#symptoms of postpartum depression and anxiety
Explore tagged Tumblr posts
Text
#Postpartum Depression Therapy#postpartum depression#post pregnancy depression#post childbirth depression#postpartum depression and anxiety#postpartum depression therapist#postpartum depression treatments#symptoms of postpartum depression and anxiety#pregnancy postpartum depression#postpartum mental health support#postpartum depression group therapy#post partum depression support group
0 notes
Text
Cognitive Behavioral Therapy (CBT) for anxiety is a type of psychotherapy that helps individuals manage and overcome their anxiety by identifying and changing negative patterns of thinking and behavior. CBT is based on the idea that our thoughts, feelings, and behaviors are all interconnected, and that by changing the way we think and behave, we can change how we feel. Cognitive Behavioral Therapy For Anxiety with the individual to identify the thoughts and beliefs that contribute to their anxiety symptoms. Cognitive Behavioral Therapy helps the individual challenge and reframe these thoughts, which can help reduce anxiety.
#Cognitive Behavioral Therapy For Anxiety#Generalized Anxiety Disorder Symptoms#Treatment For Generalized Anxiety Disorder#Symptoms Of Mood Disorder#Social Anxiety And Depression#Social Anxiety Disorder Symptoms#Premenstrual Dysphoric Disorder Symptoms#Persistent Depression Disorder#Clinical Depression Symptoms#Physical Symptoms Of Anxiety Attack#Anxiety Disorders Types#Schizoaffective Disorder Symptoms#Major Depressive Disorder Symptoms#Symptoms For Postpartum Depression
1 note
·
View note
Text
The Best News of Last Week
1. Amazon deforestation falls over 60% compared with last July

Deforestation in the Brazilian Amazon fell by at least 60% in July compared to the same month last year, the environment minister, Marina Silva, has told the Guardian.
The good news comes ahead of a regional summit that aims to prevent South America’s largest biome from hitting a calamitous tipping point.
2. 4,000 Rescued Beagles, Bred for Research, Found Homes and Best Friends

A heartwarming story unfolds as a beagle named Fin marks the end of a heroic 60-day mission to save almost 4,000 dogs from distressing conditions at a breeding facility. Beagles once underfed, sick, and mistreated have found their way into loving homes, enjoying grassy romps and birthday cake celebrations.
From "Sir Biscuit of Barkingham" to "Nervous Nellie," these four-legged heroes are adapting to their new lives with wagging tails and leaps of joy.
3. 'Cancer-killing pill' that appears to 'annihilate' solid tumours is now being tested on humans
A "cancer-killing pill" has appeared to "annihilate" solid tumours in early research - leaving healthy cells unaffected.
The new drug has been in development for 20 years, and is now undergoing pre-clinical research in the US.
4. Petting other people's dogs, even briefly, can boost your health

It turns out even short, friendly interactions with canines can be good for our health. Evidence is accumulating that levels of the stress hormone cortisol drop in people after just 5 to 20 minutes spent interacting with dogs — even if it's not their pet.
5. FDA approves first pill for postpartum depression

The Food and Drug Administration on Friday approved the first-ever pill for postpartum depression.
The medication, called zuranolone, is taken daily for two weeks. In a pair of clinical trials involving women who experienced severe depression after having a baby, the drug improved symptoms — such as anxiety, difficulty sleeping, loss of pleasure, low energy, guilt or social withdrawal — as early as three days after taking the first pill.
6. Taylor Swift Gives Bonuses Totaling Over $55 Million to Every Person Working on Massive Eras Tour

The pop superstar recently gave bonuses totaling over $55 million to everyone (from her dancers to riggers, sound technicians and catering, among others) working on her massive show.
TMZ previously reported that Swift, 33, gifted truckers on her tour $100,000 each ahead of her concert stop in Santa Clara over the weekend.
7. Successful room temperature ambient-pressure magnetic levitation of LK-99

In summary, this paper provides confirmatory synthesis and enhanced magnetic levitation of LK-99 at room temperature. The results support the possibility of intrinsic high temperature superconductivity in this system, but lack electrical evidence. More measurements and theoretical work are still needed to conclusively demonstrate and explain claimed room temperature superconductivity in this apatite material.
----
That's it for this week :)
This newsletter will always be free. If you liked this post you can support me with a small kofi donation:
Support this newsletter ❤️
Also don’t forget to reblog.
524 notes
·
View notes
Note
How’s your efforts re-adjusting after childbirth? How was recovery and everything. I know some people have little to no feeling down there after for a while (especially adult feelings, like libido killing stuff). Also have you felt any postpartum depression or anxiety or anything? Hope ur okay azi!!! And that you’ve recovered good.
I've recovered well, thank you, and thankfully, I haven't had any postpartum symptoms this time. - Aziraphale
#good omens#ask blog#aziraphale#good omens ask blog#crowley#aziracrow#ineffable husbands#ineffable spouses#good omens 2
42 notes
·
View notes
Note
Hi there! I love your headcanons and I was wondering if I could make a personal request. Let me know if this is a no-go.
I have PMDD, premenstrual dysphoric disorder, basically PMS [premenstrual syndrome] but 20x worse. It usually resolves upon the onset of the crimson wave. But not all the time.
I have been struggling really badly with the deep depression, insomnia, and self-image issues brought on by my disorder.
Do you think we can see how the Batch handles their fem reader S/O struggling with this disorder specifically? And maybe, if it's not too much, a part 2 with some of our favorite regs?
Thank you so much!
Aloha my dear!
Oh, this is a heavy hitter, I know where you are coming from. So many people out there have no idea how freaking much this can affect someone's life. PMS is already a hard thing to deal with, but PMDD brings it to yet another really shitty level. Don't worry, I got you 😊
The Bad Batch x Afab!Reader HCs - Struggling With PMDD

Warnings: Mention of PMDD (premenstrual dysphoric disorder) and its symptoms /Hurt/Comfort/Fluff
_______
AC: I'm using Techs Part first to introduce PMDD and its symptoms to those who might not know what it is. So don't be surprised about Tech's Part being longer than the others, there is a lot of information in there. So please read Tech's part, to understand what this is all about 😊
_______
Ko-Fi (If you feel like giving me some coffee)
_______

Tech
The first experiences he has with you in this context are frightening for him. Apart from the fact that you suddenly seem like a completely different person to him, he is really worried about you. But Tech wouldn't be Tech if he didn't get to the bottom of this.
It takes him a little while to find the right material.
Premenstrual dysphoric disorder (PMDD) is a much more severe form of premenstrual syndrome (PMS). It may affect women of childbearing age. It’s a severe and chronic medical condition that needs attention and treatment. Lifestyle changes and sometimes medicines can help manage symptoms.
