#Human papillomavirus (HPV) Vaccine
Explore tagged Tumblr posts
Text

Wishing a Sam a speedy recovery and smiley day! 💛🥹
#i felt like i needed to do something so i made a meme#yes it does come off as a little bit threatening but that's only because it kind of is 💛💙#critical role#sam riegel#cancer#hpv vaccine#critrole#critrole memes#vaccines#vaccination#medical#fcg#cw cancer#tw cancer#tonsil cancer#human papillomavirus#needle tw#cw needles#cr memes#cr shitpost#courtesy of me#critrole meme#crit role
655 notes
·
View notes
Text
Human Papillomavirus (HPV) Vaccines Market Analysis, Size, Share, and Forecast 2031
#Human Papillomavirus (HPV) Vaccines Market#Human Papillomavirus (HPV) Vaccines Market Size#Human Papillomavirus (HPV) Vaccines Market Research
0 notes
Text
Around 1,000 young girls vaccinated for HPV in 3-day Las Piñas City vaccination drive
Residents of the City of Las Piñas, around one thousand young girls got vaccinated for HPV during the 3-day vaccination drive at Robinsons Place Las Piñas, the City Government announced via social media. Vice Mayor April Aguilar appeared and observed the activities there. To put things in perspective, posted below is an excerpt from the social media post of the City Government. Some parts in…

View On WordPress
#anti-vaccine#April Aguilar#April Aguilar-Nery#Asia#Blog#blogger#blogging#cancer#Carlo Carrasco#cervical cancer#City Government of Las Piñas#City Health Office#City of Las Piñas#Facebook#geek#governance#health#health care#healthcare#Human Papillomavirus (HPV)#kabataan#Metro Manila#National Capital Region (NCR)#NCR#news#Philippines#Philippines blog#Pinoy#public service#Robinsons Las Piñas
0 notes
Text
Gardasil: Your Superhero in the Battle Against HPV
Unlock the Power of Gardasil: Your Shield Against HPV! Dive into a world where prevention meets empowerment. Stay informed, stay protected!
HPV (human papillomavirus) is the most common sexually transmitted infection. Nearly all sexually active individuals will contract one or more strains of HPV at some point. While most HPV cases resolve on their own, infections from high-risk strains can lead to serious health issues if left untreated. This is where the Gardasil vaccine comes in. HPV is a Common Virus HPV is primarily spread…
View On WordPress
#Cervical Cancer#Gardasil#Genital Warts#Health Prevention#HPV Protection#HPV vaccine#Human Papillomavirus#Vaccination#Vaccine Safety#Wellness Tips
0 notes
Text
Article
"Every year, over 350,000 women die from cervical cancer and another 660,000 are diagnosed. [Note: Plus trans men and other trans people with a cervix.] As a consequence, children are orphaned, families impoverished and communities diminished by the loss of mothers, wives, daughters and sisters.
And yet, unlike most other cancers, almost all these cases and deaths can be averted. We have powerful vaccines that can prevent infection with the human papillomavirus (HPV) that causes cervical cancer; we have diagnostics to detect it early; and we have treatments for those it strikes. With these tools, cervical cancer can not only be stopped; it could become the first cancer to be eliminated. Some high-income countries are already close to elimination, meaning fewer than four cases per 100,000 women.
But in many low- and middle-income countries, these tools are still not available, which is why 94% of cervical cancer deaths occur in those countries.
In 2018, WHO launched a global call to action to eliminate cervical cancer, which was followed in 2020 by the adoption by all 194 WHO Member States of a Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. The strategy calls for countries to achieve three targets by 2030: 90% of girls fully immunised against HPV; 70% of women receiving timely screening; and 90% of those found with precancer or cancer accessing treatment.
These targets are not just aspirational, they are achievable, even in low- and middle-income countries. Bhutan has already reached the targets, the first to do so in the South-East Asia region.
Since introducing the HPV vaccine in 2011, Rwanda has reached vaccine coverage of 90%, and today announced its national goal to reach the 90-70-90 targets three years ahead of schedule, by 2027. Already, in two districts – Gicumbi and Karongi – Rwanda is meeting those goals. Nigeria, which introduced the HPV vaccine in October last year [2023], has already vaccinated 12.3 million girls.
