#henoch-schonlein purpura
Explore tagged Tumblr posts
Text
I desperately want to connect with more people who were affected with hsp (henoch-schönlein purpura) as children, especially those who have become afflicted with other (physical) disabilities and autoimmune diseases later on in life. despite my wording, I do mean to include people who were diagnosed with hsp later in life, its just a very small minority of an already small group
#what do I even tag this with#autoimmune#actually autoimmune#actually disabled#physically disabled#actually physically disabled#cripple punk#crip punk#autoimmune disease#lupus survivor#(me fr)#henoch-schönlein purpura#henoch-schonlein purpura
2 notes
·
View notes
Text
Top 10 Signs of Autoimmune Disease in Children
Parents try to keep their children away from any harm coming their way. They constantly monitor their growth and development and watch for signs of illness. However, there are a few diseases in children that they find very hard to diagnose. One of these is autoimmune disease, entailing a group of intricate disorders whereby the body’s immunity stages an attack against a number of healthy cells, tissues, and organs of the body.
Autoimmune Disease in Children

When the immune system begins to attack the body’s healthy cells, tissues, and organs, results in development of autoimmune (rheumatic) disorders.
Even though autoimmune diseases are typically linked to adults, parents should be aware that children can also be affected by similar conditions, which tend to be much severe in kids. This group of diseases is often challenging to diagnose and difficult to treat in children .
The common autoimmune diseases affecting children include various subtypes of juvenile idiopathic arthritis, or JIA, a type of arthritis that lasts at least six weeks in children under the age of sixteen years; connective tissue disorders like systemic lupus erythematosus, dermatomyositis, vasculitis disorders like Kawasaki disease and Henoch schonlein purpura
Autoimmune diseases can cause problem in a single specific organ and cause organ-specific diseases (also known as localized) like liver and skin. However, most rheumatological diseases cause systemic involvement i.e., problems throughout the body. For example
-Juvenile idiopathic arthritis affects the skin, eyes, blood, and other organs like lung in addition to the joints
-Juvenile dermatomyositis affects the muscles and skin
– Lupus causes multiorgan involvement:, kidneys, joints, skin, heart, brain, liver
Top 10 Signs of Autoimmune Disease in Children

Fever – prolonged or recurrent
Pain, swelling, and stiffness in the joints
Limping of child
Weakness and pain in muscle
Loss or brittleness of hair
Skin rashes – butterfly shape across the cheeks, rash on eyelids, elbows, salmon pink rash on trunk, psoriasis , etc
Loss of weight without an apparent reason
Ongoing fatigues for which a cause cannot be identified
Poor growth
Swollen lymph glands
Enlarged liver and spleen
Redness of eyes, decrease in vision- uveitis
Changes in behavior and mood
Multiorgan involvement
What Causes Autoimmune Disease?
Unknown is the precise cause behind some children’s immune systems attacking their own bodies. We do know that there is no known etiology of autoimmune disorders, and they are not communicable. Scientists, on the other hand, think that a few steps are involved:
Heredity: Some children are susceptible to an autoimmune disease due to specific genes that are inherited from their parents.
Environmental factors: Unless an infection, exposure to sun, or other trigger occurs, an autoimmune disease may not manifest itself first.
Hormonal factors: Since many autoimmune disorders affect young women and girls in their adolescence, female hormones may also be involved in the onset of many diseases.
How are autoimmune diseases diagnosed?
Pediatricians have unique challenges while dealing with autoimmune disorders. Fever and fatigue are two of the first symptoms that are often generic, meaning they can occur in a wide range of conditions. Many times, symptoms come and go. A single autoimmune disease may present differently in each individual or might possess characteristics with several autoimmune disorders.
A pediatric rheumatologist will first do a comprehensive physical examination and review your child’s whole medical history, including any family history of autoimmune disease. The physician might suggest further lab tests to obtain more details if they suspect an autoimmune condition.
Complete blood count” (CBC) refers to a group of laboratory tests used to determine the size, quantity, and maturity of various blood cells in a given volume of blood.
The liver produces a unique protein, which is measured by the C-reactive protein (CRP). When there is significant inflammation, such as that observed in autoimmune diseases, anywhere in the body, CRP levels usually rise. The initial CBC, ESR AND CRP give a clue towards provisional diagnosis. Further testing on specific tests might be needed in symptoms
The immune system produces abnormal proteins, when it attacks its own tissues. Antinuclear antibody (ANA) and Rheumatoid factor (RF) are one among those.