The exact cause of PMDD is not known. It may be an abnormal reaction to normal hormone changes that happen with each menstrual cycle. The hormone changes can cause a serotonin deficiency. Serotonin is a substance found naturally in the brain and intestines that narrows blood vessels and can affect mood and cause physical symptoms.
What are the risk factors for PMDD?
While any woman can develop PMDD, the following may be at increased risk:
Women with a family history of PMS or PMDD
Women with a personal or family history of depression, postpartum depression, or other mood disorders
Other possible risk factors include lower education and cigarette smoking
Talk with your healthcare provider for more information.
"Healthcare provider?" he mumbles softly between reading, "As if any of us have such a thing"
Symptoms of PMDD appear during the week before menstruation and end within a few days after your period starts. These symptoms disrupt daily living tasks. Symptoms of PMDD are so severe that women have trouble functioning at home, at work, and in relationships during this time. This is markedly different than other times during the month.
There is a chart with symptoms and he worriedly starts to read it.
The following are the most common symptoms of PMDD:
Psychological symptoms
Irritability
Nervousness
Lack of control
Agitation
Anger
Insomnia
Difficulty in concentrating
Depression
Severe fatigue
Anxiety
Confusion
Forgetfulness
Poor self-image
Paranoia
Emotional sensitivity
Crying spells
Moodiness
Trouble sleeping
Fluid retention
Swelling of the ankles, hands, and feet
Periodic weight gain
Diminished urine output
Breast fullness and pain
Respiratory problems
Allergies
Infections
Eye complaints
Vision changes
Eye infection
Gastrointestinal symptoms
Abdominal cramps
Bloating
Constipation
Nausea
Vomiting
Pelvic heaviness or pressure
Backache
Skin problems
Acne
Skin inflammation with itching
Aggravation of other skin disorders, including cold sores
Neurologic and vascular symptoms
Headache
Dizziness
Fainting
Numbness, prickling, tingling, or heightened sensitivity of arms and/or legs
Easy bruising
Heart palpitations
Muscle spasms
Other
Decreased coordination
Painful menstruation
Diminished sex drive
Appetite changes
Food cravings
Hot flashes
His brows are drawn together critically. With a heavy sigh, he says quietly to himself, "Oh boy…"
Tech makes it his business to see that you are examined by a proper doctor, given appropriate medication, and change your diet. He sometimes seems stern and matter-of-fact, but only when he notices you neglecting yourself. Tech also pampers you to counteract the psychological symptoms, with picnics, massages and the like.
Don't worry too much, Tech's got your back. He won't give up on you.
Hunter
His senses already tell him what connections exist with your condition. But of course he is not a doctor and therefore informs himself accordingly without your knowledge, Tech helps him. What he learns frightens him, Hunter is really worried, and he makes it his mission to make this time, these symptoms, easier for you. Apart from making sure you always have the medication you need at hand, he is also much more attentive and caring than usual during this time.
You can let yourself go and not have to worry about anything, Hunter takes everything in hand and has it under control. He is especially gentle and forgiving with you during this time. You mean a lot to him, and he does his absolute best to help you.
He doesn't argue with you when you get your moods, if you want to be alone he respects that, but keeps an eye on you from a safe distance, just in case.
Echo
This sweet man really throws himself into the task of helping you. Whether it's getting your medications, preparing food, massages, and running relaxing baths, Echo has it all covered.
With him by your side, you will want for nothing during this difficult time. He is also not easily scared away, he is as patient as he is stubborn. You don't have to go to the doctor alone, Echo will accompany you.
He organizes your medication, your diet and everything else you need, if you want. If you don't, you must tell him clearly, because Echo will automatically see his task in taking care of everything.
Wrecker
He is warm, and lively. Contrary to the expectations of most, he is also very sensitive and attentive. Of course, he does not miss the fact that something is wrong with you. Of course, he is worried and wants to help.
Talk to him honestly, try not to withdraw, and you will have a steadfast supporter and caretaker in Wrecker. He likes to spoil you, make sure you are taken care of and have your medication.
Wrecker is happy to adapt to you, you just need to communicate with him and let him know what you need. Taking care of you is very easy for him, he likes to do that. Knowing that he can make things easier for you is also good for him in this situation. So confide in him, there is absolutely no reason to pretend in front of him.
Crosshair
He is a bit more complicated at first. Of course, you are incredibly important to him, and he also has a certain empathy, but he often stands in his own way when it comes to emotional, interpersonal things.
At first, he can't really deal with it at all and is looking for some distance at this time. But in a small conversation between brothers, in which Hunter makes it clear to him that his behavior sooner or later can seriously damage your relationship, Crosshair first informs himself more precisely about the existing problem. Finally, he approaches you with the knowledge he has gathered and tries to discuss with you what you can do together as a couple, what he can do as your partner to make the whole thing easier for you.
You talk about medications, doctor visits, relaxation techniques, and home remedies to combat some symptoms. It doesn't take long for the two of you to work out a certain routine that you can both manage and that he can use to help you get through this time okay.
@rintheemolion
@andyoufollowyourheart @clone-whore-99
@brynhildrmimi @kaliel2310
@misogirl828 @tech-deck
@meshla-madalene
@chxpsi
@thebahdbitch
@nahoney22 @ladykatakuri
@darkangel4121
@ttzamara
@arctrooper69
@padawancat97
@agenteliix
@allsystemsblue
@palliateclaw
@either-madness-or-brilliance
@ortizshinkaroff
@andy-solo1
@hunterssecretrecipe
@heyitsaloy
@greaser-wolf
@extrahotpixels
@hated-by-me
@hunterxcrosshair
@malicemercy
@bebopsworld
@echos-girlfriend
@cpnt616
@dangraccoon
@jediknightjana
@pb-jellybeans
@antishadow2021
@sleepycreativewriter
@projectdreamwalker
@1vlouds
#star wars#tbb#the bad batch#clone force 99#sw tbb#tech#tbb tech#crosshair#bad batch tech#hunter#wrecker#echo#hunter x afab reader#echo x reader#wrecker x reader#tech x reader#crosshair bad batch#bad batch crosshair#echo x you#echo x female reader#hunter x reader#star wars the bad batch#star wars: the bad batch#the bad batch fanfiction#the bad batch x reader#tbb x reader#tbb headcanons
143 notes
·
View notes
Note
howdy!! i was wonderin’ if you could list all the cats that are neurodivergent or have a mental disorder, and specifically what conditions? i was also hopin’ if you could expand upon how they present as well, but you don’t have to do all of them! you can pick and choose. or none at all if you’re tired! idm ‘:3
warriors and psychiatry are two of my SIs so i just wanna gobble up all of this information LOL
Sure! Though, I want to preface by saying that I try to make sure I'm very well acquainted with the neurodivergence I plan to add before adding it. I've always had a, "try not to overextend" sort of philosophy, trying to make sure each portrayal is going to be treated well in the narrative before promising it publicly
SO what that means is that this list is incomplete and I plan to add more, as I learn more about how to accurately portray something. Especially important with the more stigmatized disorders on this list-- for example I plan to add NPD once I have a better idea for how to feature it.
