#herpes shingles
Explore tagged Tumblr posts
Text
Herpes Cure Treatment in India, Including Free Options
The journey to find a herpes cure is often laden with questions, concerns, and a quest for accessible solutions. In the vibrant tapestry of India's healthcare landscape, both traditional and contemporary treatments converge to offer hope and relief. Let's delve into the avenues of Herpes Cure Treatment in India, exploring not only effective treatments but also options that extend a helping hand to those seeking free alternatives.
Navigating Herpes Cure Treatment in India
Traditional Wisdom Meets Modern Solutions
India, with its rich history of traditional medicine, brings forth a holistic approach to herpes treatment. Ayurveda, the ancient healing system, and contemporary medical advancements are harmoniously integrated to address the complexities of herpes management.
Accessible Healthcare for All
Recognizing the importance of accessible healthcare, various initiatives and programs in India aim to provide Free herpes treatment in India at no cost. These efforts align with the goal of ensuring that everyone, regardless of economic status, can access essential medical care.
Herpes Cure Treatment Options
Ayurvedic Treatments
Ayurveda, deeply rooted in Indian culture, offers herbal remedies, detoxification therapies, and lifestyle modifications as part of herpes treatment. Ayurvedic centers across India provide specialized care, combining centuries-old wisdom with modern understanding.
Government Healthcare Initiatives
Government-sponsored healthcare programs and clinics in India contribute significantly to Free herpes treatment in India accessibility. These initiatives aim to make quality healthcare services, including antiviral medications, available to the broader population.
Community Health Camps
In various regions of India, community health camps play a crucial role in reaching underserved populations. These camps often provide free herpes screening, consultation, and basic medications, ensuring that healthcare reaches those who need it most.
FAQs
Q: Are Ayurvedic treatments for herpes widely available in India?
A: Yes, Ayurvedic treatments for herpes are widely available in India. Renowned Ayurvedic centers, particularly in states like Kerala and Himachal Pradesh, specialize in holistic approaches to manage herpes symptoms.
Q: How can individuals access free herpes treatment in India?
A: Free herpes treatment in India options are often available through government healthcare facilities, community health camps, and nonprofit organizations. These initiatives aim to provide essential medical care without financial barriers.
Q: Are there government-sponsored medications for herpes in India?
A: Yes, government healthcare programs in India often include antiviral medications for herpes as part of their essential medication offerings. These medications are provided at subsidized or no cost to eligible individuals.
Q: What role do community health camps play in herpes treatment?
A: Community health camps serve as outreach programs, especially in rural and underserved areas. They provide free screenings, consultations, and basic medications, ensuring that individuals receive timely healthcare interventions. In conclusion, the pursuit of Herpes Cure Treatment in India is a journey encompassing both traditional wisdom and modern healthcare initiatives. With Ayurveda offering holistic solutions and free healthcare options ensuring accessibility, India stands as a beacon of hope for those navigating the challenges of herpes management. Embrace the diverse healthcare avenues, and let the journey toward healing be inclusive and compassionate.
