#misogyny in medicine
Explore tagged Tumblr posts
Text
"Joy Spence, 21, said she visited emergency departments at two hospitals in St. John's over the course of nearly two weeks this May.
What began as weakness and abdominal pain on her right side quickly deteriorated into blacking out from the agony in her torso.
But no matter how dire her symptoms got, doctors kept sending her home.
"They would just tell me, 'Your bloodwork's normal, there's nothing we can do.' They would send me home, then same thing again," she said. "I would go back again. They would get me to do the bloodwork, say everything's normal."
Ultrasound and CT scans apparently turned up nothing, but Spence, in such severe pain, says she had no option but to keep returning to the hospital, where she says she was eventually left screaming in a waiting room, ignored by hospital staff.
"If somebody doesn't help me, I'm going to die," she recalls wailing, watching doctors and nurses pass her by.
At one point, she was dismissed outright by a walk-in clinic nurse, she adds.
"Somebody said to me, 'I don't know what you expect me to do,'" she said. "'You're a healthy 21-year-old young female.'"
One night, she says, her boyfriend had to help her into an ambulance. Spence was in so much pain she couldn't stay conscious and stand on her own.
"I remember the man in the ambulance telling me … how often he sees other young women going into the hospital and seeing them be misdiagnosed and not taken seriously," she said, speaking through tears.
"He said that he would do his best to … get things going for me."
Spence says she went to an ER at the Health Sciences Centre or St. Clare's Mercy Hospital about 10 times over a 12-day period, beginning on May 21. She also visited her family doctor, who could do little except tell her to speak directly to the surgeon at Health Sciences Centre, she said.
Each time she saw a doctor, she says, she was sent home and told to dance around her living room or do yoga to cure what physicians believed was anxiety or sluggish bowels.
"I had so many laxatives," Spence recalls. "I would tell them … nothing's even coming out anymore. It's not just this, I don't think. But no, they were dead set on the constipation and only constipation. Like, it can only be that."
...
Spence says doctors only began to take her seriously once she began vomiting in a Health Sciences Centre hallway. The contents of her stomach were green and black.
An older doctor walking past her happened to notice, stopping in his tracks. Spence says he immediately identified the issue as appendicitis.
At that doctor's urging, Spence was finally wheeled into an operating room, where she says her burst appendix — now gangrenous — was removed.
"I think when I walked into the room and they seen a 21-year-old young girl, they immediately dismissed me and thought that there couldn't be anything wrong with me," Spence said.
"I was not on their minds and not on their radar. And if they didn't have that preconceived idea of me, those thoughts wouldn't have been formed and maybe I would have gotten the proper care that I should have."
...
Spence is still struggling to recover from her ordeal. Physically, she's now fine: her appendix was removed and her stitches have healed.
But she's lost an alarming amount of weight, she says, wakes up gasping in the middle of the night and can't stop herself from crying whenever she remembers the hospital.
"I've been losing a lot of hair," she said. "Mentally, it's just been a struggle."
Spence only received an apology from the health authority after CBC News requested comment and confirmed that Spence had done an interview — a move she says felt hollow and frustrating, since the manager who called her didn't give her an explanation about why she was repeatedly ignored while waiting to be admitted.
The ripple effect from her illness, and how she says she was treated when seeking care, has uprooted her life. She's taken a year off her studies in Memorial University's social work program and has lost her job. She's looking for trauma therapy, but now doesn't have the money to pay for it, she says.
"I think as young women we're always told what we're supposed to do, how we're supposed to think, and not to trust our instincts," she said.
"But most of the time … the gut instinct is right. I knew I was sick. I knew what was happening wasn't right, and I could have died if I didn't keep going back to the hospital.
"If I had listened to those doctors and went back home — what could have really happened?""
#ableism#ableism in medicine#medical malpractice#medicine#medicine dismissing patients#misogyny in medicine#hospital management system
455 notes
·
View notes
Text
Italy declares itself as pro-choice yet grants gynaecologist the “right” to refuse to perform abortions based on their personal beliefs.
A country where getting an abortion is only feasible if you find a doctor who also thinks it should be legal (64.6% of gynaecologists do not), is far from a good representation of what pro-choice should look like
#radblr#radfem#women's rights#pro abortion#abortion#radical feminist safe#mysoginy#radical feminists do interact#feminism#medical malpractice#misogyny in medicine
15 notes
·
View notes
Text
Literally mentioned a pcos diagnosis and the doctor went on a fifteen minute rant about how it’s not a real thing, and if women just lost weight they’d be fine.
I was eventually able to break in and point out that my diagnosis was actually given when I was the “ideal” weight for my height and body frame, and the obesity came later as a side affect of medications I’m on for a separate issue completely.
Never seen a grown man backpedal so fast. He wrote all the prescriptions I asked for and ordered the tests I wanted without question, so it’s fine.
Still annoying.
no clue what causes pcos. no clue what causes endometriosis. 2 year waiting lists to see a gynecologist. you'd think female bodies only started existing 50 years ago
29K notes
·
View notes
Text
So, uh, great news.
My prescription's getting adjusted.
Bad news is it's been too low long enough for me to suspect at this point my thyroid is just dead.
What a weird time to live in. I got an appointment with one female doctor and instantly we figured out that my levels were too low, that I'm also Vitamin D deficient, and that shit would only get worse if I wasn't further taken care of.
After arguing for years with a male doctor to tell me just the basic numbers of my blood tests and if they were OK....
If you suspect something is wrong and your doctor won't validate or address your concerns, get a second opinion.
I'm going to see a new specialist. Hopefully they're nice and communicative.