C-PTSD
Life in the Clans is VIOLENT. Most, or many, characters are going to end up with symptoms of PTSD, especially the cats who lived through the Plague, TigerClan, the entire Mothermouth Moorland War, and the destruction of the White Hart Woods in particular.
But C-PTSD is something I'm choosing more carefully, if that makes sense, so that it's something I write with 'higher priority' when approaching that particular character.
Birchfall (Human activity and child starvation are his triggers, also visibly unsettled by falling trees)
Brightheart (Dogs and dishonor titles, has recurring nightmares, self-harms through overexertion; refuses to take breaks to punish herself)
Stormfur (Severe trust issues, self-destructs relationships)
Lilyheart (Can't deal with water because she watched a sibling die instead of her)
Harrybrook ("big mood lilyheart")
There will also be some cats in WindClan who aren't able to eat rabbit, because it triggers memories of poison and causes them to wretch. This causes serious issues for them, because rabbit is the majority of the WindClan diet, especially in winter.
Epilepsy
Sorreltail (Absence seizures caused by brain damage from nightshade poisoning)
Shadowsight (Severe clonic-tonic seizures, Tawnypelt brings him to the Tribe to seek a very special treatment for him)
I reaaaaally need to add more here tbh
Autism
Mumblefoot (I know he's not a major character lmao but he was Pinestar's first deputy, and had dyspraxia.)
Yellowfang (It's super prevalent in her entire familial line)
Rowanberry
Stumptail
Brokenstar
Littlecloud
Rowanstar
Leafpool
Honestly I'm so autistic I kinda end up putting a little bit of autism in everyone. I feel like I can detect autism in every one of my little favorites. Spottedleaf, Speckletail, Dustpelt, etc
Borderline Personality Disorder
Cinderheart
Breezepelt
Squirrelflight
Etc/There's one cat who has it and I need to add more
Bumble, Blossom, and Briar have a lot of baggage from their parents' treatment, Bumble and Bloss are glass children.
Alderheart has anxiety
Carpwhisker might also have anxiety, she's really bad at standing up for herself
Poppyfrost is severely avoidant
Sparkpelt and Palebird both had postpartum depression
Dovewing has burnout and gets stressed out when her biofamily is around; not sure how to describe this.
Squirrelflight also has ADHD, this is kind of like Autism because I also have ADHD and it's difficult for me to imagine other 'ways' people think. like what do you MEAN, you have ONE train of thought??
81 notes
·
View notes
Text
PAIN UNSPOKEN
(DEPRESSION)
Right before your eyes we all see and deal with depression one way or another many are just better at hiding It. It gets overlooked and treated like everyone's symptom is the same. In many cases their not, there are so many different symptoms and signs of depression. Now their are some people who self afflict depression on theirselves by always wanting things their way or not being happy over what they were blessed with. The real cases are, clinical depression ( which can deal with appetite loss, energy loss, lack of sleep, self esteem, and suicide thoughts.) Persistent depressive disorder ( just like clinical but on a more milder side, also loss of sleep, appetite, energy levels, only different these symptoms are mild but can become long term in a persons life.) Bipolar disorder ( which deal with episodes of mood swings and lows and highs of manic highs, can make a person very indecisive in life and needs.) Also their is a bipolar disorder level 2 ( its the same as the original bipolar but it can make person have one particular depress state weeks at a time then jumping to another class depress state for a couple days, and make the person very irritable.) Postpartum depression ( called PPD, which a mom deals with after conceiving a newborn, she gets random mood swings, crying, anxiety, can last for weeks if not treated or recognized can become a long term illness.) The list doesn't stop. Their are so many illnesses that we all deal with everyday. Everybody brain haves something going on differently, doesn't mean that you are crazy or you should be alienated because of your symptoms. Everyone brain is unique in their own way, some just obtain knowledge faster or at a different capacity than others, while many may need to break it down and compartmentalize different situations is sections to understand. We see people behaving at a maniac and abnormal way we are so quick to judge a person and classify them in such terms like they are a subject or a science experiment. When dealing with such people it takes patience, understanding, and knowledge to apply the care and healing. This all stems from are different genetic makeups, past-life, upbringing, natal alignments, aspects, and lifestyle you live. If you are familiar with astrology there are some placements that could justify these symptoms. The moon can cause depression, not the moon alone but its conjunction or if its debilitated. The moon deals with the mind, emotions and how you react to different situations everyday. also, Saturn, Rahu, Ketu, Mercury and Jupiter can also effect your mood. If the moon is your peace and solitude and Saturn is cold and heavy these two will cause your mental to be at a detached way of thinking and look at the world as cold and not inviting. You begin to make yourself feel unworthy and criticize your own thoughts, which would put u at a depress stage. When Ketu get involved it digs in your subconscious so if you have deep rooted issues and bad habits that never been corrected it can be brought forward by a conjunction, transit, or progressed planet alignment. The moon is so sensitive in our chart, its the place we run to for solitude and protection when the world seems to be cold and not comforting. So being said, if your moon is debilitated or in conjunction with a harsh planet can cause your brain and thoughts to stem from a dark and not rational place. Like the planets the natal houses play a major factor, since they represent the part of life actions take place. The 6th, 8th, and 12th are the Dusthana houses, which means difficulties and where life is faced with challenges, bring sorrows, suffering, and so on. By having one of these houses contributing towards a bad malefic can be detrimental. not saying everyone who has planets in these houses will have mental conditions or depression just stating it can be a cause to someones symptoms. We tend to let our emotions control our actions, and mind control our thoughts, when we should always follow our hearts.
Since the heart is the first organ made in us why not follow its rhythm. Depression is a real symptom and some people cant or don't know how to accept it or deal with the symptoms that effects their brain and the way they make day to day decisions. We all have a complex brain and never really unlocked our full potentials, we cloud our brains more and more with technology and negative sensory thats helps contribute towards our unlaying illnesses. Everyone is out here crying for help in different ways we just tend to do it in our own subconscious ways. Alot of people shop, spend alot of money on items they dont need, eat alot of food, sleep excessively, and when it gets very serious some try to commit suicide thinking thats the way out. Statistics show that 7 out of 100 men and 1 out of every 100 women will go through with suicide thats crazy and messed up. This needs to change its too many people on this earth to let the next person walk by you and not try to understand these symptoms when they are shown in their body language, facial expressions, and conversations. At times their are people who are dealing with heavy cases of depression and you wouldn't even know. Thats why its important to ask a person " how you feel ? ", "how was your day ? ", " are you ok ? ", "you sure you are ok? ". These little actions can and could make a persons day better or even keep a person from trying or commiting suicide. Depression can even be a deep rooted family generational curse or bad karma that needs to be broken by you understanding its underlying habits. Medication only contains the symptoms but doesn't cure it, the more you take the meds the more you become dependent on it. These situations need to be addressed from a deeper biological method. Even the foods we consume, energy we take in puts our mental health at risk to putting us in a global detriment to society. We our so caught up in our own lifes and problems that we don't acknowledge others issues, not that its your responsibility or obligation. I do feel we all have Dharma as a collective, so helping someone when their are down and uplifting them is a strong way to create a generational revolutionary change.

