#Corticosteroids
Explore tagged Tumblr posts
Text
I have been scattered all day, like starting to do something and interrupting myself to do something else or just forgetting the second part, and rn I'm sitting on the floor to FINALLY eat the food I took out of the microwave almost ten minutes ago,
But I realized
And then couldn't stop laughing
That this? Is LITERALLY
"ADHD on Steroids"
12 notes
·
View notes
Text
Chronic hip and pelvic pain is common, and can have many causes
What are chronic hip and pelvic pains?

Pain in this region can be caused by :
* Osteoarthritis of the hip (coxarthrosis): This is wear and tear of the cartilage in the hip joint. It causes pain deep in the groin, which may radiate to the thigh or knee.
* Piriformis syndrome: The piriformis muscle in the buttock can compress the sciatic nerve, causing pain in the buttock, hip and sometimes the foot.
* Tendonitis: Inflammation of the tendons around the hip, such as the psoas tendon, can cause pain.
* Bursitis: Inflammation of the bursae, which are fluid-filled sacs that lubricate the joints, can cause pain and localized tenderness.
* Poorly-healed fractures: A hip or pelvic fracture that hasn't healed properly can cause chronic pain.
* Inflammatory diseases: Diseases such as rheumatoid arthritis or ankylosing spondylitis can affect hip and pelvic joints.
* Lumbar disc problems: A herniated disc or lumbar osteoarthritis can radiate pain to the hip and pelvis.
* Scoliosis: A deviated spine can lead to muscle imbalances and pain in the lower back and hip.
What are the symptoms?
Symptoms can vary depending on the cause, but often include:
* Persistent pain: Pain may be deep, throbbing or dull.
* Stiffness: Difficulty moving the hip or pelvis.