#rant#doctor#my hashimotos experience#hashimotos#doctors#appointments#communciation#misogyny in medicine
0 notes
Text
Autoimmune breakthrough
A reminder of why diversity in science and testing is important
“Every cell in a woman’s body produces Xist,” Chang said. “But for several decades, we’ve used a male cell line as the standard of reference. That male cell line produced no Xist and no Xist/protein/DNA complexes, nor have other cells used since for the test. So, all of a female patient’s anti-Xist-complex antibodies — a huge source of women’s autoimmune susceptibility — go unseen.”
1 note
·
View note
Text
"I fully anticipate that some within the medical and scientific communities, as well as the public, will forcefully deny that paternal drinking matters. However, until doctors start asking the father about his drinking, we will never fully know the contributions of paternal alcohol exposure to birth defects and child health."
0 notes
Link
And just think of the thousands of other women who've dealt with similar experiences. Being called hysterical, overemotional, and ridiculous, for the same symptoms that would have a man being treated right away.
Because the medical field is simply not designed to treat us. Not many are aware that drug trials were done solely on men until a few decades ago and even now there aren't many done on women, since women had more complex hormonal cycles. Essentially, doctors decided women's health wasn't worth the work of testing drugs on female bodies, so drugs ended up being centered around the male body. Even today, not much research is done on specifically female illnesses. We have no cure for endometriosis, we don't have a known cause for it. Endometriosis is one of the most under-researched diseases there is (and the little research done is severely underfunded), despite the fact that it's believed it affects / will affect 10% of women. We have no general cure for vulvodynia, we don't even know what causes it. We haven't even managed to properly study and cure the most in-your-face medical problem women face, which is menstrual cramps; we just urge women to load up on painkillers. Literally this week (in 2023 for Christ's sake), the first research done on menstrual absorption products that actually used blood instead of water was published; conducted by a woman I'll add. In all the centuries women have existed and menstruated.
The medical industry is structured to ignore women as human beings deserving of care. At best, we are nuisances and bothers to doctors who mostly do not care about helping us. Until medicine becomes a female-dominated industry, we will not see a change in this.
Some reads on Endo:
Here:
And here:
https://www.medicalnewstoday.com/articles/endometriosis-why-is-there-so-little-research#:~:text=%E2%80%9CHistorically%2C%20with%20limited%20investment%20in,be%20found%2C%E2%80%9D%20it%20says.
Read on the new menstrual research:
(Something that I noticed in this article is that it brings up how the research on erectile dysfunction vs menstrual blood outnumbered it 10,000:400 in the same timespan, meaning the medical industry is researching something that will affect about half of men rather than something that will affect essentially all women.)
Early on a Wednesday morning, I heard an anguished cry—then silence.
I rushed into the bedroom and watched my wife, Rachel, stumble from the bathroom, doubled over, hugging herself in pain.
“Something’s wrong,” she gasped.
This scared me. Rachel’s not the type to sound the alarm over every pinch or twinge. She cut her finger badly once, when we lived in Iowa City, and joked all the way to Mercy Hospital as the rag wrapped around the wound reddened with her blood. Once, hobbled by a training injury in the days before a marathon, she limped across the finish line anyway.
So when I saw Rachel collapse on our bed, her hands grasping and ungrasping like an infant’s, I called the ambulance. I gave the dispatcher our address, then helped my wife to the bathroom to vomit.
I don’t know how long it took for the ambulance to reach us that Wednesday morning. Pain and panic have a way of distorting time, ballooning it, then compressing it again. But when we heard the sirens wailing somewhere far away, my whole body flooded with relief.
I didn’t know our wait was just beginning.
I buzzed the EMTs into our apartment. We answered their questions: When did the pain start? That morning. Where was it on a scale of one to 10, with 10 being worst?
“Eleven,” Rachel croaked.
As we loaded into the ambulance, here’s what we didn’t know: Rachel had an ovarian cyst, a fairly common thing. But it had grown, undetected, until it was so large that it finally weighed her ovary down, twisting the fallopian tube like you’d wring out a sponge. This is called ovarian torsion, and it creates the kind of organ-failure pain few people experience and live to tell about.
“Ovarian torsion represents a true surgical emergency,” says an article in the medical journal Case Reports in Emergency Medicine. “High clinical suspicion is important. … Ramifications include ovarian loss, intra-abdominal infection, sepsis, and even death.” The best chance of salvaging a torsed ovary is surgery within eight hours of when the pain starts.
* * *
There is nothing like witnessing a loved one in deadly agony. Your muscles swell with the blood they need to fight or run. I felt like I could bend iron, tear nylon, through the 10-minute ambulance ride and as we entered the windowless basement hallways of the hospital.
And there we stopped. The intake line was long—a row of cots stretched down the darkened hall. Someone wheeled a gurney out for Rachel. Shaking, she got herself between the sheets, lay down, and officially became a patient.
We didn’t know her ovary was dying, calling out in the starkest language the body has.
Emergency-room patients are supposed to be immediately assessed and treated according to the urgency of their condition. Most hospitals use the Emergency Severity Index, a five-level system that categorizes patients on a scale from “resuscitate” (treat immediately) to “non-urgent” (treat within two to 24 hours).
I knew which end of the spectrum we were on. Rachel was nearly crucified with pain, her arms gripping the metal rails blanched-knuckle tight. I flagged down the first nurse I could.
“My wife,” I said. “I’ve never seen her like this. Something’s wrong, you have to see her.”
“She’ll have to wait her turn,” she said. Other nurses’ reactions ranged from dismissive to condescending. “You’re just feeling a little pain, honey,” one of them told Rachel, all but patting her head.
We didn’t know her ovary was dying, calling out in the starkest language the body has. I saw only the way Rachel’s whole face twisted with the pain.
