#neurological research
Explore tagged Tumblr posts
Text
Celebrate International Brain Day: Nurturing Your Brain for Optimal Health
Happy International Brain Day! 🧠 Celebrate the incredible power of the human brain. Learn about brain health, engage in stimulating activities, and adopt habits that nurture your mind. #BrainHealth #InternationalBrainDay
Introduction Happy International Brain Day! 🧠 Today, we celebrate the incredible complexity and power of the human brain. This global event, observed annually on July 22nd, aims to raise awareness about brain health, promote neurological research, and highlight the importance of mental well-being. Our brains are responsible for everything we do—from thinking and feeling to moving and breathing.…
#brain awareness#brain health#brain-healthy habits#cognitive function#healthy living#International Brain Day#mental fitness#mental well-being#neurological research#neuroscience
0 notes
Text
#lmao#for anyone who's curious the process went:#send ask to aita official#blog blows up#someone realizes its a chexer fic#i follow them bc they seem cool#i join their rvb server#their encouragement pushes me to finish the Actual Fic i was working on#i expand the fic to be more of a whole au after it comes out much better than expected#the next fic in the au that i work on has to do with a character's brain injury#this leads me to do research into brain injuries#''......huh. this sounds. a lot like the neurological symptoms that my doctors have been saying is just part of my anxiety disorder''#think on that for a while#go to the ER for unrelated reasons#remember my theory#bring it up to the doctor#Doctor Immediate Concern#doctors orders a ct scan#''eeyup! that there's some atrophying and a chiari malformation! y'ever had a head injury''#(i had had several)#''well! shit! time to refer you to neurosurgery :) see if we cant do somethin about all that memory loss and severe pain and shit''#and now we are here#it also lead me to research osddid systems for the first fic#and now my therapist is having me tested for osdd because i did not know that those symptoms were not a thing everyone experiences#so like. thanks for helping me meet friends who could encourage me to engage with the things i like + learn more about myself#^ ^ <3#im actually not gonna say ''ok last update fr this time'' bc idfk maybe something WOULD be funny to post on here
6K notes
·
View notes
Text
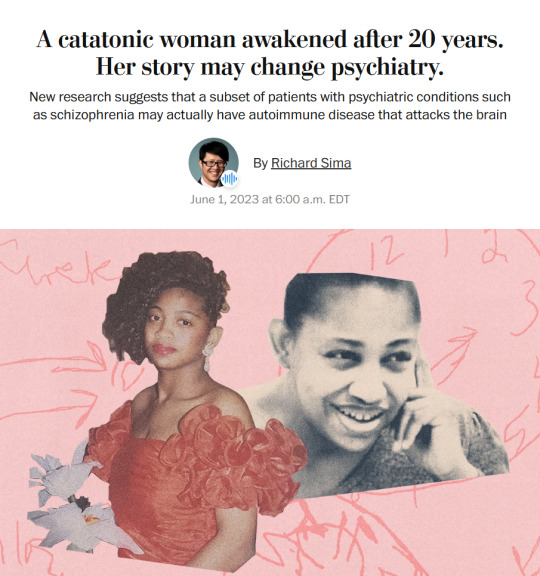
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes
Link
Highlights
SARS-CoV-2 spike protein persists in the skull-meninges-brain axis in COVID-19 patients
Spike protein is sufficient to induce brain pathological and behavioral changes in mice
Spike protein enhances brain vulnerability and exacerbates neurological damage in mice
mRNA vaccines reduce, but do not eliminate, the spike burden
#covid#long covid#pasc#research#study#cell host & microbe#journal#brain#neurology#neuroscience#brain damage#neurological damage#vaccines#vaccines work#get vaccinated
19 notes
·
View notes
Text
Thanks to our clever brains, it's not immediately noticeable to us, but our two nostrils are actually working independently in some ways and appear to have their own separate sense of smell. That's the conclusion of a new study from researchers in the US that could teach us much more about the brain and how senses are processed. The findings build on earlier studies in animals and humans, indicating that our brains might be capable of processing each nostril's input individually as well as synthesizing them into one complete whole. "Despite extensive work on odor responses in the olfactory system, relatively little is known about how information from the two nostrils is integrated and differentiated in the human olfactory system," write the researchers in their published paper.
Continue Reading.
