#open submission publishers
Explore tagged Tumblr posts
Text
DAMN WHAT THE HELL BARIQHRIQRHAUSHASHW !?!?!?!!?!?!!!!!!!!!!!!
#oh my god. anyways fun thing about college there are so many new ways that it can compliment you?????#anyways got the grade for my english paper back which like 💪💪💪💪 yeah i got the A. 😎😎😎 honestly i didnt i would have been pissed bc#that shit WAS brilliant actually but THEN my professor was like in the comments hey if you wanted you could edit this and submit it to this#fuckin. peer reviewed journal and shit like i thought it was really good“ like SIR?!?!?!?!?!? SIR!?!?!?!?!?!#its an undergrad one obviously but this is insane to me wth#he said submission closes next week but the site says thats when its opening so ill probably wait and#decide over break after talking to my parents#but thats absolutely wild#also the complements thing is crazy#like in hs its me: does smth smart someone: oh thats so smart#but then in COLLEGE i do smth smart and people start asking me to TA and submit to academic publications ahfiahdhahs#wild. anyways i need to turn in this other paper now which is what i was SUPPOSED TO BE DOING before i checked my email. anyways thats wild#i may honestly submit if i can becaused seeing if i could get published would be SICK#and would look fucking awesome on my resume. also bragging rights and the ego boost bc lets be real#esp at 18 thats wild teehee. anyways need to do real work not theoretical work atm so yeah ✌️ bye#blah
4 notes
·
View notes
Text

Submissions are officially open!
Crips for eSims for Gaza and Connecting Humanity have already done so much work bringing Internet access to the people of Gaza, but the need for funding is constant. So we are very proud to announce the submission phase of our upcoming eSim bundle on Itch.io!
Do you have a game, zine, or hell, anything else published on Itch? We would love to have you for our cause!
Submissions will be open from January 27 to February 10th!

#itch bundle#esims for gaza#video games#game development#posting this maybe half an hour early since im on break at work
2K notes
·
View notes
Text
StokerCon Highlights, Authortunity Angels, and Monstrous Books
Watch. Succeed. Repeat.
Welcome to Authortunities Forecast, my new show which covers publishing industry news and highlights some of the most noteworthy items from my Authortunities weekly calendar mail out. Follow the link to get a head start on open submission calls, grants, contests, fellowships, high value opportunities and paying markets+ weekly in your inbox.…

