschwankungen können auf emotionale Belastung hindeuten.
4. Überwältigung: Ein Gefühl der Überforderung ist ein klares Signal, das Tempo zu verlangsamen.
Strategien zur Energieeinsparung
1. Aktivitätenmanagement (Pacing): Plane Aktivitäten mit ausreichenden Pausen, um Überanstrengung zu vermeiden.
2. Ruhephasen: Regelmäßige Pausen, auch bei fehlender Erschöpfung, sind wichtig.
3. Priorisierung: Setze Prioritäten und delegiere unwichtige Aufgaben.
4. Ergonomie: Schaffe eine ergonomische Umgebung, um den Energieverbrauch zu optimieren.
Fazit:
Das frühzeitige Erkennen dieser körperlichen und geistigen Warnsignale ist entscheidend im Umgang mit ME/CFS. Höre auf die Signale deines Körpers und reagiere rechtzeitig, um das Risiko einer Verschlechterung zu minimieren. Achte gut auf deine Bedürfnisse!
©️®️CWG, 2024
#cwg64d #cwghighsensitive #mecfsNORDHESSEN #oculiauris
#cwg64d#oculiauris#claudiaweidtgoldmann#florianatopfblume#cwghighsensitive#mecfs#mecfsnordhessen#lightMEup#millionsmissing#mehilfe#fatigatio#nichtgenesenkids#nichtgenesen#mecfsportal#dgmecfs#myalgischeenzephalomyelitis#myalgischeencephalomyelitis#Instagram
2 notes
·
View notes
Text

7 Steps to Health Equity: Addressing Root Causes Now in 2024
Health equity is more than just equal access to healthcare services. It means giving everyone a fair chance to be as healthy as possible, no matter their background or circumstances. This includes addressing the social and economic factors that can create barriers to good health. Read More...
#healthequity#publichealth#healthdisparities#covid#healthcare#health#womenshealth#equity#blackhealthmatters#blackhealth#mentalhealth#community#wellness#healtheducation#communityhealth#healthdisparity#pwme#socialdeterminantsofhealth#publichealthmatters#globalhealth#myalgice#mastcellactivationsyndrome#premenstrualdysphoricdisorder#meaction#myalgicencephalomyelitis#heds#nightingales#unexplainedweightloss#saveliznevra#millionsmissing
3 notes
·
View notes
Text
Millions missing
Knapp 1 1/2 Jahre sind vergangen, seit dem ersten Verdacht, an ME/CFS erkrankt zu sein. Und dem langsamen Verschwinden, aus meinem eigenen Leben.
Kurze Zeit später fand ich raus, dass überdurchschnittlich viele, eine positive EBV Anamnese haben. Ein Virus, das meiner Meinung nach jahrzehntelang unterschätzt wurde. Dabei setzt diese Erkrankung so viele von uns, völlig außer Gefecht und befördert einige ins Krankenhaus, wie auch mich, damals mit 13 Jahren.
Angegriffene Organe, der gesamte Organismus völlig aus dem Gleichgewicht. Lebenslanges Risiko der Reaktivierung, Chronifizierung und mögliche Ursache, einer am Ende unheilbaren Erkrankung. Aber wer hätte das schon ahnen können? Am allerwenigsten ich selbst.
8 Monate, seit ich geschwächt bei meiner Hausärztin saß und ihr berichtete, dass ich nach einem schweren, aber unklaren Infekt im Sommer 2020, nicht wieder auf die Beine kam; dass ich mich mittlerweile seit Monaten krank fühle. Tägliche Grippesymptome, neurologische und motorische Ausfälle, eine bleierne Erschöpfung und starke Schmerzen.
Sie hat mich nicht ernst genommen. Der Klassiker. Schließlich war ich untergewichtig und steckte wieder tief in der Essstörung.
Für sie war mein Fall völlig klar.
Thema abgeschlossen.
Für mich allerdings nicht.
Ich kämpfte mich wieder raus aus dem Untergewicht, aber nichts hat sich dadurch verändert oder gar verbessert. Denn ich wusste, dass mit meinem Körper etwas nicht stimmt. Ich konnte es spüren.