Soon, I started to realize—in a kind of panic—that there was no system of triage in effect. The other patients in the line slept peacefully, or stared up at the ceiling, bored, or chatted with their loved ones. It seemed that arrival order, not symptom severity, would determine when we’d be seen.
As we neared the ward’s open door, a nurse came to take Rachel’s blood pressure. By then, Rachel was writhing so uncontrollably that the nurse couldn’t get her reading.
She sighed and put down her squeezebox.
“You’ll have to sit still, or we’ll just have to start over,” she said.
Finally, we pulled her bed inside. They strapped a plastic bracelet, like half a handcuff, around Rachel’s wrist.
* * *
From an early age we’re taught to observe basic social codes: Be polite. Ask nicely.Wait your turn. But during an emergency, established codes evaporate—this is why ambulances can run red lights and drive on the wrong side of the road. I found myself pleading, uselessly, for that kind of special treatment. I kept having the strange impulse to take out my phone and call 911, as if that might transport us back to an urgent, responsive world where emergencies exist.
The average emergency-room patient in the U.S. waits 28 minutes before seeing a doctor. I later learned that at Brooklyn Hospital Center, where we were, the average wait was nearly three times as long, an hour and 49 minutes. Our wait would be much, much longer.
Everyone we encountered worked to assure me this was not an emergency. “Stones,” one of the nurses had pronounced. That made sense. I could believe that. I knew that kidney stones caused agony but never death. She’d be fine, I convinced myself, if I could only get her something for the pain.
By 10 a.m., Rachel’s cot had moved into the “red zone” of the E.R., a square room with maybe 30 beds pushed up against three walls. She hardly noticed when the attending physician came and visited her bed; I almost missed him, too. He never touched her body. He asked a few quick questions, and then left. His visit was so brief it didn’t register that he was the person overseeing Rachel’s care.
Around 10:45, someone came with an inverted vial and began to strap a tourniquet around Rachel’s trembling arm. We didn’t know it, but the doctor had prescribed the standard pain-management treatment for patients with kidney stones: hydromorphone for the pain, followed by a CT scan.
The pain medicine started seeping in. Rachel fell into a kind of shadow consciousness, awake but silent, her mouth frozen in an awful, anguished scowl. But for the first time that morning, she rested.
* * *
Leslie Jamison’s essay “Grand Unified Theory of Female Pain” examines ways that different forms of female suffering are minimized, mocked, coaxed into silence. In an interview included in her book The Empathy Exams, she discussed the piece, saying: “Months after I wrote that essay, one of my best friends had an experience where she was in a serious amount of pain that wasn’t taken seriously at the ER.”
She was talking about Rachel.
“Women are likely to be treated less aggressively until they prove that they are as sick as male patients.”
“That to me felt like this deeply personal and deeply upsetting embodiment of what was at stake,” she said. “Not just on the side of the medical establishment—where female pain might be perceived as constructed or exaggerated—but on the side of the woman herself: My friend has been reckoning in a sustained way about her own fears about coming across as melodramatic.”
“Female pain might be perceived as constructed or exaggerated”: We saw this from the moment we entered the hospital, as the staff downplayed Rachel’s pain, even plain ignored it. In her essay, Jamison refers back to “The Girl Who Cried Pain,” a study identifying ways gender bias tends to play out in clinical pain management. Women are “more likely to be treated less aggressively in their initial encounters with the health-care system until they ‘prove that they are as sick as male patients,’” the study concludes—a phenomenon referred to in the medical community as “Yentl Syndrome.”
In the hospital, a lab tech made small talk, asked me how I like living in Brooklyn, while my wife struggled to hold still enough for the CT scan to take a clear shot of her abdomen.
“Lot of patients to get to, honey,” we heard, again and again, when we begged for stronger painkillers. “Don’t cry.”
I felt certain of this: The diagnosis of kidney stones—repeated by the nurses and confirmed by the attending physician’s prescribed course of treatment—was a denial of the specifically female nature of Rachel’s pain. A more careful examiner would have seen the need for gynecological evaluation; later, doctors told us that Rachel’s swollen ovary was likely palpable through the surface of her skin. But this particular ER, like many in the United States, had no attending OB-GYN. And every nurse’s shrug seemed to say, “Women cry—what can you do?”
Nationwide, men wait an average of 49 minutes before receiving an analgesic for acute abdominal pain. Women wait an average of 65 minutes for the same thing. Rachel waited somewhere between 90 minutes and two hours.
“My friend has been reckoning in a sustained way about her own fears about coming across as melodramatic.” Rachel does struggle with this, even now. How long is it appropriate to continue to process a traumatic event through language, through repeated retellings? Friends have heard the story, and still she finds herself searching for language to tell it again, again, as if the experience is a vast terrain that can never be fully circumscribed by words. Still, in the throes of debilitating pain, she tried to bite her lip, wait her turn, be good for the doctors.
For hours, nothing happened. Around 3 o’clock, we got the CT scan and came back to the ER. Otherwise, Rachel lay there, half-asleep, suffering and silent. Later, she’d tell me that the hydromorphone didn’t really stop the pain—just numbed it slightly. Mostly, it made her feel sedated, too tired to fight.
If she had been alone, with no one to agitate for her care, there’s no telling how long she might have waited.
Eventually, the doctor—the man who’d come to Rachel’s bedside briefly, and just once—packed his briefcase and left. He’d been around the ER all day, mostly staring into a computer. We only found out later he’d been the one with the power to rescue or forget us.
When a younger woman came on duty to take his place, I flagged her down. I told her we were waiting on the results of a CT scan, and I hassled her until she agreed to see if the results had come in.
When she pulled up Rachel’s file, her eyes widened.
“What is this mess?” she said. Her pupils flicked as she scanned the page, the screen reflected in her eyes.