View On WordPress
#alien horror#artificial intelligence in publishing#Authortunities Forecast#Bram Stoker Awards#career in writing#classic horror films#Contests#diversity grants#fellowships#grants#horror#Horror Writers Association#Horror Writers Association Scholarships#HWA Trustee#MONSTROUS BOOKS#open submission calls#Publishing industry#pulp#Reedsy#SFPA#short fiction#speculative poetry#speculative prose#StokerCon#Substack#young writers
0 notes
Text
poetry outlets that support a free palestine
after finding out that the poetry foundation/POETRY magazine pulled a piece that discussed anti-zionism because they "don't want to pick a side" during the current genocide, i decided to put together a list of online outlets who are explicitly in solidarity with palestine where you can read (english-language) poetry, including, except where otherwise stated, by palestinian poets!
my criteria for this is not simply that they have published palestinian poets or pro-palestine statements in the past; i only chose outlets that, since october 7, 2023, have done one of the following:
published a solidarity statement against israeli occupation & genocide
signed onto the open letter for writers against the war on gaza and/or the open letter boycotting the poetry foundation
published content that is explicitly pro-palestine or anti-zionist, including poetry that explicitly deals with israeli occupation & genocide
shared posts that are pro-palestine on their social media accounts
fyi this is undoubtedly a very small sample. also some of these sites primarily feature nonfiction or short stories, but they do all publish poetry.
outlets that focus entirely on palestinian or SWANA (southwest asia and north africa) literature
we are not numbers, a palestinian youth-led project to write about palestinian lives
arab lit, a magazine for arabic literature in translation that is run by a crowd-funded collective
sumuo, an arab magazine, platform, and community (they appear to have a forthcoming palestine special print issue edited by leena aboutaleb and zaina alsous)
mizna, a platform for contemporary SWANA (southwest asian & north africa) lit, film, and art
the markaz review, a literary arts publication and cultural institution that curates content and programs on the greater middle east and communities in diaspora
online magazines who have published special issues of all palestinian writers (and all of them publish palestinian poets in their regular issues too)
fiyah literary magazine in december 2021, edited by nadia shammas and summer farah (if you have $6 usd to spare, proceeds from the e-book go to medical aid for palestinians)
strange horizons in march 2021, edited by rasha abdulhadi
the baffler in june 2021, curated by poet/translators fady joudah & lena khalaf tuffaha
the markaz review has two palestine-specific issues, on gaza and on palestinians in israel, currently free to download
literary hub featured palestinian poets in 2018 for the anniversary of the 1948 nakba
adi magazine, who have shifted their current (october 2023) issue to be all palestinian writers
outlets that generally seem to be pro-palestine/publish pro-palestine pieces and palestinian poetry
protean magazine (here's their solidarity statement)
poetry online (offering no-fee submissions to palestinian writers)
sundog lit (offering no-fee submissions to palestinian writers through december 1, 2023)
guernica magazine (here's a twitter thread of palestinian poetry they've published) guernica ended up publishing a zionist piece so fuck them too
split this rock (here's their solidarity statement)
the margins by the asian-american writers' workshop
the offing magazine
rusted radishes
voicemail poems
jewish currents
the drift magazine
asymptote
the poetry project
ctrl + v journal
the funambulist magazine
n+1 magazine (signed onto the open letter and they have many pro-palestine articles, but i'm not sure if they have published palestinian poets specifically)
hammer & hope (signed onto the letter but they are a new magazine only on their second issue and don't appear to have published any palestinian poets yet)
if you know others, please add them on!
4K notes
·
View notes
Text
For the purposes of this poll, a book lover is anyone who would describe themselves that way. The "I don't love books" options don't necessarily mean you hate books, just that you wouldn't describe yourself as a book lover.
Anon saw a furor over someone saying most of traditional publishing catalogs these days is bad, and most respondents assumed that the person saying so must not like books very much. However, as a book lover themself, anon agrees that most books these days are bad! They're curious how these opinions vary.
–
We ask your questions anonymously so you don’t have to! Submissions are open on the 1st and 15th of the month.
#polls#incognito polls#anonymous#tumblr polls#tumblr users#questions#polls about interests#submitted feb 1#books#reading#hobbies#interests#fiction#media
331 notes
·
View notes
Text
Could This Be? (Sae Itoshi x fem!reader)
angst, fluff, slow burn, Sae Itoshi, language, smut (heavy?) fem!reader, trigger warning, hopeless/over thinker reader..?, BTW THIS IS GONNA BE A LONGGG ONE.
Yeah there's fingering, orgasms, dominate Sae, big-cocked Sae, somewhat submissive reader?, dirty talk (somewhat?), y’know all the usual.
a/n: give me ideas for who and what to write about next please🙏 cuz I got nothing.
Also, sorry if I made any mistakes on here as I have had not checked for any spelling mistakes or anything. I rushed to try and get this published because well…yeah it’s been a while.
____
(no song for this sorry😢)
Love.
It’s something everyone craves. The warmth of comfort, the security of knowing someone is truly there for you. It’s that feeling of having someone by your side, someone you can open up to without fear of judgment. It’s knowing there’s a shoulder you can lean on when life feels heavy.
Who wouldn’t want that? Everyone longs for that one person who understands them deeply, who stands by them through everything. It’s a natural part of being human.
Yet, finding true love isn’t always easy. Lustful desires can cloud our vision, making it hard to distinguish between the fleeting thrill of lust and the enduring presence of love.
Lust satisfies only for a moment, but love—love endures.
Too often, people mistake lust for love, deceiving themselves into thinking the temporary excitement is something lasting. But in truth, love is far deeper, something that grows and remains, far beyond the surface.
They convince themselves that this so-called "love" they’re experiencing is genuine, when, in truth, it’s anything but.
Then, there are those who have never been loved properly at all. As humans, we often twist the meaning of "love," reshaping it into something that barely resembles true love.
It’s disgusting, really.
The world is far from perfect, and it’s filled with deceivers and liars who spread only flames of falsehood and venom. It’s painful to think that someone like you has crossed paths with these people.
Many have tried to explain what "love" is supposed to be—pleasure, satisfaction, joy, delight, even lust. They use these words to describe love, and it’s horrifying to see how they’ve mistaken and misrepresented it.
What they experienced wasn’t real love at all. Just a shallow, distorted version of something far deeper and truer.
It’s pitiful. The "love" they’ve experienced is etched so deeply into their minds that they believe it’s real. But it isn’t.
Love is so much more. It takes many shapes, each unique to the person, and it goes far beyond fleeting pleasure or satisfaction. Some have been led to believe otherwise, brainwashed into confusing love with something shallow and empty.
They’ve never truly experienced love.
And yet, you, too, fall into this category. You’ve never been loved as you deserved.
These days, it seems like all men want is sex and pleasure. Many of the men you’ve dated claimed to “love” you, but those words quickly unraveled into hollow promises. What they felt was just a lustful attraction, nothing more.
Your heart has been broken more than once by these pretenders, each time leaving you with more questions than answers.
One day, they’d say they loved you; the next, they’d avoid you entirely. And to think, you even lost your virginity to one of these fucking scums.
They left you shattered, vanishing the moment they got what they wanted.
One guy, in particular, slipped past your defenses, convincing you he was different—that he was actually worthy of this "love." He manipulated you in countless ways, claiming it was all in the name of love. He told you that having sex, intimacy, and leaving yourself vulnerable, was the ultimate proof of love.
You were conflicted, torn by doubt, but a deep need to be loved pushed you to trust him. Yet, the days that followed left you miserable and broken, as he cut off all contact after that night.
All you wanted was to be was loved…
One by one, each guy took what he wanted and left, only adding to the ache and emptiness.
You stopped believing in love and began to hate yourself in ways you never had before.
Was love even real? Was it just a fantasy made for movies and stories, something exaggerated beyond reality? No one could convince you otherwise. All those voices claiming to know what love is, how it’s supposed to feel—they seemed almost delusional to you now.
You found yourself pitying them, those blind and hopeless creatures, chasing an illusion you no longer believed in.
What a bunch of animals.
…🌺…
You worked at a small bakery not far from home. Despite everything going on, you couldn’t afford to be broke. Thankfully, this job gave you just enough to scrape by each week. Barely.
You took the night shifts for the extra pay—just in case. A car was out of the question on your income, but that didn’t matter much; work was only a short walk away.
What they didn’t pay you enough for, though, were the rude, bitchy, demanding customers who tested your patience daily. They complained, ordered you around, and acted as if you were their work-slave, to solely serve their every whim. You were surprised you hadn’t lost your mind by now—probably thanks to your coworker or best friend might I say.
“Heyyy, Y/nnie! How’s my favorite girl?” she called out, wrapping you up in a tight hug.
Her name was Yuko. Annoying and overly extroverted as she could be, though you were grateful to have her around.
Her dark, disheveled hair, bounced as she ran toward you. “Hey, Yuko…” you managed, barely able to breathe under her tight hug. Despite her size, she was surprisingly strong.
Yuko’s eyes widened as she realized she was squeezing the air out of you, and she quickly let go. “Ha… sorry, Y/n!” she muttered, rubbing the back of her neck in embarrassment.
“Nah, you’re fine, Yuko,” you said, smiling as you met her gaze.
Your first shift here had been lonely. You hadn’t bothered much with the other coworkers, and they hadn’t really reached out to you either. You’d all just been there to do the job—nothing more.
You hadn’t really minded keeping to yourself, never making an effort to connect with your coworkers. They hadn’t shown much interest in you, either.
Then came Yuko.
She approached you, eager to get to know you better—though, to be fair, she did that with everyone. She was friends with nearly all your coworkers, and now she’d set her sights on making you her next.
You couldn’t deny that her bold personality drew you in. Something about her was captivating, though you couldn’t quite put your finger on it. Was it her loudness? Her confidence? Her outgoing spirit? Whatever it was, you felt yourself drawn to her.
And Yuko felt the same. She sensed there was something different about you, something intriguing, and that made her all the more determined to befriend you.
Who would have guessed that this mutual interest would spark such a strong friendship between the two of you?
You weren’t just another coworker to her—Yuko considered you her best friend. And, honestly, you felt the same way about her.
“I just couldn’t resist squeezing the life out of you, Y/n! You’re just so precious and adorable!” Yuko gushed, clasping her hands together with a loud smack.
“Yuko… you use that excuse every single day,” you sighed, shaking your head.
“Do I? Mmm, I don’t recall…” Yuko hummed, feigning innocence with a coy smile.
You let out a small huff, clearly seeing through her act. With a playful glare, you waited, knowing she’d slip up soon enough.
Sure enough, not even ten seconds passed before she let out a whine, squirming a little under your gaze. “Ah, Y/nnnnieee… how do you always figure me out?” she grumbled.
“You’re just that bad at lying, Yuko.” You chuckled softly, watching as she crossed her arms, giving you a mock-offended glare.
“I am not that bad at lying!” she retorted, pouting.
Lost in your banter, neither of you noticed the soft jingle of the bell signaling someone’s entrance.
“Sure, Yuko, whatever helps you sleep at night—”
“Are you going to take my order, or are you two just going to keep bickering?”
Both of you froze, turning toward the voice with wide eyes.
"Ah… my apologies, sir. Sorry for not paying attention," you muttered quickly, stepping over to the register to take his order.
The man let out a faint hum, as if to agree that yes, it was your fault. Inwardly, you stifled a groan—you could already tell he was going to be one of those bitchy customers.
"Anyway, what can I get for you, sir?" you asked, glancing up.
Your gaze lingered, almost unconsciously taking in his appearance, a habit you’d developed with customers. He had reddish-brown hair and a lean build, at least from what you could see. His eyes, a striking green-teal, were narrowed slightly, showing not a hint of emotion.
You almost paused, a bit envious of his long, dark lashes. What a lucky guy, you thought.
Overall, he gave off an air of indifference, like nothing around him could bother him in the slightest.
“A salted kombucha tea will do,” he replied, barely looking up from his phone.
“Anything else?” you asked, glancing up at him again.
He slipped his phone back into his pocket, meeting your gaze with an intensity that made it feel as if he was sizing you up, too.
“That’s all,” he said, hands shoved casually into his pockets.
You quickly typed in his order, breaking eye contact, though you could still feel the weight of his stare. It was… unsettling.
“And your name?” you asked, grabbing an empty cup, trying to brush off the strange tension.
“Sae Itoshi,” he muttered.
Sae Itoshi? The name struck a chord, tickling the back of your memory. You’d heard it somewhere before, but couldn’t quite place where.
“Alright, your drink will be ready shortly. If you could, please wait over there,” you said, gesturing toward the spot.
Sae’s gaze followed your hand, and without a word, he walked to the designated area.
With the empty cup in hand, you stepped away from the register and started preparing his drink. Just as you began brewing the tea, Yuko appeared at your side, looking as energetic as ever.
“Did I hear that right? That was Sae Itoshi?!” she practically shouted, wide-eyed as she leaned right into your face.
Already feeling the beginnings of a headache, you nudged her back. “Yeah, why are you so surprised?” you asked, raising an eyebrow.
Yuko looked at you like you’d just sprouted a second head.
“Are you serious, Y/n?” She scoffed, gripping your shoulders in exaggerated disbelief. “You call me clueless, but you don’t even know who Sae Itoshi is?”
“That, my dear Y/n, was none other than the Sae Itoshi—the famous football player!” Yuko exclaimed, rocking you back and forth.
No wonder the name had sounded so familiar. What were the odds that a famous soccer player would show up at a small bakery like yours?
“Okay, okay, you can let me go, Yuko!” you yelped, clutching the cup tightly to avoid spilling the drink.
Reluctantly, she released you but continued her excited rambling. “Do you realize how rare this is?” she squealed, practically sparkling with enthusiasm.
“Yeah, I guess it’s pretty rare,” you mumbled as you got back to preparing the drink, hoping she’d settle down.
But Yuko just stared at you, her expression twisting with utter disbelief. What’s with everyone staring today?
“The hell, Y/n? How are you not excited about this?! A famous athlete is literally in our shop right now! Out of everywhere, he chose here!” she ranted, poking the side of your head for emphasis.
You swatted her hand away. “Keep your voice down, Yuko,” you sighed, trying to focus.
But Yuko, unfazed, only leaned in closer. “And not only is he famous, he’s one of those hot athletes!” she gushed, ignoring your attempt to quiet her. “How can you stay calm when we’re literally in the presence of a sexy celebrity?”
You groaned, turning to face her. “Yuko, please. Let me finish this, okay? I really don’t need the noise right now.”
She huffed, dropping her shoulders dramatically. “Fine, whatever, Y/n. You’re so weird,” she muttered, leaning against the counter beside you.
A brief silence fell—until Yuko finally spoke up again. “So… how big do you think his dic—“
“Yuko!” you blurted, stopping her before she could finish.
“What? I’m just curious! Can’t you let a girl imagine these things?” she pouted, crossing her arms with a mischievous glint in her eyes. She knew you were already done with her antics.
“At least keep those thoughts to yourself, Yuko. And you call me weird,” you scoffed softly, snapping the lid onto the drink.
Yuko chuckled, clearly pleased with herself for getting under your skin. She lived for teasing you.
You took a steadying breath, picked up the tea, and headed over to Sae Itoshi, feeling a touch nervous to be serving someone so famous.
“Here’s your tea, sir,” you mumbled, holding the cup out to him.
He glanced up from his phone, his eyes settling on you as he reached for the drink. His fingers brushed against yours, warm and slightly rough, sending a surprising jolt through you. Shaking off the thought, you added, “That’ll be 595.31 yen.”
“Right.” He gave a soft hum and pulled out the exact amount, placing the yen in your hand before taking a sip.
You noticed his eyes widen just a fraction as he savored the tea, clearly caught off guard by the taste.
“This is surprisingly good for such a cheap drink,” he muttered, taking another sip.
You let out an irritated huff. Did he really have to say it like that?
“Glad it suits your taste buds,” you grumbled, resisting the urge to roll your eyes.
He ignored your tone. “Did you make this yourself?” he asked, studying you with unexpected interest.
Caught off guard by the question, you raised an eyebrow. “Yeah, I did. Why?”
His gaze held yours as he replied, “No reason. I just didn’t expect it to turn out this well.”
Another rude remark. Will you ever get a break from these customers?
He took another sip, looking mildly impressed. “I might reconsider coming by again for another cup. You make good tea—for a baker.”
You were sure steam was coming out of your ears by now. You just wanted him out of the shop. “Thanks, I guess,” you muttered, barely concealing your frustration.
“No problem,” he said nonchalantly, strolling out the door without a second glance.
You let out an aggravated sigh. The nerve of that guy.
Slumping your shoulders, you turned and headed back to where Yuko was waiting. The moment she spotted you, she practically skipped over.
“Sooo, Y/n, what’d you think? Pretty sexy, huh?” she laughed, leaning against your shoulder.
“Sure, I’ll admit he’s good-looking,” you muttered, rolling your eyes. “But he’s an absolute jerk. Seriously, how do people put up with him?” You groaned, burying your face in your hands.
“Woah, woah, Y/nnie, what exactly happened?” Yuko asked, pulling back to look at you.
You sighed, pulling your hands away from your face. “He practically insulted me—multiple times. And I don’t even think he realized it.”
Yuko studied your face as you ranted, wide-eyed. Clearly, you were more annoyed than usual.
“Well, look on the bright side, Y/n—he probably won’t come back! …Sadly,” she added, mumbling the last part.
“About that…” you muttered, avoiding her gaze.
Yuko’s mouth dropped open, and she grabbed your face, forcing you to look at her. “You’re telling me he’s coming back?! Oh my gosh, oh my gosh, oh my gosh—!”
“Yuko!” you exclaimed as she released her grip, realizing she’d been squeezing your face a little too hard.
“Sorry, Y/n,” she chuckled sheepishly, taking a step back. “But seriously—is he really coming back?” Her eyes were wide, fixed on you like a hawk.
“Well… yeah, he said he might, but I don’t know if he actually meant it,” you murmured, recalling Sae’s words.
Yuko let out an exaggerated groan, tugging at her hair. “Aww, come on, Y/n! Way to get my hopes up!”
“Sorry, Yuko,” you sighed. Not that you were actually sorry.
“Doesn’t mean he won’t, though! Ooh, maybe I can get his number too! I can already picture our future together—wonder how he looks naked in bed—”
“Yuko!” you shouted, interrupting her with a mix of surprise and annoyance.
“Just messing with you, Y/n!” Yuko cackled, wrapping you in a tight hug.
You couldn’t stand how easily she joked about such… lustful things, though you’d never admit it to her. It always made you uncomfortable.
“Aww, I love you, Y/n!” Yuko said dramatically, burying her head in your neck.
That, too, made your stomach turn. You hated it.
Why did everyone toss around the word "love" so casually, like it was just a meaningless phrase? You couldn’t wrap your head around it.
…🌺…
The soft, familiar comfort of your bed enveloped you as you collapsed onto the mattress. A sigh escaped your lips as you began to settle in for the night. It was already 12:05 AM, meaning your shift would start in just six hours.
You let out another sigh, staring at the ceiling, letting your thoughts wander.
Then, out of nowhere, Sae Itoshi’s face flashed in your mind.
Without thinking, you grabbed your phone and searched for his Instagram profile.
What the hell are you even doing?
You scrolled through his posts, which were mostly just photos of him scoring goals, looking effortlessly cool. What is wrong with you?
Your finger hovered over the screen as you clicked on his followers and the people he followed. It was a list of other famous football players, each name more recognizable than the last.
Are you out of your mind?
You navigated through all the social media apps, searching for his name, scrolling aimlessly.
Stop.
You froze, suddenly aware of what you were doing.
“What the hell am I doing?” you whispered to yourself, a wave of realization washing over you.
Why were you so fixated on finding Sae Itoshi online? Was he really that intriguing? Was he worth all this time and energy?
What exactly was so captivating about him?
You had no answers.
With a frustrated sigh, you closed out of every app that featured his name and set your phone down beside your bed. You plugged it in to charge, then wrapped yourself tightly in your blanket.
But despite the warmth, sleep eluded you. Instead, you lay wide-eyed, staring at the ceiling.
What made you do this? Why was Sae Itoshi still on your mind?
Why were you suddenly so desperate to know who he was?
You let out a weary groan, squeezing your eyes shut, hoping sleep would finally drown out the endless questions swirling in your mind.
And after what felt like an eternity, it finally worked. Your thoughts began to fade, and sleep claimed you.
…🌺…
“Well then, Y/nnie, who’s excited to see Sae Itoshi?! I know I am!” Yuko exclaimed, practically bouncing with energy.
“Sometimes you’re too much, Yuko,” you replied, rolling your eyes.
As expected, Yuko was absolutely ecstatic about the prospect of seeing Sae Itoshi again. But could you say the same? You weren’t so sure.
“Come on, Y/n! This is a once-in-a-lifetime opportunity! You’ve got to make the most of it!” Yuko urged, clasping her hands around yours with a grin.
“Well, I’d like to make use of my lifetime not obsessing over some famous football player,” you sighed, trying to sound indifferent.
What a lie.
“Gosh, you’re so boring, Y/n!” Yuko huffed, releasing her grip on you. “You’re hopeless,” she added with a teasing tone.
You scoffed. “Me, hopeless? I’m just trying to make enough money to survive out here,” you grumbled.
“Aren’t we all?” Yuko replied, taking a step away from you and heading off to serve other customers.
You sighed, watching her go, then rested your elbows on the counter in the back. Your phone came out of your pocket, and you began scrolling through social media absentmindedly.
Then, once again, that all-too-familiar thought of him crept into your mind.
What is happening to you?
You found yourself on his Instagram page, scrolling through his posts without even realizing it.
Just then, you heard a voice—one you knew all too well.
“You must have a really hard time noticing your customers waiting.”
Your eyes widened in shock. You quickly whipped your head up, and there he was—that stupid jerk—standing right at the register, waiting for you to take his order.
Sae Itoshi…
You quickly turned off your phone, hoping he hadn’t caught you scrolling through his profile just moments before.
Taking a deep breath, you walked up to the register, forcing a neutral expression.
“The same thing?” you asked, trying to sound casual.
“Yeah,” Sae replied, his tone as calm as ever.
With just one word from him, you got to work, preparing his tea with a practiced speed.
It didn’t take long, and within less than 10 minutes, his drink was ready.
“That’ll be—”
“Here.”
Sae handed you the money without missing a beat, then swiftly took the drink from your hands, taking a slow sip.
A satisfied sigh escaped him as he swallowed, clearly enjoying the tea.
You couldn’t help but watch him, eyes lingering on the way he drank.
This guy…
Noticing your stare, he pulled the cup away from his lips and casually spoke, “Y’know, instead of just wandering around looking at my page, you could always just follow me.”
His voice was quiet, almost teasing, but you couldn’t tell if he was joking or serious.
Nonetheless, your eyes widened at his words.
Fuck…he caught you.
“Uh… yeah, I’ll keep that in mind…” you mumbled awkwardly, the words barely escaping your lips.
You could feel your face burning with embarrassment. This is so humiliating.
Then, just as you were trying to regain some composure, Sae spoke again.
“Give me your phone.”
His words hit you like a punch. What the hell? Why would he want your phone?
“May I ask why?” you asked, raising an eyebrow, the confusion evident in your voice.
“I just want to see something,” he replied, his tone flat and unreadable.
You should’ve known better. You shouldn’t give a stranger your phone. It was basic knowledge, after all. But something about his calm, indifferent demeanor made you hesitate.
Strange, you thought, but you didn’t argue.
With a subtle sigh, you pulled your phone from your back pocket, unlocked it, and handed it to him.
Sae swiftly swiped your phone from your hand, his fingers moving quickly as he typed something and tapped on the screen.
“Here,” he said, handing the device back to you.
You took your phone, still confused, and looked up at him. He met your gaze with a calm, unreadable expression.
Without thinking, you broke the eye contact and immediately glanced at what he had done on your phone.
Your eyes widened.
You were now following Sae Itoshi.
"You needed my phone for this?" you asked, your voice laced with confusion as you shifted your gaze back to him.
He took in your baffled expression, his head tilted slightly.
“Yeah, it’s not that hard to click ‘follow,’” he replied nonchalantly, his tone almost taunting.
You glared at him, feeling a frustrated vein pulse at your temple.
Did he really not care how he affected people?
Actually nevermind. He probably didn't.
Now, you were really starting to believe that people probably were paid to put up with this egotistical jerk.
“Whatever. Is that all you needed?” you asked, forcing the frustration down as best as you could.
It was getting harder and harder to ignore his blunt, cutting words.
“Yeah, i guess.” Sae shrugged, his eyes drifting away from you to inspect the decorations and furniture around the shop.
You let out a quiet sigh of relief, grateful that he wasn’t pushing any further.
But, of course, Sae caught it.
His gaze snapped back to you, a hint of curiosity in his eyes. “What? You that eager for me to leave?”
“Somewhat,” you replied, not even hesitating.
Sae’s eyes narrowed slightly as he processed your blunt answer. His brow quirked, clearly not expecting such a direct response. He shrugged it off casually.
“Too bad. I’m coming back.”
Naturally, that soured your mood tenfold. But, oddly enough, you didn’t feel as annoyed as you’d expected hearing those words.
Odd…
"If you're done ordering, please step out of line," you sighed, shoulders slumping. You were already growing tired of his antics.
"Didn’t even get a chance to check this place out, and you’re already kicking me out? What poor customer service," Sae commented casually, holding up his empty cup in front of you. "Might as well throw this away for me, yeah? Thanks." His tone was light, as if he barely noticed how much he was testing your patience.
You let out a frustrated grumble, muttering under your breath as you snatched the cup from his hand, shooting him a glare before turning to the trash can.
Just as you tossed it away, you looked up to see Sae already strolling out, unbothered.
You felt yourself visibly relax as Sae’s figure disappeared from sight.
Seriously, could that guy be any more irritating?
But your brief moment of relief didn’t last.
"Y/NNIEEE!"
Perfect—just what you needed.
"Ah, my beautiful Y/n, how did your date go with Sae Itoshi?!" Yuko teased, a mischievous grin on her face as she draped an elbow over your shoulder.
"Really, Yuko?" you groaned, nudging her off.
"What? Didn’t go as planned?" Yuko pouted dramatically, raising her hands to her face and pretending to wipe away imaginary tears.
"Sometimes, Yuko, you do too much," you mumbled, glaring at her, hoping the hint of annoyance in your tone would get through.
"Y/n, you’re such a peculiar one. Most girls would go crazy by just seeing that guy! I mean, every time I catch a glimpse of him, my heart practically explodes!" Yuko rambled on, forming a heart with her hands and placing it over her chest, mimicking a rapid heartbeat.
"C'mon, Yuko, you know why—" you paused mid-sentence.
She didn’t know. Yuko didn’t know about the pieces of your past you’d left unspoken, buried somewhere you hoped no one would find.
She didn’t know about the heartbreaks you’d endured, the ones that had chipped away at you until even the thought of love felt distant, hollow. She didn’t know about the countless nights spent piecing yourself back together, the silent battles, the disappointments that had left scars no one could see.
Yuko didn’t know about the lies you’d had to believe, the ones that wrapped around you until you could hardly tell where the truth ended and the facade began. She had no idea how those things had worn you down, until something as simple as liking—or even loving someone, felt like too much to ask.
No, she didn’t know any of it. You’d never told her. And maybe you never would.
"Huh? No, I don’t know why. What do you mea—"
"Oh, uh, never mind, it’s nothing," you said quickly, cutting her off, hoping she wouldn’t pick up on the edge in your voice.
But you knew Yuko wasn’t stupid. You could feel her gaze linger on you, her eyes clouded with confusion and curiosity, studying you, knowing something was going on.
Yet, she knew when to let things be.
"Alright, if you say so, Y/n," Yuko murmured softly, letting it drop.
You looked away, voice barely above a whisper. "Yeah."
You exhaled, feeling a small release as her gaze finally drifted from you.
"Anyway, I’ll get back to my shift, Y/n. Talk to you later!" Yuko said with a small smile as she started to walk away, her curiosity saved for another time.
You gave her a quiet nod and returned to your work. Just a couple more hours, and you’d finally be able to go home.
…🌺…
Here you were, lying in bed, getting ready to drift into a deep slumber.
Slipping into your nightwear, you wrapped yourself snugly in your blanket, instantly enveloped in warmth and comfort. Reaching for your phone on the nightstand, you lazily glanced at your notifications.
“Sae Itoshi is now following you.”
Your breath hitched. For a moment, you thought you were imagining things. Was this real?
Heart pounding, you tapped on your profile and checked your followers.
Nope, it wasn’t a mistake. It was real.
But how? How did he even know your name?
Oh. Right. The nametag.
You tossed your phone aside with a sigh, sinking deeper into your bed.
You couldn’t quite pinpoint what you were feeling. There was happiness, maybe even excitement, but it was tangled up with annoyance and a faint thread of confusion.
Why would he follow you? He didn’t seem like the type to care about someone like you. It didn’t make sense.
But the real question lingered: how did you feel about all of this?
It was strange. These emotions felt foreign, like opening a book you hadn’t touched in years. And yet, they felt… good. Comforting, in a way.
But also terrifying.
You couldn’t remember the last time you let yourself feel like this. What if it led to the same pain, the same destruction? Wasn’t it safer to keep your guard up, to not let anyone in?
“The hell are you doing to me,” you groaned, burying your face into your pillow, trying to escape the overwhelming storm of emotions crashing over you.
…🌺…
"Let me guess—the same thing?"
"Yeah."
You let out a small sigh, already knowing the routine as you headed to the back to prepare his drink.
He came in every day, like clockwork. It was almost comforting in its predictability, though he never switched things up—always the same drink, no pastries, nothing else.
As you handed him his order, you asked, "Do you want anything else, or…?" You already knew the answer but asked anyway, half out of habit, half hoping for a surprise.
"No," he replied flatly, his tone as cutting as ever. "Though it’s pretty stupid of you to even ask. I mean, isn’t it obvious by now? I get the same thing every day."
Ah, yes. Classic Sae. Always quick with the unnecessary criticism. What a great way to dampen your already mediocre morning.
"Well," you muttered, brushing off his remark with a hint of irritation, "it’s just that you always get the same thing. Don’t you ever want to try something else?"
Your tone betrayed your annoyance, but honestly, could anyone blame you?
"If I wanted something else, I would’ve asked for it already, don’t you think?"
Now he was just being a smartass.
"I get that," you scoffed, barely holding back your frustration, "but wouldn’t you want to at least try something different?" Your fists clenched at your sides, a subtle outlet for the irritation bubbling inside you.
Sae paused, his gaze steady as he studied you for a moment. Then, with a sigh, he finally said, "If I buy something else, will you stop nagging me about it?"
"I mean… I guess?" you replied, your uncertainty creeping into your voice. A simple "yes" felt too eager, but saying "no" would make it sound like you were intent on pestering him forever. You weren't a begger. Especially not to him.
Sae gave a curt nod and glanced at the display, scanning the selection before pointing at a pastry. "That one looks decent."
Your gaze followed his finger to the pastry in question. "Alright, then," you said, moving to grab a paper bag. Carefully, you placed the pastry inside, sealed it up, and handed it to him.
"That’ll be 645.87 yen," you muttered, barely meeting his eyes as you extended your hand. He handed you the money without a word, his expression unreadable as ever.
You let out a relieved sigh, assuming this was the part where Sae would leave, as he usually did.
Usually.
Just as you thought your morning might finally return to normal, Sae took a step, then stopped and turned back to face you.
You blinked, confused. Wasn’t he done here? Apparently not.
“Before I forget,” he began, his unwavering gaze fixed on you, “I have a match coming up against this program called Blue Lock. I want you to come watch.”
Your eyes widened slightly, your mouth parting in disbelief.
Did he just… personally invite you to his game?
“Wait… what?” you mumbled, still trying to process his words.
He let out an exasperated sigh, his expression tinged with impatience. “I said I want you to come to my match. You’re not deaf, are you?”
And just like that, your initial shock morphed into irritation.
Great. Just great.
“Well, can you blame me? It’s not every day a famous player invites someone they barely know,” you grumbled, narrowing your eyes at him.
Sae shrugged, resting a hand on his hip. “I don’t have anyone else to invite,” he admitted casually. “Besides, you’re not all that bad to talk to.”
Your eyebrow shot up. “What’s that supposed to mean?” you murmured, your tone skeptical.
He met your gaze without hesitation. “You’re someone I enjoy talking to. I’m sick of people who act all formal and fake around me, putting on some persona just because of who I am.” His voice was steady, almost nonchalant. “Not to mention the crazy fans. It’s exhausting.”
He paused, then added, “It’s refreshing talking to someone who doesn’t act like that.”
You didn’t know how to respond. Was he being serious? Judging by his expression, he didn’t seem like the type to lie about something like this.
Your chest tightened, your heartbeat picking up speed.
Were you nervous? Happy? Flustered?
It was hard to tell—everything about this felt foreign, yet oddly familiar. It left you feeling strangely vulnerable.
“Our conversations are also quite pleasant,” Sae added, his tone as flat as ever.
You blinked, your expression instantly deadpan. Did he really just call our “conversations” pleasant?
What a ridiculous statement. The only thing you two ever did was bicker—and by bicker, you meant he annoyed you to no end. Pleasant? Hardly.
You let out a sigh, equal parts confused and exasperated, before replying, “Sure, Sae. I’ll accept your invite.”
The words left your mouth before you could really think about them. Why had you said yes? You could’ve said no—you should’ve said no. That would’ve been the normal response. The usual you response.
But instead, you’d said the opposite.
Strange.
What’s been up with you lately?
"I'll text you the details," Sae said, snapping you out of your thoughts.
And with that, he finally left, pastry in hand, leaving you to process the whirlwind of emotions he'd stirred up.
…🌺…
One day.
The match against Blue Lock Eleven was just one day away.
It was strange—this was the first football match you’d ever been excited about, and honestly, it didn’t feel like you at all. You’d never cared much for sports. Until now.
Was it the thrill of having a big shot like Sae personally invite you to one of his games? Or was it the curiosity of experiencing a live sports match for the first time?
Probably a little bit of both.
But alongside the excitement, there was something else. Nerves.
Actually, scratch that—you were really nervous.
You’d have to go alone—not that being alone bothered you most of the time, but this was different. It would’ve been better to bring a friend.
Maybe Yuko? She could always go, right?
But then again, Sae had personally invited you. That probably meant he’d already arranged for a seat—most likely close to the field. And with how packed the stadium would be, there’d hardly be any open seats nearby. Everyone would be scrambling to get as close as possible.
You groaned, letting your head hang low in frustration.
Looked like you’d just have to suck it up.
“What’s got you looking so down in the dumps?”
You lifted your head, only to be met with none other than Yuko herself.
Speak of the devil.
"Nothing much. Just… thinking," you replied, straightening up to regain your composure.
Yuko raised an eyebrow and stepped closer, stopping just within arm's reach. "About what?"
"Just about an upcoming game," you murmured quietly, crossing your arms as you tried to mask your nerves.
"Why would you be stressed over a game?" Yuko asked, her expression turning confused as she looked at you.
You sighed, feeling the weight of your thoughts. It wouldn’t hurt to tell her, right?
"Well, it’s just that Sae Itoshi invited me to watch one of his games and—"
"WHAT?!" Yuko screamed, cutting you off mid-sentence.
You immediately felt your face flush in embarrassment as her loud shout turned every customer and employee's attention toward you both.
"Yuko! Keep it down!" you hissed, quickly covering her mouth to stop any further outbursts.
"Sborrey," Yuko mumbled, her voice muffled as you kept your hand over her mouth.
You slowly pulled your hand away, gripping her shoulders as you gave her a stern look. "Yuko… please don't shout like that," you grumbled, scolding her gently.
"Mmm, I’ll try," she awkwardly chuckled, a sweatdrop forming on her forehead.
"Anyway… what about Sae Itoshi?" Yuko whispered loudly, leaning so close to your face that you could feel her breath.
"I said, Sae Itoshi invited me to one of his games," you repeated, trying to stay calm.
She froze for a moment, eyes wide. "He… he personally invited you?!" Her voice trailed off in disbelief as she spoke loudly.
"Yuko!" You shot her a glare, but before you could speak again, she broke into a grin that looked almost too wide.
"Yes, he personally invited me," you murmured, now feeling even more awkward under her intense gaze.
"Oh my gosh… OH MY GOSH! Y/n, do you have any idea how lucky you are?!" Yuko practically shouted, her eyes sparkling with excitement. "Any girl would kill to have THE Sae Itoshi invite them to his game! How’d you do it? Did you seduce him? Or did you promise him se-”
"Yuko!" you shouted, quickly cutting off whatever inappropriate thought was about to escape her lips.
"Sorry, Y/n… but seriously, tell me! How?" Yuko urged, clasping her hands together with excitement.
You looked away, scratching your chin, before meeting her gaze again. "Well, he just said he enjoyed talking to me and then invited me," you said, trying to downplay the whole thing.
Yuko’s expression immediately dropped, and she stared at you, incredulous. "Are you kidding me? That's it? No love confession or anything?"
"Um… no," you replied, still staring at her, not entirely sure how to react to her reaction.
"Ugh, that's so lame!" Yuko huffed, tugging at her hair in frustration. "Y/n, I thought you were better than this!"
"What do you mean—?"
"Never mind!" Yuko cut you off with an exasperated sigh. "Well, regardless, this is the first time I’ve heard of Sae Itoshi taking an interest in someone he barely knows enough to invite them to his game." She grinned mischievously, raising her eyebrows up and down as she looked you over.
"Yeah… I was kind of shocked myself," you replied, brushing off her teasing with a nonchalant shrug.
"He's definitely interested in you, Y/n!" Yuko exclaimed, grabbing hold of your arm in excitement.
You deadpanned, staring at her in disbelief. Really? The Sae Itoshi, interested in you? What a joke.
But even as you dismissed it, you couldn’t help but wonder. Why had he invited you? Sure, maybe it was because he enjoyed talking to someone who wasn’t fawning over him like the rest of the world, but was that really all?
Is that really all it took?
"You're funny, Yuko," you murmured, gently shaking her off.
"Aww, c’mon, Y/nnnieee!" Yuko whined, practically bouncing on her feet. "He invited you! He could’ve picked anyone else who was 'sane,' but he chose you!" She emphasized the word sane with a teasing grin.
"Yuko, you’re just making this into something it’s not. It’s probably nothing," you said, brushing it off as you started to move away and continue your shift.
If Yuko could, she would have slapped some sense into you.
She hated when you were this oblivious. "You’re hopeless, Y/n," Yuko groaned, shaking her head as she let you do your thing.
With that, Yuko left, leaving you alone with your thoughts.
Great. Now her words were swirling in your mind, filled with what ifs.
It felt strange—almost disorienting—as your heartbeat quickened along with the rise of these thoughts.
This was definitely not like you. It only made you feel more stressed and confused.
Maybe Yuko was right. You really were hopeless.
Although who could blame you, after everything you've been through?
…🌺…
SAE! SAE! SAE! SAE!" The crowd roared his name, their voices blending into a thunderous chant as the prodigy scored the first goal.
You were completely mesmerized, entranced by his skill. For a moment, you forgot all about the nerves that had been eating at you since this morning.
…(right before the match)…
Come on, Y/N, you'll be fine," Yuko had said earlier, her tone reassuring. "But what if I get lost?" you had asked, chewing on your lip. "I highly doubt that," she replied with a smirk.
Yuko had been trying to comfort you as she drove up to the entrance of the stadium. Since you didn’t have a car, she’d offered to drop you off. Out of the kindness of her heart, she even gave you a full pep talk on the way.
You sighed, sinking further into the passenger seat. "I just don’t get why you can’t take the day off and come with me," you murmured.
Rolling her eyes, Yuko shot you a look. "Y/N, I have another job. I don’t exactly have the luxury to tag along with you today.”
You knew about Yuko's other job. She had told you just yesterday when you asked her to come with you. Still, the idea of navigating a building packed with thousands of people on your own felt overwhelming.
"As much as I love you, Y/N... you need to get out of my car. I'm going to be late," Yuko said, leaning over to push open the passenger-side door.
The word love made you flinch slightly. You weren’t used to hearing it, at least not like that.
"Yuko..." you mumbled, watching her gesture impatiently at the open door.
"Y/N, you’re going to be fine," she said with a firm but reassuring tone. "Just ask someone for directions!"
You hesitated for a moment before sighing. "Fine. Since when did you want me gone so badly?" you asked, feigning offense as you shot her a playful glare.
"Ever since you started making me late!" Yuko shot back, her voice exasperated but light. "Come on, Y/N!"
She kept nudging you to get out, her urgency growing by the second. Despite yourself, you couldn’t help but laugh a little as you finally stepped out of the car.
"Okay, okay!" you chuckled softly as you finally stepped out of Yuko's car.
You shut the door with a solid slam and turned toward the stadium entrance. Glancing back one last time, you caught Yuko waving at you before she drove off. A frown crept onto your face as your attention shifted to the massive doors ahead.
Taking a deep breath, you stepped inside. Instantly, it felt as though someone was twisting your insides. The nerves hit hard.
You wandered through the bustling halls, clutching your ticket like it was a lifeline. But the moment you found your seat, it was like someone flipped a switch. All those negative emotions—gone, replaced by excitement and anticipation.
_______
“GO SAE!" you shouted along with the crowd as he made a goal, cupping your hands around your mouth as if that would make your voice reach him. Deep down, you knew he couldn’t possibly hear you over the deafening roar of the fans chanting his name.
Still, you couldn’t help but grin. You hadn’t expected to enjoy this, not really. But here you were, caught up in the moment, cheering louder than you thought possible.
You smiled, your gaze fixed on the prodigy dominating the field. Admiration filled you, though you couldn’t tell if it was just for his skill—or if there was something more.
From your reserved seat—the one he had bought for you—you watched him intently. And then his eyes found yours.
Your breath hitched as Sae locked eyes with you. The moment stretched, and the longer it did, the warmer you felt, your cheeks heating under his piercing stare. Was that a good thing?
Your palms grew clammy, your heart racing wildly in your chest. And then, just as you thought the intensity might be too much, he smirked. It was a sly, almost teasing look, as if to say, Did you see that?
Your eyes widened slightly as you took in his expression. For the first time, you saw something beyond boredom or disinterest—even anger—on his face. It was subtle, but it was there—a spark of something you couldn’t quite name.
Still, you preferred this over his usual expressionless gaze. That smirk, that piercing look—it made you feel something.
But as much as you enjoyed it, you hated it too. It felt familiar, painfully so. And familiar wasn’t safe. It was dangerous.
You’d felt this way before, and it hadn’t ended well. It left you shattered, broken in ways you swore you’d never let happen again. You couldn’t afford to risk those consequences a second time.
Forcing yourself to breathe deeply, you tried to steady your thoughts, keeping your composure as you held his gaze. Part of you wanted him to look away, to release you from the unspoken tension. Yet another part... didn’t.
It was as if the gods decided for you when Sae finally turned his attention back to the field.
You exhaled sharply, feeling your heart begin to slow. But even as relief washed over you, those lingering feelings—the ones you tried so hard to suppress—still churned within, refusing to let go.
It seemed these lingering "feelings" would take their time to fade, refusing to settle easily.
_______
“Come on, just give me your number, pretty boy!"
Sae didn’t even acknowledge the man’s bold remark, brushing it off as if it hadn’t been said.
Your attention shifted to the source of the comment—a guy with blond hair, the tips dyed pink. He stood out, to say the least. Odd, maybe, but he certainly wasn’t shy.
The game was already in its second half, and you felt more alive and energized than ever. You never imagined you’d enjoy something like this—not in a million years.
The next match was about to start, and you could feel the tension crackling in the air. It radiated from the players on the field and the roaring crowd around you.
They were tied.
This next goal could decide it all.
You sat on the edge of your seat, anticipation coursing through you. Deep down, you hoped for U-20 to win.
Not that you cared too much about the outcome—your loyalty was simple. Sae was on U-20, and he was the only reason you even knew about the team.
Your eyes widened as the player named Shidou seamlessly linked up with Sae. Together, they were nothing short of monsters. Their aggressive, fast-paced gameplay was unmatched, almost unreal. With every precise pass and powerful stride, they closed in on the goal.
But fate had other plans.
In a sudden turn of events, Blue Lock Eleven intercepted the ball. Before you could fully process what was happening, a player named Isagi launched the final shot.
The ball hit the back of the net.
For a heartbeat, the stadium fell silent. Then, chaos erupted—screams, cheers, and a deafening roar from the crowd.
You exhaled a breath you hadn’t realized you were holding. The tension had gripped you so tightly it felt as though the game had you in a chokehold. It was exhilarating—every second of it.
As the crowd began to disperse, you quickly gathered your belongings. But before heading out to meet Yuko, you decided there was one thing you had to do. You needed to see Sae.
Walking down the hallways, you peeked into every room, hoping to find Sae in one of them.
By the time you reached the last door, there was still no sign of him. Where the hell was he?
Letting out a frustrated huff, you pulled your head back and turned to leave. But before you could take another step, you bumped into someone.
"Ah—I'm sorry! Please forgive me, I wasn't paying attenti—"
"Do you always apologize this much, or what?"
You froze. That voice—of course, you knew that voice.
Your head snapped up, and sure enough, there he was. Sae.
"Oh, it’s just you," you said, letting out a breath. "I’ve been looking for you."
"For what?" Sae asked, his sharp gaze fixed on you, his tone as unreadable as ever.
Was he really this dense?
"To congratulate you. Why else?" you said, arching a brow at him.
Sae locked eyes with you, and once again, your heart betrayed you, picking up speed as the silence stretched. Finally, he spoke.
"What’s there to congratulate? We lost," he said flatly.
"Still, you played well," you replied earnestly.
"I guess," Sae muttered, his tone dismissive.
Your jaw tightened. Somehow, he always found a way to get under your skin.
"Could you show a little more gratitude than just ‘I guess’?" you grumbled, shifting your weight onto one foot, irritation bubbling over.
"And what do you want me to say?" he asked, his sharp eyes glancing over your figure.
"A simple ‘thank you’ would be nice," you shot back, your tone dripping with frustration.
Sae stood there, quiet for a moment. Then, in a low voice, he murmured, "Thank you."
It wasn’t much, but it was enough to catch you off guard.
You couldn’t help but smile at his response. “That’s much better. See? It wasn’t that hard, was it?” you teased, your smile unwavering.
Sae took in your smile, then shot back with a snarky reply, “What, do you want me to pick an answer that’ll satisfy you?”
Your smile faltered, and you stared at him, baffled. What was his deal? “Never mind... forget I said anything,” you muttered, letting out a sharp sigh.
A heavy silence fell between you both. It lingered, uncomfortable, as neither of you knew what to say next.
Just as you were about to break the silence, Sae spoke first
“Its best if i get goi-“
“Would you like to have dinner with me sometime?”
Sae quickly mumbled as he cut you off, his voice quieter than usual, almost as if he regretted asking.
You blinked, stunned, processing his words slowly. “Huh?” you whispered, your heart skipping a beat. It took a moment for the question to fully sink in. Did he really just ask you that?
Did Sae Itoshi—the Sae Itoshi—just ask you out to dinner?
You stood there, unsure whether you had heard him correctly, your mind racing. Sae, the same guy who had been so indifferent and sharp with you, was now asking you to dinner? The idea felt so out of place, yet somehow, it didn’t seem like a joke.
The silence stretched again, and you wondered if he was waiting for your response.
“Uh, Sae, can I ask why?" you muttered, still reeling from shock.
Sae let out an irritated grumble before responding. "I said it before, didn’t I? You’re the only person who doesn’t go crazy over me. Is it wrong to want some company?" His tone made it clear he was turning this back on you.
"Well, not exactly, no—"
"Then why is it such a problem for you?" he interrupted sharply.
You stood there, staring at him, utterly confused. Why was he blaming you now?
"It’s not a problem," you replied, trying to keep your voice steady. "It’s just… surprising, that’s all."
But Sae wasn’t ready to let it go. "Why is it such a shocker?" His agitation was growing more obvious.
"It’s not—actually, never mind," you sighed, feeling the frustration creeping in.
You knew this conversation wasn’t going anywhere, and continuing would only make things worse.
Sae let out a satisfied hum, as if your response had confirmed everything he wanted to hear.
Silence crept back in, heavy and uncomfortable. You shifted your gaze elsewhere, refusing to look at him. Something about meeting his eyes made your stomach swirl uneasily.
It was the opposite for Sae, though. His piercing gaze stayed locked on you, sharp and unrelenting like a hawk stalking its prey. He hadn’t looked away from you once.
"So? Your answer?" Sae’s voice cut through the quiet, calm yet demanding.
You responded quickly, almost too quickly. "Uh, yeah. I can. Sure.
Sae's eyes narrowed slightly. You hadn’t even looked at him when you spoke, and for some reason, that ticked him off.
"Why don’t you look at me when I’m talking to you?" he asked, his voice laced with irritation. It was clear he wasn’t just annoyed—he was genuinely angry.
Wow. What a way to cross boundaries, huh?
Still, he had a point.
Why weren’t you looking at him? Why did your palms feel clammy when he stood so close? Why did your heart race like it was trying to escape your chest? Why were you all fidgety?
It couldn’t possibly mean you liked him.
No, of course not. You were just… nervous. Right?
It had to be nerves. This was the longest time any guy had spoken to you, after all. Most of them usually got what they wanted and left.
Actually, thinking about that now made you feel ridiculous—like you were some kind of attention seeker.
Or maybe it was because you felt so small, so insignificant, under the weight of his gaze. His presence was overwhelming, suffocating—a constant reminder of how much larger than life he was. A big shot. Someone untouchable.
And yet, that only made you feel more pathetic.
But what did you really feel?
Maybe—just maybe—he had grown on you. Maybe you had caught feelings. But was it because he stayed longer than anyone else ever had? That thought alone made you feel queasy. It felt wrong.
Desperate.
Attention seeker.
The words echoed in your mind like a cruel whisper. You hated the sound of it. You didn’t want that to be the truth.
But what if you did like him? What if it wasn’t just nerves, or loneliness, or some desperate grasp at the closest thing to affection?
You’d considered the possibility, of course. You weren’t naïve enough to ignore it. But you refused to let it be true.
You weren’t ready—not for this, not for him, not for the chance of heartbreak all over again.
You’d been through it countless times before. And you weren’t sure you could survive it again.
If that’s how you felt—if you really did like him—but he ended up taking what he wanted and leaving like all the others… would you even be able to pick up the pieces this time?
The thought alone was unbearable, and it crushed any shred of hope you might have clung to.
It dampened your mood, dragging it into a deeper, darker place. You wanted to pull back, retreat while you still could. But it was too late now.
"Did you even hear me? What’s up with you and being deaf?"
His sharp tone cut through your thoughts, snapping you back to the present. The weight of your emotions dulled, if only for a moment, as irritation took their place.
"I'm not deaf," you muttered, your voice dripping with frustration.
"I doubt that," Sae shot back without missing a beat.
Resentment bubbled inside you, but before you could fully process it, Sae’s voice broke through again. "At least you’re looking at me now."
That stopped you cold.
He was right. You were looking at him now.
Your emotions screeched to a halt, forced into submission by the weight of his words. You didn’t even realize when you’d started meeting his gaze, but now there you were, staring back at him.
It felt like standing in the middle of a battlefield, with nowhere left to run.
"That aside, what time should I pick you up?" Sae asked casually, as if the question was of no real importance to him.
Your eyes widened. Right… you’d agreed to the dinner he offered.
"Uh… anytime in the afternoon is fine," you mumbled, struggling to find your voice.
"5:30 then?" he suggested, his tone as nonchalant as ever.
"Yeah, that should work," you nodded, quickly running through your mental schedule.
"See you on Sunday, then," Sae said abruptly before turning on his heel and walking off, his dismissal clear.
"Yeah… Sunday," you murmured softly, even though you knew he couldn’t hear you. He was already out the door.
The moment he left, you let out an exhausted sigh, your body finally relaxing. You hadn’t even realized how stiff you’d been.
But before you could fully unwind, your phone buzzed in your pocket. With a weary hand, you pulled it out, unsure of what—or who—was waiting for you now.
"Yuko 🤡."
The contact name flashed across your screen, pulling you out of your thoughts. Right—Yuko was supposed to pick you up.
You stared at the screen for a moment before silencing the call, deciding not to answer. There wasn’t much to say anyway, and your head felt too cluttered to hold a conversation right now.
Shoving the phone back into your pocket, you hurried toward the exit. Each step felt heavier than the last, as if the weight of the earlier exchange with Sae was dragging behind you.
You needed air. You needed to think. And maybe—just maybe—a way to stop the relentless pounding in your chest.
_______
As you stepped out of the building, the familiar sound of Yuko’s voice greeted you.
"Why didn’t you answer my call?!" she exclaimed, leaning halfway out the driver’s side window, her dramatic tone impossible to miss.
You rolled your eyes, suppressing a tired smile. "What about it? I’m here now, aren’t I? Be grateful I even saw your call."
Yuko gasped, hand to her chest as if deeply offended. "The audacity!"
You chuckled softly, shaking your head as you opened the car door and slid into the passenger seat. Her over-the-top antics were a welcome distraction from the weight still lingering in your chest.
"Sooo," she began, eyes glinting with curiosity as she waited for the seatbelt to click, "how was the game?"
"It was good," you replied, sinking into the seat as the exhaustion caught up to you. "Better than I expected."
Yuko hummed, pulling onto the road, but her sideways glance told you she wasn’t entirely convinced by your answer.
"Better than you expected, huh? Was it because Sae Itoshi was there?" Yuko teased, her grin wide as she navigated the familiar route to your beloved sanctuary—home.
You groaned, tilting your head against the seat to glare at her. "No, it wasn’t just because he was there," you grumbled, your tone sharp enough to match your annoyance.
"Oh, really? Well, if you say so…" she chuckled, clearly not buying it.
"Believe what you want, Yuko," you huffed, rolling your eyes. You knew she wouldn’t let it go, but you were too drained to argue.
"Okay, okay," she said, feigning surrender before flashing you another sly glance. "So, if it’s not because of Sae—according to you—what made it better than you expected?"
Her words hung in the air for a moment.
You hesitated, staring out the window as you mulled over her question. The truth was painfully obvious: it was mostly because of Sae. But you’d rather bite your tongue than admit that out loud.
Finally, you hummed, masking your thoughts. “The players were really skilled, and the game was super intense. I was honestly very impressed by their amazing footwork.”
Yuko raised an eyebrow, sparing you a glance as she drove. "Mmm-hmm. Sure, it was all about their footwork," she said, her tone dripping with playful disbelief.
You crossed your arms and leaned back, determined to let the conversation end there. At least, that’s what you told yourself.
You weren’t lying about the players’ skill. They really did keep you on the edge of your seat, and the game had been incredible.
"But damn… now you’re making me regret not going," Yuko groaned, dramatically slumping her head onto the steering wheel. Luckily, you were stopped at a red light. "Having more than one job sucks!"
You laughed, unable to help yourself. "It was a fun game," you admitted, watching her over-the-top display.
Yuko sighed heavily, the light turning green as she straightened up and began driving again. "Rub it in why don’t you," she muttered, though her grin betrayed her fake annoyance.
It didn’t take long for the car to fill with her usual nonsense—playful jabs, ridiculous theories, and random observations that seemed to come out of nowhere.
You quarreled the whole way home, with her spouting dumb, shitty jokes and exaggerated stories, while you did your best to tolerate it—barely. Still, there was a comfort in the banter, her chatter distracting you from the quiet heaviness that had lingered after Sae.
By the time you pulled into your driveway, you felt lighter, even if just a little.
…🌺…
Seeing the taillights of her car disappear into the night, you let out a heavy sigh and dropped onto the couch. The weight of the evening pressed down on you as you tossed the apartment keys onto the coffee table. The sharp jingle and dull clack of metal meeting wood cut through the silence, a momentary distraction as you sank deeper into the plush cushions.
Your expression darkened, a frown tugging at the corners of your lips. Why? Why was it always Sae that haunted your thoughts, filling your mind with questions you didn’t want to answer? No matter how hard you tried, you couldn’t shake the lingering echoes of your earlier conversation with him.
