#PEM management
Explore tagged Tumblr posts
Text
Calling All Beings to Send Love and Peace: A Message for Our Community
Harnessing Inner Peace: A Pacing Toolkit Tool for Those Living with ME/CFS or Long Covid As we face the approach of Hurricane Milton, we are reminded of the moment when Jesus calmed the storm on the Sea of Galilee. His disciples, filled with fear, watched as He spoke these simple yet powerful words: “Peace! Be still!” And the storm settled. This is such a time for us to look at the storm that’s…
View On WordPress
#biblical inspiration#Calming techniques#chronic fatigue syndrome#emotional wellbeing#faith-based healing#healing tools#hurricane anxiety#hurricane preparedness#Inner peace#Jesus calms the storm#Long Covid#ME/CFS#meditation for chronic illness#mental health#Mindfulness#Orgyen Chowang#pacing techniques#PEM management#post-exertional malaise#Post-Viral fatigue#pristine mind meditation#resilience in chronic illness#restful awareness#spiritual growth#Spiritual healing#storm metaphors#stress reduction
0 notes
Text
Yet another one of those days when I can't concentrate on anything because the brain fog is fogging. Maybe I should just take my painkillers and go to bed.
#no spoons only knives#my spoons are in the dishwasher#pem#brain fog#me/cfs#chronic illness warrior#chronic fatigue warrior#chronic pain warrior#cripple punk#disabled problems#pain management
13 notes
·
View notes
Text
when i got my diagnoses the cfs dx felt so secondary and less of a big deal than fibro but i wish theyd put emphasis on how much you can destroy your body permanently. but ofc they wouldnt have said that bc they were still teaching GET at the time, they were recommending treatment that wouldve damaged my body so much
#🐇#sick#chronic fatigue syndrome#fibromyalgia#like idk. tagging them bc omg if you have both they are both concerns you have to manage them both#having both at least for me i thought cfs was just the chronic tiredness and pem crashes but ppl w only cfs can have very fibro sounding#symptoms too. like maybe the pain isnt all just from fibro
5 notes
·
View notes
Text
yeesh my tremors and other non-fatigue symptoms are bad today. struggled so bad putting pills into my mouth and swallowing them earlier. bleh
#i love when i manage to steady my hands and bring a cup to my face only to then violently hit myself in the face with an unexpected movement#i normally use a cup with a lid on PEM days but I need big mouthful water when swallowing pills which i find difficult with a straw#the small shakes are fine its the big movements that ruin everything
0 notes
Text
How to Install OpenSSL on Windows Computers
In this article, we shall discuss how to Install OpenSSL on Windows Computers. OpenSSL is an open-source command-line tool that is used to generate the SSL certificate and private key and is available in both versions 32 and 64 bit. Please see How to fix Windows Update Fails with Error 0x80092004, how to Fix the Port used for the Virtualhost is not an Apache Listen Port, and Shell Scripting: How…
#convert key format OpenSSL#convert PEM to DER OpenSSL#extract public key OpenSSL#generate private public key OpenSSL#how to use OpenSSL on Windows#install OpenSSL Windows#Microsoft Windows#OpenSSL installation#OpenSSL key conversion#OpenSSL key generation tutorial#OpenSSL key management#OpenSSL public key extraction#OpenSSL Windows#OpenSSL Windows installation steps#Windows#Windows 10#Windows 11#Windows OpenSSL setup#Windows Server#Windows Server 2012#Windows Server 2016#Windows Server 2019#Windows Server 2022
1 note
·
View note
Text

Property Experience Management Systems (PEMS) streamline operations, personalize guest experiences, and ultimately cultivate exceptional stays. In this article, we will explore the impact and benefits of PEMS in transforming the hospitality landscape. Read More...
#voip technology#business phones#PEM#Property Management System#pbx system#voip advantages#hotel phone system#voip phone#phonesuite direct#phonesuite dealers#pbx communications#Cloud Telephony#hotel hospitality#Cloud Calling#VoIP Protocol#SIP Protocol#Pms integration#Call booking#Hotel hospitality#Cloud technology#Business phone#VoIP Technology
0 notes
Text

I LOVE YOU
#OOMFIES IF YOU'RE EVER IN SALEM DO YOURSELF A FAVOR AND VISIT THE PEM. PLS. IT'S SO GOOD#(also while you're there get a ticket to go on a tour of the chinese house At the pem (it's an actual qing dynasty house they managed to#move here and is a separate (although i think it's free) ticket bc they need to limit how many ppl come through)#romeo.txt
1 note
·
View note
Text
Reference saved in our archive
I know some of y'all out there are all about the diagnostic/theraputic similarities between Long Covid and other autonomic disorders. Here's a preprint ya might find interesting.
