#Central nervous system
Explore tagged Tumblr posts
Text
"The 200+ Symptoms of Fibromyalgia"
(Note: Some symptoms may overlap)
GENERAL
1. Activity level decreased to less than 50% of pre-illness activity level
2. Cold hands and feet (extremities)
3. Cough
4. Craving carbohydrates
5. Delayed reaction to physical activity or stressful events
6. Dryness of eyes and/or mouth
7. Edema (Oedema)
8. Family member(s) with Fibromyalgia
9. Fatigue, made worse by physical exertion or stress
10. Feeling cold often
11. Feeling hot often
12. Frequent sighing
13. Heart palpitations
14. Hoarseness
15. Hypoglycemia (blood sugar falls or low)
16. Increased thirst
17. Low blood pressure (below 110/70)
18. Low body temperature (below 97.6)
19. Low-grade fevers
20. Night sweats
21. Noisy joints – with or without pain
22. Poor circulation in hands/feet
23. Profuse sweating
24. Recurrent flu-like illness
25. Shortness of breath with little or no exertion
26. Severe nasal allergies (new or worsening allergies)
27. Sore throat
28. Subjective swelling of extremities – (feels swollen Bu can’t find anything)
29. Sweats
30. Symptoms worsened by air travel
31. Symptoms worsened by stress
32. Symptoms worsened by temperature changes
33. Tender or swollen lymph nodes, especially in neck and underarms
34. Tremor or trembling
35. Unexplained weight gain or loss
PAIN
36. Abdominal wall pain
37. Bad hip pain
38. Burning Nerve Pain
39. Chest pain
40. Collarbone pain
41. Diffuse swelling
42. Elbow pain
43. Exacerbated Plantar arch or heel pain
44. “Growing” pains that don’t go away once you are done growing
45. Headache – tension or migraine
46. Inflamed Rib Cartilage
47. Joint pain
48. Lumpy, tender breasts
49. Morning stiffness
50. Muscle pain - widespread
51. Muscle spasms
52. Muscle twitching
53. Muscle weakness
54. Pain that ranges from moderate to severe
55. Pain that moves around the body
56. Paralysis or severe weakness of an arm or leg
57. Restless Leg Syndrome
58. Rib Pain
59. Scalp Pain (like hair being pulled out)
60. Sciatica-like pain
61. Tender points or trigger points
62. TMJ syndrome
63. “Voodoo Doll” Poking Sensation in random places
NEUROLOGICAL
64. Blackouts
65. Brain fog
66. Carpal Tunnel
67. Feeling spaced out
68. Hallucinating smells
69. Inability to think clearly
70. Lightheadedness
71. Noise intolerance
72. Numbness or tingling sensations
73. Photophobia (sensitivity to light)
74. Seizures
75. Seizure-like episodes
76. Sensation that you might faint
77. Syncope (fainting)
78. Tinnitus (ringing in one or both ears)
79. Vertigo or dizziness
EQUILIBRIUM/PERCEPTION
80. Bumping into things
81. Clumsy Walking
82. Difficulty balancing
83. Difficulty judging distances (when driving, etc.)
84. Directional disorientation
85. Dropping things frequently
86. Feeling spatially disoriented
87. Frequent tripping or stumbling
88. Not seeing what you’re looking at
89. Poor balance and coordination
90. Staggering gait
SLEEP
91. Alertness/energy best late at night
92. Altered sleep/wake schedule
93. Awakening frequently
94. Difficulty falling asleep
95. Difficulty staying asleep
96. Excessive sleeping
97. Extreme alertness or energy levels late at night
98. Falling asleep at random and sometimes dangerous moments
99. Fatigue
100. Light or broken sleep pattern
101. Muscle spasms/twitches at night
102. Narcolepsy
103. Sleep disturbances
104. Sleep starts or falling sensations
105. Teeth grinding - "Bruxism"
106. Tossing and turning
107. Un-refreshing or non-restorative sleep
108. Vivid or disturbing dreams/nightmares
EYES/VISION
109. Blind spots in vision
110. Eye pain
111. Difficulty switching focus from one thing to another
112. Frequent changes in ability to see well
113. Night driving difficulty
114. Occasional Blurry vision
115. Poor night vision
116. Rapidly worsening vision
117. Vision changes
COGNITIVE
118. Becoming lost in familiar locations when driving
119. Confusion
120. Difficulty expressing ideas in words
121. Difficulty following conversation (especially if background noise present)
122. Difficulty following directions while driving
123. Difficulty following oral instructions
124. Difficulty following written instructions
125. Difficulty making decisions
126. Difficulty moving your mouth to speak
127. Difficulty paying attention
128. Difficulty putting ideas together to form a complete picture
129. Difficulty putting tasks or things in proper sequence
130. Difficulty recognizing faces