6 Monate, seit ich mir eingestehen musste, dass mein altes Leben, so wie ich es kannte, nicht mehr existiert.
Der Versuch eine Balance zu finden zwischen Ärzte-Odyssee, Ausschlussdiagnostik und „das bildest du dir doch eh bloß ein“ Gedanken in meinem verdrehten Kopf.
3 Monate, seit ich einen anderen Arzt fand, der sich auskennt und vor allem: der mich ernst nahm.
1 Monat, seit der immunologischen Laboruntersuchung und den erschreckenden Ergebnissen mit erhöhten GPCR Autoantikörper, Interleukin Werten und dem eindeutigen Nachweis, einer Autoimmunreaktion.
3 Wochen, seit der offiziellen ME/CFS Diagnose meines Arztes, der von Anfang an wusste, dass ich zwar eine ganze Palette an psychischen Erkrankungen mitbringe, aber das akute Problem, eindeutig körperlicher Natur ist.
Seit dem. Steht alles still.
Denn mit der Diagnose, kam die Depression. Die nackte Angst, die pure Verzweiflung.
Nie war mein Blogname passender. Aber diesmal, gibt es kein Weg raus. Die auszeitstille, ist nicht mehr nur eine Auszeit. Die Stille wird bleiben, so lange, bis die Politik endlich hinsieht. Wir brauchen Forschung, Akzeptanz, Therapie und bitte bitte bitte irgendwann eine Heilung.
Egal wer das hier liest: bitte sieh hin, werde laut. Erkundige dich über ME/CFS, kläre auf und trage unsere Botschaft in die Welt hinaus. Wir sind sichtbar, wir wollen leben.
6 notes
·
View notes
Text

At Mass General Hospital fighting to keep mask mandates! ✊😷
9 notes
·
View notes
Photo
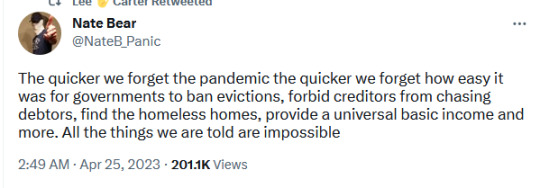
And also remember that letting people work from home, and attend virtual concerts, and go to meetings via zoom, and go to conferences virtually, and go to religious services virtually, and go to all kinds of other events virtually and thus, allowing for disabled and chronically ill folks to participate in society like never before…
But now, folks want to take so many of those options away all over again…isolating disabled and chronically ill folks from society again. It’s cruel…taking something beautiful like that away from us after showing us that something like that was possible this whole time since we have had the technology. And now that we know for a fact that the technology exists, non-disabled and non-chronically ill people want to take that away from us?
It’s beyond cruel.
If you’ve never been house bound or bed bound for months or years on end like I have? Or like others like me have? Then you have no idea what this feels like. None.
#tweet#tweets#twitter#the pandemic#pandemic#covid-19#capitalism is a scam#disabled#heds#ME/CFS#myalgic encephalomyelitis#Chronic Fatigue Syndrome#Post Viral Syndrome#H1N1#Bed Bound#House Bound#Work From Home#Virtual Attendance#Online Attendance#Chronically Ill#Chronic Illness#Disabled Adult#Millions Missing#MillionsMissing#Lung Damage#Scarred Lungs#H1N1 Gave Me Asthma#Asthma#I Am One Of The Millions Missing
71K notes
·
View notes
Text
#mecfs
#mecfsportal#mecfsnordhessen#mecfs#oculiauris#gesundheit-politik#mehilfe#nichtgenesenkids#nichtgenesen#millionsmissing#millionsmissinggermany
1 note
·
View note
Text
youtube
Fighting to live but..I've made a few videos to help better describe what's going on for me. they are of varying lengths and varying levels of brain function as I am so brutalized by attempting to stretch money on minimal treatments as there has yet to be any MSP category of coverage for my disease in any province in Canada. if the GoFundMe doesn't accrue enough money then I don't survive into January. I'm fighting to start a human rights case but I need to stay alive long enough to see it through.