89 notes
·
View notes
Text


the cuteness aggression i get from these two is gonna make me crash tf out
#karl reading dr0 like its the bible#scarposts#GOD why does he have to be an asshole 90% of the time#it just makes everything sweet he does or says 100x more impactful#matsunashi#i do love that double meaning about his research#Because he does care deeply for neurology#but he also care deeply for ryoko and junko#his research subject
7 notes
·
View notes
Text
Just remembered that there is a Sonic-Hedgehog gene and how if you discover a gene you get to name it whatever you want, time for me to dedicate my PhD to the up and coming Shadow-hedgehog gene
#and the amy rose gene#and the knuckle gene#i don’t even like genetics#but Im in neuro which is where Sonic hedgehog gene is sooo#sonic hedgehog#phdblr#sonic the hedgehog#shadow the hedgehog#Watch me#i’ll do it#neuroscience#sonic hedgehog gene#holoprosencephaly#it’s an embryology and neuroscience related thing#so cool#i love science#i Love neurology#i Love embryology#i love research#ahhhh geeking out
6 notes
·
View notes
Text
gotta wonder if extensive damage to the pinna wont somehow affect hearing and if so how/in what ways and would the same go for elves ie is mithrun’s hearing impaired?
#dungeon meshi#putting this in the tag because maybe hopefully some of yall have medical and or neurological knowledge and can#hypothesise w more validity#i tried looking it up but there’s not a whole lot of research on people having half their outer ear consumed by a demon#Late onset pinna loss.#I guess there are conditions you could compare this to but again I don’t really know enough to#Truly a certain whether those conditions are a comparable#ascertain*
9 notes
·
View notes
Text
i have a neurologist appointment in about a month that i'm quite nervous about due to previously being dismissed/not having my concerns listened to, so gonna post this to ask for some advice on getting Taken Seriously or if anyone knows things about the type of condition i might have about what i should be asking them to do/test.
might be quite long so putting it under a read more, and tw for medical stuff and doctors being dismissive. also i am So So Tired and therefore not able to think very clearly so apologies if i've messed up any of the medical info about conditions i mention and apologise just generally for the rambliness of my writing.
summary of why i'm going:
bunch of disabling symptoms that have continually progressed over the past 5+ years, including: muscle weakness, fatigue, muscle twitches/small spasms, nerve pain, blurry vision, lack of coordination (have this from autism, however has gotten significantly worse recently so might also be related to neuro stuff). first symptoms were difficulty having my arms over my head (like having to take multiple breaks while putting my hair into a ponytail because i couldn't hold my arms over my head for the like.. three minutes to do a ponytail) and blurry vision (that optometrist has said seems like might be due to a systemic disease because of how variable it is) since i was 13, which was seven years ago. i started getting more impairing symptoms when i was 15, and began needing a wheelchair for anything that required standing or walking for more than 10 - 15 minutes. i'm currently 20 and need my wheelchair whenever i leave the house, i can't leave the house or do things around the house often, i can stand for a max of like four minutes and can't hold my hands above my head for more than like 30 seconds to one minute. pretty much all my symptoms get a lot worse with any exertion.
GP thinks i have myasthenia gravis, but the test for acetylcholine receptor antibodies was negative and he doesn't have the ability to do other tests.
the neurologist has already said he thinks i have functional neurological disorder and that i should do CBT and pysio to improve my functioning (i already know CBT is horrible for me, i'm in other therapy which is good, i've done some psyio before but she just taught me some stretches and that was it, more psyio could be good but it'd have to be with someone who isn't trying to do a graded exercise therapy type thing since i get PEM). he has mentioned doing a spine MRI but this hasn't been done yet. he said he doesn't want to do further testing for myasthenia gravis but i will probably try to get him to agree to doing a repetitive nerve stimulation EMG or something.
i also have scapular winging on the side of my body with worse muscular symptoms which has also caused a lot of nerve pain, and i might also have some sort of spine issues (straightening of cervical lordosis was seen on a CT scan, they said it was probably due to muscle spasms, and i get a lot of neck pain which might be due to that? as well as a ton of back pain along my spine. might have CCI but haven't been tested yet). since it seems like i'm getting some structural changes in areas where i also get a lot of the pain and weakness and spasms i'm hoping if i bring that up the neurologist might maybe look more at organic causes + the state of those structural changes but i dunno.