131. Difficulty speaking known words
132. Difficulty remembering names of objects
133. Difficulty remembering names of people
134. Difficulty understanding what you read
135. Difficulty with long-term memory
136. Difficulty with simple calculations
137. Difficulty with short-term memory
138. Easily distracted during a task
139. Dyslexia-type symptoms occasionally
140. Feeling too disoriented to drive
141. Forgetting how to do routine things
142. Impaired ability to concentrate
143. Inability to recognize familiar surroundings
144. Losing track in the middle of a task (remembering what to do next)
145. Losing your train of thought in the middle of a sentence
146. Loss of ability to distinguish some colors
147. Poor judgment
148. Short term memory impairment
149. Slowed speech
150. Staring into space trying to think
151. Stuttering; stammering
152. Switching left and right
153. Transposition (reversal) of numbers, words and/or letters when you speak
154. Transposition (reversal) of numbers, words and/or letters when you write
155. Trouble concentrating
156. Using the wrong word
157. Word-finding difficulty
EMOTIONAL
158. Abrupt and/or unpredictable mood swings
159. Anger outbursts
160. Anxiety or fear when there is no obvious cause
161. Attacks of uncontrollable rage
162. Decreased appetite
163. Depressed mood
164. Feeling helpless and/or hopeless
165. Fear of someone knocking on the door
166. Fear of telephone ringing
167. Feeling worthless
168. Frequent crying
169. Heightened awareness – of symptoms
170. Inability to enjoy previously enjoyed activities
171. Irrational fears
172. Irritability
173. Overreaction
174. Panic attacks
175. Personality changes –usually a worsening of pervious condition
176. Phobias
177. Suicide attempts
178. Suicidal thoughts
179. Tendency to cry easily
GASTROINTESTINAL
180. Abdominal cramps
181. Bloating
182. Decreased appetite
183. Food cravings
184. Frequent constipation
185. Frequent diarrhea
186. Gerd-like Symptoms
187. Heartburn
188. Increased appetite
189. Intestinal gas
190. Irritable bladder - "Angry Bladder Syndrome"
191. Irritable bowel syndrome - IBS-C, IBS-D
192. Nausea
193. Regurgitation
194. Stomachache
195. Vomiting
196. Weight gain - unexplained
197. Weight loss - unexplained
UROGENITAL
198. Decreased libido (sex drive)
199. Endometriosis
200. Frequent urination
201. Impotence
202. Menstrual problems
203. Painful urination or bladder pain - "Interstitial Cystitis"
204. Pelvic pain
205. Prostate pain
206. Worsening of (or severe) premenstrual syndrome (PMS or PMDD)
SENSITIVITIES
207. Alcohol intolerance
208. Allodynia (hypersensitive to touch)
209. Alteration of taste, smell, and/or hearing
210. Sensitivity to chemicals in cleaning products, perfumes, etc.
211. Sensitivities to foods
212. Sensitivity to light
213. Sensitivity to mold
214. Sensitivity to noise
215. Sensitivity to odors
216. Sensitivity to yeast (getting yeast infections frequently on skin, etc.)
217. Sensory overload
218. Sensitivity to pressure & humidity changes
219. Sensitivity to extreme temperature changes
220. Vulvodynia
SKIN
221. Able to “write” on skin with finger
222. Bruising easily
223. Bumps and lumps
224. Eczema or psoriasis
225. Hot/dry skin
226. Ingrown hairs
227. Itchy/Irritable skin
228. Mottled skin
229. Rashes or sores
230. Scarring easily
231. Sensitivity to the sun
232. Skin suddenly turns bright red
CARDIOVASCULAR (Heart)
233. “Click-murmur” sounds through stethoscope
234. Fluttery heartbeat
235. Heart palpitations
236. Irregular heartbeat
237. Loud pulse in ear
238. Pain that mimics heart attack - "Costochondritis"
239. Rapid heartbeat
HAIR/NAILS
240. Dull, listless hair
241. Heavy and splitting cuticles
242. Irritated nail beds
243. Nails that curve under
244. Pronounced nail ridges
245. Temporary hair loss
OTHER
246. Canker sores
247. Dental problems
248. Disk Degeneration
249. Hemorrhoids
250. Nose bleeds
251. Periodontal (gum) disease
252. Need for early hysterectomy
#fibromyalgia#chronic pain#chronic illness#chronically ill#invisible illness#spoonie#pwd#disability#hidden disability#sharing is caring#disorder#neurological disorder#central nervous system#nervous system disorder#mental health#health#awareness
199 notes
·
View notes
Text
Welcome to the Premium Autoimmune Package
Hi. I’m not new to being sick, but I’m very new to being taken seriously. That only happened because my body is currently collapsing fast enough that doctors couldn’t look away anymore.