I disabled comments as with my dyslexia combining with my myalgic encephalomyelitis and fibromyalgia it's too difficult for me to read or respond. if you want to connect with me Twitter is where you'll find me more often as a cope better with that short form text
Podcast 1st ep
https://anchor.fm/i-am-madeline/episodes/Ep--1---How-do-you-solve-a-problem-e110jks
general podcast link
https://anchor.fm/i-am-madeline
GoFundMe ( keep in mind that this money has been used up on minimal treatments and supports over the past 3 years)
https://gofund.me/cff39173
RICHOCHET article
https://ricochet.media/en/3991/Canada-MAID-policy-death-by-poverty
Also the journalist did a tweet thread with highlights from the article if that's something that you're interested on sharing Facebook and Instagram won't let you share a news links from Canada https://twitter.com/SpichakSimon/status/1707785829433618864?t=RowAITYe-W17QLiZRGTNMQ&s=19
#millionsmissing
op-ed
Dabc Nov 2022
Blog
https://disabilityalliancebc.org/article-im-fighting-to-live-but/
politics Nov 15 2021
https://ipolitics.ca/2021/11/15/the-disabled-are-choosing-to-die-because-they-cant-afford-to-live/
Gender bias in research med article
https://pubmed.ncbi.nlm.nih.gov/33232627/
Twitter @IamMadelinePod pinned tweet has all the media pieces done so far
Facebook & Instagram @Madelinenerdfighter.
#british columbia#canada#canadian#disability#disability pride#myalgic encephalomyelitis#podcast#pwme#canpoli#chronic illness#youtube#millionsmissing#chronic pain#chronically ill#disability human rights#human rights#nerdfighter#nerdfighteria#project for awesome#p4a
1 note
·
View note
Text
Millions of American adults are impaired by long Covid. They have a vision for what our society owes to chronically ill and disabled people.
April 11, 2023
On a muggy late-summer day in September 2022, dozens of disabled protesters lay on the sidewalk outside the White House. The ground was hot, and sweat clung to their faces under their masks. Many would pay the price with their health in the weeks to come. But the protesters felt they had no choice. The night before, President Biden had announced that “the pandemic is over.” The protesters knew that this wasn’t true. Long Covid, they argued, is a national emergency.
#MillionsMissing demonstrations like this one began in 2016 to raise awareness about myalgic encephalomyelitis, an infection-associated complex chronic illness (often abbreviated as ME/CFS). The hashtag alludes to the millions of dollars missing from research into ME/CFS and the millions of patients who are so marginalized from society that they sometimes seem to have disappeared. In the past three years, there has been an explosion of ME/CFS cases. According to #MEAction, the group that organizes #MillionsMissing, nearly half the current cases of long Covid meet the criteria for ME/CFS, and the majority of people with ME/CFS today are Covid-19 long-haulers.
Top Stories 00:04 01:12 Donald Trump Sinks to a New Low by Dog-Whistling an Old Racist Tune The Fifth Circuit’s Abortion Pill Ruling Was All About Sowing Confusion The Corrupt Courts and the Feckless Senate Judiciary Committee The Brief Death and Miraculous Resurrection of the “Texas Observer” Chicago’s Rich Organizing Tradition Paid Off, Delivering Victory for Brandon Johnson Donald Trump Sinks to a NewLow byDog-Whistling an Old Racist Tune
Long Covid symptoms, which commonly include persistent headaches, cognitive-functioning issues, fatigue, neuropathies, dizziness and fainting, significant sleep disturbances, gastrointestinal issues, and post-exertional symptom exacerbation (the worsening of symptoms after physical, mental, or emotional exertion), can affect every system of the body and, like those of ME/CFS, can range from mild to very severe. It’s common for Covid-19 long-haulers to receive additional diagnoses for related chronic illnesses. Because scientists also believe Covid may reactivate dormant viruses such as Epstein-Barr, some people with long Covid have been diagnosed with Lyme disease, shingles, and herpes, among other viruses. Many Covid long-haulers share symptom clusters and illness experiences, but “long Covid” also serves as a political term: It is a way for Covid patients who never fully recovered to advocate for research, public education, and economic support, no matter where they fall on the severity spectrum.