In order to rule out conditions like infections, tumors, and fractures, the doctor might also choose to examine your child’s organs and tissues more closely. Imaging tests like Magnetic resonance imaging (MRI) and ultrasound will be needed.
Sometimes, in order to diagnose the illness or obtain an indication of how it is developing, your child’s physician will actually take a sample of your child’s tissues, a procedure known as a biopsy.
How are Autoimmune Diseases Treated?
Pediatric rheumatologists are often the primary carers for patients with autoimmune diseases. The care of your child may involve other experts such as a dermatologist (skin), hepatologist (liver), and a nephrologist (kidneys), depending on which tissues or organs are affected. Most autoimmune disorders have no known cure, clinicians strive to do much more than simply treat your child’s symptoms can be well controlled with proper treatment and can lead a normal life.
Your doctor will prescribe medications that combat the damaging inflammation brought on by an autoimmune attack by controlling the immune system.
#Autoimmune Disease in Children#dermatomyositis#systemic lupus erythematosus#lupus#juvenile idiopathic arthritis#vasculitis disorders#Kawasaki disease#Henoch schonlein purpura#rheumatological diseases#Juvenile dermatomyositis#Pediatric rheumatologists
0 notes
Text
The CDC has quietly changed who should AVOID the MMR vaccine.
https://www.cdc.gov/vaccines/vpd/mmr/public/index.html
They now state that ANYONE that “Has a parent, brother or sister with a history of immune system problems��� should AVOID THE MMR VACCINE!
What exactly is an 'immune system problem?" Every autoimmune disorder.
* Achalasia
* Addison’s disease
* Adult Still's disease
* Agammaglobulinemia
* Alopecia areata
* Amyloidosis
* Amyotrophic lateral sclerosis (Lou Gehrigs)
* Ankylosing spondylitis
* Anti-GBM/Anti-TBM nephritis
* Antiphospholipid syndrome
* Autoimmune angioedema
* Autoimmune dysautonomia
* Autoimmune encephalomyelitis
* Autoimmune hepatitis
* Autoimmune inner ear disease (AIED)
* Autoimmune myocarditis
* Autoimmune oophoritis
* Autoimmune orchitis
* Autoimmune pancreatitis
* Autoimmune retinopathy
* Autoimmune urticaria
* Axonal & neuronal neuropathy (AMAN)
* Baló disease
* Behcet’s disease
* Benign mucosal pemphigoid
* Bullous pemphigoid
* Castleman disease (CD)
* Celiac disease
* Chagas disease
* Chronic inflammatory demyelinating polyneuropathy (CIDP)
* Chronic recurrent multifocal osteomyelitis (CRMO)
* Churg-Strauss Syndrome (CSS) or Eosinophilic Granulomatosis (EGPA)
* Cicatricial pemphigoid
* Cogan’s syndrome
* Cold agglutinin disease
* Congenital heart block
* Coxsackie myocarditis
* CREST syndrome
* Crohn’s disease
* Dermatitis herpetiformis
* Dermatomyositis
* Devic’s disease (neuromyelitis optica)
* Discoid lupus
* Dressler’s syndrome
* Endometriosis
* Eosinophilic esophagitis (EoE)
* Eosinophilic fasciitis
* Erythema nodosum
* Essential mixed cryoglobulinemia
* Evans syndrome
* Fibromyalgia
* Fibrosing alveolitis
* Giant cell arteritis (temporal arteritis)
* Giant cell myocarditis
* Glomerulonephritis
* Goodpasture’s syndrome
* Granulomatosis with Polyangiitis
* Graves’ disease
* Guillain-Barre syndrome
* Hashimoto’s thyroiditis
* Hemolytic anemia
* Henoch-Schonlein purpura (HSP)
* Herpes gestationis or pemphigoid gestationis (PG)
* Hidradenitis Suppurativa (HS) (Acne Inversa)
* Hypogammalglobulinemia
* IgA Nephropathy
* IgG4-related sclerosing disease
* Immune thrombocytopenic purpura (ITP)
* Inclusion body myositis (IBM)
* Interstitial cystitis (IC)
* Juvenile arthritis
* Juvenile diabetes (Type 1 diabetes)
* Juvenile myositis (JM)
* Kawasaki disease
* Lambert-Eaton syndrome
* Leukocytoclastic vasculitis
* Lichen planus
* Lichen sclerosus
* Ligneous conjunctivitis
* Linear IgA disease (LAD)
* Lupus
* Lyme disease chronic
* Meniere’s disease
* Microscopic polyangiitis (MPA)
* Mixed connective tissue disease (MCTD)
* Mooren’s ulcer
* Mucha-Habermann disease
* Multifocal Motor Neuropathy (MMN) or MMNCB
* Multiple sclerosis
* Myasthenia gravis
* Myositis
* Narcolepsy
* Neonatal Lupus
* Neuromyelitis optica