I live with overlapping autoimmune diseases, but recently I got upgraded to the “CNS involvement” tier. Think brain inflammation, spinal pressure, hallucinations, cognitive fog, and one healing spinal fracture I didn’t even realize I had. I thought it was just my usual back pain. Turns out it was… a broken bone.
I’ve been hospitalized twice in the last month. A spinal tap showed my brain pressure was way too high, 32 cmH₂O, where normal is typically between 10 and 20. My spinal fluid was full of immune cells , 40% of them, when 0–5% is normal. My MRI has white matter lesions. It’s not MS. It likely neuropsychiatric lupus. It might be a weird intersection of multiple things. No one’s totally sure yet.
What I do know is I’m on IVIG now, possibly headed for a brain shunt, and trying to stay out of the hospital. Also, I’m trans and had to pause testosterone because of clot risks from treatment. No, there’s no workaround. Yes, it sucks.
This blog is my space to document what it’s like to be visibly declining after years of being invisibly sick. No pity required. Just here to tell the truth about what it’s like to have the Premium Autoimmune Package, full access unlocked.
Current Working diagnoses:
• Neuropsychiatric Lupus (NPSLE)
• Myasthenia Gravis
• Psoriatic Arthritis
• Intracranial Hypertension
• Ehlers-Danlos Syndrome
#chronic illness#autoimmune#autoimmine disease#neuropsychiatric lupus#NPSLE#IVIG#Disability#chronic pain#myasthenia gravis#invisible illness#invisible disability#disabled and queer#disabled and trans#spoonie#brain fog#medical trauma#hospital life#rare disease#rare disability#rare disorder#chronically ill#central nervous system
13 notes
·
View notes
Text
Q: Are the eyes and optic nerve (aka CN II) part of the central nervous system or peripheral nervous system?
A: CNS
I know we say that the PNS has 12 cranial nerves, but that is false. It has 11 (CNI,CNIII-CNXII). How do we know this? Embryology, my dude (and pathology)
So the eyes come out of the brain around 3 wks after fertilization. They are a diverticulum of the brain (as everything in your body is a diverticulum of something else). The retina and optic nerve come out of the neural ectoderm. The lens comes from the surface ectoderm. If you know embryology, everything in medicine and anatomy will become so much clearer, trust me.
*we are like balloon dogs, just one long tube that got twisted around a bunch*
Anyways, pathologically, we can tell that the eyes are part of the CNS as well. What does Multiple Sclerosis do? It demyelinates the CNS....and the optic nerve. What does Guillian-Barre do? It demyelinates the PNS...but not the optic nerve.
So why do we call the optic nerves...nerves when they should be a tract? (remember that axons of the CNS are called tracts, and in the PNS they are called nerves) Honestly, I have no idea. It was probably some dumbass anatomist...and he probably also thought humans have one heart...
#med student#medical school#medicine#med school#med studyblr#biology#mcat#optics#eyes#embryology#central nervous system#nervous system#peripheral nervous system#questions#ocular posting
12 notes
·
View notes
Text
PNS and CNS
PNS=Peripheral Nervous System
CNS=Central Nervous System
Creidts to Amoeba Sisters
10 notes
·
View notes
Text
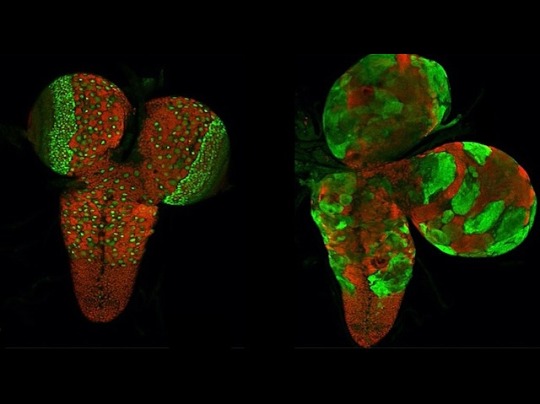
Nervous System Shapers
Identifying the genes that regulate the shaping and maintenance of the fruit fly central nervous system – insight for possible roles for homologous genes in mammals
Read the published research article here
Image from work by Haluk Lacin and Yuqing Zhu, and colleagues
Division of Biological and Biomedical Systems, University of Missouri-Kansas City, Kansas City and Department of Genetics, Washington University School of Medicine, St. Louis, MO, USA
Image originally published with a Creative Commons Attribution 4.0 International (CC BY-NC 4.0)
Published in bioRxiv, February 2024 (not peer reviewed)
You can also follow BPoD on Instagram, Twitter and Facebook
18 notes
·
View notes
Text
Spasticity
Let's start by clearly defining spasticity:
Spasticity is a neuromuscular disorder characterized by increased muscle tone, stiff, involuntary movements and exaggerated reflexes. It is often associated with lesions of the central nervous system, such as those caused by stroke, multiple sclerosis or spinal cord injury.