* Lameness: An abnormal gait to avoid putting weight on the painful hip.
* Radiating pain: Pain may radiate to the thigh, knee, or even the lower back.
How can chronic hip and pelvic pain be relieved and treated?
Treatment will depend on the underlying cause, and may include :
* Rest: Avoid activities that aggravate pain.
* Ice: Apply ice to the painful area to reduce inflammation.
* Medication: Non-steroidal anti-inflammatory drugs can help relieve pain and inflammation.
* Physiotherapy: Specific exercises can strengthen muscles, improve mobility and relieve pain.
* Orthotics: A lumbar belt or hip brace can provide support.
* Injections: Corticosteroid injections can reduce inflammation in some cases.
* Surgery: In more severe cases, surgery may be required.
Go further
#chronic pain#hip pain#pelvis pain#injury#health#joint#osteoarthritis#piriformis syndrome#tendinitis#bursitis#fracture#rheumatoid arthritis#ankylosing spondylitis#herniated disc#lumbar spinal stenosis#scoliosis#stiffness#limp#radiating pain#diagnosis#treatment#rest#ice#anti-inflammatories#physical therapy#brace#corticosteroids#surgery
3 notes
·
View notes
Text
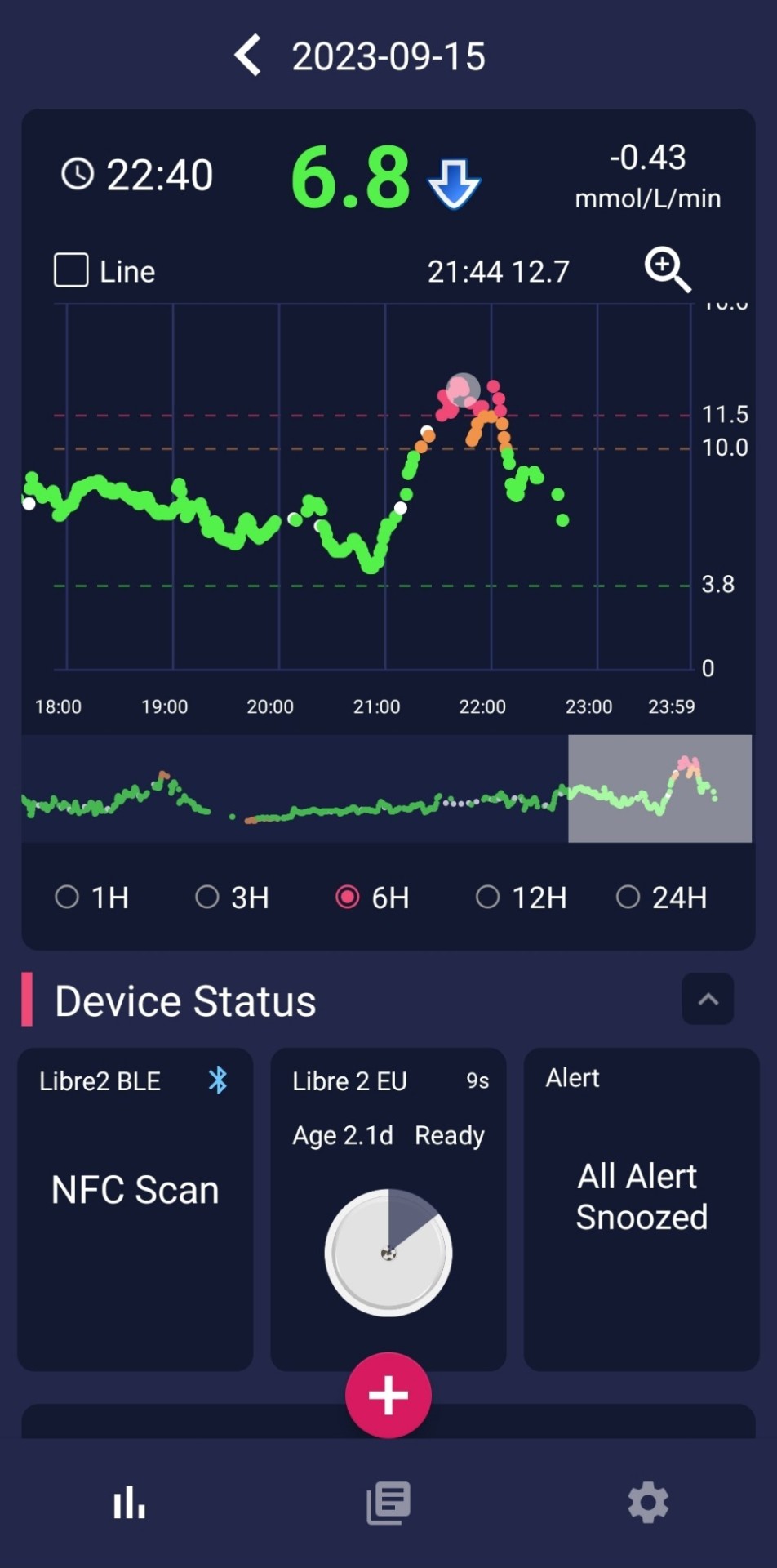
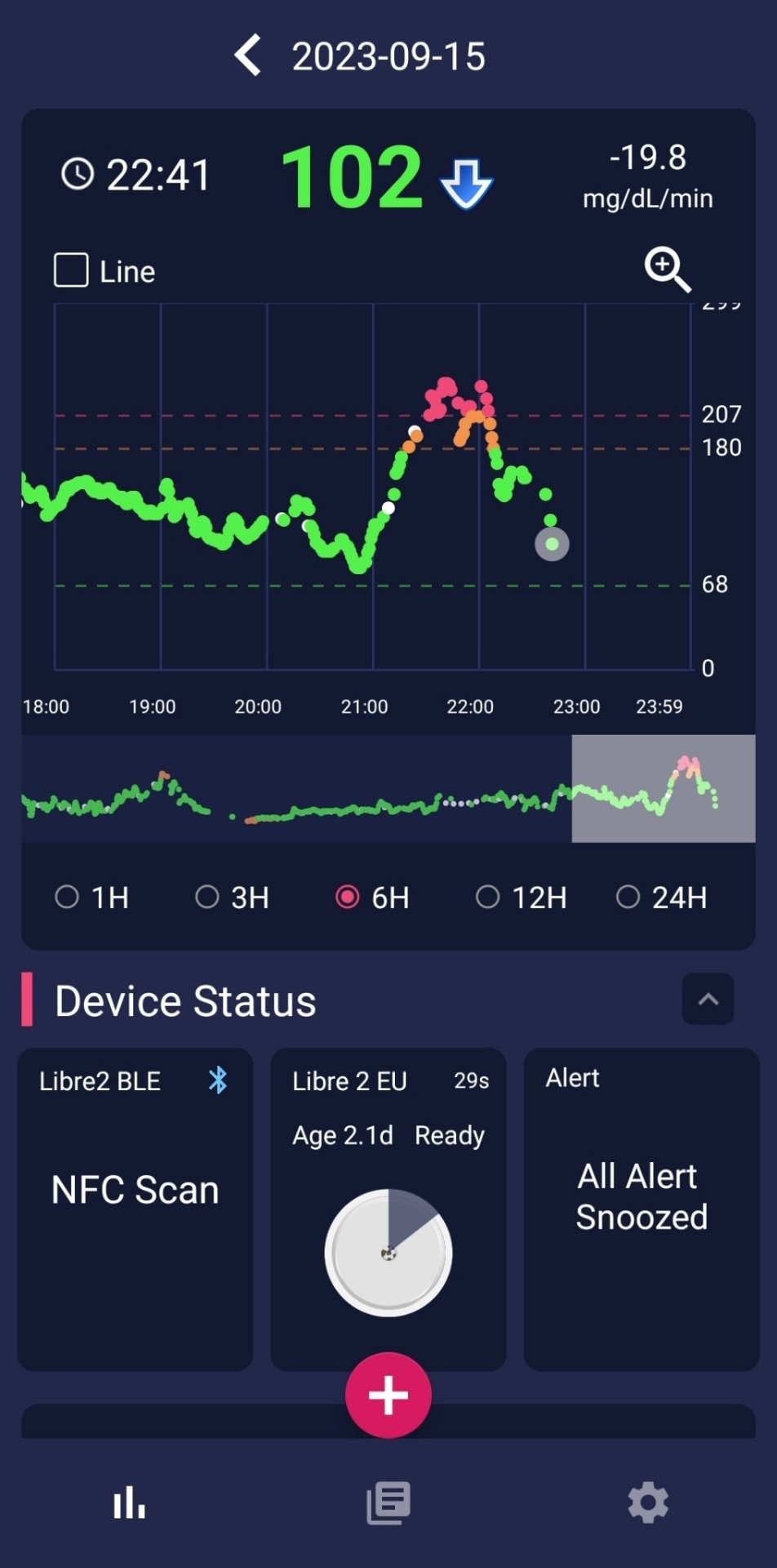

Me, every time I eat a full meal lately. Thanks to the steroids they have me on for my throat. This isn't even the worst example recently, since I have been hesitating less to really hit the insulin hard.
(This is after bumping the long-acting background insulin up quite a bit, and making sure I wait long enough for the numbers to start heading down after taking the Novorapid before I actually start eating.)
