#bowel cancer treatment
Explore tagged Tumblr posts
Text

What is Colorectal Cancer?
Colorectal cancer is a neoplastic disease of the large intestine from Ileo-cecal junction till the rectum. Unregulated growth of their cell lining lead to polyps and cancers.
The exact cause of colorectal cancer is not known, but several factors can increase risk of developing colorectal cancer.
Age: Elderly people are at risk of colorectal cancer. It is most common in people over 50 years of age.
Family history:��People with history of colorectal cancer in family (first degree relatives) are at increased risk.
Genetic factors: They are associated with some hereditary syndromes like lynch syndrome, familial Adenomatous polyposis, etc.
Lifestyle factors: A diet rich in red and processed meats and low in fibres or lacking fruits and vegetables can increase risk of colon cancer. Obesity, reduced physical activity, alcohol consumption or smoking also increase risk of colorectal cancer.
Medical Conditions: Certain medical conditions like inflammatory bowel disease (Crohn’s disease and ulcerative colitis) can increase the risk of colorectal cancer.
It is important to note that having one or more risk factors does not mean that a person will develop cancer. Regular screening tests such as stool occult blood and colonoscopy, can help to detect as well as prevent it at the early stage.
#Colorectal cancer#colon cancer#colorectal cancer#bowel cancer#sigmoid colon#rectal cancer#colorectal#stage 4 colon cancer#colon cancer treatment#adenocarcinoma colon#stage 4 bowel cancer#malignant neoplasm of colon#colon health#colorectal cancer treatment#bowel cancer treatment#the colon#colorectal carcinoma#rectal cancer treatment#rectal adenocarcinoma#sigmoid cancer#large intestine cancer#colonic neoplasm#rectal tumor#colon tumor#carcinoma colon#colorectal adenocarcinoma#large colon#cancer intestinal#colon rectum#sigmoid colon cancer
4 notes
·
View notes
Text

Are you experiencing blood in stool or black stools, changes in bowel movements, abdominal pain or cramping, unexplained weight loss, or fatigue and weakness? Don't wait! Consult Kaizen Gastro Care's experts.https://www.kaizengastrocare.com/
#Bowel cancer treatment#Bowel cancer specialist#Colorectal Cancer treatment#colorectal surgeon#gastroenterologist
0 notes
Text
youtube
#Colorectal cancer#colon cancer#rectal cancer#polyps#malignant tumors#colonoscopy#screening#early detection#chemotherapy#radiotherapy#immunotherapy#surgical treatment#biomarkers#genetic testing#risk factors#inflammatory bowel disease#family history#cancer prevention#survival rate#tumor progression.#Youtube
0 notes
Text
Treatment options for stage four bowel cancer
Explore the latest treatment options for stage four bowel cancer, from surgery to experimental therapies, designed to extend life and improve overall well-being.
0 notes
Text
4 Warning Signs of Colon Cancer You Should NEVER Ignore
#ColonCancer #CancerAwareness #HealthTips #EarlyDetection #CancerPrevention #HealthScreening #ImmunoOncology #CancerResearch #HealthyLiving #KnowTheSigns #CancerSymptoms #ProactiveHealth #ColonHealth #CancerScreening #HealthEducation #StayInformed #FarehaJamal #BioNTech #MedicalAdvice #FamilyHealth #WellnessJourney #HealthMatters #CancerTreatment #HealthyHabits #PreventiveCare
Hey there! Let’s talk about something important today—colon cancer. I know, it’s not the most glamorous topic, but it’s one of those things we really need to pay attention to, especially because it can be sneaky. Many cases of colon cancer don’t show symptoms early on, which is why knowing the warning signs is so crucial. I recently had a chat with Dr. Fareha Jamal, a Doctor of Pharmacy and…
#abdominal pain#American Cancer Society#BioNTech#blood in stool#bowel habits#cancer awareness#cancer prevention#cancer research#cancer risk factors#cancer screening#cancer screening guidelines#cancer treatment#cell binding assays#Colon Cancer#colon cancer symptoms#colorectal cancer#early detection of colon cancer#family history of cancer#Fareha Jamal#health tips#Healthy lifestyle#high-content screening#immuno-oncology#Mayo Clinic#proactive health management#unexplained weight loss#warning signs of colon cancer
0 notes
Text
I wonfer if the other cats get upset with how much the husband and I praise DC for eating all her food or if they sideeye us for not complaining or scolding her when we clean up her poop off the floor.