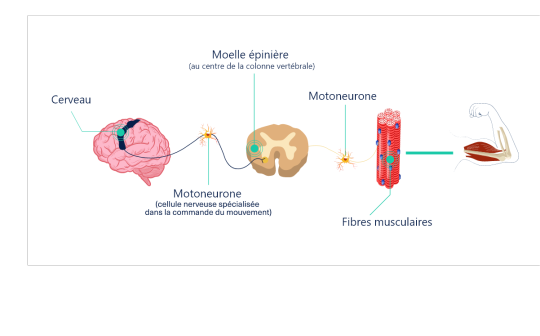
Causes of spasticity:
* Cerebral lesions: stroke, head trauma, brain tumors.
* Spinal cord injuries: road accidents, sports injuries, degenerative diseases.
* Neurodegenerative diseases: multiple sclerosis, amyotrophic lateral sclerosis (ALS).
* Other: encephalitis, meningitis, certain infections.
Symptoms of spasticity:
* Increased muscle tone: muscles stiff and difficult to move.
* Involuntary movements: spasms, muscle contractions.
* Exaggerated reflexes: excessive muscular reactions to a stimulus.
* Walking difficulties: stiff gait, leg spasms.
* Pain: muscle contractures, joint pain.
Diagnosis of spasticity :
* Clinical examination: assessment of reflexes, muscle tone, muscle strength.
* Medical imaging: MRI, CT scan to identify underlying cause.
* Electromyography: measurement of muscle electrical activity.
Treatments for spasticity :
* Medication: muscle relaxants, baclofen.
* Physical therapy: stretching, muscle-strengthening exercises.
* Orthoses: splints to support joints and improve function.
* Botox: injections of botulinum toxin to reduce muscle spasms.
* Surgery: in the most severe cases, to correct deformities or contractures.
Living with spasticity:
* Adapting to everyday life: technical aids, home improvements.
* Psychological support: to cope with difficulties and improve quality of life.
* Patient associations: to exchange ideas and find support.
Advice for caregivers:
* Training: to understand spasticity and its consequences.
* Get informed: about treatments and available aids.
* Take care of yourself: to avoid exhaustion.
Go further
#spasticity#neuromuscular disorder#central nervous system#muscle tone#reflexes#involuntary movements#AVC : stroke#sclérose en plaques : multiple sclerosis (MS)#spinal cord injury#traumatic brain injury (TBI)#brain tumor#neurodegenerative diseases#encephalitis#meningitis#spasticity diagnosis#spasticity treatment#spasticity medications#physical therapy for spasticity#braces for spasticity#botox for spasticity#spasticity surgery#living with spasticity#caregivers for people with spasticity
2 notes
·
View notes
Text
Primary dural-based parafalcine diffuse large b-cell lymphoma mimicking meningioma by Amr El Mohamad in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
Background: Primary dural-based diffuse large B-cell lymphoma is very rare. Only few cases were reported in the literature. Case presentation: Herein, we present a case of an immunocompetent patient with primary dural-based diffuse large B-cell lymphomas mimicking meningioma associated with ghost tumor phenomenon without any evidence of a systemic lymphoma. Conclusion: Primary central nervous system lymphomas are rare. Clinicians should always consider this lesion as a differential diagnosis if radiological findings are not indicative of typical one meningiomas.
Key words: Dural-based tumor, diffuse large B-cell lymphoma, ghost tumor, MATRIX regimen, central nervous system.