“Oh my god,” she murmured, as though I wasn’t standing there to hear. “He never did an exam.”
The male doctor had prescribed the standard treatment for kidney stones—Dilauded for the pain, a CT scan to confirm the presence of the stones. In all the hours Rachel spent under his care, he’d never checked back after his initial visit. He was that sure. As far as he was concerned, his job was done.
If Rachel had been alone, with no one to agitate for her care, there’s no telling how long she might have waited.
It was almost another hour before we got the CT results. But when they came, they changed everything.
“She has a large mass in her abdomen,” the female doctor said. “We don’t know what it is.”
That’s when we lost it. Not just because our minds filled then with words liketumor and cancer and malignant. Not just because Rachel had gone half crazy with the waiting and the pain. It was because we’d asked to wait our turn all through the day—longer than a standard office shift—only to find out we’d been an emergency all along.
Suddenly, the world responded with the urgency we wanted. I helped a nurse push Rachel’s cot down a long hallway, and I ran beside her in a mad dash to make the ultrasound lab before it closed. It seemed impossible, but we were told that if we didn’t catch the tech before he left, Rachel’s care would have to be delayed until morning.
“Whatever happens,” Rachel told me while the tech prepared the machine, “don’t let me stay here through the night. I won’t make it. I don’t care what they tell you—I know I won’t.”
Soon, the tech was peering inside Rachel through a gray screen. I couldn’t see what he saw, so I watched his face. His features rearranged into a disbelieving grimace.
By then, Rachel and I were grasping at straws. We thought: cancer. We thought: hysterectomy. Lying there in the dim light, Rachel almost seemed relieved.
“I can live without my uterus,” she said, with a soft, weak smile. “They can take it out, and I’ll get by.”
She’d make the tradeoff gladly, if it meant the pain would stop.
After the ultrasound, we led the gurney—slowly, this time—down the long hall to the ER, which by then was completely crammed with beds. Trying to find a spot for Rachel’s cot was like navigating rush-hour traffic.
Then came more bad news. At 8 p.m., they had to clear the floor for rounds. Anyone who was not a nurse, or lying in a bed, had to leave the premises until visiting hours began again at 9.
When they let me back in an hour later, I found Rachel alone in a side room of the ER. So much had happened. Another doctor had told her the mass was her ovary, she said. She had something called ovarian torsion—the fallopian-tube twists, cutting off blood. There was no saving it. They’d have to take it out.
Rachel seemed confident and ready.
“He’s a good doctor,” she said. “He couldn’t believe that they left me here all day. He knows how much it hurts.”
When I met the surgery team, I saw Rachel was right. Talking with them, the words we’d used all day—excruciating, emergency, eleven—registered with real and urgent meaning. They wanted to help.
By 10:30, everything was ready. Rachel and I said goodbye outside the surgery room, 14 and a half hours from when her pain had started.
* * *
Rachel’s physical scars are healing, and she can go on the long runs she loves, but she’s still grappling with the psychic toll—what she calls “the trauma of not being seen.” She has nightmares, some nights. I wake her up when her limbs start twitching.
Sometimes we inspect the scars on her body together, looking at the way the pink, raised skin starts blending into ordinary flesh. Maybe one day, they’ll become invisible. Maybe they never will.
44K notes
·
View notes
Text

source

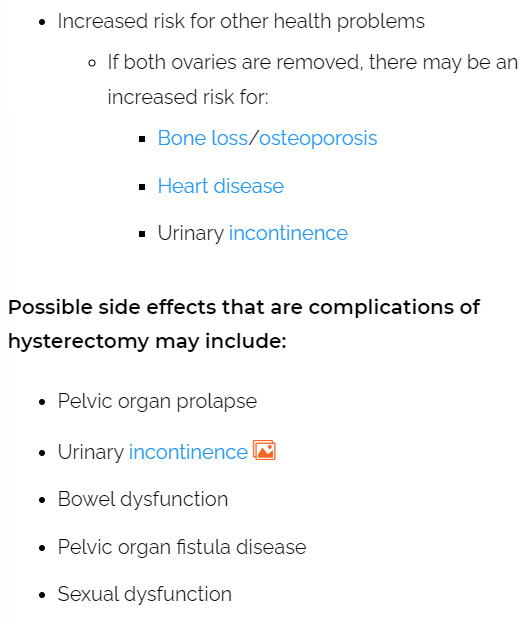
source
and, probably the most interesting thing I have read so far about uteruses:

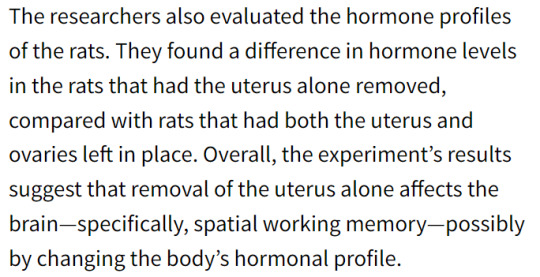
source
"the uterus is only for making babies and if I don't want to have babies I actually don't need it and they can just cut it out" is really just medical misogyny but you aren't ready for that conversation
#radical feminism#reproductive health#uterus#hysterectomy#transmen#transmasc#transmasculine#terfs#sex essentialism#medical misogyny#medical essentialism#medicine#birthing person#queer#radical feminists please touch#radfem safe#trans#transgender
1K notes
·
View notes
Text
The ongoing war in Sudan and the ensuing humanitarian crisis has pushed people to the brink. At the borders of conflict zones, selling a kidney is becoming a currency of last resort for people seeking refuge. In June 2023, I managed to contact two young Sudanese women who had fled the fighting in Khartoum. In April 2023, Rania was with her friend Fatima, both students at the University of Khartoum, when the RSF raided the main campus, on the banks of the Nile. “We were trying to hide from the fighting,” Rania told me on the phone. “There were a lot of [female] students there who were afraid to leave. We thought we would be safe, but they found us and forced us to have sex with them.”