We have the tools and the opportunity to eliminate cervical cancer.
Since WHO issued the global call to action in 2018, more than 60 countries have introduced the HPV vaccine into their immunisation programmes, bringing the total to 144 countries that are routinely protecting girls from cervical cancer in later life. With scientific advances, we can now prevent cervical cancer with just a single dose, which 60 countries are now doing.
The largest provider of HPV vaccines to low- and middle-income countries is Gavi, the Vaccine Alliance, which plans to vaccinate 120 million children between now and 2030. But this plan requires that investments in health are sustained. We are also counting on manufacturers to confirm and honour their commitments to provide HPV vaccines to low- and middle-income countries in the coming years, to avoid the supply constraints that held back progress in the past.
But we cannot rely on vaccines alone. The impact of the rapid scale-up in vaccinating girls now will not be seen for decades, when they reach the adult years when cervical cancer typically appears. To save lives now, we must match the increase in vaccination with increases in screening and treatment.
Decades ago, as more women gained access to pap smears in developed countries, the mortality associated with cervical cancer dropped rapidly. Today, even better tests are available. Over 60 countries now include high-performance HPV tests as part of their screening programs. Women can even collect their own samples for HPV testing, removing more barriers to life-saving services. In Australia – which is on track to become one of the first countries in the world to achieve elimination – more than a quarter of all screening tests are now done this way...
Several countries are also investigating the use of artificial intelligence to enhance the accuracy of screening in resource-limited settings. When women are found with precancerous lesions, many are now treated with portable battery-powered devices, which can be operated in remote locations."
-via The Telegraph, November 18, 2024. Article written by Dr Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization (WHO).
#cancer#cw cancer#fuck cancer#vaccines#hpv#cervical cancer#women and girls#vaccines work#public health#world health organization#womens health#healthcare#pap smear#obgyn#cancer treatment#cancer awareness#good news#hope
1K notes
·
View notes
Text
Original article submitted:
“Let’s stop spreading fake news.”
This is the appeal of the panel of doctors and specialists who spearheaded the freshly held health talk on cervical cancer titled #TimeToTalkAboutHPV: A health forum on HPV prevention and cancer control. Organised by the Cervical Cancer Prevention Network of the Philippines (CECAP), together with the Asia & Oceania Federation of Obstetrics & Gynecology (AOFOG), the Philippine Obstetrical and Gynecological Society (POGS), and MSD in the Philippines, the media forum aims to serve as a reminder that cervical cancer is preventable with regular screening tests and the HPV vaccination.
“We should stop spreading wrong information that cervical cancer immediately means a death sentence. We must stop encouraging wrong beliefs about the disease, screening and the vaccine,” patient advocate Carmen Auste appealed to the media.
Cervical cancer is largely preventable through both vaccination and screening for precursor lesions (pap smear at least every three years and HPV DNA testing for women starting age 30), with appropriate follow up and treatment. With access to accurate information, preventive services, and routine gynecological care, most cases of the disease can be prevented and successfully treated at an early stage.
In spite of this, cervical cancer ranks as the 2nd most frequent cancer among women in Philippines and the 2nd most frequent cancer among women between 15 and 44 years of age. Current estimates indicate that every year 7,897 women are diagnosed with cervical cancer and 4,052 die from the disease.
Cervical cancer develops at the entrance to the uterus from the vagina and around 99 percent of the cases are linked to HPV or human papillomaviruses. Modes of transmission include sexual contact, skin-to-skin contact and rarely, through objects exposed to the virus.
It’s a highly-treatable disease if detected at its early stages. The precancerous stage provides ample window for detection and treatment, and it could take as long as 30 years before it reaches malignancy. However, it is one of the most common type of cancers and common cause of cancer-related deaths worldwide, affecting mostly young, uneducated women from poor countries.
But more recently, COVID-19 has taken a toll on women’s health as studies have shown a gap in missed routine preventative exams and screening visits. “I think the world has been focused on Covid for the past 2 ½ years and we have overlooked other health concerns,” said Dr. Anna Lisa Ong-Lim, professor and chief of division of infectious and tropical disease in Pediatrics University of UP Manila College of Medicine. “It is only recently when vulnerabilities to vaccine-preventable diseases are being noticed once again.”