I told the gastro endoscopy people who prescribed this shit that it was really screwing with my blood sugar when I had to go in the other day. The guy just shrugged, but of course he's not living with any of this. Hopefully they will not continue this garbage indefinitely. It's getting hard to deal with.
Tonight, I preemptively dosed about double the insulin that I normally would for the same supper. Then I may have slightly overdone the extra correction dose that I reached for after it hit 11/200 with a red arrow still pointing straight up.
So yeah, I may need to grab a little something else before it crashes too hard from that. This is all trial and error. That wasn't even a particularly big bowl of food, and I won't be that sorry to grab a snack.
I really do not want or need to go lower carb, but I may need to in another way for a while just to cut back on these crazy steroid spikes. As it is, I have purposely not been eating as much as usual in general, which is probably even less helpful with ED Jerkbrain always lurking around and waiting for a chance.
Trying pretty hard to just consider the numbers as useful data points. But, this can be harder to keep in mind when you have gotten blamed and browbeaten enough over the years over them running high due to, erm, misdiagnosis and treatment that did more harm than good. I do have slightly more control over things now, but not by very much because Steroid Chaos. Which is well known to do this shit.
ETA: And yes, now endocrinology is getting all the CGM data. Which makes me more nervous with the numbers looking worse. Nobody there has wanted to act like a complete asshole so far, at least. I know I don't have to take any unwarranted shit onboard if they did decide to start up with that, but I am still not particularly happy about every single "bad" reading being open to scrutiny these days.
