#stage 4 bowel cancer
Explore tagged Tumblr posts
Text
I hope tonight is your last night suffering. I can’t stand to hear you struggling to breath. I can’t stand to watch your once vibrant color fade to grey. I can’t stand grabbing for your warm loving hands…but catching cold frail lifeless ones. I can’t stand the thought of losing the most important person in my life.
This makes every heartbreak feel like a splinter in my finger. This makes all betrayal feel like a joke I just didn’t understand. This makes all the horrible things happening all around the world feel like simply an annoyance in comparison to this.
I hate all moments in the past when I was angry with you. I hate the cruel words I spewed your way. All you ever did was love me unconditionally… why did I feel the need to test that so often?
I’m sorry Mommy, for not always being easy to love. And thank you Mommy for always choosing to love me through it.
Without your love, I would have never learned how to truly love myself.
I love you Mom. I will miss you everyday until the end of time. You are the best.
Please rest easy, and please don’t be afraid to let go of that painfully sick body holding you back. You were meant for more.
5 notes
·
View notes
Text
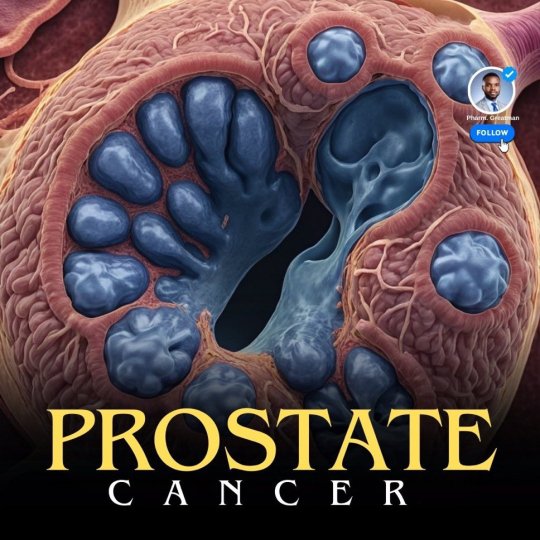
PROSTATE CANCER AWARENESS
Prostate cancer is one of the most common cancers in men, but detecting it early is a game changer.
I'll explain all you need to know about this condition in simple terms, I try to answer some famous questions you may have..
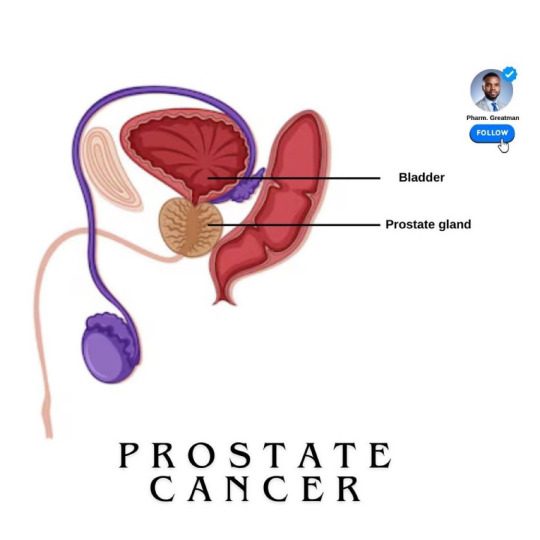
What is Prostate cancer?
It is a type of cancer that begins in the prostate gland The prostate gland is part of the male reproductive system.
It is located below the bladder. This gland is responsible for producing the fluid that nourishes and transports sperm.
Prostate cancer is one of the most common cancers as they age.

What are the risk factors?
The exact cause of prostate cancer is unknown, but the risk factors are certain, they include:
- Age is a major risk factor for prostate cancer, with most cases occurring in men over 50.
- family history; as men with close relatives who had prostate cancer are at a higher risk. Having a father or brother with prostate cancer more than doubles a man’s risk of developing this disease.
- there are changes that could occur in your genes that can also increase your risk.
- men of African descent face an even greater risk and are more likely to be diagnosed at an advanced stage
A study showed that 1 in 4 black men will have prostate cancer in their lifetime, scary

Stages of Prostate cancer
Based on how far it has spread, it is classified into stages from stage I to IV
- Stage I is early and confined to the prostate, while Stage IV indicates the cancer has spread to other parts of the body, like the bones
Knowing the stage of cancer helps your doctor determine the best way to treat
Can regular sexual intercourse prevent prostate cancer, or prostate issues?
Important to state that “regular ejaculation alone is not a guaranteed preventive measure for prostate cancer”
Some studies suggested that regular ejaculation, whether through sex, masturbation, or nocturnal emissions, may reduce the risk of prostate cancer.
Research, including a notable study by Harvard University, found that men who ejaculated 21 or more times per month had a 20% lower risk of prostate cancer than those who ejaculated less frequently. The reasons are not fully understood, possibly that frequent ejaculation might help clear potential toxins or reduce inflammation in the prostate.
However, while this association exists, it’s still under investigation.
More evidence is needed… for example, a study in 2008 revealed that frequent sex in younger men increases prostate cancer risk compared to older men…

Stay active and monitor your health with Inspire 3, a tracker that supports prostate health by encouraging regular activity, reducing stress, improving sleep, and tracking key wellness metrics.
~~~~
Treatment Options
It depends on the stage of cancer and overall health. Options include:
- monitoring the cancer (active surveillance) - surgery to remove the prostate - radiation to destroy cancer cells - hormone therapy to reduce hormones that fuel cancer growth, and chemotherapy.
Treatments for prostate cancer can lead to side effects like difficulty controlling urine, erectile dysfunction, and bowel issues.
They must be communicated to patients beforehand
11 notes
·
View notes
Text
honestly, one of the underrated things about homestuck is that despite featuring dozens of ascended mortals, greek titans, gnostic archons, elder gods, omniscient faceless entities, the grim reaper, and a frog who is the physical embodiment of the cosmos, the only thing the characters ever really seem to talk about as if it were a deity is the allegedly sentient atmosphere of a planet with stage-4 bowel cancer, which appears to control the timeline using a missile defense system
6 notes
·
View notes
Text
New's unexpected new diagnosis
A whole month after surgery, I finally got my results. Lots to talk about here.
Based on my symptoms and medical history, the surgeon said he went in fully expecting severe endometriosis with adhesions. He identified the cyst on my left ovary and removed it (kicking myself because I forgot to ask what kind of cyst it was). My uterine tubes were also easily removed, so sterilization was successful. I asked about my chart reading “unilateral oophorectomy” but he assured me that was a typo, they did not in fact have to remove one of my ovaries. Phew. (Also re: being sent home without pain meds, he was like WHAT. He pulled up the records and there it was, he had it noted that I was to be sent home with meds. So someone at the hospital messed up. He asked me, “but you eventually got meds, right?” Yeah, but it was oxycodone and that barely touches my pain. I told him when I go to the ER for flare ups multiple times a year, they have to give me hydromorphone every 2-4 hours because it’s that bad. So he’s sending me to a new pain doctor and pelvic PT, but we’ll see if my insurance even lets me.) But other than that, he didn’t actually see any obvious endometriosis implants. Not even adhesions that would indicate it either. Nothing was stuck together like he expected. But he did stress, and I knew this from research already, that just because he didn’t see anything obvious doesn’t mean I don’t have endo. This is pretty common for patients on the first surgery. Sometimes not much is seen because it’s really the specialists who know how to identify other less-obvious lesions or hidden pockets of endo. My surgeon is very knowledgeable and I really like him, but he’s not actually an endo specialist (I can’t access them with my insurance, and even if I did have better insurance the co-pay would still be many thousands of dollars). Here’s where he was genuinely surprised: When he checked the backside of my uterus, he said it’s just completely scarred up. Rough and damaged from inflammation. Which could still be superficial endometriosis but is a giant red flag for adenomyosis (though it’s possible to have both). Quick explanation for those who need it: endometriosis is when tissue similar (but not the same as) the lining of the uterus grows outside of the uterus. It can grow on the surface, the ovaries, the bladder, kidneys, bowel, liver, nerves, lungs, or even the brain. These lesions bleed within the body and cause a lot of damage and often infertility. People have lost organs and their lives from this disease being so mismanaged by doctors. It spreads like cancer so it’s diagnosed in stages the same way. Adenomyosis has a lot of the same symptoms but the process is different. The lining instead grows into the muscle of the uterus, causing damage and often infertility. Both of these diseases can be painful, debilitating, and disabling no matter what stage. Though the endometriosis is still uncertain, my surgeon has diagnosed me with adenomyosis. Just to be extra certain, he’s sending me for a pelvic MRI with contrast during my period so he can have a better look. I actually had an MRI 2 years ago that had me questioning if I had adeno because I thought my uterus looked weird and stained, just dark and splotchy and roughly textured but no one noted it (radiologists are not trained well in identifying these diseases). I was mostly focused on the ovarian cyst so I kind of forgot about it.
