#intrauterine infection
Explore tagged Tumblr posts
Text
#best female gynaecologist in mumbai#list of gynecologist in mumbai#gynecologist in mumbai#best gyno in mumbai#intrauterine infection#intrauterine infection treatment#Chorioamnionitis#female gynaecologist and laparoscopic surgeon in mumbai#best gynecologist in mumbai#famous gynecologist in mumbai#mumbai best gynaecologist#top gynecologist in mumbai
0 notes
Text

Explore the meaning of high-risk pregnancy. Understand the factors and care needed for a healthy pregnancy journey. Learn about High Risk Pregnancy.
Do Read: https://www.drshubhragoyal.com/welcome/blogs/introduction-to-high-risk-pregnancy--what-does-it-mean
#High Risk Pregnancy#Pregnancy with heart disease#Rh incompatibility#Oligohydramnios#Uterine fibroids pregnancy#Pregestational diabetes#Cervical insufficiency#Pregnancy after 35#Recurrent miscarriages#Intrauterine growth retardation#Placental abruption#VBAC risks (Vaginal Birth After Cesarean)#Perinatal infections#Pregnancy-induced hypertension#Chronic kidney disease pregnancy#Antiphospholipid syndrome pregnancy#Congenital anomalies risk
1 note
·
View note
Text
A Masterpost About Long-Acting Reversible Contraceptives (LARCs)
During the upcoming presidency, it is likely that people in the US will lose many options that keep them from getting pregnant (contraceptives). The right-wing Project 2025 is against birth control pills, abortion, emergency contraception, and the government-provided health insurance ("Obamacare," Medicaid, and Medicare) that helps people afford these.
If you or your partner are concerned about the possibility of losing access to those options soon, you can ask your doctor or Planned Parenthood about getting a Long-Acting Reversible Contraceptive (LARC). The two kinds of LARCs are IUDs and the implant. If you get a LARC right now, it can protect you for years, without you having to do anything to maintain it. A LARC isn't permanent, so you can get rid of it if you later decide that you're ready to have a baby.
Hormonal Intrauterine Device: 3, 5, or 8 years of protection, depending on brand
An IUD is a T-shaped object that a nurse or doctor puts into your uterus. It's tiny, just a little more than an inch. The procedure for getting an IUD isn't surgery, it lasts just a few minutes, and it goes much better if you ask for an anti-anxiety medicine and the right type of painkiller.
Hormonal IUDs work because they slowly release progestin. That's the main hormone in birth control pills. Like pills, they can make your periods get lighter or stop, which is helpful for people who need to get rid of cramps and PMS.
Of the brands of them in the US, the FDA currently approves of using Kyleena for up to five years, Liletta for eight, Mirena for eight, and Skyla for three. Kyleena and Skyla are smallest and therefore easiest to insert.
I have more info in my tags about IUDs.
Copper IUDs: 12 years of protection
The other type of IUD is a copper IUD. Instead of changing your hormones, it works because copper makes the place unfriendly to sperm. Another difference is that this kind can make your periods heavier. Its brand name is Paragard. The FDA approves of using it for ten years, but studies show it's still good at twelve or longer. More info in my tags.
The birth control implant: 5 years of protection
It's a rod the size of a matchstick. A nurse or doctor uses an applicator to put it under your skin in your arm. There, it will slowly release progestin to protect you from getting pregnant. It can make your periods get lighter or stop. The FDA approves of using it for three years, but a study shows it's still 100% effective five years later, and so does another study. Its brand name is Nexplanon, which has improvements over the older Implanon, such as being visible on X-ray. More info in my tags.
Some honorable mentions
There are some other contraceptives that last a long time but aren't considered LARCs. The diaphragm and the cervical cap are two kinds of plastic cap that you put on your cervix each time before sex, and you can keep using the same one for two years. The birth control ring, Annovera, lasts one year. Each injection of the birth control shot, Depo-Provera, lasts three months.
Only barrier methods such as condoms, internal condoms, and dental dams can protect against sexually transmitted infections. The right wing wants to stop people from getting condoms, too. That's another problem, but LARCs can help us get through the next four years without unplanned pregnancies.
#contraceptive#contraception#IUD#birth control#Project 2025#intrauterine device#long-acting reversible contraceptive#LARC#birth control implant#Mirena#Nexplanon#Paraguard#sex education#hormonal IUD#copper IUD#US politics#relevant for people who can get pregnant#please reblog and circulate this widely; you're also welcome to reblog from my older posts on these topics#if you don't want to see this content from my blog: i always tag thoroughly so you can blacklist the tags 'sex education' etc#rated PG-13#no-ai#screen reader friendly#menstruation#menstrual suppression#AFAB#relevant for transgender men and trans masculine nonbinary people and others on the female to male spectrum#relevant for cisgender women and transgender men and others who were assigned female at birth#relevant for people in relationships where someone could get pregnant#relevant for people who menstruate#original post
41 notes
·
View notes
Text
Summary Chart of U.S. Medical Eligibility Criteria for Contraceptive Use (U.S. MEC)
This information is no longer on the CDC website and was generally pretty poorly distributed prior to that, so I am posting it here. These are BROAD guidelines about the safety of different contraceptive options in the context of specific health conditions. They are useful on their own and also as a resource to bring to a care provider who is unsure about contraceptive safety in the context of your health condition.





Abbreviations: ARV = antiretroviral; C = continuation of contraceptive method; CHC = combined hormonal contraceptive (pill, patch, and ring); COC = combined oral contraceptive; Cu-IUD = copper intrauterine device; DMPA = depot medroxyprogesterone acetate; I = initiation of contraceptive method; LNG-IUD = levonorgestrel intrauterine device; NA = not applicable; POP = progestin-only pill; P/R = patch/ring; SSRI = selective serotonin reuptake inhibitor; STI = sexually transmitted infection; VTE = venous thromboembolism. ‡ Condition associated with increased risk as a result of pregnancy.
*PDF version here- https://smallpdf.com/file#s=79d002b3-77c2-4046-89fe-c0487fa56b37
8 notes
·
View notes
Text
Microcephaly is an underdevelopment of the skull and brain, accompanied by mental retardation and neurological abnormalities.