11 notes
·
View notes
Text
Yall i haaaaaate being on corticosteroids this shit makes me very hungry and at the same time forever sugar crashed and nauseous. I don't need more sugar, it's high! But it makes me want it and feel honger
4 notes
·
View notes
Text
prednisolone my beloved <3
#allergies#asthma#allergic rhinitis#chronic rhinitis#chronic illness#disability#chronic disability#invisible disability#prednisolone#prednisone#corticosteroids#corticoids
8 notes
·
View notes
Text

Egypt Atopic Dermatitis Therapeutics Market
The Egypt Atopic Dermatitis Therapeutics Market was valued at $34M in 2022 and is projected to grow at a 10.3% CAGR, reaching $75M by 2030. Growth is fueled by rising disease prevalence, improving healthcare infrastructure, and environmental factors. AD affects 5–10% of Egyptian children, increasing demand for treatments such as corticosteroids, calcineurin inhibitors, and immunosuppressants.
#AtopicDermatitis#EgyptHealthcare#EczemaTreatment#PharmaceuticalMarket#Dermatology#MedicalInnovation#Corticosteroids#HealthcareGrowth#SkinCare
0 notes
Text

The Science Research Diaries of S. Sunkavally, p 604.
#halogenation#corticosteroids#inflammation#blood glucose levels#rheumatoid arthritis#streptomycin#adrenal cortex#penicillamine#chlorpromazine#imidazole-N-methyl transferase#histamine#ascorbi acid#cortisol#Rubner's law#satyendra sunkavally#manuscript#cursive handwriting
0 notes
Text
Netra Eye Hospital – 6 Common Causes of Glaucoma
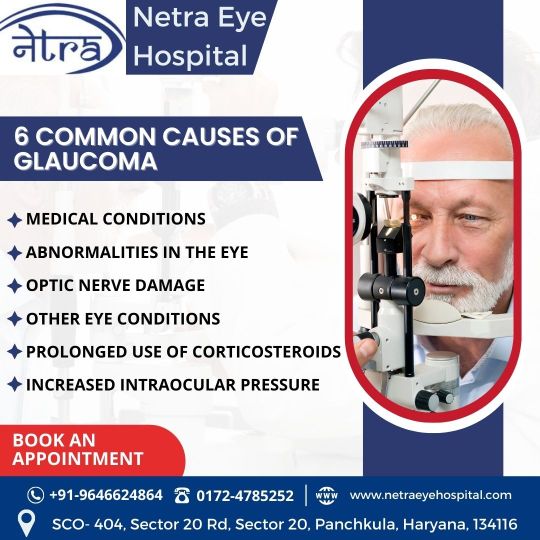
At Netra Eye Hospital, we specialize in the diagnosis and treatment of various eye conditions, including glaucoma. Glaucoma is a serious eye condition that can lead to vision loss if left untreated. Here are 6 common causes of glaucoma:
Medical Conditions: Certain systemic diseases like diabetes, high blood pressure, and heart conditions can increase the risk of glaucoma.
Abnormalities in the Eye: Irregularities in the eye's anatomy can cause glaucoma by obstructing fluid drainage within the eye.
Optic Nerve Damage: Damage to the optic nerve, often caused by high intraocular pressure, can result in glaucoma.
Other Eye Conditions: Eye conditions such as cataracts and eye infections may contribute to the development of glaucoma.
Prolonged Use of Corticosteroids: Long-term use of corticosteroids, particularly in eye drops, can increase the risk of developing glaucoma.
Increased Intraocular Pressure: Elevated pressure inside the eye is the most significant risk factor for glaucoma and can damage the optic nerve over time.
If you are experiencing any symptoms or have a family history of glaucoma, it’s essential to get regular eye check-ups. Book an appointment with us today for a comprehensive eye examination.
Contact Information:
Phone: +91-9646624864 / 0172-4785252 Website: www.netraeyehospital.com Address: SCO-404, Sector 20 Rd, Sector 20, Panchkula, Haryana, 134116 Your eye health is our priority. Visit Netra Eye Hospital for expert care and treatment.