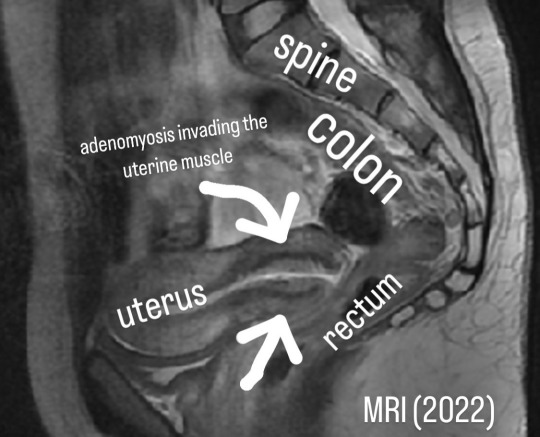

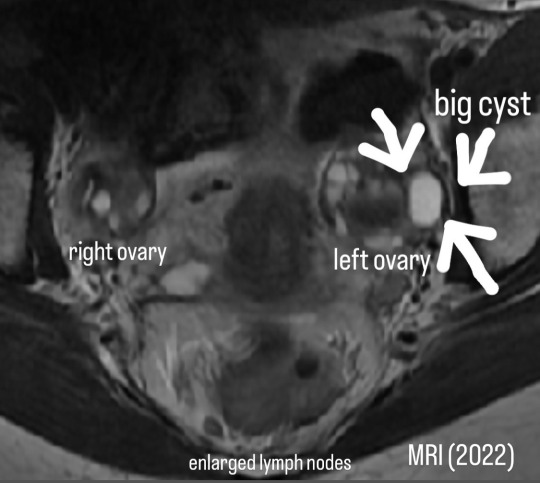
But yeah, this explains a lot, because the back of the uterus is up against the rectum, which is where my colitis is the worst. The inflammation is close enough to affect the organs around it. This explains why my colitis seems so unmanageable, yet every time I have a colonoscopy they tell me it’s mild and act like I’m just being dramatic. This explains why everything’s just been getting worse and worse seemingly every year. The anemia, intense fatigue, weakness, nausea, and pain that hardly any meds (that will be given to me) can touch. Frustratingly, he didn’t have the pictures to show me despite multiple people telling me he would have them. I called and emailed the hospital all day today and thankfully they’re mailing everything my way. Where to from here? The only cure for adenomyosis is hysterectomy. I was considering getting a partial one (saving my ovaries so I don’t go into menopause) in a year or two anyway if my condition doesn't improve. There's still a potential risk of ovarian dysfunction/failure after 5 years but I'm getting older anyway and I need to move on. I can go on HRT if needed. Surgeon is in full agreement that this is the best way forward to improve my quality of life. Though this won’t cure any endo that might still be hiding, it will be a dramatically different experience without this diseased organ constantly ruining my life (and no more periods! I can’t even imagine that freedom). I’m overwhelmed at having to start this process again to get a whole nother surgery that’s much more intense than what I just had, but I had also prepared myself knowing that this was only the very first surgery. It wasn’t meant to “fix” me but to finally get eyes on my insides. Hopefully it doesn’t take a whole year again between the consult and the actual surgery. Glad there’s no damage from adhesions we’d have to deal with either, so that simplifies things a lot. I’m so thankful to finally have actual answers and a clear path moving forward for future recovery. I’ll never be “normal”, I have so many other chronic illnesses that I’ll have to keep working hard at managing, but we can at least do something about this one. I’ll update more when I get the surgery pictures and the new MRI. Surgeon has officially cleared me to take baths again, so I’m going to go luxuriate for a while. Thank you to everyone for the support, the donations, and the kind messages.
11 notes
·
View notes
Note
delete this please I have depression, anxiety, panic, post traumatic stress disorder, psychosis, high blood pressure, low blood pressure, hpv, hiv, dengue, zika, chikungunya, black plague, polio, infantile paralysis, osteoporosis, swine flu, yellow fever, meningitis, meningitis b, gonorrhea, herpes, pharyngitis , Chagas disease, bronchitis, leptospirosis, cancer, measles, chickenpox, smallpox, mumps, gastritis, tetanus, hepatitis, conjunctivitis, stroke, whooping cough, labyrinthitis, scabies, leukemia, rabies, cirrhosis, scoliosis, microcephaly, anencephaly, ebola, ingrown toenail, autism, asperger's syndrome, arrhythmia, pneumonia, diabetes(type 1 and 2), heart failure, petho envy, dwarfism, gigantism, down syndrome, asthma, liver cancer, esophageal cancer, brain cancer, stomach cancer, skin cancer , leprosy, homosexuality, herniated disc, thrombosis, elephantiasis, passion fruit heel, phimosis, prostate cancer, testicular cancer, parkinson's disease, headache, malformation of the ovaries, lymphoma, lead poisoning, severe allergies, endometriosis, stomach ulcers, irritable bowel syndrome, appendicitis, chronic migraines, graves disease, blindness, deafness, stage 4 kidney disease, organ failure, 90% stage 3 burn, urinary tract infection, cervical cancer, uterine tuberculosis, uterine fibroids, uterine prolapse, anal prolapse, hemorrhoids, dermatillomania, coronavirus, contact dermatitis, eczema, athletes foot, fungal infection, bacterial infection, and veganism
Have you tried yoga.
11 notes
·
View notes
Text

Dear Friends and Community,
We are reaching out to you with a heartfelt request to support our dear friend, Dan, who has bravely for the past 18months been battling stage 4 bowel and bladder cancer. After a year of intense chemotherapy and radiotherapy, the side effects caused Dan to have many hospital stays away from his family, by helping to keep him fit, well and infection free this will allow him to spend quality time with his family at home,making memories that they all deserve.
At just 38 years old, Dan is a loving husband to his wonderful wife Laura and a devoted father to two beautiful daughters, aged 6 and 15.
Dan's journey with cancer has been incredibly challenging, with one set back after another these included bowel blockages, infections, 3 major abdominal operations, blood clots alongside a missed diagnosis of bladder cancer.
Dans strength and determination are truly inspiring. In May this year Dan and his family were told that Dans cancer was no longer curable, however, his oncologist has agreed for Dan to start on Immunotherapy ASAP, as a family we are thankful to have been offered this treatment on the NHS as we know from data that immunotherapy on the NHS is very rare. We now as a family have a little bit of hope.The care, empathy and support we have had from palliative care and district nurses has been incredible.
Alongside his conventional treatment of immunotherapy Dan is seeking complementary therapies that can provide relief and improve his quality of life during this difficult time. These therapies, however, come with significant costs that are not covered by the NHS.
We are rallying together to raise funds to support Dan and his family in accessing these vital complementary treatments. Your generous contribution, no matter the amount, will make a tremendous difference. It will not only help Dan manage his symptoms and side effects but also give him the strength to continue fighting for the sake of his beloved family.
Please consider donating to Dan's fund and sharing his story with others who might be able to help. Together, we can make a profound impact and offer Dan and his family the hope and support they need during this trying time.
Thank you from the bottom of our hearts for your kindness and generosity.
5 notes
·
View notes
Text
Hi all, thank you for taking the time to read our story.
My name is Nicky, wife to my lovely husband Jim.

Things took a drastic turn in May 2022 when Jim was diagnosed with inoperable stage 4 bowel cancer that had spread to his liver. I knew cancer was a cruel disease but never in a million years did I expect it to turn our worlds up side down in the way it has!
Jim began gruelling chemotherapy shortly after diagnosis leaving him bedridden for days on end, however he had an excellent response to treatment and things were looking positive.

After recovering from this op he went on to undergo more chemo, an intense course of radiotherapy and caught Covid twice! Unfortunately Jim did not have such a good response to the chemo and the cancer started to progress.
If the side effects of chemo and radiotherapy wasn’t enough to contend with the tumour was also pushing on nerves causing unbearable pain in his back and rectum. He spent 2 weeks in St Helena hospice in July for pain management and after many hurdles managed to come home and continue with chemo.
However Jim’s pain returned with a vengeance along with a high temperature which saw him back in hospital. It was discovered Jim’s tumour had perforated causing a large abscess in his bowel and was the cause of ongoing infections. This was managed for 7 weeks between hospital and hospice and eventually after much conflicting information, finally it was drained. Wow what a relief, maybe now Jim could get some quality of life back and we could enjoy some much needed family time.

Jim has now moved on to third line treatment Lonsurf which is an oral chemotherapy. After much research I have discovered another drug Bevacizumab, also known as Avastin that studies show strong evidence to suggest it works effectively alongside Lonsurf and has shown to extend overall survival compared to Lonsurf alone.
Unfortunately this drug is not available on the NHS and has to be self funded privately.
This is an opportunity we CANNOT turn down, after the battle Jim has been through he deserves the chance to stabilise the cancer in the hope it will improve his quality of life.

This drug is extremely expensive to fund. We are looking at over £1000 per treatment which is given every two weeks plus additional fees for follow up consultations. For 12 months of treatment we are looking at around £25,000!
Just to add into the mix, Jim was made redundant after diagnosis so as you can imagine we are not in a position to fund this alone.
Asking for help is not something that comes easily to either of us and we have thought long and hard about whether to set this page up. However, without additional support we wont be able to fund this treatment.
Jim, nor I are ready to give up, he has two young children that need him here for as long as possible, as well as the rest of his family and friends!

If you are unable to donate then please don’t worry. If you could share Jim’s story to raise awareness of bowel cancer that would also be amazing.
Thank you for taking the time to read our story and thank you in advance.
Loads of love Nicky Jim, Archie and Izzy xx
#donations#fundraising#gofundme#donate#philanthropy#nonprofit#crowdfunding#charities#planned parenthood#volunteering
6 notes
·
View notes
Text
Colon Cancer Treatment in Pune | Dr. Pratik Patil – Best Oncologist in Pune
Colon Cancer Treatment in Pune – Get Early Diagnosis and Expert Care
Introduction
Colon cancer, also known as colorectal cancer, begins in the large intestine (colon). It is one of the most treatable cancers if detected early. In India, awareness about colon cancer is growing, and Pune has become a trusted centre for modern cancer care. If you’re searching for expert colon cancer treatment in Pune, Dr. Pratik Patil is a well-known and experienced specialist you can rely on.