Soon after that they packed up their belongings and took a bus heading towards the border with South Sudan. They had heard the route south was cheaper than trying to go north to Egypt, and Rania had a brother living in Kampala, Uganda, whom they hoped to join. It was a seven-day journey from Khartoum to Renk, a small town in South Sudan close to the border where thousands of people had set up temporary camps in bleak conditions. A lack of food, water, healthcare and sanitation had left people at increased risk of disease, malnutrition and violence. There were hundreds of new arrivals each day. “People are crammed together under tarpaulins,” Rania said. “There are mosquitoes everywhere. There’s not enough food, water, soap. Everyone is desperate for assistance. It’s chaos.”
When Rania and Fatima arrived at a makeshift camp on the outskirts of the town, they were approached by soldiers in plain clothes selling tickets for flights from a small airstrip outside Renk to South Sudan’s capital, Juba, and the city of Nimule. The flights, which should form part of the humanitarian corridor, are being controlled by armed militias charging exorbitant fees to board them. “They wanted a lot of money,” Rania said. “The price would go up every day. They said if we didn’t have any money we could have sex with them.”
When they refused, they were told there was something else they could sell: a kidney. “They said that this was the only way we were going to get a flight out of here,” Fatima said. “There were two men who had agreed to this [selling a kidney], but I don’t know what happened to them. I was worried that they would kill me and take my kidney.”
Two weeks after Rania and Fatima first arrived in Renk, they messaged me from Kampala. “We received some money from family members in Uganda. They paid a smuggler $500 to take us to Kampala.” Raina said. “There were no humanitarian agencies or government officials transporting people. The drivers, the militias, they are exploiting people every step of the journey.”
In Renk, they had watched as large trucks carried hundreds of people further south to transit camps that were rumoured to be less crowded and better resourced. Others boarded cramped and overcrowded boats down the Nile to the city of Malakal, from which they would attempt to reach Juba, 970km to the south. Each stage of the journey would come at a cost.
“We are telling you this for a reason,” Fatima said. “We desperately need more support for people trapped in Sudan. In Darfur, there is genocide. But no one is talking about it. Women are being raped every day. Children have been killed and abducted. People are desperate. This is when you sell your kidney.”
— ‘For me, there was no other choice’: inside the global illegal organ trade
#seán columb#‘for me there was no other choice’: inside the global illegal organ trade#current events#medicine#medical ethics#sociology#poverty#exploitation#war#immigration#refugees#human trafficking#organ transplantation#organ trafficking#misogyny#rape#sudanese civil war#war in darfur#sudan#uganda#south sudan#darfur#khartoum#renk#kampala#university of khartoum#rapid support forces#kidneys
45 notes
·
View notes
Text
I'm going to provide advice so that anyone American and younger than me can skip over this unwanted experience:
When you show up to an Urgent Care or a doctor's office for a medical concern and after briefing them on your issue they then ask you, "What are you hoping to get out of this visit?", or, "What are you hoping for us to do?"—or any variation thereof that essentially is a gaslighting form of "So what do you expect us to do?"
Either have a direct plan in mind, i.e., "I'm hoping you will test my glucose levels", "I'm hoping you can rule out the flu", etc.
Or return the question and ask, "What tests can you do to determine the cause of [symptom]?"
Or "based on my symptoms I'm hoping you're able to provide me with a referral to this type of specialist".
I have learned to do this only after several times showing up and being ask this, and then feeling hurt and angry because I want them to take professional responsibility for going through the process in figuring out my medical issues based on my concerns. Instead I have been mostly approached with what seems like very performative confusion and as if I shouldn't have never come to them. There's been so many times I've left somewhere without getting any help or answers.
So the last time I did this the Urgent Care doctor wasn't expecting me to clearly state what tests I wanted done that I knew they were able to do at an Urgent Care. So she asked me again, and I just stared blankly and repeated myself followed with, "Are you able to do these tests?" And I got the tests.
87 notes
·
View notes
Text
This shit kills women and nobody even cares. Not the medical industry, and certainly not men.
From heart disease to IUDs: How doctors dismiss women’s pain
Several studies support the claim that gender bias in medicine routinely leads to a denial of pain relief for female patients for a range of health conditions
One woman was told she was being “dramatic” when she pleaded for a brain scan after suffering months of headaches and pounding in her ears. It turned out she had a brain tumor. Another was ignored as she cried out in pain during a 33-hour labor. She was supposed to be getting pain medication through her epidural, but it had fallen out. Dozens of women complained of torturous pain as their vaginal walls were punctured during an egg retrieval process. They were told their pain was normal, but, in actuality, they were getting saline instead of anesthesia. These are just some of the stories of women who say their pain and suffering has been dismissed or misdiagnosed by doctors. Although these are anecdotal reports, a number of studies support the claim that women in pain often are not taken as seriously as men.
This year, the Journal of the American Heart Association reported that women who visited emergency departments with chest pain waited 29 percent longer than men to be evaluated for possible heart attacks. An analysis of 981 emergency room visits showed that women with acute abdominal pain were up to 25 percent less likely than their male counterparts to be treated with powerful opioid painkillers. Another study showed that middle-aged women with chest pain and other symptoms of heart disease were twice as likely to be diagnosed with a mental illness compared with men who had the same symptoms. “I was told I knew too much, that I was working too hard, that I was stressed out, that I was anxious,” said Ilene Ruhoy, a 53-year-old neurologist from Seattle, who had head pain and pounding in her ears. Despite having a medical degree, Ruhoy said she struggled to get doctors to order a brain scan. By the time she got it in 2015, a tennis ball-sized tumor was pushing her brain to one side. She needed surgery, but first, she rushed home, hugged her 11-year-old daughter and wrote her a letter to tell her goodbye.