Abstract Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and Long COVID are persistent multi-system illnesses affecting many patients. With no known effective FDA-approved treatments for either condition, patient-reported outcomes of treatments are invaluable for guiding management strategies in patient care and generating new avenues for research. Here, we present the results of an ME/CFS and Long COVID treatment survey with responses from 3,925 patients. We assessed the experiences of these patients with more than 150 treatments, as well as their demographics, symptoms, and comorbidities. Patients with each condition who participated in the study shared similar symptom profiles, including all the core symptoms of ME/CFS, e.g., 89.7% of ME/CFS and 79.4% of Long COVID reported post-exertional malaise (PEM). Treatments with the greatest perceived benefits were identified, which had varied effects on different core symptoms. In addition, treatment responses were significantly correlated (R² = 0.68) between the two patient groups. Patient subgroups with distinct profiles of symptoms and comorbidities showed varied responses to treatments, e.g., a POTS-dominant cluster benefiting from autonomic modulators and a cognitive-dysfunction cluster from CNS stimulants. This study underscores the symptomatic and therapeutic similarities between ME/CFS and Long COVID and highlights the commonalities and nuanced complexities of infection-associated chronic diseases and related conditions. Insights from patient-reported experiences, in the absence of approved treatments, provide urgently needed real-world evidence for targeted therapies in patient care and for developing future clinical trials.
(Disclaimer: The findings presented in this paper are based on patient-reported information and are intended for research purposes only. They should not be interpreted as medical advice. Patients are advised to consult their healthcare provider before initiating or altering any treatment.)
#mask up#public health#wear a mask#pandemic#wear a respirator#covid#covid 19#still coviding#coronavirus#sars cov 2
55 notes
·
View notes
Note
Hi there! I'm working on a modern supernatural story, and I've got a side character (the main character's best friend) who deals with chronic fatigue syndrome. He's a sweet, goofy, confident guy, and he has friends who are happy to change plans to accommodate him when he has flare-ups. They'll also help him out with chores or errands when he needs, with his consent. Naturally he gets bummed about his condition from time to time, but he's accepted that it's how he lives and with the help of therapy he's found ways to manage it. He also has plenty of hobbies and interests and grievances outside of his condition.
My question is this: I have a side-plot where the characters learn that a vampire has been feeding off him for weeks without his knowing, most likely using some kind of hypnotism. I'm wondering if the effects of consistent blood loss - fatigue, headaches, dizziness, etc - could reasonably be chalked up to a particularly bad CFS flare-up. Or would that be something where it's more likely he would notice the difference in severity of his symptoms and realize something else was wrong? Assuming the vampire can heal up any bite marks he leaves.
For the sake of clarity, he's had CFS most of his life and I'm taking care to avoid implying that it has anything to do with the vampire attacks. I'm just wondering if his symptoms would help hide the feedings or not.
Thank you!
The short answer: absolutely yes, this seems like it could be chalked up to a bad flare-up.
The long answer: I'm going to use the CDC's description of CFS/ME to lay out pretty exactly why it would work for both you and anyone wondering why exactly it would work.
A list of symptoms from the CDC has 3 core and 2 that you only need 1 out of 2 symptoms to have CFS.
Core: Lowered ability to do usual activities due to fatigue [that is not relieved by sleep/rest] that wouldn't have been an issue before illness
Core: Post-exertional malaise (PEM), which is a worsening of symptoms after physical or mental activity that wouldn't have been an issue before illness. Often described as a 'crash' and can include feeling dizzy, having difficulty thinking, headaches, or feeling ill. It can take days, months, or longer to recover from a crash and it's hard to predict how long a crash will last or what will cause it.
Core: Sleeping problesms; even a full night's sleep doesn't help symptoms much and might not help at all. Might have trouble falling or staying asleep.
