#mast cell disorders
Explore tagged Tumblr posts
Text
why the fuck is my immunologist allowed to just... not write a prescription for a refill of my mast cell stabilizers without warning. I have MCAS. I am allergic to literally everything. OTC antihistamines hardly put a dent in my allergies, even if i quadruple the doses (which is generally the highest you can safely go).
i could literally die without these meds.
#guess ill die#MCAS#mast cell activation syndrome#mast cell activation disorder#mast cell disorders#disabled#actually disabled#chronically ill#chronic illness#allergies#healthcare
22 notes
·
View notes
Text
I don’t see other people discussing mast cell disorders much (they’re pretty rare, so no criticism is implied by that comment) but I have a family member who was diagnosed pretty late in life with a mast cell disorder, and counted lucky to get diagnosed in just a few years after it got bad. Another family member had celiac long before gluten free became cool, so “is there a restaurant we can trust to not poison/kill family members we can meet at?/somebody is bringing food everyone can safely eat, right?” has been a concern for family gatherings for my extended family my entire life.
Anyways, the fad of gluten free eating involved both a lot of annoying and obviously dishonest people inadvertently convincing others that “gluten free” people are all dishonestly being obnoxious on purpose AND people who discovered they had an undiagnosed sensitivity or allergies to wheat or wheat pesticides or something because they felt a lot better when they didn’t eat gluten.
The reason some people are irritated about gluten free labels isn’t so much because of complex psychological process around the food system; these people generally don’t like seeing kosher or halal labels either, because they’re all seen as a “kiss the ring” submission to or alliance with a group they see as in conflict with their group. People don’t like to buy products they see as supporting or submitting to groups they consider hostile to them; the left-libs do that too.
I don’t think that gluten free is entirely a left-lib dog whistle at this point though, given that Akins/keto is, as mentioned above, right wing coded and gluten free is adjacent to that, and adjacent to Asian cuisine (all that rice) and kosher, and well, it’s JAWs for a reason.
it is weird that celiac stuff has become part of the 'culture war'. because it's literally just a medical thing.... I get super anemic unless I cut a certain protein out of my diet, because it bulldozes the villi in my intestines. but if I post about it, right-wingers send me gore images. I guess you can't expect shitty people to be logical, but I've even heard lefty people make fun of gluten stuff, and it's like why are you mad about this??? why are you pissed off that I'm eating bread that doesn't taste as good so that I can have blood in my body? it's so morally neutral.
#mast cell activation syndrome#mast cell disorders#gluten free#food#boycott#big ag#diet and exercise#kosher#race in america#wheat and wheat biproducts#celiac#no war but culture war#keto#clearing the drafts
32K notes
·
View notes
Text
we are about an hour into rare disease day in my timezone! (it's always the last day of february, whether that's the 28th or the 29th.) the true prevalence of mast cell disorders is unknown, as they are often misdiagnosed or ignored. and mast cell activation syndrome, the most prevalent kind of mast cell disorder, only had diagnostic criteria laid out for the first time in 2010. so whether or not it's truly rare is really up in the air!
(personally I suspect it is just aggressively underdiagnosed but I'm not a research scientist or diagnostician right now. and even if it is rare, it's gonna be a lot less so than it was 5 years ago as certain respiratory infections are known to trigger it into visibility. that's what happened to me when I got mono at the end of 2015, further compounded when I got covid in 2022.)
all chronically ill people face a lot of hurdles when it comes to seeking diagnosis, accommodation, and treatment (all of which can be severely complicated by any intersecting marginalities), but rare diseases present a special challenge.
for example, I have an immune disorder. my immune system does not like being alive, my mast cells are way too jumpy and throw a tantrum over every little thing. you'd think an immunologist would be the one to treat me, right?