The date you’d agreed to—it was just two days away. The thought twisted your stomach into knots. You wanted to back out, to call it off before it began, but the idea of standing someone up felt even worse. Disappointment was something you despised, even more so when you were the one responsible for it.
A frustrated groan escaped your lips as you buried your face in your hands, rubbing at your skin with rough, almost punishing force. Agitation bubbled beneath the surface, a bombardment of emotions you couldn’t quite name. The room felt suffocating, the silence too loud, and yet all you could do was sit there, wrestling with a decision you didn’t know how to make.
You dropped your hands into your lap, staring blankly ahead as your thoughts swirled like a relentless storm, each one louder and more suffocating than the last. The idea of possibly liking him—or worse, getting attached—clawed at your mind. It was a question you couldn’t stop asking yourself, no matter how much you wanted to bury it.
You clung to the hope that it was merely the second option, attachment. Even though you despised both possibilities, the latter felt like the safer bet. Safer, because it didn’t require vulnerability. Safer, because it didn’t come with the promise of heartbreaking pain.
But the thought of giving yourself to someone—as a lover, as a partner—sent a wave of nausea through you. It was too much. The mere idea of trusting someone with the fragile pieces of your heart again was unbearable. You’d rather push them away, let them detach cleanly and painlessly, than risk being left exposed, broken, and abandoned once more.
Hope? No, that was long gone. It had slipped through your fingers like sand, scattering into nothingness long before tonight. You had stopped believing in the gentle caresses and warm embraces of true love. Those things weren’t meant for you. They were for people who hadn’t already been shattered. People who hadn’t spent years picking up pieces they could never fit back together.
You slumped further into the couch, letting the weight of that realization press down on you. The silence wrapped itself around your thoughts, heavy and suffocating, as the void within you grew wider. If love had ever been a possibility, it wasn’t anymore. And you’d made peace with that. Or so you told yourself.
…🌺…
As the hours passed, your anxiety and stress got worse.
You were basically going to have a ‘date’ with Sae in less than 24 hours. And of course with the weight of this realization—it didnt help as Yuko was nagging your ear off as usual.
”Oh come on Y/n, are you even listening to me?”
“Sorry Yuko, what was that?”
You were pulled away from your thoughts as Yuko called you out.
Yuko gave you a slight scowl before returning to her unnecessary speech. However, as soon as she started speaking, your mind subconsciously ignored her words as you began to think about it Sae once more.
It started to become a habit now—thinking about Sae. It was indeed a troublesome habit you’ll admit, but you couldn't help it.
It’s weird. A guy with few words who started showing up at the place you worked at not that long ago—now starting to take such an impactful and heavy toll on you? It was something you could have never predicted.
“And then she thought it was a good idea too—Y/n!” Yuko shouted, grabbing your attention once more.
Your gaze snapped back to Yuko as you were met with an angry look. “Sorry Yuko.” you apologized.
“Are you serious Y/n? Is my story not that entertaining to you?” Yuko spoke as she took a step closer.
“No that's not it all. It's just…somethings been on my mind lately.” you spoke earnestly.
“Spill.” She demanded, not wasting a breath.
You let out a soft chuckle at her antics as you basically gave her a rundown on the encounter with Sae.
_______
“Y-You mean…its an actual DATE?!” Yuko shouted as a very unnatural, wide grin overtook her face.
“Uh I guess..” you sweatdropped, taking a step away from Yuko.
Yuko squealed like a fangirl as she ran up to you, squeezing the life out of you as she gave you her signature hug, pushing your face down to the plush of her breasts.
“Yuko! That's enough…” You mumbled out as she had you caged in.
Yuko reluctantly let you go as she gave you some space.
“Y/n, I told you. WHAT DID I SAY FROM THE BEGGINING! This man is into you! And its Sae Itoshi out of all these men!
“Yuko…its just a friendly date. He's not into me like that…I think.” You spoke with a bit of uncertainty.
“Why are you in denial Y/n?! I have never heard from the media or anywhere of Sae Itoshi inviting a girl he just met not that long ago to dinner just for ‘friendly talk’. I am telling you he's into YOU!” Yuko rambled on, getting some sense into your head.
“Yuko…i think your overlooking this maybe a bit too much,” you mumbled as you tried to drop Yuko’s accusations.
Yuko paused. She slowly turned her head towards you with a deadpan expression. “Are you fucking with me right now?”
“Y/n…are you fucking serious right now?” Yuko spoke with an alarming calm tone.
Yuko took a couple step towards you as she stared you down. An unreadable glint flashed in her eyes as she stood quiet. “If I could Y/n…i would beat you senseless if it means I can finally get this through your head. Its a shame I love you too much to do that.” Yuko finally spoke as she let out a sigh.
“Do I take that as a threat or…” you mumbled, slightly startled by her actions and words.
“Nope!” Yuko chuckled as she stepped away from you. “Ill let you be Y/n. But trust me when I say he’s interested.” Yuko voiced as she looked at you.
“How can you be certain though Yuko?” you spoke.
Yuko smiled at you before she left. Her steps slowly receding as she gave you one last glance before leaving you to do your job. “I know men, Y/n.”
…🌺…
“I'll pick you up. What's your address?"
"It's *****”
"Alright. I'll be there in about 10 minutes."
You set your phone down on the nightstand, releasing a shaky exhale. Even texting Sae was nerve-wracking.
Rising slowly from the couch, you headed into your bedroom to give yourself one last look in the mirror. You didn’t want to seem underdressed—not for a date with Sae. Oh, especially not with the Sae Itoshi.
Dragging your feet across the creaking floorboards, you pushed open the bedroom door. You stopped short in front of the full-length mirror, taking a moment to steel yourself.
You stared at yourself, your own reflection staring back. But the image before you felt foreign, like a mask you no longer recognized. The girl in the mirror seemed whole, unbroken, but you knew better—everything she showed was a lie. Beneath her composed surface was the weight of every heartbreak, every whispered promise that shattered like glass.
You saw your past in her eyes, a pool of anguish and betrayal. Men who touched but never stayed, who spoke of love yet only took what they wanted—leaving nothing but fragments of yourself behind. They had used you, consumed you, and discarded you, their intentions never pure, their affection hollow. You craved love, dreamed of it as something beautiful, but each experience taught you the same painful truth: love wasn’t real. It was an illusion, a cruel trick life played to make you believe in something that didn’t exist.
And yet, as much as you wanted to give up, as much as the mirror whispered that hope was foolish, you couldn’t stop the ache. The craving for love was carved within you. You wanted to be held, cherished, seen—not for what you could offer, but for who you were. But with each passing day, fear groped tighter around your heart. What if love would only break you again? What if the cost of trying was more than you could bear?
You longed for someone to prove you wrong, to show you love wasn’t just a fantasy crafted by movies and books. But even that hope felt dangerous. Could you risk it? Could you open the door to your heart one more time, knowing it could destroy you if it all fell apart again? If someone could rewrite what love means to you, would you let them?
It was odd. Very odd, indeed, that in the midst of such vile and upsetting thoughts, Sae appeared in your mind.
But why?
Why was it him who came to mind?
You’d only known the guy for barely two months. Was that really enough time to feel yourself growing... attached? The thought was confusing—so confusing it made your head spin.
A frown crept across your face. Yes, confusing was the perfect word. It was almost impossible to imagine Sae and love in the same sentence. The word felt foreign and distant, like it belonged to a language you could never hope to understand.
The sudden chime of your doorbell snapped you out of your thoughts. Sae was here. How much time had passed?
You grabbed your belongings in a rush, practically stumbling to the front door. Pausing for a moment, you let out a deep breath, steadying yourself. The nerves were hitting you like a shit ton of bricks, threatening to overwhelm you.
But you could manage. At least, you hoped you could.
You opened the door, and there he was—Sae Itoshi, standing casually yet exuding that air of quiet confidence he always seemed to carry.
Your eyes trailed over his figure, taking in his outfit: a brown blazer layered over a plain white T-shirt and a pair of fitted black pants that somehow managed to look both fitted and effortlessly relaxed.
As you took in his appearance, it seemed he was doing the same to you.
“You actually look decent for once. I was half-expecting your outfit to be as bad as those crappy work uniforms,” Sae remarked, his tone as dry as ever.
Of course. Not a single day passed without at least one of his signature insults.
“Thanks. You don’t look bad yourself,” you muttered, biting back your irritation—a skill you’d honed to near perfection in these past two months.
Sae let out a low hum, a sound that could almost be mistaken for agreement. The corners of his lips tugged upward ever so slightly, a ghost of a smile flickering across his face. “The car’s outside. Let’s go.”
You gave a short nod and stepped out, pausing only to lock the door behind you. The cool night air greeted you as you followed him down the path, nerves still fluttering in your chest but your steps steady enough to keep up.
You followed behind Sae as he led the way to his car, his confident strides making it clear he expected you to keep up. When you reached the sleek vehicle, he headed straight for the driver’s side without so much as a glance in your direction.
What a gentleman.
Suppressing an irritated sigh, you opened the passenger door yourself and slid into the seat. As you settled in, your gaze drifted—unbidden—to Sae. His hands, calloused and veined, gripped the handle firmly as he opened his door. Slim, strong, and steady, they were surprisingly... attractive.
A sudden warmth rushed to your cheeks, and you blinked, snapping yourself out of it. Really? Were you seriously paying attention to his hands? This wasn’t like you. But, embarrassingly, you could now understand Yuko’s endless rants about the appeal of a man’s hands.
You shook the thought away, pressing your lips into a thin line as Sae slid into the driver’s seat. He shot you a brief glance, his teal eyes sharp, curious, but ultimately uninterested enough to probe further.
“So, uh... you have a destination in mind?” you asked, your voice cutting through the awkward silence.
“Of course. I wouldn’t have invited you if I didn’t have a place in mind, would I?” Sae replied, his tone matter-of-fact as he started the car.
“Yeah...” you mumbled, feeling a little embarrassed by your question. Why was it always so hard to hold a normal conversation with this man?
The drive was quiet at first, the low hum of the engine filling the space. But you couldn’t help noticing Sae glancing at you every so often, his teal eyes flicking toward you before quickly returning to the road. It wasn’t subtle—he was clearly taking in your appearance.
The attention made you squirm slightly in your seat, the silence growing heavier with every glance. Finally, you broke it. “Do I have something on my face or...?”
Sae’s gaze shifted fully to you for a brief moment, his expression calm but entirely unreadable. Caught in the act, it seemed. “No,” he said, his voice as smooth and detached as always. “I’m just... still surprised you managed to look this put together outside of your uniform.”
“Put together?” you repeated, eyebrows raising as you tried to determine whether or not to be offended.
“Yeah. You look good.”
The words landed like a wave out of the blue. Your eyes widened, and an undeniable blush crept across your cheeks.
Sae Itoshi—the Sae Itoshi—just said you looked good.
You opened your mouth, searching for a response, but nothing came out. All you could do was turn your gaze toward the window, attempting to hide the warmth that flooded your cheeks. Meanwhile, Sae returned his attention to the road, his expression as unreadable as ever, as if he hadn’t just sent your heart racing.
Your stomach churned, a confusing mix of queasiness and ecstasy, while your heart hammered relentlessly in your chest. You hated it—and enjoyed it at the same time.
Out of the corner of your eye, you caught Sae glancing at you through the faint reflection in the window. A quiet chuckle escaped his lips, low and rich, breaking the silence in the car.
The sound sent a shiver down your spine. It was a rare, almost musical laugh that you hadn’t heard from him before.
Your ears perked up instinctively, and before you could stop yourself, you turned to look at him. Sae’s face, usually so composed and indifferent, held the faintest trace of a smile. The corners of his lips curved softly, and even his sharp teal eyes seemed to soften, crinkling ever so slightly with the expression.
His smile—rare and beautiful—was utterly mesmerizing. His smile resembled something of a masterpiece, delicate and breathtaking, like standing before the most sacred painting in a museum. The kind of art that pulls you in, making the world fade around you, leaving only the singular beauty in front of you. The curve of his lips, the gentle crinkle at the corners of his eyes, the faintest hint of warmth softening his usually stoic expression—it all felt impossibly sacred. It was the kind of sight that engraved itself into your memory, refusing to be forgotten.
"You laughed," you whispered, your voice barely above a breath, as if speaking too loudly would shatter the fragile perfection of the moment. Your gaze stayed fixed on him, wide-eyed and awestruck, unable to look away.
His expression shifted, the corners of his mouth faltered yet still tilted upward, though now tinged with faint curiosity at your reaction. You barely noticed. The sight of him like this—so unguarded, so human—had stolen every ounce of your focus, making your chest ache with something you couldn’t put into words.
“Am I not allowed? Why is it such a shock to you that I can smile?” Sae asked, the same soft expression lingering on his face as he spoke.
Your face flushed with embarrassment. “No, that’s not what I meant! It’s just... I’ve never seen you make any expression other than annoyance or indifference,” you said earnestly, your words tumbling out before you could stop them.
Sae tilted his head slightly, as though your statement was absurd. “I’m not some expressionless robot. You do realize that, right?” he replied, his usual sarcasm laced with a surprisingly lighthearted tone.
Before you could open your mouth to defend yourself, his voice cut in again, smooth and unbothered.
“Well, would you look at that—we’re here.”
_______
The restaurant was... nice. No, very nice. The kind of nice that made you sit a little straighter in your chair and second-guess your outfit. Everything from the polished marble floors to the soft glow of chandeliers above screamed luxury. You couldn’t help but feel out of place.
You’d never set foot in a restaurant like this before—linen napkins folded like origami, waiters moving with the precision of dancers. It wasn’t hard to imagine that Sae frequented places like this. He looked perfectly at home, his tailored outfit exuding effortless sophistication. Even his so-called “casual” attire seemed worlds apart from your own, and the subtle glint of jewelry he always wore hinted at an expensive taste you couldn’t begin to comprehend.
"Have you decided what to order yet?" Sae’s calm voice broke through your thoughts. He was still scanning the menu, his expression unreadable as ever.
You glanced back at the glossy menu in your hands, the rows of elegant dish names doing little to help your decision. "No, not really," you admitted, glancing up at him. "Everything looks good. I can’t decide."
Sae set his menu down, his gaze shifting to you with that steady confidence of his. "Then order whatever you find even slightly appetizing," he said, as though it was the simplest solution in the world.
You hesitated, your eyes lingering on him as you wrestled with a pang of guilt. "Are you sure? Is that okay...?" you asked softly, your voice trailing off. The weight of the prices on the menu and the sheer grandeur of the place were making you second-guess everything.
"Y/n, I have more than enough to cover the meal," Sae said, his tone as casual as ever. He leaned back slightly, glancing around the restaurant with an almost bored expression. "I could buy this entire place if I wanted to."
Wow. Nothing quite like Sae's unintentional flexes to remind you just how wide the gap was between your lives. Standing next to him on any given day was enough to make you feel like an unemployed, wandering vagabond.
"Ah, right. I forgot how disgustingly rich you are," you grumbled under your breath, a sigh slipping past your lips as you slouched back into your chair.
He didn’t react, just offered you a faint shrug as if to say, Well, it’s true.
Soon enough, the waiter returned, and you gave your order, still feeling a pang of guilt for indulging in food you weren’t even sure you’d like. But as the thought lingered, you steeled yourself. Actually, no—screw the guilt. If Sae wanted to flaunt his wealth and bring you to a place like this, the least you could do was enjoy it. Think of it as compensation for dealing with his bluntness and lack of tact on a daily basis. Yes, this was your reward.
Still, the moments after the waiter left were... awkward. Sitting across from Sae in silence was like waiting for a storm that may or may not ever hit. The quiet wasn’t necessarily tense, but it wasn’t exactly comfortable either. You debated pulling out your phone but ultimately decided against it. It would feel rude, and you weren’t about to be that person.
To your surprise, Sae broke the silence first.
"So," he began, his voice low but steady, "how was your day?"
You blinked, caught off guard by the sudden shift. "Uh... it was fine, I guess. Nothing exciting," you replied, wondering what had prompted him to initiate small talk.
He nodded, his gaze fixed on you in a way that made it clear he wasn’t just asking out of politeness. "Do you have any pets?" he asked next, his tone still casual but carrying a thread of genuine curiosity.
The question made you pause. This was... new. Sae wasn’t exactly known for his conversational efforts, and yet here he was, actively engaging. You decided to roll with it. "No, I don’t, but I’ve always wanted a dog," you admitted, a small smile tugging at your lips. "What about you? I can’t imagine you having time for a pet."
He shrugged again, the corners of his mouth twitching ever so slightly. "You’re right. Too much effort," he said simply, though there was a faint amusement in his tone.
The conversation had been flowing smoothly, surprisingly so, until Sae’s next question brought it to an abrupt halt.
"Have you dated anyone?" he asked, his voice casual but direct, the weight of his gaze making it impossible to avoid.
Your eyes widened slightly at the unexpected question, and for a moment, you froze. Quickly, you composed yourself, forcing a small, nonchalant smile onto your face. "Yeah, actually. I’ve dated a couple of people," you replied evenly, though your voice carried a faint tension that betrayed you.
Sae’s sharp eyes didn’t miss it. He wasn’t just observant—he was a prodigy at reading between the lines, piecing together the truths people tried to hide. The brief flicker of discomfort that passed over your face before you answered didn’t go unnoticed. He didn’t pry, though. Instead, he filed it away silently, as if respecting a boundary you hadn’t explicitly set.
"Well, what about you?" you asked, seizing the opportunity to shift the focus onto him. Your tone was light, almost teasing, though a part of you was genuinely curious. "Have you dated anyone?"
Sae leaned back in his chair, letting out a quiet hum as if considering how much he wanted to say. "Not really," he began, his tone even. "Just a couple."
You raised an eyebrow, surprised by his candor.
"The girls I dated were... aggravating," he admitted with a sigh, tilting his head back and closing his eyes briefly. His expression was calm, but the faint furrow in his brow suggested lingering annoyance. "They wanted too much. Too clingy, too demanding. I couldn’t stand it."
A small chuckle slipped past your lips, the sound light and unrestrained. "That’s surprising," you said with a laugh, covering your mouth with the back of your hand as if to stifle it.
Sae opened his eyes at your reaction, turning his attention to you. For a moment, he didn’t speak, his gaze steady as it lingered on your face. He studied you—the curve of your smile, the sparkle in your eyes that hadn’t been there a moment ago. Finally, he broke the silence. "How so?"
Your laughter quieted, but a playful smile lingered as you met his gaze. "Well, you don’t exactly look—or act—like the type of guy who indulges in relationships," you admitted, leaning back slightly in your chair.
Sae cocked an eyebrow, his expression unreadable at first. Then, a small smirk tugged at the corner of his lips. "Really? That’s funny, because at first, you didn’t look like the type of girl to even know what a relationship is," he quipped, the smugness in his tone unmistakable.
You blinked, caught off guard by the remark, before narrowing your eyes at him. "Oh, come on," you muttered, deadpanning as you leaned forward. "That’s so unfair."
He chuckled softly, the sound rare but genuine, and you couldn’t help but feel the tension in your chest ease. "Jokes aside," he said, his smirk fading into something more sincere, "you’re quite the looker. You’re on the attractive side, you know." His tone was casual, but his gaze held steady, focused entirely on you. "I’m not really surprised you’ve been in relationships."
A faint blush spread across your cheeks as his words settled in, leaving you flustered in a way that made your heart race. Sae always had this way of throwing you off balance, his calm yet blunt remarks stirring a confusing mix of emotions. Why did he affect you like this? You glanced away shyly, mumbling, "Thanks, I guess... you’re not bad yourself."
You fiddled with the hem of your shirt beneath the table, trying to focus on anything but the heat rising to your face. But, of course, Sae couldn’t let you off that easily.
"I know I am," he said, his tone dripping with casual arrogance. "My looks are way above average, after all."
You snapped your head up at his words, a small grunt of frustration escaping your lips. Your narrowed gaze locked onto him. "You know," you grumbled, crossing your arms, "I liked it better when you were expressionless."
But even as the words left your mouth, you knew they weren’t true. If anything, you lived for the rare moments when Sae’s stoic mask slipped, revealing hints of his humor, his smugness, or even just his rare smiles.
Sae’s lips twitched slightly, a hint of amusement playing at the corners of his mouth as he shrugged. "Life doesn’t always give you what you want," he remarked, his voice calm and measured but laced with the slightest tease. "Guess you’ll just have to deal with it."
The sheer smugness in his tone made your irritation bubble over, and an exasperated scoff slipped from your lips. You glared at him, but Sae remained unbothered, his smirk now fully formed as he leaned back in his chair.
He was enjoying this—enjoying the way he was getting under your skin, the way he could pull these reactions out of you so easily
After a round of playful—and not-so-playful—bickering, the food finally arrived.
The dishes were plated with such precision and artistry that they looked almost too good to eat. Almost. The aroma wafted up, rich and tantalizing, and your mouth watered instantly. Your excitement was palpable, your gaze flitting from one dish to the next as the waiters carefully placed them on the table. Words failed to describe the sheer joy your taste buds anticipated, and your expression said it all.
Sae glanced up from his plate, his eyes settling on you. A soft chuckle, barely audible, slipped past his lips as he took in the sight of your excitement. It wasn’t loud or mocking—more like a quiet, amused acknowledgment of how endearing you looked. From his perspective, it was as if this was your first real meal. He found himself wanting to memorize the moment, the way your eyes sparkled, your lips curving into an unconscious smile at the sight of the food.
You didn’t waste a second. Grabbing your utensils, you dug in, the first bite sending a wave of satisfaction through you. The flavors were indescribable—rich, balanced, and utterly heavenly. Each morsel seemed to melt in your mouth, and your body visibly relaxed with each bite.
Meanwhile, Sae hadn’t touched his food. He rested his chin on one hand, watching you with a soft, almost imperceptible smirk. He wasn’t sure what was more fascinating—the way you seemed utterly transported by the meal or the unguarded happiness on your face. You were like an open book in this moment, and he found himself… intrigued.
When you finally noticed his lack of movement, you paused mid-bite, narrowing your eyes at him. "What?" you asked, your voice muffled by food but still laced with suspicion.
Sae shook his head slightly, his smirk growing. "Nothing. Just… you really like your food, huh?"
"Of course, I do," you shot back, quickly swallowing so you could defend yourself properly. "It’s amazing! How are you not eating yet?!"
"I was just enjoying the view," he remarked casually, his tone as calm as ever, though his words carried a teasing edge.
Your cheeks flushed, and you glared at him. "Well, stop staring and eat your food before it gets cold," you muttered, your irritation half-hearted.
Sae finally relented, picking up his utensils and diving into his own meal. The two of you ate in companionable silence after that, the earlier tension easing into something more comfortable.
Between bites, your gaze flickered to him, catching the subtle way his posture relaxed, the way he seemed content. Maybe it was the food, or maybe it was the company, but the moment felt… nice. Natural.
And though neither of you said it aloud, the quiet comfort of eating together spoke volumes on its own.
…🌺…
"The food was great. I really enjoyed it," you said as the two of you walked toward his parked car. The evening air was cool, and the soft glow of the streetlights painted everything in a warm, muted hue.
Sae glanced at you, his hands casually tucked into his pockets. "It sure looked like you enjoyed it, considering the way you stuffed your face," he remarked, his tone as deadpan as ever.
Your face instantly flushed a deep red, embarrassment creeping up your neck. "Hey!" you shot back, turning toward him with wide eyes. "You can’t criticize me for that! This was… new to me! I was just… excited, okay?"
The words tumbled out in your attempt to defend yourself, but the more you spoke, the more you realized how ridiculous you sounded. You huffed, crossing your arms as you stole a glance at Sae, waiting for his response.
But he didn’t say anything. Instead, he just looked at you, his expression softening as a warm, genuine smile spread across his face.
It caught you completely off guard.
The embarrassment that had been bubbling inside you vanished almost instantly, replaced by a strange, calming warmth. There was something about the way he smiled—rare and unguarded—that made everything else seem trivial. For a moment, it was just the two of you, standing there in the quiet evening, and all the teasing, awkwardness, and uncertainty faded away.
This whole evening had been… different. Odd, yes, but enjoyable in a way you hadn’t expected.
Sae opened the car door for you, gesturing for you to get in. As you slid into the passenger seat, you found yourself sneaking one last glance at him, his faint smile lingering in your mind.
Maybe this wasn’t just dinner. Maybe it was the start of something more.
_______
"That’s your apartment, right?" Sae asked, pointing toward the familiar building as he brought the car to a stop.
"Yeah," you replied with a nod, unbuckling your seatbelt and stepping out of the car.
To your surprise, Sae stepped out as well, his movements casual as he fell in step behind you. You turned to face him, your brows furrowing in confusion. "What are you doing?"
He met your gaze, hands shoved into his pockets, his tone as calm and nonchalant as ever. "Walking you to your apartment. Isn’t that how you’re supposed to treat a lady?"
You blinked, caught off guard by his unexpected reply. Of all the times for him to act like a gentleman, now was the moment he chose? His words felt both sincere and teasing, leaving you feeling both confused and slightly amused.
Shaking your head, a small laugh escaped your lips. "Whatever," you muttered, rolling your eyes but unable to hide your smile.
The two of you walked up to the building together. As you reached your door, you fished around in your pocket for your key. The sound of metal jingling filled the air as you finally pulled it out and unlocked the door, turning the key with a satisfying click.
Pushing the door open, you stepped inside and turned around, expecting Sae to leave. But he was still there, standing just outside the doorway, his expression unreadable.
The longer he stood there, the more awkward the moment became. You felt a twinge of guilt, unsure if he was waiting for something or simply being polite. After a beat of hesitation, you sighed and pushed the door open wider, gesturing for him to come in.
"You might as well come in," you said, your voice soft but resigned.
Sae raised an eyebrow, as if slightly amused by your reaction, but he didn’t say anything. With a small nod, he stepped inside, his presence instantly filling the space in a way that felt both strange and oddly comforting.
Sae kicked off his shoes at the entrance and stepped further inside, his eyes sweeping over the room. His gaze lingered on the various pieces of decor and furniture, taking everything in with an unreadable expression. One by one, his eyes moved from the small bookshelf in the corner to the slightly mismatched throw pillows on the couch. Finally, he spoke, his voice calm and measured. "So this is your apartment, huh? Cozier than I expected."
You turned your gaze sharply toward him, a familiar irritation bubbling within you. It seemed Sae had an unmatched talent for making even his compliments sound like backhanded remarks. "You always think so little of me, don’t you?" you grumbled, crossing your arms as you watched him continue his casual inspection of your space.
Sae glanced at you briefly, unfazed. "I judge based on what’s shown on the outside," he said with a shrug, his hands still buried in his pockets. His tone was neutral, almost indifferent, but you could sense a hint of teasing beneath it.
Letting out a sigh, you brushed past him and made your way to the couch, the plush cushions welcoming you as you sank into them. You stretched out slightly, the tension in your body melting away as you made yourself comfortable. "Well, I guess that makes you the ultimate judge of character, huh?" you muttered, your voice tinged with sarcasm.
You slouched into the couch, exhaling a breath you hadn’t realized you were holding. The day had been long, but the quiet hum of the apartment seemed to melt the tension from your body. You turned your head, and your gaze was immediately captured by Sae's piercing teal eyes, watching you with a calm intensity.
A strange warmth bloomed in your chest, fluttering like an unspoken secret between you. "So," you started, your voice laced with casual curiosity as you fought to push the feeling aside, "why did you willingly step into my apartment? Not exactly your usual scene."
He tilted his head slightly, his expression unreadable as always. "Why not? I was bored." Sae's reply was as nonchalant as ever, but the way he strolled over to join you on the couch betrayed a certain comfort in being here. He sank into the cushions beside you, letting out the faintest of sighs, as if your living room had somehow become his sanctuary. "Besides," he added after a beat, "it was pleasant hanging out with you. I wasn’t ready for that to end yet."
His words struck you harder than you cared to admit, and a maddening blush began to creep up your cheeks. You quickly turned your head, a small, nervous laugh escaping your lips as you scrambled to keep your composure. "So, you're saying I'm fun to be around, huh?" you teased lightly, hoping the playfulness would mask the sudden erratic rhythm of your heart.
For a moment, Sae’s face remained impassive, but then a subtle smile curved his lips—rare and fleeting, like a secret he allowed you to glimpse. "More or less," he said, his voice low but tinged with an undeniable warmth.
The silence that followed wasn’t uncomfortable. If anything, it felt charged, like the pause before a thunderstorm. You weren’t sure if it was the proximity, the way his knee almost brushed yours, or the way he looked at you as if he could see past every wall you’d carefully built.
"You’re full of surprises, Itoshi," you murmured, leaning back against the couch. The teasing edge in your voice was softer now, replaced by a quiet curiosity you couldn’t quite hide. "Never thought I’d hear you admit to enjoying anyone’s company."
He glanced at you, the corner of his mouth twitching as though considering whether to respond. Then, without warning, he leaned forward, elbows resting on his knees, his eyes locked onto yours.
"Maybe you’re an exception," he said simply.
The words hung in the air between you, heavy with implications you weren’t sure either of you were ready to unpack. Your heart skipped a beat, and for once, you didn’t have a clever retort.
The faint sound of rain began to patter against the window, filling the silence. You turned your gaze toward it, your mind racing. "Exception, huh?" you finally murmured, trying to sound indifferent, though your voice betrayed the faintest waver.
He didn’t reply immediately, and when you dared to glance back at him, you found him watching you again, his expression softer now. "You don’t have to overthink it," he said, his tone a touch gentler than before. "I just… didn’t feel like being alone today."
Something in his admission made your chest tighten, but instead of pressing him further, you simply nodded. "Well," you said lightly, offering him a small smile, "good thing you’re here, then. I wasn’t planning on being alone either."
The rain continued its rhythmic melody, and as the evening stretched on, the distance between you seemed to shrink, both physically and emotionally. Neither of you said much, but in the quiet company of one another, there was a sense of understanding that didn’t need words.
The two of you sat in a comfortable silence, the hum of the television filling the air. You glanced over at Sae, wondering what was running through his mind. After a moment, you decided to break the quiet.
"So, Sae," you began, your voice trying to sound casual. "Do you want to do anything, or...? I imagine you’re probably getting bored by now."
His eyes met yours, his gaze unwavering. He looked... contemplative, as if he were lost in thought about something important, though he didn’t seem eager to share.
"I’m fine," he mumbled after a long pause, though his words didn't match the slight tension in his expression. It was clear there was something on his mind, something weighing him down, but he wasn’t ready to say what it was.
You nodded, respecting his silence, and leaned back into the couch, glancing out the window. The evening sky was a soft mix of dark colors, but your mind kept drifting back to him. The way his demeanor shifted, how he seemed a little distant.
After a second, you decided to try again, pushing past the silence. "So, tell me about your career," you asked, your voice gentle but curious. "What’s it like—"
Before you could finish, Sae’s hand shot out, and in one swift motion, he grasped your chin, gently but firmly, and tilted your face towards his.
Your breath caught in your throat, and your heart skipped a beat. You were so close, your eyes wide in shock as you stared at him, feeling his breath against your skin. The moment hung between you like a fragile thread. You were frozen, not sure what was happening or what had made him do this.
He stared into your eyes, his gaze flicking briefly to your lips before meeting your eyes once more. Every movement of his felt deliberate, almost like he was studying you, and you couldn’t look away. It was as if the world had paused around the two of you, the silence between you thickening with each passing second.
You felt your heart pounding in your chest, its rapid beat deafening in your ears. It was as though your entire body was on edge, strung taut with anticipation, and yet you couldn’t move. You were frozen, caught in the intensity of the moment.
Sae shifted his grip, his fingers tracing your jawline before he cupped your cheek, his thumb brushing gently beneath your eye. The touch was soft, almost tender.
And that’s when you saw it—love.
You almost flinched at the thought. His eyes were so focused, so soft, as if they were seeing you in a way no one ever had before. There was something vulnerable in the way he looked at you, something raw.
Love?
The word echoed in your mind, heavy and foreign. You hadn’t used that word in so long, not with anyone. And certainly not with him. It was difficult to fathom that someone like Sae—so guarded, so distant—could feel that way, could look at you like this.
The panic started to rise in your chest. If this was what he felt—love—then what did that mean for you? For this? You weren’t sure if you were ready to love again. Not like this, not so suddenly, and not with someone who seemed so far removed from the idea of it.
It felt as though the weight of the world was pressing down on you, immense and overwhelming. Would you let him love you like this? Could you let him?
More importantly, could you let yourself love him?
You weren’t ready. Every thought in your mind screamed for you to pull back, to protect yourself from whatever this was. What if Sae broke you? What if you let yourself fall into this and it all came crashing down, just like before? You didn’t want to be broken again. You didn’t want to be tossed aside, left alone to pick up the pieces of a love that wasn’t real.
It hurt. The weight of your own fears, of what could happen, felt suffocating. You didn’t know what to do, torn between wanting to return his feelings and the fear of what would happen if you did. You wanted so badly to let love consume you, to let him pull you in, but you couldn’t ignore the voice that warned you against it.
What if he was just using you?
You couldn’t risk it. The idea of being hurt again, of losing yourself in someone else only to be discarded, was too much to bear. But still, the desire to let go, to give in, lingered within you like a quiet ache. Were you really this hopeless? Pathetic, even?
Tears threatened to spill as you felt Sae’s palm still resting against your face, his touch a tender reminder of everything you wanted but couldn’t allow yourself to have. You tried to swallow the lump in your throat, but it was no use. The tears slowly began to fall, too overwhelming to hold back.
Sae’s eyes widened in surprise at the sight of you, but he didn’t pull away. Instead, his other hand moved to cup the other side of your face, his touch gentle and careful, as though he was afraid of breaking you, too.
With a softness that took you off guard, Sae wiped away the tears that slipped down your cheeks, his fingers brushing lightly against your skin. You didn’t know what to make of it. It was so different, so unexpected. No one had ever been this gentle, this affectionate with you before, not in the way Sae was. His touch felt like he was holding you together, not pulling you apart.
Sae’s gaze softened as he looked at you, his eyes full of something you couldn’t quite place—gentleness, sincerity, something that made your heart flutter in spite of the walls you had built. "Y/n," he whispered, his voice calm, almost tender. "Please don’t cry."
Quiet tears continued to fall, each one carrying the weight of everything you’d been holding back for so long. His thumb gently traced your reddened cheek, and his face leaned in closer, his presence both soothing and overwhelming. The warmth of his touch felt so different—so real.
"You don’t have to cry," he murmured again, his voice low and soft, carrying an unmistakable sense of care. "Y/n… I don’t know what happened for you to tear up like this, but I promise you… whatever happened in the past, I won’t replicate it." His words were sincere, the kind of promise that, for a brief moment, made the pain inside you seem a little more bearable.
For a split second, you searched his face, desperately trying to find any hint of insincerity, any trace of deception hidden beneath the calmness in his eyes. But there was nothing—nothing that suggested he was lying. His tone was steady, unyielding.
Could you trust him? Could you really let him in?
The vulnerability he was showing, the way he was looking at you, it warmed your heart in a way that felt so foreign. So safe. It was everything you didn’t know you needed, and yet it was right in front of you.
"You promise…?" Your voice was small, shaky, as the uncertainty you’d been carrying for so long finally slipped into your words.
Sae’s eyes softened even more, and he lowered his gaze slightly, as if he could feel the weight of what you were carrying, of the hesitation in your voice. He didn’t speak for a moment, just letting the silence stretch between you two, as if understanding how deep the scars of your past must have been.
Whatever had happened to you, whatever pain you’d endured before—it had clearly left a mark on you. A deep, unhealed wound that made it hard to trust, to let anyone close. Sae understood that, and for the first time, you saw that in his eyes: understanding, not judgment. Compassion, not pity.
"Yes," he finally said, his voice firm but gentle. "I promise."
The sincerity in his words felt like a lifeline, like the first breath of air after being submerged in water for too long. And in that moment, despite the storm of emotions inside you, you allowed yourself to believe him. Maybe you didn’t have all the answers, but you could take this one step.
You could let him in.
(Song recommendation: Im Yours - Isabel LaRosa)
Sae's smile softened at you, a warmth in his gaze that spoke more than his actions ever could. Then, without a word, he leaned in, slowly pressing his lips to yours. The kiss was soft at first, gentle as though testing the waters, but it quickly deepened as his hands moved to the side of your neck, holding you closer, grounding you in the moment.
Your hands instinctively moved to his chest, resting against the firm muscles you could feel even through his clothes. The warmth of his body against yours was intoxicating, and you couldn't help but be drawn further into him.
For a moment, Sae pulled away, just enough to catch his breath, but his eyes never left yours. And then, just as quickly, he recaptured your lips in his, this time more urgent, more insistent.
His tongue gently brushed across your lips, a silent request, and you gasped, heart racing at the intensity of it all. He took that moment to slip his tongue into your mouth, and it was like electricity sparked between you. His tongue moved against yours in a slow, deliberate dance, each movement an invitation to fall deeper into him, into this moment.
Everything else faded away. The world outside, the thoughts racing through your mind—none of it mattered now. All that existed was the heat between you two, the closeness that felt like it had been building for so long.
Sae groaned softly into your mouth, his hand threading gently through your hair, tugging just enough to send a shiver down your spine. There was hesitation in the movement, as though he was aware of the fine line between desire and discomfort, but the tension in his touch made your pulse race.
The gentle tug on your hair pulled you back slightly, causing your lips to break apart for a fleeting moment. But before you could gather your breath, Sae's lips were back on yours, this time with a bit more force, more urgency. The kiss deepened, and the pressure pushed you slightly back onto the couch. Sae didn’t hesitate—he used the shift in position to his advantage, quickly climbing over you, his body covering yours, pinning you gently but firmly to the soft cushions beneath.
His legs shifted, placing themselves outside of yours, trapping you in place with a controlled intensity that made your breath catch. His chest pressed against yours, the warmth of his body melding with yours as you felt his weight settle over you.
After a moment, Sae reluctantly detached his lips from yours, his breath coming shallow and quick. He gazed down at you, his eyes no longer just filled with tenderness or care. There was something new there. Something darker, deeper. Lust.
His voice was soft, almost hesitant, but there was an undeniable edge to it. "Y/n... would you let me?" he murmured, his gaze never leaving yours, his body still hovering over you, close enough that you could feel the heat radiating off of him.
A wave of emotion swelled within you, something foreign and stirring. Sae had asked for permission—something none of the others had ever done. Usually, it was a matter of taking what they wanted without a second thought, but not Sae. His consideration, his respect, made you pause. Maybe this was different. Maybe this could be different.
Your heart fluttered, a warm smile spreading across your face as you met his gaze. "Yes, Sae. I will."
Sae’s smile mirrored yours, soft and genuine, before he placed a tender kiss on your cheek—a silent thank you. There was an unspoken understanding between you now, a connection that was more than just physical. It felt like trust, like a promise he was making without words.
He stood, slipping off his blazer with a fluid motion, letting it fall carelessly to the floor. Then, without hesitation, he pulled off his shirt, revealing his toned, muscular chest. The sight made your breath catch. He was... built. Strong, defined—everything about him was a reflection of strength, of control.
Your eyes lingered on his body, taking in every detail. You could feel the heat rise in your cheeks as you tried to focus, your heart racing in your chest.
Sae noticed your reaction, a playful chuckle escaping his lips. His eyes twinkled with amusement, yet there was something more behind his gaze, something deeper.
"Don’t worry," he murmured, his voice low and soothing, yet filled with a hint of confidence. "It’s all yours, Y/n. You’re going to have to get used to it."
Your cheeks burned with a deep blush at his words, but before you could process it fully, his lips were back on yours, pulling you into the kiss with a hunger that matched your own.
As the kiss deepened, your hands instinctively trailed up the firmness of his abs, feeling him shiver beneath your touch. The sensation of his skin under your fingertips made your pulse quicken. Sae groaned into your mouth, his tongue seeking entrance, and this time, you didn’t hesitate—your lips parted, allowing him to deepen the kiss.
It was a kiss that was both aggressive and tender. Sae’s neediness was noticeable, desperate even, but there was a gentleness in his touch, a carefulness that kept the intensity from crossing into something too overwhelming. He was savoring the moment, as if he was afraid of breaking something fragile.
His hand moved to the collar of your shirt, his fingers pausing, hesitating just for a brief second. He broke the kiss, his gaze locking with yours, silently asking for permission.
A soft laugh escaped your lips at the look in his eyes—this was different, this was him. There was no pressure, no rush. Just the quiet, mutual understanding between you two.
You nodded, giving him the confirmation he needed, and without another word, Sae yanked your shirt off in one swift motion, tossing it carelessly to the side.
Now, with both of you half-dressed, skin brushing against skin, the weight of the moment settled around you. Sae’s chest pressed against yours, his heartbeat as erratic as yours. The closeness was dizzying, but it felt right.
You shifted, slowly leaning up as you looked into his eyes, silently acknowledging what was next and what he wanted. Sae's gaze flickered down to you, a silent question in his eyes, asking if you were ready.
You nodded. Sae's hands trembled slightly as he reached behind you to unclasp your bra, the lacy garment falling away to reveal your perfect, plump breasts. His gaze raked over your exposed skin, drinking in every inch of you as he felt a familiar heat building low in his belly.
"Fuck, Y/N..." Sae breathed, his voice rough with desire. "You're so perfect."
He leaned down, his chest pressing against yours as he claimed your mouth in a bruising kiss. It was hungry and desperate, as if you were the only thing keeping him chained to this earth.
One large hand came up to cup your breast, thumbing over your nipple almost earnestly. Although being gentle, there was nothing gentle about the way he wanted to touched you - he wanted to possess you, to mark you as his and his alone.
A low groan escaped your lips at his touch, and Sae's cock twitched eagerly in response. The sound of your pleasure was like music to his ears, spurring him on.
Sae's hands continued their sensual massage of your breasts, thumbs circling your nipples until they pebbled beneath his touch. Each stroke of his fingers sent sparks of pleasure racing through your veins, stoking the fire building between your thighs.
Breaking away from your lips, Sae latched onto the smooth column of your throat, his mouth hot and demanding against your skin. He sucked and nipped, leaving a trail of marks in his wake as he made his way lower.
When he reached your breast, Sae took your nipple into his mouth, tongue swirling around the sensitive bud. He suckled greedily, the wet sound obscenely loud in the quiet room. Your back arched off the couch, a needy moan spilling from your lips.
He pulled off with a lewd pop, smirking up at you with pure, unadulterated lust. But there was something else in his eyes too - a tenderness, an adoration that made your heart skip a beat.
This time, you met his gaze head-on, not looking away. Because despite everything, despite the scars on your soul, you knew you were safe with him. Cherished.
Sae's smile widened as he took in the sight of you - flushed and panting, your body laid bare before him. He had done this, reduced you to a needy, senseless mess with just his hands and mouth.
"Look at you," he purred, fingers dancing along the hem of your pants. "So beautiful like this.”
He glanced up at you, seeking permission even in the heat of the moment. That was Sae - always making sure you were okay, that you wanted this as much as he did.
"Please," you breathed, lifting your hips in silent offering.
Something dark and possessive flashed in Sae's eyes as he slowly unbuttoned your pants, dragging the zipper down with agonizing leisure. He peeled the fabric away, leaving you clad in nothing but panties.
A noticeable dampness revealed your growing arousal, drawing Sae's attention. His breath hitched, his jaw tightening. An irresistible urge surged within him—he needed you.
Sae tossed your panties aside carelessly, leaving you completely exposed and vulnerable beneath his intense gaze. Every inch of your bare skin was on display for him, a feast for his hungry eyes.
Bending lower, he nuzzled into your inner thighs, kissing and licking a path towards your core. You trembled beneath him, hands fisting in the fabric as he inched closer to where you needed him most.
Your body jerked at the contact, instinctively trying to close your legs. But Sae's strong hands on your hips held you open, keeping you spread wide for his ministrations.
"Open for me, Y/N," he commanded, his voice a heady mix of sternness and care.
Obediently, you let your thighs fall open, granting him unrestricted access to your most intimate places. Sae grunted approvingly as he took in the glistening pink of your aroused sex.
Gripping your knees, he pushed your legs back and apart, forcing you into a position of total surrender. The new angle had your entrance on full display.
"So gorgeous, Y/n,” he murmured appreciatively. "And all mine."
Slowly, teasingly, he slid a single finger into your dripping core. Your back arched off the couch as pleasure sparked through you, a needy moan spilling from your lips.
Sae crashed his mouth to yours, swallowing your moans as he fingered you with increasing intensity. Your velvety walls gripped him like a depravity, fluttering and clenching around his plunging fingers.
"You're so tight," he grunted against your lips. “I love it. You’re so good to me Y/n.”
He curled them just right, rubbing mercilessly against that sensitive bundle of nerves deep inside you. Your hips bucked wildly, seeking more of that friction, chasing the pleasure only he could give you.
Sae obliged, plunging his fingers faster, harder, driving into your soaked heat with relentless precision. Lewd squelching noises filled the air as he fucked you with his hand, the vulgar sounds spurring him on.
"That's it, Y/n," he groaned roughly. " ‘m gonna make you feel good.”
He could feel you tightening, your inner muscles starting to flutter and ripple around him. Your moans grew higher, needier, and Sae knew you were close.
Sae's fingers stilled as he felt your walls start to quaver, signaling your impending orgasm. He slowly withdrew his hand, denying you that release.
Your eyes fluttered open, hazy with need and confusion. "Sae? Why did you stop?" you murmured breathlessly.
He smirked down at you, his voice low and commanding. "Not yet, Y/N. I want to feel you come undone on my cock."
With quick movements, Sae unbuckled his belt and shoved his pants down, kicking them off impatiently. He stood before you, clad only in a pair of straining boxer briefs. The sizeable bulge at the front left no doubt as to his arousal.
You sat up slowly, eyes widening as you drank in the sight of his powerful body. Sae's smirk widened at your reaction. He grabbed your hips, pulling you flush against him as he guided your hands to the waistband of his underwear.
"Pull them down for me, Y/N," he ordered, his tone leaving no room for argument.
Trembling with anticipation, you hooked your fingers under the elastic and slowly dragged the fabric down.
Your eyes widened as Sae's impressive length sprang free, bobbing mere inches from your face. It was thick and heavy, the bulbous head already glistening with precum. A thrill of excitement mixed with nervousness raced down your spine. Could you really take all of that?
As if sensing your hesitation, Sae cupped your cheek, his thumb brushing over your bottom lip. "Don't worry, Y/n. You can handle it," he reassured, his voice a low rumble. "I'll start slow, ease you into it.”
He pushed you back onto the couch, his larger body covering yours. You felt trapped beneath him, pinned in place by his solid weight. Sae reached between your bodies, grasping his throbbing cock and giving it a few slow strokes.
Then, with agonizing leisure, he placed the tip against your entrance. You held your breath, every muscle tensing in anticipation. This was really happening.
"Tell me when, Y/N," Sae murmured against your ear, his hot breath sending shivers down your spine. "Remember, I'm yours. You're in control here."
He sealed his lips over yours in a long kiss, his tongue delving deep inside. You moaned into his mouth, your hands fisting in his hair as you lost yourself to the sensation.
When he finally pulled back, you were both panting harshly. Sae's eyes bore into yours, dark with desire but also filled with a tender understanding. He would follow your lead, let you set the pace.
All you had to do was say the word.
“Make me feel good, Sae," you breathed against his lips, pulling him in for a quick, heated kiss.
"Of course. Anything for you," he murmured back, a small smirk playing on his lips.
Sae's tip nudged against your entrance, teasing you. You squirmed beneath him, aching to be filled. His large hands gripped your hips, holding you steady as he slowly pressed forward.
"If you need me to pause at any point, just say the word," Sae reassured, his voice low and soothing. "You can tell me anything, and I'll do it. This is all about you, Y/N."
You nodded, trusting him. Then, with a slow, deliberate push, Sae sheathed himself inside you. A low groan rumbled from his chest as your velvety walls stretched to adjust his girth.
He gave you a moment to adjust, peppering kisses along your jaw and neck as he waited patiently. When he started to move, it was with shallow, careful thrusts. Each roll of his hips sent sparks of pleasure shooting through your core.
Sae's breath came in ragged pants as he pounded into you, his brow glistening with sweat. Each thrust drew a groan from his lips, especially when your walls clenched around his throbbing shaft.
"Fuck, Y/N... so tight," he grunted, his pace growing more erratic. "Feels…amazing”.
You could only moan in response, your head thrashing on the fabric of the couch as he hit that perfect spot inside you over and over. The wet slap of skin on skin filled the room.
"S-Sae," you gasped out, wrapping your legs around his waist.
His name coming from your lips made him eager, slamming into you with ease. The new angle had him nailing your G-spot with overwhelming precision, sending bolts of electric pleasure zinging through your nerve endings.
Sae's breath came in harsh, ragged pants as he pounded into you, chasing his rapidly approaching climax. The way your walls clenched around his throbbing shaft, the sting of your nails scratching his back, the breathy cries of his name falling from your lips - it was all driving him wild with lust.
"S-Sae..." you stammered out, your voice high and needy. "I'm so close..."
He could see it in the glazed look of your eyes, feel it in the way your body was starting to tremble and tighten around him. Sae knew he wouldn't last much longer either.
"Me too, Y/n," he grunted, his movements growing sloppy and erratic.
With a final, powerful thrust, he buried himself to the edge, grinding against your G-spot. At the same time, he reached between your bodies to circle your swollen clit with his fingers.
Sae let out a low, satisfied groan as he felt your warm essence dripping down his softening cock. With a final, shallow thrust, he pulled out completely, shooting his load onto your lower abdomen.
Exhausted, he collapsed on top of you, nuzzling his face between your breasts. His arms wrapped around your waist, holding you close as he caught his breath. You both lay there in the afterglow, the only sound the soft panting and huffing filling the room.
No words were spoken for a long moment, the silence comfortable and intimate. You gently ran your fingers through Sae's hair, massaging his scalp soothingly. He let out a contented hum, burrowing further into your embrace.
“Sae..." you murmured softly, breaking the quiet.
"Hm?" he mumbled, his voice slightly muffled by your skin.
You bit your lip, suddenly feeling vulnerable. "Everything you said... did you mean it? About me being yours, and you wanting to take care of me and make me feel good?"
The words tumbled out in a rush, tinged with uncertainty. In the heat of passion, it had all seemed so real, so intense. But now, in the calm aftermath, doubt began to creep in.
Was it just dirty talk, empty promises made in the act of lust? Or had Sae truly meant every word, genuine in his desire to cherish and care for you?
You needed to hear him say it again, unclouded by the haze of sex. You had to know if this was something real, something that could grow into more than just a physical connection.
You held your breath, waiting for his response, your heart fluttering with a mixture of hope and fear.
Sae lifted his head from the plush of your breasts, his teal eyes locking onto yours with an intensity that stole your breath. "I meant every word, Y/N," he murmured, his voice low and earnest. "I'll take care of you, I promise."
A small, shy smile tugged at the corners of your lips, hope blooming in your chest. Sae's hand cupped your cheek, his thumb brushing tenderly over your cheekbone.
"I like you, Y/N. More than you know. Maybe even love,” he confessed, his gaze never wavering. "These past two months, spending every day with you at the bakery... I've fallen for you. Hard."
He let out a soft chuckle. "To be honest, you're the only reason I keep going there. Just to see you, to be near you, even if it's only for a few minutes."
Your heart swelled at his words, a warm sensation flowing through your entire being. This was everything you'd secretly hoped for, dreamed of, but never dared to believe could be real.
Until now.
Leaning into his touch, you let yourself get lost in the depths of Sae's eyes, seeing the sincerity and affection shining there. In that moment, you knew with absolute certainty what you wanted, what your heart craved.
You wanted this. You wanted him.
The walls you'd built around yourself, the barriers you'd made to keep people out and protect your fragile heart... they crumbled to dust, swept away by the force of your feelings for this incredible man.
Now, it was time to let him in, to entrust him with your heart and let yourself be loved in return. No more holding back, no more running from what you truly desired.
"Sae..." you whispered, your voice trembling with emotion. "I... I think I'm falling for you too. I want this, I want you. I'm ready to let you in.”
You gazed up at Sae, your heart swelling with a love so profound it threatened to burst from your chest. In his warm teal eyes, you saw a reflection of everything you'd ever wanted, everything you'd been searching for all these years.
Comfort. Affection. Devotion. Love.
With Sae, you felt safe, cherished, whole. Like all the broken, jagged pieces of your soul had finally clicked into place, forming a beautiful painting of love and trust.
"Let me be in your life, Y/N," Sae murmured, his voice raw with emotion. "Let me love you, the way you deserve to be loved."
Tears pricked at the corners of your eyes, overwhelmed by the depth of his words. How had you gotten so lucky, to find someone who saw past your walls, your wounds, straight to the tender heart underneath?
"And I shall let you love me, as I will love you, Sae," you whispered, a radiant smile blooming on your face.
This was everything you'd ever wanted, everything you'd never dared to dream possible. A love that healed, that uplifted, that made you feel invincible.
With Sae by your side, you finally felt complete. Like you'd found your home, your haven, your happily ever after.
"I'm yours," you breathed, reaching up to cup his cheek. "Now and forever."
Sae surged forward, capturing your lips in a searing kiss that poured every ounce of his love, his commitment, into the press of his mouth on yours. You melted into him, losing yourself in the exquisite taste of his devotion.
In that perfect moment, the rest of the world fell away. There was only you, only him, only the infinite love binding your hearts and souls together.
Forever and always.
a/n: omg im so sorry this took so long I didnt expect it to take a while😭
Btw sorry if the ending is rushed and crappy I just wanted to end it since it was getting too long. Plus…he was a bit too ooc for me🙁
I was originally going to make two parts but somehow I didn't so it took longer to post!!! I'm so sorry!!!
I should've made this a wattpad instead…yo wait hold up⁉️ I should make a wattpad‼️
Regardless…SAE IS SO FINE WHAT. He looks so scrumptious in these new bllk episodes😫 (Rin’s better tho. THE BETTER BROTHER!)
Yum😋