Other: Problems with thinking and memory, like 'brain fog' or slowed thinking or trouble remembering things or paying attention.
Other: Orthostatic intolerance, meaning that symptoms can get worse while standing up. This can make people feel lightheaded, dizzy, weak or even faint.
I've bolded the symptoms on the list that match your stated symptoms of vampiric blood loss: "fatigue, headaches, dizziness, etc." and as you can see they match up pretty exactly!
Your character could perhaps do something that required a decent amount of mental or physical extertion, and perhaps it did or didn't cause a crash but at around the same time the vampire could have started to feed off of him. This might seem to prolong the 'crash' and your character might not think twice about it, just realize that they're feeling pretty miserable in a way not unknown to them.
I hope this helped!
PS, I really enjoy modern supernatural stories, and if you ever feel like sharing it I'd love to read this.
— Mod Sparrow
#chronic illness representation#chronic fatigue representation#mod sparrow#fantasy setting#anonymous
80 notes
·
View notes
Text
Coping with ME/CFS in the Aftermath of Hurricane Helene: On-the-Spot Practices for Pacing and Recovery
Rest now, breath by breath,Let each moment cradle you—And nourish your soul. As we recover from the aftermath of Hurricane Helene here in Florida, many of us are left not only dealing with physical damage and power outages but also with the internal toll such intense stress can take. For those of us living with chronic fatigue syndrome (ME/CFS), the impact can be particularly difficult, as our…
#calming the nervous system#chronic fatigue syndrome#chronic illness recovery#energy conservation#grounding techniques#healing after hurricane#health#hurricane recovery#hurricane stress#managing tinnitus#ME/CFS#ME/CFS coping strategies#meditation#meditation for fatigue#mental-health#Mindfulness#mindfulness for chronic fatigue#pacing and recovery#pacing strategies#PEM management#post-exertional malaise#post-hurricane care#Post-Viral fatigue#second arrow#sensory overload#stress management#Stress relief#tinnitus#tinnitus relief#wellness
0 notes
Text

From The #MEAction Network
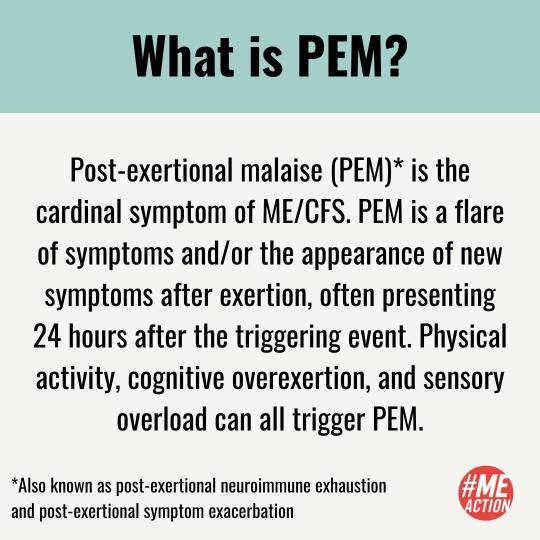
Wondering about the terms PEM or pacing? Have you seen #StopRestPace and were curious as to what it referenced? Maybe you have been in our community a long time and want to save some easy ways to explain these concepts to others. Perhaps you have seen pacing misused and want to help clear that up. We hope this post helps!
#StopRestPace is a campaign created by #MEAction to help our community spread the word to those who were experiencing PEM after COVID-19 to rest and pace their activity.
What is PEM? Post-exertional malaise (PEM) is the cardinal symptom of ME/CFS. PEM is a flare of symptoms and/or the appearance of new symptoms after exertion, often presenting 24 hours after the triggering event. Physical activity, cognitive overexertion, and sensory overload can all trigger PEM.