Ruhoy did not die on the operating table, but her tumor had grown so large it could not be entirely removed. Now, she has several smaller tumors that require radiation treatment. She said many of her female patients have had experiences similar to hers. “They’re not validated with regards to their concerns; they’re gaslit; they’re not understood,” she said. “They feel like no one is listening to them.”
Doubts about women’s pain can affect treatment for a wide range of health issues, including heart problems, stroke, reproductive health, chronic illnesses, adolescent pain and physical pain, among other things, studies show. Research also suggests that women are more sensitive to pain than men and are more likely to express it, so their pain is often seen as an overreaction rather than a reality, said Roger Fillingim, director of the Pain Research and Intervention Center of Excellence at the University of Florida. Fillingim, who co-wrote a review article on sex differences in pain, said there are many possible explanations, including hormones, genetics and even social factors such as gender roles. Regardless, he said, “you treat the pain that the patient has, not the pain that you think the patient should have.”
Women say reproductive health complaints are commonly ignored
Women often cite pain bias around areas of reproductive health, including endometriosis, labor pain and insertion of an intrauterine device, or IUD. When Molly Hill made an appointment at a Connecticut clinic in 2017 to get an IUD, she said she was warned it would be uncomfortable, but she was not prepared for “horrific” pain. Hill, now 27 and living in San Francisco, recalled that during the procedure, she began crying in pain and shouted at the doctor to stop. “We’re almost done,” she said the doctor told her and continued the procedure. “It was full-body, electrifying, knife-stabbing pain,” she said. After it was done, she said she lay sobbing on the table in physical and emotional pain. “It felt violating, too, to have that pain that deep in your core where you feel the most vulnerable.”
Studies consistently show that women who have not experienced vaginal birth have much higher pain during IUD insertion compared with women who have given birth. A Swedish study found that among 224 women who had not given birth, 89 percent reported moderate or severe pain. One in six of the women said the pain was severe. Although numbing agents and local anesthetics are available, they are rarely used.
In some cases, women have sued physicians for ignoring their pain. Dozens of women sued Yale University claiming that during an egg harvesting procedure at its infertility clinic, they were supposed to be receiving the powerful painkiller fentanyl. But some women were getting only diluted pain medication or none at all, according to lawsuits filed in the state Superior Court in Connecticut. Later, the clinic discovered a nurse had been stealing vials of fentanyl and replacing the painkiller with saline solution. The nurse pleaded guilty last year and was sentenced for tampering with the drugs. One of the plaintiffs, Laura Czar, wrote about her experience for Elle magazine, describing it as “a horrible, gut-wrenching pain,” and told a doctor at the time, “I can feel everything you’re doing.” Despite her protests, the doctor continued. Yale said in a statement that it “deeply regrets” the women’s distress and has “reviewed its procedures and made changes to further oversight of pain control and controlled substances.”
Racial disparities in pain management
For Sharee Turpin, the pain of sickle-cell disease sometimes feels like tiny knives slicing her open. Sickle cell disease is an inherited blood disorder that can cause suffering so severe, its attacks are called “pain crises.” But when Turpin, who is Black, experiences a pain crisis, the 34-year-old does not rush to the ER in Rochester, N.Y. Instead, she combs her hair, mists some perfume and slips on her “Sunday best” in hopes that the doctors and nurses won’t peg her as a drug seeker, she said. Sometimes, Turpin gets a care team that understands her pain. Other times, she is treated as a bother. “I’ve even been told ‘shut up’ by a nurse because I was screaming too loud while I was in pain,” she said.
Abundant research shows racial bias in pain treatment. A 2016 study found half of white medical students and residents held at least one false belief about biological differences between Blacks and Whites, and were more likely to underestimate Black patients’ pain. “The management of pain is one of the largest disparities that we see between Black people and White people in the American health-care system,” said Tina Sacks, an associate professor at the University of California at Berkeley and author of “Invisible Visits: Black Middle-Class Women in the American Healthcare System.”
Labeling women “hysterical” or blaming psychological causes
Research shows men in chronic pain tend to be regarded as “stoic” while women are more likely to be considered “emotional” and “hysterical” and accused of “fabricating the pain.” Carol Klay, a 68-year-old from Tampa, had endured years of chronic pain from arthritis, degenerative disk disease and spinal stenosis. During a hospital stay last year, her doctor noted in her medical record that she was crying “hysterically.” Klay said she was crying because she was unable to sit, stand or walk without agony, and the doctor had removed morphine from her cocktail of pain medications. She wonders whether the doctor “would have called me hysterical if I was a man,” she said. Tampa General Hospital said it could not discuss specific patients, but stated: “Patient treatment plans, including medication orders to reduce pain, are prescribed by multi-disciplinary clinical teams.” Research shows women’s physical pain is also often attributed to psychological causes.
Jan Maderios, a 72-year-old Air Force veteran from Chipley, Fla., said the trauma of having pain dismissed by doctors has stayed with her for years. She saw about a dozen doctors in the early 1970s for pelvic pain. When clinicians could not identify the cause of her pain, she was referred to a psychiatrist.
“You start to doubt yourself after so many medical experts tell you there’s nothing wrong with you,” she said. After a hysterectomy in 1976, Maderios learned that fibroid tumors in her uterus had been the source of her pain. She said learning her pain was real — and physical — “made all the difference in the world.”