#and if they do then shrug emoji#sorry boys the old girl's dying of bowel cancer#dying kitties get special treatment
1 note
·
View note
Text
Colorectal Cancer: Important Types, Risk Factors, Treatment, And Prevention
Colorectal Cancer: Important Types, Risk Factors, Treatment, And PreventionIntroductionWhat is Colorectal Cancer?Types of Colorectal Cancer Adenocarcinomas Carcinoid Tumors Gastrointestinal Stromal Tumors (GISTs) Lymphomas SarcomasRisk Factors for Colorectal Cancer Age and Gender Family History Personal Medical History Lifestyle Factors Inflammatory Bowel Disease (IBD)Symptoms and Early Detection…

View On WordPress
#Adenocarcinomas#Bowel Cancer#Carcinoid Tumors#Chemotherapy for Colorectal Cancer#Colon Cancer#Colorectal Cancer#Colorectal Cancer Awareness#Colorectal Cancer Diagnosis#Colorectal Cancer Prevention#Colorectal Cancer Screening#Colorectal Cancer Staging#Colorectal Cancer Surgery#Colorectal Cancer Treatment#Early Detection of Colorectal Cancer#Gastrointestinal Stromal Tumors#Genetic Risk of Colorectal Cancer#Healthy Diet for Colorectal Cancer#Immunotherapy for Colorectal Cancer#Lymphomas#Radiation Therapy for Colorectal Cancer#Rectal Cancer#Risk Factors for Colorectal Cancer#Sarcomas#Symptoms of Colorectal Cancer#Targeted Therapy for Colorectal Cancer
0 notes
Text
Global Small Bowel Cancer Treatment Market Size & share Forecast 2031.

Global Small Bowel Cancer Treatment Market Size, Share & Trend Analysis- By Treatment Type, By Cancer Type, By End-user, By Drug Class, Regional Outlook, Competitive Tactics, and Segment Forecast to 2031
0 notes
Text
Delicious Syrniki! 😋💕 (first solid food I was able to have since 2023)

Screw it. I made and had those a few weeks ago.
Sharing this picture and moment is a big deal & emotional for me, because it's the first solid food I've eaten in 19 months.
You may think that's impossible. Well, it's not. Let me tell you why:
🏥 I've been struggling with an autoimmune condition (MAS, among them severe, chronic inflammatory bowel disease) since years & couldn't digest anything anymore since August/September 2023 after it got worse due to massive adrenaline & cortisol overproduction in my body; hormones that are notorious for causing autoimmune diseases & making them flare/worsen significantly. 💊 ❄️ In fall/winter 2023 doctors informed me my condition has become so severe it's considered terminal & I started to require palliative care in the shape of parenteral feeding (= bypassing the digestive tract) via an intravenous port & nutrient/fat/glucose solutions being dripped into me to keep me alive a little longer & try to see if any treatment still works, after about 2 years of almost exclusively being able to have "space food" - high caloric drinks to sustain me - along with starting to receive high doses of tranquilizing pain killers & immune blockers, which were helpful, but have severe side effects. 🛌 ☢️ In March 2024 I was then diagnosed with stomach & duodenal cancer as a result to how severely the disease had escalated. 🤕



More of the story below the cut. Otherwise please just appreciate the delicious food. 🌈🥞✨
Bottom line is, I was very reluctant to share this, bc I'm very emotional about this. I cried while eating those, bc tasting something sweet, creamy, delicious & warm on my tongue has been something I couldn't experience in so long & there was a real risk for me to die without ever being able to taste something nice again. 🙈🥲 It was a bit too ambitious, so for now I'm back to broth and space food and the occasional spelt porridge. But here's to celebrating a huge win in my life! 💗🌼🌈



On with the story of how all this developed: By May 2024 I was being treated with 3x the regular amount of blockers to regulate these stress hormones, but it didn't do much, since the underlying reasons for them being as high were nothing I could resolve, however hard I tried. There were many additional health issues I went through and in parts am still going through in this time as well, that put me in critical condition, such as a bone inflammation caused by an infection merging with arthritis in my foot, resulting in a debridement surgery in September 2023, phlebitis as a result to wearing the intravenous parenteral port for so long in June 2024; having sinusitis for months, as a result from a lacrimal gland inflammation due to too much crying, inflammation in many organs connected to the digestive system (autoimmune pancreatitis, hepatitis, cholecystitis etc.) due to the intestinal and stomach inflammation and ulcers spreading and severe heart problems, due to a preexisting heart condition being worsened by the anesthesia during treatments, the physical weakness all this caused, as well as severe and ongoing stress that persisted daily due to a social situation over the course of 14 months. Eventually the underlying situation lessened a bit and I felt confident that my upcoming cancer surgeries & treatments would go well and finally bring the anticipated relieve I've waited for for so long with the necessary peace to prepare, go through all this and recover, before a final escalation happened, just days before the long-planned hospital stay for surgeries to cauterize the ulcers and remove cancerous growths in my digestive tract started on 16th September 2024. It continued to escalate in the background throughout this time.