#herpes cure#free herpes treatment in india#herpes treatment in india#herpes simplex virus#treat herpes#cure for herpes in india#herpes outbreak#herpes treatment#herpes shingles#herpes medication treatment
0 notes
Text

O'nekataniel and O'qiwilqilth (not to be confused with Q'wilqilth), an unlikely friendship When the putrid one was awakened, there weren't enough healwings to combat it, O'nekataniel made the hard decision of freeing the plague angels to banish the tumor once and for all
started with O'qiwilqilth, O'nekataniel and them fought side by side against the putrid one, when their combined forces wasn't enough, they freed more plague angels to push back, by the time the army was arranged, the putrid one grew too large
Both O'qiwilqilth and O'nekataniel had decided to lead the putrid one outside of God's body, a strategy that would likely doom both of them, during the final part of their plan, O'qiwilqith went ahead with O'nekataniel, sacrificing themself to banish the putrid one
After this debacle was over, plague angels would be free to wander around again, having proven that they can aid and help around the Great Body of Heaven just like God's cells can, a decision that would be revoked by M'ôu-arráial later on
O'qiwilqilth's sacrifice also positively impacted them- they said loud and clear their Vows to God and said that they would die in His name, one of the ideas at the time were that plague angels, were uncapable of following their vows like the others
#worldbuilding#ocs#n before anyone asks#O'nekataniel is a macrophage cell (white healwings as theyre called)#O'qiwilqilth is a herpes zoster / shingles plague angel
33 notes
·
View notes
Text

10 causes of a skin outbreak. #skincare #Herpanacine
#acne#cold sores#herpes#eczema#shingles#healthy#dr wayne diamond#vitamins#healthy living#naturopath#skincare#health#herpanacine#psoriasis#immune support#skin
2 notes
·
View notes
Text
I’m on sick leave for another week. This morning I thought it would be fine to go back to work (though I was unsure even then, but I thought I’d try), but after a few hours I realized that... nah, I’m still in pain and can’t focus. And I realized that if this was anyone else, I’d tell them to go take more time off until they’re fully healthy again - and if I’d be nice to someone else, I shouldn’t be mean to myself.
Like, for some reason, just because it’s not a “gives you a fever” type of illness, my brain keeps telling me I’m “not sick enough” to not work and that I’m lazy and just looking for an excuse, even though I literally have shingles, a painful disease that can cause permanent nerve damage and chronic pain if not treated properly.
I thought I’d have to justify myself at the doctors’ and explain why I need a bit more time off - like a day or two - so I kept saying stuff like “I know it doesn’t look that bad anymore, but...”. And the doctor just went “Let me stop you right there”, then explained how shingles is a nerve disease and not a skin disease so the worst part of it is internal where you can’t see it, and then she prescribed me new pain meds and gave me another whole week off - gosh, I was so thankful.
7 notes
·
View notes
Text
I was vaccinated against chickenpox, and my parents were vaccinated against it, but my grandparents were not vaccinated. The virus that causes chickenpox likes to hide away in your body for decades after you first catch it, and eventually comes back as a horrible painful rash spread throughout your nervous system, known as shingles. That happened to my grandpa a few years ago, with the rash spreading across his back, left side, and left leg. It lasted for days. He couldn't sit or lie on his back because doing so caused so much agony.
Make sure you're vaccinated against chicken pox. You really don't want to deal with that.
I have a theory about gen z and millennials, so please help me out with this poll.
Please make sure to vote as to whether you got vaccinated as a child or not, if you did not get chicken pox. Take care, spread this around, and vaccinate your fucking kids. Poll is not exclusive to any country. Vote no matter where you're from.
#chicken pox#chickenpox#vaccination#polls#shingles#zoster#herpes zoster#varicella zoster virus#varicella
12K notes
·
View notes
Text
#Skin diseases#Skin disorders#Common skin conditions#Types of skin diseases#Chronic skin conditions#Skin rash treatment#Skin condition symptoms#Skin disease causes#Treatment for skin diseases#Skin health#Specific Skin Diseases:#Acne#Psoriasis#Eczema#Rosacea#Melasma#Vitiligo#Fungal skin infection#Ringworm#Dermatitis#Hives#Seborrheic dermatitis#Shingles (Herpes Zoster)#Lupus (Skin lupus)#Warts#Cold sores#Actinic keratosis#Basal cell carcinoma (BCC)#Squamous cell carcinoma (SCC)#Skin cancer
1 note
·
View note
Text
The link between shingles and herpes zoster oticus: from chickenpox to facial nerve paralysis - Dr Sharad ENT
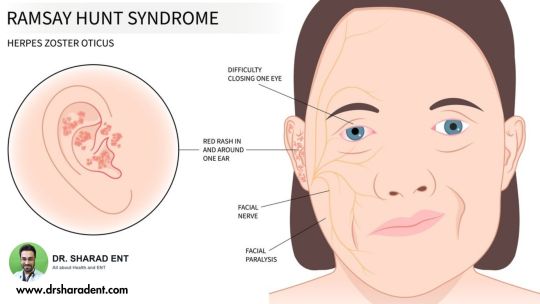
Understanding the progression: The correlation between the Varicella-zoster virus, responsible for chickenpox, and its reactivation as herpes zoster oticus, leading to facial nerve paralysis commonly known as shingles.