I will not consider the causes of microcephaly yet, because this is a very complex topic of chromosomal mutations, intrauterine infections and pathologies, birth injuries, etc.


I rely solely on the unofficial concept of Pyro's face, so looking at the concept of signs of microcephaly, what am I trying to pull on the arsonist:
1) The predominance of the facial skull over the cerebral one.
2) Narrow and sloping forehead, prominent brow ridges, large ears.
I also love fanon, that Pyro has big and sparse teeth, the wrong taste.
3) Disproportionate physique – a change in the parts of the figure (feet, hands) and their unexpected growth.
Further, what I can add from myself are possible signs:
a) A gross delay in speech development.
b) Indistinctness of articulation (articulate pronunciation) – is further complicated by tightening the face with a gas mask, the tongue and lips may not move well.
c) Limited vocabulary – exclamations and repetition of the same expressions heard earlier.
d) Violation of the understanding of the addressed speech – ignoring, misunderstanding that they are addressing him, "withdrawal into oneself".
I consider Pyro to be an erectile group of patients: hyperactivity, fussiness, mobility, unstable attention.
The degree of intellectual disability varies from imbecility to idiocy.
19 notes
·
View notes
Text

‘I was only a child’: Greenlandic women tell of trauma of forced contraception (Miranda Bryant, The Guardian, March 29 2024)
"Hedvig Frederiksen had been at her new school in Paamiut, Greenland, for only a couple of days when she was summoned from her dorm to the local hospital by a Danish caretaker.
She was 14 and had no idea what was going on.
“But back then [1974], when a Danish person said something, their word was law, you had to listen to them,” said Frederiksen, speaking from her home in Nuuk, Greenland’s capital.
About a dozen girls went to the hospital, some as young as 13.
One by one they went into the doctor’s room and one by one they came out crying. Frederiksen was terrified but felt compelled to stay put.
Her daughter Aviaja Fontain told the story as Frederiksen quietly wept.
“When she came in [to the doctor’s room], her memory just disappears and she thinks it’s because of the trauma, what happened in there.
Her friend from the same dorm said the doctor didn’t have a helper; he was alone putting spirals [contraceptive coils] inside girls.”
Frederiksen, now 63, is one of 143 Greenlandic women who this month announced they were suing the Danish state, demanding a collective payment of close to 43m Danish kroner (£4.9m) for what they describe as a violation of their human rights.
They accuse Danish doctors of fitting girls as young as 12 with intrauterine devices (IUDs) in an attempt to reduce the population of the former colony, now an autonomous Danish territory.
It is believed that 4,500 women and girls were affected between 1966 and 1970, with many more procedures carried out without consent in subsequent decades, but it has taken a long time for the reports to surface – and to be taken seriously. (…)
After a visit last year, the UN special rapporteur on the rights of Indigenous peoples, Francisco Calí Tzay, highlighted the scandal as a particularly disturbing element of Denmark’s colonial legacy, condemning the structural and systemic racial discrimination inflicted on Greenland’s Inuit people and its ongoing repercussions.
“Despite significant progress, the Inuit people still face barriers to fully enjoying their human rights in both Denmark and Greenland,” Calí Tzay said, adding that he was “particularly appalled�� by the testimonies of women forcibly fitted with IUDs.
Greenland ceased being a Danish colony in 1953, although it did not have its own government and parliament until 1979.
Healthcare and living conditions improved, life expectancy increased and the Greenlandic population grew.
It was then that the Danish authorities are believed to have staged their drastic intervention.
The programme of involuntary birth control would go on to halve the birthrate within a few years. (…)
She remembers the cold tools he used to insert the IUD, the shock she felt and “tremendous pain”.
She said he told her that the reason it was being fitted was “so I shouldn’t get pregnant”. “I was only a child,” she said.
“I was only 14. And when I was back at the dorm I cried in the evening because I couldn’t talk with my parents and I hadn’t given any consent, nor did my parents.”
Contraceptive coils are now a safe and highly effective form of birth control.
But Larsen, like many of the women who have come forward since the 60s and 70s, went on to experience serious reproductive difficulties – a consequence, they say, of being forcibly fitted, with no consent or information, with unsophisticated devices that were often too big for their young bodies, bringing with them additional risk of infection.
For Larsen, that experience felt like an assault. She was in so much pain that “afterwards I felt like I had shattered glass in my abdomen”.
Later, after she got married and tried to get pregnant, she found that she could not.
Years later when she was examined at a hospital, they found her fallopian tubes were closed because of the coil, which had caused severe bleeding and left her sterile. (…)
After being fitted with the coil, Frederiksen remembers, she was in a huge amount of pain.
All the girls walked back to their dorms crying and feeling ashamed, she said, and they started getting extremely painful periods.
The coil remained inside her for eight or nine years because the doctor did not tell her when it should be removed.
After having it taken out she became pregnant with Aviaja, but the next time she became pregnant her fallopian tube ruptured and she lost a lot of blood.
Her lawyer has said this is a common side-effect in women who were forcibly fitted with coils. Many years later, Frederiksen had two more children.
While she is happy about the legal case and the support they have received, she is filled with anger and sadness when looking back on what she endured as such a young child.
“If that had not happened to me, I wouldn’t be as shy and ashamed for many years,” she said. “And if that had not happened, my life could have been very different.”"
24 notes
·
View notes
Note
Hello, I remember finding something about a year ago listed online as “pre-birth programming.” I assumed it had something to do with the torture of fetuses while still in the womb since this is an established tactic by advanced groups to induce dissociation, but what it actually described had something to do with regressing someone back to a fetal state of consciousness (possibly including making sure the subject remains in the fetal position?)… I’m a little fuzzy on the details. Recently, someone close to me confided in me about being instructed re: this exact tactic while still in the network as a child, and I went to find this information again to corroborate their experience, but I can’t find it anywhere and it’s driving me crazy. I am positive I’ve seen this somewhere and I’d really like to support this system—we’re very close and they are incredibly important to me.