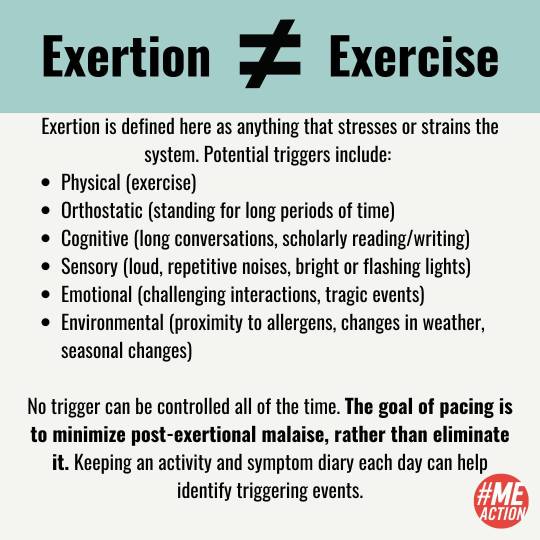
Sometimes exertion is misunderstood as exercise. Exercise is simply one form of exertion. Exertion is defined here as anything that stresses or strains the system. Exertion can be physical, orthostatic, sensory, cognitive, emotional, or environmental. No trigger can be controlled all of the time. The goal of pacing is to MINIMIZE post-exertional malaise rather than eliminate it.
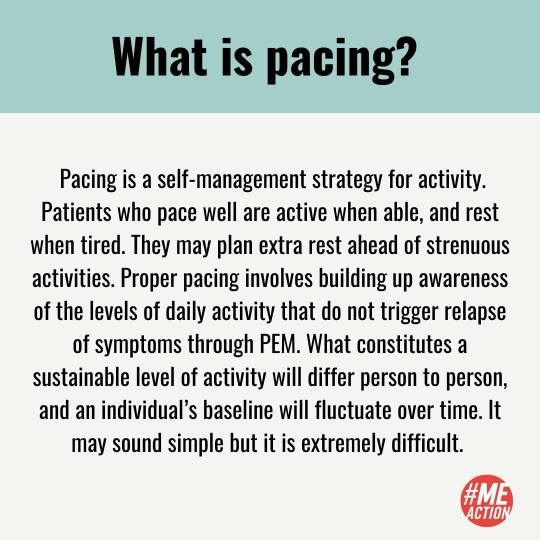
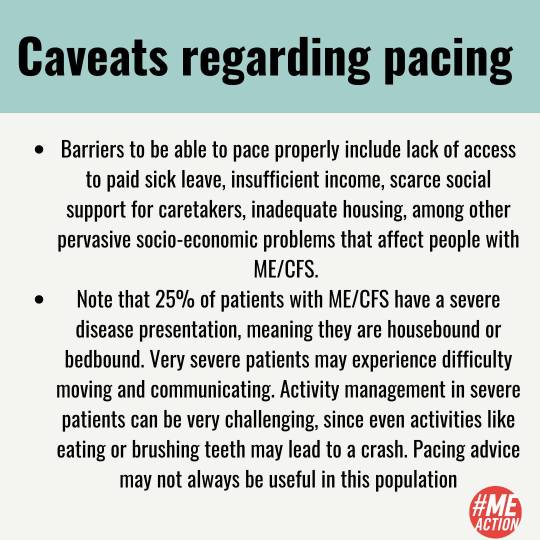
Pacing is a self-management strategy for activity. Patients who pace well are active when able and rest when tired. Proper pacing involves building up awareness of the levels of daily activity that do not trigger relapse of symptoms through PEM. While this sounds simple, it is incredibly difficult. Activity management in severe patients can be very challenging since even activities like eating or brushing teeth may lead to a crash. Pacing advice may not always be useful in this population.
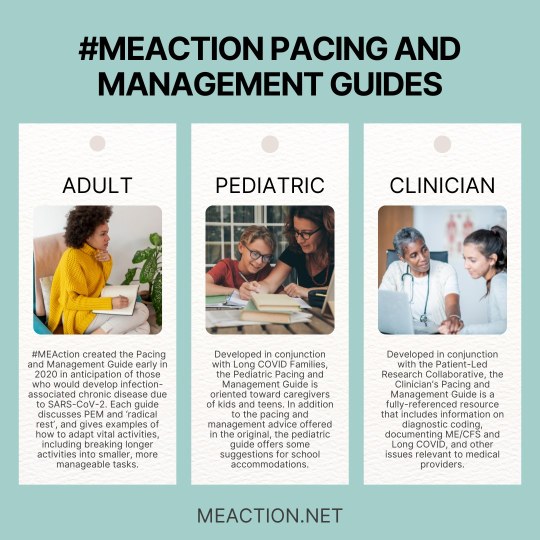
#MEAction offers three pacing guides - adult, pediatric, and clinician - on our site. Our pediatric guide was developed in conjunction with Long Covid families. Our clinician's guide was developed with Patient-Led Research. https://www.meaction.net/resource/pacing-and-management-guide
268 notes
·
View notes
Text
My 2024:
started while still in that horrible crash where I could barely manage to go to the bathroom once a day.
slowly got a bit better but I'm still stuck in the a bit better stage where i can't really go anywhere or do anything unless it's not far and i can lie down and it's quiet and it doesn't take too long.