Even before reports of long Covid emerged in the spring of 2020, people with ME/CFS had ample reason to predict a surge in chronic illness; many had been disabled by similar infections. Not all cases of long Covid are ME/CFS, but many cases fit the criteria after six months. Covid long-haulers, like people with ME/CFS, report an impaired ability to work, which often results in substantial financial hardship. As of August 2022, it was estimated that as many as 16 million working-age US adults were living with long Covid, and as many as 2.5 million were living with ME/CFS. Two to four million Americans may be out of work as a result of long Covid, and people with long Covid and ME/CFS often struggle to access what are already often insufficient disability benefits. Facing financial hardship as the result of a disability is not an unusual experience, and while the Biden administration recognized long Covid as a disability in 2021 and has released several reports outlining recommendations for addressing the crisis, it has yet to provide new, direct economic support for Covid long-haulers or respond to calls to expand Supplemental Security Income and to update Social Security Disability Insurance. The expiration of the federal pandemic emergency in May will also mean the end of some enhanced social-safety-net benefits.
The Covid-19 Pandemic
The #MillionsMissing protesters who put their bodies on the line last fall were hoping to halt the push to “move on” from the Covid pandemic. Their actions build on a long history of disabled and chronically ill people mobilizing on behalf of their communities—from the HIV/AIDS advocates who staged massive street marches campaigning for better research in the 1980s to the disability rights activists who crawled up the steps of the US Capitol in 1990 to demand passage of the Americans With Disabilities Act and the disabled activists who protested inside the Capitol in 2017 to fight cuts to Medicaid. People with long Covid, ME/CFS, and related diseases are fighting for patient-centered approaches to research, strengthened social services and financial support, and a societal shift in how disabled and chronically ill people are treated. With millions more now in their ranks, the “missing” are fighting to be seen.
Senator Tim Kaine
Show of solidarity: Despite lobbying by Senator Tim Kaine, himself a long-hauler, Congress allocated just $10 million for long Covid research, treatment and support in December. (Amanda Andrade-Rhoades / AP Photo )
In December 2020, Congress allocated $1.15 billion in funding for National Institutes of Health research into long Covid. But advocates say progress has been slow and argue that it’s long past time the government allowed patients to have “meaningful involvement” in setting research agendas and designing studies—an idea largely inspired by HIV/AIDS activists, who physically occupied parts of the NIH campus to demand that researchers expedite clinical trials for HIV drugs. Instead, advocates say, NIH researchers seem to be wasting time revisiting treatment approaches that have already been discredited rather than incorporating feedback from patient communities.
HIV/AIDS activists fought for and won an Office of AIDS Research, coordinating information across the whole of the nation’s biomedical research establishment. Similarly, Covid long-haulers are pushing for a new NIH institute dedicated to studying diseases like long Covid, ME/CFS, and similar post-infectious illnesses—a National Institute of Complex Chronic Conditions. Three years into the pandemic, the economic case for such an institute is clear. In October, the Center for Economic Policy Research released an analysis of the latest Census Bureau data about long Covid’s new epidemic of disability. The study found that of the more than 119 million Americans who had tested positive for Covid by late September 2022, about 15 percent reported symptoms lasting longer than three months, which is consistent with US government findings that estimate between 10 and 30 percent of Covid-19 survivors develop prolonged post-viral symptoms. In all, there are 9.9 million long-haulers who said their daily activities are slightly reduced and 4.4 million who reported “a lot” of day-to-day impairment. Because it’s common for long-haulers to experience temporarily or permanently worsened health after periods of exertion, pushing past symptoms in order to work can be dangerous. Some long-haulers are not able to work at all. Those who can but lack the workplace accommodations necessary to perform their jobs safely are likely to get sicker.
And as long Covid destroys livelihoods and contributes to the labor shortage, it also overwhelms the patchwork array of clinics set up around the country that provide multidisciplinary care for the complex constellation of symptoms that long-haulers face. These clinics are riddled with issues. There is no uniform standard of care (no specific license is required for a clinic to call itself a “long Covid” clinic), and the clinics that do exist can be costly and are hampered by long waiting lists and limited capacity. For providers, hour-long appointments are frequently needed to evaluate patients with a dozen distinct symptoms, but billing codes only accommodate 15-minute visits.