Why women’s pain complaints often aren’t taken seriously
During a 33-hour labor with her first child in 2011, Anushay Hossain, 42, of D.C., opted for epidural pain relief but said she still felt it all — every contraction, every cramp and every dismissal of her pain by her medical team. The doctor reassured her that she was getting the maximum dosage of pain medication.
In fact, she wasn’t getting any at all. She said her epidural had slipped out. By the time the error was caught, she was shaking uncontrollably and in need of an emergency Caesarean section, she said. “There’s a pain gap, but there’s also a credibility gap,” said Hossain, author of “The Pain Gap: How Sexism and Racism in Healthcare Kill Women.” “Women are not believed about their bodies —period.”
This pain gap may stem, in part, from the fact that women have historically been excluded from medical research. It wasn’t until 2016 that the National Institutes of Health (NIH) required sex to be considered as a biological variable in most studies it funded. “We’re making progress,” said David Thomas, special adviser to the director of NIH’s Office of Research on Women’s Health. “But we do have a long way to go because there’s this whole institutional approach to doing research — pain and beyond — where it tends to be male-focused.”
Nearly 95 percent of U.S. medical school students said instruction on sex and gender differences in medicine should be included in curriculums, according to a 2015 survey. But only 43 percent said their curriculum had helped them understand those differences and only 34.5 percent said they felt prepared to manage them in a health-care setting.
“It is changing, but it’s changing very slowly,” said Janice Werbinski, immediate past president of the American Medical Women’s Association and chair of the mentorship committee of the association’s Sex and Gender Health Collaborative.
How women can advocate for better pain care
It took decades to solve the mystery of Maureen Woods’s chronic pain. Woods, 64, of Myersville, Md., started having joint pain in her teens and, over the years, told dozens of doctors her pain was “debilitating,” she said. Some told her it was all in her head. In 2017, she was diagnosed with hypermobile Ehlers-Danlos syndrome, a connective tissue disorder often causing loose joints, dislocations and chronic pain. She said women who are not being heard should keep advocating for themselves. “You have to go with your gut — something is wrong and I need to find a doctor who can figure it out,” she said. Marjorie Jenkins, dean of the University of South Carolina School of Medicine Greenville, urged women against feeling pressured to accept an “everything is normal” non-diagnosis. “If your provider does not appear to be listening to you or believing what you’re saying, then you need a new provider,” Jenkins said. “You are the client, you are the customer and you are the owner of your health.”
Women can also take a family member, friend or other support person who can corroborate their stories, said Alyson McGregor, an emergency medicine professor at the University of South Carolina School of Medicine Greenville and author of the book “Sex Matters: How Male-Centric Medicine Endangers Women’s Health and What We Can Do About It.” Particularly in emergency departments, she said, there can be an inherent bias. “There’s this assumption that women are emotional and they’re anxious and that that’s the main issue,” she said.
542 notes
·
View notes
Note
Hey. How are you?
Not good. I hope you have heard of what happened in RG Kar Medical College in my city? I am not exaggerating when I say that I am actually fearing for my life right now and thinking of quitting the profession. Because where is our safety? I had kind of already become numb to the invisible misogyny in the field (my male co-interns are addressed as "doctor" but I am always "didi") but this... This goes beyond words. Can anyone just barge in and rape and murder a female doctor while she is ON DUTY at night? Is our life so cheap?
Just this Wednesday, (literally the night before the incident), at 4 am, when I went to catch some sleep in our tiny unit room, and was walking through the empty surgery ward corridors, no nurses, no guards, NOTHING, the thought crossed my mind that if someone was to enter the room while I was sleeping, no one would even be able to hear me scream, not even my male co-intern sleeping in the next room. And mind you, NOTHING had happened at that point. No one had given me a dirty glance, no one had threatened me or anything. It was just a base level of fear that I, as a woman, was operating under. And somehow that is NORMALIZED.
Sorry for the vent, I am just so scared and tired. Because the victim literally could have been ANYONE. Hell, it could have been me had someone actually barged into my room that night. And that scares me a lot
#ask me anything#ask reply#ask#original post#not incorrect quotes#medblr#medicine#ambidextrousarcher#desi tag#desi#desi tumblr#desiblr#misogyny#india#bangla#bengali#banglable#bengblr#bengaliblr#kolkata
55 notes
·
View notes
Text
Medical research has a major problem: an alarmingly high number of trials are based on fake, fraudulent or misinterpreted data.
Research misconduct sleuths call them “zombie” studies. They look like real research papers but they’re rotten to the core. And when these studies go on to influence clinical guidelines, that is, how patients are treated in hospitals and doctors’ rooms, they can be dangerous.
Professor Ben Mol, head of the Evidence-based Women’s Health Care Research Group at Monash University, is a professional zombie hunter. For years, he has warned that between 20 and 30 per cent of medical trials that inform clinical guidelines aren’t trustworthy.
“I’m surprised by the limited response from people in my field on this issue,” he says. “It’s a topic people don’t want to talk about.”
The peer review process is designed to ensure the validity and quality of findings, but it’s built on the assumption that data is legitimate.
Science relies on an honour system whereby researchers trust that colleagues have actually carried out the trials they describe in papers, and that the resulting data was collected with rigorous attention to detail.
But too often, once findings are queried, researchers can’t defend their conclusions. Figures such as former BMJ editor Richard Smith and Anaesthesia editor John Carlise argue it’s time to assume all papers are flawed or fraudulent until proven otherwise. The trust has run out.
“I think we have been naive for many years on this,” Mol says. “We are the Olympic Games without any doping checks.”
How bad science gets into the clinic
Untrustworthy papers may be the result of scientists misinterpreting their data or deliberately faking or plagiarising their numbers. Many of these “zombie” papers emerge from Egypt, Iran, India and China and usually crop up in lower-quality journals.
