#experiencing dysregulation of your nervous system
Explore tagged Tumblr posts
Text
Do you find yourself feeling overwhelmed, exhausted, and struggling to cope with life’s demands? No one would know, on the outside your ‘I’m OK’ Mask is firmly in position. The only way to get things done is to get things done. The key is to understand the symptoms of dysregulation and use specific tools to bring your body back into a state of homeostasis. There are many ways to regulate your nervous system so you can experience lasting well-being. Here’s a couple of ideas to get you started. Check this out!
#are you hiding behind the I'm OK mask?#kate mccarthy#Business Coach#Executive Coach#Health And Wellbeing#Leadership Coach#Life Coach#Personal Development Coach#feeling overwhelmed#exhausted#struggling to cope with life’s demands#experiencing dysregulation of your nervous system#dysregulation#ways to regulate your nervous system#thecoachingdirectory
0 notes
Text
nervous system regulation.
this post is especially dedicated for my fellow neurodivergents, specifically those who have add/adhd.
it’s normal for all of us to feel stressed sometimes. stress, as well as anxiety, are both feelings we all experience from time to time. however, dealing with a lot of stress is proven to have a negative impact on your body, more specifically your (autonomic) nervous system. by understanding how to regulate your nervous system, you will have an easier time managing stressful moments, and overall live a lot more balanced and peaceful life. ⋮ © credits
the nervous system.
your nervous system is the control center of your body. it is the part of your body that’s responsible for regulating your breathing, your heartbeat, your blood pressure, your digestion, and also the way you feel. the part of your nervous system that deals with the emotional wellbeing of yours is called "autonomic nervous system".
when feeling stressed, your body naturally reacts in a way to prepare you for the situation. it could respond through an increased heart rate, sweaty palms or the tension of muscles. nevertheless, our bodies cannot constantly withstand stress. continuously experiencing high levels of cortisol and adrenaline can lead to (sometimes serious) health issues.
a dysregulated nervous system.
a nervous system becomes dysregulated when the body cannot properly handle certain situations the way it used to. the body's way of responding to certain situations falls out of sync. it indicates a state of imbalance as you experience your body not being able to keep up with you.
signs.
these are some of the signs indicating you might have a dysregulated nervous system:
anxiety
easily irritated
memory problems
difficulty concentrating
headaches
quickly overwhelmed
mood swings
panic attacks
digestive issues
trouble sleeping
constant fatigue
chronic pain
persistent muscle tension
weakened immune system
stressors.
here is a list of stressors that are known to disrupt your nervous system balance:
chronic stress
burnout
traumatic events
poor sleep habits
unhealthy diet
no time for relaxation
support.
here are things you can do to help regulating your nervous system again:
meditating and resting
listening to music
dancing and moving
stretching and walking
eft tapping
massaging yourself
affirming
practicing mindfulness
reconnecting with nature
hugging someone or yourself
somatic shaking
rubbing ice cubes on face
taking a cold shower
sleeping and waking up early
grounding yourself
humming, singing and laughing
talking to someone
reading or listening
using a weighted blanket
drinking herbal tea
engaging in calming activities
deep breathing exercises
prioritising your sleep
with love, ella.
#nervous system regulation#nervous system#law of assumption#neville goddard#loassumption#loa#loablr#loa tumblr#manifesting#manifestation#how to manifest#manifest#master manifestor#the law of assumption#spiritual#spirituality#edward art#neurodivergent#adhd#add#positive thinking#mental health#mental heath support#mental heath awareness#mental help#mental heath issues#positivemindset#affirmations#positive thoughts#positive affirmations
309 notes
·
View notes
Text
It's frustrating to me that so many resources for coping with suicidal ideation seem to run on the assumption of SI being an exclusively acute experience. Almost all of them start with something like "Remember, this is just a temporary feeling, and like all feelings they pass eventually!" and then they give short term solutions like grounding techniques, or distraction techniques, or breathing exercises, or nervous system regulation exercises with the purpose of calming down enough to get through these few rough moments of being dysregulated and upset.
And I'm not saying they're bad techniques, a lot of these things can be helpful when you're dealing with distressing emotions and feelings and can help them pass more smoothly. It just doesn't really translate to my experience of chronic, near constant suicidal ideation on some level for years, regardless of the circumstances and what I'm feeling.
When suicidality has just been your default, when it doesn't matter what emotions you're experiencing, when it's just a reality you have to deal with... you can't "calm your nervous system down" to a point where it gets rid of the thoughts; you experience them dysregulated and you experience them calm. You can't distract yourself from your entire life. "Don't worry, this is just temporary!" feels insensitive bordering on cruel.
I get that it's harder to give generic advice or coping skill in the situation of always having some level of suicidal ideation going on. But it sucks trying to seek help and basically none of the solutions are super helpful for your situation.
#non religion#mental health stuff#suicide //#it's similar energy to “suicide is a permanent solution to a temporary problem”#to me#bc functionally it is a permanent problem for me. so what the fuck am i supposed to do?#I'm safe etc it's just like. i can't square breathe out of chronic SI#and i wish more resources at least acknowledged that
20 notes
·
View notes
Quote
When you are multidimensionally birthing, when you are creating, producing, curating, or sculpting signature work, you may have birthing pains that remind you of a mother in labor. I have assisted in delivering a baby alongside my friend who was working as a midwife at the time, and I am grateful to have experienced the primality and passion of a natural birth experience. I wasn't professionally trained to be an aide, an unofficial doula, but she and the mother and father trusted my temperament, breath, and heart to be of service which was more than enough reason for me to say "YES!" to their request. Of course a mother laboring a child spirit into this reality is a high octane energy that nothing could EVER compare to, and it was also very real for me in a deeply spiritual way. I didn't feel physical pain, but spiritual/energetic, (meta)physical, the incredibly overlooked and undocumented kind of birthing pains I felt. Earlier this evening I had the deepest guttural cry. I was wailing, sobbing and making loud heaving sounds while profusely shaking and unaware that I was bent over in a deep squat position. My partner was at an event and I knew if called, would have been worried and came home right away and I really didn't want that to happen. I really didn't want to talk to anyone to be honest. What calmed me into harmony was realizing that I was squatting like a sovereign mother about to have an unassisted birth. With my postural awareness and growing comfort in a resting deep squat position like the Grandmothers who flexibly squatted while prepping and cooking garri or egusi soup on the ground, I felt primordially held and cared for. After thumbing through my body of work and being taken aback by the content and page petals, feeling the potency, vulnerability, and magic and at the same time, feeling devastated and a bit scared, all I could do was surrender and sob. Encoded within our the female line and feminine psyche is a fear of being harmed whenever we speak uncommon truths that change lives, expands hearts, and free minds. These memories can put us in unconscious "fight or flight" or freeze states. I can't explain the polarity much more than my exhilaration and excitement was coupled with deep grief and devastation like "will someone come for me?" Weep, weep! There is some subtle part of my system--your system-- that remembers --this ancient fear fermenting in the female line. A signature body of body full of divine wisdom and here I feel mixed dense contradictory emotion. The last time I held this level of mixed emotion was in 2006 when my mum transitioned from breast cancer. As her primary caregiver, I felt a sense of relief that she was no longer in chronic pain but was also incredibly devastated and couldn't imagine living life without her. Being able to feel what we are actually feeling is an immeasurable blessing that I won't ever take for granted. Deeply listening to our tissues and becoming emotionally attuned to the needs of our body are gifts we give back to a world that lacks deep feeling and deep listening skills. This way our female tissues- breasts, vulva, and vaginal canal--and heart do not become contracted and hardened. And the accompanying nerve endings do not numb out. Nor does our nervous system normalize dysregulation. Like "this is it, India. Time to let it go." And I wailed and screamed because my body felt safe to release what was there. I feel tears bubbling up again as I type. It's all stunning and achy. This too is part of the love story. When there is new love, when you meet a potential new lover, there is also this fear of waiting-for-the- other-shoe-to-drop so I feel like the presence of oppositional states are a kind of creational thrust of the universe, similar to feminine and masculine energies elevating in divine union. I know authors are usually not emoting their authoring struggles online- I'm not like them. I live with an immense amount of self-generating pleasurable energy streaming through my body and on the rare occasion pain arrives at this time in my life, it's also immense. I don't care to live life like other authors. No shade to anyone but I feel things in my body that a person who lives mostly in their left brain would not be able to fathom. I know the difference because I have lived both realities. No advice needed from anyone...only vulnerably documenting this part of my journey. I will graciously receive energetic hugs though. :)
India Ame’ye, Author
60 notes
·
View notes
Text
This guide is provided for informational purposes only and is not a substitute for professional mental health care. We are not licensed mental health professionals, therapists, or counselors. The content in this guide is based on knowledge, resources, and techniques that we have researched and applied in our own journeys. While we hope the guide is helpful and supportive, it should not be considered medical advice, and it is important to consult with a qualified mental health professional for diagnosis, treatment, or therapeutic guidance specific to your needs.