“Many centers—like my own—do not have those [necessary] resources and may even close or stop taking patients,” says Dr. Monica Verduzco-Gutierrez, the medical director of the Post Covid Recovery Clinic at the University of Texas Health Science Center at San Antonio. “To put it plainly, the need for these clinics far outstrips the resources available in many areas of the country.”
Some larger medical centers have the funds to cover the extensive costs of maintaining an adequate level of services, but many community health centers do not. To make matters worse, a lack of clinical education on ME/CFS and related diseases means that the few providers who were well-versed in them before the pandemic are now in short supply. Some are leaving ME/CFS patients for the growing ranks of Covid long-haulers, exacerbating tensions between two patient communities that have shared interests. Solving this problem will require centers of excellence that can treat long-haulers and those with related illnesses. It also requires that medical schools update their curriculums to help develop a new generation of providers who are better educated on post-infectious illnesses.
In order for long-haulers to get the multidisciplinary health care they need, the federal government must act urgently, says Dr. Steven Flanagan, the president of the American Academy of Physical Medicine and Rehabilitation. During the pandemic, the AAPM&R has helped 41 long Covid clinics around the country publish consensus guidance statements for health care providers. It has also championed several bills in Congress, including the TREAT Long Covid Act, proposed by Representative Ayanna Pressley, which would provide up to $2 million in grants for community health clinics dedicated to long Covid.
Flanagan notes that the Biden administration has made progress recently by publishing its national action plan on long Covid, but, he says, “there’s more work to be done.” Last fall, as part of the administration’s initiative, the Department of Health and Human Services sent Congress a $750 million budget request for the long Covid agenda that included research, treatment, and support for community-based organizations providing case management for patients. But despite lobbying by Senator Tim Kaine, himself a long-hauler, Congress allocated just $10 million for it when it passed its end-of-year omnibus bill in December.
Another important measure would be a national fund to process claims from the millions disabled by long Covid and provide compensation based on standardized diagnostic criteria. Such a program might take inspiration from the September 11 Victim Compensation Fund, established in 2001. Like those made ill by 9/11, many Covid long-haulers feel that the government is responsible for their acquired disability because of its failures to adequately mitigate Covid infections, provide safe workplaces, or publicly warn of the harms of long Covid after the disease was identified in the spring of 2020.
“The consequences of such an exposure…should not be the burden of the individual who did not give their consent to be exposed,” says Netia McCray, the director of education for the Covid-19 Longhauler Advocacy Project. “If Covid exposure and subsequently long Covid is a necessary risk, for the sake of society, it should be compensated. That’s the cost of doing business.” Howard Bauchner, a former editor in chief of the Journal of the American Medical Association, suggested in an article in Health Affairs that a long Covid compensation program could be funded by pharmaceutical companies or a tax on vaccines.
Dangerous burnout: A common effect of long Covid is post-exertional symptom exacerbation, the worsening of symptoms after physical, mental, or emotional exertion. (Martin Pope / SOPA Images / LightRocket via Getty Images)
In the absence of robust federal funding to secure care, the advice of grassroots activists and online peer-support groups has often been the most effective prescription for patients in need. When Dr. Raven Baxter began to develop long Covid, her doctors didn’t have answers. So Baxter turned to a robust online community of long Covid patients for advice. When she tweeted about feeling worse after physical activity, patients explained post-exertional symptom exacerbation. When Baxter’s heart rate spiked upon standing, patients with orthostatic intolerance recommended increased sodium. When Baxter’s mobility decreased, patients and wheelchair users offered tips on the best mobility aids and how to access them. “I felt so grateful to have that type of support,” Baxter says.
When the first wave of Covid long-haulers got sick in the winter and spring of 2020, there was little public information available about the disease, and patients were forced to rely on one another for guidance and support. Today the information landscape looks different. People who have developed long Covid in the past two years face an intimidating slew of online information and misinformation on the disease, some of which is put out by the anti-vax movement, people who desire to move on from the pandemic, or businesses attempting to profit off of patients. Some articles on long Covid argue that its symptoms and prevalence have been exaggerated, or that the disease may have no connection to Covid-19 and is instead driven by “psychosocial distress,” patient-support groups, or media coverage of the disease.