#bllk#blue lock#writeblr#anime x reader#bllk x reader#fanfic#fanfiction#female reader#angst#blue lock x you#itoshi sae#sae itoshi#sae x reader#sae x you#sae blue lock#sae itoshi x reader#sae itoshi x you#sae itoshi x y/n#sae itoshi fluff#sae itoshi smut#itoshi brothers#bllk smut#smut#fem reader#x reader#fluff#slow burn#bllk x you#bllk slowburn#blue lock x reader
457 notes
·
View notes
Text
The Art of Submission (1)

[minors don't interact, 18+]
pairing: wanda maximoff x fem!reader
summary: As a growing author, you're grappling with a frustrating writer's block while trying to craft your next lesbian erotic novel. With a lack of personal experience holding you back, inspiration seems just out of reach. But when a captivating neighbour steps in, offering unexpected support and a tantalizing invitation to explore the depths of desire, you find yourself on a journey that blurs the lines between reality and fiction, leading to a discovery that you definitely weren't expecting.
content warnings: lead up, talk of submission and sadomasochism, flirty touches and conversation.
note: This is the first chapter of a new story that I'm writing, any ideas or inspiration would be appreciated so if you have any ideas feel free to drop them in my requests, other than that buckle in! (I will try to get the next part out as soon as possible)