I've had 6 immunology referrals rejected in the past 9 months alone. multiple major immunology clinics in my major city tied to a major research university outright refuse to see patients with "mcas" written anywhere in their chart.
after 8 years of being debilitatingly ill, and suspecting it was immune mediated for 6, and getting it confirmed beyond a shadow of a doubt by the bone marrow biopsy last month, I will have my second ever appointment with an immunologist. another 2 1/2 months from now. the first immunologist lied to me about the reliability of the one available blood test, when I first came up with the hypothesis by myself 6 years ago, and forced me to abandon my (correct!!! now proven!!!) hypothesis for 3 entire years while we wandered around lost and got nowhere other than even more thorough process of elimination.
okay, well if my immune system is attacking me, maybe it's technically autoimmune? that's the rheumatologists instead of the immunologists, what do they have to say? dick all my dude, I don't have rheumatoid arthritis so they just shrug at me and go "idk, fibro? I don't know why you're here" and send me home with nothing. (I literally had a rheumatologist say to me, verbatim, "I don't know why you're here." buddy it's your job to read the chart and decide if I get seen or not, you tell me. at least he had a snazzy outfit.)
being chronically ill can be a terrible struggle no matter what, but a disease that is perceived as rare, accurate or not, adds a whole new layer of bullshit. (and of course there are much much rarer diseases out there, with even more hoops and dead ends and struggles and all-new layers of bullshit that even I don't have to deal with!)
anyway I'm having a shit time and using this awareness day as an excuse to productively bitch about it 👍
#it is okay to reblog this btw!#I know sometimes ppl get skittish when posts seem personal#(but I also know a wall of text is not Aesthetique™️ which like fair it's your blog yknow?)#kirby#swearing#long post#daily kirby#my art#digital#hal laboratory#nintendo#rare disease day#mcas#mast cell activation disorder#one time my wife took me to a gathering with her (at the time future-)doctor friends#and they were asking me about what I do and stuff and I was like 'oh I'm disabled'#so of course they're like 'oh with what?' basically#so I had to explain that we didn't know#and *why* we didn't know#and they seemed deeply disquieted that it could take even that long to find answers.#(this was coincidentally 6 years ago.)#it's a good lesson for them to learn early.
157 notes
·
View notes
Text
I should actually just belong in a monastery with the patience level I have for being in the middle of a medical episode and answering the phone for a pharmaceutical company that way I can continue getting treatments that makes my body stop attacking itself 🤏🏻 this much slower
#personal#my GOD#my entire body heated up from that one call#I’m in the dark lying down too#just let me rot on the forest floor— I am begging you#ehlers danlos syndrome#chronic illness#chronic pain#arthritis#mcas#mast cell activation syndrome#disabled#disability#autoimmune disorder
20 notes
·
View notes
Text
"Allergy" means you have IgE antibodies against that food. Antibodies will show on tests, but, if you dont eat that food, you can still be allergic without showing it on a test because you dont currently have the antibidies/enough antibodies. When you come in contact with that food again, your body will produce them. The cells know how, they just haven't "needed" to in a while.
"Sensitivities" may be mild allergies or they may be mast cell reactions. Some allergists incorrectly believe mast cell reactions always cause anaphylaxis, but they can be isolated to certain systems and areas of systems (like intestines but not stomach, esophagus, or mouth) and be mild (diarrhea, cramping, migraines, rashes, but no anaphylaxis). A mild allergy will have a positive antibody test and an elevated tryptase level. A mast cell reaction will have elevated tryptase without antibodies. Tryptase is released by mast cell degranulation, which is supposed to be triggered by antibodies or, extremely mildly, by muscle work. Some allergists also incorrectly believe that tryptase will never show as elevated if you haven't had anaphylaxis in the past 24-48 hours, and so there's no point in testing if you haven't had anaphylaxis.