This sort of skepticism is not new. People with ME/CFS have fought, arguably for centuries, to be accurately diagnosed and treated by providers who were eager to assign symptoms to psychological causes. The disproportionate impact of these diseases on people assigned female at birth and the fact that these disabilities are sometimes “invisible” have likely played a part in these hasty diagnoses. The results have been harmful for patients. Interventions designed for mental illness—such as exercise and cognitive behavioral therapy—are often detrimental for people with energy-limiting illnesses that cannot be cured by modifying behavior. Skeptics eager to frame long Covid as psychosomatic also often disingenuously omit the evidence of biomedical abnormalities found in long-haulers, or the fact that many patients have already tried ill-advised interventions such as graded-exercise therapy in desperate attempts to find a cure.
The lack of investment in ME/CFS research and awareness has directly contributed to the proliferation of articles in the media casting doubt on long Covid’s origins and to research trials that attempt to reinvent the wheel. It has also meant that providers and policy-makers are ill-prepared to support long Covid patients. Public health messaging still fails to adequately identify long Covid as a primary pandemic harm. According to a May 2022 study, state health departments posted 49,310 times on Facebook about Covid between July 2020 and February 2022, but only 137 of those posts mentioned long Covid.
The emergence of grassroots support groups and advocacy networks has been a lifeline for long-haulers who are struggling, but three years into the pandemic, community leaders are burning out. “We have done this work in the absence of the kind of philanthropic or government support that a mass disabling event such as this should warrant,” says Angela Meriquez Vázquez, a disabled long Covid patient advocate and children’s activist who runs the Body Politic Covid-19 Support Group. JD Davids, a longtime AIDS and chronic illness activist who is a co-founder of Long COVID Justice, recounts attending a New York City Council hearing on long Covid at which Ted Long, the executive director of the NYC Test & Treat Corps, mentioned the Body Politic support group as a primary resource but failed to explain that “the city doesn’t give a penny to Body Politic, which basically has no funding.”
Long Covid advocates are not the first people who have filled gaps in information through community efforts, and they’re not the first advocates who have struggled to maintain this work in the absence of significant support from the government. From the mid-1980s through the early 2000s, HIV/AIDS groups emerged to disseminate crucial information about prevention, care, and eventually access to testing and treatment. But after antiretroviral therapies became available in the United States in the mid-1990s, funding and media attention were redirected toward fighting the disease abroad, while HIV rates continued to climb in Black communities here.
As a result, some smaller community organizations were forced to shut down, which left many patients without access to information and treatment. According to Kenyon Farrow, the former managing director of advocacy and organizing at PrEP4All, far too many people still aren’t aware of current HIV treatment and prevention options. “Information is not received by everyone equally,” he explains. “You do need messengers in communities…to reaffirm or translate that information in ways that specific communities understand.”
Long Covid advocates face similar issues. Vázquez is “incredibly concerned” about low-income people of color who have not received proper information about the symptoms of long Covid or how to manage them and may risk undermining their health further with ill-advised exertion.
Vázquez and Davids say the government must do more to provide existing groups of community health workers (CHWs) with resources and information on long Covid. Most CHWs are funded by Medicaid and serve as nonclinical liaisons between medical and social services and their local communities, with whom they share identities and experiences. “There will not be adequate care [until] we have an integrated, strategic, and well-funded system bridging research and care from the neighborhood level—where people you know and trust speak your language to accompany you through the systems of care you may need,” Davids says.
The time is ripe for this, says Vázquez, who points out that the Department of Health and Human Services recently invested millions of dollars in strengthening the CHW workforce. “We need to significantly increase investments and [build the] capacity of community health workers to disseminate information and facilitate access to health care for these marginalized groups,” Vázquez says. She adds that any future legislation on long Covid must “actively incorporate state Medicaid agencies” to advise them on releasing state guidance on long Covid and provide incentives for states to invest in local public health campaigns.
In 1990, disability activists staged direct actions in Washington, D.C.