If you are experiencing a mental health crisis, please seek immediate assistance from a licensed professional or contact emergency services.
Understanding Triggers in PTSD and DID
Dissociative Identity Disorder (DID) is a complex and often misunderstood mental health condition characterized by the presence of two or more distinct identities or personality states, often referred to as "alters." These alters may have their own unique memories, behaviors, and ways of interacting with the world. DID is typically the result of severe trauma, usually during early childhood, such as prolonged abuse or neglect. Understanding how to avoid triggering someone with DID involves recognizing different types of triggers, identifying signs of distress, and implementing supportive strategies.
Types of Triggers
Triggers for people with DID can vary widely and are often unique to each individual. They generally fall into several categories:
1. Stress and Emotional Intensity
Broad Impact of Stress: High levels of stress or emotional intensity can provoke a switch between alters. This stress can stem from everyday situations, like work pressure, or from more intense experiences, such as interpersonal conflict. Chronic or cumulative stressors can also contribute to triggering dissociation due to the underlying dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis in individuals with DID[^1][^2].
2. Memories and Reminders of Trauma
Internal and External Triggers: Specific memories or reminders of past trauma, whether external (e.g., smells, sounds) or internal (e.g., intrusive thoughts, emotional states), can trigger a switch. State-dependent memory is particularly relevant in DID; memories encoded in a dissociative state may only be accessible or triggered in a similar state, complicating the identification and management of those triggers[^1][^3].
3. Environmental Sensory Triggers
Diverse Sensory Inputs: Sights, sounds, smells, textures, or even specific colors linked to traumatic memories can cause a dissociative response. For example, the feel of certain fabrics or the sight of specific colors may remind someone of their trauma and trigger a switch[^3][^4].
4. Changes in Relationships or Social Dynamics
Broader Social Dynamics: Interactions with specific individuals or shifts in social roles (e.g., becoming a caregiver or joining a new social group) can act as triggers. This can include encountering someone who resembles an abuser or experiencing changes in group dynamics[^4].
5. Substance Use and Medications
Impact of Substances: Alcohol and drugs can lower the threshold for switching and may trigger dissociation. Certain medications, particularly those affecting the central nervous system (e.g., benzodiazepines, some antidepressants), can also exacerbate dissociative symptoms in some people[^5][^6].
Identifying Triggers
For the Person with DID
Self-awareness is crucial for individuals with DID to identify their triggers:
Monitoring Emotional, Physical, and Cognitive Responses: Beyond just emotional and physical responses like mood changes or physical symptoms, individuals should also pay attention to subtle cognitive shifts, such as difficulties with concentration or memory lapses, which can signal an approaching dissociative episode[^7][^8].
Journaling: Keeping a detailed journal of daily experiences, emotional states, and dissociative episodes can help identify patterns. Trauma-focused cognitive-behavioral therapy (TF-CBT) techniques within journaling can further enhance this process, helping individuals process traumatic memories more effectively[^7].
Internal Dialogue: Communication between alters can provide insights into triggers and it's also recommended that you internally communicate with the other alters of your system. [^9][^10].
For Friends and Caregivers
Friends, family, and caregivers can play a vital role in identifying triggers:
Recognizing Baseline Behavior: Understanding the baseline behavior of the individual is important, as different alters may exhibit unique behaviors. Familiarity with "co-consciousness," where multiple alters are aware of and can influence each other's actions, can help caregivers interpret whether behavioral changes are due to a switch or a co-conscious alter exerting influence[^11].
Recognizing Physical Symptoms and Motor Phenomena: Caregivers should be aware of dissociative motor phenomena, such as unexplained muscle weakness or paralysis, which can occur in some individuals with DID. Interdisciplinary collaboration between mental health professionals and neurologists is often necessary to avoid misdiagnosis[^12].
Listening for Distress Signals and Offering Grounding Support: Caregivers should be trained in grounding techniques, which can help reorient the individual to the present moment during a dissociative episode. Techniques like deep breathing, tactile objects, or sensory focus are particularly effective[^9].
Strategies to Avoid Triggering
1. Creating a Safe and Emotionally Secure Environment
Minimize Sensory and Emotional Overload: Avoid environments that are loud, chaotic, or emotionally charged. Ensuring that interactions are calm and free from potential emotional triggers is crucial. Additionally, providing a "safe space" or "safe object" can help anchor the individual in the present[^9][^13].
2. Predictability and Routine
Use of Shared Calendars and Anchoring Events: Maintaining a consistent routine is important. Providing access to a shared calendar or schedule can help the individual anticipate changes and reduce anxiety associated with the unknown. Incorporating "anchoring events," or predictable, regular activities, can further help maintain stability[^9][^13].
3. Respecting and Re-Evaluating Boundaries
Continuous Communication and Informed Consent: Boundaries may change over time as the individual’s alters interact and evolve. Regularly checking in and respecting these changing boundaries is key to maintaining trust and safety. Ensuring "informed consent" among all alters for certain activities or discussions is also crucial[^14].