The problem gets bad when these poor-quality papers are laundered by systematic reviews or meta-analyses in prestigious journals. These studies aggregate hundreds of papers to produce gold-standard scientific evidence for whether a particular treatment works.
Often papers with dodgy data are excluded from systematic reviews. But many slip through and go on to inform clinical guidelines.

My colleague Liam Mannix has written about an example of this with the hormone progesterone. Official guidelines held that the hormone could reduce the risk of pre-term birth in women with a shortened cervix.
But those guidelines were based on a meta-analysis largely informed by a paper from Egypt that was eventually retracted due to concerns about the underlying data. When this paper was struck from the meta-analysis, the results reversed to suggest progesterone had no preventative effect.
There’s a litany of other examples where discounting dodgy data can fundamentally alter the evidence that shapes clinical guidelines. That’s why, in The Lancet’s clinical journal eClinical Medicine, Mol and his colleagues have reported a new way to weed out bad science before it makes it to the clinic.
Holding back the horde
The new tool is called the Research Integrity in Guidelines and evIDence synthesis (RIGID) framework. It mightn’t sound sexy, but it’s like a barbed-wire fence that can hold back the zombie horde.
The world-first framework lays out a series of steps researchers can take when conducting a meta analysis or writing medical guidelines to exclude dodgy data and untrustworthy findings. It involves two researchers screening articles for red flags.
“You can look at biologically implausible findings like very high success rates of treatments, very big differences between treatments, unfeasible birth weights. You can look at statistical errors,” says Mol.
“You can look at strange features in the data, only using rounded numbers, only using even numbers. There are studies where out of dozens of pairs of numbers, everything is even. That doesn’t happen by chance.”
A panel decides if a paper has a medium to high risk of being untrustworthy. If that’s the case, the RIGID reviewers put their concerns to the paper’s authors. They’re often met with stony silence. If authors cannot address the concerns or provide their raw data, the paper is scrapped from informing guidelines.
The RIGID framework has already been put to use, and the results are shocking.
In 2023, researchers applied RIGID to the International Evidence-based Guidelines for Polycystic Ovary Syndrome (PCOS), a long misunderstood and misdiagnosed syndrome that affects more than 1 in 10 women. As a much maligned condition, it was critical the guidelines were based on the best possible evidence.
In that case, RIGID discounted 45 per cent of papers used to inform the health guidelines.
That’s a shockingly high number. Those potentially untrustworthy papers might have completely skewed the guidelines.
Imagine, Mol says, if it emerged that almost half of the maintenance reports of a major airline were faked? No one would be sitting around waiting for a plane to crash. There would be swift action and the leadership of the airline sacked.
#australia#women's health#medical misogyny#radblr#this feels particularly important with the huge gender data gap in medicine and the cass review's findings of bad research in the UK
78 notes
·
View notes
Text
So I'd like to shift my critical gaze for just a moment to focus on the institution of western medicine. Let's remember that men founded it, with the help of the Catholic Church, by torturing and murdering millions of women practicing indigenous health care in Europe during the women's holocaust, the Burning Times. (Indigenous systems of health care around the world are still being destroyed today and replaced by systems based on the consumptive western model.) These self-styled doctors consolidated their power by denying women access to medical education, while making medical education a prerequisite for the practice of health care. Since then, among other things, medical men have pathologized (in order to "treat" and control) the natural body experiences of womanhood—menarche, menstruation, pregnancy/childbirth and menopause. They cut out our clitorises if we showed too much interest in sex and locked us in mental institutions when our husbands wanted control of our property. They prescribed us, our mothers or grandmothers the dalkon shield, thalidomide, diethyl-stilbestrol, silicone breast implants, and hormone replacement therapy by the millions. They sterilized thousands of women without their consent. They perform "medical research" on people in prison or mental hospitals without their consent. For a hefty fee, they are happy to surgically remove a chunk of nose, breasts, or stomach so we can better fit the cultural beauty imperative of the moment. They capitalize on the confusion of women who don't fit the "feminine" stereotype, handing out a convenient diagnosis, bilateral mastectomies and a lifetime prescription for testosterone. They routinely announce discoveries about "human" health based on studies with only male subjects. They believe the despair and rage of women who have been raped, sexually abused, battered or just overworked are appropriately and sufficiently addressed with Prozac. They cannot conceive of a woman collecting information, interpreting it, and coming to a conclusion different from theirs; the only word in their vocabulary for a patient who does not follow a doctor's advice is "noncompliant." In short, this system and its adherents are not on the side of women.
-Amy Winter, “Women, Health, and the Politics of Fat” in Rain and Thunder, Autumn Equinox 2003
40 notes
·
View notes
Text
What they could have looked into is this relationship between early PIV sex and endometriosis. Maybe there's some sort of damage that can come from being young and sexually active, that can kickstart it or make it worse?
Instead, they pull this weird marker of "attractive = endometriosis". As if science waits around to find out out a woman is hot before spreading to her a deadly disease. Men need to be kept out of medicine.
did yall know that a study done on the perception of attractiveness to men of women with endometriosis. we scored higher than the baseline in every category but waist to hip ratio. anyways there’s no new or non hormonal treatments that are receiving any funding so i’ll just die i guess
2K notes
·
View notes
Text
The fact that most women are taking wrong dosage of medicine because they were tested upon men only which is causing long term side effects is proof the world is male centered.
#Medicine Misogyny#gender bias#medicine#radblr#radical feminism#radical feminists do interact#radical feminists do touch#terfsafe#radical feminist safe#trans exclusionary radical feminist#healthcare#women health
58 notes
·
View notes