If you have any information about this, I would really, really appreciate if you could share it. Thank you for all the work you do.
Babies in the womb feel, taste, learn, and have some level of consciousness. Attachment also begins in the womb. The earlier the trauma occurs in the womb, the more disastrous the effects. Mothers who have suffered childhood trauma can pass this memory down to an unborn baby. This is one reason TBMC seeks to be generational.
Christiane Northrup (2005) If a pregnant mother is going through high levels of fear or anxiety she creates a “metabolic cascade.” Hormones known as cytokines are produced and the mother’s immune system is affected, including her child’s. Chronic anxiety in the mother can set the stage for a whole array of trauma based results.
Early trauma is encoded in the implicit memory of the fetus. An unborn child is a feeling, remembering, and aware being, and the 9 months between conception and birth are the crucial first phase of shaping personality and emotional development.
Therefore, the presence of trauma during the critical 9 months of pregnancy can have profound impacts on the development of the fetus.
Traumas experienced in utero for example lack of sufficient oxygen is a horrifying stressor. If it continues, death is the result. Further, it leaves the fetus with insufficient resources to combat future stress, and a lack of feelings of safety. The danger remains underlying so that any later trauma can trigger it. This can lead to anxiety reactions to seemingly non-stressful situations that do not match the current situation.
Womb-life traumas can also deplete serotonin supplies as a result the child may grow up feeling continuously uncomfortable, a chronic depression and anxiety because the readjusted set points fixed during gestation were low.
Stress is an example of how a fetus responds to stimuli in the womb and adapts physiologically. "When the mother is stressed, several biological changes occur, including elevation of stress hormones and increased likelihood of intrauterine infection," Dr. Wadhwa says. "The fetus builds itself permanently to deal with this kind of high-stress environment, and once it's born may be at greater risk for a whole bunch of stress-related pathologies." Source
Maternal (Klaus, Kennell & Klaus, 1996) bonding during pregnancy is associated with positive infant attachment, whereas unresolved, dissociated trauma, chronic affect dysregulation, and obstetric complications during pregnancy seem to alter the bonding experience often resulting in broken bonds. The Calming Womb Family Therapy Model (CWFTM) is a comprehensive, collaborative, team-based, early intervention approach which is intended for treating mothers and their babies from conception through the first year after birth.
Source
There is growing evidence that even milder forms of maternal stress or anxiety during pregnancy affect the fetus causing possible long-term consequences for infant and child development. The mechanisms through which prenatal maternal stress may affect the unborn are not yet entirely clarified. Due to limited self-regulatory skills after birth, infants depend on sensitive behavior of their parents to regulate affective states and physiological arousal.
Source
You're most welcome. Take care, Oz
11 notes
·
View notes
Text
Is the removal of a retained IUD a complex procedure?
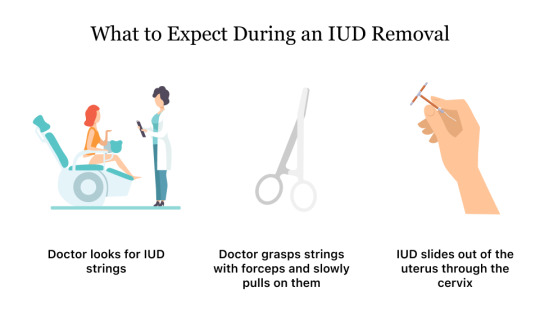
The removal of a retained Intrauterine Device (IUD) is typically a straightforward and routine procedure. However, the complexity can vary based on several factors:
1- Location of the IUD:
If the IUD is easily visible and located within the cervix, the removal is usually simple. However, if it has migrated or embedded in the uterine wall, extraction may be more challenging.
2- Time Since Insertion:
The longer the IUD has been in place, the more likely it is to become embedded. This can make removal more complex, as the device may become surrounded by tissue over time.
3- Experience of the Healthcare Provider:
A skilled and experienced healthcare provider, such as a gynecologist, is better equipped to handle challenging cases. They can employ various techniques to safely retrieve the IUD.
4- Patient Comfort:
The procedure is generally well-tolerated, and healthcare providers may use local anesthesia or recommend pain relief measures to enhance patient comfort during removal.
In most cases, the removal of a retained IUD is a quick office-based procedure. The healthcare provider may use forceps or special instruments to grasp the IUD strings and gently guide it out. If the strings are not visible, imaging studies such as ultrasound may be used to locate the device.
It's crucial for individuals experiencing difficulty with IUD removal to seek prompt medical attention. Delayed removal can lead to complications, such as infection or perforation. Healthcare providers are experienced in managing such situations and will take necessary steps to ensure a safe and effective removal process.
Experience comprehensive women's health care with Dr. Neha Lalla, your trusted Uterine Polyp removal in Dubai . Book your appointment today for expert guidance and personalized care.
#gynaecologist in dubai#dr. neha lalla#best indian gynaecologist in dubai#gynecologist#Uterine Polyp removal in Dubai#IUD removal#gynecological care
2 notes
·
View notes
Text
Sherika Mayo, 23 (USA 2008)
In 2008, 23-year-old Sherika Mayo had an abortion when she was 25 weeks pregnant.
Sherika had sickle cell disease and a low level of hemoglobin. Healthy hemoglobin levels would have been between 12 and 16 (for a woman her age), but Sherika’s hemoglobin measured in at only 7.3 gms. Since the abortion was purely elective, the safest decision would have been to not proceed with the abortion and to instead give Sherika a blood transfusion until her hemoglobin was at least 9 gms. She needed real medical care, not abortion.
Instead of sending Sherika to get medical help, Tyrone Maloy proceeded with the abortion, killing both Sherika and her baby. Records show that he told Sherika her baby was younger than the actual age.
Sherika’s heart stopped. She was transferred to the hospital (Atlanta Medical Center) while the paramedics continued CPR. Upon arriving at the hospital, Sherika had a distended abdomen and vaginal bleeding. ER staff called for a gynecologist. Emergency surgery was performed to remove Sherika’s damaged uterus and repair an injured bowel. (The abortionist insisted that the bowel was injured during this surgery, not during the abortion. There was no evidence whatsoever that this was true.) It was also noticed that Malloy lacerated Sherika’s cervix.