Things you need to know about HPV
One life-altering issue that deserves focus is the huge burden that continues to threaten women and men, including teenagers worldwide, caused by the human papillomavirus (HPV). “HPV is a virus that causes a wide-range of diseases,” said MSD executive director of medical affairs for vaccines and infectious disease Dr. Mel Kohn.
“Apart from cervical cancer, the 2nd leading cancer for Filipinas, HPV can give men head and neck cancer, anal cancer for both sexes and a variety of less common but also devastating kinds of cancers,” he enumerated. Examples are vaginal and vulvar cancers, and penile cancer.
“Genital warts, while it doesn’t kill you, can be quite devastating,” interjected Dr. Kohn. “It is quite common and very difficult to eradicate. Imagine the psychological toll on the patient. Again, prevention is the best approach here.”
HPV is common. It is passed from one person to another during sexual contact. “It’s a quiet epidemic unlike COVID,” he warned. Unlike the measles that have obvious expression, “you don’t immediately see it when you meet somebody but it’s there and has been growing rather insidiously.”
The Philippines has a population of 37.8 million women ages 15 years and older who are at risk of developing cervical cancer. About 2.9% of women in the general population are estimated to harbor cervical HPV-16/18 infection at a given time, and 58.6% of invasive cervical cancers are attributed to HPVs 16 or 18.
Although some of the infections from this commonly occurring virus with more than 100 types usually go away on their own, at least 14 types of HPV have been found to be cancer-causing.
The age indication for HPV vaccines is as young as nine years old to both girls and boys. Teens and young adults through age 26 years who didn’t start or finish the HPV vaccine series also should have HPV vaccination. Women up to age 45 may be eligible for vaccination after discussing with their provider.
According to Dr. Ong-Lim, they are targeting the young ones because of their increased susceptibility to infections.
“That particular age group demonstrates optimal immune response. Also, only two doses are needed to achieve protection,” she shared.
But more importantly, giving the vaccine at a younger age ensures that they are already protected before they become sexually active. “HPV vaccines work best when given before exposure to the virus. We must try to catch that window when the immune system really responds very well to it,” explains Dr. Ong-Lim
Manila Declaration: Call to Action Against Cervical Cancer chair and practicing OP-Gynecologist Dr. Jean AnneToral mentions that the young and adult fertility study done recently, indicates that the average age Filipina women become sexually active is 18.2 years old. “Giving the vaccine at age 9-15 would be beneficial as there is no life event that exactly pinpoints exposure to HPV apart from age of sexual debut,” she said.
There will be seven to eight out of 10 women who would be exposed to HPV at one point in their life, “But not all women will develop cervical cancer,” assures Dr. Toral. The probability of HPV exposure developing into cancer increases if a patient smokes, is exposed to other sexually-transmitted diseases and has HIV.
School-based HPV vaccination
As part of the government’s effort to protect children and adolescents from vaccine-preventable diseases, the Department of Health together with partner agencies, rolls out the School-Based Immunization (SBI) Program.
The SBI Program includes measles, rubella, tetanus, diphtheria (MR-TD) and human papillomavirus (HPV) vaccines that are administered to eligible students in public elementary schools. The inclusion of HPV vaccination in the SBI Program aims to protect young women from cervical cancer later in life, among other diseases associated with HPV.
Under the DOH’s SBI Program, HPV vaccination is given to grade 4 based on DOH’s recommended age group to receive the two doses of HPV vaccine, six months apart, for protection against cervical cancer.
Prior to administering the vaccine, parents’ consent must first be obtained by school officials. That is why vaccination education campaigns usually highlight the role of parents in fortifying the health shield of their children through timely vaccination against diseases.
Due to the COVID-19 pandemic, the HPV vaccination, which was formerly delivered through the SBI Program is now being shifted as part of the Community-based Immunization to be able to still deliver HPV vaccination to young girls amidst the pandemic to protect them against cervical cancer and other HPV-related diseases and cancers.