Taking inspiration: In 1990, disability activists staged direct actions in Washington, D.C., to demand the passage of the Americans with Disablities Act. (Jeff Markowitz / AP Photo)
It’s been clear ever since the first cases of long Covid were documented that the disease would take an economic toll. It’s expensive to be sick, and disabled people in the US are twice as likely to live in poverty as nondisabled people. A recent CDC study found that four out of five people with long Covid report trouble performing day-to-day activities.
While a compensation fund could provide long-haulers with immediate support, it’s unclear how eligibility for such a fund would be determined and who might get left out. The diagnostic criteria for long Covid are still developing, and some patients have already been shut out of care and benefits because they lacked medical documentation. Some advocates have pushed for a guaranteed income to support chronically ill and disabled people regardless of their diagnoses. The debate raises a question that long Covid advocates have grappled with from the start of the pandemic: Can the long Covid crisis be a turning point in the fight for better safety nets for all disabled and chronically ill people?
Most of the legislation that’s been proposed so far has failed to address the systemic causes of poverty among disabled populations, focusing instead on research, education, and clinical care that is specific to long Covid. Lisa McCorkell, a founding member of the Patient-Led Research Collaborative, says these bills are important in order to sustain current clinics and make sure that people with long Covid are aware of the benefits and services that do exist. But, she adds, “the point of these bills is not to improve overall disability policy.” They don’t shorten application-processing times for Social Security disability benefits, nor do they recommend updates on asset limits or increases in benefits. “We need big policy solutions that will address larger systemic issues,” she says, “and we need those solutions to be created with a disability-justice lens in order to…ameliorate the cycle of poverty that is disabled poverty.”
Ultimately, the long Covid advocacy movement’s ability to address these systemic issues will determine its success. Sixty-one million US adults—about one in four eligible voters—have a disability, and disabled people represent a historically overlooked voting bloc. More than 30 years after the passage of the Americans With Disabilities Act, disabled Americans still face food insecurity at three times the rate of nondisabled people, and they make up roughly half of those who turn to homeless shelters every night. The 2020 election cycle was a breakthrough, with nearly every major Democratic candidate releasing a full disability policy platform. Still, though, just three in 10 disabled voters believe that leaders in Washington care about people with disabilities, according to a recent poll by the Century Foundation and Data for Progress. “The economic crisis facing the US disability community long predates Covid-19,” says Rebecca Vallas, a senior fellow at the Century Foundation and codirector of the Disability Economic Justice Collaborative. But “one takeaway at this moment in our nation’s history must be that we can no longer afford to ignore disabled people in our policy-making.”
0 notes
Text

I'm one of millions missing from our lives due to Myalgic Encephalomyelitis, each with their own challenges and losses. Unlike Covid lockdowns, the lockdowns we have dealt with for years due to #ME continue
17 notes
·
View notes
Text
I watched Unrest yesterday and I was near tears in the end.
This is why I do what I do. This is why I am an advocate. There are so many people who are so much less fortunate, less privileged, than I am, whose voices are so much harder to be heard.
I will never stop fighting. I will never give up. I am here for the #millionsmissing.
#millions missing#me/cfs#chronic illness warrior#chronic fatigue warrior#spoonie community#disabled community#global voice for me#ally for me#me/cfs advocacy#me/cfs warrior#cripple punk#spoonie strong
2 notes
·
View notes
Text
#covid19#cwg64d#oculiauris#claudiaweidtgoldmann#cwghighsensitive#florianatopfblume#mecfs#mecfsnordhessen#millionsmissing#millionsmissingdeutschland#mehilfe#mecfsportal#dgmecfs#fatigatio#lightMEup#nichtgenesenkids#nichtgenesen#postvacc#longcovid#postcovid
0 notes
Text
Mega post
Please share
World Health Network global
Protect Their Future (Grassroots org of parents & pediatricians advocating for protection for ALL children)
linktr.ee/laughterinlight_sciencelibrary
PeoplesCDC.org
longcovidlearning.org
covidresearch.net
#ME Action Network
Long COVID with ME
Long Covid Advocacy Ireland
Dysautonomia International
DecodeME the ME/CFS Study (The world's largest study ever into #MEcfs.Take part today (UK, 16+) #pwME [email protected] - 0800 196 8664 #DecodeMEStudy #pwME #MillionsMissing)
Dysautonomia Society (💜We aim to increase global awareness of Dysautonomia. Join us!)