For More Visit- https://www.drsharadent.com/from-chickenpox-to-nerve-infection-the-link-between-herpes-zoster-oticus-and-shingles/
0 notes
Text
A little microbiology lesson for folks who caught an active virus of chicken pox. Chicken pox is caused by a virus called: varicella-zoster virus.
THIS VIRUS GOES DORMANT IN YOUR BODY. Like a criminal on the run, it hides out in the neurons near your spinal cord. Until it thinks the coast is clear. THIS VIRUS CAN REACTIVATE AND GIVE YOU SHINGLES.
If you thought the Chicken Pox was uncomfortable and bad, well...its usually worse than Chicken Pox. THIS VIRUS NEVER GOES AWAY IT JUST GOES BACK TO SLEEP So if you went to a chicken pox party, and caught an active form of Chicken Pox and you are now an adult and you are getting these GNARLY ITCHY patchy sometimes bubbly rashes that are scab over...it might be Shingles, and that's from the same virus and its just been squatting around in your spine. If you're mad finding this info out, join the club, I read this in a textbook and asked my mom and she admitted to letting me hang out with someone with chicken pox. And I told her if I get shingles, I'm gonna be double mad, because I DID NOT SLEEP during that rash.
I just noticed that I still have some chicken pox scars even as an adult, so i'm curious. If you have scars from it, are they more on the left side of your body or the right? Mine are all on my right!
I wasn't given it on purpose, but I had a very miserable summer break in elementary school where i just stared out the window and tried not to itch.
#chicken pox#chicken pox parties#herpes#shingles#dermatitis#health#vaccine#rash#science#microbiology#virus
1K notes
·
View notes
Text
What Exactly is Shingles (Herpes Zoster)?

Shingles, also referred to as herpes zoster, is a viral infection caused by the reactivation of the varicella-zoster virus, the same virus responsible for chickenpox. This reactivation can occur years after the initial infection or exposure to the virus, as it remains dormant in the body for life. Visit www.shinglesprotection.sa.com to know more about shingles.
0 notes
Text
Understanding Herpes Outbreaks and Medication Treatment
Herpes, a viral infection caused by the herpes simplex virus (HSV), often manifests in periodic outbreaks that can be both physically and emotionally challenging. While there is no cure for herpes, herpes medication treatment play a crucial role in managing outbreaks and alleviating symptoms. Let's delve into the intricacies of herpes outbreaks and the medications designed to provide relief.
Understanding Herpes Outbreaks: The Storm Within
Herpes outbreaks occur when the virus, lying dormant in nerve cells, becomes reactivated. Factors such as stress, illness, hormonal changes, or a weakened immune system can trigger the reemergence of the virus, leading to the characteristic symptoms of herpes, including painful sores, itching, and flu-like symptoms.
Herpes Medication Treatment: Calming the Storm
In the realm of herpes management, antiviral medications take center stage. These medications, including acyclovir, valacyclovir, and famciclovir, work by inhibiting the replication of the virus. When taken during an outbreak, they can reduce the severity and duration of symptoms, providing much-needed relief.
Antiviral Medications: A Closer Look
Acyclovir: A pioneer in herpes medication treatment, acyclovir is available in various forms, including oral medication and topical cream. It effectively curtails the replication of the virus, minimizing the impact of outbreaks.
Valacyclovir: Known for its convenient dosing schedule, valacyclovir is the prodrug of acyclovir. Once ingested, the body converts it into acyclovir, enhancing its antiviral properties.
Famciclovir: This antiviral medication is particularly effective against the herpes simplex virus. It hinders the virus's ability to reproduce, mitigating the severity of outbreaks.
Medication Treatment Timing: Key to Efficacy
Initiating antiviral herpes medication treatment at the onset of symptoms or during the prodromal phase (early warning signs before visible sores appear) is crucial for optimal efficacy. Early intervention can shorten the duration of outbreaks and reduce symptom intensity.