Towards a cervical cancer-free future
The elimination of cervical cancer has been defined as achieving an incidence rate low enough for the disease to be considered controlled as a public-health problem; this threshold has been defined by the WHO as fewer than 4 cases per 100,000 women per year.
To accomplish this, every country must reach and maintain three key targets, within the lifetime of today’s young generation. The first is for 90 per cent of girls to be fully vaccinated against the human papillomavirus (HPV) by the age of 15. The second is to ensure that 70 per cent of women are screened using a high-performance test by the age of 35, and again by age 45. The final target is for 90 per cent of women with pre-cancer to receive treatment and for 90 per cent of women with invasive cancer to have their condition properly managed.
Achieving this vision and each of the elimination targets will require a whole-of-society and multisectoral approach to ensure health systems prioritize women and girls. Individuals, families, communities, , civil society, and government agencies at all levels have a role to play in championing greater awareness, education, and social support.
Auste said that the Philippines is among the countries that declared commitment together with WHO to finally eradicate cervical cancer in the country by 2040, and by 2030 worldwide. “There is already one type of cancer that we can delete or ‘block’ like social media,” she humored. “To attain that goal, we must augment HPV vaccine uptake and educate the Filipinos on HPV, vaccines and cancers caused by HPV,” she said.
Auste mentioned SUCCESS ('Scale-up Cervical Cancer Elimination with Secondary prevention Strategy') project as one of the advocacies recently launched in selected barangays. Led by Expertise France and delivered in collaboration with Jhpiego and Union for International Cancer Control (UICC) in support of WHO, the project aims to deploy innovative solutions to fight cervical cancer in four countries, including the Philippines.
At this critical juncture, we must empower women and rally our neighbors, community leaders, and governments to take action and save thousands of lives. If widespread, high coverage of these interventions can be achieved by 2030 and maintained, research predicts cervical cancer can be eliminated in most countries globally by 2120—avoiding over 63 million deaths of women globally.
Together, let’s commit to women everywhere to end cervical cancer. ###
#TimeToTalkAboutHPV: A health forum on HPV prevention and cancer control#MSD Philippines#human papillomavirus#HPV#cervical cancer#HPV Vaccine#preventable disease
0 notes
Text
"Understanding Human Papillomavirus Infection: Causes, Symptoms, Treatment, and Prevention"
I. Introduction Human Papillomavirus Infection “HPV infection” is a common sexually transmitted infection caused by a virus that affects both men and women. It is estimated that approximately 79 million people in the United States are currently infected with HPV, with 14 million new infections occurring each year. HPV is spread through skin-to-skin contact during sexual activity, including…
View On WordPress
0 notes
Text

Looking for travel clinic, vaccination, prescription, and health support services at Burnham, Slough, Maidenhead, and Windsor.
#Human papillomavirus (HPV) Vaccine#vaccination clinic#healthcare centre Sweden#Vaccination in Sweden#Get travel clinic vaccination service#Travel Clinic FactSheet
1 note
·
View note
Note
hi. is it true that you can get hpv without having sex ? my parents opted me out of getting the vaccine for it . if it is possible, how? and also how do i ask them if i can get the vaccine for it ? or can i ask the pediatrician next time i go there and ask them to ask my parents about it ?
hi anon,
I'm going to go ahead and link the Center for Disease Control's fact sheet on HPV, which I think will be helpful to have on tap here:
HPV is spread through close skin-to-skin contact, primarily vaginal, anal, or oral sex - you're not going to get it by giving someone a hug or a high five or sharing food.
an important thing to know about HPV is that it's extremely common, to the point that virtually every person who is ever sexually active can be reasonably assumed to have it at some point. and it's usually no big deal! as our friends at the CDC tell us, about 90% of cases of HPV go away after about 2 years without ever causing any health problems at all.
the HPV vaccine is to look out for the other 10% of cases. an important thing to understand about HPV is that it comes in a lot of different varieties, called "strains." most of the strains are pretty harmless, as noted above; they're viruses that just freeload in your body for a while trying to spread to other people and then go away again, easy peasy. but some strains can cause genital warts, which can be uncomfortable and cause some health complications, and cervical cancer.