But anyways, in early October 2024 I finally was able to start chemotherapy, away from all this. It works well so far, I'm doing better since, the hormonal overproduction has lessened somewhat & my mental health has stabilized somewhat. I'm still getting IVs, because my ability to digest is still inconsistent and there's been some throwbacks due to side effects of the chemo. And after over a year of no digestive function it was also questionable whether my system would be able to pick up work again at all or whether I'd simply kick the bucket and starve to death eventually. The IV nutrition was already a slow version of that, I lost more than half my weight since September '23, I barely have any muscles left and need to recover from all that and mental health damage... The bottom line is, 2024 and a large chunk of 2023 were really bad and thankfully 2025 looks significantly better. There's finally a treatment that works a bit and helps my health improve, although chemo mostly kills the diseased tissue and regrowing fresh one takes time, regeneration will never be flawlessly possible and there will be a lot of permanently impairments and scarred tissue inside of me. And the places I'm in and people I surrounded myself with are respectful of this and I feel at peace, loved and confident once more.
🌈🌼✨ But after all the hardships, I have a positive thing to share today 🌈🌼✨
I had these delicious thingies up there a few weeks ago, sharing them with a kind neighbour who supported me with when I needed help bc of mobility issues and other problems throughout this time. I actually made a post mentioning it but was so was reluctant to share and celebrate this milestone, because I'm very emotional about this whole journey, but it is such a huge win for me!!!!! 😭 I already said it above, but I actually cried while eating this, just because tasting something sweet and creamy and delicious and warm on my tongue and in my tummy that is so much in pain the entire time, is such a comforting sensation and has been a pleasure denied to me for so so many months and also because there was a serious risk for me to die while all these horrible things were happening and for months I didn't think that I'd ever live to taste something nice again. 💔 I'm still here every day, feeling like "oh gods, I'm still alive, I can't believe I'm still alive and get to experience goodness". 😖😭🫂 I went a bit too ambitious with trying these and still got symptoms again and had to go back to space food, broth and some low acidic fruit. Taking it slow rn. But you know. It's a progress. Healing is messy and not gradual. There is no such thing as perfection in human beings. Decency and trying, sometimes failing, but always staying in motion is quite enough. 🌼🌌
#food#the chthonic originals#foodie#food photography#foodpics#baking#dessert#cuisine#slavic#slavic cuisine#russian cuisine#polish cuisine#syrniki#pancakes#cheesecake#spilled thoughts#mental health#chronic illness#terminal illness#psychology#physical health#life#journal entry#healing#healing journey#body healing#disability#physical disability#cottage core#cooking
21 notes
·
View notes
Note
Good morning! I have a question. When I look up info about vitamin D, I come across many claims that people generally don't get enough of it. In a recent episode of Maintenance Phase, however, the hosts called it a "scam" or overblown, at least (I don't remember the exact wording). So, like, what's the deal with vitamin D? Do Americans get enough of it?
Probably, mostly. At the very least, people should be tested before starting repletion. It probably has a role in osteoporosis treatment and prevention, BUT how much to take and what form and when is HOTLY debated and frequently conclusions are changing.