he did a basic neurological exam in my initial appointment with him and said that i have give way weakness/waxing and waning weakness because when he got me to do the pushing my limbs against resistance i could do okay for a couple seconds but couldn't maintain it. he also said in the letter that i had positive hoovers sign however i am.. very confused by this because from my understanding hoovers sign is mainly looked at when someone has one limb that's at least somewhat "normal" and one that either can't be moved or is very weak, and then the person can't move the weak leg but when asked to push the stronger leg against resistance they push the weak leg down. both my legs are strong enough that i can stand and whilst one leg is a bit weaker they're relatively similar. i lifted and pushed against resistance with both legs so.... i am not sure how hoovers is applicable here? does anyone know why it was applied and if that was correct or if i should be challenging that? he's saying that the give way weakness and positive hoovers are indicators that the problem is "non-organic" and therefore should be treated with CBT and pysio.
i'm not sure what i think is actually going on. i think myasthenia gravis might make sense, but also so could other neuromuscular diseases like a mitochondrial disease or something. also very possible it's myalgic encephalomyelitis (aka chronic fatigue syndrome) but obviously that one is a diagnosis of exclusion so i want to rule other things out if possible. i want to know what's going on so i can have the best chance of being as well as is possible for me. i know CBT is not right for me and whilst some type of pysio could help a bit/prevent some decline (based on past experience i know it won't Cure Me but obviously it can help a bit to build some muscle or maintain range of motion and things like that which are important) if there's other things i can do on top of that i want to.
i've tried to do research to work out the best tests to ask for and i think EMG might be good but also know a normal EMG doesn't typically pick up myasthenia gravis so it needs to also have repetitive nerve stimulation i think?
i can't see a different neurologist at least not anytime soon, so i need to get this neurologist to do as much to help as possible. a social worker from where i get therapy is coming to the appointment to help me so that should be good but i need to work out what the best way to advocate for myself is and what tests are going to be the most useful to ask for.
if anyone has any advice for getting doctors to take you seriously or for any tests i should be advocating for or conditions i should be looking into or anything i would really appreciate it <3 (emoticon description: heart)
#in case it's relevant: i also have type one diabetes autism and POTS#things i've had ruled out : FSHD and multiple sclerosis (had brain mri and spinal tap) tho a nurse told me she thinks i should get checked#for multiple sclerosis again because it can have false negatives? not sure#FSHD was tested through a research project thing and the result was negatiev#medical tw#doctors tw#gonna put this in a couple of tags so people who have had similar experiences/might have advice might see it#cripplepunk#actually disabled#neurological disease#neuromuscular disease#ME/CFS
31 notes
·
View notes
Text
Why do dogs shake even when they are barely wet?
ITA version ESP version
Many furry mammals perform quick shakes to remove water and irritants from their fur, following a typical pattern of three shakes back and forth. But what is the mechanism that triggers this innate response? Dr. Dawei Zhang and his team from Harvard Medical School asked themselves this question and, in the lab, sought to understand it by using mice as a model.
The first step was to observe if different stimuli on the mice’s skin could trigger the “wet dog shake.” Researchers blew air on the mice, sprayed them with water, and even immersed them briefly in a bath. Surprisingly, a small drop of oil on the neck was enough to trigger the shake, suggesting that a light, annoying touch was the triggering factor.
At this point, the researchers aimed to understand which part of the nervous system “felt” this drop, initiating the shake response. They genetically modified some mice, eliminating specific skin receptors. First, they removed the receptors that perceive temperature changes, noting that the mice continued to shake. Temperature, therefore, was not a decisive factor. Then, they eliminated mechanoreceptors, which respond to tactile stimuli. This time, the mice shook far less than unmodified ones, suggesting that tactile sensitivity was key.
The team then focused on a specific group of mechanoreceptors, the low-threshold C fibers (C-LTMR), located around hair follicles and responsive to light touches. To confirm the hypothesis, the researchers used optogenetics, a technique that activates nerves with light. By stimulating the C-LTMR optically, the mice shook as if wet; blocking them, however, reduced the shake, confirming the role of the C-LTMR.
But the team also wanted to understand where the signals from C-LTMR travelled and which part of the brain processed them to generate the shake response. They traced the path of these signals, discovering they travelled from hair follicles to the spinal cord, and from there to a specific region of the brain called the parabrachial nucleus, which processes sensations like pain and itching. This pathway called the C-LTMR-spinoparabrachial circuit, turned out to be the mechanism behind the “wet dog shake.”
This discovery is significant because C-LTMR represents an evolved defence system that removes annoying stimuli like drops of water or parasites. Thanks to a system of specialized tactile receptors and neural pathways, shaking vigorously is the most efficient way for many mammals to eliminate these irritants.