4. Supportive Grounding Techniques
Personalized Techniques and Evidence-Based Methods: Different alters may respond to different grounding techniques. Having a range of strategies available, such as deep breathing, tactile objects, or visualization, ensures that support is tailored to the individual’s needs. The "5-4-3-2-1" grounding technique, which focuses on immediate sensory experiences, is particularly effective in reducing dissociative symptoms[^15].
5. Educating Yourself and the Support Network
Utilizing Reputable Resources: Educating yourself about DID is essential. Recommending specific books, reputable websites, and suggesting participation in support groups for caregivers can further enhance the support network’s effectiveness. The International Society for the Study of Trauma and Dissociation (ISSTD) offers resources and guidelines for understanding and treating DID[^16].
Neurobiological Aspects of DID
Recent research indicates that DID is associated with structural and functional changes in the brain. For instance, studies have shown that individuals with DID often have alterations in the hippocampus, amygdala, and prefrontal cortex—areas of the brain involved in memory, emotional regulation, and executive functioning[^17]. These neurobiological findings help explain the memory disturbances and emotional dysregulation commonly seen in DID.
Integration as a Treatment Goal
Integration, the process of merging separate identities into a unified self, is a controversial and complex goal in DID treatment. While some individuals with DID may pursue integration, others may focus on improving cooperation and communication between alters. This decision should be made collaboratively between the patient and therapist, taking into account the individual's preferences and therapeutic progress[^18].
Cultural and Societal Influences
Cultural factors significantly influence how DID is perceived and diagnosed. In some cultures, dissociative symptoms may be interpreted through spiritual or religious lenses, which can affect both the individual’s experience of the disorder and the approach to treatment[^19]. Understanding these cultural influences is crucial for providing culturally sensitive care.
Comorbid Conditions
DID often coexists with other mental health conditions such as depression, anxiety, PTSD, and borderline personality disorder. These comorbidities can complicate the diagnosis and treatment of DID. Effective treatment plans must address these comorbid conditions, often requiring an integrated approach involving multiple therapeutic modalities[^20].
Conclusion
Supporting someone with DID involves a commitment to creating a safe, predictable, and emotionally secure environment. By identifying and avoiding triggers, utilizing grounding techniques, respecting boundaries, and ensuring that support is informed by current best practices, caregivers and friends can significantly reduce the frequency of dissociative episodes and promote stability and safety for individuals with DID. Ongoing therapy, both individual and possibly group-based, remains essential in helping the person manage their condition and work towards integration or more harmonious coexistence of their alters.
Recommended Books on DID
"The Haunted Self: Structural Dissociation and the Treatment of Chronic Traumatization" by Onno van der Hart, Ellert R.S. Nijenhuis, and Kathy Steele
This book provides a comprehensive exploration of the theory of structural dissociation and offers detailed guidance on treating DID and related disorders.
"Coping with Trauma-Related Dissociation: Skills Training for Patients and Therapists" by Suzette Boon, Kathy Steele, and Onno van der Hart
A practical guide that offers skills training to help individuals with DID manage dissociation and related symptoms.
"Dissociative Identity Disorder: Theoretical and Treatment Controversies" edited by John L. Spira and Elizabeth K. Bowman
This book provides a balanced view of the theoretical and treatment controversies surrounding DID, making it an excellent resource for both professionals and interested readers.
4."Amongst Ourselves: A Self-Help Guide to Living with Dissociative Identity Disorder" by Tracy Alderman and Karen Marshall
A self-help guide written by therapists with experience in DID, offering practical advice and exercises for individuals with DID and their support networks.
These books provide in-depth knowledge and practical tools for understanding and managing Dissociative Identity Disorder, making them valuable resources for anyone looking to support someone with DID or further their own understanding of the condition.
References
[^1]: Ross, C. A. (2018). Dissociative Identity Disorder: Diagnosis, Clinical Features, and Treatment of Multiple Personality. John Wiley & Sons. [^2]: Brand, B. L., & Loewenstein, R. J. (2010). Dissociative Identity Disorder as a Complex Posttraumatic Stress Disorder. The Psychiatric Clinics of North America, 33(3), 509-530. [^3]: van der Hart, O., Nijenhuis, E. R. S., & Steele, K. (2006). The Haunted Self: Structural Dissociation and the Treatment of Chronic Traumatization. Norton. [^4]: International Society for the Study of Trauma and Dissociation (ISSTD). (2011). Guidelines for Treating Dissociative Identity Disorder in Adults, Third Revision. [^5]: DID Research. (n.d.). Substance Use and DID. Retrieved from https://did-research.org/treatment/issues/substance_use [^6]: Dell, P. F., & O'Neil, J. A. (Eds.). (2009). Dissociation and the Dissociative Disorders: DSM-V and Beyond. Routledge. [^7]: Boon, S., Steele, K., & van der Hart, O. (2011). Coping with Trauma-Related Dissociation: Skills Training for Patients and Therapists. W. W. Norton & Company. [^8]: DID Research. (n.d.). Identifying Triggers in DID. Retrieved from https://did-research.org/treatment/issues/triggers [^9]: Chu, J. A. (2011). Rebuilding Shattered Lives: Treating Complex PTSD and Dissociative Disorders. Wiley. [^10]: Kluft, R. P. (2003). Current Issues in Dissociative Identity Disorder. The Psychiatric Clinics of North America, 26(2), 257-292. [^11]: ISSTD. (2011). Guidelines for Treating Dissociative Identity Disorder in Adults, Third Revision. [^12]: Scaer, R. C. (2005). The Trauma Spectrum: Hidden Wounds and Human Resiliency. Norton. [^13]: DID Research. (n.d.). Supporting Someone with DID. Retrieved from https://did-research.org/caregivers/support [^14]: Herman, J. L. (2015). Trauma and Recovery: The Aftermath of Violence—From Domestic Abuse to Political Terror. Basic Books. [^15]: Levine, P. A. (2010). In an Unspoken Voice: How the Body Releases Trauma and Restores Goodness. North Atlantic Books. [^16]: ISSTD. (2011). Guidelines for Treating Dissociative Identity Disorder in Adults, Third Revision. [^17]: Reinders, A. A. T. S., Willemsen, A. T. M., den Boer, J. A., & Vos, H. P. J. (2014). Differences in the Brain Structure of Women with Dissociative Identity Disorder and Healthy Women. PLOS ONE, 9(6), e99888. [^18]: Steele, K., Boon, S., & van der Hart, O. (2017). Treating Trauma-Related Dissociation: A Practical, Integrative Approach. Norton. [^19]: Castillo, R. J. (1997). Culture and Dissociative Identity Disorder. The Psychiatric Clinics of North America, 20(3), 563-581. [^20]: Foote, B., Smolin, Y., Kaplan, M., Legatt, M. E., & Lipschitz, D. (2006). Dissociative Disorders and Suicidality in Psychiatric Outpatients. The Journal of Nervous and Mental Disease, 194(8), 599-601.