Because of her abortion injuries, Sherika developed a disorder called DIC (disseminated intravascular coagulopathy, a life-threatening clotting disorder sometimes caused by trauma or infection), a complication frequently seen in abortion deaths. She was treated with blood products but died in the ICU on March 21, 2008.
After Sherika was killed, the State Medical Board of Georgia reviewed the case and determined that abortionist Tyrone Malloy “failed to conform to minimal standards of acceptable and prevailing medical practice” in the following ways:
Sherika’s blood count was low; since this was an elective procedure, she should have been provided with a transfusion to bring her blood hemoglobin level up to at least 9 gm.
Blood clotting tests should have been performed prior to the abortion.
Malloy should have more accurately determined the gestational age because the risk of amniotic fluid embolism (which can cause the clotting disorder that ultimately killed Sherika) increases with increased gestational age and additional “intrauterine manipulation.”
Malloy, who had already been responsible for the death of a newborn in 1999, was ordered to pay a $10,000 fine and to take continuing education classes. After this, he was allowed to continue with his career as an abortionist, leading to more deaths. He was later convicted and jailed for felony offenses, and yet was still allowed to sell abortions after he got out of jail. He is still allowed to continue his abortion business to this day despite a long criminal record and list of malpractice lawsuits.
(Georgia Composite Medical Board public reprimand)
(other Medical Board documents)

#tw abortion#pro life#pro choice#abortion#tw murder#abortion debate#unsafe yet legal#tw ab*rtion#tw death#black lives matter#death from legal abortion#tw blo0d#tw injury#abortion kills women#unsafe but legal
9 notes
·
View notes
Text
IUDs in Singapore – All You Need to Know About Costs and Types of IUDs
It might be difficult to determine an effective birth control form, but have you thought about an IUD? Due to their effectiveness, comfort, and affordability, these little devices are widely used in Singapore. If you're wondering how much an IUD will cost, look no further. We'll provide you with a thorough breakdown of the costs related to this long-term contraceptive form in Singapore in this article. We'll even discuss the many IUD types and potential costs to you. Find out all you need to know about obtaining an IUD in Singapore and don't let uncertainty stop you.
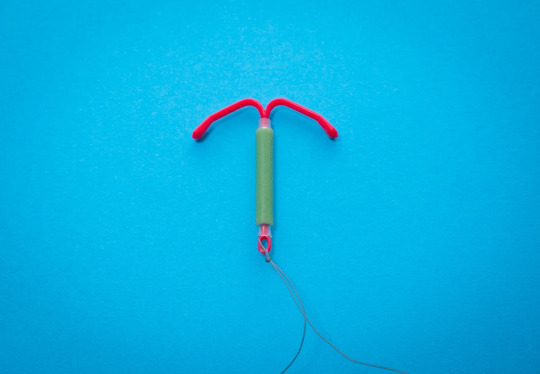
What are IUDs?
Do you know what an IUD is? The term "intrauterine device," as the abbreviation indicates, refers to contraception that is placed inside the uterus. By blocking sperm from reaching an egg, it not only prevents pregnancy but also offers reliable birth control. IUDs come in two primary types in Singapore: copper and hormonal.
1. The copper IUD releases copper ions to stop sperm from fertilizing an egg, making it a very effective form of long-term contraception. It serves up to 10 years by producing a hostile environment that includes white blood cells and other elements. It does not interfere with the body's regular hormonal cycle, unlike hormonal IUDs, and fertility returns to normal within 24 hours following removal. So the copper IUD is absolutely something to think about if you want a non-hormonal that you can put in your drawer and forget about for years at a time.
2. The unobtrusive Hormonal IUD may serve as your own personal pregnancy prevention wingman. The Hormonal IUD, which may last up to five years, is implanted directly into your uterus rather than fiddling with pills or injections. The Hormonal IUD discreetly affects cervical mucus thickness, uterine lining thinning, and even ovulation inhibition. All of these actions combine to effectively stop sperm from fertilizing an egg and stop any probably fertilized eggs from implantation in the uterus. You may rest easy knowing that you are 99% prevented from becoming pregnant. However, keep in mind that the hormonal IUD does not provide protection against STDs, so be careful to continue using a condom to be protected.
What Can I Expect With IUDs in Singapore?
Are you interested in receiving an IUD in Singapore? You may relax knowing that everything will go well thanks to your healthcare provider's skillful guidance. Your healthcare provider will check that the IUD can be securely implanted into your uterus during your examination. Rest comfortably knowing that any pain should subside in a few hours if there is any mild cramping. In order to keep an eye on your IUD and any potential adverse reactions, your healthcare provider will also offer you the appropriate after-care instructions.
Is there any risk?
It's important to keep in mind that there are certain risks involved while thinking about getting an IUD.
1. If the device is not positioned correctly or if changes to your uterus occur that might move the device, expulsion is a potential problem.
2. Infection may happen if germs enter the uterus during or just after implantation, however, it's unusual.
3. If the device is contaminated, there is a chance to get a pelvic inflammatory disease. It's crucial to discuss these concerns and if an IUD is suitable for you with your healthcare professional.
4. Migration, which is a chance that the IUD may move from its initial location and become less effective in preventing conception.
IUD advantages
Looking for birth control that is reliable and easy to use? Consider the IUD. This durable contraceptive is inexpensive, simple to use, and effective in preventing conception. Additionally, an IUD won't adversely affect your fertility if you decide to stop taking it, unlike some other forms of birth control. IUDs provide worry-free contraception, so say goodbye to daily pills and welcome to an IUD.
IUD disadvantages
Despite the fact that an IUD may be an effective form of birth control, there are a few considerations to make. IUDs do not provide protection against STIs, thus if you have several partners or an STI, you need also to wear a condom. This is an essential fact to keep in mind. Depending on the type of device they use, some women may encounter adverse effects including cramping or irregular periods. Insertion may be difficult or painful for certain people, and there is a chance of consequences including perforation. Before selecting anything, it's critical to thoroughly weigh the disadvantages that can be involved.
