#provide healthcare
Explore tagged Tumblr posts
Text
So funny how Blue Cross basically went "You guys make a great point" and rolled back their anesthesia policy after the United CEO was killed
Seems like we might have found a form of protest that works
#not art#politics#united ceo#united healthcare#united states#leftism#fuck ceos#kill ceos#kill your insurance provider!!!#deny defend depose
11K notes
·
View notes
Text
Support people impacted by the violence in Haiti!

The allocation from the UN’s Central Emergency Response Fund (CERF) will go towards providing food, water, protection, healthcare, sanitation and hygiene support to displaced people and host communities in the capital and in the neighbouring Artibonite province. A $12 million contribution from a United Nations emergency humanitarian fund will support people impacted by the violence that broke out in Haiti’s capital, Port-au-Prince, in March.
Learn more about the fund of $12 million for Haiti.
#unocha#humanitarian aid#haiti#cerf#provide food#provide water#provide protection#provide healthcare#provide sanitation & hygiene#relief workers#emergency relief coordinator#host communities
0 notes
Text
I really try not to be a conspiracy theorist but I’m seriously flip flopping on whether or not I believe Luigi Mangione actually did it, on one hand this guy’s digital footprint is too vast to not be a real person with real motive, but on the other hand the circumstances of how they caught him are so odd that it just doesn’t add up, like, he wore very nondescript clothing and a mask the day of the shooting, suggesting he doesn’t want to be identified, despite this they were somehow able to identify him at a hostel in different clothing without a mask, he not only fled the scene but allegedly fled New York with a fake ID that the police recovered, several days later they found him in Pennsylvania carrying around all of the evidence in his backpack, including a manifesto, gun, and fake ID, the police also claim he had somewhere between $8,000-$12,000 in his bag, yet when asked about it Luigi claims he had no idea where the money came from and suggests it was planted (which raises several more alarm bells because if this “evidence” was planted then what else could they have fabricated to “catch” this guy?)
this not mentioning the fact that I find it really odd that this guy didn’t digitally publish his manifesto and instead chose to carry a physical copy of it around for days
this all could mean that he wanted to get caught but if that’s the case why go to Pennsylvania at all? why not just stay in New York?
I will say, though, that I think some of this can also be explained by this comment on Reddit:

regardless, the circumstances are suspicious as hell
edit: I realized I forgot to mention this part but it’s also so suspicious how everyone, the police, the media, whatever, are all 100% certain that Luigi Mangione did it, I’ve seen so many high profile cases where cops do press conferences and say “this is America, the suspect is innocent until proven guilty!” yet they’re not even calling Luigi a suspect, they’re outright saying he is the shooter and that he did do it, that’s just weird to me
#fae.txt#luigi mangione#united healthcare#long post#hope this makes sense#no sources because I’m lazy but if you’d like them I’d be happy to provide
5K notes
·
View notes
Text
I went to the emergency room the other day to get an MRI after I tripped over my own feet and fell face-first three feet down into a window well. Crazy that didn’t kill me. Anyway, I’m in the ER getting an IV put in by this nurse, and he’s joking with me, I’m joking back, it’s lighthearted, fine time, etc. I go back to the waiting room, then about 20 mins later, I get called back to the same booth where I got my IV so I can get some Ativan prior to the MRI.
(Even they were explaining I was gonna get an MRI, they were like “are you claustrophobic?” And I was like “in some circumstances yes, and in others no. Let’s not roll the dice on which circumstance an MRI would fall under. It went fine, no worries, definitely could have gone without the Ativan, but I can get why going headfirst into the screaming tube that thumps like a dryer with a shoe inside could stress some people out.)
Anyway, I’m back there, and the same nurse comes over, confused to see me, and goes, “huh did I forget something?”
And me, thinking he’s joking around again and knows that I’m here to get a medication, go “haha I guess there’s something else you gotta stick in me.”
Then he didnt say anything, and I played back what I said, just as another nurse came over and told him, “oh she’s here to get the Ativan,” so he gave me Ativan, and I smiled and thanked him, and the second he left, I grabbed Katie’s arm and hissed in complete mortification, “I guess there’s something else you gotta stick in me????” And she was like, yeah. You did a very bad job talking.
Anyway at least medically my brain is fine
#b.#nursing tag#just not me as the nurse#Christ I hate telling my healthcare providers I’m a nurse#i actually don’t want to feel like I’m discussing my health with colleagues#when it’s my own health I don’t want ppl being like ‘you’re deficient in X and obviously you know what that means’#if I was good at critically thinking about my health the way I think about patient health I would be healthier
474 notes
·
View notes
Text
Yesterday was my first time in the ER since my hEDS diagnosis was officially added to my file (instead of me having to tell them and hoping they’d believe me), and everyone in my emergency care team was on top of it. Like on the ball, fully engaged and interested in keeping the zebra in the hospital comfortable.
They also all knew what MCAS and POTS were and deferred to me when it came to medication and pain management. Which was also wild, because they were not shy at all about offering pain relief. They straight up offered me narcotics, when usually the most I get offered is Tylenol.
Even the CT tech knew what MCAS was and asked if we should pre-treat with Benadryl because he knew some patients could experience mast cell destabilization from the radiation even without the contrast dye.
He and the nurse even helped brace my neck when I was going into the CT machine because I mentioned having cranial instability, and the position I was in was making my neck click, so they stopped everything to find multiple pillows to brace my neck and shoulders while I was on the table.
Afterward, while being bussed through the corridors in my bed (because they had to dehydrate me to take the CT scan and my POTS was going haywire, and they made sure I had to be upright as little as possible), I commented to my nurse that I was startled that everyone I’d spoken to that day knew about EDS/MCAS/POTS and were so accommodating.
He paused before answering, then told me, “We probably don’t know as much about EDS as we should, but we’ve seen a lot of the other two over the last few years. Covid really messed people up. Did yours start with covid?” No, I told him. We think I was probably born with it and a dental infection turned it lethal. He expressed his sympathy and again reminded me I didn’t need to be a hero and I could press the pain med button whenever I needed to.
Back in my room, they started me on IV fluids to combat the dehydration from the POTS. And I was laying there, I became aware of the nurse bracing my elbow so it wouldn’t hyperextend while he futzed around with the IV and I remember thinking, “this is how it always should have been.”
The kindness and care shown to me were in such stark contrast to past experiences it made me quite tearful. There were no accusations of anxiety, no referrals to psyche, and no implications that I was over-exaggerating my pain. No denying of my experiences.
Just a quiet, vocal acceptance that I “knew my body best” and that they’d do whatever they could to help.
It was nice.
#chronic health tag#posting for bad days when I need to remember there are good healthcare providers#long post#medical trauma
4K notes
·
View notes
Text
there is a special place in hell for cat owners who allow their cats to free-roam a residential neighborhood because it's ~natural~.
The amount of devastation and heartbreak I have seen from loved ones whose cats accidentally got out makes me like twice as mad too because I cannot. I cannot fathom the cruelty and selfishness required to ignore what we know to be best practice for cat husbandry because your feefees get uncomfies when people tell you it's animal abuse to wilfully, knowingly cut your cat's expected lifespan from 15-20 years to 2-3.
KEEP. YOUR. FUCKING. CATS. INSIDE.
#this does not apply to people who are doing their best to care for feral colonies while providing TNR and other essential healthcare#it also does not apply to people who are trying to keep their cats indoors#it's the people who have four or five outdoor cats and an ostentatious tesla and a ~wild pollinator~ sign in their garden#guess what sweetie fluffy does more damage to wild pollinators than twenty grass lawns#the performative environmentalism paired with blasé attitudes towards the welfare of animals in their care makes me fucking seethe
326 notes
·
View notes
Text
FBI say they're closing in on him....but why offer up more money if that's the case?
Also they found monopoly money in a bag they believe to be his lmfao
*EDIT*
OMG UHC WAS BEING INVESTIGATED BY THE DOJ FOR INSIDER TRADING AND MONOPOLIZING
#united healthcare#someone said that the CEO is getting more coverage than UHC provided#claims adjuster
99 notes
·
View notes
Text

#going w/o ur meds thru no fault of ur own is ungood#when it happens every month its double plus ungood#bad healthcare provider bad insurance bad pharmacy#shame on u all
845 notes
·
View notes
Text
"depose," "deny," and "defend" being scratched on the shell casings is likely a play on what's known as the "3 D's of Health Insurance," which are "delay, deny, defend:" all slimy tactics that insurance companies deploy to increase profit margins
#brian thompson#united healthcare#qi.txt#uhc is my insurance provider my premium better not go up next year
111 notes
·
View notes
Text

To all of the lovelies that are concerned about having access to contraceptives in the USA, please know that Plan B has a shelf life of a few years when stored properly (Plan B Fact Sheet, 2024). The same can be said for Julie Plan B.
These are not abortion pills. These morning-after pills delay the ovulation process, which means the menstrual cycle starts quicker and prevents the fertilization of the egg. Take when needed and store safely. All of these can be bought online and/or Target and CVS.
#contraceptives#And call with your healthcare provider to see what works best for you#women’s health#I’m being mom/auntie/foxy grandma today
90 notes
·
View notes
Text