Introduction
Primary central nervous system lymphomas (CNSLs) (PCNSLs) are rare and account for 2%–5% of all brain tumor cases, whereas secondary CNSLs are more common [1,2]. One study has shown that the most common intraparenchymal histological type is diffuse large B-cell lymphoma, as among 26 patients with PCNSL, 25 had diffuse large B-cell lymphoma [3]. Although primary dural-based lymphomas are rare, the most common area of involvement is the cerebral hemispheres. Most dural-based lymphomas are secondary and present as extra-nodal systemic diffuse large B-cell lymphomas. Primary dural-based lymphomas are usually histologically marginal-zone lymphomas, representing a group of lymphomas that have been historically classified together because they appear to arise from post-germinal center and marginal-zone B cells and share a similar immunophenotype, and few cases were reported to be diffuse large B lymphomas [4]. Here, we present a case of an immunocompetent patient with primary dural-based diffuse large B-cell lymphomas mimicking meningioma associated with ghost tumor phenomenon without any evidence of systemic disease.
Case Presentation
A 58-year-old male individual previously healthy and immunocompetent presented with headache, recurrent vomiting, and memory problems lasting for 3 days. No loss of consciousness, seizure, subjective weakness, or fever was observed. On physical examination, the patient’s Glasgow coma scale score was 15; his pupils were 3 mm in diameter, equal, and reactive; and the patient had nominal aphasia without motor and sensory deficit. He had normal cerebellar functions, and cranial nerve exams revealed no deficit. Head computed tomography (CT) (Fig. 1) showed a 2.2 × 3.8 cm (transverse × anteroposterior) iso-dense lesion with internal hypodensity in the left parasagittal frontal region extending to the right frontal region. Extensive perilesional edema was observed with effacement of the sulci and mass effect on bilateral frontal horns, associated with 3-mm midline shift. Head magnetic resonance imaging (MRI) showed an isointense parasagittal lesion on T1 and heterogeneous intense on T2, with redemonstration of perifocal edema (Fig. 2). Head T1-weighted imaging with contrast enhancement (Fig. 3) showed a large, left frontal, parafalcine, irregular-shaped mass located below the superior sagittal sinus level. It measured 4 × 3 × 3.3 cm in anteroposterior, mediolateral, and craniocaudal, respectively. It showed diffusion restriction (Fig. 4). There was central hyperintensity on T2-weighted imaging, without post-contrast enhancement area representing cyst formation. It exerts a mass effect characterized by effacement of the adjacent sulci, compression of the left lateral ventricle, and a 3-mm shift of the midline structures to the right side, and the impression of our neuroradiologist was atypical meningioma. Regarding extensive edema, dexamethasone was started at a dose of 4 mg, thrice a day, and the patient was planned for craniotomy and resection of the tumor. Initially, the patient was reluctant to undergo surgery; however, subsequently, the patient agreed to undergo surgery after approximately 10 days. During surgery, parasagittal craniotomy was performed; however, to our surprise, no definite mass lesion was found at the proposed site, in contrast to the findings described on imaging. The falx was thinned out and partly deficient. A biopsy sample was obtained from this abnormally appearing falx. Moreover, we obtained biopsy samples under neuronavigation guidance from abnormally appearing tissue, which was completely intra-axial, deep down in the lesion visualized on navigation. On postoperative day 1, MRI head with contrast enhancement (Fig. 5) showed that the previously seen lesion had a significant regression in size. Its right frontal extension and adjacent enhanced meningeal tail showed size reduction. Moreover, some regression in the perilesional vasogenic edema was observed. A significant regression in the previously described enhancement was noted at the left-side lentiform nucleus and external capsule. The MR spectroscopy study showed an increased choline/N-acetyl aspartate ratio and elevated lactate level within the lesion.
The histopathology results of the first brain biopsy samples (Figs.6–7) obtained from the falx cerebri showed meningothelial hyperplasia with calcification and focal perivascular lymphocytic infiltrate composed of small and large, atypical lymphocytes. Immunohistochemical staining was performed; however, the area of interest disappeared. The pathology team recommended another fresh biopsy to have the final diagnosis and flowmetry studies. So, the patient underwent redo craniotomy using the same incision, and multiple biopsy samples were taken. The second fresh brain biopsy (Figs. 8–9) showed multiple brain fragments with predominant perivascular atypical lymphoid infiltrates. Most cells were medium to large with moderate cytoplasm, atypical irregular nuclei having vesicular chromatin, variably prominent nucleoli, and several mitoses, including atypical one. Necrotic areas were also seen. Immunohistochemistry of the second biopsy (Fig.10 A-D) showed that atypical perivascular cells were positive for CD45, CD20, CD79a, BCl2, BCl6, MUM1, OCT2, and C-MYC, and negative for CD10, CD21, TDT, ALK1, EBV-LMP1, CD3, and CD5; however, few reactive/residual lymphocytes were positive for these enzymes. Moreover, 80% of lymphoid cellular nuclei were positive for Ki67. These findings were consistent with diffuse large B-cell lymphoma, not otherwise specified.