important to note: cervical cancer is HIGHLY treatable if caught early and managed properly, which is why it's very important to get regular pap smears if you've had partnered sex. (the current recommendation is every 3 years until you turn 65.) pap smears screen for irregularities in the cervix that can serve as an early warning for cervical cancer, allowing you and your healthcare providers to pursue treatment as quickly as possible.
now, back to the HPV vaccine, which can lower the risk of cervical cancer even further by providing inoculation against HPV. it's a great long-term health investment against one of the most common STIs in the world, which is a great point to bring up with your parents. your pediatrician can also be a good advocate to have in this discussion if your parents are, for some reason, opposed to you receiving the vaccine, so by all means feel free to involve them!
I don't really know how else to tell you to ask your parents other than, you know, saying you want to get the HPV vaccine. that's hardly an unreasonable request; the ideal time to get an HPV vaccine is when you're young and haven't had a chance to be exposed to HPV yet.
for anyone who's not that young or has already had sex, worry not: you can still get the vaccine up to the age of 45, and a vaccine that's a little less effective is much better than no vaccine at all. I didn't get mine until I was 25! so, for anon: if your parents really decide to be hardasses about this for some reason, you're still hot to go as soon as you're 18 and can pick your own vaccines.
I hope this helps!
120 notes
·
View notes
Text
Laura Clawson at Uncharted Blue:
There will be a sustained assault on vaccinations over the next four years and people will die as a result. Donald Trump has chosen anti-vaccine crusader Robert F. Kennedy Jr. to lead the Department of Health and Human Services, and even if Trump gets sick of Kennedy and dumps him publicly, as we've seen Trump do so many times, his administration will be stocked with other anti-vaccine officials.
And as we consider the awful outcomes possible from this set of Trump choices, we have gotten one more piece of evidence to add to not just a mountain but a full mountain range of evidence that vaccines work. A new study conducted by researchers at the Medical University of South Carolina and published in JAMA finds a 62% drop in cervical cancer deaths in women under 25 since a vaccine for human papillomavirus (HPV) came into widespread use. HPV is the leading cause of cervical cancer. Though the numbers of cervical cancer deaths in women under 25 are typically low, the researchers isolated that age group as the most likely to have been vaccinated, given that the vaccine was originally only available to adolescents. This is a vaccine that could virtually eliminate a type of cancer – and maybe more than one. HPV causes six types of cancer, and the vaccine prevents 90% of cases of those cancers. But if vaccines in general are contested, the HPV vaccine comes in for especially fierce resistance, because HPV is sexually transmitted. As a result, many on the right, especially religious conservatives, oppose vaccination in the view that it might encourage sexual activity in teens or protect people from what they see as the natural and righteous consequences of having multiple sexual partners. The authors of the JAMA study note that HPV vaccine uptake has declined and is only around 60%.
The Trump Misadminstration’s 2nd go-around features picks that will surely appease anti-vaxxers, such as picking RFK Jr. to head the HHS.
#Vaccines#Anti Vaxxer Extremism#Anti Vaxxers#Trump Administration II#Trump Misadministration#Robert F. Kennedy Jr.#HPV Vaccines
20 notes
·
View notes
Text
More good news!