3 notes
·
View notes
Text
I have to share because now that everything is over and I’m fine - this picture makes me laugh
So last night I had the panic attacks of all panic attacks. Every panic symptom I’ve ever experienced all at once at the highest intensity I’ve ever experienced. And I’ve experienced many panic attacks in my long life. This was so intense I had moments of not knowing who or where I was and eventually the paramedics were called. They confirmed it was not a heart attack and that there wasn’t anything really they could do “unfortunately there really isn’t any community support for this type of thing”
Anyway after it was all said and done, the panic attack subsiding, I took out my phone to see what I looked like and took the picture. And now this morning now that I’m feeling better I’m looking at this picture just laughing because of dnp’s expressions.

“Aww you had a panic attack?? Your nervous system got so dysregulated you forgot who you were?? Aww you’ve got a traumatized brain?? Aww that sucks.”
2 notes
·
View notes
Text
You know what? I finally have an answer.
The biggest green flag, or the biggest red flag, for meeting new people (partners, friends, chosen family) when you have D.I.D./OSDD/PTSD/C-PTSD or any other trauma based disorder. It's green or red depending on a yes/no.
Green: They turn *off* survival mode. This may take a while, weeks to months to years of consistency. But if your nervous system & emotions recognize how safe this person is, enough to relax around them and NOT be hypervigilant, that's a major green flag. They make you comfortable, they make you feel safe, and for folks who also dissociate, you feel better and safer in reality with them (dissociating less often, less intensely, or not at all; able to exist in reality &/or enjoy reality). Your mind is quieter. You're able to catch and soothe your own spirals with facts about their patterns/consistencies. Your nervous system recharges and is more regulated around them. (Ironically, if you have PTSD/C-PTSD, this may also mean you get more nightmares &/or flashbacks than you did before, but that's because your body feels safe to remember/recover/heal now.)
Red: They turn *on* survival mode. This can mean they directly do this, by gaslighting you or yelling or actively abusing you. But it may be more subtle, more like something we just experienced where our system members were always blended/blurry when we spoke to them & we would be more dissociated and more anxious when talking to them. It may be louder anxiety, louder depression, they make you uncomfortable, they drain you, they make you hypervigilant....your nervous system is dysregulated around them. It may be difficult to recognize this if you're still in survival mode most of the time, but if they make it louder/worse, that's a red flag.
This applies to chosen family, friends, QPR partners, AND romantic/sexual partners. All of the above. The nervous system never lies.
~Nico
#our girlfriend taught us this#green flag#green flags#red flag#red flags#platonic relationships#romantic relationships#~Nico
29 notes
·
View notes
Text
Dating Someone With PTSD: What to Know and How to Navigate

If you are dating or in a relationship with someone who suffers from PTSD, you may be wondering how you can help or what you can expect. You already know there is much to love about your partner and that they are much more than their trauma. You also see how they are hurting and struggling. There is absolutely hope and there are effective ways to treat trauma and PTSD. Together, you can work towards more effectively managing symptoms and ultimately towards healing, so that a new sense of security and freedom can be found in the present.
PTSD is not just for war vets
Many times I have spoken to a therapy client about a PTSD or complex PTSD diagnosis fitting and been met with confusion partly because of the media tendency to exclusively depict PTSD as something that happens as a byproduct of war. In addition to experiences like rape or serious accidents, anything that someone experiences as deeply threatening can cause PTSD-like symptoms. Another working definition of trauma is too much too soon or too little for too long - when our coping skills and nervous systems are overwhelmed or we experience physical or emotional neglect.
What is traditional PTSD?
Traditional PTSD can arise from a single traumatic event or traumas that happen in a short amount of time.
What is complex PTSD?
Complex PTSD is caused by chronically experiencing traumas, oftentimes in childhood (for instance, consistently not getting physically or emotional needs met or experiencing physical or sexual abuse or ongoing bullying).
Individuals who have complex PTSD are sadly more susceptible to developing traditional PTSD later from single incident traumas, as they have less neural networks and experiences of safety internalized that can act as protective barriers.
PTSD symptoms may include
Avoidance
Your loved one is likely to avoid anything that may act as a trigger for their traumas. They may avoid talking about their traumas or any people, places, or activities that could serve as unwanted reminders. Substance use or constantly trying to stay busy and distracted can also be ways to avoid unwanted thoughts or feelings.
Intrusions
Your partner may have intrusive memories of the event, this can look like flashbacks, nightmares, or unwanted images that negatively impact their life. This could also look like somatic intrusions - where their bodies suddenly have a response that feels similarly to how they felt during the traumatic moment.
Thinking Patterns
If your partner is suffering from PTSD, they are likely to struggle with negative self-talk and a negative worldview generally. They may feel hopeless about the future. They could also struggle with memory, including not remembering many aspects of their trauma, as this can be an unconscious protective strategy. Trauma can lead to a sense of detachment from self and others and a sense of emotional numbness.
Reactivity
Someone with PTSD is likely to be easily startled, to be in a state of hyper-vigilance and on the lookout for danger. Your partner may be more irritable or quick to have an angry outburst.
All of these symptoms can be viewed through the lens of nervous system dysregulation, or being stuck in states of fight, flight, and freeze or moving between all three.
The gift of co-regulation
As a partner to someone suffering from PTSD, you have the ability to greatly help your partner through something called co-regulation. As social creatures, we look for cues of safety and danger from others, particularly from those we are most strongly attached to, typically our parents when we are kids and our romantic partners when we are adults. Helping your partner to find calm in their nervous systems through co-regulation can be incredibly healing.
Ways to co-regulate and help soothe your partner
● Use a calm, warm, and loving tone of voice
● Use gentle eye contact and smile at your partner
● Say simple and soothing statements to your partner that show you are with them to communicate safety
○ “I see you”
○ “I’m here for you”
○ “I hear you”
○ “I’m safe”
● Use reflective listening skills and validate your partner when they share with you. Ex: “So what you're saying is __________? Is that right? That must be really hard.” “Tell me more”
● Help your partner know that it is okay to have big feelings and that you can stay with them as they feel. Resisting or suppressing feelings usually only makes them bigger and more persistent. Feeling emotionally attuned to and seen can be incredibly calming. Avoid toxic positivity or minimizing your partner’s feelings.
● Use supportive touch if your partner is receptive to this. This may look like hand holding, hugging, cuddling, or back massages (check to make sure these aren’t triggers).
● Breathe slowly together as you hug or hold hands and face each other. Try and make your breaths match each other and have extra long exhales (try breathing in for 4, holding for 7, and breathing out for 8)
● Toss a ball back and forth together (this requires being in tune with one another and the repetition and focus can be soothing. This can also help someone to escape a flashback and return to the present.)
● Go on walks together
● Ask: “Is there anything you need from me right now? “How can I help?”