Just to take you on a spin through the most recent Cochrane reviews (THESE ARE NOT SINGLE STUDIES, in case any of the research-naive out there want to get pissy about them; look up what a Cochrane review actually is before trying to shit on it; also note that I did NOT say this will cover every fucking person and every hypothetical they can come up with, jesus CHRIST):
No role for vitamin D in asthma
Insufficient evidence to recommend it in sickle cell
Raising vitamin D levels in cystic fibrosis patients is not beneficial
No evidence of benefit of vitamin D in MS
Supplementing vitamin D in pregnancy may have small benefits but also risk of harms
No clinically significant benefit from vitamin D supplementation in chronic pain
Insufficient data on vitamin D in inflammatory bowel disease, but no evidence of benefit
No evidence of benefit of vitamin D supplementation in liver disease
Vitamin D does not appear to prevent cancer in general population
No evidence for benefit in supplementation of vitamin D in premenopausal women to prevent bone density loss
Possible small mortality benefit of D3, but not D2, in elderly patients, but also increased risk of kidney stones and hypercalcemia
Vitamin D alone ineffective, but combined with calcium may be effective, in preventing bone fractures in older adults
Insufficient evidence for vitamin D improving COVID-19 outcomes
Now, vitamin D plus calcium in people who have post-menopausal bone density loss does seem to prevent fractures. This is why doctors routinely recommend it. However, dosage and formulation are still debated as data are insufficient, and uncertainty still large.
So, do you need to supplement? Probably not. There is some fairly weak evidence that vitamin D supplementation may help with depression, but I would argue that it's going to be most relevant in people with pre-existing deficiencies, which Medicare is just hellbent on not letting me test for anymore. They've narrowed the coverage codes for testing so now even know vitamin D deficiency isn't considered a good enough reason to test. So Medicare has very clearly decided it's not relevant, for whatever that's worth, I spit on their graves, etc. Of course, then you get into the question of what counts as a deficiency, which we also really don't know.
And to be clear, I wasn't looking through the Cochrane review results with an angle--those are most of the first page of search results on their site, with the only one skipped being similar to another one I mentioned, and I stopped when I got bored. These should not be paywalled, as I am not logged into anything and I can read it all, so try clicking the side menu on the right if you have trouble getting into the weeds.
If anything, running through this little exercise has made me less likely to recommend vitamin D supplementation, so do with that what you will.
59 notes
·
View notes
Text
In a medical first, scientists have hindered the growth of bowel cancers in mice by harnessing immune cells in the large intestine. One of the most exciting new cancer treatments is immunotherapy, which works by training the body's immune system to identify and destroy cancer cells. However, most current immunotherapies only benefit a small minority of patients with bowel cancer – fewer than 10 percent. "We have discovered that an important group of immune cells in the large bowel – gamma delta T cells – are crucial to preventing bowel cancer," says immunologist Lisa Mielke from the Olivia Newton-John Cancer Research Institute at La Trobe University in Australia.
Continue Reading.
100 notes
·
View notes
Text
PROSTATE CANCER AWARENESS
Prostate cancer is one of the most common cancers in men, but detecting it early is a game changer.
I'll explain all you need to know about this condition in simple terms, I try to answer some famous questions you may have..
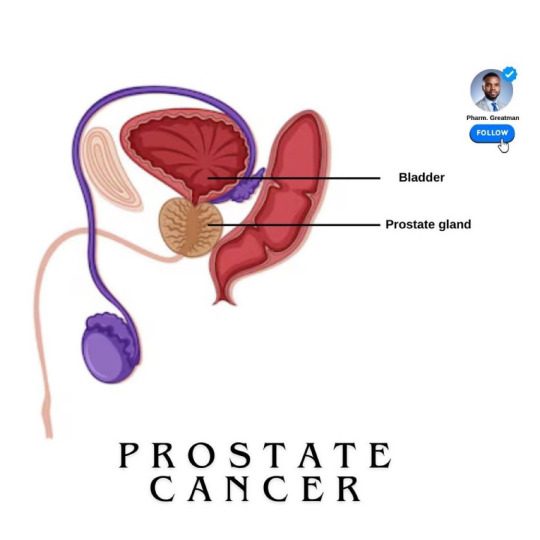
What is Prostate cancer?
It is a type of cancer that begins in the prostate gland The prostate gland is part of the male reproductive system.
It is located below the bladder. This gland is responsible for producing the fluid that nourishes and transports sperm.
Prostate cancer is one of the most common cancers as they age.

What are the risk factors?
The exact cause of prostate cancer is unknown, but the risk factors are certain, they include:
- Age is a major risk factor for prostate cancer, with most cases occurring in men over 50.
- family history; as men with close relatives who had prostate cancer are at a higher risk. Having a father or brother with prostate cancer more than doubles a man’s risk of developing this disease.
- there are changes that could occur in your genes that can also increase your risk.