"Intolerances" are caused by missing enzymes. Enzymes break down complex proteins into their simpler and smaller components that can then be absorbed by the intestines and transported to where they need to be used. Without the enzyme needed to break down the protein, the body will try to break it down other ways like increasing acid production (cue acid reflux), slowing motility if you have low levels of the enzyme rather than lack it completely which also allows bacteria to reproduce more to feed on the food (bloating, gas, constipation), and also increasing motility to get the offending food out of your system (cramping, inflammation, diarrhea). These usually also can be tested for by testing for the enzyme, and some have known genetic variations (yes enzyme or no enzyme) that can be tested for. The classic example is lactose intolerance - lacking the gene that allows your body to produce the enzyme lactase. Some enzymes can be synthesized in labs and made into enzyme replacement treatments.
So I would like to make a post about food allergies given the information I've been taught by my allergist regarding my food allergies.
The difference between food allergy, sensitivity, and intolerance.
Allergy. This is the classic anaphylaxis.
Sensitivity. This is caused by allergies, but the risk here isn't anaphylaxis. It's inflammation in gut that can cause fatigue, nausea, diarrhea, constipation, generalized ick feeling.
Intolerance. Your body is literally unable to process the food. It lacks the ability to, which means the food causes inflammation in the gut, causing similar symptoms as sensitivity.
Sensitivities will show up on an allergy test. Intolerance has to take a different test specific for that type of intolerance.
I mention this because I see a lot of fake claiming food allergies that's like "Yeah but I cross contaminated the food with eggs and that didn't kill her. She must be lying." Yeah food sensitivities can be pretty mild. Where if you give them an egg salad, they're gonna be having a bad day. But if you rub egg on their burger, they may not even notice.
Also like there's a lot of medical conditions that can affect a person's diet. They may have stomach issues that means they can't eat a lot of acidic foods, and if saying "Hey, I'm allergic to pineapple" gets you to not put pineapple juice in their drink because it'll cause a flare-up. I'm all for people doing whatever they need to make sure their health is taken seriously. Even if it's outright lying because food allergies is the only fucking thing people seem to take seriously in this world.
Anyways take people's "I can't eat this food" seriously. And don't fake claim them if they go "I can't eat this food but I'm not at risk if there's cross contamination"
-fae
7K notes
·
View notes
Text
What is Idiopathic Mast Cell Activation Syndrome?
Idiopathic Mast cell activation syndrome (MCAS) is one of several mast cell disorders. MCAS occurs when there are a normal number of mast cells in a person's body but they over-release mast cell mediators causing random allergic reactions in multiple systems of the body. MCAS is incredibly common being present in an estimated 17% of the population.
Symptoms
MCAS symptoms are incredibly varied and always occur in multiple systems of the body. Anaphylaxis is common.
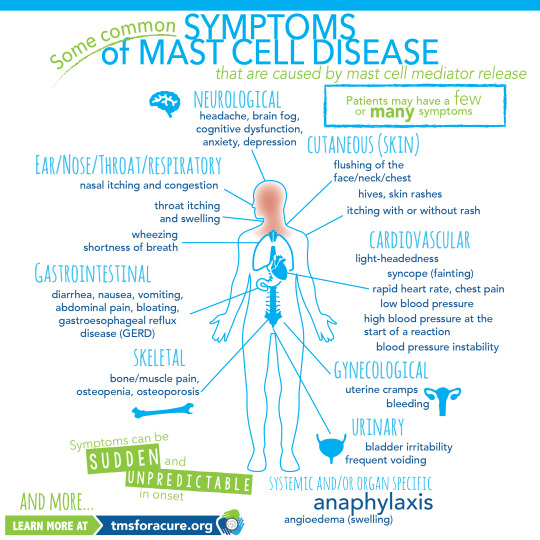
[ID: A graphic labeled "Some common symptoms of Mast Cell Disease" A graphic of a person standing in the center with multiple organs visible is shown. Around the person are lines pointing to specific areas of the body labeled with the body system and symptoms. Clockwise these read "Neurological headache, brain fog, cognitive dysfunction, anxiety, depression Cutaneous (Skin) flushing of the face/neck/chest, hives, skin rashes, itching with or without rash Cardiovascular light-heartedness, syncope (fainting), rapid heart rate, chest pain, low blood pressure, high blood pressure at the start of a reaction, blood pressure instability Gynecological uterine cramps, bleeding Urinary bladder irritability, frequent voiding Systemic and/or organ specific Anaphylaxis angioedema (swelling) Skeletal bone/muscle pain, osteopenia, osteoporosis Gastrointestinal diarrhea, nausea, vomiting, abdominal pain, bloating, gastroesophageal reflux disease (GERD) Ear/Nose/Throat/Respiratory nasal itching and congestion, throat itching and swelling, wheezing, shortness of breath and more" In the bottom left corner "Symptoms can be sudden and unpredictable in onset learn more at tmsforacure.org"]
MCAS symptoms are specifically not allergies. the reactions may look like allergies but the two are not the same and MCAS is not a condition meaning "many allergies" While MCAS can have some consistent triggers one of the defining features of the disease is that reactions are random and happen unpredictably.