11 notes
·
View notes
Text
📢📢📢
6 notes
·
View notes
Text
Discover Comprehensive Vaccination Services at Happy Jabs Travel Clinic in Glasgow Planning a trip or looking to stay up-to-date with your routine vaccinations? Look no further than Happy Jabs Travel Clinic, based in the heart of Glasgow. Open seven days a week, Happy Jabs offers a convenient and stress-free way to safeguard your health with pain-free travel vaccinations, catering to both children and adults. Why Choose Happy Jabs? Happy Jabs Travel Clinic stands out for its customer-centric approach: ● Flexible Hours: Open every day of the week to fit your busy schedule. ● Same-Day Appointments: Perfect for last-minute travel or urgent requirements. ● Fully Licensed: The clinic is registered with the General Pharmaceutical Council (GpHC), ensuring the highest standards of care. ● Family-Friendly Services: Vaccinations are available for both adults and children, making it a one-stop destination for your family’s needs. Vaccinations Offered Happy Jabs provides a wide array of vaccinations tailored to your travel and health requirements: ● Travel Vaccinations: ○ Cholera ○ Dengue Fever ○ Diphtheria ○ Hepatitis A ○ Hepatitis B ○ Japanese Encephalitis ○ Malaria ○ Meningococcal Meningitis ○ Polio ○ Rabies ○ Tetanus ○ Tick-Borne Encephalitis ○ Typhoid ○ Yellow Fever ● Routine and Other Vaccinations: ○ Chickenpox (Varicella) ○ Human Papillomavirus (HPV) ○ Influenza (Flu) ○ Measles, Mumps, and Rubella (MMR) ○ Shingles ○ Whooping Cough (Pertussis) In addition to these, more vaccinations are available depending on your specific needs. Easy Online Booking Scheduling an appointment with Happy Jabs is as simple as a few clicks. Their user-friendly online booking system allows you to choose a time that suits you best. Whether you’re preparing for a trip abroad or ensuring your family stays protected, Happy Jabs Travel Clinic is your trusted partner for comprehensive vaccination services. Visit them in Glasgow today and experience healthcare with convenience and care.
Website: https://happyjabs.com
Address: First Floor, 22 Milnpark Street, Kinning Park, G41 1BB
Phone Number: 0141 459 0020
Email ID: [email protected]
Business Hours: Mon - Sun: 10:00 am - 09:00 pm
2 notes
·
View notes
Text
Just think: not long ago adults objected to teenage girls geting the HPV vaccine because STDs were for sluts. I'm sure now doctors who recommend it are being called "groomers" or somesuch. Soon we will have an HHS secretary who thinks it will make the girls autistic or something. Meanwhile, we can see from these charts how many lives have been saved by the vaccine and consequent declines in cervical cancer rates among young women. One can only rage at the numbers of cases among girls who did not receive the vaccine for religious, granola, or misogynistic reasons.
Full disclosure: I received the HPV vaccine because for some reason my hands were very susceptible to warts. Warts are caused by certain strains of the human papillomavirus. The only side effect I experienced from the shots has been my not having gotten a wart since. It is as safe and effective as vaccines come. Shame on all those who discourage it.
2 notes
·
View notes
Text
okay. fellas. i know I'm just being pedantic but we have a vaccine for HPV (human papillomavirus) which can cause cervical cancer, not just "a vaccine for cervical cancer". if scientists anywhere had managed to develop a vaccine for any kind of cancer that would be INSANELY groundbreaking, earth shattering even
6 notes
·
View notes
Note
what advice would you give to a trans person who is terrified of getting health checks such as pap smears? I'm generally rather touch-averse and that doubled with the dysphoria makes it very scary to think about.
Hi Anon,
This is a topic close to my heart, because I myself am touch-averse and have a trauma response to pelvic examinations. I also want to make sure everyone understands why it's important to get pap smears!
Let's start with what pap smears are, why they're important, and who they are for. Maybe understanding that will be the first step in finding the strength and courage to go through with them.
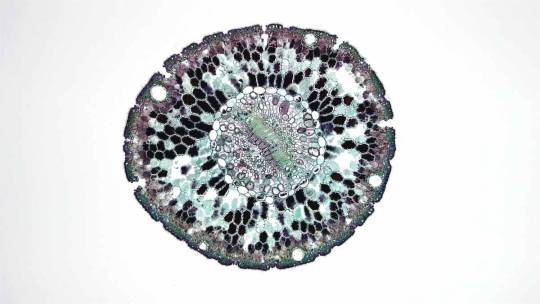
QUICK ANATOMY & PHYSIOLOGY LESSON - THE PAP SMEAR
What is a pap smear for?
Your cervix is the gateway to your uterus, sitting atop the vagina. It's a thick ring of muscle that is normally closed, opening just a tiny bit for menses to escape (the sensation of the muscle opening is what causes cramps).