#NetraEyeHospital#Glaucoma#EyeCare#MedicalConditions#IntraocularPressure#OpticNerveDamage#Corticosteroids#EyeHealth#Panchkula#Haryana#BookAnAppointment#VisionCare#EyeTreatment#GlaucomaAwareness
0 notes
Text
IoT and Virtual Hospital Industry: Global IoT Enabling Next Generation Virtual Hospital
The healthcare industry is embracing new digital technologies at a rapid pace to improve patient outcomes and transform the delivery of care. Internet of Things (IoT) powered solutions are connecting medical devices, integrating telehealth capabilities, and enabling new care models like virtual hospitals that remove geographic barriers. By 2023, IoT healthcare spending is projected to reach $217 billion globally as innovations reshape every aspect of the patient experience from diagnosis to long-term wellness. Connecting Medical Devices with IoT and Virtual Hospital Industry At the core of Global IoT and Virtual Hospital is their ability to remotely monitor patients anytime from anywhere. This relies on medical devices being networked and sensors wirelessly transmitting vital sign data in real-time to the cloud for analysis. IoT is enabling a wide range of devices from blood pressure cuffs and glucose monitors to EKG and pulse oximetry equipment to seamlessly integrate with electronic health records systems. Doctors can easily access streams of patient data via mobile or web applications to track recovery, identify issues early, and proactively adjust care plans as needed from a distance. For example, IoT enabled ventilators allow respiratory therapists to monitor lung function remotely for COPD and asthma patients at high risk of exacerbations. Delivering Telehealth at Scale One of the key benefits of IoT powered virtual hospitals is their ability to provide telehealth services to many more patients across broader geographies. Instead of relying on in-person clinic or hospital visits which can be time-consuming and costly for those in remote areas, IoT infrastructure facilitates real-time video consultations, remote patient monitoring, and live specialist evaluations anytime via mobile or web. This improves access to quality care for underserved communities worldwide. Leading health systems are implementing IoT ecosystems that seamlessly integrate telehealth capabilities like virtual check-ins, remote patient monitoring, and medical device data straight into their telemedicine portals and workflows. The Doximity platform, for example, connects over 560,000 physicians virtually to deliver telehealth at an unmatched scale. Transforming Care Delivery Models IoT is revolutionizing traditional care delivery models through new virtual hospital concepts that reimagine where and how healthcare is provided. Remote patient monitoring is shifting many services like post-acute care, senior care, and chronic disease management to the home. U.S. virtual health provider BestDOT utilizes an IoT platform to enable full service hospitals without physical infrastructure by leveraging connected medical equipment, EHR integrations, telehealth carts and a care coordination system available anywhere. Their virtual hospitals can stand up pop-up clinics or replace facilities damaged by natural disasters, improving both capacity and disaster response. Get more insights on Global IoT and Virtual Hospital
About Author:
Money Singh is a seasoned content writer with over four years of experience in the market research sector. Her expertise spans various industries, including food and beverages, biotechnology, chemical and materials, defense and aerospace, consumer goods, etc. (https://www.linkedin.com/in/money-singh-590844163)
#Global IoT and Virtual Hospital#Classical MWS#MWS amyloidosis#MWS without amyloidosis#Overlap MWS#Anti inflammatory drugs#Immunosuppressants#Biologics#JAK inhibitors#Corticosteroids#Analgesics
0 notes
Text
Understanding the Difference Between Antihistamines and Corticosteroids
When treating allergic reactions or inflammations, two types of medicines are most commonly known as antihistamines and corticosteroids although they function differently. Antihistamines act on histamine secretion to counter common allergy effects such as sneezing, congestion as well as itchiness. There are two kinds H1 for allergy conditions and H2 for gastrointestinal conditions. Corticosteroids, on the other hand are potent anti-inflammatory agents of the glucocorticoids and they belong to the family of steroid hormones. They are commonly used in management of conditions such as asthma, arthritis and inflammatory bowel disease. In contrast to antihistamines, corticosteroids inhibit the activity of the immune system and decrease irritation at its root.
Read more: What sets antihistamines apart from corticosteroids
0 notes
Text
Thyroid Eye Disease: Expert Treatment and Care by Dr. Surbhi Kapadia
Thyroid Eye Disease (TED) is a condition that not only affects ocular health but also significantly impacts the quality of life. In Vadodara, Dr. Surbhi Kapadia stands as a beacon of hope for those suffering from TED, offering advanced treatment options and comprehensive care.

Advanced Treatment Options for Thyroid Eye Disease
Dr. Kapadia employs a multifaceted approach to treating TED, tailored to the severity of each case. Her treatment regimen includes:
Medications: Utilizing corticosteroids and immunosuppressants to manage inflammation and other symptoms.