Anaphylactic shock is not a requirement for diagnosis.
Diagnosis
MCAS is diagnosed by an immunologist. It is in part a diagnosis of exclusion and requires ruling out both allergies and systemic mastocytosis as well as other conditions such as certain types of tumors.
Diagnostic criteria for MCAS is debated. Some immunologists follow the symptom-based diagnosis approach in which case the diagnostic criteria are:
Recurring and severe anaphylactic-like episodes that involve more than one organ system
and
Positive response to mast cell stabilizing or mediator medications anaphylaxis-type symptoms
Others follow diagnostic criteria based on laboratory findings. In this case the diagnostic criteria are:
Episodic symptoms consistent with mast cell mediator release affecting two or more organ systems evidenced as follows:
Skin: urticaria, angioedema, flushing
Gastrointestinal: nausea, vomiting, diarrhea, abdominal cramping
Cardiovascular: hypotensive syncope or near syncope, tachycardia
Respiratory: wheezing
Naso-ocular: conjunctival injection, pruritus, nasal stuffiness
and
A decrease in the frequency or severity; or resolution of symptoms with anti-mediator therapy: H1 and H2 histamine receptor antagonists, anti-leukotriene medications (cysLT receptor blockers or 5-LO inhibitor), or mast cell stabilizers (cromolyn sodium)
and
Evidence of an elevation in a validated urinary or serum marker of mast cell activation: Documentation of elevation of the marker above the patient’s baseline during a symptomatic period on at least two occasions; or if baseline tryptase levels are persistently >15ng, documentation of elevation of the tryptase above baseline on one occasion. Total serum tryptase is recommended as the markers of choice; less specific (also from basophils) 24 hour urine histamine metabolites, or 11-beta-prostaglandin F2.
and
Primary (clonal) and secondary disorders of mast cell activation ruled out.
These are not all proposed diagnostic criteria as the subject is heavily debated. Generally, a laboratory-confirmed MCAS diagnosis is considered more legitimate.
Treatment
MCAS is a very treatable condition. Generally treatment follows a path from antihistamines -> mast cell mediators -> biologics.
Epipens are given to MCAS patients with a history of anaphylaxis.
Antihistamines are divided into 2 categories: H1 antagonists and H2 antagonists. These categories are determined based on the histamine receptor each one targets.
H1 antagonists mostly deal with systemic and cutaneous symptoms. H1 antagonists are also further divided into first and second generation antihistamines. first generation antihistamines include diphenhydramine (Benadryl) and Hydroxyzine. These tend to cause drowsiness. With second generation H1 antagonists cause fewer side effects and include drugs like loratadine (Claritin) and cetirizine (Zyrtec)
H2 antagonists primarily affect the gastrointestinal tract and include medications like famotidine (pepcid)
Typically when treating MCAS a person will be put on both a second generation H1 antagonist and an H2 antagonist.
When antihistamines do not treat symptoms well enough the next step is a mast cell mediator. The most common mast cell mediator is cromolyn sodium which is available by prescription only. (this is technically available OTC but it is at 1/50th the dose used for MCAS) Mast cell mediators work by preventing the degranulation of mast cells in the first place.