The Art of Submission - Chapter One
The soft glow of your laptop illuminated the cluttered desk, your cursor blinking impatiently on an empty document. You stare aimlessly at the screen, your fingers hovering above the keys waiting desperately for inspiration to strike. It had been hours since you sat down, hoping to squeeze out something, but your mind felt trapped and foggy, yet every time you wrote a sentence, you only sank deeper into it. The end result had started to feel completely out of reach.
Your last book had done okay. It wasn’t groundbreaking or a bestseller, but it was just enough to remind you that you could do this. You could write and publish your writing and make some level of a name for yourself in the world of lesbian erotica. Not that it was hard considering the low level media attention that your field rarely gained. The reviews had been mostly kind and the sales had trickled in steadily enough that you were managing to stay afloat, but nowhere near the level of success that you first imagined when you wrote your first novel.
Your apartment is a mess, the evidence of your creative block scattered pointlessly across the room. Empty coffee mugs crowded your desk, some still holding the cold remnants of yesterday's caffeine-fueled desperation. You’d also not left the apartment in days, time becoming a blur of restless nights and sluggish mornings, avoiding stepping outside. You found it was easier to stay here, trapped within the confines of your own thoughts, hoping something would come to you.
You lean back in your chair, groaning in frustration. You thought about getting up and attacking the massive pile of laundry that had sat abandoned in the corner for days, but you quickly pushed that aside, realising that there was no point until you at least got another page written. The cursor was blinking furiously at you and you felt yourself going slightly insane. You wanted to smash your head into the keyboard, but instead you imagined yourself doing it which brought a small smile to your lips.
It was at this moment that a sharp knock sounded at the door, you spin in your chair, frowning as you try to glance over at the entrance to the apartment. You wracked your brain trying to remember if you’d ordered something, but you couldn’t work it out and you knew you definitely wasn’t expecting company. You push yourself out of the chair with a deflated sigh, stretching your legs out as you go towards the door. The knock came again, firmer this time. Whoever it was, they weren’t planning on leaving.
Shuffling to the door, you don’t bother to smooth the wisps of your hair or fix the crumples in your shift, you just swung it open.
“Hey, I hope I’m not intruding, but I thought you could use a break.”
You blink in shock, momentarily stunned. Wanda stood in your doorway, her familiar yet distant neighbour from across the hall. You knew her as the woman who you occasionally exchange small talk with in the corridor, but there she was holding a bottle of wine like she’d been planning this all along. Her reddish-brown hair flowed over her shoulders, perfectly catching the dimming light of the room, the colours of her striped blouse almost too cheerful for the cluttered mess that she would soon walk into.
“I can basically hear your sighs from across the wall. Writer's block?” Wanda smiled, her green eyes warm but with a hint of darkness behind them, as if she knew something that you didn’t. She stepped further inside, her presence filling the small apartment yet you didn’t move to stop her, you didn’t feel the need to.
“Yeah no of course, come on in.” You say, brows furrowed in confusion. You hadn’t told anyone that you were trying to write again, come to think of it, you hadn’t even told her that you were a writer in the first place. Suddenly, your cheeks flushed pink in the realisation that she knew who you were.
Wanda set the bottle down on the counter, next to a half empty cup. The sound of it landing felt louder than it should, cutting through the quiet tension that was arising around the pair of them.
“You’ve been in here too long, I thought wine might be a good excuse to step away from the screen for a bit.” Wanda spoke with a caring tone beneath her soft voice, yet you found it unsettling in how she acted so naturally, offering up solutions to problems that you hadn’t even told her about.
Wanda always seemed to have a way of appearing when you least expected it, offering little moments of relief, like that time she helped carry groceries up the stairs. She was friendly, sure, but there was an edge to her friendliness. A knowing look, like she was always a step ahead of you, just waiting for the right moment to weave her way into your life. You didn’t know why, but you weren’t exactly complaining about it.
“You know, I’ve read some of your stuff.” There it was, you freeze, your heart skipping a beat. Your eyes dart to Wanda’s face, as if you were searching for any hint of a joke but instead you’re met with a calm, confident smile. That wasn’t what you were expecting. You’d always presumed that your audience was horny teenage girls, but Wanda was a mind-blowingly gorgeous woman, the exact opposite of who she was expecting. Besides that, your books lived in a cosy corner of the erotic fiction world, usually flying under the radar, definitely not the type of thing a neighbour casually brings up over wine.
“You have?” You ask, trying to sound casual but your voice comes out a little more strained than intended. You walk around the kitchen counter where Wanda had perched herself, your hands almost shaking from the unexpected social encounter. You reach into the cupboard, finding two wine glasses and placing them down between the two of you.
“Mhm.” Wanda leans against the counter, an almost playful spark in her eye, “You’re good. The way you write about submission, it’s real, raw. It’s incredible.”
You feel your cheeks warm up, unsure on how to respond. This was the first piece of praise you’d received from inside your own kitchen. You felt your pulse quicken, the fact that Wanda had read those words, the intimate fantasies that you’d put into your stories was making this situation way more intimate than deemed necessary.
You literally were stuck in a state of speechlessness, but Wanda was acting like she expected this. She lets you stand with your back against the counter opposite her, fiddling with the ends of your hair while she pulls up a stool. “Corkscrew?”
“Oh yeah, of course.” As you turned you wanted to slap yourself, why were no words coming out, you are absolutely embarrassing yourself, yet the redhead was still gleaming at you as if you were adding something to the interaction. You rummage through your drawers to find what you needed before handing it over to her.
“You know, when I first picked up one of your books I wasn’t sure what to expect.” She chuckled, tilting her head thoughtfully as she worked on opening up the bottle. “But then, well, I couldn’t put it down. Dangerous stuff.”
This time you manage a small laugh, still processing the idea of Wanda - the beautiful and put-together woman from across the hall - curled up reading the things you’d written. “I guess it’s not what most people expect from their neighbours.” Once again you’d tried so hard to sound casual that your voice was wavering in response.
“Well maybe we just don’t know our neighbours as well as we think we do.” With that, she pulled the cork from the bottle and filled up the two glasses, leaning in a little closer as a smile grew into a smirk.
You glance down at her as you reach for the glass, “I never really imagined someone like you reading my books you know.” You say sheepishly, taking a sip of the wine hoping to mask the nerves that were creeping up your spine.
Wanda raises an eyebrow, her smirk more prominent now. “Someone like me?”
You shrug, avoiding her gaze as you fiddle with the stem of your glass. “You know, my audience is usually different. Younger maybe.”
She chuckles softly at your response, “Are you saying I’m too old for erotic fiction?” Her tone is teasing, yet there's a glint in her eye that makes your palms sweat. Her comment about submission still lingers in the air, your cheeks continually growing warmer.
“No! No, I just-” You stammer, flustered by how casually she was controlling this conversation, “I didn’t think you’d be into, you know, that kind of thing.” Your voice is desperately pathetic and all you can do is smile shyly, trying to lighten the tension that was twisting in your chest.
Wanda takes a slow slip from her glass, her eyes never once leaving yours. “Don’t assume you know what I’m into,” she comments, voice soft but full of unspoken meaning. There's that look again, the one that says she knows more than she lets on. “But seriously, I thought your writing was refreshing. You don’t hold back and that's what makes it compelling.”
You feel the blush rise again, her praise catching you off guard. “Thanks, I guess.” You mumble, feeling a little more exposed than you’d like.
She waves a hand in the air, brushing off the awkwardness as she crosses her leg over the other. “I could tell you were stuck though,” She adds, swiftly changing the topic with a casual flick of her wrist. “So I figured I’d rescue you from yourself for a bit.”
It was your turn to raise an eyebrow, “Rescue me?”
She nods, her eyes twinkling. “I’ve been hearing you pace around for days, It’s not hard to guess you’ve got yourself into a block.”
You can’t help but laugh, the conversation switching to something that was making you more comfortable to talk about. “Yeah, something like that. I’ve been staring at that god stupid screen for hours.”
Wanda shakes her head, mock disapproval on her face. “That’s no way to get inspired, sometimes you just need to step away.” She gestures to the wine and the dim, cosy lighting of the room. “This is your moment to relax.”
You take a deep breath, feeling the weight on your chest lighten ever so slightly. “I guess I have been driving myself crazy.” This would usually be an overstep in a first proper conversation, but the curious look behind Wanda’s eyes made you feel like she was making you say all of this, like she was dragging the vulnerability out of you.
Wanda smiles at your openness, a knowing, almost secretive smile as she lifts her glass to her lips again. “There's a reason they say inspiration strikes when you least expect it, maybe you just need to stop expecting it.”
The laughs were more relaxed now, “Oh, is that how it works?” You tease playfully, finally getting to a point where your nerves have stilled out. You could feel the tension in your body loosen just a little, but Wanda’s gaze still never faded.
She grins at your response, swirling the wine around in her glass. “Well sometimes it helps to just let go.” Her eyes sparkling as she watches you. “So what’s this book about anyway? What's got your pretty little head in a spin?”
You hesitate for a moment, unsure how to respond. There's no easy way to explain what you’re writing without dipping into something personal and intimate. But the way Wanda is watching you so intently, waiting, you decide to just go for it. You’re thinking maybe talking about it will help you sort out what’s been blocking you.
You clear your throat, and look down at the glass in your hands. It’s, uh well, it's another one in the same genre as the others.”
Wanda cocks her head at you, leaning in again. “Mhm, go on.” She pulls out the stool next to her, tapping on the top of it. You smile in the safeness of her space, walking round the counter and sitting down next to her.
“It’s about sadomasochism actually. I’m trying to explore that dynamic, the balance between pleasure and pain, trust and submission.” You feel your face flush, realising that there's no backing out now. This is supported by Wanda’s lips curling into an all too well knowing smile.
“So you’re digging into the darker side of submission? That’s bold.”
You nod, your voice barely above a whisper. “Yeah it’s more about the psychological aspect of it - how it feels to surrender completely to someone else but it's hard to get it to feel real rather than just something for someone to get off on.”
There's a brief pause, both of you deep in thought, but you can feel Wanda’s gaze like a weight on your skin. Her eyes darken, just for a moment, as she processes your words. “Sounds intense.” She murmurs, her voice dropping a little lower.
You let out a nervous laugh, trying to break the tension that you’d created. “Yeah well it’s not exactly an easy thing to write about. I want to portray it with respect.”
The redhead has now turned in her chair to face you completely head on, her head tilted as she rolls her lips together. “Maybe that’s because you’re overthinking it.” She pauses, then adds, almost as an afterthought, “Or maybe because you haven’t experienced it enough yourself.”
Your breath catches in your throat at her suggestion and you can’t hold her stare anymore, quickly glancing away with a small cough. “I- Well I’ve written about it plenty.”
She chuckles gently at your answer, her tone life but her words heavy with meaning. “It’s not quite the same thing though is it?” Wanda’s fingers gently brush against yours as she reaches for the wine bottle to refill her glass. The touch is light, fleeting, but she doesn’t pull her hand away immediately. Instead her fingers linger just long enough to make you wonder if it was an accident or something more deliberate.
You attempt to laugh it off, but your voice falters slightly. “I guess not.”
She meets your eyes again, her gaze almost daring, “You know, sometimes the best way to get through the writer's block is to immerse yourself in the subject matter.”
You swallow hard, praying that she didn’t hear the gulp that erupted in the back of your throat. The air between you had grown thicker than before. “Yeah I’ve heard that before.”
She smiles, leaning just a little closer, her arm brushing against yours as she picks up her glass. “So what’s tripping you up? The emotional stuff, or you know the physical details.”
The way she’s looking at you, so calm yet so confident. It’s like she’s pulling the words out of you without you even realising it. “Both. It’s hard to get the balance right, making the dynamic feel believable.”
Wanda nods thoughtfully, biting the tip of her finger as she indulges herself into your problem. “Have you thought about how you’re building the dynamic between them?” She shifts closer and in the process her knee scrapes past yours under the lip of the counter top. You’re hyper aware of every small movement now and it's impossible to be an accident. “Like what does submission look like to you? What does it feel like in the story?”
You blink, caught off guard by the directness of her question. “God, I don’t know, It's like surrender, like when you trust someone enough to give them complete control.” You pick up your glass again, taking a massive chug in order to keep your hands steady. “It’s like you know they won’t hurt you, even when you’re in your most vulnerable state.”
She nods understandingly, leaning ever so slightly closer to you. “Okay so what does that look like physically, how are you going to write that?”
Your pulse is going crazy now, you’re convinced that Wanda can hear your heartbeat quicken from just her words. “It’s about touch,” You say, your voice almost wobbling, “The way they respond to each other. The way a person can take control with just a look or a gesture.”
As you speak, Wanda’s lips turn up into a smirk, her gaze still unwavering. She’s so close to you now that the warmth of her body is radiating off of your skin. Her hand rests slightly above your knee, the touch intimate, sending a shockwave up the back of your spine. “Show me.”
Your breath hitches, heart racing as her fingers begin to trace a small circle against your leg. The motion is almost absentminded, yet it feels nothing but deliberate. She maintains her eye contact, her expression open but charged with a spark of something playful and dangerously enticing.
You freeze, caught in a whirlwind of sensations as the room feels smaller now, the air thick with unspoken tension. You know exactly what she’s suggesting without her having to say it.
You open your mouth to respond, but immediately close it, earning a small chuckle from the redhead. “If you can describe it so well, you shouldn’t be stuck here right.” The dangerousness in her tone makes the words evaporate and you become acutely aware of the heat radiating from her body, the way her thumb brushes softly against your skin, drawing you in deeper.
Wanda pulls back just slightly, but her hand lingers where it is, a gentle weight that feels both reassuring and electric. Her eyes lock back with yours, searching, waiting for your answer. “It’s okay.” She whispers, her voice soft yet commanding, as if she's completely in control in this delicate moment, “I’m just trying to help you get… unstuck.”
You can’t look away from her, caught in her captivating gaze. Her confidence is wrapping itself around you, urging you to step closer to the edge of your own desires. The space between you is charged, the possibilities suddenly hanging thick in the air as you contemplate what she could do next.
“Have you thought about drawing from your own experiences?” Wanda questions, still attempting to find a solution to a problem you couldn’t tell whether she was actively helping or not. “You know, sometimes personal stories can ignite that spark of inspiration.”
You swallow hard, feeling a mix of excitement and apprehension. “I wish I could.” You admit, your pulse is still racing from her touch that she has now released, yet her body still remains just as close. “I’ve never really had anything that intimate.”
A playful glint flickered within the green of her eyes, her gaze sharpening. “Really? Nothing? Not even a fleeting moment that made your heart race?” She tilts her head slightly, studying your face as if searching for unspoken truths buried inside of you.
You shake your head, feeling the embarrassment paint itself across your face. “Not like that, I mean I’ve had relationships, but nothing that’s ever made me feel like I was completely out of control, everythings always felt so safe.”
“Safe can be good, but isn’t there something thrilling about stepping outside of your comfort zone?” Her face leans closer to you once more, the feeling of her leg permanently resting against yours now.
You nod, the thought resonating with you, but you’re still hesitant. “I just don’t know how to write something so raw and believable if I haven’t experienced it myself.”
Her expression softens, shifting her weight slightly. Her gaze drops to your lips for the briefest moment before locking back onto your eyes. “Kiss me,” She whispers, the command both shocking and exhilarating.
Your heart races, a jolt of electricity coursing through you at her words. You can’t look away, caught in the depths of her stare. The space between you feels impossibly small, filled with a tension that pulses with possibility. “Just one kiss,” She adds, her voice a sultry invitation. “It might just unlock everything you’ve been trying to write.”
With her eyes gleaming into yours, the world around you fades into the background leaning only the two of you in this moment. You’re drawn to her, every instinct telling you to surrender to the rush of desire coursing through your veins. You lean in, heart racing as you connect your lips together. The kiss is soft at first, a small tentative exploration, but it quickly deepens, igniting something almost primal within you. Wanda’s hand slides from your knee to the back of your neck, pulling you closer as if she wants to consume every part of you. You pull back, the softness of her lips still lingering against yours. You’re panting slightly, taking in the depths of what you just happened.
Wanda’s eyes gleam with satisfaction, her finger touching her lip and you can’t help but smile widely at her. “See.” She murmurs, her tone low and teasing. “Just a taste of what it feels like to let go.”
#wanda maximoff#mommy wanda#wanda maximoff x reader#wanda x reader#wanda#wanda maximoff x you#wanda maximoff x female reader#wanda maximoff fanfiction#wanda fanfic#wanda maximoff smut#wanda x you#marvel#mcu#wanda marvel#dom!wanda#lesbian#writing#wlw#wlw smut#bottom reader#x reader#wanda mcu#wanda smut
551 notes
·
View notes
Text
Welcome to the MCYT Longfic Database Project
Hello!! My name is Jim ( @rocketships07 , he/him), and I'm just a guy with a passion for data analysis and cubitos. I have been compiling, for a few months now, a small google sheets file of my favorite mcyt longfics, because I enjoy being able to see some stats and have everything in a place I can access. However! It ocurred to me that it would be very fun to develop a much larger database so that I could share it with friends!
So, the MCYT Longfic Database Project was born.
IMPORTANT LINKS:
MCYT Longfic Database SUBMISSIONS Form
Publishing site voting (closed)
FAQ
MCYT Longfic Database
Here's how it's going to work.
1. Interest Check (due: jan. 27)
I'm going to first compile information on what fandoms most people want me to compile fics of. This can be any MCYT fandom! As long as someone requests it, it'll have a place in the database. To do so, please send me asks through my tumblr page with your fandom(s)!!
CURRENT FANDOMS ADDED:
Hermitcraft
Traffic Life Series
Empires SMP
Dream SMP
QSMP
Scott's Life series (X life/Afterlife/New life)
POW Creations (Pirates SMP, Rats SMP 1&2)
The Realm
Fable SMP
Life Steal
Outsiders
Yogscast
2. Fanfic submission form is released (jan. 27 - feb. 28)
I will be releasing a form, where you can submit your favorite longfics! This form will include plenty of different sections for you to fill, such as title, fandom, word count, main character(s), ship (or ships), main tropes or au, amongst other categories with the purpose of data analysis! Mainly because the database will also have an analysis tab, where you can see some fun stats about the database!
During this period, the database will not be public. This is due to the fact that Google Forms does not format the information correctly, and I will be creating a much easier to read file for everyone to see!
After the end of this period, the forms will continue to be open! I will not be updating it constantly after that, but I'll try my best to keep it updated!
3. Database publishing (march 1)
After March 1st, the database will go live!!! I will continue to update it and add fics as long as people keep submitting them.
Feel free to share it with your friends and use it to find new fun fics to enjoy!
#mcytlongficdatabase#ao3 fanfic#mcytblr#empires smp#hermitcraft#dream smp#life series#jimmy solidarity#grian#goodtimeswithscar#mumbo jumbo#scott smajor#geminitay
246 notes
·
View notes
Note
Inspired by the moment in ACOSF when it’s mentioned Cassian likes physical contact. A fic where reader and cassian are besties and hanging all touchy, maybe reader is braiding his hair and the mating bond snaps.
Kindly requested to be tagged if written/published.
𝐬𝐩𝐢𝐭𝐞𝐟𝐮𝐥, 𝐰𝐢𝐜𝐤𝐞𝐝 𝐦𝐚𝐭𝐞
pairing; cassian x fem!reader
warnings; porn with plot, basically just smut tbh but smut with FEELS (the best kind), p in v, oral (f!receiving), cassian is a sexy bitch
word count; 2.4k
a/n; dooo we want a p2 (and to find out what reader has planned...) i'm planning one in my head so if you guys are interested please let me know! @bxm-1012 enjoy!
Cassian shows love through touch- whether that be an affectionate squeeze, a kiss on the forehead or a playful shove; it's how he expresses love for the people around him.
You often take the brunt of this, being his best friend. You walk the streets of Velaris arm in arm, squeeze into one armchair that really isn't built to hold even Cassian alone, but somehow manages to fit the both of you, fall asleep on top of each other in a heap of skewed limbs after hours of partying and drinking and dancing at Rita's. You fit together like two pieces of a puzzle.
You're really not sure how you didn't see it earlier.
You're lounging in the aforementioned armchair when the bond snaps. Your legs are thrown over the arm and Cassian is settled in the centre, head to your chest as you scratch and tug at his shoulder-length hair, pulling it up into a braid. He tilts his head up, grinning at you through the dark lashes framing his eyes, and the whole world shifts on its axis.
Something stirs to life inside of you, a warmth blooming and spreading and seeping into your every pore; you can feel the way you're tethered to him, the gravitational pull between you.
You go stock still and your lips part in a silent gasp. Cassian's grin grows tenfold.
"You knew?"
"I suspected," he murmurs. He twists his body to face you. "I hoped."
"Oh," you breathe. You can't help it when your hand comes up to trace his cheekbones, the tip of your thumb skimming the bridge of his nose. His eyes fall closed and the bastard tugs on the bond so hard it emits a squeal from you, and you're pressing a palm to the centre of your chest to soothe the entirely unfamiliar feeling.
His mouth opens to break the silence but you're already moving, careening into his chest and burrowing yourself in tight. Your body sags with pure, uninhibited relief.
"You feel the same, then?" he teases.
Your eyes are glassy when you peel your face far enough to meet his stare.
"I always thought I'd have to make peace with it when you found your mate. I'd have to settle for loving you from a distance and that would be enough. As long as you're happy, I'm happy." He softens at the admission- your voice rasping and raw as you lay your feelings bare for him- hooking an arm beneath your own to drag you up his chest until you're nose to nose. "But I guess I can be selfish now, and keep you to myself," you whisper.
"Mm," he purrs, and the sound turns your core molten. "I like the sound of that."
He doesn't waste any more time before his mouth is on yours, lips slanting hungrily over your own; you part your lips in submission, granting him access to lick into your mouth, his tongue tangling with your own. He rises to tower over you until you're flattened against the curve of the chair, and plants his hands either side of your head to cage you in. His wings flare where they'd been previously tucked against his back. Your body goes involuntarily soft and pliable, heat prickling under your skin at his every touch. Instinct takes over- it's as if it's muscle memory. Giving yourself to him is as easy as breathing.
Your head swims at the feel of his body under your roaming hands, his scent that seems to shift from affection to something deeply primal and dominating. You urge him closer with a whine and a pathetic tug at his t-shirt. How has this man reduced you to a mess with no more than a kiss?
"Cass-" you gasp when his head turns and his mouth latches onto the sensitive spot beneath your ear; teeth sink into flesh and you have to bite your lip to conceal a wanton moan. "We-we should go somewhere... more private."
"Oh, don't stop on our account," comes Rhysand's amused drawl through the closed door. "We're vacating the premises as we speak."
A growl rips through Cassian and searing, unyielding need barrels to your core and pools there; it takes every ounce of willpower to not rut your hips against him and demand his clothes off that very instant.
"Sorry!" you squeak; as quickly as the word leaves your mouth, Cassian's smothering it with another eager kiss. You lose any semblance of control you were clinging to, a moan dragging its way from your chest and into his waiting mouth. A string of saliva stretches and bows between you when he lifts his head to look at your face.
"My mate," he purrs. "My beautiful mate."
Your eyes cloud when you gaze at him through half-lids, reaching down to grab the thick length of him and squeeze. His hips grind into your palm, something deep and almost terrifying loosing from the depths of his chest. It only serves to make your cunt drool.
"Wicked thing," he gasps. "Spiteful female."
You grin, wide and unabashed, before your hands grapple for purchase to tear at his clothes until his toned abdomen is revealed to you; you want to lick every inch of him.
"Desperate little creature, aren’t you?" he teases.
"Shut up!"
His eyes roll when you at last wrench his pants and underwear down his thick thighs, freeing his cock, hard and weeping and begging for your touch.
"Who’s desperate now?" Your brow quirks.
He echoes your sentiments, cadence deep and gravelly with lust. "Shut up."
Your snarking comments seem to loosen the tether he’s kept on his desire to hold you down and have his way with you, and you gasp when thick, calloused fingers curl their way around your windpipe; his fingertips are bruising against your jaw, tipping your head back to bare your soft throat for him. You go boneless in his grasp, eager to take whatever he gives you at whatever pace.
"So you do know how to behave," he muses, free hand coming between your bodies to paw at your clothes until they come away in ribbons, torn from your form and leaving you bare before him.
The first inch of him inside of you is a delicious stretch; your cunt parts and flares to make room for him. He pauses, and when he finds nothing but pure, unadulterated lust in your blown out pupils, he gives you the rest.
Slowly, agonisingly, he drags it out; moaning praises fill your ears as he grants you inch after inch of him until he's seated firmly to the hilt. His fingers are bound to leave bruises where they're curled around your waist.
You whine, fingernails digging cruelly into his sides. He’s so deep you’re sure you can feel him in your throat.
"Cassian."
"Fuck, sweet girl," he hisses. "Usually I’d take my time with you, work you up first until you’re crying. But I need you right now."
The breath is punched from your lungs as he sets a punishing pace; your spine curves and moulds to the arm of the chair when Cassian’s hands venture lower to cup the swells of your breasts. You feel his cock kick up inside of you when he catches sight of your pert nipples, hardening into buds at the exposure of the cool air and the feel of his hands brushing the sensitive beads.
"I’ll get my mouth on you later, baby."
You’d melt at the words if you weren’t already reduced to nothing more than mush from his dick alone. The thick girth of him splits you wide, nestling deep against spots you have yet to discover, pushing you further towards a precipice you’re almost terrified of— you’ve never experienced pleasure like this, to this degree. The insurmountable, unfathomable pressure builds until you’re coming with a scream, your body trembling around his own, cunt clamping down around him to suck him in further.
"There’s my girl," he coos, slowing inside of you to brush away the hair sticking to your slick face. "You’re perfect.”
You whine and cant your hips downward to rock yourself onto his cock, and the bellow that rips through him would have you flushing white-hot under any other circumstances; you’re too far gone to care, a shaking hand splaying against the ridges of his wing until he shudders under your touch. You moan at the sight.
"Now that’s just mean, baby."
You suck your bottom lip into your mouth, gaze flitting up to meet his own with a coy smile. He brushes a slow line with his knuckles against your cheekbone— a loving gesture that has your heart clenching as well as your pussy.
"I love you," he says. "I love you so much."
"I love you," you repeat his words as he smears a kiss between your pinched brows. His forehead presses to yours as his hips rut up into your own. Dewiness clings to every inch of your skin and your knuckles bleed of colour where you cling to Cassian.
He brings you to completion four more times before he reaches his own peak, and only when you're reduced to tears beneath him does he crawl the length of your body, lips grazing over the slick skin beneath him until he reaches your cunt once more.
"Cass-" you gasp; your voice comes out a broken, strangled jumble of noise and he grins wolfishly up at you before licking a broad, long stripe from your spasming hole to your clit. Your back arches and you're not sure whether it's towards or away from his touch, but he stops you short when his fingers curl around your ribcage to press you to the plush fabric of the armchair.
"Told you I'd get my mouth on you, didn't I?"
Everything is simultaneously too much and not enough, and you're torn between grinding down into his mouth and shying away. Pleasure licks white-hot up your spine and you writhe against his bruising hold on your hips when the stubble on his chin scratches against your sensitive bundle of nerves. It's red and angry, swollen from Cassian's undivided attention, and it has tears gathering at your waterline once more. Your eyes are glassy and half lidded and he reaches up to brush the tip of his thumb against your cheek, his head never coming up from between your thighs.
Your skin sheens under the soft lights of the living room, sweat beading across the crown of your skull and your temples; you whine and thrash beneath him until your muscles seize and go taut like a bowstring, and pleasure drags you under once again. You're screaming - comes the dazed realisation - and your chest heaves as Cassian works you through it, offering up sweet praises for your orgasm. He smiles as if he hasn't just given you the best sex of your life.
You're utterly limp, boneless in his firm hold when he lifts your body to cradle you to his naked chest. The bridge of his nose presses into the softness of your cheek, skin rubbing against skin where he nuzzles into you.
"That was fucking amazing," you breathe with a laugh. "We should do that again."
"Mm," he hums. "Don't tempt me."
You giggle, pressing your face closer to his; everything about him intoxicates you: his smell, the feel of him under your hands, the dominating rasp of his cadence.
"We have something else to do first."
"What?" he asks, visibly deflating when you push yourself up on wobbling legs; your knees almost give out instantly. You can feel his smirk forming, burning into your naked form.
"Don't. Say. Anything," you grit. Your fingers brush the carpet when you bend to grasp a slip of fabric, and you quirk a brow at your sheepish mate. "My clothes, Cass!"
"I'll get you some more. Anything you want," he immediately says, watching you through half-lidded eyes. The love swirling in his irises almost has you staggering.
"While I appreciate that..." You lean down to press your lips against his, only pulling back to rest your brow against his own. "That doesn't solve my problem right now."
He snorts. "I like you naked. Maybe you should never wear clothes again."
"I'm not sure anyone would approve of that but you." Your smile is devilish. "Maybe I could distract a few High Lords at the next meeting..."
His teeth bare, a low warning growl reverberating through your very bones. You laugh, light and airy, and Cassian's sure you're heaven sent even as you send red-hot fury roiling through his veins.
"I'm sorry," you trill. "That was mean." You snag his own t-shirt, still predominantly in one piece, and slip it over your head; it lays against your mid-thighs and the scent of him cloys in your nostrils. "C'mon." You beckon him up with an outstretched hand, wiggling your fingers until he stands and slips his fingers between your own. A smirk pulls at the corners of your mouth. "Um, darling?" A pointed gaze has him grinning in return, clasping his chest in faux disappointment.
"I thought you liked me naked!"
"Oh, I do," you muse. "I'd just like to not scar everybody else in this house for life."
"It'd hardly be an unpleasant sight-"
"Yes, but I'm sure everyone would prefer it if I didn't try to kill them for looking." Your smile oozes saccharine, and then you're nudging him towards where his underwear lays discarded on the carpet. He pulls the material up and over his thick thighs and then he's back by your side in an instant; you preen under his adoring touch, pushing into the hands that slip underneath your shirt to grope at your bare skin.
"C'mon," you repeat, begrudgingly denying yourself the pleasure of sinking into his arms for another round of slow sex. "We need to do this first." You press your lips to the corner of his mouth. "Mate."
#cassian fic#cassian imagine#cassian x reader#acotar cassian#cassian#acotar fanfiction#acotar#acotar x you#acotar x y/n#acotar x reader#cassian x y/n#cassian x you#cassian acotar#acotar fluff#acotar fic#cassian smut#cassian fluff#writer#writers on tumblr#writing#writing for fun#writing for myself#smut writing#fluff writing#smut with plot#smut with feelings
1K notes
·
View notes
Text
pavlov's dog
»» ──────ஓ๑ ღ ๑ஓ ────── ««
pairing || mob boss!bucky barnes x f!reader
word count || 1812
summary || he kept you waiting and it's his honour to make it up to you.
warnings || smut! loosely depicted mafia business, daddy kink, oral fem receiving, pet names, begging, mild degradation, dacryphilia, pussy slaps, cmnf, subspace, dom!bucky
author's note || 18+ ONLY. hi. i haven't written for more than a year and a half. ive been feeling some type of way about bucky and maybe getting back to writing mindless porn is what i needed to get my creative fulfillment ive been severely lacking. please don't mind the potentially choppy smut as i haven't written in a long while. feel free to reblog and leave comments!!
»» ──────ஓ๑ ღ ๑ஓ ────── ««