Mast Cell Disease Society (Transforming lives of patients and families while finding a cure for #mastcelldisease since 1995. #Mastocytosis #MCAS #HereditaryAlphaTryptasemia #raredisease)
Mast Cell Action (We exist to promote progress in the awareness, diagnosis and treatment of Mast Cell Activation Syndrome and to provide support to people affected by MCAS)
Awareness for POTsies (POTS, Chronic Illness, & Mental Health Support. Compassion, Awareness, Education, Empowerment)
linktr.ee/longcovidlife
linktr.ee/longcovidfam (Long Covid Families)
Long Covid Kids (UK, Ireland)
Clinically Vulnerable Families
Abrome (Self-Directed Education community)
Long COVID Physio
NotRecovered.org (Support for chronically ill)
Covid Persistente México Comunidad Solidaria
Long Covid Latin America (Twitter & Instagram) & André Saravia (Twitter & Instagram)
Long Covid Chile (Instagram, Twitter & YouTube)
Linktr.ee/wearebodypolitic (Support for chronically ill)
Linktr.ee/patientled (Patient led research)
Long Covid Advocacy
RTHM.com (RTHM Health, biotechnology research. Transforming care for complex illnesses starting with long covid).
Linktr.ee/covidisntover (Virtual hangout)
CovidSafeDentists.ca
CovidConsciousTherapists.com
Covid Safe Cuties (dating) Twitter & Instagram
CovidMeetUps.com (Covid safe networking & listings)
Linktr.ee/PenGwenWithLC (Project in progress for long haulers)
Bheecollective.org (Send letters to White House)
International Long Covid Awareness
MandateMasksUS.org
PandemicAidNetworks.org (Organizing and info hub)
High Impact Strategies (S4HI builds the power of chronically-ill & disabled people, our groups & networks. #NothingAboutUsWithoutUs #PandemicsAreChronic)
Birch Health (Twitter & Instagram (Infographs and amplifying stories of black, indigenous and racialized peoples)
The Chronic Collaboration
Linktr.ee/equiinstitute
CoalitionForCovidJustice.com
Long Covid Justice
Linktr.ee/Project_N95 (PPE)
Linktr.ee/DonateAMask (PPE)
Clean Air Crew (Airborne pandemic tips and tools)
Clean Air Stars (Helping businesses protect their customers from viruses like SARS-CoV-2)
Aaron Collins (@/masknerd) Twitter & YouTube "Goal is to test and evaluate the best masks out there."
Breathe Safe Air (Everything that you need to know about air pollution. Respirators, masks, air purifiers, monitors and more)
Clean Air Club (Ensuring accessible and cleaner air for Chicago artists and venues. ☁️ a new project by @/nora_barnacles)
*List updated periodically*
You are not alone
Your life has inherent worth
Sars CoV-2 and long covid are real
The pandemic is not over
#Covid-19#covid 19#sars cov 2#covid#long covid#long haul covid#The Pandemic#pandemic#public health#Resources#Info#Information#Mega Post#Please share#Feel free to share!#Feel free to reblog and add more#Especially resources in other languages and countries
27 notes
·
View notes
Video
youtube
#MillionsMissing 2023 Pillowcases
3 notes
·
View notes
Text
youtube
This is a powerful new song by Ren, about getting a virus at 19 and never getting better. Initially diagnosed with depression and ME/CFS, he declined for 7 years until finally his diagnosis was finally refined to Lyme disease, and MCAS caused by the untreated infection. This song is meant to raise awareness for the #MillionsMissing due to chronic illness and pain -- please pass it along if the music and the message matters to you!
The only good thing about long COVID is that it made the medical community admit myalgic encephalomyelitis is likely caused my viral exposure. We were like “Hey, I had a virus and just never got better.” and doctors were like “That’s silly. And stupid. Chronic fatigue syndrome is just a random vague constellation of symptoms. Or just depression. It’s all in your head.” and now doctors are experiencing it.
20K notes
·
View notes