Learn your partner's triggers and boundaries
Communicate with your partner about what is triggering for them so that you can best support them in those moments (for instance parties where there are a lot of people). Understand if there are certain sexual or physical boundaries that could be triggering and respect any boundaries that your partner needs. Together, you may be able to soften those boundaries with exposure and with creating a new experience of safety in these moments, but this should be at the pace your partner is ready and highly collaborative. Maintain an open dialogue about what they may find helpful when triggered or when they experience flashbacks
Help to create a calm home environment
Predictability, stability, and routines can be calming and help your partner’s nervous system to feel more settled. This may mean doing rituals together, like cooking or eating together at a consistent time, having morning coffee together, or going on after work walks together. Don’t discount the impact that our senses can play in helping us to feel safe. Consider paying attention to your lighting, play calming music, light scented candles, and minimize clutter.
Putting your own oxygen mask on first
Dating and loving someone with PTSD can be hard. It is painful to know that our loved one is suffering and it can feel like a lot of pressure to fix it for them.
Know that there is only so much that you as their partner can do, especially if you are emotionally depleted or dysregulated yourself.
Take care of your own needs, work on learning self regulation skills and also confide in your partner and allow them to be a source of co-regulation for you when they are able to be. Lean on other supports in your life, like friends or family to help fill your own emotional cup up.
It may feel hard to reach your partner at times if they are numb or retreating. If could feel like you are walking on eggshells if their PTSD manifests in a quick temper. You can both have empathy and also not allow yourself to be mistreated. You may need to set your own boundaries at times - “please lower your voice, I can’t engage well with you when you're speaking like that to me. I will need to leave the room if you continue.”
You may benefit from your own therapy to help you more effectively navigate the stress and challenges that you may be facing in your relationship.
Encourage your partner to get professional trauma treatment
PTSD is serious and as much as your love can be a source of healing, your partner likely needs professional trauma treatment to truly get the relief they need from their trauma symptoms and to not spend their lives avoiding possible triggers.
As trauma lives in the nervous system and body, therapies that are body-based and not only cognitive are needed for PTSD treatment. EMDR is a gold standard treatment for trauma. Other modalities and approaches that can be highly effective, especially when incorporated with EMDR, include parts work, attachment-based therapy (particularly for childhood trauma), and somatic approaches. Therapy that incorporates mindfulness, acceptance of feelings, as well as calming exercises (like breathing strategies) are also helpful.
At Rise Healing Center, we incorporate all of these modalities and approaches, as we aim to treat trauma in the most effective way possible. If your partner lives in California, consider having them book a free consultation call to see if our practice might be a good fit for them.
3 notes
·
View notes
Text
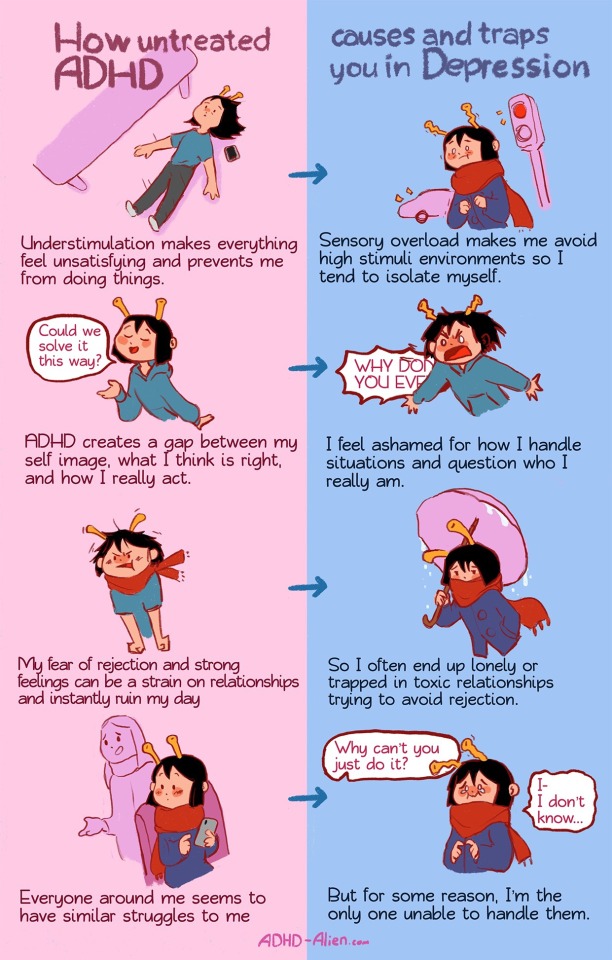
So. It's not specific strategies or anything (legally and ethically I **cannot**)
But I've always found that understanding not just the whats (so wonderfully reflected above in the comic) but also the whys/hows can help me cope better over all.
So let me see if I can take each of these one at a time.
Habits and patterns not sticking tends to stem from a few places: all or nothing thinking/perfectionism, executive dysfunction around working memory and task breakdown/management, and lack of internal bio-chemical reward responses at task initiation, just prior to task completion, and following task completion.
Some examples of how this can look:
All or nothing thinking says that if I can't "make a real dent" in a task, there's no point wasting my vanishingly rare energy and functioning on it, and that if I fall off of "keeping up on maintenance" then my routine is over rather than having been interruped, and lacking the greyspace of thought to "remember-believe" that I can return to the routine or even plan ahead for how to deal with interruptions and intermittent roadblocks as part of my routine. It also prevents me from being able to prioritize tasks in my brain, which is part of why tasks always seem to expand when I try to interact with them, leading me to get distracted or overwhelmed or otherwise wander off from my needs. And the reason my energy and functioning is so vanishingly rare, is that my brain is "understimulated" without the necessary function of reward responses, and my autonomic system is "overstimulated" without the ability to consistently regulate environmental, emotional, and social stressors.
Things that help are often things that help me intentionally mamage stressors and regulate my nervous system, as well as ways of introducing reward responses I do experience into my "task work" process to make up for the absence of them organically (part of this for me is medication, part is coping strategy, part is "grazing" food rather than eating separate sit down meals, etc). And what always always matters is that I take shame out of how I talk to and about myself. This feels silly at first, it really does. You feel ridiculous doing it, and then you kinda start shittalking the process and yourself and how you experience it and then one day you kinda look at that way you have of talking to yourself and realize it. It just sucks all the good out of your life. And you start to feel more comfortable with the new ways of talking to yourself. And you start to notice all the little shames that pile up throughout the day and how scary it is that letting go of that shame will mean things never get done but then somehow they do. And you realize the shame made it harder. Makes everything harder. Letting it go doesn't end mistakes or mishaps sure, but they somehow **genuinely** matter less? Not just to you, but in their impact and damage on your life.