Innovative Surgical Techniques: For severe TED cases, Dr. Surbhi Kapadia offers surgical options such as orbital decompression, which alleviates pressure on the eye, and eyelid surgery to correct vision-related issues and improve cosmetic appearance.
Living with Thyroid Eye Disease: Insights and Tips
Living with TED involves continuous management. Dr. Kapadia advises:
Regular Monitoring: Keeping track of symptom progression and adjusting treatment plans accordingly.
Lifestyle Modifications: Implementing lifestyle changes like quitting smoking, which is known to exacerbate TED.
Eye Protection: Using sunglasses to protect the eyes from UV rays and environmental irritants.
Frequently Asked Questions About Thyroid Eye Disease Answered
Dr. Kapadia addresses common queries regarding TED, offering clear and concise information:
Diagnosis: Explaining the methods used to diagnose TED, including clinical assessments and imaging techniques.
Treatment Effectiveness: Discussing the success rates of different treatment options and what patients can expect.
Post-Treatment Care: Highlighting the importance of follow-up care post-treatment to ensure the best outcomes.
Conclusion:
Dr. Surbhi Kapadia's expertise in treating Thyroid Eye Disease makes her one of the best ophthalmologists in Vadodara for patients seeking specialized eye care. Her dedication to her patient's well-being ensures that they receive not only the best medical treatment but also the support and guidance needed to navigate through the complexities of TED.
#Thyroid Eye Disease (TED)#Dr. Surbhi Kapadia#Ocular health#Advanced treatment options#Corticosteroids#Immunosuppressants#Orbital decompression#Eyelid surgery#Vision-related issues#Lifestyle modifications#Eye protection#UV protection
0 notes
Text
What is chronic knee pain?
Chronic knee pain can be caused by a multitude of factors, ranging from natural cartilage wear to more specific injuries. Here are some of the most common causes:
* Osteoarthritis of the knee: This is the progressive wearing away of the cartilage covering the ends of the knee bones. It is one of the most common causes of chronic knee pain, especially in the elderly.
* Tendonitis: Inflammation of the tendons around the knee, such as the patella or patellar tendon, can cause pain.
* Meniscus damage: The meniscus is the shock-absorbing cartilage in the knee. A tear or lesion can lead to pain and stiffness.
* Patellofemoral syndrome: Often called “jumper's knee”, this syndrome is due to misalignment of the patella. It causes pain in the front of the knee.
* Other causes: Poorly-healed fractures, inflammatory diseases (such as rheumatoid arthritis), infections and circulation problems can also cause chronic knee pain.

What are the symptoms?
Symptoms can vary depending on the cause of the pain, but often include:
* Persistent pain: Pain may be constant or appear during specific activities.
* Swelling: The knee may feel swollen and warm to the touch.
* Stiffness: Difficulty bending or fully extending the knee.
* Instability: A “loose knee” sensation.
How can chronic knee pain be relieved and treated?
Treatment will depend on the underlying cause. It may include :
* Rest: Avoid activities that aggravate pain.
* Ice: Apply ice to the knee to reduce inflammation.
* Medication: Non-steroidal anti-inflammatory drugs can help relieve pain and inflammation.
* Physiotherapy: Specific exercises can strengthen the muscles around the knee and improve mobility.
* Orthotics: A knee brace can help stabilize the joint.
* Injections: Corticosteroid injections can reduce inflammation in some cases.
* Surgery: In more severe cases, surgery may be required.
Go further
#chronic pain#knee pain#injury#health#joint#osteoarthritis#tendinitis#meniscus#patellofemoral pain syndrome#fracture#rheumatoid arthritis#inflammation#swelling#stiffness#instability#diagnosis#treatment#rest#ice#anti-inflammatories#physical therapy#brace#corticosteroids#surgery
0 notes
Text
Juvenile Rheumatoid Arthritis
Juvenile rheumatoid arthritis (JRA), also known as juvenile idiopathic arthritis (JIA), is a form of arthritis that affects children. JRA causes inflammation and pain in one or more joints. The cause of JRA is unknown, but it may be the result of an immune system response gone wrong. It is not contagious.