- men of African descent face an even greater risk and are more likely to be diagnosed at an advanced stage
A study showed that 1 in 4 black men will have prostate cancer in their lifetime, scary

Stages of Prostate cancer
Based on how far it has spread, it is classified into stages from stage I to IV
- Stage I is early and confined to the prostate, while Stage IV indicates the cancer has spread to other parts of the body, like the bones
Knowing the stage of cancer helps your doctor determine the best way to treat
Can regular sexual intercourse prevent prostate cancer, or prostate issues?
Important to state that “regular ejaculation alone is not a guaranteed preventive measure for prostate cancer”
Some studies suggested that regular ejaculation, whether through sex, masturbation, or nocturnal emissions, may reduce the risk of prostate cancer.
Research, including a notable study by Harvard University, found that men who ejaculated 21 or more times per month had a 20% lower risk of prostate cancer than those who ejaculated less frequently. The reasons are not fully understood, possibly that frequent ejaculation might help clear potential toxins or reduce inflammation in the prostate.
However, while this association exists, it’s still under investigation.
More evidence is needed… for example, a study in 2008 revealed that frequent sex in younger men increases prostate cancer risk compared to older men…

Stay active and monitor your health with Inspire 3, a tracker that supports prostate health by encouraging regular activity, reducing stress, improving sleep, and tracking key wellness metrics.
~~~~
Treatment Options
It depends on the stage of cancer and overall health. Options include:
- monitoring the cancer (active surveillance) - surgery to remove the prostate - radiation to destroy cancer cells - hormone therapy to reduce hormones that fuel cancer growth, and chemotherapy.
Treatments for prostate cancer can lead to side effects like difficulty controlling urine, erectile dysfunction, and bowel issues.
They must be communicated to patients beforehand
11 notes
·
View notes
Text

SOURCE
Elliot Pfebve, 55, is the first patient in England treated with a personalized vaccine for bowel cancer at Birmingham’s Queen Elizabeth Hospital.
Thousands more patients will receive the experimental vaccine, not as a cure but to target remaining cancer cells after treatment.
The NHS will match patients to clinical trials for their specific tumors via the Cancer Vaccine Launch Pad, using mRNA technology to train immune systems to combat cancer cells.
#sulemio news#sulemio#suletta mercury#miorine rembran#g-witch#g witch#uk news#uk nhs#uk national health service#cancer vaccine#cancer#english cancer patients#nhs cancer patients
26 notes
·
View notes
Text


The rapid advance of Katie's rectal cancer was marked by a series of life altering indignities. She went to the doctor because she noticed she was bleeding out of her butt and, after the diagnosis of Stage IV rectal cancer with limited metastases was confirmed, spent the next 7 months with a team of oncologists waging, as she darkly called it, "the war on ass cancer."
She started concurrent radiation and chemo while still working her job as a receptionist, which in reality meant showing up to her job wearing a Depends and struggling with the alternating side effects of agonizing constipation and never ending diarrhea on the company toilet.
By the time she checked herself into the hospital for intrarectal brachytherapy she could feel the tumor burning almost constantly and was having to use heavy duty opioids to control her pain enough to get out of bed. That lovely treatment involved a really painful prep enema -- because definitely what you want in your irradiated anus is enema solution! -- followed by the insertion of a catheter directly into the tumor to deliver a low dose of radiation over several days. She had to lie there, immobile and too drug resistant at this point for the PCA to do much more than take the edge off, and feel the tumor in her butt being burned with radiation.
[Because America sucks she had to go back to work two days later. Her boss found her unconscious on the bathroom floor, face down with her bloody, swollen, shit covered ass mooning him, after she'd fainted from the pain of trying to take a bowel movement. That was the day the prick finally approved her long term medical leave.]
Through it all -- and all of it was terrible -- the thing that drove Katie absolutely up the wall was what she later learned was called tenesmus, a common rectal cancer symptom.
From about 3 weeks before her diagnosis through her entire treatment regimen, every single minute, she felt like she needed to shit. It caused a few accidents, of course, because she never knew when she truly truly needed to empty her bowels, but shitting herself had become an almost daily occurrence and she employed her dark humor to cope by buying all new brown towels, bathroom rugs, and underwear. But the psychological effect of needing to poop every single second of every day for seven months felt like one of those "would you rather games." Would you rather have your toenails ripped out every day or feel like you need to shit every second of every day? Katie thought, with that she knew now, she'd definitely choose the toenails.