Weirdly, it's not the understimulation (exactly) that causes dissatisfaction and mental/emotional restlessness! It's the autonomic hyperactivity (this is why we see similar expressions in our PTSD cousins). Calming our autonomic system can actually increase our overall satisfaction with life, hobbies, relationships, etc. It's something to do with how our body and brain are activated to direct and prioritize bodily resources when our nervous system dysregulates (the "hyperactive" in attention deficit hyperactivity disorder is referring to autonomic hyperactivity that causes chronic or irregular autonomic dysregulation - often experienced in ADHD expressions as intense emotional escalations that are hard to "come down from" and/or general psychological/physiological symptoms resulting from chronic stress). Folks with chronically hyperactive autonomic systems are prone to needing activity to regulate their autonomic system, rather than stillness or rest (although of course everyone needs a little of both, it's more a ratio thing I think) and so while we often think of "destressing" as "resting", that can actually be **stressing** for us instead. I do a lot of puttering around outside in the yard doing garden or animal stuff as "rest" or like fidget crafts like finger weaving or idle tap games while I listen to music or watch a show. The expression and release of autonomic hyperactivity is super soothing, and generally lets me feel more consistently relaxed. I do a lot of fun and weird diaphraghmatic breathing exercises (polyvagal approaches to autonomic regulation), a lot of low impact- movement based activities, and create "planned unstructured time" each day to just sort of putter around and follow my brain like a dog chasing a bone dangling in front of its face by a stick stuck in its own collar. I always do weird stuff. Not like. Interesting weird. Just weird. But it helps!
Building up skills around the general vibe of "this too shall pass, and here's how i can be kind to myself in the meantime" tends to be really valuable to those rejection sensitivity moments. I've got some great structured journal prompts I worked out with a therapist's help to "self reflect" on what feelings or needs are being communicated via the rejection experience, a self care plan to get through the parts I have less control/influence over and a processing/coping plan to get through the parts I can be more proactive about. I do a lot of checking in with my body and brain (I set timers/alarms for this) and use a lot of visual thought mapping and prompting in my environment (e.g. task step lists for cleaning a room pre-written on a whiteboard in that room, shared calendars, etc) to reduce the demand of routine/cyclical tasks on my executive functioning.
I have a reward jar!
The jar gets filled over time by routine task completion on a task by task basis, and when it's full, I get to buy new plants :)
It's a system I learned while training dogs (I know I know) and developing a "no failure" system of training for them. I realized I needed to change my own concept of/relationship to failure states. I really have a hard time coping with failure. And like. That'll probably always be true. But I can remove failure states from my life until they're rarer to encounter, so that overtime my sensitivity to it can scale down from lack of repeat trigger, and my coping skills for bleedthrough failure state emotional care and response can be more consistently effective.
One of the ways I do this is that I keep an extended documentation of things I "need to do" but I only allow myself to keep a max of 3 of them on my mind at once. And once I have interacted with one of these "priorities" to the extent of my comfort both physical and psychological, I put the task's respective reward marker in the jar. Tasks I struggle with the most get the biggest reward markers that take up the most space in the jar while the tasks I am more currently more consistent with get the smaller reward markers (think a silver dollar versus a dime).
I like getting my lil thing. I like how colorful my jar is. I like taking my little $10 allowance to the plant store like an excited 9yr old who has only just heard of allowances. I like having a plant to putter around and relax with. All positives in my book. Gotta find your own positives and way of removing failure states as an option.
It's not easy. And it's more of a process than a skillset? Because my relationship with myself and my environment is always changing, which means the way I need support in that environment is always changing even if the base kind of support needed doesn't. So I'm constantly adjusting and modulating and just. I dunno being really intentional about everything all the time. And it can suck sometimes, but other times its really really good, and mostly I'm just. Doing okay. Which is pretty cool :)
Anyway. I dunno if that's closure really, but I think it's worth more of us making our way through life acknowledging our experiences in ways that are mechanical and constructive when we can, rather than always hanging out in the self-deprecating space I think aot of us are prone to occupying due to our battles with shame. It's like building muscle memory. The more you do it, the easier and more reflexive it becomes.
The incorrect and negative beliefs we can get from years of negative feedback not knowing we have ADHD or how it affects our lives. While not everything is solely caused by ADHD, it can affect us and our comorbidities in many, many ways. Good news is, treating ADHD can do wonders for Anxiety and Depression!

85K notes
·
View notes
Text
tw: child torture, SA
I was raised by someone who catastrophized everything. Pfft, all my friends' fathers were gonna rape me according to her (which in retrospect is so funny coming from her) and that's why I could never hang out with them, but this treatment was localized to just me. I haven't really gotten the chance to talk about how not being able to escape her torture for a decade had long lasting effects of dysregulation on my nervous system. As a result, I had a really intense flight response like... "jump up and leave to another state with less than $200 to my name" flight response. I think I did it with $25 once. If that sounds intense, it is. In my defense, it was valid because abuse was escalating. If I wasn't scared of planes, I'd probably be living in Japan right now on some one way ticket shit. I should've did it honestly. Because fuck it.
I don't know how to describe it, but when you grow up with a pathological liar who is lying to you and exaggerating to control you, it's like your sense of judgment and trust and your ability to assess danger become so impaired and it works in extremes, or at least for me, it did. I feel like I experienced actual brainwashing sometimes.
It's taken years to separate fact from fiction, just alone being told my mother never loved me did so much damage. I remember she told me my mom was getting high again and that I wasn't gonna talk to her anymore and my mom was literally on fucking methadone for almost 20 years. It makes you nod out.
Then my mom died later that year from the same disease I have, that could've been caught early (but abusers avoid doctors because they're mandated reporters) and she swore that my mom overdosed even though it was just a cardiac arrest. It was unrelated to my mom's addiction because my mom was in recovery. Just lying for no reason. Like it's the chaos of it all. That woman hated me fr. Hated me over her man who wasn't her man anymore.
My internal monologue was fucked up for years because of her. I can't even really talk about how fucked up it was.
0 notes
Text

What Resistance & Self-Sabotage mean from the perspective of the dysregulated nervous system:
1. I FEEL UNSEEN AND UNHEARD.
We often respond to "resistance" by pushing through, shaming, or judging ourselves. But for a dysregulated system, resistance and self-sabotage are a cry for help.
The dysregulated system feels unseen, unheard, judged, shamed and unsupported, reenacting one of the original wounds you have experienced early in life of not being seen, heard and supported. Shifting your perspective from frustration to understanding allows you to meet your system where it is.
2. I HAVE NO ENERGY.
When your system resists or self-sabotages, it’s not an enemy—it’s depleted. Holding onto a state of dysregulation requires immense energy, leaving little for anything else. What your system truly needs is more safety and less pressure before it can do what the mind wants to do.
2. I'M OVERWHELMED BY SO MUCH PROCESSING I HAVE TO DO.
Resistance arises when your nervous system is overloaded with more than it can process. Whether mental, emotional, or sensory, the system will resist when it perceives the need for space and rest are unmet. This resistance is your system’s way of saying, “It’s too much—I need space, rest.”
3. I'M NOT SAFE ENOUGH
The nervous system cannot discriminate between "what is good" and "not good for you." Instead, it responds based on "Is this within my capacity?" "Is this familiar?" Anything unsafe, unfamiliar or too intense leads to resistance/self-sabotage.