* Neutropenia
* Ocular cicatricial pemphigoid
* Optic neuritis
* Palindromic rheumatism (PR)
* PANDAS
* Parkinson's disease
* Paraneoplastic cerebellar degeneration (PCD)
* Paroxysmal nocturnal hemoglobinuria (PNH)
* Parry Romberg syndrome
* Pars planitis (peripheral uveitis)
* Parsonage-Turner syndrome
* Pemphigus
* Peripheral neuropathy
* Perivenous encephalomyelitis
* Pernicious anemia (PA)
* POEMS syndrome
* Polyarteritis nodosa
* Polyglandular syndromes type I, II, III
* Polymyalgia rheumatica
* Polymyositis
* Postmyocardial infarction syndrome
* Postpericardiotomy syndrome
* Primary biliary cirrhosis
* Primary sclerosing cholangitis
* Progesterone dermatitis
* Psoriasis
* Psoriatic arthritis
* Pure red cell aplasia (PRCA)
* Pyoderma gangrenosum
* Raynaud’s phenomenon
* Reactive Arthritis
* Reflex sympathetic dystrophy
* Relapsing polychondritis
* Restless legs syndrome (RLS)
* Retroperitoneal fibrosis
* Rheumatic fever
* Rheumatoid arthritis
* Sarcoidosis
* Schmidt syndrome
* Scleritis
* Scleroderma
* Sjögren’s syndrome
* Sperm & testicular autoimmunity
* Stiff person syndrome (SPS)
* Subacute bacterial endocarditis (SBE)
* Susac’s syndrome
* Sympathetic ophthalmia (SO)
* Takayasu’s arteritis
* Temporal arteritis/Giant cell arteritis
* Thrombocytopenic purpura (TTP)
* Tolosa-Hunt syndrome (THS)
* Transverse myelitis
* Type 1 diabetes
* Ulcerative colitis (UC)
* Undifferentiated connective tissue disease (UCTD)
* Uveitis
* Vasculitis
* Vitiligo
* Vogt-Koyanagi-Harada Disease
Wonder how many doctors are paying attention?
~shared from Jodi Wilson
31 notes
·
View notes
Note
If you get this, answer w/ three random facts about yourself and send it to the last seven blogs in your notifs. anon or not, doesn’t matter, let’s get to know the person behind the blog! ♡ (if u wanna, no pressure!)
hmmm lets see
i have an arrowhead shaped birthmark on my left ankle
i have clinodactyly (my pinkies are bent)
when i was a little kid i got a rare disease called henoch-schonlein purpura and it's even rarer for afab ppl =w=
3 notes
·
View notes
Text
Wait, so my stomach thing might be connected to my ADHD? I swear having ADHD is like the opposite of being overweight in the medical community. Being overweight, everything is blamed on my weight. Hell, I just had a weird German Auto-Immune Disorder that's rarely seen in anyone over the age of 6, and the doctor briefly tried to blame it on my weight (Henoch Schonlein Purpura if anyone is curious.) But it seems like every time I learn about ADHD someone's tell me that some of the stuff I suffer from for seemingly no good reason might be connected, and a doctor has literally never brought that up.
comorbid disorders are either like "yeah ok, makes sense" or "what the fuck"
adhd and autism having a high comorbidity rate? yeah checks out
adhd and autism both having high rates of comorbidity with hypermobility and GI issues? thats an evil curse
14K notes
·
View notes
Text
i love conditions like henoch schonlein purpura bc i think it's cool when things look very crazy but then self-resolve and require no treatment. therapeutic nihilism but make it the actual best option
0 notes
Text
I frequently care for children with serious blood disorders like hemolytic uremic syndrome (HUS) and idiopathic thrombocytopenic purpura (ITP). I also often receive referrals to evaluate kids with symptoms concerning for Henoch-Schönlein purpura (HSP... #Mirari #MirariDoctor #MirariColdPlasma #ColdPlasma
0 notes
Text
All Saints Day
I grew up in a devout Catholic family and attended Catholic schools from Kindergarten through college. As a result, I was deeply immersed in our parish church and actively volunteered for various ministries in our community and at school. However, during my college years, I received a diagnosis of Lupus, Henoch Schonlein purpura, and Rheumatoid Arthritis. After a prolonged period of treatment, my doctor recommended that I begin a Novena to St. Jude, the Patron Saint of Hopeless Cases. My health condition felt quite challenging, and I was in desperate need of divine intervention. This marked the beginning of my devotion to St. Jude.