Holistic Approaches: Beyond Medication
While antiviral medications form the cornerstone of herpes outbreak management, adopting holistic approaches can enhance overall well-being. Stress reduction techniques, maintaining a healthy lifestyle, and staying informed about triggers contribute to a comprehensive strategy for managing outbreaks.
Empowering Individuals: Knowledge is Key
Understanding the dynamics of herpes outbreaks and the available medication treatments empowers individuals to take an active role in their healthcare. Regular communication with healthcare providers ensures that treatment plans are tailored to individual needs, fostering a collaborative approach to managing herpes.
Conclusion: Riding the Waves of Resilience
Herpes outbreaks may create stormy moments, but with the right tools and knowledge, individuals can navigate the waves of resilience.Herpes medication treatment provide a beacon of hope, offering relief during outbreaks and contributing to the overall management of herpes. By combining medical interventions with holistic approaches and staying informed, individuals can ride the waves with strength and fortitude, embracing a journey of resilience and well-being.
#herpes cure#free herpes treatment in india#herpes treatment in india#herpes simplex virus#treat herpes#cure for herpes in india#herpes outbreak#herpes treatment#herpes shingles#herpes medication treatment
0 notes
Text

In 2024, Herpanacine Skin & Immune Support has already won FOUR awards for the BEST SKIN SUPPLEMENT and the BEST IMMUNE SYSTEM SUPPLEMENT! Why you might wonder... Because it works!! Millions have achieved CLEAR SKIN, RADIANT SKIN, and a BALANCED IMMUNE SYSTEM. Formulated by Dr. Wayne Diamond, Herpanacine has been on the market for over 34 years with excellent results!
#Skin#healthy#skincare#health#vitamins#dr wayne diamond#herpanacine#natural#acne#eczema#psoriasis#herpes#cold sores#shingles#rosacea#dermatitis
0 notes
Text
Have this annoying itching rash on one side of my back and stomach which might be shingles.
Ugh, why can I never have just one weekend without any pain or illness? As if my chronic digestion problems which already ruin most weekends weren’t enough.
#I'm seeing a dermatologist tomorrow to be sure#One of the emergency ones who works on weekends because if this is shingles it can't wait until monday#personal#Shingles#Herpes Zoster#Gürtelrose
6 notes
·
View notes
Text
Herpes Zoster
Herpes zoster is a skin rash that occurs due to varicella zoster virus (the same virus that causes chicken pox).
0 notes
Text
Decoding Shingles: Insights and Prevention!
Shingles, also known as Herpes Zoster, is like a spectre that can appear out of nowhere and disrupt your life with its painful presence. Imagine this: you’re going about your day, and then, out of nowhere, you start experiencing an intense, burning sensation on one side of your body. Shortly after, a rash of red, blister-like sores appears, leaving you in discomfort and confusion. What’s…
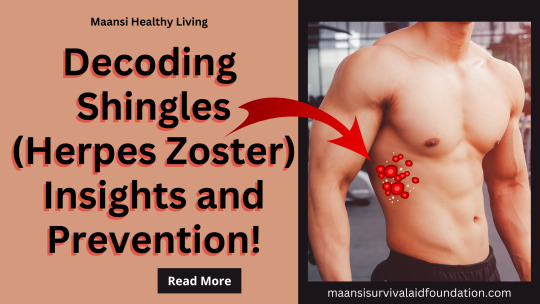
View On WordPress
#Health Insights#Herpes Zoster#Holistic Wellness#Immune system#Prevention tips#Shingles#Shingles Symptoms#Shingles Treatment#Skin Health#Vaccination
0 notes
Text