What is Colon Cancer?
Colon cancer occurs when cells in the lining of the colon grow uncontrollably. Over time, these cells can form polyps, and some of them may turn cancerous. If untreated, the cancer can spread to nearby organs or lymph nodes.
Common Symptoms of Colon Cancer
Colon cancer may not show clear symptoms in early stages. Some warning signs include:
Change in bowel habits
Blood in stool
Unexplained weight loss
Stomach pain or discomfort
Weakness or fatigue
Feeling that the bowel doesn’t empty fully
If you experience any of these symptoms, it is important to consult a cancer specialist immediately.
How is Colon Cancer Diagnosed?
To confirm colon cancer, the following tests may be done:
Colonoscopy – A camera is used to examine the colon
Biopsy – A sample of tissue is taken during colonoscopy
CT Scan or MRI – To detect the spread of cancer
Blood Tests – Including CEA marker for colon cancer
PET Scan – Used in advanced cases
Dr. Pratik Patil offers advanced diagnostic tools to detect colon cancer at its earliest and most treatable stage.
Stages of Colon Cancer
Colon cancer is generally classified into these stages:
Stage 0: Cancer is in the inner lining only
Stage 1: Cancer has spread into deeper layers of the colon wall
Stage 2: Cancer has spread through the colon wall but not to lymph nodes
Stage 3: Cancer has spread to nearby lymph nodes
Stage 4: Cancer has spread to other organs such as the liver or lungs
Best Treatment Options for Colon Cancer in Pune
Treatment depends on the stage and overall health of the patient. Dr. Pratik Patil offers the following treatment options:
1. Surgery
Surgery is usually the first step, especially in early-stage colon cancer. The part of the colon with cancer is removed.
2. Chemotherapy
Chemotherapy is used after surgery or in advanced stages to kill remaining cancer cells.
3. Radiation Therapy
Used in certain cases, especially when cancer is in the rectum.
4. Targeted Therapy
These medicines target specific cancer cells and work well in certain patients.
5. Immunotherapy
For patients with specific genetic changes (like MSI-H or dMMR), immunotherapy offers promising results.

Why Choose Dr. Pratik Patil for Colon Cancer Treatment in Pune?
Over 14 years of experience in treating gastrointestinal cancers
Specialist in targeted therapy and immunotherapy
Trained from Michigan State Cancer University, USA
Practising at Jupiter Hospital, Baner, and available at Healthbay Clinic
Successfully treated over 5000+ cancer patients
Book an Appointment
If you are experiencing symptoms of colon cancer or have already been diagnosed, do not delay expert care. You can consult Dr. Pratik Patil, a trusted cancer specialist in Pune, at Jupiter Hospital located on Baner-Balewadi Road. To schedule an appointment, call 9637439163. For more details about available treatments, you may visit the official website of Dr. Pratik Patil at pratikpatil.co.in. Getting timely treatment can make a big difference in your recovery.
#colon cancer treatment in Pune#colon cancer doctor in Pune#colorectal cancer specialist Pune#best oncologist in Pune#cancer treatment Baner Pune#Dr Pratik Patil cancer specialist#colon cancer surgery Pune#gastrointestinal cancer treatment Pune
0 notes
Text
Rectal Cancer Treatment After Surgery
Rectal cancer treatment doesn't end in the operating room. In fact, for many patients, the most critical phase begins after surgery. This post-operative period is essential for long-term health, recurrence prevention, and emotional recovery. Understanding what lies ahead empowers patients to actively participate in their recovery journey.

Types of Surgery for Rectal Cancer
Low Anterior Resection (LAR): This procedure is used when the tumor is located in the upper part of the rectum. Surgeons remove the cancerous section and rejoin the healthy ends of the colon and rectum. A significant advantage of LAR is the preservation of the anal sphincter, allowing patients to maintain normal bowel function and avoid permanent colostomy. This type of surgery is often followed by careful rectal cancer treatment after surgery, including monitoring and possible adjuvant therapy.
Abdominoperineal Resection (APR): When the tumor is located near the anus, making sphincter preservation impossible, APR is performed. It involves removing the rectum and anus, resulting in a permanent colostomy. Recovery can be physically and emotionally demanding. Patients often need colostomy education, psychological support, and lifestyle adjustments.
Transanal Local Excision: For early-stage tumors that haven’t penetrated beyond the rectal wall, this less invasive method allows removal without abdominal incisions. It helps maintain normal bowel function and usually does not require additional treatments like radiation or chemotherapy.
Pelvic Exenteration: Reserved for advanced rectal cancers that have spread to adjacent organs. This extensive surgery removes the rectum and surrounding organs like the bladder or uterus. While recovery is complex, it offers a potential cure when non surgical treatment for rectal cancer is no longer effective.
Recovery After Rectal Cancer Surgery
1. Initial Hospital Stay
Post-surgery, patients typically spend several days in the hospital. Medical teams monitor pain, infection, bowel function, and surgical wound healing. Tubes may be inserted to drain fluids or assist with urination. Intravenous pain medications gradually shift to oral medications. Early ambulation (walking) is encouraged to prevent blood clots and pneumonia.
2. Physical Adjustments and Bowel Habits
It is common to experience bowel irregularities post-surgery, such as increased frequency, urgency, or incontinence. Patients might need to follow a low-fiber diet initially, gradually transitioning to a more varied diet. Medications can help manage symptoms. Over time, the body adapts, and bowel function typically improves.
3. Emotional and Psychological Recovery
A cancer diagnosis and major surgery can deeply affect mental health. Anxiety, depression, and body image issues—particularly after a colostomy—are common. Counseling, support groups, and open communication with family and healthcare providers are vital components of holistic rectal cancer treatment after surgery.
4. Returning to Daily Activities
Fatigue may persist for weeks or months post-surgery. Patients should start with gentle physical activity and increase intensity gradually. Proper rest, hydration, and nutrition support the healing process. For many, it takes time to return to work or regular routines. Patience and self-care are key.
5. Ongoing Monitoring and Follow-Up
Post-surgical care doesn’t stop once the incision heals. Regular follow-up appointments include blood tests, imaging scans, and colonoscopies to detect any recurrence early. Adjuvant therapy such as chemotherapy or radiation may be recommended based on surgical pathology findings.
Life Expectancy and Long-Term Outlook
The prognosis after rectal cancer surgery depends on various factors, including cancer stage, response to treatment, patient age, and general health. Many patients go on to live long, fulfilling lives. Early detection, appropriate treatment, and strict follow-up care significantly enhance long-term survival and quality of life.
Postoperative Care Essentials
Tubes and Drains: Drains and urinary catheters are used to prevent fluid buildup and support healing. These are usually temporary and removed within a few days, depending on the patient’s condition.
Pain Management: A personalized pain control plan may involve oral or IV medications. Effective pain relief enables early mobility and reduces complications.
Dietary Adjustments: The digestive system often needs time to restart. Patients typically begin with clear liquids, gradually advancing to soft foods. A dietitian can assist in crafting a diet that supports bowel health and healing.
Mobility: Getting out of bed and moving as soon as possible is crucial. It reduces the risk of complications and accelerates physical recovery.
Wound Care: Surgical sites are monitored closely for signs of infection. Patients are given instructions for keeping wounds clean and dry at home.
Discharge Planning: Patients are discharged when they can manage pain, tolerate food, and move independently. A detailed recovery plan includes medications, wound care, and upcoming appointments.
Other Rectal Cancer Treatment Methods
Chemotherapy: This treatment targets residual cancer cells and reduces the risk of recurrence. It is commonly used before or after surgery, especially if lymph nodes were involved.
Radiation Therapy: Radiation shrinks tumors before surgery and eliminates remaining cancer cells afterward. It is essential for local control and is a cornerstone of rectal cancer treatment after surgery.
Targeted Therapy: These drugs focus on specific molecules involved in cancer growth. For example, bevacizumab cuts off the tumor’s blood supply.
Immunotherapy: For rectal cancers with certain genetic profiles, immunotherapy boosts the immune system to recognize and destroy cancer cells.
Watch-and-Wait: In cases of complete response to chemoradiation, surgery may be avoided in favor of active surveillance. This method requires frequent checkups and imaging.
Palliative Care: In incurable cases, symptom relief becomes the focus. Pain management, radiation for bleeding, and minor surgeries help maintain quality of life.
Preparing for Rectal Cancer Surgery
Understand the Surgical Plan: Know the goal of your surgery—whether curative or part of a multimodal plan. Understanding the procedure helps manage expectations and reduces anxiety.
Preoperative Therapy: Chemoradiation may be used before surgery to reduce tumor size and improve resection margins. In some cases, surgery might be delayed or avoided based on response.
Know the Risks: It’s reasonable to ask, "Is rectal surgery dangerous?" Complications can include bleeding, infection, or leakage, but skilled surgical teams manage these risks effectively.
Ostomy Planning: Some patients require temporary or permanent colostomies. Ostomy nurses offer guidance on managing this change.
Nutrition and Bowel Prep: Follow instructions for bowel preparation and eat nutritious foods before surgery to improve recovery.
Strengthen Body and Mind: Quit smoking, exercise lightly, and treat underlying health issues. Emotional preparation through counseling or connecting with survivors also helps.
Life After Surgery: Ask about long-term changes in bowel habits, diet, and intimacy. Understanding these changes helps you plan for a smoother transition post-surgery.
Conclusion
Recovery and healing after rectal cancer surgery are both physical and emotional journeys. From tubes and dietary changes to psychological adaptation and long-term follow-up, every step contributes to regaining a sense of control.