What to Know About Singapore IUD Prices
If you're thinking about having an IUD in Singapore, you may be concerned about the price cost. There are other expenses to think about, including the price of the device, the implantation, any further consultations, and eventual removal. Although the actual cost depends on what type you prefer, it's important to note that hormonal IUDs are often more costly than copper.
The price range for hormonal IUDs like Mirena, Skyla, and Jaydess is $400 to $600.
Costs for copper IUDs including Copper-T, TCu380A, and ParaGard typically range from $200 to $300.
Your readiness for this important investment in your health might be aided by being aware of the pricing range.
Summary
An IUD can be the ideal form of contraception for you if you want something that's effective well and lasts. With the right care and maintenance, this long-term birth control may provide several years of pregnancy prevention. It's crucial to weigh the prospective expenses, such as follow-up visits or removal, before deciding to use an IUD. To decide whether this is a suitable form of contraception for you, it may be beneficial to ask your healthcare provider about all costs involved.
Before considering any means of birth control, it's crucial to discuss any health issues you may have with your healthcare provider. by placing an excessive emphasis on your overall health and obtaining the ideal type of contraception for your requirements.
2 notes
·
View notes
Text
Introduction to High-Risk Pregnancy- What Does It Mean

Pregnancy can indeed be a joyous time, but it can also be overwhelming and stressful. Expectant mothers need to take care of themselves and their unborn babies. However, for some women, their pregnancy is considered high-risk.What is a high-risk pregnancy? It means the mother has an increased chance of experiencing complications during pregnancy, labor, delivery, and even after birth. Understanding this can help expectant mothers plan accordingly.Factors that contribute to high-risk pregnancy can vary from woman to woman. Some common factors include age, weight, medical history, and lifestyle choices. Awareness of these factors can help women make informed choices during this crucial time.So, let's dive deeper and understand what medical conditions can cause high-risk pregnancies and how to reduce the risks.So, let's get started!High Risk Pregnancy: Quick Overview!Pregnancy is a unique and beautiful journey, but it has challenges. As the name suggests, a high-risk pregnancy involves a higher likelihood of complications than a typical pregnancy. These complications can arise due to various factors, such as pre-existing medical conditions, age, or a history of pregnancy-related issues. Let's explore some common aspects that can categorize a pregnancy as high-risk.Factors that Contribute to High-Risk Pregnancy!Age is one of the factors that contribute to high-risk pregnancy. Women older than 35 are at increased risk. Other factors include Pre-existing medical conditions, Multiple pregnancies, substance abuse, and more.According to the insights, high-risk pregnancies accounted for 11.5% of all pregnancies, whereas moderate pregnancies accounted for 21.6%. 33.1% of pregnancies overall had high or medium risk.Pregnancy brings a lot of physical changes in a woman's body, making it more vulnerable to certain medical conditions. Some medical conditions that can cause high-risk pregnancy include hypertension, gestational diabetes, and preeclampsia.1. HypertensionHypertension or high blood pressure is a condition in which the mother's blood pressure is higher than the ideal range. Hypertension can lead to complications such as preterm labor, low birth weight...2. Gestational DiabetesGestational diabetes is a condition that can really affects pregnant women who didn't have diabetes before pregnancy. It indeed leads to high blood sugar levels, which can indeed cause complications such as preterm labor, macrosomia or a giant baby, and respiratory distress syndrome.3. PreeclampsiaPreeclampsia is a condition that affects pregnant women after 20 weeks of gestation. It leads to high blood pressure and damage to organs like the kidneys and liver. Preeclampsia can cause complications such as preterm delivery, low birth weight, and long-term health problems for both the mother and the baby.
Continue Reading: https://www.drshubhragoyal.com/welcome/blogs/introduction-to-high-risk-pregnancy--what-does-it-mean
#High Risk Pregnancy#Pregnancy with heart disease#Rh incompatibility#Oligohydramnios#Uterine fibroids pregnancy#Pregestational diabetes#Cervical insufficiency#Pregnancy after 35#Recurrent miscarriages#Intrauterine growth retardation#Placental abruption#VBAC risks (Vaginal Birth After Cesarean)#Perinatal infections#Pregnancy-induced hypertension#Chronic kidney disease pregnancy#Antiphospholipid syndrome pregnancy#Congenital anomalies risk
1 note
·
View note
Text
Uterine Tenaculum: A Crucial Tool in Gynecological Procedures

A uterine tenaculum is a specialized surgical instrument used in gynecology for grasping and stabilizing the cervix or uterus during various medical procedures. It plays a vital role in procedures such as intrauterine device (IUD) insertion, dilation and curettage (D&C), hysteroscopy, and other gynecological surgeries. Its uterine tenaculum ability to provide a firm grip on delicate tissues makes it an essential tool in women’s healthcare.
Design and Structure
The uterine tenaculum features a long, slender handle with a locking mechanism that allows the surgeon to maintain a steady grip. The working end of the instrument consists of sharp, hook-like tips designed to securely grasp the cervix without excessive pressure. These hooks allow the tenaculum to hold the uterus in place while minimizing slippage, which is especially important for procedures requiring precision and stability.
Tenacula are typically made of high-quality stainless steel to ensure durability, resistance to corrosion, and ease of sterilization. Some modern versions are available in disposable forms, providing convenience and reducing the risk of cross-contamination.
Common Medical Applications
One of the most frequent uses of a uterine tenaculum is during intrauterine device (IUD) insertion. The instrument is used to gently grasp the cervix and stabilize it, making it easier for the healthcare provider to insert the IUD correctly. This ensures accurate placement and reduces the risk of complications.
In dilation and curettage (D&C) procedures, the tenaculum is essential for holding the cervix steady while the uterus is gently dilated. This stability allows for safe and effective removal of uterine lining in cases of miscarriage, heavy menstrual bleeding, or diagnostic testing.