Whole-body positron emission tomography (PET) showed intense fluorodeoxyglucose (FDG) uptake higher than that in the healthy brain cortex, without evidence of coexisting systemic disease. In addition to PET scan, contrast-enhanced chest, abdomen, pelvis CT did not show any other lesions in the body; furthermore, workup for viral markers and autoimmune conditions were all unremarkable, thus confirming the diagnosis of “primary dural-based diffuse large B-cell lymphoma,” distinguishing it from secondary CNSL. The patient was transferred to the Oncology Department and started on three cycles of the methotrexate, cytarabine, thiotepa, and rituximab (MATRIX) protocol, which is the current standard treatment regimen for PCNSLs [5]. Three months after the diagnosis and after receiving two cycles of the MATRIX protocol, brain MRI with contrast enhancement (Fig. 11A, B) showed regression of the lesion, and PET scan showed complete metabolic resolution in terms of decreased FDG activity of the previously seen PCNSL without signs of lymphoma activity elsewhere. Subsequently, the patient received the third cycle of the MATRIX protocol without specific complications. Two weeks later, autologous stem cell transplantation (50 × 106/kg) was performed as part of the consolidation phase of treatment. Six weeks later, conditioning chemotherapy with carmustine–thiotepa was administered, followed by stem cell infusion (CD34 = 12 million/kg). The post-transplant course was complicated with mucositis, folliculitis, diarrhea, febrile neutropenia, and prolonged thrombocytopenia. Two months after transplantation, PET scan was repeated and showed complete metabolic resolution of initially seen PCNSL involvement. Currently, the patient is being followed by the hematology team; the patient is in good health and remission. The last outpatient follow-up was 8 months after the first surgery. The patient was seen by the vascular surgery (for permcath removal) and oncology teams. At this time, the patient was stable with complete remission; then, the patient was lost to follow-up. Another head MRI was performed and showed almost total regression of the lesion.
Discussion
Lymphomas in CNS are classified as primary, arising de novo from brain parenchyma, leptomeninges, eye, and spinal cord and as secondary to systemic lymphoma, which can be dural-based lesions. Secondary CNSLs are more common than PCNSLs. Most PCNSLs are intraparenchymal diffuse large B-cell lymphomas with a predilection to occur in the frontal lobe and then deep nucleic and periventricular locations; the infratentorial cerebellum is the most common location. However, primary dural-based lymphomas are rare, and even when found, they are histologically marginal-zone lymphomas. Few cases of primary dural-based diffuse large B-cell lymphoma have been reported in the literature [4,6]. Furthermore, PCNSLs are more common in immunocompromised patients with a mean age of 34 years, and they occur in immunocompetent individuals at an older age with a mean of 52 years [7]. The patient in this case report was 58 years old and immunocompetent without significant previous medical conditions. The latest review of the literature on primary dural-based lymphoma has been conducted by Quinn et al., who have found only 24 reported cases of primary dural-based diffuse large B-cell lymphoma, which confirms the rarity of the disease and subsequently the limited knowledge regarding this disease entity [8]. CNSLs have rapid response to steroids with shrinkage in size and initial remission [9]. Moreover, the initial response to steroids is associated with a better response to chemoradiotherapy and good prognosis [9]. In the patient in this case report, there was an unintentional delay of surgery for approximately 10 days, and the patient was on steroids (dexamethasone). In this case report, the failure to identify a discrete lesion of the size expected as perceived on initial imaging, despite proper surgical planning using neuronavigation, was probably due to the rapid regression of the tumor in response to steroids. This phenomenon agrees with the scientific literature reporting about the disappearance of lymphomas in response to steroids (ghost tumors) [10,11]. The pathogenesis of primary dural-based lymphoma remains unknown as there is no lymphoid tissue in the dura. It is hypothesized that it is related to chronic infection, autoimmune disease, or chronic inflammatory condition, which recruits polyclonal lymphocytes resulting in monoclonal lymphomas [6]. In contrast, the patient in this case report did not have any chronic conditions. All workups were negative, including the entire viral panel and autoimmune markers. Basic research is needed to determine the etiology of PCNSL, especially dural-based lymphomas. In the patient in this case report, the initial radiological findings were mimicking those of a meningioma: dural-based and uniformly enhanced. There was significant surrounding edema, significant diffusion restriction, and blooming in susceptibility-weighted image, which goes more with higher-grade meningioma or another high-grade lesion. One review has shown that primary dural-based lymphomas can display the “dural tail “sign, further confusing the preoperative diagnosis with meningioma [12], which did happen in the patient in this case report. Therefore, we suggest that in case of a dural-based lesion that has non-typical features of grade 1 meningioma, clinicians should consider lymphoma in the differential diagnosis and avoid steroids unless necessary due to edema and mass effect keeping in mind the ghost tumor phenomena of lymphoma.