Do you feel stuck, pressured or confused on your healing path? Do you feel you understand cognitively but not much changes in your body?
I created the audio practices inside The Self-Attunement Audio Toolkit to ease your way into an embodied healing experience.
You can access the toolkit via my Instagram/FB profile or comment the word Attuned, and I'll DM you the details.
Love,
Ally.
0 notes
Text
Hypothalamic Amenorrhea Recovery update no... 85?
I promise this isn’t just another “me me me” post about my recovery journey, but I feel like it’s important to share my experiences, especially in an area of women’s health that’s often under-documented. So here’s a quick update on my recovery journey.
It’s been almost two years since my menstrual cycle and hormone levels started normalizing, and wow, the changes are still unfolding. In the first year, I noticed shifts, but it’s only now, as I approach the two-year mark, that I’m experiencing some pretty intense transformations in my personality, emotions, and empathy. It seems like the more primal parts of my nervous system had to heal first before the secondary aspects could catch up.
Lately, I’ve been blown away by how different my social needs have become. For the past 12 years, when my hypothalamus went dormant, social interactions felt like a burden. I knew logically that I should have friends and care about them, but my nervous system saw people as exhausting and overwhelming. Now, however, I’m finding myself deeply invested in others’ lives, genuinely caring about what they’re going through in a way I never did before.
And here’s a real eye-opener: I’m discovering this intense desire to give love to others. During my period of dysregulation, I could only take—attention, sympathy, care. But now, I feel like I have this incredible backlog of love from the past 12 years that I just want to share. It’s like I want to shower people with affection—buying gifts, cooking their favorite meals, meeting up to hear about their day.
Navigating these new emotions at 30 has been challenging. It feels like I have the wisdom of an 80-year-old but the emotional and relational maturity of a 16-year-old who missed out on her wild teenage years. I’m still figuring out how to be “me” with people I care about, and it’s a bit of a learning curve. I’m more comfortable being a professional or a student, but being socially “me” is still a work in progress. To help with this, I’ve been joining clubs and making a point to attend more social events with people my age. It’s all part of the journey.
Thanks for following along with my recovery story. It’s been a wild ride, and I’m grateful for your support as I navigate these new emotional territories.
1 note
·
View note
Text
Expanding Your Window Of Tolerance

Expanding the “window of tolerance” in a relationship is a concept that often comes up in couples counseling. It can be useful in helping to slow down conflict escalation. Franklin, TN based therapist Barbara Wyer, LMFT explains that broadening the window can help couples foster a more secure connection. So what exactly is the window of tolerance, and how can it be expanded to benefit a relationship?
The Window Of Tolerance
The window of tolerance is a term used to describe an individual's optimal emotional zone. It’s essentially where we can remain reasonably calm, think more clearly and handle unexpected upsets. Inside the window of tolerance, we have the ability to regulate our emotional responses.
When we are too overwhelmed (hyperarousal), we move outside of this window, and it’s more difficult to control our responses to negative stimuli. In hyperarousal, we feel overly anxious, angry, or defensive. It is essentially when we get stuck in “fight or flight” mode.
Conversely in hypoarousal, we can feel disassociated and disconnected from ourselves or our partner. Hypoarousal looks like freeze, shut down, and we may feel hopeless and numb. Couples counseling in Franklin, TN, helps each partner identify ways to enlarge the window of tolerance to remain engaged in the relationship.
Past Trauma
It's important to understand that the window of tolerance is not solely affected by one's current surroundings or present relationship. It is also linked to a person’s past trauma. Partners who have experienced emotional neglect, physical abuse, or other harmful circumstances may have a smaller window of tolerance. Couples counseling in Franklin, TN, can also support each individual partner in healing from personal trauma and identify tools to expand their window of tolerance for more “breathing room.”
Relationship Benefits
During couples counseling sessions in Franklin, TN, partners can explore triggers and “raw spots” and safely work together to create a more connected relationship. Just a few benefits of widening the breadth of what we can and can’t actively cope with include:
Improved communication. As each partner's window of tolerance widens, they are more aptly able to regulate strong emotions during conflict. The logical part of the brain stays "online" so they can communicate more effectively and actively listen to each other, leading to more productive conversations.
Enhanced problem-solving. When partners stay in their window of tolerance, problem-solving abilities are greater. Partners can then work collaboratively to identify and overcome the emotional triggers in their relationship and within themselves.
Deeper connection. An important goals of couples counseling in Franklin, TN, is helping couples establish a deeper connection. When each partner can maintain emotional regulation during difficult conversations/moments, increased experiences of connecting on a deeper level helps to reinforce that being vulnerable with each other is safe.
Coping Strategies
The window of tolerance is fluid. It may expand or contract based on one's current state and life situation. Change begins with self-awareness, when we understand signals from our bodies that tell us that our nervous systems are on high alert.
A powerful way to minimize dysregulation is to learn how to identify emotions and sit with them instead of allowing them to threaten our mental, emotional, and physical regulation. By staying present in an emotionally charged experience rather than being completely overwhelmed by it, we can better control how we respond to each other.
Ultimately, couples counseling in Franklin, TN, is offered to support couples working to overcome the obstacles that keep them from maintaining a healthy, securely attached relationship. The Window of Tolerance is just one of many moving pieces that Barbara Wyer suggests must be addressed by couples wishing to maintain and strengthen their bond.
#Barbara Wyer#Couples Counseling#Couples Counseling Franklin TN#Marriage Counseling#Marriage Counseling Franklin TN
0 notes
Text
The Role of the Nervous System in Rebuilding Trust After Betrayal

Betrayal can shatter the foundation of trust in any relationship, leaving emotional scars that are often difficult to heal. Rebuilding trust after such an experience is not just a matter of willpower, betrayal can impact our nervous system’s capacity to feel fully safe and secure in our relationship.
Understanding Betrayal and the Nervous System
Because humans our deeply relational creatures with emotional needs, our relationships can deeply impact our sense of safety and security. This is reflected in the way that our nervous systems respond to betrayal. Infidelity, a particularly painful type of betrayal, has been found by one study to result in PTSD symptoms in up to 45.2% of unmarried adults who experienced a partner’s infidelity.
Our nervous system interprets and responds to the experience of betrayal as a threat to our emotional safety and relational security. This threat activates our limbic system, the part of the brain that regulates our fight/flight/freeze survival responses. This nervous system activation can manifest as heightened alertness, anxiety, and a readiness to protect oneself from further harm. This state can make it difficult to trust again, as the body remains on high alert, wary of potential threats. This response may be particularly intense and prolonged in individuals who already have a history of relational trauma, making the process of rebuilding trust even more challenging.
The Role of the Nervous System in Healing
Healing from betrayal and rebuilding trust involves calming the nervous system and re-establishing a sense of safety. In the context of relational betrayal, both partners play an important role in re-establishing a sense of emotional safety and supporting nervous system regulation.