Take charge of your healing—ask questions, follow your care plan, and never hesitate to advocate for your well-being. With the right medical support and personal resilience, a fulfilling life after rectal cancer is not only possible but well within reach. For more details visit https://thearcgut.clinic/benign-colorectal/parastomal-hernia/
0 notes
Text
Advancements in Gastrointestinal Diagnostics at Desai Surgical Hospital: What Patients Should Know
Contemporary medicine has evolved in identifying and managing gastrointestinal (GI) conditions. Modern diagnostic technologies, such as noninvasive imaging and sophisticated endoscopy, allow you to learn more about what's happening inside your digestive system more quickly, accurately, and comfortably. Because of technological advancements, patients are getting answers faster than ever before, whether they are dealing with problems like acid reflux, chronic stomach pain, or inexplicable weight loss.
What Are the New Advancements
1. High-Definition Endoscopy
Traditional endoscopy has long been the gold standard for visualizing the GI tract, but high-definition (HD) scopes now provide enhanced clarity. This allows more precise detection of ulcers, inflammation, tumors, and early-stage cancers. The best gastroenterologists in Vadodara use HD endoscopy to ensure patients receive accurate diagnoses with minimal discomfort.
2. Capsule Endoscopy
A revolutionary advancement, capsule endoscopy involves swallowing a tiny, pill-sized camera that captures thousands of images as it moves through your digestive tract. It's beneficial for examining the small intestine, an area difficult to reach with traditional methods. This noninvasive test is painless and ideal for patients with unexplained bleeding or suspected Crohn's disease.
3. Endoscopic Ultrasound (EUS)
EUS provides fine-grained pictures of the digestive tract and adjacent organs by combining endoscopy with ultrasound. It is useful for assessing bile duct obstructions, pancreatic disorders, and specific tumor types. The top gastroenterologists in Vadodara can use this technology to identify anomalies early and develop focused treatment plans.
4. Advanced imaging, including enterorrhaphy based on CT and MRI
These imaging methods allow for a cross-sectional view of the digestive tract. One can identify strictures, malignancies, and inflammatory bowel disease (IBD) using the digestive tract. CT and MRI enterorrhaphy give physicians a comprehensive grasp of anatomy and disease progression without requiring invasive treatments.
5. Molecular and Genetic Testing
Molecular diagnostics can offer early warnings for people with inherited cancer syndromes or gastrointestinal diseases in their family. These tests can identify genetic alterations that raise the likelihood of illnesses, including colon cancer and celiac disease. These findings can be used to create monitoring programs and individualized treatment regimens.
The Benefits of Timely Recognition
Many gastrointestinal disorders, including cancer, respond better to therapy when detected early. Clinical expertise and modern technologies are combined to guarantee accurate and timely disease diagnosis. Choosing the best gastroenterologists in Vadodara is essential since it gives you access to the most cutting-edge diagnostic equipment and evidence-based care in one place.
CONCLUSION
Thanks to advancements in diagnostic techniques, patients no longer have to undergo outdated or uncomfortable procedures to get clear answers about their digestive health. If you're experiencing persistent digestive symptoms, don't delay. Like Desai Surgical Hospital, the best gastroenterologists in Vadodara are equipped with the latest. We provide the tools to diagnose and treat your condition effectively and comfortably.
Visit Desai Surgical Hospital for Expert Gastro Care!
Location: Near G.P.O, Kharivav Road, Dandia Bazaar Road, Raopura, Vadodara,
Gujarat 390001
Contact: 0265 2435153
OPD Timings:
Monday - Friday: 12:30 PM - 02:30 PM & 06:00 PM - 07:00 PM
Saturday: 12:00 PM - 02:30 PM
Sunday: Closed
Emergency Services: Available 24/7Choose expert care at Desai Surgical Hospital, where the Top Gastroenterologists in Vadodara ensure optimal digestive health.
#GastroCare#DigestiveHealth#Endoscopy#Gastroenterologist#VadodaraDoctors#AdvancedDiagnostics#GIHealth#CapsuleEndoscopy#EarlyDetectionSavesLives#DesaiSurgicalHospital
0 notes
Text
Decoding Ovarian Cancer Symptoms: Communicating the Silent Signs

Ovarian cancer remains one of the most challenging gynaecologic malignancies, often referred to as a “silent killer” due to its subtle onset and late-stage diagnosis.1 In 2022, 324,603 women worldwide were diagnosed with ovarian cancer. By 2050, the annual incidence is projected to rise to nearly half a million, representing a 55% increase compared to current levels.² With over 200,000 lives lost globally in 2020, this disease continues to be a significant public health concern.3 The prognosis of ovarian cancer remains disappointing, with a mere 46% of women surviving beyond 5 years after diagnosis.3 Its ability to progress without clear early symptoms makes it particularly dangerous, but early detection can dramatically improve outcomes. A powerful ally in this effort—often underrecognized—is effective medical communication.
Why Early Detection Makes All the Difference
The statistics speak for themselves. Ovarian cancer that remains localized to the ovaries (stage I) has the potential to be effectively treated in as many as 90% of patients, whereas malignancy limited to the pelvic region (Stage II) correlates with a 5-year survival rate of 70%. Conversely, neoplastic disease that has disseminated beyond the confines of the pelvis (stage III-IV) exhibits a long-term survival probability of 20% or lower.4 This stark difference underscores the importance of timely diagnosis.
From a patient’s perspective, early detection can mean a less aggressive treatment course. In some cases, surgery alone may suffice, avoiding the physical and emotional toll of chemotherapy.5 For younger women, early intervention also opens the door to fertility-preserving options.6
From a provider’s standpoint, diagnosing the disease at an early stage facilitates more personalized care, reduces treatment complications, shortens hospital stays, and ultimately improves the quality of life for patients. Additionally, early-stage management is often more cost-effective and resource-efficient, which benefits the healthcare system as a whole.
The Challenge: Recognizing the Subtle Symptoms
One of the biggest hurdles in ovarian cancer care is identifying it early. The symptoms are often vague and easily mistaken for common digestive or urinary issues. But when these signs occur frequently—12 or more times a month—they shouldn’t be ignored.7
Watch out for:
Bloating or a swollen tummy
Pelvic or abdominal pain
Feeling full quickly or loss of appetite
Needing to urinate more often or urgently
Additional symptoms may include indigestion, unintentional weight loss, changes in bowel habits (constipation or diarrhoea), back pain, fatigue, and postmenopausal vaginal bleeding.7 Although these symptoms may be dismissed as minor or attributed to other causes, persistent occurrence warrants medical evaluation.
Who’s at Greater Risk?
Several risk factors further increase susceptibility, such as:8
Being over 50, particularly post-menopausal
Having BRCA1 or BRCA2 gene mutations
A family history of ovarian, breast, or colorectal cancer
A history of endometriosis
Never having been pregnant
Long-term use of hormone replacement therapy
Obesity
In individuals with these risk factors, proactive monitoring and timely screening become even more critical.
How is Ovarian Cancer Detected Early?
Unfortunately, there is no universally recommended screening test for ovarian cancer in asymptomatic women at average risk. However, several biomarkers and imaging tools are used—especially in high-risk individuals or when symptoms are present.
Key biomarkers encompass elevated levels of CA-125 (Cancer Antigen 125) and HE4 (Human Epididymis Protein). Diagnostic modalities like Risk of Ovarian Malignancy Algorithm (ROMA) integrates CA-125, HE4, and menopausal status to generate a risk score for malignancy, thereby facilitating the early detection of ovarian cancer. Furthermore, OVA1 test, a multivariate index assay, evaluates multiple protein levels in the blood to determine the risk of ovarian cancer in women presenting with an ovarian mass.8
There exist specific imaging tools that contribute to the early detection of ovarian cancer. Transvaginal ultrasound (TVUS) is instrumental in visualizing the ovaries and identifying abnormalities, such as masses or cysts, while pelvic MRI or CT scan may further assist in evaluation when ultrasound findings lack clarity.8
In women with familial predisposition to breast or ovarian cancer, genetic testing is crucial for the identification of BRCA1/2 mutations and other hereditary cancer syndromes linked to ovarian cancer. Understanding one’s genetic risk facilitates the implementation of preventive measures, including enhanced surveillance or prophylactic surgical interventions.8
Where Medical Communication Comes In?
While awareness of symptoms and risk factors is essential, medical communication serves as the cornerstone in bridging knowledge and action. Its role is multifaceted, benefitting both patients and healthcare providers.
Empowering Patients Through Education: When patients understand early signs of ovarian cancer, they’re more likely to seek care promptly. Campaigns like the CDC’s Inside Knowledge show that clear, accessible information leads to earlier recognition and action.9
Facilitating Early Diagnosis: Empathetic, attentive dialogue from healthcare providers encourages patients to report unusual symptoms, building trust and enabling earlier detection.
Enabling Shared Decision-Making: Clear, compassionate communication helps patients understand their diagnosis, explore treatment options, and actively participate in their care—improving both outcomes and satisfaction.
Overcoming Communication Barriers: Poor communication can delay diagnosis. Culturally sensitive, respectful interactions make patients feel safe, heard, and more likely to engage in their care.
Enhancing Screening and Prevention: Regular discussions about risk, symptoms, and family history motivate patients to adopt preventive behaviours and pursue early screening—critical for early-stage detection.