As I've grown older, I've continued to seek the intercession of several other saints, including St. Clare, Padre Pio, St. Therese, and many more. On this All Saints Day, I want to take a moment to remember and express my deep gratitude for all their intercessions.
Have a blessed All Saints Day!
#all saints day#faithoverfear#saints#catholic#mother mary#padre pio#st clare of assisi#st therese of lisieux#st jude#novena#prayer#catholicism#christianity#blessed virgin mary#faith#faith in jesus
1 note
·
View note
Text
I had very very mild asthma when I was 4-5, so that'd probably make quality of life worse but not kill me. But at age 6-7, I was diagnosed with henoch schonlein purpura, so that'd be what would take me out
Lol, here’s a fun one: if you had been born in the medieval era and without access to modern medicine, how long would you have lived? If I managed to survive being born (unlikely) I would have died at age 22 from appendicitis :) hbu?
112K notes
·
View notes
Text
Henoch Schnolein Purpura (HSP) – Diagnostic criteria Calculator
Henoch-Schonlein Purpura Overview
0 notes
Photo
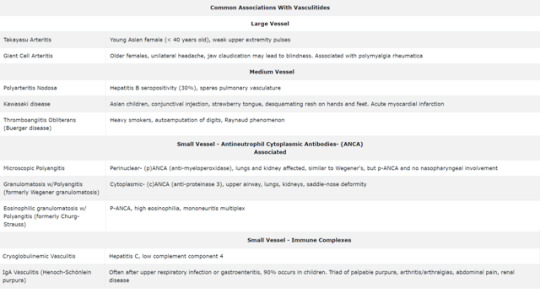
#vasculitis#vasculitides#takayasu arteritis#takayasu#giant cell arteritis#PMR#PAN#Kawasaki#Kawasaki disease#Thromboangiitis Obliterans#Buerger disease#Raynaud phenomenon#MPA#GPA#Churg strauss#Eosinophilic granulomatosis with Polyangitis#PANCA#CANCA#Henoch-Schönlein purpura#Henoch Schonlein purpura#HSP
2 notes
·
View notes
Text
Medical/Life Update
Sup duders so I haven't posted a ton of personal info here in awhile but the past 6 months have been wild. Starting in December 2021 I've had a fluctuating rash on my arms, legs, and trunk that at first I thought was an allergic reaction, hence my post about having the worst "hives" ever on Christmas. After an emergency room trip on New Years Eve and month of phone tag I finally got referred to a rheumatologist in February and diagnosed with Henoch-Schonlein Purpura (HSP) also known as IgA vasculitis. Which is an autoimmune disease more common in children but super rare in adults where the blood vessels in your skin and internal organs/joints become inflamed. Usually it goes away in a few months and leaves no lasting effects which is good.
Except now it's June and it hasn't gone away. In fact, at my last rheumatology appointment 2 weeks ago they said my inflammation markers in my blood have started going up again instead of down so we may need to move on to more intense treatment. For the past few months I've been taking a steroid (prednisone) and an immunosuppressant (mycophenolate) to hopefully counteract my dumb immune system, which has made my flare ups less intense than they were in Dec-Feb pre treatment. But even as they've increased the immunosuppressant my skin has not been totally clear in over six months and every time I so much as step outside my apartment, walk around too much, or wear tight clothing I have massive flare ups. The rash itself is not painful but with friction around my feet and thighs it starts to burn and itch which is no fun at all. And unfortunately having this disease for this long could be bad news for the rest of my organs, which thankfully so far have shown up fine in tests.
So basically at my last rheumatology appointment I was put on the max dose of the mycophenolate with the idea that if this doesn't work we will have to move on to different treatment. There are two options if this happens: a similar immunosuppressant called methotrexate that would basically work like the mycophenolate but maybe magically would do better, or a strong iv infusion called rituximab. Now I have been through my share of weird medical shit but the one thing that still terrifies me is an iv. One of the worst experiences of my life was being hospitalized for a week stuck to an iv in 2012 and the whole time it felt like my arm was being broken. I've always been afraid of needles and in fact my first blood draw at the rheumatologist in Feb I fainted and threw up so now I'm famous with the phlebotomists. So just hearing iv I started to panic a little.