Self-Regulation
Self-regulation is when we use internal or external resources to regulate. This can include mindfulness and meditation, breathing exercises, and grounding skills. Self-regulation requires that we build awareness of our internal experience so that we are able to identify and respond to our nervous system dysregulation when we are reminded of the betrayal.
Co-Regulation
As they begin rebuilding trust, individuals who experienced betrayal may begin to seek emotional support from their partners. Creating new, positive relational experiences can foster a sense of safety and reinforce nervous system regulation.
Consistency and Reliability
For trust to be rebuilt, there needs to be consistent, reliable behavior from the person who committed the betrayal. This consistency helps to reassure the nervous system that it is safe to trust again.
Open Communication
Honest and transparent communication is crucial. Transparency from the partner who committed the betrayal can support the betrayed partner in re-establishing a sense of predictability and trust and reduce anxiety. Open, empathetic communication from all partners also allows for greater opportunity to process emotions and fears as they arise and creates more opportunity for the couple to re-establish emotional connection, both of which are critical to rebuilding trust.
Attachment-Based Therapy
Therapy approaches such as Emotionally Focused Therapy (EFT) can help individuals understand and change their attachment patterns, promoting secure attachment and trust.
Rebuilding trust after a betrayal can feel like a monumental process. By calming the nervous system and creating new, positive relational experiences individuals can gradually restore trust and heal their relationships.
If you are looking for professional support around rebuilding trust in your relationship, schedule an appointment with me today. Please do not hesitate to reach out to us at Love Heal Grow to get in touch with our highly trained therapists.
0 notes
Text
Discover the Transformative Power of Somatic Therapy in Sydney
Welcome to Maxwell's Smart Health, where we specialize in offering cutting-edge somatic therapy services in Sydney. Our mission is to empower individuals to overcome trauma, reduce stress, and enhance their overall well-being through the powerful healing modality of somatic experiencing.
Somatic therapy is a holistic approach to healing that recognizes the intimate connection between the mind and body. Unlike traditional talk therapy, which primarily focuses on verbal communication, somatic therapy incorporates techniques that engage the body's physical sensations and movements to address emotional trauma and promote healing from within.
At Maxwell's Smart Health, our team of highly trained therapists utilizes somatic experiencing techniques to help clients release pent-up tension, regulate their nervous system, and restore balance to their body and mind. Whether you're struggling with the effects of past trauma, chronic stress, or anxiety, somatic therapy offers a safe and effective path to healing that honors your body's innate wisdom.
One of the key principles of Somatic Therapy Sydney is the understanding that traumatic experiences can become trapped in the body, leading to a wide range of physical and emotional symptoms. Through gentle and mindful exploration of bodily sensations, our therapists guide clients towards accessing and releasing these stored traumas, allowing for profound healing to occur at the deepest levels.
Our somatic therapy sessions are tailored to meet the unique needs of each individual client. Whether you're seeking relief from physical pain, emotional distress, or the effects of chronic stress, our therapists will work collaboratively with you to create a personalized treatment plan that addresses your specific concerns and goals.
During a somatic therapy session, you will be guided through a series of gentle exercises and mindful practices designed to help you reconnect with your body's innate ability to heal. Through breathwork, movement, and guided awareness, you will learn to listen to the subtle cues of your body and cultivate a greater sense of presence and self-awareness.
One of the key benefits of Somatic Therapy Sydney is its ability to promote nervous system regulation, allowing clients to experience a greater sense of calm and resilience in the face of life's challenges. By learning to regulate your nervous system responses, you can reduce the frequency and intensity of stress reactions, leading to improved overall health and well-being.
Somatic therapy is particularly effective for addressing a wide range of issues, including:
Trauma and PTSD
Anxiety and depression
Chronic pain
Relationship difficulties
Emotional dysregulation
Body image issues
And much more
At Maxwell's Smart Health, we believe that everyone deserves to live a life free from the burden of past trauma and chronic stress. Our somatic therapy services offer a safe and supportive space for you to explore your inner landscape, cultivate self-awareness, and unleash your body's natural healing potential.
If you're ready to embark on a journey of healing and transformation, we invite you to experience the power of somatic therapy at Maxwell's Smart Health. Contact us today to schedule your initial consultation and take the first step towards a brighter, more vibrant future. Your body knows the path to healing – let us help you find it.
0 notes
Text
Brainspotting Therapy Oakland Park, FL

Traumatic experiences lead to dysregulated nervous systems and brain dysfunction; any attempt to restore balance will be ineffective if the treatment does not address the issues that are stored within the nervous system and the mid-brain. Traditional talk therapies activate the part of the brain associated with higher order thinking. During cognitive-based approaches, information is processed in the session and is typically focused on questioning, processing, and analyzing; however this these types of therapies are limited to the executive processing systems of the neo-cortex. Brainspotting targets information in the mid-brain and nervous system, which is where trauma, emotional stress, and sensory experiences are stored.
What is Brainspotting?
Brainspotting is a liberating, non-invasive, holistic mind-body therapy that was developed by David Grand, Ph.D. The technique originated from EMDR (Eye Movement Desensitization and Reprocessing) which is also a therapeutic treatment used to alleviate distressing memories associated with trauma. Brainspotting is based on the premise that where you look, or gaze affects how you feel. The therapist may use a pen-shaped pointer to guide your eyes along your vision field to locate brainspots. Negative emotions are targeted as the individual focuses on the brainspots which allows the body to access and process unresolved accumulated toxic stress
What is a Brainspot?
“A Brainspot holds emotional experiences in memory form. It is the eye position which is related to the emotional activation of a traumatic or emotionally charged issue within the brain. This is most likely in the amygdala, the hippocampus, or the orbitofrontal cortex of the limbic system. A Brainspot is a located eye position, paired with externally observed and internally experienced reflexive responses.” – David Grand, Ph.D.
How will Brainspotting Help me heal from Trauma?
Accumulated toxic stress is typically stored in the nervous system when the traumatized person is not able to properly deal with the trauma that he or she has experienced due to lack of appropriate coping skills. Brainspotting stimulates the body’s natural ability to heal itself from trauma and restore dysregulated nervous system. Brainspotting also helps the body to release accumulated toxic stress and restore balance to within the system.
Your therapist will simultaneously facilitate the healing process by creating a safe, non-judgmental compassionate, space for you to develop a dual attuned therapeutic relationship. Brainspotting is used to target traumatic memories and physiological issues that is stored in the body and help the client to gain relief from the emotional distress. Bio-Lateral sounds are also used during Brainspotting sessions. Sound waves alternate back and forth across the audio field at a steady state negative experiences are triggered.
What is Brainspotting used to treat?
Brainspotting is effective for treating the following conditions:
Post-Traumatic Stress Disorder (PTSD)
Anxiety
ADHD
Anger
Substance Abuse Issues
Poor Impulse Control
Sport Performance Issues
Chronic Fatigue
Book Your Appointment and let us help you get back on track!
0 notes