20 notes
·
View notes
Note
Do you have a perspective on why stimulants aren’t currently widely prescribed as weight loss drugs? Im guessing it’s related to it being a ‘controlled substance’ and ‘scary drug’ but drug marketing in pursuit of pharmaceutical profits is pretty powerful… I wonder why I haven’t seen (effective?) efforts to try to ‘overhaul’ the image of stimulants as only associated with “addiction”, “hyperactive children”, finance bros, and “lazy adults”.
I know vyvanse is also prescribed for binge eating but I get the sense most people are unaware of that. I tried many stimulants and I had the most rapid and “easy” (found food repulsive) weight loss on vyvanse. Granted all of the many prescribed stimulants I’ve tried all greatly suppress my appetite.And I’ve seen it described as a benefit by some people who have it prescribed for adhd (I understand why people do and I sometimes see it as a very depressing benefits because lack of food security despite). Binge eating disorder and prescribing for general weight loss aren’t too far from each other in the fatphobic society we live in but I guess I’m curious how it hasn’t had the ozempic treatment already/ when will it happen. People already look down of folks who can’t function by society’s standards in certain contexts and I see that similarity in how people talk about people who take ozempic for weight loss (admonishing and a moral failure).
stimulants absolutely still are prescribed for weight loss lol, in addition to Vyvanse for 'binge eating' (v unreliable diagnosis that many people receive when they are in fact dealing with subjective loss of control around food as a direct result of restrictive behaviours...) there's also Desoxyn (methamphetamine) and Phentermine (a substituted amphetamine), which are both still FDA-approved for short-term weight management. and yes that's Phentermine as in half of fen-phen. you also have to keep in mind that off-label prescribing is hard to track but is probably still occurring at not-insignificant rates (i know it happens with Ephedra and Clenbuterol, for example). and then there are also patients who use stimulants for weight loss without a doctor's knowledge, either by obtaining them on the black market or by simply getting a doctor to prescribe them for something else.
anyway in regards to pharma marketing strategies i think there are a few things going on here:
weight loss has never actually been the sole market for these drugs, nor was it the first. amphetamine was first synthesised in 1929; it was put into asthma inhalers almost immediately and by the late 30s was being sold as a kind of generalised wellness-producing drug, used by, for instance, college students as a 'pep pill'. the Allies used quite a bit of amphetamine in WWII to keep soldiers alert (the US military was still doing this in Iraq and Afghanistan in the 2000s; afaik they have not stopped this practice). by the late 50s stimulants were also marketed as pick-me-ups for unhappy housewives and for a dizzying array of depression 'subtypes' (postpartum, old age-related, disability-related) and 'modern miseries' (atomic anxiety, economic and political unrest). it wasn't until the 50s and 60s that stimulants really started to be marketed as diet pills, with 'overeating' configured as a symptom of depression. even those formulations also had other use markets: professional athletes, for example. i'm sure pharma companies would love to have the stimulant dominance they once did in weight loss, but it's not really necessary in order to move product: these days the ADHD diagnosis will generally do the job just fine. nicolas rasmussen's book On Speed has more on this history.
speaking of the ADHD diagnosis, i have observed that in the last two or so decades, it has increasingly been invoked in bioessentialist narratives of either 'chemical imbalances' (usually dopamine, norepinephrine) or distinct 'neurotypes' that are said to cause, worsen, or be susceptible to 'overeating', which can therefore be treated by the use of stimulant drugs. i strongly suspect an effect here is that 'overeating', weight gain, or 'obesity' are de facto being used as diagnostic criteria for ADHD, or for other psychiatric diagnoses considered to have high overlap in behavioural presentation. this is not dissimilar to the formulation in the 60s of 'overeating' as a result of depression; in both cases the narrative elides the appetite-suppressant effects of stimulants and presents them as aiding with weight loss by treating an underlying bio/psychiatric pathology. an interesting historical note here is that Adderall is simply a rebrand of the second-gen formulation of the weight-loss drug Obetrol.
presently, weight loss is largely marketed using the language of health rather than aesthetics. although pharma companies are certainly not morally above lying, i do think it would be a tough pill to swallow (pun intended) if they tried to convince anyone that a stimulant prescription is part of this sort of 'wellness' scene. that could change in the future, ofc; these perceptions and associations are socially and historically contingent. in the US even as recently as the 90s, people were definitely still presenting fen-phen as health-promoting (tautologically, because it caused weight loss!), at least until the valve disease scandal.
glp-1 agonists like ozempic are, i think, getting a lot of extremely credulous coverage, from both the medical establishment and health journalists, that is obfuscating the fact that they basically also work by suppressing the appetite. whether it is 'healthier' to do this with a substance that alters endocrine function than to do it with a substance that acts on adrenergic receptors is unclear to me. certainly there are many 'side effects' of the glp-1 agonists that are simply the results of rapid / significant weight loss (fatigue, weakness, osteoporosis, hair loss, gallstones, 'ozempic face', &c). that a process that causes these things can be marketed as health-promoting is a whole other topic lol. but i think the perception of the glp-1 agonists as healthful weight-loss agents has to do with certain misunderstandings of diabetes, metabolism, and body weight, as well as a degree of... not quite blackboxing, but something adjacent, on the part of pharma companies in their promotional materials. which is to say, it wouldn't surprise me if, in the future, people looked back at glp-1 agonists as also being risky drugs to use for weight loss, and only being worth using in specific, limited circumstances.
42 notes
·
View notes
Note
Pregnant Lin head cannons ? Was conceiving easy for her or was she infertile ? What symptoms does she experience ? What cravings does she have ? Any complications ? How does the birth go ? After birth what is her postpartum experience like ? Does she experience ppd ? Is breastfeeding easy for her ?
Hi! Thanks for the ask! (I'd like to preface this post with a disclaimer that I have never been pregnant, so this may not be entirely accurate)
Lin conceived relatively easily and never had any fertility issues. Her pregnancy was actually unplanned.
She had pretty bad morning sickness during her first trimester. She was especially sensitive to smells and sometimes the scent of certain ingredients cooking would make her queasy. She also experienced a lot of fatigue during her pregnancy and needed a lot more sleep than she was used to.
Lin's biggest craving was for citrus fruits like tangerines and pomelos Her partner would always make sure the apartment was well stocked with them, and peel them for her when she wanted a snack. (I wrote a linzolt oneshot called Tangerines around this idea). Her pre-existing love of spicy foods was intensified while she was pregnant, so she ate a lot of fire noodles and fire flakes.