The Role of Medical Communication Agencies
At every stage—from raising awareness to supporting diagnosis, treatment decisions, and prevention—medical communication agencies act as strategic partners in improving outcomes. By transforming complex medical information into patient-friendly content, developing provider training tools, and designing culturally sensitive campaigns, these agencies ensure that critical health messages resonate. Their expertise in crafting clear, compassionate, and actionable communication bridges the gap between medical knowledge and patient engagement, ultimately driving earlier detection and better care experiences across the board.
Conclusion
Ovarian cancer remains challenging due to its silent onset and rapid progression, but early detection can shift outcomes dramatically. Medical communication is not just supportive—it’s a strategic enabler, driving awareness, encouraging timely symptom reporting, and building trust between patients and providers. As diagnostics advance, the impact of clear, compassionate communication remains vital in bridging the gap between symptom onset and timely intervention.
Turacoz specializes in in transforming complex medical information into clear, actionable content that supports both patients and healthcare providers. From developing symptom awareness tools to creating dialogue aids and educational campaigns, we enable early recognition, informed decision-making, and timely action. With expertise in oncology communication, we craft materials that foster trust, encourage preventive behaviour, and enhance patient-provider conversations—ultimately contributing to earlier detection and improved outcomes in ovarian cancer care.
References
Feeney L, et al. Liquid biopsy in ovarian cancer: Catching the silent killer before it strikes. World J Clin Oncol. 2020;11(11):868-889.
World Ovarian Cancer Coalition. Available at: https://worldovariancancercoalition.org/wp-content/uploads/2024/04/2024-Global-Priority.pdf. Last accessed: May 2025.
Wang M, Bi Y, Jin Y, and Zheng ZJ. Global Incidence of Ovarian Cancer According to Histologic Subtype: A Population-Based Cancer Registry Study. JCO Glob Oncol. 2024;10:e2300393.
Elias KM, Guo J, and Bast RC Jr. Early Detection of Ovarian Cancer. Hematol Oncol Clin North Am. 2018;32(6):903-914.
Fishman DA and Bozorgi K. The scientific basis of early detection of epithelial ovarian cancer: the National Ovarian Cancer Early Detection Program (NOCEDP). Cancer Treat Res. 2002;107:3-28.
Kim SY and Lee JR. Fertility preservation option in young women with ovarian cancer. Future Oncol. 2016 Jul;12(14):1695-8.
Ovarian cancer. Available at: https://www.nhs.uk/conditions/ovarian-cancer/symptoms/. Last accessed: May 2025.
Fernandes B. A Review on Emerging Biomarkers for Early Detection of Ovarian Cancer. Ind J Pharm Pract. 2024;17(1):17–20.
Cooper CP, Polonec L, and Gelb CA. Women’s knowledge and awareness of gynecologic cancer: a multisite qualitative study in the United States. J Womens Health (Larchmt). 2011;20(4):517-524.
0 notes
Text
5:15pm It is the stage of luekemia Where I lose my bowels in public
---------------------------
Just so happens to be the day Dad sends me $100 I already ordered clothing and shampoo and food But I'm already to 401 Division & Back Twice Before I realize why I feel like one of the bar strobe lights That goes into the night sky on event nights
Miles away.
I feel you can feel how alone I feel from space.
------------------------------------------------------------------------------
I think I had the "I had leukemia & chemo therapy treatment aged 4 & 5" twice. Mom cut my bangs. I was pale. She thought it was lice. IT must of bin. Then she seen the shape of eggs and food against my freckles and skin.
Ant then she realized some were purple spots like the inside of cooked chicken.
F e v e r
And then she cut my hair and i had to wear head wraps and head scarves, and i told mom i would never forgive her for making me look like a boy, and then i'm 28, its may 19th, I'm homeless and i have a full head of hair but i feel like i'm 5 in the washroom at Harmony Rd Corner unit, and I'm sad because there was no end date for chemo until there was. "I rather be in heaven with sadie." but there was no sadie. there was shadow. sadie died in 2002 when we were in pefferlaw.
anyways, i wanted to be in heaven, looking like a 5 year old boy that was fat and "i don't know what heaven looks like but I just want to go"
----------------------------------
and I wondered about pooping myself at the mall, out with mom and the lessons just breezed right by when something so odd turns up as really bad life long cancer signs, a few days later
-----------------------------------
I had that talk once with myself. The week before Tulloch with mom and papa, at Nana and Papas house, they had that talk with me.
Then,
Once on Grenfell, when my heart knew I was beyond the point of finding a job in time to afford rent. Or reverse out of the arrears.
I forgave myself in that instant. I also realized it must have been the first day.
the point of no return
like a stuttering house, as it losers power, of a generator running out of gas
shoop
shoop
sheeeeeew
0 notes
Text
Stages of uterine cancer
Uterine cancer, also known as endometrial cancer, begins in the lining of the uterus and is one of the most common gynecologic cancers. Early detection plays a vital role in successful treatment, which is why understanding the stages of uterine cancer is so important. At Deepa Hospital, we are committed to providing personalized, comprehensive care including precise cancer staging to ensure each patient receives the most effective treatment based on their unique condition.
Why Staging Matters
The stage of uterine cancer describes how far the disease has spread in the body. Accurate staging helps doctors plan the best course of treatment and provides insight into the likely outcome. Staging is determined through imaging tests, biopsies, and surgical procedures, including lymph node assessment. The earlier the cancer is diagnosed, the greater the number of treatment options and the better the chances of recovery.
Finding Out Your Stage: Common Questions Answered
What stage is uterine cancer usually found? Most uterine cancers are detected in the early stages (Stage I or II), especially when women report unusual symptoms like abnormal bleeding.
What is Stage 4 uterine cancer? Stage IV uterine cancer is the most advanced form of the disease, where the cancer has spread beyond the pelvis to distant organs such as the bladder, rectum, lungs, or liver.
The Stages of Uterine Cancer
Stage I: Cancer Confined to the Uterus
Symptoms:
Abnormal vaginal bleeding (especially after menopause)
Pelvic discomfort or pressure
Sometimes, no symptoms at all
Treatment:
Total hysterectomy (removal of the uterus and cervix)
Possible removal of nearby lymph nodes
Radiation therapy may be recommended to prevent recurrence
Note: Fertility-sparing treatment may be considered in selected early cases.
Stage II: Cancer Spreads to the Cervix
Symptoms:
Persistent abnormal bleeding
Pelvic pain
Vaginal discharge
Treatment:
Surgery to remove the uterus, cervix, and sometimes surrounding tissues
Chemotherapy or radiation may be added depending on the spread
Stage III: Cancer Extends Beyond the Uterus
Stage IIIA:
Spread: Cancer reaches the outer uterus layer or nearby tissues.
Symptoms:
Abnormal bleeding
Painful urination or bowel movements
Treatment:
Surgery plus chemotherapy
Radiation depending on tumor spread
Stage IIIB:
Spread: Involves the vagina or nearby pelvic tissues
Symptoms:
Vaginal bleeding
Pelvic pain
Discomfort during urination
Treatment:
Surgical removal of the uterus and affected tissues
Followed by chemotherapy and radiation therapy
Stage IIIC1:
Spread: Pelvic lymph nodes
Symptoms:
Swelling or pain in the pelvic area
Irregular bleeding
Treatment:
Hysterectomy with lymph node removal
Chemotherapy to destroy remaining cancer cells
Stage IIIC2:
Spread: Abdominal (para-aortic) lymph nodes
Symptoms:
Bloating
Pelvic pressure
Fatigue and weight loss
Treatment:
Multimodal approach with surgery, chemotherapy, and radiation
Stage IV: Cancer Spreads to Distant Organs
This is the most serious stage, where the cancer has metastasized to distant areas such as the bladder, rectum, lungs, or bones.
Symptoms:
Pelvic and abdominal pain
Unintended weight loss
Fatigue
Trouble urinating or digestive problems
Treatment:
Surgery if feasible
Chemotherapy and/or radiation
Targeted therapy or immunotherapy (based on specific cancer markers)
Palliative care to manage symptoms and maintain quality of life
How do you beat Stage 4 uterine cancer? While curing Stage IV uterine cancer is more challenging, many patients can still achieve improved outcomes and quality of life through aggressive and individualized treatment plans. At Deepa Hospital, we take a multidisciplinary approach to offer hope and support at every stage.
Fertility and Uterine Cancer
Stage I and II:
Fertility-preserving options such as hormonal therapy or localized surgery may be offered to young women desiring children.
Stage III and IV:
Fertility-preserving treatments are generally not advisable due to the extent of disease spread.
The focus is on survival and disease control.
Post-Treatment Fertility Considerations:
Chemotherapy and radiation can affect ovarian function.
Egg freezing, embryo preservation, or surrogacy may be discussed prior to treatment if future fertility is a concern.
How Is Endometrial Cancer Staged?
Staging involves multiple diagnostic steps:
Pelvic Exam & Imaging: MRI or CT scans assess tumor size and spread.
Biopsy: Confirms the presence and grade of the cancer.
Surgical Staging: During hysterectomy, lymph nodes are removed and analyzed to determine if cancer has metastasized.
FIGO System: The International Federation of Gynecology and Obstetrics (FIGO) system is used worldwide to classify uterine cancer from Stage I to IV.