I went to my monthly doctor's appointments so I'm legally allowed to continue not going to work & getting my sick pay.
started wearing support stockings bc my blood flow is fucked up, tried to get a doctor to prescribe me medical ones but he refused
was told by ~3 doctors that I should do sports and go to a Reha and do physiotherapy, which is exactly what experts say NOT to do when you have PEM
shitty doctor told me I'm just lazy and don't want to go to work and it's my own fault I'm feeling like this bc I'm just not working on myself.
switched doctors! new doctor was better for a few months but then started recommending the same stuff, hasn't called me lazy yet at least.
felt worse in the summer bc my body can't really adjust to temperatures anymore so the heat was fucking me up.
was referred to a cardiologist who didn't find anything. which makes sense bc my heart feels completely fine.
went to physio for a few weeks bc we found one who only did massages so i could lie down and not be forced to do sports. woman who did it was convinced i was only "scared" of doing sports.
we got an inflatable shower thingy so my mom can now wash my hair while I'm lying on the couch!! my mom has also started washing my body for me (in small increments, immediately toweling the individual parts off so the temperature difference isn't too big)
visited the cats a lot :)
watched lots of shows and movies and TV in general (quietly)
Thatse it. Wear a mask everyone! 😷
#doddie redet#long covid#me/cfs#year in review#next year hopefully I'll get an official diagnosis. bc my Krankengeld will be running out.#2024
16 notes
·
View notes
Text
Post Exertional Malaise (PEM) - What is it?
describes the worsening of your symptoms after minor physical and/or minor mental exertion.
can occur within 48 hours of activity, leaving you worse for days, weeks, months or even years.
What it DOES NOT describe is that the minor physical or minor mental exertion can come from*:
- sitting up or rolling over in bed
- a coughing fit
- DIY noise
- the TV being too loud
- using the bathroom
- getting too cold or too warm
- too much light in the room
- a phone call or text conversation
- a hot shower or bath
- the noise of a hairdryer, of dishes being put away, the vacuum
*this is not a complete list by any means, it's all I can manage
For me, PEM has been one of the hardest to accept, knowing that the smallest of things will make my symptoms worse.
I genuinely used to think it was something people were wrongly trying to pinpoint because we usually have no other reasons & crave reasoning, so "it can't be from doing ONLY that," right?? Wrong.
I'm already having these symptoms, but now I'm going to suffer more with the symptoms because of some hollow event like brushing my damn teeth??
It's hard to accept because these things did not affect me this way before, but now, I cannot bear them.
Being in a state of PEM is to be in a state of pure suffering. You feel like you're dying but you're not, you're waiting for it to stop.
PEM makes me extremely depressed & all I want to do is be alone. In fact I HAVE to be alone, because everything is too overstimulating & makes it last longer.
It makes me extremely irritable, when I have to strain my way through the day, forcing my head to stay up with my hands, when all I may have done is fold some washing.
Stretching and straining my eyes open like I have been awake for 3 weeks. Trying to stand up but it's like someone in front of you forcing you back down with their body weight, every single time.
I get unbelievably apathetic towards PEM, because "this is who I am now" & I DESPISE IT.
Being ill, PLUS being in a state of PEM is living torture. It's the antithesis of everything I aspired to be. It is NOT ME.
#post exertional malaise#PEM#chronic life#chronic pain#chronic illness#chronically ill#chronic fatigue#fibromyalgia#myalgic encephalomyelitis#mental health#spoonie problems#chronic migraine#out of spoons#sorry for being depressing#i'm so tired#chronic disability
120 notes
·
View notes
Text
ME/CFS AWARENESS MONTH
Hello and happy May! As of today, it's officially ME/CFS Awareness Month, so I have compiled some resources to spread in the hopes of informing and bringing attention to this disease.
What is ME/CFS?
ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome) is a complex and debilitating systemic disease that varies in severity and presentation between patients. Some common symptoms are fatigue, sleep problems, widespread pain, difficulties in thinking and memory, and PEM. PEM (post-exertional malaise) is a hallmark of this illness, defined as a worsening of symptoms after mental, physical or emotional exertion that can last from days to even weeks.
Some other symptoms include: gastrointestinal problems, dizziness, difficulty concentrating, changes in mood, headaches, sore throat, skin rashes, musculoskeletal pain and heart palpitations. Science is still unsure how ME/CFS affects the body, but in many patients it appears after an infection with a virus.
There are no tests for ME/CFS as of May 2024, and the only method of diagnosis is a process of exclusion. As such, ME/CFS is critically underdiagnosed and many suffer without knowing. People with this disease are often recipients of medical gas lighting and negligence, with the average diagnosis taking around 1-5 years.
There is no cure, and there are limited treatments, most aiming to address individuals symptoms or comorbidities. Despite the misinformation still spread around, exercise is not a recommended treatment and can cause great harm to ME/CFS patients.
How Can You Help?
There are many organizations working toward awareness and quality of life for ME/CFS patients, and I'll list some of them below. This is not an exhaustive list, but be aware that there are many web sites that spread misinformation and harmful statements: any that talk about a cure or exercise therapy are generally ones to avoid.
If you can, please take a look at the information the listed sites provide and share their knowledge in whatever ways possible. I'll also include some resources for ME/CFS patients, and I encourage allies to look as well.
I hope you have a wonderful May, and to all fellow ME/CFS sufferers, know that you are not alone. We can do this.
(Also, please let me know if there are other sites you recommend, or if there are any personal experiences you would like to share. Treat this as an open invitation to share your stories if you are comfortable.)
Links;
#chronic illness#disability#me/cfs#myalgic encephalomyelitis#chronic fatigue syndrome#chronic pain#me/cfs awareness month
17 notes
·
View notes
Text
TRYING TO GET BETTER MAKES ME (CFS) WORSE
im showing all the textbook symptoms. i even bought books about it that i'll have to read. i'll have to learn how to pace and spend the rest of my life using half my energy to manage where i spend my energy.
my life is ruined. it was already an uphill climb from where i ended up, and now the engine has crapped out.
im wasted. every aspiration, hope and dream, goal and expectation, wish and passion. dead.
im a supplement junkie, an impossible patient, a zebra with no stripes and no reason to test or treat. im a faker freak misanthrope. im a covid dead-ender, a victim of victim mindset; a statistic.
i will never be able to live and have fun doing active things again, and i will look back on when i could (and at everyone who still can) with envy and shame and grief and frustration. anger i can't let myself feel because getting worked up triggers PEM and anything could worsen my baseline, including worrying about worsening my baseline.
im finally exactly what i wanted to be at 14 when my mental health was at its worst: a perfect candidate for voluntary euthanasia.
3 notes
·
View notes
Text
Also preserved in our archive
By Simon Spichak
The proposed Canadian guidelines for treating Long COVID pose harm to patients and risk psychologizing the disease.
Researchers involved in the organizations Cochrane Canada and the McMaster GRADE Centre at McMaster University are developing guidelines to prevent and treat Long COVID in Canada. Their effort is supported by the Public Health Agency of Canada and their recommendations would likely have major sway in the way Long COVID is treated if adopted.
Every month, they release new recommendations and provide an opportunity for public comment. On November 20th, the group released a new set of Canadian Post-COVID Condition (CAN-PCC) recommendations which propose harmful and ineffective treatments: Exercise to prevent Long COVID and cognitive behavioral therapy (CBT) to treat post-exertional malaise (PEM).
The recommendations are made on the basis of what CAN-PCC describes as “very low certainty” evidence and disregard the lived experience of patients living with Long COVID and similar conditions like myalgic encephalomyelitis (ME/CFS).
Several patient advocates and groups have mobilized in response. Adriana Patino, who leads Long COVID Canada said that group members were shocked and angered by the recommendations who are losing trust in the guidelines as the authors “are not following the most recent research nor listening to the patients' voices.”
Many don’t want to comment on the recommendations any longer because they feel they aren’t being listened to in the first place.
“Why are they asking for us to review these recommendations when it doesn't seem like they're listening?” Susie Goulding, a Canadian with Long COVID and CEO of the newly formed Long COVID Society told me over the phone.