8:53.
8:53 PM, and you were still waiting for Bucky to finish his meeting. A recent competitor was threatening Bucky’s monopoly in New York, apparently, something to do with some guy who owned a publishing company inherited by his grandpa, who was looking to buy one Bucky already owned.
Whatever. You weren’t really listening when Bucky was talking about it over the phone because you were too busy keeping his cock warm.
You watch the digital clock flash another minute, and finally, your phone dings with an activity notification at the front door. Before you can try to be chill about it, you all but run to the door to greet your man, practically jumping on the balls of your feet with excitement. The door swings open, and you barely glimpse Bucky's tired and frustrated expression before it morphs into a sweet smile reserved for you, making his eyes crinkle at the corners and shine.
Running into his arms, you koala hug him as you nuzzle your nose into his neck. He expertly toes his shoes off while showering you with the same attention. “Were you waiting by the door for me the whole time, baby?” He asks with a smile.
Nodding your head yes and widening your eyes while twisting your lips into a pout, you decide to play the sweet, patient girlfriend who Bucky knows you really aren’t. “You kept me waiting for 4 whole hours, Jamie, 4 hours. I stood right by this door and didn’t take a single break until you came home.”
A hearty laugh escapes his lips at that, and you can feel the tension from his shoulders leaving as you gently rub them while still managing to cling onto him as he maneuvers you two to your bedroom. Unfortunately, both of you are well aware that patience is a virtue that you very simply do not possess.
“My poor, incredibly patient and honest baby. How rude of me to keep you waiting like this, huh?” He keeps his voice low, both in pitch and volume. It sends a tangible shiver down your spine as he sets you down on the bed. You bite your bottom lip, subconsciously spreading your legs, unable to hide your reactions from him.
Bucky loves how responsive you are to him.
“So mean to me daddy.” You whisper, “need you to make it up to me.”
Bucky licks his lips and clenches his jaw because fuck he needed this, especially after being stuck at his office for nearly 4 extra hours while you were at home looking like this. So sweet and soft and submissive for him; all he needed was someone to control because his empire in New York was being tried.
But Bucky had it under control. He always did. This wasn’t the first time he had to deal with a newcomer who decided to get a little ballsy and try and take over some of his territory.
He always did fuck you more aggressively when work had more hiccups than usual.
“Yeah, honey baby? How do you want Daddy to make it up to you? Use your words.” Bucky’s tone kept dropping, getting deeper and deeper with each delicious word he spoke to your somehow already foggy brain.
Even while he was giving you some control, he managed to maintain dominance over you, and that just flared the heat pulsing between your thighs.
“Need you, daddy, want your mouth.” You whisper, heat spreading your cheeks as you voice what you want, but a surge of pride goes through Bucky. At the beginning of the relationship, you had really struggled with voicing what you wanted, whether it was something like telling him you didn’t feel like getting dolled up to eat at a luxury French restaurant and wanted some burgers instead or how you struggled to say to him you wanted him to take his shoes and coat off before he came inside your apartment and sat on your couch. He dealt with people who feared him every day, people who never corrected him or crossed him. It was made abundantly clear you are not one of those people; you need to tell him what to do and how to do it, and he will. Bucky would bring the moon and the stars to you if the thought ever crossed your mind.
Dropping to his knees will have to do for now, he thinks.
His large palms spread your thighs as your pliant body falls back, but you prop yourself up on your elbows to watch the show. Bucky smiles at you with hunger in his eyes as he licks his lips once again while gingerly sliding your pajama shorts down your legs. You inhale sharply as the cool air from the open balcony doors hits your core. Bucky can’t help the rumble emerging from his chest as takes in your already wet pussy, bringing his thumb up to flick your swollen clit and messily run the tip of his finger around your pussy. “You were waiting for me without any panties on? You’re that fucking desperate for me, sweetheart? Ready to bend over for me as soon as I walk through the door?”
You whimper at his fingers and throw your head back, nodding it desperately fast.
“Aww, don’t go quiet on me now,” Bucky teases, “you were being such a good girl telling me what you want. Don’t stop now, angel baby.”
You whine high in your throat as you tug on his hand that is still purposefully brushing over your clit, “Please, Daddy, just- just-”
Before you can finish your plea, Bucky licks up your slit, expertly swirling his tongue around your clit as your thighs jolt around his head, and a surprised mewl leaves your lips. “Oh god, Daddy, need more, please more,” your hands reach out to grab onto whatever you can, one hand gripping Bucky’s hair, making him hiss and buck his own hips against his tight slacks while the other latches onto the silk bedsheets.
“Greedy girl,” Bucky hums against your pussy, but to your delight, he indulges you, slipping a thick finger into your pulsing hole. Still, before you have time to react to that, he’s wrapping his lips around your swollen clit for the first time tonight and sucks on it. Making your back arch up and your legs quake as you try to simultaneously push yourself away from him but pull him closer. A near-pornographic moan leaves your swollen lips as your chest heaves. You cry out his title as he slides another long finger inside you, hollowing his cheeks as he sucks on your poor little clit and soothes it with kitten licks every few seconds.
“Oh Daddy, you’re gonna- fuck, you’re gonna make me cum please, Daddy, please can I cum!” You babble, drool seeping from your lips as Bucky always manages to reduce you to a mindless, pathetic mess. It had never been easy for you to stop or slow down your orgasm, as Bucky always tended to barrel it out of you. Although you had noticed that the high that spread through your body when he permitted it was much more euphoric than the orgasms that slipped out of you.
Maybe it was something akin to Pavlov’s dog effect. Conditioning.
Bucky was aware of this fact as well. He knew your body, your mind, better than you did.
A satisfied smirk works itself onto his lips, and he grumbles something against your sensitive cunt, enjoying the way you struggled to keep your body at bay. “I dunno, my stupid little baby, dunno if you’re desperate enough yet.” Bucky’s words vibrate against you and propel you towards your high even quicker. Your whines get more high-pitched and breathy as you struggle against your boyfriend’s relentless tongue. “I am Daddy, I am desperate. Always am for you, please, Daddy, make me cum.” You whine a bit petulantly as your orgasm is right there. But he’s dangling it above your head and forcing you to obey him. So, you try the guilt-tripping route.
Tears well in your eyes, and your lip quivers, “Please, Daddy, don’t you wanna make me cum? Don’t you wanna take care of me? Make me cum all over your tongue and make a mess? Please, Daddy, need you so bad!” You cry, tears slipping down your face, and Bucky grunts, closing his eyes as he tries not to cum in his pants at the sound of your breathy pitch and the sight of tears slipping down your face.
He pulls back and curves three fingers toward your special spot, and takes his other hand to slap at your swollen clit in quick succession, making you squeal. Arousal paints your thighs as he quickly switches back to overstimulate your poor button by sucking on it so hard that your orgasm squirts onto his bearded face, making him groan in appreciation as he mumbles something like: “That’s it, there’s my good girl making a fucking mess like Daddy taught you.” But you are too out of your mind to really process his words as you struggle to breathe down from your high, tears slipping down your face as you bask in the overwhelming feelings of such an intense orgasm.
Bucky kisses up your thighs and stomach, easing his fingers out and tongue away slowly so you don’t go from overstimulated to zero all at once. He cups your face in his hands and kisses your cheeks as he shushes you, bringing you down from your high with soft words and coos that appeal to your clouded brain. You cup his much larger hands in yours, pouting your lips up for a kiss, and he chuckles before placing a soft kiss against your swollen lips. He can taste the salt from your tears, and it sends even more blood rushing straight to his dick as he ruts his hips against yours, making you pull your lips apart on a mewl.
“Daddy, will you fuck me now?” You ask with a certain lilt to your voice. Bucky scoffs before pressing his lips to yours and rumbling against your lips, “You’re an insatiable little whore you know that?”
Manhandling you to the top of the bed, he throws you against the pillows as unbuttons his slacks and pulls his hard cock out, pre-cum oozing from the swollen red tip as he looks like he could destroy you. “I’m your little whore daddy.” You tease, spreading your shaky legs apart, and he licks his lips.
—--------
Bucky worked from home the next morning. Needing the extra time to make up for the late nights and the particularly strenuous activities that led into the early morning hours.
As you sat on his lap, peacefully dozing in and out of sleep, he knew he had made the right choice that morning.
#bucky barnes#bucky barnes smut#bucky barnes x reader#bucky barnes imagine#bucky barnes fanfiction#bucky barnes x yn#mob!bucky barnes x reader#mob!bucky barnes smut#mafia! bucky barnes x reader#mafia! bucky barnes smut
1K notes
·
View notes
Text
Aromantic short fiction open call!