Conclusion: Your Partner in Cancer Care
Understanding the stages of uterine cancer is essential for timely and effective treatment. From the localized early stages to the more advanced Stage IV, each level of progression requires a tailored treatment plan. At Deepa Hospital, we believe in empowering our patients through education, advanced diagnostics, and compassionate care. Our expert team of gynecologic oncologists, surgeons, radiologists, and fertility specialists work together to guide
you every step of the way. Whether you’re seeking early diagnosis, treatment options, or fertility counseling, Deepa Hospital is here to support you with comprehensive, state-of-the-art care. If you or a loved one is facing uterine cancer, trust Deepa Hospital to provide clarity, care, and hope. Read Also : https://deepahospital.in/blogs/best-hernia-repair-surgery-in-chennai/
0 notes
Text
Top Reasons Why Doctors Recommend Uterus Removal Surgery
By Dr. Deepti Asthana – Leading Gynecologist in Gurgaon
The idea of removing the uterus, or undergoing a hysterectomy, can be overwhelming for many women. For some, it marks the end of menstruation and childbearing; for others, it’s a long-awaited relief from chronic pain, bleeding, or health complications. But what leads a doctor to suggest this major step?
As a practicing gynecologist in Gurgaon, I, Dr. Deepti Asthana, often see women struggle with the decision of whether to go ahead with uterus removal surgery. This article explains the reasons for uterus removal, clears common doubts, and helps you understand when uterus removal is necessary.
What is Hysterectomy?
A hysterectomy is a surgical procedure that involves the removal of the uterus (womb). Depending on the patient’s condition, it may also involve the removal of the cervix, fallopian tubes, or ovaries. Once the uterus is removed:
Menstruation stops permanently.
Pregnancy becomes impossible.
Hormonal changes may or may not occur depending on whether the ovaries are removed.
While it is a major procedure, it is also one of the most commonly performed surgeries in gynecology. But it is not the first step in most treatment plans—it is usually considered only when other methods have failed or when medically necessary.
Why Hysterectomy Is Done – Common Medical Reasons
Doctors recommend hysterectomy only after carefully evaluating the patient’s symptoms, medical history, and treatment goals. Here are the most common medical reasons for uterus surgery:
1. Uterine Fibroids
These non-cancerous growths can cause heavy bleeding, severe pelvic pain, bloating, and fertility issues. When fibroids are large, numerous, or resistant to other treatments like medication or uterine artery embolization (UAE), hysterectomy may be recommended as a permanent solution.
This is one of the top reasons for uterus removal among women over the age of 35 who have completed childbearing.
2. Abnormal Uterine Bleeding
Chronic heavy menstrual bleeding that does not respond to medications or other interventions (such as endometrial ablation or hormonal therapy) may eventually require hysterectomy, especially if it leads to anemia or affects daily life.
This is a common doctor recommendation for hysterectomy, particularly for women nearing menopause.
3. Endometriosis
In this painful condition, tissue similar to the uterine lining grows outside the uterus. When endometriosis affects the uterus severely and doesn't respond to medical therapy, removing the uterus can bring long-term relief. However, it is usually recommended only in severe cases or when other treatments fail.
4. Adenomyosis
A condition in which the inner lining of the uterus (endometrium) grows into the muscular wall of the uterus. It causes intense cramps, chronic pelvic pain, and heavy periods. In some cases, hysterectomy is the only lasting solution.
5. Uterine Prolapse
This occurs when the uterus slips down into the vaginal canal due to weakened pelvic floor muscles. It can lead to urinary problems, difficulty with bowel movements, and pelvic pressure. In advanced cases, uterus removal surgery is often required to restore normal anatomy and quality of life.
6. Gynecological Cancers or Precancerous Conditions
Cancer of the uterus, cervix, or ovaries often necessitates hysterectomy. Even in cases of early-stage cervical or endometrial cancer, surgery may be the best treatment to stop the spread. For women with precancerous changes that are at high risk of progressing, hysterectomy may be advised as a preventive measure.
This is one of the most urgent medical reasons for uterus surgery.
7. Chronic Pelvic Pain
When pelvic pain is persistent and the cause is traced back to the uterus—especially in cases of endometriosis, fibroids, or pelvic inflammatory disease (PID)—a hysterectomy may be considered if all other treatments fail.
When Is Uterus Removal Necessary?
Hysterectomy is typically necessary only when:
The condition is not responding to non-surgical treatments.
The symptoms are significantly affecting quality of life.
There's a life-threatening condition, such as cancer or severe bleeding.
Fertility is no longer a concern for the patient.
There's a structural problem like severe prolapse or uterine rupture.
It’s important to note that many uterine conditions can be managed conservatively—through medication, hormone therapy, or minimally invasive procedures. But when all else fails or the risk is high, uterus removal may be the best option.
Types of Hysterectomy – What Your Doctor May Recommend
Depending on the specific condition, your doctor may recommend one of the following types:
Total Hysterectomy: Removes the entire uterus and cervix.
Subtotal (Partial) Hysterectomy: Removes only the uterus, leaving the cervix.
Hysterectomy with Salpingo-oophorectomy: Removes the uterus along with one or both ovaries and fallopian tubes.
Radical Hysterectomy: Performed mainly for cancer; removes the uterus, cervix, part of the vagina, and surrounding tissues.
Alternative Treatments Before Opting for Surgery
Before making the decision to go for uterus removal, your doctor will often explore less invasive options, such as:
1. Medications
Hormonal birth control, GnRH agonists, anti-inflammatory drugs, and pain relievers are used to control symptoms in cases like fibroids, endometriosis, or heavy bleeding.
2. Non-Surgical Procedures
Uterine Artery Embolization (UAE): Used to shrink fibroids.
Endometrial Ablation: Burns the uterine lining to stop abnormal bleeding.
Laparoscopic Procedures: Used for fibroid removal or treating endometriosis.
These options are often suitable for women who want to preserve fertility or avoid major surgery.
Psychological and Emotional Considerations
Choosing to undergo a hysterectomy is not just a medical decision—it’s a deeply personal one. Many women experience a mix of emotions including relief, anxiety, sadness, and even guilt.
As a gynecologist, I ensure that my patients are not only medically prepared but also emotionally supported throughout the process. Open conversations, counseling, and clear communication can make the journey smoother.
Doctor Recommendation for Hysterectomy – How the Decision Is Made
If you’re wondering whether your doctor’s advice for hysterectomy is the right one, here’s what’s typically considered:
Severity of your symptoms
Your age and reproductive goals
Response to other treatments
Diagnosis confirmed via imaging or biopsy
Risk of complications or malignancy
Remember, a second opinion is always an option—especially when considering a major surgery.
My Advice as a Gynecologist in Gurgaon
As a specialist in women’s health, my approach is conservative whenever possible. I recommend hysterectomy only when it's truly necessary, and when the benefits clearly outweigh the risks.
If you’re experiencing any of the conditions discussed in this article, it’s important not to delay seeking professional advice. Early diagnosis and treatment often make a huge difference—and in many cases, can help you avoid surgery altogether.
Final Thoughts
There are several valid reasons for uterus removal, ranging from fibroids and prolapse to cancer and chronic pain. But the decision should never be rushed or taken lightly.
If you're facing this decision, ensure that your doctor has explained:
All possible alternatives
The risks and benefits of surgery
The long-term impact on your health and fertility
The emotional and lifestyle changes that may follow
When done for the right reasons, hysterectomy can dramatically improve a woman’s quality of life, relieve years of pain, and prevent serious health complications.
Dr. Deepti Asthana Consultant Obstetrician & Gynecologist – Gurgaon Specialist in advanced gynecological surgery, uterine disorders, and hormonal health Reach out to schedule a consultation and get clarity on your best treatment options—from conservative care to surgery.
0 notes
Text
Spine Tumors on the Rise: Why Are Young People Being Affected and Where to Get the Best Treatment in UP?
In recent years, doctors across India have observed a noticeable increase in spine tumor cases, especially among young adults. This growing health concern has left many asking: Why are spine tumors becoming more common, and why are they affecting the younger population? Just as important—where can patients get the best treatment for spine tumors in UP (Uttar Pradesh)?
Let’s explore the causes behind the rising trend and the best options for diagnosis and treatment.
What Is a Spine Tumor?
A spine tumor is an abnormal mass of tissue that grows within or around the spinal cord or spine. These tumors can be:
Primary (originating in the spine)
Secondary/Metastatic (spreading from cancers in other parts of the body)
They may be benign (non-cancerous) or malignant (cancerous), but even non-cancerous tumors can cause serious complications if they press on the spinal cord or nerves.
Why Are Spine Tumor Cases Increasing?
Several factors have contributed to the rise in spine tumor cases, particularly among younger individuals:
🔍 1. Advanced Diagnostic Tools
Modern imaging technologies like MRI and CT scans have made it easier to detect spinal tumors, even in their early stages.
📱 2. Lifestyle and Environmental Changes
Young people today face more screen exposure, poor posture, radiation from electronic devices, and reduced physical activity—all of which can indirectly impact spinal health.
🧬 3. Genetic and Hereditary Factors
Some young patients have inherited conditions such as neurofibromatosis, which increase their risk of developing spine tumors.
🧠 4. Lack of Awareness
Many people ignore symptoms like back pain, assuming it's due to stress or a sedentary lifestyle, delaying diagnosis and treatment.
Symptoms of Spine Tumors
Persistent back or neck pain
Tingling or numbness in arms or legs
Weakness or muscle loss
Difficulty walking or maintaining balance
Loss of bladder or bowel control
Early diagnosis is critical, so these signs should not be ignored.
⭐ Best Treatment for Spine Tumor in UP – Valentis Cancer Hospital
If you’re searching for the best treatment for spine tumor in UP, Valentis Cancer Hospital stands out as a trusted and highly specialized center.
✅ Why Choose Valentis Cancer Hospital?
🧠 Expertise in Neuro and Spine Oncology
Valentis Cancer Hospital houses experienced oncologists, neurosurgeons, and spine specialists who are skilled in treating complex spinal tumors using advanced medical and surgical techniques.