When both antihistamines and mast cell mediators are insufficient someone with MCAS might be prescribed a biologic such as Xolair to treat their remaining symptoms.
Sources:
American Academy of Allergy, Asthma, and Immunology
Mast Cell Hope
Mast Cell Activation Syndrome: Proposed Diagnostic Criteria
#mast cell activation syndrome#mcas#mast cell disease#mast cell activation disorder#mcad#chronic illness#chronically ill#physical disability#physically disabled
104 notes
·
View notes
Text
crying alone in my room as i process that realistically im going to need a cane at the very least, for my entire life. probably more than a cane. im gonna be on meds for who knows how long probably my whole life for a couple of them. im gonna be in pain forever. i almost wish i didnt get diagnosed because then i could live in denial
#chronic pain#chronic illness#ehlers danlos syndrome#joint pain#mobility aid#pots syndrome#hypermobile ehlers danlos#migraine#cane user#headache#mast cell activation syndrome#mcas#mast cell activation disorder
23 notes
·
View notes
Text
Does this mean we can finally get rid of soy in literally everything
#mcas#mast cell activation disorder#histamine intolerance#chronic illness#chronically ill#why is there soy in celestial seasons tea#don't worry I've found way better tea since then
107 notes
·
View notes
Text
Post 4/7
Meme dump for my fellow spoonies! Sending 🥄🥄🥄 and 🩵🩵🩵










#disability#disabled#ehlers danlos syndrome#fibromyalgia#hypermobile eds#pots syndrome#potsie#rheumatoid arthritis#spoonie#chronically ill#chronic illness#funny memes#funny#meme#mast cell activation syndrome#mast cell activation disorder
18 notes
·
View notes
Text
hey turns out if i have a manic/depressive episode i get a full body allergic reaction for free
NEAT.
#chronically ill#chronic illness#mast cell activation syndrome#mast cell disease#bipolar disorder#actually bipolar#bipolardepression
7 notes
·
View notes
Text
Lately, i have been coming to terms with the fact that i have might have chronic illness and that i might actually be disabled and i am not just making up the amount of pain i am constantly in
#it's a little scary and overwhelming#i think i might have#pots#and#mcas#if anyone who is diagnosed is ok with reaching out i would really appreciate that#i am also neurodivergent#and i am aware that the comorbidity rates are high#but i have always thought maybe i am making up the pain I have#putting tags so it reaches people ig??#pots syndrome#potsie#mast cell activation syndrome#mast cell activation disorder#autism#actually autistic#actually audhd#adhd#audhd
7 notes
·
View notes
Text
Introduction 🌟🎭

Hi! We're The Asterism Theatre, we're a polyfragmented DID system, but you can just call us Asterism. We use they/them pronouns collectively, and our system as a whole is systemfluid, abrosexual (+mostly demiromantic), intersex, and polyamorous. Bodily in our early 20s, very queer, autistic (+ADHD), trans, and disabled.
We're a introject-heavy, polyfrag DID system, with a very high alter count (at least hundreds), and an absolute ton of amnesia, and will probably post about that! While we have subsystems and layers that have less introjects, our introjects are usually who front most often; We also have a lot of nonhumans in system (especially demons/angels and such due to ramcoa).
Some of us are pagan too, particularly eclectic pagan witches, mainly interested in deity work and cartomancy.
We also do a lot of digital art (2D illustration), and are also starting to learn 3D! We also love music, both listening to it, and writing/singing our own.
Special interests include (but are not limited to) DID/OSDD, fandoms (many of which are also sources for our introjects), art and animation, theatre and acting (aspiring actor!), mythology and stories (of any kind really, written, comics, fanfic, visual, tv/movies and theatre), and animals (peticularly wolves and dogs).
Ask us stuff!
Please feel free to send asks about DID/system related stuff ,or about our system! For the most part as long as everything's respectful we love answering questions and just talking about our system and DID in general. If you're also a system please interact! We'd love to interact more with systems in general as well as with shared sources too.