Hey! We're doing an open call for submissions for Being Aro, which released from Page Street Publishing next summer. Submission guidelines here!

Text: Editor of BEING ACE Madeline Dyer and author of TARNISHED ARE THE STARS and FIRE BECOMES HER Rosiee Thor's BEING ARO, an anthology of short stories in multiple genres from contemporary to fantasy to science fiction that celebrate and explore the sub-identities of the aromantic spectrum from a mixture of established and emerging YA writers, to Tamara Grasty at Page Street, in a nice deal, in an exclusive submission, for publication in summer 2026, by Saba Sulaiman and Amy A. Collins at Talcott Notch Literary Services (world English).
Submissions are open between March 31st-April 28th 2025!
Stories should be:
approximately 5000 words long
any genre/subgenre of young adult fiction
centered on aromantic characters/themes
written for a young adult audience
original fiction (no fanfiction, no AI)
written by new/emerging authors who identify on the aromantic spectrum and are 18+
Once again, here's the link to the full guidelines! Please don't self-reject! We hope to see your submissions in the inbox!
#aromantic books#aromantic spectrum#arospec#aroace#aromantic#aromantism#actually aro#being aro#being ace#open call#short fiction#queer books#anthology#lgbtq books#aspiring writer#aspiring author
161 notes
·
View notes
Text
Call of Duty - Masterlist:

The Complete Masterlist of: peachetteprice.
Asks and submissions are open!
Feedback Policy
External Links | Ao3 | Wattpad: Peachette_Price
–––––––––––––––––––––––––––––––––––––––––
Key
× NSFW content - ranging from sexually suggestive themes to explicit smut. This content is not to be interacted with by minors. I give you my partial trust to adhere to this, but I will regularly check the age of the blogs following me and block when necessary.
// This is an ongoing work.
< / > This work is unlikely to be completed now and/or in the future.
(REQ) This work is published as a request by a user.

TF141 Headcanons:
Driving Habits - How would the boys usually drive? What are their habits when in the hot seat?
Cheating Partners - POV: I let an anon down by not fulfilling their request and still posting it anyway. Ft. Phillip Graves. ×

Captain John Price:
42-Year-Old John Price - He isn't as sprightly as he used to be. ×
Eighth Date - John reveals to you about his profession, but you're much too taken by something else!
Speak Up, Love - Uh-oh. John's lost his voice. Wouldn't it be such a shame if someone teased him about it? ×
Stern Captain John Price - He really... really... becomes accustomed to the life of a cat owner despite his penchant for dogs. ×
How it Should Be - John's a hardened war veteran... but he still gets flustered every time you call him handsome. ×
A Deal of Cards - (REQ): How might Price deal with his gorgeous, talented partner: a spiritulist, working in the creative field with a rather earthly aesthetic? With love, of course.
What a Bargain - John is a man who loves bargains. That's it.
Jeweller!Price - Uh... John's a jeweller. That's it. Pretty straight-forward, innit. Pt. 2 ×
Accountant!Price - He's an accountant. You get it by now, right? ×
The Gloves are On - The gloves stay on, even when he's finger-fucking the ever-living daylights out of you. ×
Neuroscientist!Price - Price is a neuroscientist with a dark present. ×
Coworker!Price - don't get it twisted. This isn't 'accountant' Price. ×
Domestic!Price - He's just a little guy with fuzzy socks on.
Agent!Price - He's only ever been an Agent: what are you on about 'Captain'?
EmotionallyUnbalancedWriter!Price - He reminisces on a love lost.
The Uniform - John lets you have all the fun 'playing Lieutenant'. Don't worry, he knows his place, too. ×
CultLeader!Price - Oh, how we rejoiced!
(REQ) Neighbour!Price - John is your bird-watch loving neighbour!
Husband's Best Friend - John Price is your HBF.