The instrument is also used in hysteroscopy, where a thin camera is inserted into the uterus to examine the lining. By stabilizing the cervix, the tenaculum aids in smooth insertion of the hysteroscope, ensuring a clear view for the physician. Additionally, in certain types of gynecological surgeries, such as fibroid removal or cervical biopsies, the tenaculum provides the necessary traction to facilitate precise surgical movements.
Benefits of Using a Uterine Tenaculum
The primary advantage of the uterine tenaculum is its ability to provide a secure hold on the cervix or uterus, allowing for controlled and efficient medical procedures. This reduces the risk of complications and ensures that instruments can be used with precision.
Another benefit is its role in minimizing patient discomfort by making procedures quicker and more accurate. While the sharp hooks of the tenaculum may cause slight discomfort, the stability it provides ultimately contributes to a smoother experience for both the patient and the healthcare provider.
Furthermore, the tenaculum’s design ensures minimal tissue damage. Although small puncture marks may be left on the cervix, these typically heal quickly without complications.
Proper Handling and Sterilization
To ensure patient safety, proper sterilization of reusable uterine tenacula is essential. The instrument must be thoroughly cleaned and sterilized using autoclaving or chemical disinfection methods. Disposable versions offer a sterile, single-use alternative, reducing the risk of infection and cross-contamination.
Healthcare providers must also use the instrument with care, applying gentle but firm pressure to avoid unnecessary trauma to cervical tissue. Proper training in its use helps minimize patient discomfort and enhances procedural success.
Conclusion
The uterine tenaculum is an indispensable tool in gynecological and obstetric procedures, offering stability, precision, and ease of use. Whether in routine procedures like IUD insertion or more complex surgical interventions, this instrument plays a crucial role in ensuring effective and safe medical care for women. With careful handling and proper sterilization, the uterine tenaculum remains a vital component of modern gynecological practice.
0 notes
Text
Empowering Women’s Health: Women’s Clinics in Singapore

Women’s health is a crucial aspect of overall well-being, and women’s clinics in Singapore provide specialized care to address the unique health needs of women. Whether you are looking for routine checkups, family planning services, or support for more complex conditions, these clinics are dedicated to offering comprehensive care. In this article, we will explore the importance of women’s clinics Singapore and how they support women in maintaining optimal health at every stage of life.
The Importance of Women’s Clinics in Singapore
Women’s clinics in Singapore focus on providing high-quality healthcare that caters specifically to women. From adolescence to menopause and beyond, women face health challenges that differ from those of men. By visiting a specialized clinic, women benefit from expertise in gynecology, reproductive health, hormonal management, and more. These clinics are designed to create a safe and supportive environment where women can seek medical advice, treatment, and preventative care.
Key Services at Women’s Clinics in Singapore
Women’s clinics in Singapore offer a variety of services to support women’s health. Whether you’re looking for routine care or treatment for specific conditions, these clinics ensure that all aspects of women’s health are covered.
1. Gynecological Care and Preventive Services
Routine gynecological exams are essential for maintaining reproductive health. Women’s clinics in Singapore offer regular screenings such as Pap smears, pelvic exams, and breast exams to help detect early signs of cancer, infections, and other gynecological issues. Preventive care is a cornerstone of women’s health, and these screenings are crucial in identifying potential health problems before they become serious.
2. Fertility Services
For women trying to conceive or facing fertility challenges, women’s clinics in Singapore offer comprehensive fertility assessments and treatments. From ovulation tracking to advanced procedures like In-Vitro Fertilization (IVF), these clinics provide personalized care to help women achieve their dream of becoming mothers. Fertility specialists also offer guidance on lifestyle changes and medical interventions that can improve fertility outcomes.
3. Pregnancy and Maternity Care
Pregnancy is an exciting but sometimes overwhelming experience. Women’s clinics in Singapore offer comprehensive prenatal care, including regular checkups, ultrasounds, blood tests, and screenings to monitor the health of both mother and baby. Postpartum care is also provided to ensure new mothers recover and receive the emotional and physical support they need during the early stages of motherhood.
4. Contraceptive Advice and Family Planning
Family planning is a personal decision, and women’s clinics in Singapore offer a variety of contraceptive options to help women make informed choices. Whether you prefer oral contraceptives, intrauterine devices (IUDs), implants, or natural methods, healthcare professionals at women’s clinics will help you choose the most suitable method based on your health, lifestyle, and family planning goals.
5. Hormonal Health and Menstrual Disorders
Hormonal imbalances can affect women at various stages of life, from puberty through menopause. Women’s clinics offer treatments to address conditions like Polycystic Ovary Syndrome (PCOS), endometriosis, and irregular periods. By managing hormonal health, women can improve their overall well-being and prevent conditions that may lead to more serious health issues in the future.
6. Menopause Management
Menopause marks a significant transition in a woman’s life, and it can bring a range of symptoms, including hot flashes, mood swings, and sleep disturbances. Women’s clinics in Singapore provide specialized care to manage these symptoms, including hormone replacement therapy (HRT) and other non-hormonal options. The goal is to help women navigate this transition smoothly and improve their quality of life during menopause.
7. Sexual Health and Wellness
Sexual health is an important aspect of overall well-being, and women’s clinics in Singapore offer services to promote sexual wellness. These services include screenings for sexually transmitted infections (STIs), HPV vaccinations, and treatments for sexual dysfunction. Clinics also provide counseling and support for women experiencing sexual health concerns or relationship issues.
8. Mental Health and Emotional Well-being
Mental health plays a crucial role in women’s overall health, and many women’s clinics in Singapore now offer counseling and mental health services. From dealing with stress, anxiety, and depression to addressing the emotional challenges that can come with pregnancy or menopause, these clinics offer support to help women manage their mental health.
Benefits of Visiting a Women’s Clinic in Singapore
Expert Care Women’s clinics in Singapore are staffed with healthcare professionals who specialize in women’s health. This specialized care ensures that women receive the most up-to-date and effective treatments for their unique health needs.
Comprehensive Services Women’s clinics offer a wide range of services, from routine checkups and pregnancy care to fertility treatments and menopause management. This makes it easier for women to access all the healthcare they need in one location, saving time and reducing the stress of visiting multiple specialists.