Because she was having twins, Lin was at a higher risk for preterm labor and gestational hypertension. However, her medical team (including Katara) monitored the situation and she ultimately didn't experience those effects.
Lin has a pretty high threshold for pain, but nothing could have prepared her for childbirth. She was in labor for fourteen hours and it was a bit of an ordeal. Her partner was with her the whole time, holding her hand and feeding her ice chips and sips of water.
When she came home from the hospital, Lin's partner did not let her lift a finger. She got to rest and recover from the birth, taking naps and listening to probending on the radio and just bonding with her new babies. Her partner took care of everything around the house so she could relax.
Lin doesn't have postpartum depression, but she does experience some anxiety around being a new mom.
Breastfeeding is relatively easy for her, but after a few weeks she switches to bottle feeding because she wants to start checking in with Saikhan at the RCPD.
#lin beifong#chief beifong#legend of korra#headcanons#linzolt#but i think these can work with most lin ships
20 notes
·
View notes
Text
You are loved. What to do in a crisis and resources on how to get help with mental illness.
If you can, please reblog this so people can be aware of how they can get help.
Hello world! I just thought I’d provide some resources for all the mentally ill out there in this existence. These all worked for me and hopefully they can work for you. If you think you may be suffering from mental illness go to section two and three. If you are currently in crisis, which means you think about or have planned your suicide, go to section one and read through the rest of this post. You are not alone, 792 million people live with mental illness. 264 million live with depression, and 284 million live with anxiety. If you are reading this, it’s a sign to start getting help. If you are struggling, these resources can help you. Just give it a try, it’s worth it. Just remember. You are loved. You are wanted. You are cared for. You are noticed. You deserve to live.
IF YOU ARE IN CRISIS:
Call a suicide hotline!!!!
Hotlines can be helpful at calming you down in a time of high emotion or stress, these people are literally trained to distract you. I’ve called them a few times in my life and it does work I promise. Just try it out.
The U.S number is 988
If you don’t live in the U.S, follow this link to find your countries hotline. Hotlines. Find it on the site and give it a call. Here are some additional hotlines and resource specific help.
Directory of international mental health helplines
A second list of global hotlines
Crisis hotlines for teens and youth
LGBT crisis support
Substance abuse crisis support
Postpartum support
National Domestic Violence Hotline: 800-799-7233
National child abuse hotline
Literally just a list of hotlines for everything
Either while you are on the phone with a hotline or after, send your location to a friend or family member so that someone can come get you or check on you. If that is not an option you can ask the hotline to send someone to come get you. DO NOT. I REPEAT. DO NOT. Stay by yourself in a time of need or crisis. The longer you are alone the more dangerous the situation can become. You are not a burden if you ask someone you love for help, that is what they are there for. Most likely you will be collected by emergency services and they will go from there.
IF YOU HAVE ALREADY TAKEN AN ACTION TO KILL YOURSELF DO THE FOLLOWING:
Call 911 if you are in the U.S
If you are not in the U.S call your countries emergency number. Here is a list of countries numbers:
List of emergency telephone numbers
If you are at home with family members go to your family and let them know what happened. Even if they are asleep, wake someone up if you have to. Do this AFTER you have contacted emergency services .
If you are on a college campus, contact your RA or your campus crisis line AFTER you have contact emergency services.
If you are by yourself, WAIT FOR EMERGENCY SERVICES TO ARRIVE. Do not move from your location.
In crisis and after you need to make a safety plan. Safety plans reduce risk of future harm by planning out actions that you can do yourself to reduce emotional stress. Here’s how:
Safety Plan
After crisis assistance:
After crisis assistance can include therapy and psychiatry. I will provide thinks for find both of these things. If you are not currently in crisis but you are experiencing symptoms of mental illness, please make an appointment with one of these assistances. Below there are additional resources for mental health that can also be used as a first step.
Therapists
International therapy directory
Psychiatrists
American Psychiatric Association
How to find a psychiatrist and other therapists
U.S Government resources
National hotline for resources
General mental health resources
GLOBAL mental health resources
Coping strategies:
Coping strategies are how you individually can cope and process emotions, thoughts, and feelings. They can be hobbies or things like journaling or writing or just something as simple as going on a walk. I will give links to lists of coping strategies that might help you.
Coping with anxiety
Self-harm coping strategies
Coping skills for depression
How to cope with suicidal thoughts
35 coping skills to try
Self- help techniques for mental illness
100 coping strategies for all things
#stay here#stay with me#dont let go#dontgiveup#dontgivein#mental illness#mentall illness#mental health#i love you#just know#therapist#therapy#coping#strategies#psychiatry#psychiatrist#mental health resources#help hotline#crisis hotline#howtogetbetter#coping strategies#safety plan#get help#stay alive#mental illness recovery#emotional health#psychiartist#psych usa#governmentresources#findatherapist
108 notes
·
View notes
Text
Postpartum Depression Symptoms
Postpartum Depression is the onset of a depressed mood and its associated symptoms within the first year of childbirth, lasting more than two weeks with or without treatment.
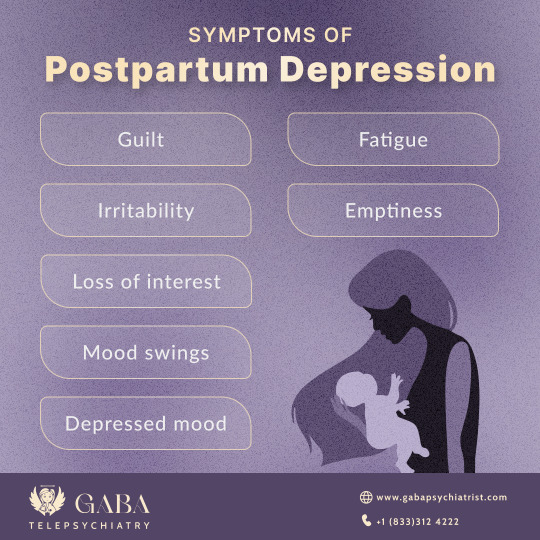
It is vital to seek help and treatment for postpartum depression. Failure to do so may result in long-term negative consequences for both the mother and the baby.
What are the Symptoms of Postpartum Depression?
Since postpartum depression arises during a time in a mother's life when society expects her to be happy about the arrival of her new baby, it can be very isolating for mothers.
Postpartum depression symptoms can manifest in a variety of ways. It may affect one's emotions, perception, ideas, and bodily experiences. Postpartum depression can cause hallucinations, delusions, and paranoia in severe cases.