Two months after the intrarectal brachytherapy her oncologist sat her down and told her the less aggressive treatments hadn't worked as they had hoped. Her only hope for beating the cancer was a posterior pelvic exenteration. She sat, shell shocked, as he explained how her rectum would be removed and a colostomy created to remove waste into a bag. He wants to excise her vagina too, just to be safe, but thinks he'll be able to spare her bladder. The surgery will take about 12 hours and she'll be in the hospital for up to a month after to begin the arduous recovery.
She walks out of the office with a date on a card to have her ass and vagina removed. She and her wife, Violet, sit in the car in silence for a long time, pondering the future. They clutch hands, both crying silently. Finally Katie clears her throat and smiles, a hint of dark humor in her eyes.
"Well, at least without an ass I won't feel like I need to shit all the time!"
Katie spends the next several weeks going to imaging appointments, meeting with counselors, and preparing for the major surgery. On the big day she is nervous, of course, but so worn down from the months of pain and fatigue from the cancer and the treatments that she's ready for it to just happen. Go to sleep and let the doctors take care of her for a while. Her main fear is waking up in uncontrollable pain but they reassure her she will have an epidural and the anesthesia team will aggressively control her post-surgical pain.
After 13 hours the lead surgeon comes to find Violet in the waiting room to brief her about her wife's condition.
"Katie made it through the surgery. She's stable and being monitored in the ICU. It was grueling but we accomplished what we needed to in order to give her the best shot possible to beat the cancer. She's still on the ventilator, which is not uncommon after such a long procedure. She’s conscious and aware, but we’re managing some significant pain, which is also expected after a surgery of this magnitude. Right now, her pain is not as well-controlled as we’d like, but we’re actively working to get her some relief. It’s going to take some time to fine-tune her medications and ensure she’s as comfortable as possible.”
It's clear when Violet is finally allowed to see her wife that "comfortable" is a very long way off at this point. Katie's wrists are restrained -- a nurse tells her she was trying to pull out the endotracheal tube -- and she's naked and exposed from the waist down, showing off the horror show of her drains and incisions. Violet lets out a cry as she looks to where her wife's vagina and ass used to be and sees the lines of staples that have made her null. There's a bag of fecal matter resting on her bloated belly, attached to a swollen stoma.
But the most heartbreaking thing to see if Katie's red, puffed face crunched up in agony, tears streaming down her cheeks, a thick endotracheal tube down her throat secured by medical tape on her lips. Violet approaches and Katie's dull, glassy eyes follow her. She can see clearly she's pleading for her wife to do something about the excruciating pain in her abdomen and pelvis.
Violet looks up, alarmed, at the ICU nurse. "She's supposed to have an epidural. Why is she in this much pain? You have to do something!"
The nurse nods somberly. "I assure you we're working on it. Your wife was already on very heavy pain killers to deal with the effects of cancer treatment so she's become pretty resistant. We're doing everything we can to get her pain under control."
Violet is loathe to accept that but the anesthesia team is in and out, clearly trying to address her wife's pain. All she can do is stroke Katie's hair, wipe her tears, and reassure her she's not alone as she endures the most painful and terrifying hours of her life.
Finally a cocktail of fentanyl and ketamine are able to provide Katie enough relief that she is able to be extubated. Even will the strong drugs coursing through her system she's incoherent for hours, still in enough pain that she groans under her breath almost constantly, occasionally crying out "my belly" or "oh God I hurt!"
Violet stops Katie's doctor at one point and asks him what her wife is feeling as she writhes in the bed. He explains she's likely experiencing sharp burning sensations from the incisions and a deep, aching pressure radiating through her pelvis and abdomen from the trauma of the cavity clearance. From the way she keeps grabbing her belly, he thinks she's likely experiencing cramps in her stoma and, from the way she keeps trying to move her hips and then screaming from the pain it causes, extreme soreness from the way she was positioned for so long.
Sixteen hours after surgery Katie opens her eyes and Violet can tell she's really there, groggy and trembling in excruciating pain but, at last, coherent. She opens her mouth, closes it, and opens it again before letting out a pained sob. Suddenly she's crying again and Violet braces herself for whatever her wife is about to say.
Violet's been preparing for this moment, has a big speech planned that will reassure her beloved wife she loves her no matter what her lower body looks like and they will get through this together. She just needs Katie to give her an opening.