Confidential and Supportive Environment Visiting a women’s clinic provides a safe, confidential, and non-judgmental space for women to discuss sensitive health concerns. This is particularly important when addressing sexual health, mental health, or other issues that may feel uncomfortable to discuss in a general healthcare setting.
Early Detection and Prevention Women’s clinics in Singapore place a strong emphasis on preventive care, offering regular screenings and checkups to detect health conditions early. Early diagnosis and treatment are crucial for improving outcomes and preventing more serious complications down the road.
Personalized Treatment Plans At a women’s clinic, healthcare providers take the time to understand each woman’s unique health history and needs. This allows them to create personalized treatment plans that focus on the individual’s goals and health concerns, ensuring that women receive the best care possible.
How to Choose the Right Women’s Clinic in Singapore
When selecting a women’s clinic, consider the following factors:
Reputation: Look for clinics with positive reviews and a good reputation for providing quality care. Recommendations from other women or healthcare providers can also be helpful.
Range of Services: Ensure that the clinic offers the services you need, whether it's routine gynecological exams, fertility treatments, or menopause management.
Experienced Healthcare Providers: Choose a clinic with qualified and experienced healthcare professionals who specialize in women’s health.
Convenience: Consider the location and accessibility of the clinic. Choose one that is conveniently located and offers flexible appointment hours.
Cost and Insurance: Verify that the clinic accepts your insurance or provides affordable options. Many clinics offer payment plans to make healthcare more accessible.
Conclusion
Women’s clinics in Singapore are essential for supporting women’s health throughout life. By offering specialized care in a range of areas, from gynecological services to mental health support, these clinics ensure that women receive the comprehensive care they need to live healthy and fulfilling lives. If you are looking for personalized healthcare that understands the unique needs of women, visiting a women’s clinic in Singapore is a step toward maintaining your health and well-being.
0 notes
Text
Understanding Fertility Treatments & IVF: A Guide for Hopeful Parents
Starting a family is a dream for many, but for some, the journey to parenthood can be challenging. Fertility issues affect numerous couples and individuals worldwide, making advanced reproductive treatments a beacon of hope. This guide will help you understand fertility treatments, IVF procedures, and how choosing the right approach can increase your chances of success. If you are searching for reliable treatment options, an Indore fertility & IVF center could be an ideal choice for modern and effective solutions.

Understanding Fertility Issues
Fertility problems can stem from various factors, including hormonal imbalances, lifestyle choices, medical conditions, and age-related decline in reproductive health. Both men and women can face fertility challenges, which is why a thorough evaluation is crucial before beginning any treatment.
Common Causes of Infertility
Ovulation Disorders: Conditions like PCOS (Polycystic Ovary Syndrome) can affect regular ovulation.
Blocked Fallopian Tubes: Often due to infections or endometriosis, blocked tubes prevent sperm from reaching the egg.
Low Sperm Count & Quality: Male factor infertility can significantly impact conception chances.
Uterine Conditions: Fibroids, polyps, and irregularities in the uterus can make implantation difficult.
Age-Related Decline: As women age, egg quality and quantity decrease, making conception harder.
Fertility Treatments: An Overview
Fertility treatments range from simple medical interventions to advanced assisted reproductive techniques (ART). The right treatment depends on the underlying cause of infertility.
1. Ovulation Induction
For women who have irregular ovulation, medications like Clomiphene Citrate and Letrozole can stimulate ovulation, increasing the chances of natural conception.
2. Intrauterine Insemination (IUI)
This procedure involves placing washed and concentrated sperm directly into the uterus during ovulation, increasing the likelihood of fertilization.
3. In Vitro Fertilization (IVF)
IVF is one of the most effective fertility treatments available today. Couples seeking treatment at an Indore fertility & IVF center can benefit from advanced technology and experienced specialists in this field.
Steps Involved in IVF:
Ovarian Stimulation: Medications stimulate the ovaries to produce multiple eggs.
Egg Retrieval: Mature eggs are collected from the ovaries using a minor surgical procedure.
Fertilization: The eggs are fertilized with sperm in a laboratory.
Embryo Transfer: The healthiest embryo is transferred to the uterus for implantation.
Pregnancy Test: After two weeks, a blood test confirms whether implantation was successful.
4. Intracytoplasmic Sperm Injection (ICSI)
ICSI is an advanced IVF technique where a single sperm is directly injected into an egg. This method is beneficial for couples with severe male infertility.
5. Egg Freezing & Embryo Preservation
For individuals who want to delay parenthood due to medical or personal reasons, egg freezing and embryo preservation offer future fertility options.
6. Donor Eggs & Sperm
When natural conception is not possible due to poor egg or sperm quality, donor eggs or sperm can be used in IVF treatments.
Choosing the Right Fertility Treatment
With numerous treatment options available, choosing the right one depends on factors like age, medical history, and the specific cause of infertility. Consulting a specialist at an Indore fertility & IVF center can provide personalized treatment plans tailored to your needs.
Lifestyle Factors & Fertility
While medical treatments play a crucial role in fertility, lifestyle changes can also significantly improve reproductive health.
Tips to Enhance Fertility:
Maintain a Healthy Diet: A diet rich in antioxidants, folic acid, and essential vitamins supports reproductive health.
Regular Exercise: Moderate exercise helps maintain hormonal balance and weight.
Reduce Stress: Chronic stress can interfere with ovulation and sperm production.
Avoid Smoking & Alcohol: Both can negatively affect fertility in men and women.
Track Ovulation: Understanding your ovulation cycle can help time intercourse for optimal conception chances.
The Emotional Journey of Fertility Treatments
Undergoing fertility treatments can be emotionally challenging. Many couples experience stress, anxiety, and uncertainty during the process. Seeking support from counselors, support groups, or friends and family can help you navigate this journey with a positive mindset.
Success Rates of Fertility Treatments
The success of fertility treatments varies based on age, underlying conditions, and treatment type. IVF has a higher success rate compared to other treatments, especially for women under 35. At an Indore fertility & IVF center, advanced technology and specialized care improve the chances of achieving a successful pregnancy.