Symptoms of postpartum depression are usually classified as follows:
Physical Symptoms of Postpartum Depression
Fatigue
Headache
Back pain
Muscle ache
Joint pain
GI upset
Abdominal pain
Low sex drive
Cognitive Symptoms of Postpartum Depression
Inattention
Impaired executive functioning
Impaired problem solving
Impaired neuroplasticity
Memory loss
Slow reaction time
Mood Symptoms of Postpartum Depression
Bad mood
Low motivation
Loss of ambition
Loss of enjoyment in activities
Loss of will to live
Sleep disturbance
Loss of appetite
Psychotic Symptoms of Postpartum Depression
Hallucinations
Delusions
Loss of touch with reality
Paranoia
When psychotic symptoms occur together with postpartum depression, this is known as 'Postpartum Psychosis'. It is critical to seek immediate support if such a situation arises.
Thought Distortions with Depression
Negative thoughts about oneself
Negative thoughts about others
Pessimistic thoughts about the future
Excessive guilt about the past
Low confidence in abilities
Low self-worth
Angry thoughts
Nihilistic thoughts
Suicidal thoughts
Existential angst
How can untreated Postpartum Depression Symptoms impact your Career?
Mothers experiencing postpartum depression may experience problems with:
Energy levels
Motivation levels
Attention
Concentration
Irritability
Engagement with colleagues
Reasoning and problem-solving abilities
Frustration tolerance
Productivity
They may require help to complete tasks, meet deadlines, or take excessive time off work. They may find themselves in conflict with colleagues and supervisors with whom they previously worked well.
Similarly, colleagues and supervisors may be perplexed, frustrated, and unsure of how to address the issue of change in a beloved colleague and friend. After all, nobody wants to be a "workplace bully" or impolite to a new mother.
Working mothers who suffer from PPD are also more likely to be passed over for promotion or even fired from their current jobs.
What is the Treatment for Postpartum Depression?
Finally, treatment for postpartum depression must address the underlying cause.
Check for medical causes of postpartum depression, including anemia, thyroid disease, Sheehan's syndrome, nutritional deficiencies, and polycystic ovarian syndrome
Establish sleep hygiene and work with a partner to schedule catch-up sleep times
Educate both the mother and the partner
Document workplace accommodations
Consider what assistance is required so the mother can continue working if desired or needs to take time off
Use available resources, such as childcare, and, if possible, contact family members, including grandparents
Nutritional supplementation, if necessary
Counseling on breastfeeding and other issues
Psychotherapy
Individual Psychotherapy
Medications if symptoms persist and interfere with social and occupational functioning
Alternative treatments include meditation, yoga, acupuncture, and exercise
Why is it important to get Treatment for Postpartum Depression?
Untreated postpartum depression symptoms can disrupt both your personal and professional lives. Consequences for babies include disruption of attachment and bonding, anxiety, failure to thrive, feeding difficulties, developmental delay, long-term relationship difficulties, cognitive impairment, failure to meet milestones, and difficulty with social or occupational functioning.
Effects of Postpartum Depression on Health
Significant drop in energy and motivation levels
Feelings of restlessness
Disrupted sleep cycles
Insufficient or excessive sleep
Chronic stomach issues, headaches, or body pain
Poor self-care
Help for Postpartum Depression
It is critical to seek treatment for postpartum depression. Untreated depression can have long-term consequences for academic performance, careers, relationships, and physical health.
Call +1(833)312-4222 for Postpartum Depression help. For more information, visit https://gabapsychiatrist.com/postpartum-depression-treatment/
Seek effective and barrier-free treatment from a board-certified and licensed Online Psychiatrist at Gaba Telepsychiatry.
#health & fitness#mental health#postpartum#healthcare#motherslove#motherhood#parenting#momlife#post partum
7 notes
·
View notes
Text
I'm impatient, so does anyone want to hear any Egon and Cathleen during her pregnancies headcanons?
*no one raises their hands* Okay, here we go... It's all under the cut.
As I've brought up before, Egon and Cathleen struggled to conceive, and Cathleen suffered a second-trimester miscarriage.
After some time to heal and take a break (as well as Cathleen's struggles with alcoholism), Cathleen becomes pregnant with Callie.
They're living in Cambridge at the time, as Egon is studying at MIT, so Cathleen rushes to the campus to tell Egon as soon as her doctor confirms it.
Egon is just... so happy. But he's also very scared, as he's afraid what a second miscarriage or a stillbirth would do to Cathleen, as well as losing another baby.
Cathleen deals with a lot of morning sickness during the first trimester and well into her fourth month. Egon tries various cures that he's either read about or learned from his mother and his sister-in-law, but the most that Cathleen can keep down are water and saltines.
Doctors' appointments are always a source of anxiety for the both of them, but they're always relieved when they hear their baby's heartbeat.
Cathleen steals a lot of Egon's clothes as she gets bigger. By her ninth month, she's usually curled up in bed with a pillow between her legs and swimming in his MIT sweatshirt.
They both KNOW that the baby's a girl, but they still refer to the baby in a gender neutral way throughout the pregnancy.
You KNOW that Egon goes deep into researching everything there is to know about pregnancy. He also keeps logs of Cathleen's symptoms and the size of her growing belly.
He reads about bonding with the baby while they're still in the womb, and talks to the belly before he leaves for the day and when he comes home. He reads aloud to the baby, and Cathleen plays music.
Cathleen mostly craves sweets during her pregnancy, with her favorite being her mother-in-law's recipe for brownies.
Cathleen is a week or two overdue when she finally goes into labor. As she and Egon are leaving for the hospital, her water breaks in the car. Labor is long and grueling, but it's all worth it in the end when Callie Violet Spengler is born.
Cathleen deals with some pretty rough postpartum depression for the first few months of Callie's life. She's convinced that Callie hates her, that Callie loves Egon more than her, and that she's a terrible mother. Thankfully, she has a good support system (especially since she went no contact with her side of the family) and is able to develop healthier coping mechanisms.
In the Cathleen Lives AU, Marie is a bit of a surprise.
Cathleen is 44, not to mention Callie was the only child that she had carried to term up to that point, so she and Egon assumed that their childbearing days were behind them.
So imagine how shocked Cathleen is when her doctor tells that it's not early menopause, she's pregnant.
It takes about a day for her to let it sink in before she tells Egon.
While Egon is just as shocked as her, he is very happy.
Callie, who is nearing her ninth birthday, is excited about the idea of a little brother or sister, which relieves her parents.
Surprisingly, despite being an older mother, this pregnancy seems to go off without a hitch. I mean, she still has awful morning sickness, but there's no dire health concerns.
During the events of Ghostbusters II, Cathleen is very close to her due date.
Egon is pretty concerned with her being out in the field, but she insists that she can take care of herself.
Eventually, the stress of being wrongfully committed and learning that Callie followed Dana to the museum is a factor in sending her into labor, and she has contractions throughout the night.
After Vigo's defeat, her water breaks and she confesses to Egon that she tried to hide that she was in labor.
While Egon is upset that she didn't tell him, that is quickly swept away by excitement and happiness.