Katie's still sputtering, trying to get words out of her pain and anesthesia addled brain. She looks so miserable and affronted, tears running down her red, bloated face.
"They cut my ass off and I still feel like I need to shit!"
#medfet#surgery fet#anesthesia#hospital#surgery#medical kink#dark medfet#dark#posterior pelvic exenteration
16 notes
·
View notes
Text
https://www.telegraph.co.uk/health-fitness/conditions/cancer/the-little-known-cancer-thats-linked-to-the-gut/
“The surge in cases of cancer in the under-50s has made many of us worry, with bowel, breast and lung cancers among those increasing most rapidly. But what is more surprising is that rates of aggressive gallbladder cancer have risen even more sharply, affecting many more women than men, particularly those who have had children. It’s also more likely in those who have suffered from the common problem of gallstones.
The figures are alarming, with cases having doubled in British people aged between 24 and 49 in the past three decades, according to Cancer Research UK. But the good news is that there are measures you can take to limit the risk of the disease, through changes to your diet and lifestyle.
Here, our experts explain what exactly the cancer is, the reasons it is spiking in younger people and what we can do to increase our chances of avoiding it.
What is gallbladder cancer?
The gallbladder is an apple-sized organ near the liver and is primarily responsible for storing bile, a substance produced by the liver and used by the body to break down the fats we eat.
Thousands of years ago, humans might have eaten one big meal every few days and “we might have needed that extra boost of bile to help us digest it, if the liver couldn’t produce it fast enough,” says Dr Anita Balakrishnan, a consultant hepatopancreatobiliary (HPB) surgeon at Addenbrooke’s Hospital and an associate lecturer at the University of Cambridge..
“The gallbladder is a vestigial organ, like the appendix – now we don’t really need it for normal digestion, and sometimes it causes trouble.’”
Cancer occurs when healthy cells in the gallbladder develop genetic mutations that cause them to grow and multiply out of control. Just over 1,000 cases have been diagnosed in the UK each year, equivalent to about three per day and, “sadly, it’s an aggressive cancer,” says Dr Balakrishnan.
What are the risk factors?
According to Cancer Research UK, women account for 71 per cent of cases. In women who have given birth, particularly those who have had five or more children, the risk is increased.
The reason for this is not fully known, but women are two to three times more likely to suffer from gallstones, which are a major risk factor for gallbladder cancer. Oestrogen can increase cholesterol levels in bile and decrease gallbladder contractions, which can lead crystals to form in the bile and create stones. During pregnancy, the gallbladder also grows in volume.
“Having gallstones doesn’t necessarily mean you’ll get cancer, but they cause inflammation of the gallbladder, which puts people at a higher risk,” says Mr Shahid Farid, a consultant surgeon with a specialism in gallbladder surgery at Nuffield Health Leeds Hospital.
People with a family history of gallbladder cancer are five times more likely to develop the disease, and it is more common in people of Asian descent.
Smoking and obesity also increase the risk, with the rise in obesity since the mid-1990s believed to be a major factor in the increase in cancer among younger people, in particular.
What are the main symptoms, treatment and survival rate?
Unfortunately, gallbladder cancer is often a silent disease which becomes symptomatic only in its later stages.
“Any symptoms people have are usually non-specific, such as tiredness and perhaps some abdominal discomfort,” says Mr Farid.
Eventually, symptoms can include jaundice, pain in the upper right abdomen, weight loss, nausea and vomiting. “By that stage, it has usually grown beyond the gallbladder and is at an advanced stage,” he says.
It is often detected by chance during operations, for instance to remove gallstones, and if it is contained within the gallbladder, the five-year survival rate is 60-70 per cent. If it has spread to local tissues or lymph nodes, survival rates are almost 30 per cent, while if it has spread to more distant areas, rates are under 5 per cent.
If possible, treatment involves surgery, along with chemotherapy.
What can we do to minimise our risk?
1. Maintain a healthy weight
Being overweight and obese is the second biggest cause of cancer in the UK, after smoking. Several studies have found a link between an increased risk of gallbladder cancer and a BMI of over 25, with the World Cancer Research Fund stating that the risk increases by 25 per cent per 5 kg/m2 increase in BMI.
One recent Norwegian study found a concerning 47 per cent increased risk in women per 5 kg/m2 increase in BMI, while the increased risk in men was smaller and not statistically significant. It also showed a decreased survival rate for overweight and obese women with gallbladder cancer.