🏥 World-Class Infrastructure
With cutting-edge technologies like MRI-guided surgery, CT-navigation, and precision radiation therapy, Valentis ensures accurate diagnosis and effective treatment with minimal complications.
🩺 Comprehensive Care Under One Roof
From diagnosis to rehabilitation, Valentis offers complete care. This includes:
Minimally invasive spine surgery
Chemotherapy and radiotherapy
Pain management and physiotherapy
Regular monitoring and follow-ups
💰 Affordable and Accessible
Patients from across Uttar Pradesh and nearby states choose Valentis for its affordable packages, transparent pricing, and high success rates.
🎯 Why Timely Treatment Matters
Delaying spine tumor treatment can lead to permanent nerve damage, paralysis, or even life-threatening complications. That’s why choosing the best treatment for spine tumor in UP is not just important—it’s critical.
At Valentis Cancer Hospital, every patient receives individualized care from a multidisciplinary team. Their goal is not just to treat the tumor but to improve the patient’s quality of life.
📍 Conclusion
Spine tumors are no longer rare, and the increasing number of cases in young people is alarming. Early detection, lifestyle awareness, and access to expert care are key to successful outcomes.
If you or someone you know is experiencing symptoms of a spine tumor, don’t wait.
👉 Choose Valentis Cancer Hospital for the best treatment for spine tumor in UP. Experience excellence, compassion, and innovation in cancer care.
Book your consultation today at Valentis Cancer Hospital – Where Healing Begins.
0 notes
Text
PROSTASCINT IMAGING in DETECTION of BONE METASTASES in PROSTRATE CANCER: EXAMINATION of FALSE POSITIVE and FALSE NEGATIVE RESULTS and the ACCURACIES & INACCURACIES in DETECTION & DIAGNOSIS The objective of this work is to make an extensive review of literature in the area of ProstaScint imaging effectiveness and accuracy in detecting distant metastases, and specifically bone metastases. This study specifically seeks findings concerning false positive and false negative results and the inaccuracies or accuracies in diagnosis of metastatic bone lesions due to prostrate cancer. As the knowledge and experience in the clinical use of ProstaScint Imaging in detection of bone metastases in prostrate cancer grows the capacity to use this imaging in detection of prostrate bone metastases grows as well as does the accuracy of the use of ProstaScint imagine in this area of cancer detection, diagnoses and treatment. LITERATURE REVIEW The work of Samir Taneja (2004) entitled: "Imaging in the Diagnosis and management of Prostrate Cancer" published in the Urology Review relates a study of 160 men with high-risk disease defined by Gleason score, PSA, and clinical stage, 152 were studied with ProstaScint prior to surgical staging. www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1472828" of 64 patients with positive lymph nodes, 40 were read as positive by ProstaScint scan (PPV = 62%). Of 88 patients without lymph node metastases, 63 were read as negative by ProstaScint (specificity = 72%). Overall, the sensitivity for detection of lymph node metastases was 62%." Taneja states that in the reported study that CT and MRI "...demonstrated PPV of only 4% and 15%, respectively. Given the poor sensitivity and predictive value of CT/MRI in predicting extraprostatic disease, many clinicians rely upon algorithms or monograms to predict the risk of lymph node metastases." (Taneja, 2004) Taneja relates that Polascik and colleagues conducted a comparison of www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1472828" the ability of several clinical algorithms and ProstaScint scans in their prediction of lymphatic metastases. The participants in the study were 198 men with clinical T2-3 disease undergoing radical prostatectomy. The study states findings that "...of 39% of patients in this high-risk cohort were found to have lymph node metastases at surgery. From 40.5% to 45.4% of lymph node positive patients were predicted by clinical algorithm compared to 66.7% by ProstaScint alone. When integrating ProstaScint with clinical algorithms based upon Gleason score, disease volume, and pre-operative PSA, a PPV of 72.1% could be achieved." (Taneja, 2004) Included in the study's findings is that in the evaluation of patients "...prior to treatment, the use of ProstaScint scan may be particularly useful in staging individuals in the intermediate- to high-risk category. Although limited by its risk for false positive readings in inexperienced hands, the ProstaScint scan offers a useful tool for detection of lymph node metastases in newly diagnosed prostate cancer. Its use in high-risk disease allows the appropriate selection of candidates for potentially curative therapies. Current efforts to further improve specificity include fusion of the SPECT acquired images with 3D reconstructed MRI or CT." (Taneja, 2004) it is particularly important to note the statement of Taneja as follows: "The staging ability of the ProstaScint scan has been evaluated by a number of investigators. A fundamental necessity of the scan is experience in the interpreter. As the findings of the study are often subtle, with a high risk of false positive due to bowel or blood vessels overlying the lymph nodes, there may be an improvement in interpretive accuracy as the reader becomes more experienced. In the hands of experienced readers, the scan does appear to offer a valuable tool for staging of prostate cancer. The importance of reader experience in interpretation of ProstaScint scans is made evident by the reported data regarding staging. The PPV of the study varies in published reports from 11% to 66.7% in patients selected for radical prostatectomy (RP). In those series evaluating high-risk patients, the PPV was improved, probably due, in part, to the increased prevalence of metastatic nodal disease. In most studies to date, the predictive ability of ProstaScint is superior to that of CT/MRI in detecting lymph node metastases prior to therapy." (2004) Taneja (2004) claims that ProtaScint is capable of identifying the pelvis and retroperitoneal region nodes and when tested "against the pathologic outcome of lymph node sampling, the test displayed 89% sensitivity and 76% specificity." (Tenaja, 2004) ProstaScint is stated of Tenaja (2004) to have identified 42% of extraprostatic recurrence of patients evaluated. The study of Kahn (2007) reports 42% extraprostatic recurrence in 42% of evaluated patients evaluated. In a separate and larger study, Sodee and Faulhaber (2000) followed a cohort of patients for primary or recurrent disease and relates that "ProstaScint outcomes correlated significantly with the likelihood of isolated fossa recurrence." The work of Quintana and Blend (2000) entitled: "The Dual-Isotope ProstaScint Imaging Procedures: Clinical Experience and Staging Results in 145 Patients" published in the Journal of Clinical Nuclear Medicine reports a study evaluating the effectiveness of ProstaScint for staging 145 patients with prostrate cancer, 19 newly diagnosed and 126 with recurrence. Results of the study that: "With clinical follow-up in 13 of 19 (68%) patients with primary disease, 10 of 13 (78%) had organ-confined disease. With follow-up in 64 of 126 (51%) patients with possible recurrent disease, 49 of 64 (77%) were found to have prostatic fossa activity only. Disease stage was deemed more advanced in 3 of 13 (22%) patients with primary cancer and in 13 of 64 (20%) of those with recurrent disease based on ProstaScint findings when all other imaging tests were inconclusive. Six patients with recurrent disease had negative results of their scans. In the 16 patients with more advanced disease, 3 of 59 lesions (5%) were documented as false positive, and there were no reported cases of false-negative findings." (Quintana and Blend, 2000) in one of two open-label, multi-center, uncontrolled pivotal phase 3 trials, 160 patients with a tissue diagnosis of prostrate cancer and who were considered to be high risk for lymph node metastases underwent Prostascint staging. Of these 160, 152 had an interpretable scan and surgical staging with 40 scans being true positive, 25 being false positive, 63 true negative and 24 false negative. The following figure shows the results for immunoscintigraphy. The report states that sixty-five patients, or 43% had positive Indium in 111 ProstaScint images for pelvic lymph node metastases. Of these 65 patients 25 patients (38%) did not have metastatic prostrate cancer at surgery. Eighty-seven patients (57%) had negative Indium in 111 ProstaScint imagines: Of these 24 patients (28%) did have metastatic prostrate cancer at surgery. The overall accuracy in 111 ProstaScint immunoscintigraphy was 68%. A second open label, multi-center, uncontrolled pivotal phase 3 trial involving 183 patients with a high clinical suspicion of residual or recurrent prostate cancer following radical prostatectomy underwent evaluation. Patients with a rising PSA, a negative bone scan and a negative or equivocal standard diagnostic techniques underwent ProstaScint immunoscintigraphy before biopsy of the prostatic fossa. Results shown that 158 patients had a scan that was interpretable and prostatic fossa biopsy. Of these 158, 29 scans were false positive, 70 were true negative and 30 were false negative. The following figure shows the results of this study. The study states: "Fifty-eight patients (37%) had positive Indium in 111 ProstaScint images in the prostatic fossa: Of these 50% (29 patients) did not have recurrent prostate cancer on biopsy. One hundred patients (63%) had negative Indium in 111 ProstaScint images: Of these 30% (30 patients) had recurrent prostate cancer on biopsy. The overall accuracy of Indium in 111 ProstaScint® immunoscintigraphy, as measured against prostatic fossa biopsy, was 63% (99/158)." (Rieger, 2001; ProstaScint Kit, nd) It is related that clinical trials have not studied specifically the ability of ProstaScint to image distant (extra-pelvic) metastases, and a limited number of patients with distant (primarily bone) metastases were enrolled. The study states that 13 of 16 patients, or 81% with CT evidence of distant soft tissue disease had positive extrafossa ProstaScint scans. Of the 61 patients, 35, or 57% with bone scan evidence of disease had positive Indium in the 111 ProstaScint skeletal uptake; however Indium in 111 ProstaScint imaging did not identify most sites of abnormal bone uptake on bone scan. The Indium in 111 ProstaScint scan did, however, demonstrate sites of bone marrow metastases that were not seen on bone scan in 2 of 43 patients in the phase 