#Juvenile rheumatoid arthritis#anti-inflammatory#joint pain#swelling#stiffness#warmness#corticosteroids#physical therapy#and surgery
1 note
·
View note
Text
Unraveling the Mystery: Diagnosis and Treatment of aTTP - Conquering a Rare Blood Disorder
In the vast world of medical conditions, some rare and lesser-known disorders can significantly impact the lives of those affected. One such condition is acquired Thrombotic Thrombocytopenic Purpura, commonly known as aTTP. This rare blood disorder is characterized by the formation of blood clots in small blood vessels throughout the body, leading to a low platelet count and potential organ damage. Despite its rarity, aTTP demands urgent attention and specialized care. This blog explores the diagnosis and treatment approaches for this challenging and potentially life-threatening condition.
Write to us at [email protected] Learn how GRG Health is helping clients gather more in-depth market-level information on such topics.
Understanding aTTP
Thrombotic Thrombocytopenic Purpura (TTP) is a group of disorders, with aTTP being an acquired form of the disease. It primarily affects the microvasculature, leading to clot formation within small blood vessels, especially in the brain, heart, kidneys, and other vital organs. The formation of these clots can obstruct blood flow and cause damage to the affected tissues.
The exact cause of aTTP is not always clear. Still, it often involves an autoimmune response, where the body's immune system mistakenly targets and damages its own blood vessels and platelets. Certain triggers, such as infections, medications, or pregnancy, can potentially set off the disease in predisposed individuals.
Diagnosis of aTTP
Diagnosing aTTP can be challenging due to its rarity and similarity in symptoms with other conditions. A prompt and accurate diagnosis is crucial to initiate appropriate treatment promptly.
Healthcare providers may consider the following steps in diagnosing aTTP:
Clinical Assessment: The initial step involves a comprehensive review of the patient's medical history, including any recent infections or potential triggers, and a thorough physical examination.
Blood Tests: Blood tests are critical in diagnosing aTTP. The analysis may include a complete blood count to check for a low platelet count and a peripheral blood smear to look for abnormal red blood cells and platelet clumps.
ADAMTS13 Activity Test: This specialized test measures the activity of ADAMTS13, a specific enzyme responsible for breaking down large von Willebrand factor multimers in the blood. Reduced activity of ADAMTS13 is a hallmark feature of aTTP.
Other Tests: Additional tests, such as kidney and liver function tests, coagulation profiles, and assessment of organ damage, may be performed to evaluate the severity of the disease and its impact on vital organs.
Treatment of aTTP:
Treating aTTP requires a multidisciplinary approach involving hematologists, nephrologists, and other specialists. The main goals of treatment include stopping the formation of blood clots, increasing platelet count, and preserving organ function.
Depending on the severity of the disease, the following treatments may be employed:
Plasma Exchange (PE): PE is considered the first-line treatment for aTTP. During this procedure, the patient's plasma containing faulty antibodies and other pro-clotting factors is removed and replaced with fresh frozen plasma or other plasma products. This helps to remove the pathogenic components and restore the balance of clotting factors.
Corticosteroids: Corticosteroids, such as prednisone, are often used in combination with PE to suppress the immune response and reduce the production of autoantibodies that attack ADAMTS13.
Rituximab: In cases where PE and corticosteroids are insufficient, the monoclonal antibody rituximab may be used to target and deplete specific immune cells involved in the autoimmune response.
Immunosuppressants: Drugs such as cyclosporine or azathioprine can dampen the immune system and prevent further attacks on ADAMTS13.
Splenectomy: In some refractory cases, surgical removal of the spleen (splenectomy) may be considered to reduce the destruction of platelets and enhance treatment efficacy.
Supportive Care: Patients with aTTP often require supportive care, including close monitoring, pain management, and treatment for any associated organ damage.
Conclusion:
aTTP is a rare but serious blood disorder that demands timely diagnosis and appropriate treatment. The collaboration between medical professionals, advanced diagnostic tools, and novel therapies plays a vital role in improving outcomes for those affected by this condition. While aTTP presents significant challenges, ongoing research, and medical advancements offer hope for better management and potentially a cure in the future. Early recognition, proper intervention, and continuous support are essential in the journey towards bettering the lives of individuals battling this rare blood disorder.
Visit our website now: https://www.grgonline.com/
0 notes
Text

TSRNOSS, p 487.
#isoniazid#aquiline nose#malnutrition#tuberculosis#hookworm#phrenic nerve#corticosteroids#metronidazole
0 notes
Text

Teddy is debuting his summer body
74 notes
·
View notes