“Eating a healthy diet and staying within a healthy BMI range will help avoid gallbladder cancer,” says Dr Balakrishnan. “Giving up smoking and keeping alcohol consumption under recommended limits is also vital.”
2. Look after your microbiome
In recent years, scientists have increasingly focused on the microbiome, the ecosystem of bacteria which populates the gut, when searching for causes of the increase in early-onset cancers.
“Research into the influence of the microbiome on cancers including gallbladder cancer is still in its early days, but it’s only logical that it plays a part,” says Mr Farid. “Our microbiome can contribute to inflammation, and that can predispose us to cancer.”
A Chinese study from 2023 investigated the microbiome of patients with biliary tract cancers, of which gallbladder cancer is one. It found patients with the disease had increased levels of the Enterobacteriacae bacteria, and decreased levels of others including Clostridia, suggesting an imbalance. Both are associated with inflammation.
We can boost the diversity and good bacteria in our microbiome with fermented foods such as kefir, sauerkraut and kimchi, and prebiotic foods like mushrooms, onions, garlic, asparagus, leeks and apples, which feed the bacteria in our gut.
Good bacteria such as Clostridia can naturally be found in food such as vegetables, while high-fibre foods such as fruit, wholegrains and nuts will also nurture the microbiome.
3. Avoid fried, fatty foods and sugary drinks
The link between different types of diet and higher rates of gallbladder cancer is still being researched, but some studies have highlighted certain principles by which it’s best to live.
Eating too many fatty and fried foods have been linked to an increased chance of getting the disease because they raise cholesterol which is linked to gallstones, which are in turn strongly linked to gallbladder cancer.
Red meat, and particularly processed meat containing nitrates, is also associated with a higher risk, so cutting down to 455g of cooked lean red meat per week is recommended.
Drinking sugar-sweetened and artificially sweetened beverages has been shown to double the risk of gallbladder cancer when individuals drank 400ml or more per day. This is thought to be because increased sugar consumption is linked to a higher BMI, and also to Type 2 diabetes, which increases the risk of cancer.
Ultra-processed foods (UPFs) are linked to a higher incidence of all cancers, and researchers believe they may be a major driver of the increase in cancers among under-50s. “Reducing the amount you consume and eating unprocessed food where possible is best,” says Mr Farid.
4. Eat the DASH diet
One Swedish study revealed that two types of healthy diet are associated with a lower risk. One is the Dietary Approach to Stop Hypertension, or DASH, which includes fruits, vegetables, whole grains, low-fat dairy, and lean protein from chicken, fish, beans and nuts. It avoids foods high in salt, saturated fat, and added sugar. The second is the Mediterranean diet, which follows very similar principles.
One Indian study reported that eating sweet potatoes was associated with a lower risk of gallbladder cancer, along with green chillis, radish, mango, orange and melon – all of which contain high levels of antioxidants.
5. Exercise regularly
Regular physical activity has been shown to be likely to reduce the risk of gallbladder cancer, and studies have shown it can increase the diversity of the gut microbiome.
“Exercise also promotes cell turnover in a different way to when you’re sedentary,” says Mr Farid. “It also reduces the amount of fat and also inflammatory cytokines in your blood. So it’s one of the most important things you can do to modify your risk of many cancers, including gallbladder.””
6 notes
·
View notes
Note
Hello, I am Israa, I have two children (Nasser and In'am). In'am was born two months ago in the midst of this war and genocide. She needs milk, some treatment, and healthy food. I hope that you and your loved ones are well. We are not well. We live in difficult circumstances in the war after I lost my entire family except for my father, and my house was completely destroyed. My father suffers from the spread of cancer in his body and needs urgent surgery. I need your support and donations. I hope you can do so. Recently, I have been suffering from severe pain in my irritable bowel syndrome and my health has deteriorated. No one supports my father and children except me. We have no one. Today, the army informed us that we are in a dangerous area and we must evacuate the area immediately. We do not know where to go and how to go. I am a woman who cannot carry my father and children. I am alone. This is too much for me, and they are targeting us directly. I need you here. I am struggling to get milk and healthy water. I need diapers for my children and father, and they cost ($50). Everything is bad, and I do the simplest things with difficulty. Here, they are killing us slowly. I feel like I've lost hope and there's no hope of survival and I'm going to lose the rest of my family, please help me save what's left for me. 💔🙏
Vetted.
11 notes
·
View notes