The role of surgery in PCNSLs is limited mainly to histological diagnosis through biopsy or tumor debulking in case of increased intracranial pressure or impending brain herniation. Some studies have shown no benefit of complete surgical resection of PCNSLs; however, a recent systematic review of 244 articles has shown evidence in support of cytoreductive surgery [13]. Previously, whole-brain radiotherapy (WBRT) was the recommended treatment; however, this treatment modality resulted in a high rate of relapse and a decrease in performance status and cognitive impairment, and with the improvement in survival with high-dose methotrexate, WBRT is no longer recommended. Currently, newly diagnosed PCNSLs are initially treated with induction chemotherapy until complete radiological response, followed by consolidation therapy, to prolong the overall survival [14]. The International Extra Nodal Lymphoma Study Group-32 trial has shown that a methotrexate-based MATRIX regimen results in a good outcome and control rate in PCNSL [5], and it is the standard induction chemotherapy. Ferreri AJM, in his article “The role of autologous stem cell transplantation in PCNSL” has compared various consolidation phase treatment modalities, including beam radiation, carmustine–thiotepa regimens, and autologous stem cell transplantation, and the results showed that autologous stem cell transplantation resulted in good outcomes [15]. The patient in this case report showed a good response to treatment with almost total resolution of PCNSL with three cycles of MATRIX chemotherapy, followed by conditioning chemotherapy with stem cell infusion.
Conclusion
PCNSL is a rare entity. Clinicians should always consider it in differential diagnosis of meningioma if the radiological findings are not typical for meningioma. When there is a high index of suspicion of lymphoma, repeating neuroimaging, particularly MRI, before surgery, especially if the surgery is delayed while the patient is on steroids, may help develop a better management plan while dealing with this rare lesion. In case of lesion disappearance, falx biopsy can be an option. The aim of surgery in PCNSL is mainly biopsy or debulking to decrease intracranial pressure in case of significant mass effect.
List of abbreviation:
Primary central nervous system lymphomas (PCNSLs)
Central nervous system lymphomas (CNSLs)
Head computed tomography (CT)
magnetic resonance imaging (MRI)
positron emission tomography (PET)
fluorodeoxyglucose (FDG)
whole-brain radiotherapy (WBRT)
#Dural-based tumor#diffuse large B-cell lymphoma#ghost tumor#MATRIX regimen#central nervous system#jcrmhs#Clinical decision making#Is Journal of Clinical Case Reports Medical Images and Health Sciences PubMed indexed
2 notes
·
View notes
Text
3 notes
·
View notes
Text
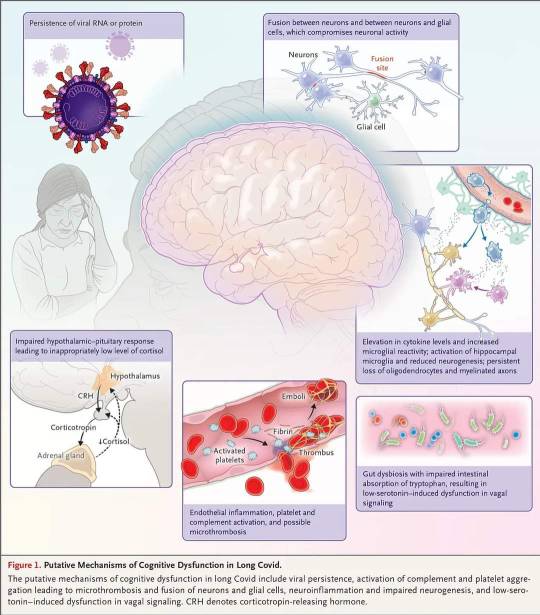
#LongCovid and Cognitive Deficits by @EricTopol
"None of this is good news for Long Covid and the brain, folks."