An ambulance is waiting outside to take Cathleen to the hospital, and by the time they arrive, she's fully dilated.
Marie Rae Spengler is born half-past midnight on New Year's Day.
#Cathlegon#I Want To Know Your Story#Cathleen Lives AU#Where The Cards May Fall#Ghostbusters#Ghostbusters II#Egon x Cathleen#Egon Spengler x Cathleen Paige#Egon Spengler#Cathleen Spengler#Cathleen Paige Spengler#Callie Spengler#Marie Spengler#Harold Ramis#Linda Purl#Carrie Coon#Kara Lindsay#Headcanons#My Headcanons#OC: Cathleen Paige Spengler#OC: Marie Spengler#OC: As Long As You're By My Side#TW Miscarriage
9 notes
·
View notes
Text

Obsessive Compulsive Disorder is a serious mental health condition that requires treatment. It is important to know the Symptoms Of Obsessive Compulsive Disorder. There are effective treatments available for OCD. Cognitive Behavioral Therapy (CBT) and Exposure and Response Prevention (ERP) are two evidence-based therapies that are effective in reducing symptoms of OCD. Medications such as selective serotonin reuptake inhibitors (SSRIs) may also be prescribed in conjunction with therapy. With proper treatment, individuals with OCD can learn to manage their symptoms and improve their quality of life.
#Symptoms Of Obsessive Compulsive Disorder#Seasonal Depression Treatment#Seasonal Affective Disorder Treatments#Signs Of Bipolar Disorder#Major Depressive Disorder Symptoms#Symptoms For Panic Attack#Best Medication For Panic Attacks And Anxiety#Premenstrual Dysphoric Disorder Symptoms#Symptoms For Postpartum Depression
0 notes
Text
New Data: Pregnant Women More Vulnerable to Long COVID - Published Aug 14, 2024
Victoria Coble, 39, of Greensboro, North Carolina, was 4 months pregnant when she started having symptoms of COVID-19. Things got much worse with the birth of her son, including intense anxiety, depression, and trouble concentrating, which expanded into nausea, chest pain, post-exertional malaise (PEM), and more.
At first, she had trouble disentangling her pregnancy and postpartum symptoms with symptoms that are common with long COVID. "At the time, I confused all of it with postpartum depression," Coble said. But 4 years later, the mother of two is still struggling just to get through the day.
Experts say pregnant women are diagnosed with long COVID in higher numbers than previously thought, although little historical data exist, and their symptoms are often misinterpreted for the normal signs of pregnancy. All of it makes motherhood and starting or expanding a family more difficult.
While it's hard to separate symptoms of pregnancy from long COVID, one of the key distinguishing factors is symptom persistence, said Ziyad Al-Aly, MD, a global expert of long COVID and chief of research and development at the Veterans Affairs St. Louis Health Care System, St. Louis, Missouri.
"Pregnancy symptoms eventually cycle out versus the fatigue with long COVID and post-exertional malaise, which often lingers," said Al-Aly. Pregnant women with long COVID are an understudied patient population. How often they get the disease and how it affects their pregnancy and their children were largely unknown until recently. But new research is beginning to unravel a mystery nearly 5 years in the making. Experts want to better understand how developing long COVID during pregnancy affects both mother and child and how new moms can care for their children while grappling with this debilitating disease.
In a study published this month in the journal Obstetrics & Gynecology, researchers found that nearly one in 10 pregnant women got long COVID after acute COVID-19 during pregnancy. Many went on to experience serious symptoms, including PEM — which occurs when symptoms worsen after even minor physical or mental exertion — gastrointestinal issues, and brain fog consistent with those experienced by the wider long COVID community. The numbers caught researchers by surprise.
"As an obstetrician, we typically take care of a younger, mostly healthy population in comparison to other specialties," said study author Torri Metz, MD, vice chair of research for obstetrics and gynecology at University of Utah Health, Salt Lake City, Utah. "To see that over 9% of this population went on to have symptoms consistent with long COVID was a higher number than I would have expected."
Additionally, said Al-Aly, during the height of the pandemic, COVID anti-vax rhetoric spread like wildfire, becoming a battle for the hearts and minds of a vulnerable patient population. A small study published in the November 2022 issue of the journal Midwifery found that even among those who later got the jab during pregnancy, anti-vaccine rhetoric fueled their hesitancy to do so.
Lower vaccination rates, due to early misinformation about the safety of COVID shots in pregnancy, may have increased long COVID numbers in this patient population.
In pregnant women, the benefits of the COVID vaccine are far more than the small risks from vaccination, Al-Aly said. In a study Al-Aly and his colleagues released this month in The New England Journal of Medicine, researchers found that vaccinations resulted in a 70% reduction in the risk of developing long COVID. "This applies to everyone, including pregnant people who are also at risk of developing the condition," said Al-Aly.
Medical Gaslighting, Complications Common Coble first experienced symptoms of COVID-19 in January of 2020, before tests were available in her area. She said that without a positive COVID test and because of her pregnancy she's experienced medical gaslighting from clinicians who doubted her condition. "Doctors never listen to me and it's dehumanizing," she said.
For pregnant women who do develop long COVID, it comes at a sensitive time and can put undue pressure on moms who are already experiencing an entirely new stage of life, said Obstetrics & Gynecology study author Vanessa Jacoby, MD, professor of obstetrics, gynecology, and reproductive sciences and associate vice chancellor for clinical research at the University of California San Francisco.
In addition, experts say women with COVID-19 have an increased risk for pregnancy complications such as preterm birth and neurodevelopmental disorders compared with women who do not have COVID-19 during pregnancy. And a new study in Scientific Reports found that individuals who developed long COVID during their pregnancy had an increased risk for gestational hypertension, gestational diabetes, and fetal intrauterine growth restriction, a condition that results in the baby not gaining enough weight in utero.
On the whole, most of the treatments for long COVID are used to treat symptoms and it's hard to make generalizations about their safety during pregnancy or breastfeeding. Women seeking treatment for long COVID should make sure that any medication taken for the treatment of symptoms is also safe for their child.
Impact of Long COVID on Children Not only are new parents unduly affected by long COVID, researchers are also looking into what this might mean for their children. Acute COVID can cause preterm birth and long COVID can cause pregnancy complications that may have repercussions down the line. Still, there's a lot that we don't know about child outcomes, and considering how common the condition may be, it's a hole in the research that needs to be filled, said Metz.
Metz and Jacoby are working on a forthcoming study that gathers data on this important and understudied patient cohort. The study, funded by the National Institutes of Health's long COVID RECOVER Initiative, will be enrolling children who were infected with COVID and also the children of women who were infected with COVID during pregnancy. According to the study's preliminary preprint findings, children exposed and unexposed in utero to SARS-CoV-2 maternal infection undergo neurodevelopment screening tests at 12, 18, 24, 36, and 48 months of age.