Final Thoughts
Fertility treatments have transformed the lives of countless couples struggling with infertility. Whether through IVF, IUI, or other assisted reproductive techniques, modern medicine provides hope for those facing difficulties in conceiving.
If you are looking for expert care and advanced reproductive solutions, an Indore fertility & IVF center can offer comprehensive treatment options to help you fulfill your dream of parenthood. Understanding your fertility options and making informed decisions can bring you one step closer to embracing the joys of parenthood.
0 notes
Text
“Ivy Roe”, 31 (UK 1971)
A study published in a 1971 edition of the British Medical Journal reports the painful death of a 31-year-old woman who underwent a “safe and legal” abortion at a hospital. She was later given the name Ivy Roe.

Abortion on demand was illegal in the UK until the 1967 Abortion Act, which allowed them to be done up to 28 weeks (later reduced to 24 weeks in 1990) and sometimes later. After abortion was legalized, the West Middlesex Hospital began conducting “safe and legal” abortions with various methods. The data on the side effects to the clients was used to determine the risk of the different methods.
Out of all the West Middlesex Hospital abortion clients undergoing “safe and legal” abortions with experimental techniques, 83 underwent intrauterine insertion of a substance referred to as utus paste. Contrary to an earlier claim from abortion supporters that this method had no serious complications, the clients suffered severe fever, UTI, retained fetal tissue, abnormal bleeding, cervical trauma, suspected peritonitis, tachycardia, sepsis, uterine perforation and death.
One of the 83 clients was 31-year-old Ivy Roe. The study notes that she was married and was 16 weeks pregnant. Before the abortion, Ivy was in good condition. It is unclear if Ivy knew that she was being tested on and she may not have ever consented to being part of an experiment.
Ivy went into contractions and premature labor as planned. 20 hours after the abortion was started, she had her dead baby. 4 hours after that, her uterus was dilated and curettage was used to remove any body parts or placenta that might have been left behind. This was the procedure for all of the 83 test subjects whose abortions were considered successful at that point.
By the next day, Ivy was already showing signs that something was seriously wrong. She had a fever and her uterus was swollen to the size that it would have been if she were 12 weeks pregnant. She was given antibiotics for 3 days and then sent home even though her uterus was still swollen.
When she was home, Ivy was still in pain. She had to urinate far too frequently, and suffered abdominal pain. She went to a doctor, who noticed her tachycardia but didn’t find a fever and gave her sulphonamides and antibiotics.
A week after being discharged from West Middlesex Hospital, Ivy was dead.
Ivy’s autopsy was sickening and horrifying. Her uterus was ruptured and had necrotic tissue. The uterine walls were congested and there was thick green pus. She died a slow and excruciating death from her severe infection and internal injuries.
Ivy was promised a “safe and legal” abortion, but she didn’t know that legalization didn’t make it safe.

#death from legal abortion#tw abortion#unsafe yet legal#pro life#abortion#abortion debate#tw ab*rtion#pro choice#tw murder#tw human experimentation
4 notes
·
View notes
Text
Male Infertility: Causes, Diagnosis, and Treatment

Infertility is a growing concern among couples, with male infertility contributing to nearly 50% of cases. It is defined as the inability to conceive after a year of regular unprotected intercourse. Understanding the causes of male infertility is crucial for early diagnosis and effective treatment.
Common Causes of Male Infertility
1. Hormonal Imbalances
Hormones play a crucial role in sperm production. Conditions like hypogonadism, thyroid disorders, and testosterone deficiencies can lead to low sperm count and poor motility.
2. Varicocele
A varicocele is an enlargement of veins within the scrotum that affects sperm production and quality due to increased temperature in the testicles.
3. Infections and STDs
Sexually transmitted diseases (STDs) and other infections like prostatitis and epididymitis can cause inflammation and block sperm movement.
4. Genetic Disorders
Certain genetic conditions, such as Klinefelter syndrome, Y chromosome microdeletions, and cystic fibrosis, can lead to abnormal sperm production or absence of sperm.
5. Lifestyle Factors
Unhealthy habits such as smoking, excessive alcohol consumption, drug use, and obesity negatively impact sperm quality and fertility.
6. Environmental and Occupational Hazards
Exposure to chemicals, radiation, heavy metals, and excessive heat can impair sperm production and function.
7. Medications and Treatments
Certain medications, including anabolic steroids, chemotherapy, radiation therapy, and antidepressants, can affect male fertility.
Diagnosis of Male Infertility
To determine the cause of infertility, a doctor may recommend the following tests:
Semen Analysis: Evaluates sperm count, motility, and morphology.
Hormonal Testing: Measures testosterone and other hormone levels.
Genetic Testing: Identifies underlying genetic abnormalities.
Imaging Tests: Ultrasound or MRI to check for blockages or varicoceles.
Testicular Biopsy: Determines sperm production capability.
Treatment Options for Male Infertility
1. Lifestyle Modifications
Quit smoking and alcohol.
Maintain a healthy diet rich in antioxidants.
Exercise regularly and manage stress.
2. Medications and Hormone Therapy
Hormonal treatments to restore balance.
Antibiotics to treat infections.
Medications to improve sperm production.
3. Surgical Interventions
Varicocele Repair: Surgery to remove enlarged veins.
Vasectomy Reversal: Restores sperm flow in cases of previous vasectomy.
Sperm Retrieval Techniques: Used in cases of zero sperm count.
4. Assisted Reproductive Techniques (ART)
Intrauterine Insemination (IUI): Direct placement of sperm into the uterus.
In Vitro Fertilization (IVF): Combining sperm and egg in a lab.
Intracytoplasmic Sperm Injection (ICSI): Injecting a single sperm into an egg.
Conclusion
Male infertility can be distressing, but with the right diagnosis and treatment, many couples achieve successful pregnancies. If you are facing fertility issues, consult Dr. Swapnil Langde for expert guidance and personalized treatment options.Post navigation
#infertility treatment in hadapsar#low amh treatment in hadapsar#ovarian rejuvenation and treatment in hadapsar#recurrent pregnancy loss in hadapsar
0 notes