https://erictopol.substack.com/p/long-covid-and-cognitive-deficits?utm_campaign=post&triedRedirect=true
#psychiatry #neuroscience #BrainHealth #Neurology #brain #SARSCoV2 #COVID19 #CentralNervousSystem #NervousSystem #BrainFog
#Long COVID#psychiatry#Neuro Science#Brain#Brain Health#Neurology#SARSCOV2#COVID19#Brain Fog#central nervous system#nervous system
4 notes
·
View notes
Text
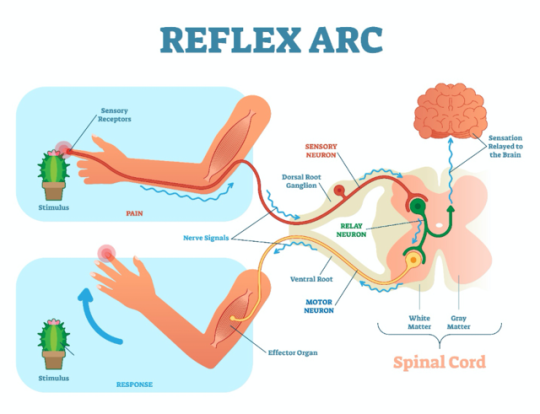
Outstanding Understanding the Nervous System: Parts and Functions 1
Have you ever wondered how your body coordinates all its movements and processes? It’s all thanks to an incredible network known as the nervous system. In this article, we’ll take a journey through the intricate workings of the nervous system, breaking down its parts and unveiling its fascinating functions. The Central Command: Brain and Spinal Cord The brain and spinal cord are the dynamic duo…

View On WordPress
#Autonomic Nervous System#Blood-Brain Barrier#brain function#Central Nervous System#Limbic System#Motor Function#nervous system#neurological disorders#Neurology#Neurons#Peripheral Nervous System#Reflexes#Sensory Perception#Spinal Cord
2 notes
·
View notes
Text
Fibromyalgia: Latest Findings and prevention tips!
Fibromyalgia is a chronic disorder characterized by widespread musculoskeletal pain, tenderness, and other symptoms. Despite its prevalence, fibromyalgia has long been shrouded in mystery due to its complex and often elusive nature. However, recent research has shed new light on the condition. In this blog, we will be discussing fibromyalgia, Its latest findings, and prevention tips. We will also…
View On WordPress
#Anti-inflammatory diet#Balanced nutrition#Central nervous system#Chronic pain#Cognitive difficulties#Diagnosis criteria#Exercise benefits#Fatigue#Fibromyalgia#Genetic factors#Mind-body techniques#Mood disorders#Neurochemical imbalances#Quality of life#Research findings#Sleep disturbances#Sleep hygiene#Stress Management#Symptom clusters#Tender points#Treatment strategies#Widespread pain
1 note
·
View note
Text
"When it comes to having a central nervous system, and the ability to feel pain, hunger, and thirst, a rat is a pig is a dog is a boy."
Ingrid Newkirk, animal rights activist (b. 11th June 1949)
0 notes
Text

TSRNOSS, p 531.
#superoxide#collagen#hyperkalaemia#accelerated ageing caused by diabetes#peripheral neuropathy#central nervous system#aortic aneurysm#Marfan's syndrome#diabetes#kidney#branched chain aminoaciduria#hypoglycemia#salicylates#Reye's syndrome#phenytoin#tumours#tryptophan metabolites#Grave's disease
0 notes
Link
#Multiple sclerosis#Central nervous system#Dietary assessment#Food frequency questionnaire#Arab countries
1 note
·
View note
Text
Central nervous system? Yeah we’re pretty nervous. What about it?
0 notes
Text
New study shows a simple blood test may predict MS
New study shows a simple blood test may predict MS #study #research #ms #multiplesclerosis #nervoussystem #pathology #science #health
In the journal, Nature Medicine, a new study, “An autoantibody signature predictive for multiple sclerosis,” shows that approximately 10% of people in the wide-ranging study with Multiple Sclerosis, or MS, harbored antibodies that target a specific sequence contained in human proteins. These antibodies could be detectable years before the long-lasting, chronic disease’s onset or other markers of…

View On WordPress
0 notes