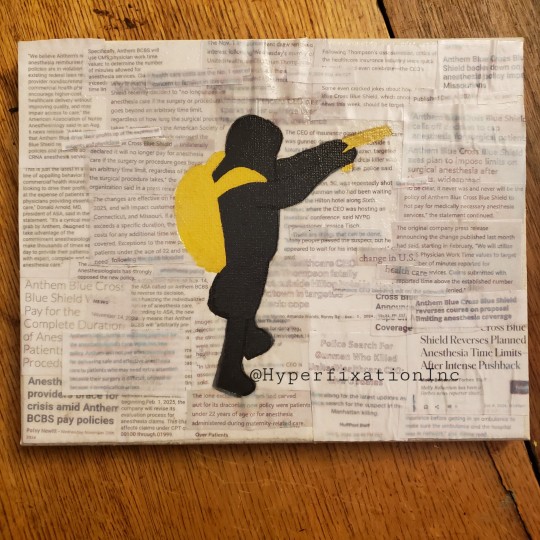
DENY, DEFEND, DEPOSE
-
Instagram
Bluesky
Tiktok
Redbubble
Tips
-
December 2024
#deny defend depose#art#artists on tumblr#artwork#2024#traditional art#digital art#acrylic#acryloncanvas#acrylart#acrylic on canvas#acrylpainting#collage#united ceo#united healthcare#kill your insurance provider!!!#blue cross blue shield#the adjuster
49 notes
·
View notes
Text
As someone who works with health insurance daily as part of my job, going after the CEO of UHC was great, I literally came back from lunch & said to my coworkers “you’ll never believe what just happened”.
But also we can aim higher. UHC is small potatoes. You know who has their hands in everything? UHG. The parent company. UHC, Optum, Humana, EXL health, hell they even have a hand in a decent portion of Anthem plans PLUS control a large portion of the Community Care Network for the Veterans’s Administration.
You know what else they control? BILLING. FOR MEDICAL PROVIDERS. More providers than you’d ever want to think use Optum as their billing company! So not only do they likely have their hands in your health insurance, they are also the company BILLING your insurance. Hello, incorrect CPT & DX codes that get denied!
Change Healthcare? A massive medical billing agency. Services a lot of EMS providers. It’s Optum owned. They got hacked at the beginning of this year. There are medical providers who still cannot bill insurance for their services at least 8 months later because they have no access to the system. So they send a bill to the patient hoping to recoup something because they can’t generate the ‘official’ bills insurance needs. (If you want my rant about false medical bills you’ll have to ask cause that’s a different conversation.)
Guess who else had a major hack this year? United Healthcare. I didn’t mention it earlier but they’re also AARP! So the company that has a strong hold on retired veterans, retired citizens, and people who are disabled/on SSDI basically had 2 major data breaches this year. Your health insurance has all of your info; age, date of birth, SSN, address, job, pretty much everything.
Optum also used to have its hands in Harvard Pilgrim Health Care, although I believe HPHC split from them either last year or this year. It was recent.
It’s insane. Almost the entire healthcare system relies on United Healthcare Group (not UHC, but close enough). I say burn it to the ground.
#sorry I’m ranting#health insurance makes me crazy#United healthcare#Optum#fuck them all honestly#I mean humana once tried to stonewall a settled for $1.41#literally#that’s it#$1.41#I love my job but seeing how bullshit healthcare is has been both a blessing and a curse#my partner & I are looking at houses right now#after seven years!#and we’ll find a place we like that’s near perfect & I’ll be like#oh no it’s [this medical provider] I don’t want to live in a spot where they’re my only choice
40 notes
·
View notes
Text

hate hate hate hate
#why is amazon providing health care#we got company town shit happening#but it's the entire fucking country#healthcare#amazon#hate#doom 2024#merica#capitalism
231 notes
·
View notes
Text
every service crucial to the functioning of society, namely government, healthcare, banking, etc, needs to at all times consider that people who are very stupid need to be able to navigate and use these services with minimal struggle, and people who don't have easy access to the internet or a smartphone also need to be able to navigate and use these services with minimal struggle. unfortunately many of the people who design these systems and services are in possession of a higher education a smartphone with consistent high speed internet connection and a critical lack of awareness about how universal these experiences are
#anyway i love cuchulainn#got a questionnaire from a healthcare provider asking about their digital services that did not consider it might suck
135 notes
·
View notes
Text
This is an announcement and a promise: if you are a bad nurse, I am coming for you. If you are rude and judgemental to patients, deny them basic human decency you will face my wrath. If you take shit care of them, think you know better than not only the patients and your coworkers but the whole medical team then you cannot hide from me. I will find you and I will go toe to toe with you bc even the worst human alive deserves care and respect and I will beat that lesson into you and maybe make you grow a heart.
#adventures in nursing#to be deleted#personal#Im raging yall#absolute shit night shift with a shit nurse who did unsafe Callous care to a patient#she purposefully neglected him and I didnt realize til several hours in#US healthcare is inherently predatory and threatens our most vulnerable#it is our job as nurses to provide the best care to Everyone and to do our best to get them better#And I mean e v e r y o n e: the complex the homeless the assholes the ones with no money family connections#we take an oath to treat everyone with kindness respect and dignity#if you're a dick yeah I may complain about you to the other nurses to cope but I will still do everything to help you#I'm enraged I've let my manager know and absolutely screamed at another nurse who blessedly let me call her at 8am on her day off#i want her the fuck off my unit and i dont want her involved in healthcare anywhere but I cant help that#I did my best to care for the patient she abandoned but i will take ownership for not intervening sooner#and I will carry this rage in my heart and do my best to once again foster an enviornment of spiteful love on my unit#we love when it is hard when it is unwanted when it is neccesary bc it is my job to care when no one else does#god idk how much longer I can do this Im so burned out
47 notes
·
View notes