What about humans? Like other mammals, we have something similar. Our receptors, called C-mechanoreceptors, have adapted to perceive pleasant sensations like caresses and hugs. Yet, many people feel a slight chill when someone lightly touches their neck. This reaction may be a distant “evolutionary memory” of the response that triggers the shake in dogs and other animals. In us, however, this reflex has lost its defensive function, transforming into a response linked to pleasure and social connection.
See you soon, and Good Science!
Source

#science#natural sciences#animal curiosities#animal behavior#neurology#tactile receptors#nervous system#defense mechanism#innate behavior#neuroscience#drops of science#research#scientific discovery#science education#science communication#animal biology#animals#ethology#dogs#mice#mouse
3 notes
·
View notes
Text
#science#science communication#scicomm#stem#science education#science blog#biology#neurology#neuroscience#medical research#medical science
9 notes
·
View notes
Text
Analyzing An Ataxic Dysarthria Patient's Speech with Computer Vision and Audio Processing
Hey everyone, so as you know I have been doing research on patients like myself who have Ataxic Dysarthria and other neurological speech disorders related to diseases and conditions that affect the brain. I was analyzing this file
with a few programs that I have written.
The findings are very informative and I am excited that I am able to explain this to my Tumblr following as I feel it not only promotes awareness but provides an understanding of what we go through with Ataxic Dysarthria.
Analysis of the audio file with an Intonation Visualizer I built
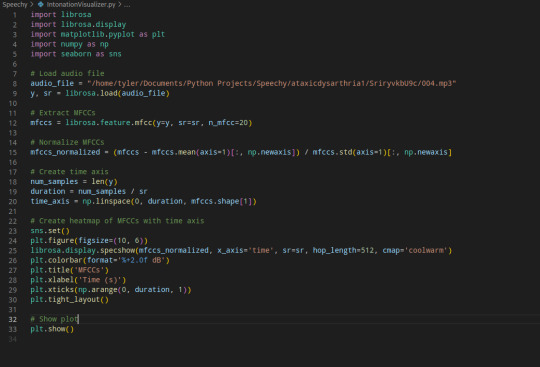
As you can tell this uses a heatmap to visualize loudness and softness of a speaker's voice. I used it to analyze the file and I found some really interesting and telling signs of Ataxic Dysarthria

At 0-1 seconds it is mostly pretty quiet (which is normal because it is harder for patients with AD to start their speaking off. You can notice that around 1-3 seconds it gets louder, and then when she speaks its clearer and louder than the patients voice. However the AD makes the patients speech constantly rise and fall in loudness from around -3 to 0 decibels most of the audio when the patient is speaking. The variation though between 0 and -3 varies quickly though which is a common characteristic in AD
The combination of the constant rising and falling in loudness and intonation as well as problems getting sentences started is one of the things that makes it so hard for people to understand those with Ataxic Dysarthria.
The second method I used is using a line graph (plotted) that gives an example of the rate of speech and elongated syllables of the patient.
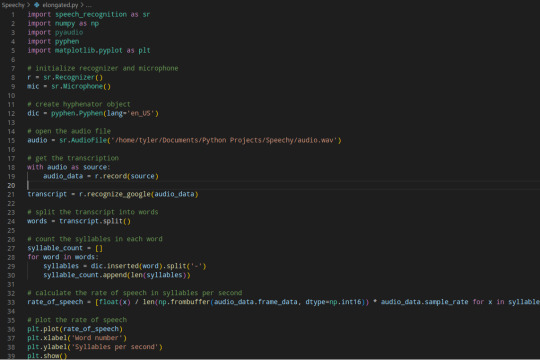
As you can see I primarily used the Google Speech Recognition library to transcribe and count the syllables using Pyphen via "hyphenated" (elongated) words in the speech of the patient. This isn't the most effective method but it worked well for this example and here is the results plotted out using Matplotlib:

As you can see when they started talking at first there was a rise from the softer speech, as the voice of the patient got louder, they were speaking faster (common for those with AD / and HD) my hypothesis (and personal experience) is that this is how we try to get our words out where we can be understood by "forcing" out words resulting in a rise and fall of syllables / rate of speech that we see at the first part. The other spikes typically happen when she speaks but there is another spike at the end which you can see as well when the patient tries to force more words out.
This research already indicates a pretty clear pattern what is going on in the patients speech. As they try to force out words, their speech gets faster and thus gets louder as they try to communicate.