1 study. (Rieger, 2001; ProstaScint Kit, nd) The work of Mark Scholz entitled: "Newly Diagnose Prostrate Cancer: Evaluating the Options" states that in a multi-center study that compared ProstaScint imaging to PLND in 51 prostrate carcinoma patients who were identified as high risk for lymph node metastases, "ProstaScint surpassed the combined diagnostic performance of CT, MRI and U.S. with an overall accuracy of 81%." (2004) Scholz additionally states that other data from this study "provided evidence of the potential beneficial impact of ProstaScint imaging on health outcomes. Two patients were found to have histologically proven 'skip metastases' near the level of the aortic bifurcation, which is outside the conventional location of standard pelvic exploration. Both patients had previous pelvic lymph node dissections that were pathologically negative, but ProstaScint scans that were abnormal. The investigators noted that because patients who have skip metastases and negative pelvic lymph nodes have been found to later develop distant metastases, ProstaScint imagine was instrumental in detecting metastatic disease and prompting further investigation." (2004) The work of Murphy and Troychak (2000) entitled: "Follow-Up Prostascint Scans Verify Detection of Occult Soft-Tissue Recurrence After Failure of Primary Prostate Cancer Therapy" published in the Prostrate Journal reports a study conducted for the evaluation of the ability of ProstaScint scan in the detection of prostatic bed recurrent and metastases to regional or distant lymph nodes. The study reported is of one hundred sequential patients who were evaluated with repeated ProstaScint scans due to evidence of recurrence during the disease course. These patients were followed from November 1994 and April 1999 and had "concurrent bone scans and serum prostate-specific antigen (PSA) evaluations. They have had hormone therapy (n = 53) and/or experienced a rising PSA after radical prostatectomy (n = 38) or after radiation therapy (n = 56). Scan images were scored 0-3, where score 0 = negative, score 1= prostate bed uptake, score 2 = regional lymph node uptake, and score 3 = distant lymph node uptake. In each patient, the uptake of the follow-up scan(s) was compared to that of the initial scan." (Murphy and Troychak, 2000) Results of the study relate that the median age of participants was: "...70 years (range, 45-87), and 23 patients had a positive bone scan. The average PSA was 40.5 ng/ml (standard deviation, 223.5). There was 257 scans representing 100 patients. All patients had at least 2 scans, 35 patients had 3 scans, and 11 patients had 4 scans. No individual exhibited detectable adverse clinical reactions during or after the scan. The findings of the initial and consecutive scans were anatomically consistent in 79%, whereas in 21% there were skip metastases. In 24 patients the lesions progressed by scan and PSA, 10 patients showed progression of scan but no PSA progression, 49 patients showed no change, and 17 patients showed a remission related to adjuvant therapy." (Murphy and Troychak, 2000) Conclusions of this study state: "The consistency on repeating the scan (79%) and the high percentage of patients showing persistent uptake at the prostate bed (43%) as well as the percentage of detection of regional nodes (20%) and distant nodes (32%) reflects the importance of using the ProstaScint scan in finding occult recurrences after primary treatment failure of prostate cancer. These results are similar to those reported earlier in autopsy series studies in similar populations." (Murphy and Troychak, 2000) The work of Murphy, Snow, Brandt and Brawer (2000) reports the evaluation of prostrate cancer patients who received multiple staging tests including ProstaScint scans and states that: "Multiple serum tests were performed on archival samples from patients who participated in trials to assess the ProstaScint scan staging ability. Traditional statistical analysis as well as artificial neural network (ANN) analysis were employed to evaluate individual patients and the group as a whole. The results were evaluated so that each factor was tested for prognostic value." (Murphy, Snow, Brandt and Brawer, 2000) Methods used in this study include data which was obtained from: "...serum tests, bone scans, and ProstaScint scans were evaluated by traditional statistical methods and ANN to determine the individual value in clinical staging of prostate cancer." (Murphy, Snow, Brandt and Brawer, 2000) Results of this study state: "Two hundred seventy-five patients (180 postprostatectomy, 95 intact prostate) with prostate cancer (14 with distant metastases) were available for analysis. Data available included: clinical state (remission or progression), most recent clinical TNM stage, bone scan, and ProstaScint scan. Serum was tested for prostate-specific membrane antigen (PSMA), prostate-specific antigen (PSA), free PSA (fPSA), and complexed PSA (cPSA). Additional calculations included percent free PSA, and percent complexed PSA. Spearman individual statistical assessment for traditional group evaluation revealed no significant factors for T-stage. The free PSA and complex PSA had a significant association with node status. The distant metastases (M) stage correlated well with the bone scan and clinical stage. ANN analysis revealed no significant T-stage factors. N-stage factors showed a 95% sensitivity and 49% specificity. These factors included the presence or absence of a prostate, PSA serum levels, bone scan, and ProstaScint scans as major associated indicators. ANN analysis of the important variables for M-stage included ProstaScint scan score, and PSA levels (total, percent complexed, percent free, and fPSA). These factors were associated with a 95% sensitivity and 15% specificity level." (Murphy GP, Snow PB, Brandt J, Elgamal a, Brawer MK. (2000) Evaluation of prostate cancer patients receiving multiple staging tests, including ProstaScint scintiscans. Conclusions of the study state that: "Two hundred seventy-five patients receiving treatment for prostate cancer were evaluated by ANN and traditional statistical analysis for factors related to stage of disease. ANN revealed that PSA levels, determined by a variety of ways, ProstaScint scan, and bone scan, were significant variables that had prognostic value in determining the likelihood of nodal disease, or distant disease in prostate cancer patients." (Murphy, Snow, Brandt and Brawer, 2000) The work of Elgamal, Troychak and Murphy (1998) entitled: "Prostascint Scan May Enhance Identification of Prostate Cancer Recurrences After Prostatectomy, Radiation, or Hormone Therapy: Analysis of 136 Scans of 100 Patients" published in the Prostate Journal relates that: "Primary extraprostatic spread or failure after prostate cancer treatment can occur locally in the prostatic fossa and/or metastasize to regional and/or distant lymphatics and/or in bone." (Elgamal, Troychak and Murphy, 1998) it is reported by Elgamal, Troychak and Murphy that an evaluation of the "...ability of the ProstaScint (Cytogen Corp., Princeton, NJ) scan to identify soft tissue recurrence of prostate cancer in patients who failed primary treatment, and we monitored their responses to a secondary treatment. ProstaScint was evaluated in a series of 136 consecutive scans associated with a complete set of relevant clinical and biochemical data. These scans represented 100 patients, imaged between November 1994-May 1998, who underwent a definitive prostate cancer treatment followed by evidence of recurrence. All patients had serum prostate-specific antigen (PSA), Western-blot serum prostate-specific membrane antigen (PSMA), and bone scans. Prostatic fossa and/or lymph node biopsies were available in 33 patients." (Elgamal, Troychak and Murphy, 1998) Results of the study state: "Overall, no adverse reactions were related to any of the radioactive antibody infusions. The average age was 69 years (range, 48-89 years), serum PSA was 55.9 ng/ml (range, 0-2,185 ng/ml), and serum PSMA was 0.32 (relative intensity levels range, 0.04-0.55). The initial therapies given were radical prostatectomy (55 scans), prostate radiation (74 scans), and/or hormonal therapy (77 scans). Twelve patients exhibited a negative scan. Local recurrence alone was identified in 58 scans (42.6%). Lymph node metastases were identified in 66 scans (48.5%). Of these, 21 had regional metastases alone, and 45 had distant lymph node metastases. Ten scans showed skip lymph node metastases without regional failure. PSA significantly correlated with negative, pelvic, and extrapelvic scan findings (P < or = 0.02). PSMA correlated best with pelvic recurrence and extrapelvic metastases in prostatectomized patients. Thirty-four patients had repeated scans for monitoring treatment response. Of these patients, 19 (56%) showed progression on the second scan, consistent with persistent increase in PSA and PSMA levels in all but 2 patients. Another 11 patients showed no change, and 4 patients showed partial remission, suggesting a response to the salvage treatment. All 20 positive prostate biopsies and 4 of the 7 positive lymph node biopsies correlated with ProstaScint findings, whereas 4 of the 6 patients with a negative biopsy had negative scans (i.e., 89% sensitivity and 67% specificity). Bone metastases were identified in 42 bone scans; 45% of these showed no lymph node metastasis on ProstaScint. In another 24 patients (57%), bone metastases were detected on ProstaScint examinations." (Elgamal, Troychak and Murphy, 1998) The work of Petronis, Regan, and Lin (1998) reports a study which evaluated the usefulness of in-111 capromab pendetide imaging in the detection of prostate cancer metastases or local recurrence. The study relates that scan outcomes were "correlated with prostate-specific antigen levels, pathologic stage, Gleason score, weighted Gleason score, and clinical data. Of 51 scans, 70.6% (36 of 51) were positive. Eight patients had abnormal activity in the prostatic fossa, 12 patients had abnormal activity in the abdominal or pelvic lymph nodes, and 16 patients demonstrated abnormal activity in both areas. One patient with a positive scan underwent lymphadenectomy and was confirmed to be a true positive. Patients with a prostate-specific antigen level greater than 10 ng/ml, a weighted Gleason score higher than 4.5, or prostate-specific antigen levels greater than 2 ng/ml plus a weighted score higher than 4.5 showed positive rates of 100% (6 of 6), 88.2% (14 of 16), and 100% (6 of 6), respectively. in-111 capromab pendetide imaging was useful to detect metastases or local recurrence. Read the full article
0 notes