Just FYI with medical chaos and life chaos our posting as well as checking our tumblr in general will likely be pretty irregular.

Fandoms (including sources):
(sidenote: some of our fandoms and sources we do not support the creators, to be clear. We're also not caught up on most of these but don't usually mind spoilers!)
• Lucifer
• Hazbin Hotel & Helluva Boss
• Marvel
• Merlin
• FNAF
• The Amazing Digital Circus
• Doctor Who
• Good Omens
• Star Wars
• Generation Loss
• Our Flag Means Death
• Wednesday
• CW Arrowverse shows
• Edge of Sleep (show)
• DSMP related introjects (not really in the fandom, and most intojects are cc! not c!)
• probably more that we can't remember and will add to this list later

DNI List
Also, we're medically/formally diagnosed, but are pro self diagnosis; We'd never have gotten our dx had we not been self dx-ed and learnt as much as we did first!
• Minors DNI
Elsewise essentially please just don't be shitty:
• Transphobes, homophobes, queerphobia of any variety, ableist, sexist, racist, pedos/MAPs, fakeclaimers, anything like those really.
• We're not anti-endo (used to be but since are trying to be more respectful, we're prob more like neutral) but don't really know much about it as a traumagenic system, and post about our experiences (of which being traumagenic); Please no syscourse debates from either side though! Wanna keep our blog chill. Endos feel free to interact.

Blogs/etc of ours:
@theasterismtheatre
This one! Our main blog of whatever we wanna post, system stuff, fandoms, and memes. Maybe we'll post our art here too at some point.
@shitoursystemsays
Side blog we'll start posting on at some point, of funny shit our system says. We've got a list on google docs but have yet to post any if it, haha.
We'll probably also make a fanfic specific blog sometime soon since we're starting to write fic now! For now here's our AO3:
https://archiveofourown.org/users/TheAsterismTheatre

We'll probably write our names / who's fronting when we post, though we almost always have a shell in front as well. We have some subsystems of alters who are hard if not impossible to differentiate from each other, so if people seem confusingly different and yet have the same name, that's probably why. If we're blurry and/or a shell posting, we'll either not put a name, or sign off with a seashell emoji. Alter (or subsystem) intros will be tagged as #alter intro and/or #subsystem intro.
Anyhow yeah, we're The Asterism Theatre. Nice to meet ya!

Dividers credit:
@/saradika-graphics
@/thecutestgrotto
#lgbtqia#did system#did memes#did#dissociative identity disorder#lgbtq#exvangelical#introduction#pinned intro#blog intro#traumagenic system#otherkin#ramcoa survivor#systemfluid#abrosexual#genderfluid#intersex#disabled#ehlers danlos#postural orthostatic tachycardia syndrome#mast cell activation syndrome#borderline personality disorder#autism#digital artist#dissociative system#did osdd#hc did#polyamourous#trans#pagan
5 notes
·
View notes
Text
Hey y'all! I just got diagnosed with MCAS and have been told to follow a low histamine diet.
Do any of you have any tips? Perhaps food brands you can eat?
9 notes
·
View notes
Text
hi! my name is theo and i am a disabled, neurodivergent artist. please consider checking out my kickstarter for an enamel pin of my most popular sticker design!
because of the current amount of pledges and the amount of time until the deadline, i fully expect these to be produced and shipped *before* december.