I hope this has been informative for those who don't know much about speech pathology or neurological diseases. I know it's already showing a lot of exciting progress and I am continuing to develop scripts to further research on this subject so maybe we can all understand neurological speech disorders better.
As I said, I will be posting my research and findings as I go. Thank you for following me and keeping up with my posts!
#research#medical research#medical technology#speech pathology#speech disorder#neurology#ataxic dysarthria#ataxia#machine learning#artificial intelligence#ai#computer vision#audio processing#audio engineering#data analysis#data analyst#data science#python 3#python programming#python programmer#python code
40 notes
·
View notes
Text
"It’s long been supposed that implants could connect prosthetics to the brain in a way that stimulates nervous system commands with electrical signals.
Now, this idea is closer than ever to realization in a meaningful way, as one man paralyzed from the hips down is able to walk unsupported, even up stairs, thanks to such electrical nerve stimulation.
The patient, Gert-Jan Oskam, lost all movement in his legs after suffering a spinal cord injury in a motorbike accident. After using a precursor technology to gain back a little bit of mobility, Oskam enrolled in a proof of concept study to perhaps make further advances...
Now, with an implant in his brain, when Oskam thinks about moving his legs, it sends a signal to a computer he wears in a backpack that calculates how much current to send to a new pacemaker in his abdomen. It in turn sends a signal to the older implant in his spinal cord that prompts his legs to move in a more controllable manner. A helmet with antennae helps coordinate the signals.
The scientists developing the technology and working with him detail that he can walk around 200 meters a day, and stand unassisted for around 2-3 minutes. Once, Oskam details, there was some painting that needed to be done, but no one was around to help him. With the new technology, he simply took his crutch and did it himself.
youtube
Incredibly, after less than a year, and completely unexpectedly, scientists believe the technology closed the gap in his nervous system, and he can now lift himself out of a chair, and even walk with the help of a crutch, even when the device is turned off.
The scientists are planning in the future to work with patients with paralyzed arms and hands, and even with stroke victims, as the “digital bridge” is a massive advancement in nervous system stimulation technology."
-via Good News Network, June 16, 2023. Video via NBC News, May 24, 2023
#medical news#medical research#paralysis#neuroscience#nervous system#neurology#neuroplasticity#neuroplasticity is presumably the reason the “gap” in his nervous system closed?#and neuroplasticity is fucking amazing#the implications of this for medical science are potential HUGE#transhumanism#spinal cord injury#spinal cord stimulator#good news#hope#Youtube#cyberpunk
645 notes
·
View notes
Text
Book of the Day - The Brain That Changes Itself
Today’s Book of the Day is The Brain That Changes Itself, written by Norman Doidge in 2008 and published by Penguin. Norman Doidge M.D. is a psychiatrist, psychoanalyst, researcher, author, essayist, and not to forget, a poet. He is on the Research Faculty at Columbia University’s Center for Psychoanalytic Training and Research, in New York, and the University of Toronto’s Department of…
View On WordPress
#addiction#Book#book recommendation#book review#bookstagram#booktok#brain#depression#meditation#mindfulness#neurologic damage#Neuroplasticity#Neuroscience#Norman Doidge#Penguin Books#Raffaello Palandri#Research#science#The Brain That Changes Itself
20 notes
·
View notes
Text
SLYM, an abbreviation of Subarachnoidal LYmphatic-like Membrane.
The discovery of a new anatomic structure that segregates and helps control the flow of cerebrospinal fluid (CSF).
CSF plays not only in transporting and removing waste from the brain, but also in supporting its immune defenses.
Multiple sclerosis, central nervous system infections, and Alzheimer’s might be triggered or worsened by abnormalities in this structure.
A mesothelium divides the subarachnoid space into functional compartments
The central nervous system is lined by meninges, classically known as dura, arachnoid, and pia mater. We show the existence of a fourth meningeal layer that compartmentalizes the subarachnoid space in the mouse and human brain, designated the subarachnoid lymphatic-like membrane (SLYM)
10 notes
·
View notes
Text


“grumpy boy” as the tech called him got the diagnosis from the vet of “weird but not a crime”. they all loved him and said he is very handsome
we were told though he is an absolutely perfect health 🧡
#he does this weird shivering thing when he sleeps sometimes#only when he sleeps and it isn’t even all the time#wake him up and he stops#vet was baffled by it and did her research and it seems like as long as he doesn’t do it awake it isn’t neurological#but she wants videos for more research lmao#i love this little brat#santiago#cat#kitten
3 notes
·
View notes