I know this is rather well tread ground but I truly cannot IMAGINE the level of western european pussy stank that was going on before the widespread implementation of the indoor plumbing system and the advent of germ theory. Walking around with layers upon layers of wool and cotton, stepping in sheep shit and cow shit and pig shit and chicken shit and human shit and dog shit and cat shit and vomit and blood and phlegm and everyone was sneezing and coughing into each other’s faces and they were drinking directly from Poop and Pee River and putting leeches on their herpes sores and syphilis noses and gonorrhea and scabies and shingles and mumps and measles and smallpox and eating their boogers and leaving shit caked to their ass and shitting in buckets and leaving it then throwing it on people and not brushing their teeth and touching their dicks and clits with long dirty fingernails and chewing with their mouths open and bursting their boils and having sex with horses and donkeys and their siblings and their cousins and drinking raw milk and hawking loogies at children and wearing their long pointy shoes in the house and cutting their toenails with their teeth and just cumming in the street in front of everyone and leaving it there and no one gives a shit and only washing their bedding when someone shits or dies on it and you knowwww they let their dogs lick their mouth and never washing their cauldrons and cleaning their hair with spit and burping loud as fuck all the time and it smells like boiled liver… Dude
118 notes
·
View notes
Text
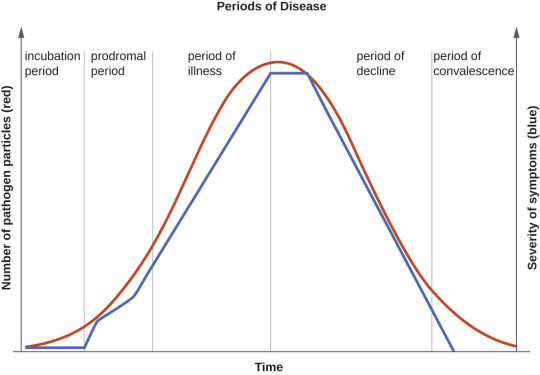
Incubation Periods List
Hi all!
The following is a list of incubation periods for various infectious diseases for all your writing needs. An incubation period is the amount of time between exposure to an infectious agent (bacteria, virus, protozoa or prion) and the person having the first symptoms of the resulting illness. Knowing this is helpful in creating a timeline for your story.
Anthrax: Incubation period of 1-60 days
Avian Flu: Incubation period 3-9 days
Botulism: Incubation period 12-72 hours
Chikungunya: Incubation period 3-7 days
Chlamydia: incubation period 7-21 days
COVID-19: Incubation period 5-10 days
Creutzfeldt-Jacob Disease: Incubation period 10-20 years
Dengue: Incubation period 5-7 days
Diphtheria: Incubation period 2-5 days
Ebola: Incubation period 2-21 days
Hantavirus: incubation period 1-8 weeks
Hepatitis A: incubation period about 28 days
Herpes: Incubation period 2-12 days
Herpes Zoster/Varicella (Chickenpox): Incubation period 14-16 days
Herpes Zoster (Shingles): Incubation period- technically none, as this is a reactivation of the virus that causes chickenpox
HIB: Incubation period 2-10 days
HIV: Incubation period 1-6 weeks to prodrome, approximately 10 years to AIDS
Influenza: Incubation period 1-4 days
Legionnaires Disease: Incubation period 5-6 days
Leprosy: Incubation period 9 months to 20 years
Lyme Disease: Incubation period 3-30 days
Malaria: Incubation period 7-30 days
Measles: Incubation period 10-12 days
Meningitis, Bacterial: Incubation period 2-10 days
Meningitis, Viral: Incubation period 3-10 days
Monkeypox: Incubation period 1-2 weeks
Mumps: Incubation period 16-18 days
Norovirus: Incubation period 12-48 hours
Pertussis: Incubation period 7-10 days
Plague: Incubation period 2-8 days
Pneumococcal Pneumonia: Incubation period 1-3 days
Polio: Incubation period 7-10 days
Q-Fever: Incubation period 2-3 weeks
Rabies: Incubation period 20-90 days
RSV: Incubation period 4-6 days
Smallpox: Incubation period 7-17 days
Syphilis: Incubation period 10-90 days
Tetanus: Incubation period 3-21 days
Tuberculosis: Incubation period 2-10 days
Typhoid: Incubation period 6-30 days
Typhus: Incubation period 1-2 weeks
West Nile Virus: Incubation period 2-6 days
Yellow Fever: Incubation period 3-6 days
Zika: Incubation period 3-14 days
176 notes
·
View notes