Experts contend that the impact on offspring is an important piece of the puzzle. We know that you can get long COVID during pregnancy and that it can be devastating to new moms. Now we need to know what this means for their children.
Coble is increasingly concerned about her children and how they will fare down the line. She's often immobile because of her extreme fatigue and can't be with her children. She tears up talking about it.
"I just worry how having a mom who can't play with them will impact them later on. It's just so hard," she said.
#covid#mask up#long covid#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#still coviding#public health#wear a respirator
5 notes
·
View notes
Note
Hey I’m here for sleepover Friday can i ask if its still a mood disorder if its hormonal and also can i enter your house to take a nap?
So mood disorders are a classification within the DSM-5 that include disorder categories like anxiety disorders and depressive disorders. (Note, BPD is not a mood disorder and is actually a personality disorder).
So if you fit a certain amount of criteria for a certain disorder under the mood disorder category, then in theory you have that disorder. A lot of the criteria is based on how much it affects your day-to-day life.
Medical professionals, for the most part, would prefer to give people an “official” diagnosis of these disorders, instead of having a patient look at the DSM-5 and decide whether or not a person fits a disorder. This has it’s flaws, including but not limited to biases like race, gender, sexuality, and culture; a patient not always disclosing all relevant information; medical professionals disagreeing on diagnosis’s; the monetary barrier to get official diagnosis’s and what that could mean if you DO get one.
There is a link to hormonal levels and disorders. That’s why SSRIs are a common prescription for people with anxiety disorders, depression disorders, and more.
When I was doing research into pedophilia, part of my research showed that there was a commonality in patient’s levels of testosterone (can’t remember if it was higher or lower).
There are mood disorders that specifically have to do with estrogen and progesterone levels after a woman gives birth (Postpartum Depression Disorder).
So yes, there is 100% a link between not only hormonal levels and mental illness, but many other physical symptoms and mental illness. Physical and mental health are intrinsically linked, which is why learning about the human body is important when dealing with mental health studies, and is why I’ve taken a number of anatomy, biology, and physiology courses my pursuit of my psychology degree.
Also yes, you are more than welcome to come and take a nap. My home is open to all well-meaning friends, and we have a guest room that’s full of plants right now during the winter, so it’s rather cheery. We have plenty of pets to keep you company and plenty of good food. There are fun activities abound.
9 notes
·
View notes
Text
1 in 10 dads experience postpartum depression, anxiety: How to spot the signs
Subjects surrounding mental health and well-being are being more widely discussed today than ever before. This includes postpartum depression – but not just for women. Studies show that 1 in 10 dads struggle with postpartum depression and anxiety as well. Their symptoms are slowly becoming more recognized, diagnosed, and treated. A mom recently shared the story of her husband’s postpartum depression in The New York Times, and health care providers are encouraging pediatricians to incorporate postpartum depression screenings of fathers as well as mothers during well-child visits. Parents’ mental health greatly affects the well-being of a child. Research has shown that depression in fathers is associated with:
Less attention to baby’s health and well-check visits
Higher risk of behavioral problems in preschool-age children
Children with more physical and mental health problems
Poor family and marital relationships
The stakes are high – fortunately, treatment and support are available when we recognize prenatal and postpartum depression and anxiety in any parent.
Paternal depression can set in before or after birth
As with women, men can experience depression at any time – including before a baby is born.
Women often show symptoms of postpartum depression within four to six weeks after delivery, but signs can appear as late as three months after birth.
A 2019 meta-analysis of studies found that the highest risk of depression during pregnancy for expecting fathers occurred during the first trimester. The study also showed that postpartum depression was highest among men when the baby was 3- to 6-months-old.
A variety of factors can play a role in dad developing prenatal or postpartum depression, including:
Hormones: Research has shown that fathers experience hormonal changes during and after their partner’s pregnancy, particularly declines in testosterone.
Partner’s depression: Up to half of men with depressed partners show signs of depression as well.
Feeling disconnected from mom and baby: Dads want to be part of the newborn experience, but often they feel as if they’re on the “outside.” Moms may not always realize they’re excluding dad from caring for the baby. Or they may be so caught up in bonding with the baby, they fail to recognize dad wants time with the little one, too.
Personal or family history of depression: Any history of depression or other mental illness raises the risk of prenatal or postpartum depression.
Psychological adjustment to parenthood: Becoming a parent requires significant coping skills. This can be overwhelming for moms and dads.
Sleep deprivation: Most new parents underestimate the role a lack of sleep can play in developing symptoms of anxiety and depression. They also often underestimate just how sleep deprived they are!
Other factors that may contribute to paternal postpartum depression include having a colicky or premature baby, financial stress, relationship problems, recent loss or trauma, and lack of social support for parenting, such as not having parental leave at work.
Watch for signs of paternal depression and anxiety
Prenatal and postpartum depression can look different in men than it does in women. Men may experience some “traditional” symptoms – fatigue and changes in sleep or appetite – but they often exhibit fewer outwardly emotional expressions, such as crying.
Common symptoms for paternal prenatal or postpartum depression include:
Anger, sudden outbursts, or violent behavior
Increase in impulsive or risk-taking behavior, including turning to substances such as alcohol or prescription drugs
Irritability
Low motivation
Physical symptoms such as headaches, muscle aches, stomach, or digestion issues
Poor concentration
Suicidal thoughts
Withdrawing from relationships
Working a lot more or a lot less
Anxiety is also common in men during and after pregnancy. A 2021 study showed that 1 in 10 men experience prenatal and postpartum anxiety. In the general population, approximately 14.3 percent of men have anxiety – approximately 9 percent less than women.
Anxiety can cause:
Persistent, excessive worry about life in general
Nervousness or a sense of impending doom
Trouble concentrating
Panic attacks
Symptoms of obsessive-compulsive disorder
If you or a loved one experience prenatal or postpartum anxiety or depression symptoms that intensify or last longer than two weeks, talk with your doctor about possible treatment options.
Future screening for paternal postpartum depression
Most Ob/Gyns check new moms for depression and anxiety symptoms during a postpartum visit. But there is no such check-up for men.
In 2019, the American Academy of Pediatrics recommended that postpartum depression screenings not be solely the responsibility of obstetricians. They urged pediatricians to incorporate maternal postpartum depression screenings and referrals for treatment during well-child visits.
In 2020, an editorial in the Journal of the American Academy of Pediatrics called on pediatricians to assess the mental health of all new parents, regardless of gender, and to make appropriate referrals when necessary.
Don’t be surprised if your partner’s Ob/Gyn or baby’s pediatrician asks about your mental health during a visit. This evaluation could range from engaging in an informal discussion to filling out the Edinburgh Postnatal Depression Scale (EPDS), a simple screening tool consisting of 10 questions. Prioritizing the mental well-being of moms and dads is not only good for them, but for the baby.
https://utswmed.org/medblog/paternal-postpartum-depression/
49 notes
·
View notes