I asked experts to take a look at the recommendations as well.
“The first thing that strikes me about the recommendations is that they are opposed to current clinical guidelines in Long Covid and ME/CFS,” said Todd Davenport, professor of the physical therapy program at the University of the Pacific. He added the recommendations are too strong given the low level of evidence underpinning them.
Davenport explained that most policymakers and doctors are unlikely to read through the weak underlying evidence and take the recommendations at face value.
“I'm honestly just so flabbergasted,” Jessica DeMars, physiotherapist and owner of BreatheWell Physio told me. “It feels a lot like they decided beforehand what they were going to recommend and then somehow managed to manipulate the study findings ever so slightly, giving themselves an inch to take the mile.”
I took a deep dive into the recommendations and put together insights from patient advocates and experts about the potential harm they pose to people with Long COVID.
The guidelines are open for public comment until November 27th at 11:45 P.M. The group in charge of developing these guidelines may update the recommendations in response to the comments.
Summary Recommendation #1 to research the keto diet is based on incomplete data presented at one scientific conference. It hasn’t been peer-reviewed or published in any journals.
Experts say that Recommendation #2 which suggests exercise to prevent Long COVID is not supported by the evidence, and could actually increase the chances of developing Long COVID.
Recommendation #3 recommends against chest X-rays for Long COVID patients who weren’t hospitalized. This contradicts guidelines in The Lancet and evidence showing lung problems can be spotted using chest imaging.
Recommendation #5 risks further stigmatizing and psychologizing Long COVID.
Recommendation #8 which suggests the use of cognitive behavioral therapy (CBT) to treat post-exertional malaise is made on the basis of weak evidence, contradicts existing clinical guidelines for ME, and poses direct harm to patients.
Recommendation #1: Research the Keto Diet for Prevention The first recommendation, which is meant to guide researchers who are studying Long COVID, is made on the basis of a research conference abstract.
A conference abstract is a poster or talk that is presented at a scientific meeting but importantly the data that’s presented has not yet passed scientific peer-review and has not been published in a scientific journal. The recommendations is based off of the incomplete information from the abstract.
“The conference abstract did not provide information on when and how long to start the ketogenic diet,” CAN-PCC writes.
It isn’t clear why this one unpublished study was picked as the basis of a research recommendation. Ketogenic diets are very restrictive, expensive, and many people even in a research setting give up on them making it unlikely that research into the ketogenic diet would translate into real world benefits.
Recommendation #2: Exercise to Prevent Long COVID The CAN-PCC makes this recommendation on what they admit is “very low certainty” evidence. The researchers developing the guidelines compiled the evidence from clinical trials that tested exercise in people with COVID-19. But none of the studies measured whether participants developed Long COVID.
DeMars and Davenport don’t think the evidence the researchers compiled supports their recommendation.
Davenport explained that exercising during an acute COVID-19 infection is dangerous. Exercise while you’re sick can worsen myocarditis, inflammation of the heart muscles caused by SARS-CoV-2, and increase the risk of a blood clot. Exercise around others “is also an efficient way to spread COVID-19,” he added.
Many people develop post-exertional malaise (PEM) as a result of exercise. PEM is a common symptom of Long COVID and ME/CFS that leads to an energy crash after minimal physical or mental exertion.
“There is a very real risk that we actually increase the number of individuals with Long COVID by asking people to exercise too soon,” said DeMars.
Many people with Long COVID experience their first crash by exerting themselves too soon after an initial infection, leading to worsening symptoms.
“There's also several thousands testimonials from patients who were previously very active and/or athletes who tried to remain active during or shortly after their Covid infection and now they have organ damage and/or developed PEM and/or increased the severity of their symptoms,” Patino said.
None of the studies the researchers used to make this recommendation measured PEM.
The recommendation comes with a note that says that for individuals with post-exertional malaise “exercise or rest recommendations should be made under the supervision and guidance of a health care professional.”
This statement may imply that the CAN-PCC authors believe that exercise may be effective for treating PEM, though it is neither safe nor effective. At the time of publication, the team developing these guidelines has not responded to a request for clarification.