if you'd prefer just the sticker version, it can be found on my website here: https://www.obsidianoddities.shop
kickstarter
#disabled#dynamic disability#disability struggles#disability pride month#disabled and proud#disabled owned business#disabled af#disability#disabled adult#pots syndrome#postural orthostatic tachycardia syndrome#dysautonomia#hypermobile eds#heds#hypermobility spectrum disorder#mcas#mast cell activation syndrome#the trifecta#long covid#chronic illness#chronic pain#interstitial cystitis#audhd#actually audhd#audhd artist#neurodiversity#neurodivergence#nonbinary#alternative#small business owner
30 notes
·
View notes
Text
having the hEDS trifecta + lupus is very frustrating because it's just like "okay where is this symptom coming from?" and no doctor can agree so it doesn't get treated
I have professionally diagnosed MCAS
I'd like to share the symptoms of MCAS can cause:
Constitutional : Fatigue, subjective hyperthermia and/or hypothermia, sweats, change in appetite, weight gain/loss, chemical/physical sensitivities, poor healing
Dermatologic : Urticaria, itch, flushing, hemangiomas with itch/pain, various rashes, telangiectasias, striae, skin tags, folliculitis, ulcers, eczema, angioedema, alopecia, onychodystrophy
Ophthalmologic : Irritated, “dry” eyes, difficulty focusing, blepharospasm
Otologic : Tinnitus, hearing loss, coryza, rhinitis, nasal congestion, epistaxis
Oropharyngeal: Pain, burning, leukoplakia, ulcers, angioedema, dysgeusia, dental and/or periodontal inflammation/decay
Lymphatic: Lymphadenopathy, rare splenomegaly
Pulmonary: Dry cough, dyspnea (difficulty taking a deep breath), wheezing, obstructive sleep apnea
Cardiovascular: Presyncope, hypertension, blood pressure lability, palpitations, edema, chest pain, allergic angina (Kounis syndrome)
Gastrointestinal: Dyspepsia, gastroesophageal reflux, abdominal pain, nausea, vomiting, diarrhea and/or constipation, gastroparesis, angioedema, dysphagia (usually proximal), bloating (post-prandial or spontaneous), malabsorption
Genitourinary: Menorrhagia, pelvic pain, endometriosis, vulvodynia, vaginitis, dysmenorrhea, miscarriages, infertility, dysuria
Musculoskeletal: Myalgias, migratory bone/joint pain, osteopenia/osteoporosis
Neurologic : Headache, migraine, sensory neuropathies, dysautonomia, episodic weakness, seizure disorders, non-epileptic seizures, cognitive dysfunction, insomnia, hypersomnolence, restless leg syndrome
Psychiatric: Depression, anger/irritability, mood lability, anxiety, panic, obsession–compulsion, attention deficit/hyperactivity
Hematologic: Easy bruising, polycythemia, anemia
Immunologic: Hypersensitivity reactions, increased risk for malignancy and autoimmunity, impaired healing, increased susceptibility to infection
source
"well that's just everything" ya. that's why I can't figure out where my symptoms are coming from. lupus is also like this. autonomic neuropathy is also like this. my doctors run in circles pointing at the other doctors to solve the problem but none of them want to.
#physical disability#physically disabled#chronic illness#chronically ill#mast cell activation syndrome#mast cell disease#mast cell activation disorder#hypermobile ehlers danlos syndrome#hEDS#systemic lupus erythematosus#dysautonomia#pots syndrome#postural orthostatic tachycardia syndrome#autonomic neuropathy
33 notes
·
View notes
Text
first time taking my forearm crutch out in public. i only took one, idk what but 2 felt like too much, even though i definitely needed both. it went well! no weird looks, nobody even acknowledged it which i loved, i didnt want any attention on it, so to see it get ignored was great. i think using the aids puts my pain into perspective for my family though because while i was waiting in line, my beother pulled me out and had me sit down and he took my place. i was really thankful because it was closer to the end of the trip so the pain was really setting in
on that note, my mcad meds arent ready. they wont be till next monday at the earliest which sucks i was so hoping to try them right away and see how they help! the dr said they could help my constant nausea and make it easier to eat, because my body wont be as upset about things? idk i cant actually remember exactly what he said.
#chronic pain#chronic illness#ehlers danlos syndrome#joint pain#pots syndrome#mobility aid#hypermobile ehlers danlos#cane user#mast cell activation disorder#mast cell activation syndrome#mcad
14 notes
·
View notes