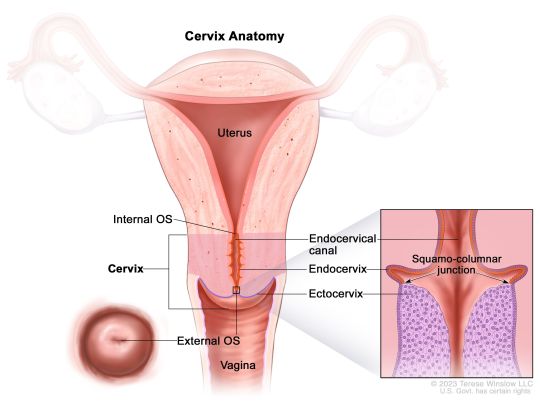
Now, the trouble comes when cervical cells have been infected with a virus called human papillomavirus (or HPV) - especially certain "high-risk" strains. HPV is very common in the human population - almost everyone sexually active has had it at some time, with about 50% of infections being a high-risk type. Most people just clear the virus themselves and never even know. But sometimes, this viral infection will start a process of dysplasia (basically growing weird cells), which can be the start of cervical cancer.
The job of a pap smear is to check the cervical cells for dysplastic changes that indicate things might progress towards cancer, or for the virus itself. (What it looks for specifically depends on your age and previous results, but the process is the same for you). When lesions are found early, they are VERY easily treatable. The pap smear saves thousands of lives every year by preventing cervical cancers.
How is a pap smear performed?
A device called a speculum will need to be inserted into your vagina to hold open the walls of the vagina and allow the provider to visualize the cervix. Once this is in place, a soft brush-like device is passed up through the vagina, pressed against the cervix, and swirled around several times to collect cells. This may feel weird or uncomfortable, but shouldn't cause pain. Most people don't feel it at all, the speculum being the worst part. The whole thing takes about one minute.
Separate from the pap smear, the provider may also perform a bimanual exam, which is when they insert fingers from one hand into the vagina while pressing down on the abdomen, to look for masses, abnormalities or tenderness.

Who needs a pap smear?
CURRENTLY (as of 2023), everyone with an intact cervix who is 21 or older is recommended to get pap smears, regardless of gender identity, sexual orientation, or sexual history. Between ages 21-29, you should go every 3 years, and after age 30, every 5 years (depending on results - if you get a positive, you would need more frequent observation).
If you are older than 21 and have never had any kind of sexual contact with anyone at all (including hands, mouths, or sharing toys!), you can discuss with your provider to see if a modified schedule may make sense based on your risk level.
Note: The HPV vaccine may change these recommendations in the future! I strongly recommend getting the vaccine if you have not already!
---
OK, Anon. With that public service announcement out of the way, let's talk about the real meat of your question.
The best thing I can recommend is to take the time to find a provider you vibe with. Someone with whom you feel safe, with whom you have mutual respect. See if your local LGTBQIA+ support group has recommendations, or if any clinics in your area have providers that specialize in LGTBQIA+ or trauma-informed care. Call and ask providers questions about how they handle people who struggle with pelvic exams. Generally, avoid crusty old men.
A good provider will warn you before ever touching any part of your body, go slowly, and ask permission each time, and stop the second you tense up. A GREAT provider will make you feel in control the whole time - they may let you insert the speculum yourself and not make you use stirrups if they're triggering for you. Medical consent is the same as sexual consent - just because you're disrobed in that room doesn't mean you need to let anyone touch you. You do not have to undergo a pap smear with a provider you don't trust. You are allowed to walk away.
Other things to try:
You can ask for a short-acting anti-anxiety medicine, like Xanax, to take before the visit, provided you've got a ride.
You can bring a companion, or ask for a nurse to hold your hand.
Chat nonstop, tell stupid jokes, or listen to music on headphones, whatever kind of distraction works best for you.
Meditate, practice belly breathing, really focus on full body relaxation, especially of the pelvic muscles
Remind yourself that it's one minute every few years for the piece of mind that you won't get cancer.
Be open to the possibility that it won't be as bad as you're fearing.
Know that you are brave and strong. You can do hard things. You can do anything for one minute.
If any other trans folx out there want to share tips with Anon for how to navigate gynecologic exams, please share!
#reproductive health#sex education#midwifery#gynecologic care#pap smear#pelvic exams#gender affirming care#lgtbqia+#transgender#trans health care
15 notes
·
View notes