Recommendation #3: No X-Rays CAN-PCC advises against ordering chest X-rays for people with Long COVID unless they were hospitalized due to their initial infection, based on a “very low certainty” or evidence. They make this recommendation because there is no evidence of doctors using X-rays as a diagnostic test.
Even though a chest X-ray won’t definitively diagnose Long COVID, it provides important clues about a person’s symptoms. Many people with Long COVID develop persistent respiratory issues that affect their quality of life. Researchers have spotted respiratory issues using CT scans in people with Long COVID who weren’t initially hospitalized. CT scans are a medical imaging tool powered by X-rays.
A recent set of clinical guidelines published in The Lancet also recommends a chest X-ray for people with Long COVID who are feeling breathless after exercise. Spotting the problem allows doctors to refer patients to the right specialist for treatment.
Recommendation #5: Using Quality of Life Questionnaires The recommendation suggests using psychological tests to assess Long COVID patients based on a “very low certainty” of evidence.
In his blog, Brian Hughes, psychologist and professor at Galway University wrote:" “For persons of all genders, anything that reinforces a stereotype of Long COVID as a psychological state risks deflecting patients onto an irrelevant (e.g. psychiatric) treatment pathway and away from appropriate medical care.”
He also raised concerns that doctors will use these psychometric measures more often in in women, who are more likely to develop Long COVID and less likely to be believed by doctors.
The right questionnaires could be helpful though. Better measures like the DePaul Symptom Questionnaire take stock of fatigue and PEM.
Recommendation #8: CBT for Post-Exertional Malaise (PEM) CBT is a form of therapy that helps people work to change their beliefs. While it can be effective for mental health, there is no evidence that it works for chronic illness or PEM.
As with the other CAN-PCC guidelines, the authors made this recommendation based on “very low certainty” evidence.
Since studies have found that many people with Long COVID develop ME/CFS, another post-viral condition that causes PEM, the guideline’s authors took a look at the evidence of using CBT for people with ME/CFS.
“I can't even believe we are going there,” DeMars said. “Yes people are dealing with newfound mental health issues - primarily due to having to deal with new onset chronic illness and disability, but learning to "think positively" is not going to make their health issues go away.”
Davenport added that the studies the researchers used to arrive at this recommendation didn’t require PEM for diagnosis or use objective measures in the study.
The recommendation also ignores what leading ME experts and patients already know: CBT doesn’t work for ME. The CAN-PCC team failed to engage with any research that exposed methodological flaws in major studies that have assessed CBT as a treatment for ME. The UK’s national health insurer, NICE, advises against the use of CBT for ME.
“By making a suggestion that CBT will somehow improve recovery, [CAN-PCC] pushes the idea that LC is psychosomatic - and blatantly ignores the plethora of data that shows otherwise,” DeMars said.
There is mounting evidence that PEM has a biochemical basis. A viral infection that leads to the development of post-exertional malaise may disrupt the healthy function of mitochondria, which turn nutrients into energy. People with post-exertional malaise also show a build up of lactic acid in the blood which is associated with the severity of symptoms.
“An illness is not going to be cured by thinking happy thoughts,” Goulding said.
These recommendations repeat the same mistakes researchers made with ME. The condition was stigmatized by doctors who pinned it on women being hysterical in the 1980s, shutting down any research into the underlying causes and making it one of the most stigmatized and misunderstood diseases. Even today, many doctors still don’t understand ME and assume that patients aren’t trying hard enough to get moving and improve.
“Recommendation #8 is simply making all the same mistakes in Long Covid that we have made historically in ME/CFS,” Davenport added.
We Can Do Better Experts and patients are equally frustrated that the guidelines are ignoring existing research and clinical guidelines.
“I think I’m just incredibly disappointed that we seem to be repeating the same mistakes every time a new group of individuals are left chronically ill after an infection,” Sabrina Poirier, a patient advocate and co-founder the ICanCME Research Network told me.
I reached out to the committee developing these recommendations for comment but have not heard back at the time of publication.
“Exercise and CBT are just not appropriate treatments to be pushed and we’ve known that for so long now,” Poirier said. “Why is it that community knowledge and wisdom are still so undervalued in science? Why is the research we have on this topic ignored or explained away?”
#mask up#public health#wear a mask#pandemic#covid#wear a respirator#covid 19#still coviding#coronavirus#sars cov 2#long covid
68 notes
·
View notes