Simon "Ghost" Riley:
Strangers in the Night - Simon has a waking nightmare; you're always there to provide comfort.
A Hand for Radio - You're not just on the team to dilly-dally, something that everyone, including Soap, finally needs to understand. ×
Some Days - (REQ): Simon and Reader have a spat. Reader feels invalidated and rightfully tells him so, because what a bitch, honestly.
Fisherman!Simon - it's Simon... but as a fisherman. I don't know what more you want from me.
Full-length works:
27 Hawthorn Court - Simon "Ghost" Riley finds himself in hot water after the Greater Manchester Police suspect him of murderering his family: his brother, his brother's wife, and their son. < / >

Kyle "Gaz" Garrick:
Could Have Been - Didn't you know, Gaz could have been a professional footballer?
One of Those Nights - It's your favourite thing about him, truly. ×
Born For It - Oh, but he's just so rich and handsome, whatever shall you do? ×
Morning Brew - Kyle likes his coffee like he likes his coffee, and his mornings, entirely unlike his coffee: full of lazy sex! ×
Backshots with Kyle? - The one thing he loves to do more than anything ×

Bar Meet - You meet Gaz in a bar. Even after the night is over, he isn't done. ×
Crawley - Kyle is your flatmate in a two-bed flat share. Things are predictable, right up until they aren't.
John "Soap" MacTavish:
The Ever-forgetful John "Soap" MacTavish - Poor bastard never remembers not to use the water when you're mid-shower!
A Dream to Build a Life On - It's tough to have almost everything you've ever wanted right at the tips of your fingers, but have one thing... just one thing... that seems entirely out of reach. ×
Days of Old - It's never easy to watch something drag the life out of a loved one's eyes. ×
The Highlands - A short drabble about Johnny coming back to Scotland every once in a while to re-live the simplicity of rural life. Ft. Part 2
Charity Dinner Ball - Soap relieves his OWN Charity Dinner Balls... pause... after being drawn to you the entire evening. ×
Needy Soap - I need him biblically, I fear. ×

Phillip Graves:
Full-length works:
Mister Commander - (DBF) Winnie Collins knows better than anyone that a homestead requires up-keep. When she returns home to Texas, following the dissolvement of her engagement to the man she thought she loved, there's a stranger on her parent's ranch, during the height of May heat, in a town where nothing but dirt and sweat remain. Phillip Graves. He's her father's best friend - and he's here to stay. × //

Ghost x Soap
Two Men in a Boat - A boat bobs along the ocean. Within, there are two men.

#call of duty#captain john price x reader#simon ghost riley x reader#john soap mactavish#captain john price#simon ghost riley#kyle gaz garrick#phillip graves#callofduty#call of duty fanfiction#masterlist#cod masterlist#call of duty fanfic#call of duty fandom#cod fanfic#cod#cod mw2#cod mw3#cod ghosts#call of duty ghosts#call of duty modern warfare#john price#captain jonathan price#ghost cod#soap cod#soap x reader#ghost x reader#john price x reader#call of duty masterlist#ghoap
461 notes
·
View notes
Text
For example, you're generally content in your career; then you imagine a situation in which you're being interviewed about a book you published, and as a result you start considering becoming a writer instead of continuing on your current path.
–
We ask your questions anonymously so you don’t have to! Submissions are open on the 1st and 15th of the month.
#polls#incognito polls#anonymous#tumblr polls#tumblr users#questions#existential polls#submitted feb 1#imagination#daydreaming#decisions
154 notes
·
View notes
Text
Adapt. Evolve. Become.: The Genderqueer Fandom of NBC's Hannibal - SECOND EDITION!
In 2023 we released a fan-led volume of fanworks by and about trans non-binary, genderqueer and otherwise non-cis Fannibals. Now we're back by popular demand, to create a second edition and YOU can be involved!
We've extended submissions! You can now submit until February 28th 2025!
We'd especially love to see more:
Essays
non-fiction
personal pieces
memes
cosplay
fanart
We're still open to fanfic but as we have quite a lot on that front, we'd love to see other types of submissions.
SUBMIT HERE
NBC's Hannibal has resonated with many queer fans, and we know that being in the Hannibal, Hannigram and Hannibal Extended Universe fandom, and the support of Fannibals, has been part of many people's gender identity journeys. We want to capture that in a fandom led volume of non-fiction, featuring essays, creative nonfiction, personal accounts and art.
You may have even seen that Hugh Dancy was gifted a copy and had a very thoughtful conversation about the interpretation of Will Graham as a trans man.
IF YOU WISH TO SUBMIT WE URGE YOU TO READ THE EXISTING EDITION FIRST! You can read or download free here!
WHO should submit: Please ONLY SUBMIT IF:
you are aged 18 or over. For the sake of legalities, we are only accepting submissions from those legally considered adults in the region of publication - UK.
you are transgender, non-binary, genderqueer or otherwise non-cis.
OR you have a close relationship (sibling, partner etc) with someone who is transgender, non-binary, genderqueer or otherwise non-cis.
NB: The reason for the edition of cis creators is as a result of the feedback on the first edition regarding how much it spoke to people who had trans relatives or a trans partner and how it resonated with them and their (often) non-fandom partner/relative. We wanted to give them a chance to voice the impact of the show and fandom on their lives as people with close relationships with trans people.
WHAT submissions do we want:
Fanfiction (100 to 5000 words)
Fanart (including comics)
Personal piece / statement / testimony (pref. under 3000 words)
Creative non-fiction (up to 5000 words)
Essay (up to 5000 words)
Cosplay (photos of yourself in cosplay and/or instructions/tips on how to make trans friendly cosplay)
Other (any form of art, photography or writing not covered here including crafts, memes, playlists???)
Theme: Via one of the above mediums, we want you to share with us in as much or little detail as you’d like, your journey as a non-cis Fannibal in the Hannibal fandom, and/or the impact NBCs Hannibal has had on your gender journey.
A few points for consideration you may wish to explore:
Has the show and/or being part of the fandom helped you explore your gender, or made you feel more confident in expressing it - even if only online.
Has the fandom helped you with your transition and/or medical needs, such as donating for trans-clothing or surgeries?
Do you want to write an essay exploring the connection between NBCs Hannibal and non-cis fans? Or explore the trans-coding of Francis Dolarhyde?
Do you want to submit fic or art of Hannibal, Will or another character that expresses how you feel about your own gender identity?
PLEASE NOTE: if your submission is successful you are welcome to use your real name or an online handle for authorship, but you will have the option to publish anonymously or under a pseudonym if you would prefer.
YOU CAN submit multiple works. We may publish up to two pieces from each person if they are different types, e.g. one fanart AND one essay.
Timeline:
Submission period: ENDS 28 February 2025
Editing: March 2025
Final edited copies for proof by 31st May 2025
Publication: July 2025
Compensation: As a fan-led project we do not have any funding and so cannot offer monetary compensation. All contributors will receive at the least an e-copy of the collection. If we are able to establish funding (potentially via Kickstarter) we may be able to send each contributor a print copy, but will not be able to confirm until further in the process and cannot guarantee this.
If funding is not available, we will be able to offer contributors reduced cost print copies by charging only cost price. However, given the quality of the art printing of the print copies, this will still be a significant cost.
Content Restrictions:
Contributors must be transgender, non-binary, genderqueer or otherwise non-cis, OR in a close relationship with someone who is transgender, non-binary, genderqueer or otherwise non-cis.
Contributions must relate to NBCs Hannibal, HEU and/or the fandom
The contribution must be original. Previously published works may be considered, such as existing fanfic and fanart.
ABSOLUTELY NO GENERATIVE AI.
Explicit works welcome, but please give details in the sign up form, especially for any visual media.
It should go without saying, but we will not accept bigotry and hate speech: We may consider works that feature these things but do not glorify them. For example, we will consider works that discuss transphobia but not works that are transphobic.
FAQ under the cut!
What is Trans Hannigram Day? Trans Hannigram Day or TransHanniDay is a day of celebration for trans* fanworks and creators in the Hannibal, Hannigram and Hannibal Extended Universe fandom. On this day, old and new fanworks are shared with the intention of filling the timeline with trans* love!
Originally this event was Transcendence Fest, first held in December 2020. The first TransHanniDay was held on 8th April in 2022 in reaction to the release of a certain movie on that day.
Is this edition also for charity? We were thrilled to donate the profits from the 23-24 fiscal year to The Okra Project, and we're already on track for a similar donation to this year's nominated charity - Gendered Intelligence.
Will this collection only be focused on Hannigram? Technically the focus is on the fans, but we know the influence of NBCs Hannibal and the fandom itself goes beyond Hannigram. Both in written works and in art, other characters are accepted including those from NBCs Hannibal and those from other Mads and Hugh projects (Hannibal Extended Universe).
For example, if Bedelia De Maurier or Adam Raki resonated with you as part of your gender journey, we’d love to hear about it.
How can I prove I’m Trans*? We aren't expecting you to and in no way expect you to out yourself either online or in real life. We will take on trust that you are who and what you say you are, including if you are questioning, between labels or do not like to use labels.
As noted above, those who would feel more comfortable doing so, can have their work published under a pseudonym or anonymously.
Who is publishing this collection? This collection will be edited and published by Max Turner. Max is a gay transgender writer based in the UK, a Fannibal and the publisher of small indie press A Coup of Owls Press. This publication will not be associated with A Coup of Owls Press directly.
#transgender#nonbinary#genderqueer#fannibals#fannibal#hannibal#hannigram#hannibal extended universe#TransHanniDay#trans hannibal lecter#trans will graham#trans hannibal#hannibal lecter#will graham#nbc hannibal
153 notes
·
View notes
Note
what’s your internship like? (in your better cr)
page turners
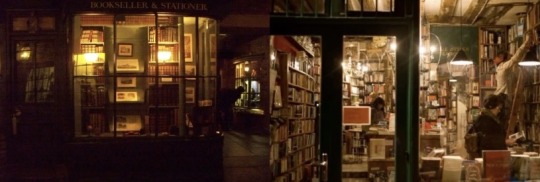
.
.
.
you can’t blame me for wanting to live in a world where society doesn’t reserve value and recognition to only be rewarded if you follow the standard, left brained, logical mindset of stem and maths and science and technology — and this is coming from someone who loves those very subjects and excels in them — i’m very much a maths lover, i enjoy solving logical problems, it brings a satisfaction that cannot be described, and yet . i don’t feel as alive as when i’m writing, when i’m reading, when i’m analysing, pulling apart, breaking down the intricate threads of thought that make up a story, or an essay, or a poem
my mind may find satisfaction in solving page after page of algebra, but my soul will only find its spark when i give in to emotion and empathetic analysis, and for that very reason, i scripted a different degree for my dr-self, and with that came a different internship in a publishing company that does not exist in this reality — Page Turners
in my dr at the midpoint of my first year in uni, i had gotten into a year long internship at a government office, hired because of my degree in entertainment law majoring in copywriting
but i have a double degree, my second being a degree in arts majoring in literature and creative writing, and i always knew i wanted a more creative job, rather than the technical, legal side of the publishing industry (no matter how well it pays)
so at the end of my first internship, i started exploring different avenues, and Page Turners was brought to my attention (ironically, by my english tutor from high school)
they advertise mainly to young writers, they have an open submission for a monthly online magazine, curated by a theme (think dakota warren’s nowhere girl collective but only focused on writing — whereas dakota includes submissions for art and music too)
Page Turners wasn’t hiring anyone who hadn’t gotten a full degree but with the help of my ex-tutor (and ex-boss bcs i used to mark papers for her every now and then) i was able to make a case for an internship position
it took a while, a whole year in fact, but Page Turners thought that a way to reach the youth would be to start as early as possible and the best way to do so is by implementing internship programs into their business plan — essentially, my drive to work in the creative field (and mostly due to my connections bcs networking sucks but it is everything) i was able to convince an up and coming publishing house to start hiring students, who may be exactly like me, just waiting for the opportunity to do something creative
i haven’t scripted much on the actual internship program and what it entails but i get accepted and start working at the beginning of my third year (honestly year 3 of uni has a lot of firsts for me — first longterm internship, first boyfriend who i can actually see a future with, first new car, first youtube play button for my anonymous cover channel w two of my high school friends — theres probably more but i don’t wanna sound cocky T^T)
anyway, back to the point — my internship essentially allows me to explore the workings of a publishing house, and with my background in copy write law and creative writing, i’m able to dabble in many different divisions and subdivisions, getting a chance to see how the writers, lawyers, agents and editors work — it’s where i find my passion for developmental editing : the profession of assisting with the creative process of a book, primarily a novel, where you go through a synopsis, a story board, and the overall themes and acts of the story, it’s less about the in-debt typo-prevention of editing and more about the overall narrative — stuff like helping to pivot the story or guide the plot in a certain direction to achieve everything the writer hopes for, or, my personal favourite and my special skill if i do say so myself which is patching up plot holes to be seamless and make sense
finally, this internship, the people i worked with, they are the reason i felt confident enough to go back to uni and do a postgrad degree for a masters in creative writing and a specialisation in editing, so i could officially work full time as a developmental editor
meaning i could read and write and help create stories for a living
.
.
.
if i ever script more or after i’ve properly experienced this internship, i will definitely update this post, or just make another one!! but for now, this is all i’ve got <333

cuppa queries; order in — ask responses
2025 © chaaistained
#by chaaistained#teacup anons !!#better cr#better cr dr#desired reality#dr self#shifting realities#reality shifting#shifting script#shifting ideas#dr ideas#shifting thoughts#shiftblr#loa#loablr#loassumption#law of assumption#manifestation
111 notes
·
View notes
Text
Celebrity Crushes
Pairing: Damien Haas x gn!Reader
Summary: "He had never said it was for a video, though maybe at this point you should’ve been able to guess that being asked for a list of three top choices was for this series."
Warnings: Brief mention of being drunk but otherwise none :)
AN: Hi guys!! I wrote this in 20 minutes so it’s…rough around the edges….but you’ve been so sweet and patient with me while I get my shit together now that I’m back from school!! I have many many WIPs that I plan on publishing soon that will have much more substance than this, but I still hope this helps hold you over for another week or so <3
You delayed your own emergence from sleep. Your bed was comfortable, warmer than usual, maybe thanks to the open blinds that let sunlight dapple the room. It was so easy to fall back into the snug embrace of slumber as you stretched against your sheets. You rolled over, eyes still heavily lidded and blinking to avoid the light as you felt around for your phone on the nightstand.
You yawned, stretching again; you let your back arch off the bed, feet poking out from beneath your blanket as you let your ankles crack—a quiet, congenial noise, and an even more satisfying feeling.
There were several messages waiting for you when you unlocked your phone.
Ang: UM??
Ang: New games vid????
Ang: 😵💫😵💫
You: What?
Ang: Dude🫠
You: What??
You: Isn’t it a Shayne guesses
You: I just woke up
Ang: Hold on
They were not the messages you’d been anticipating on a peaceful morning off from work. Angela’s texts woke you up immediately, her words burying themselves in your head as adrenaline took hold, muscles tensing, and you felt something pull at your stomach.
Had someone said something? Had you said something? Had you been somewhere you weren’t meant to be? Did it even involve you? Was she simply acknowledging something fucked up or funny that you had played no part in?
You held your phone in a vice grip, white-knuckling it and waiting to hear how exactly the new upload pertained to you—if it pertained to you—and whether you’d still have a job or any friends by the end of the day.
You felt a soft buzz on your fingers and snapped your attention to the screen, hoping to see Angela’s name.
Court: Was the new video planned or…
You: What is happening
You: Angela texted me too
You: I literally just woke up
Court: omg🥹
You felt hot. Not in the cozy way you had been when you woke up, but in a burnt cheeks and stomachache way. This was not something you had ever woken up to before, it was not at all routine, and you worried that your time at Smosh was up based solely on the manner in which your friends were texting you.
Another buzz. Kiana this time.
Kiana: I told Spencer not to keep it in the final cut
Kiana: But it’s really cute actually
You wanted to throw up. Shakily leaning back in bed, you tried to type out a response to Kiana that would help you wrap your mind around what exactly it was that you should be worried about.
Another buzz alerted you to Angela’s late reply, and you abandoned the message you had been drafting for Kiana.
Ang: https://www.youtube.com/watch?v=vzUs87BMpsc
Ang: 26 minute mark & then watch to the end
Ang: 🥴🥴🫶🏻
You had been right. It was another installment of Shayne Guesses, but you had no recollection of sending in a formal submission of…
“Can I identify someone, based on their top three celebrity crushes?”
Your heart jumped to your throat.
If this was going where you thought it was, you’d send in your letter of resignation by tonight.
You found the timestamp Angela had sent you, and immediately grimaced, folding your body into itself. You wiped a hand over your face, as if rubbing your eyes hard enough would make this all go away, leaving you to wake up fresh and unabashed.
“Ok—ok, I can work with this,” Shayne’s eyes darted over the screen, shouting a laugh when he took in the options given to him. “So Pedro Pascal—expected—Cillian Murphy, and he looks younger there. Is that what he looks like now? No…”
“No, that’s from like, 2000-something,” Spencer responded off camera, “I did not choose that picture.”
“Ok, 2000s Cillian Murphy, Pedro Pascal, and Damien Haas.” Shayne paused to stifle a chuckle. “This is the second time you’ve broken your own rule!” He stared pointedly at Spencer.
“Bro, that’s Shez from Fire Emblem!” Spencer argued, still out of frame, and Shayne bit the inside of his cheek.
“I mean,” Shayne looked at the list of names in front of him, “I feel like, you know, maybe it’s not…maybe it isn’t super obvious to people watching, but I think it’s a pretty easy guess for anybody in the office.”
“So what’s your answer?” Spencer asked.
“Oh, come on, like you need to ask,” Shayne crossed his arms before triumphantly declaring your name. “Final answer, look—” He clicked to the next page, and there was your headshot.
Your headshot.
Because Damien was one of your celebrity crushes.
One whom you worked with, and were friends with, and hung out with, and ate lunch with.
You felt your eye twitch.
You paused the video in a huff, too mortified to follow Angela’s instructions and watch it to the end.
You might’ve laughed if you weren’t so besides yourself with embarrassment. You were deeply confused as to how that list had even made it into the upload when you hadn’t sent it in.
You racked your brain, trying to remember if you’d drunkenly sent an email, or given an ok when you were only half awake.
You could recall, vaguely, a text exchange with Spencer a few weeks ago, where he had asked, out of the blue, about your top three celebrity crushes. And you gave your answers, sent a few googled pictures, all in good fun, to your friend.
He had never said it was for a video, though maybe at this point you should’ve been able to guess that being asked for a list of three top choices was for this series.
You: Charles.
You: What happened to confidentiality.
Spence: I CNA EXPLIAN
Spence: CAN
Spence: EXPLAIN
You: 🤨
Spence: LISTEN
Spence: I THOUGTH YOU KNWE
Spence: I THOIGHT IT WASSON PURPOSE
Spence: I THOUGHT HE KNEW??
Spence: BECAUSE HIS??
Spence: Please don’t kill me I have a family.
Spence: And I’ll buy you lunch.
You: You’ll buy me lunch for a month.
Spence: A week
You: Two weeks
Spence: Deal🤑
Spence: I love you❤️❤️
Spence: And I’m sorry I went over y’all’s heads
You weren’t mad.
Honestly, you couldn’t bring yourself to be genuinely angry; it was hard to be mad at one of your dearest friends over something that was so clearly a misunderstanding. Especially when it had no real bearing on your career or public image.
This just meant that people would now be fully aware that you had the hots for a coworker.
And said coworker would also be fully aware of it. You tried to push down the shame.
You: Accepted
You: I love you too❤️
You: I want Thai tomorrow
Spence: Would you settle for shirt?
You: I'll kill you.
Spence: Don’t you have another smosh man to bother🧐
You smiled at your own reassuring words, and Spencer’s acknowledgement of his fuckup was equally as helpful in improving your mood, as was his casual banter. For a moment that was enough to make you forget why your stomach was still in knots.
It could be argued that it was an open secret, it certainly seemed as though your friends were more shocked to see your list make it into the final cut of the video than they were to see the list itself. You counted on your fingers: who had you told, who figured it out like a child's simple jigsaw puzzle, who had asked point-blank after seeing you interact with Damien.
You ran out of fingers.
Still, you felt that you’d been cautious enough about it, to the point that Damien himself, at least, hadn’t seemed to figure it out, despite the amount of time you spent together, and the large portion of that time that you spent with a dopey grin on your face and a blush creeping up your cheeks.
Maybe he hadn’t seen the video. Maybe he’d never see the video. Maybe he wasn’t even planning on being online today at all.
Or maybe you could change your name and disappear for a while.
Maybe you’d be in the clear.
You took deep breaths, trying to settle your brain and your heart and the shakiness of your hands.
And then Damien’s name lit up your phone screen, and the results of your impromptu meditation were immediately gone, thrown out the window with your composure.
Damimen: Very interesting list
You: I’m so sorry
Damimen: What?
Damimen: Why?
You: I didn’t mean for you to find out this way
You: Very publicly on a Wednesday morning
Damimen: Who said I was just finding out?
You: Shut up
You: I’m good at keeping secrets
Damimen: I know
Damimen: Angela and Chanse aren’t tho
You: Oh god dammit
Damimen: Which is why I knew not to tell them anything about my list
Damimen: And I mean
Damimen: Stuff that I'd generally like to be kept under wraps
You: So the launch codes are safe?
Damimen: Are they safe if they're with me?
Damimen: 🤯
You: MR PRESIDENT!!
You: Wait
You: Joking aside
You: What are you talking about
You: Wdym “not telling them about your list”
Damimen: Did you not watch the whole video?
You: Got kinda distracted
You: Needed to make Spencer fear for his life a little
Damimen: ???
Damimen: Watch til the end
Damimen: And then come over?
Damimen: If you want?
You furrowed your brow, questions still unanswered, but pleased that he wasn’t upset with you.
You found your way back to the video, clicking forward again until you saw Damien’s headshot and then rewinding to see his list.
Pictures of you.
Three pictures of you. Pictures he had taken when you were together; at the ren faire, getting coffee, in the office.
And now the texts from everybody remarking on how cute the video was made sense. They hadn’t been referring to your list, they’d been referring to Damien’s more than forward response that worked in tandem with yours.
“Not a lot of variety to this one,” Shayne laughed into his hands, “I don’t really have to guess cause there’s only one name left on this list, but even if there wasn’t…This is Damien. Yeah, no, this is Damien. Final answer.”
“How do you know?” Spencer pushed.
“Well I mean, I, y’know, I received these pictures from Damien when they were taken,” Shayne spoke as if it should’ve been apparent, “But also. Come on. I know. See,” he clicked to the next page, where Damien’s name and picture appeared. Shayne raised his arms in triumph.
Your mouth fell open and your lips curved up into a subtle smile.
If you hadn’t been obvious, you’d certainly been oblivious.
The pictures of you that Damien had taken lined up on the screen paired with Shayne’s assurance in his answer, the knowing chuckles from off screen, it all made your heart skip. You felt it sinking from your throat and back into your chest where it belonged, thrumming contentedly.
Damien’s handle on your heart didn’t worry you. If anything, it relaxed you, made you feel safe, collected despite the rollercoaster of a morning you’d had. The discovery of a crush requited made you feel giddy; young and in love.
You: On my way
You: Gimme 20 minutes
You: And send me those pictures
You: 😘
Damimen: 🫡🥰
#damien haas#damien haas fic#damien haas fanfiction#damien haas x reader#damien haas x you#smosh#smosh fic#smosh fanfiction
515 notes
·
View notes