Then the doctor went on to describe the procedure being similar to chemotherapy/biotherapy and included the fun fact of a small risk of deadly anaphylactic shock. I ended up having a full panic attack and sitting on the floor of the office next to an open window while my lovely boyfriend fanned me and got me to drink some water. The doctor kept apologizing for freaking me out but I was just apologizing back like "I have an anxiety disorder it's fine not your fault".
So yeah I go back in on July 12th to see how the max dose and potential last hurrah of my og immunosuppressant works out and meanwhile I am firmly camped in my apartment trying desperately to avoid any flare triggers. I have a spreadsheet now where I rate the rash on each area of my body cause ya girl loves data. My boyfriend Sam has been absolutely wonderful taking care of me throughout this, running urine samples back and forth to the hospital when they kept scheduling my appointments a month apart exactly in line with my period. I am so glad this happened after we moved in together rather than before so I don't have to do this alone or move back in with my parents. My family has tried to understand what's going on but I think only recently started seeing the severity. They've at least stopped trying to guilt me into coming over. Being immunocompromised during a pandemic wasn't enough for them I guess, but minimizing flares so I don't have to do hours of ivs worked. Now we wait.
3 notes
·
View notes
Text
CLOSER - 1: The Courtesy Call
~Pediatric Rotation~
“Hey, Dara! When are we going to do the powerpoint presentation for the final reporting?” Daesung asked Dara while they were doing rounds in the Pediatric ward.
Dara stopped checking the list of admissions on her duty yesterday to answer Daesung. “Hmm. Probably tonight? Do we have a case yet?”
“None yet. But I had a patient last night with fever and rashes on his extremities. It was a Dengue Fever although the rashes were a little different. I was thinking if our differential diagnosis could be Henoch-Schonlein Purpura,” Daesung answered diligently.
“Okay, dibs on that case. Let’s focus on the Dengue Fever and dehydration. Give me the patient’s details later and I’ll print the medical records. Thank you, Dae! I’ll just finish this admission’s list and see you at lunch?” Dara didn’t wait for Dae’s answer. She gave him a big hug and hurriedly left.
Daesung bumped into Chaerin and Bom. “Daesungggg! Where is Dara? We’ve been texting her because our group will be having a courtesy call and orientation in Orthopaedic Department this afternoon,” Chaerin told Daesung.
“Well, she was in Pediatric ward few moments ago. As usual, she’s so focused doing all the senior’s paperworks that she tends to ignore our SMS.” Daesung told them while scrolling on his phone. “But whatever! I am lucky she’s my besty. She’ll save my life from this final report. It’s such a pain in the ass! Dibs on the Dengue Fever case, arasso?”
“Okay. We’ll look for her. I heard the Ortho Chief Res is unpredictable. I don’t want to leave any wrong impressions with the seniors. 😭 Let’s go, Chaerin,” Bom said.
——
Dara finally finished her paperworks and her senior’s backlogs when she checked her phone. “Oh, shoot! It’s already 2pm!” Dara said to herself. She opened her phone’s contacts and dialed Daesung’s number. “Hey, Dae! Did you—“
“Yes, you flaker. I ate in the cafeteria with my groupmates. I knew you were going to miss our lunch so I bought you a burrito. Is that ok? Where are you?” Daesung cut what she was going to say.
“Here in the residents’ call room. Will meet you in our callroom. Thank you and sorry.” Dara said before hanging up the phone. She replied to several SMS including Chaerin’s and Bom’s.
——
After eating late lunch, Dara met up with Chaerin and Bom in front of Orthopaedics Surgery. “Are you ready?” Chaerin and Bom both said at the same time.
“Uh... Actually, I am nervous. This is one of my weakest fields in medicine. I hope the residents are just chill about everything,” Dara honestly said.
“I am nervous too! Uuugh! Let’s go inside!” Chaerin told the two, then she knocked before opening the slide door.
As they entered the room, they found the supposed Orthopedic residents on the opposite side of the room, facing their respective computers and seemed to be doing paperworks and reports. The room was huge, with a large whiteboard in the front. The room could be used for meetings. “Uhm... Hello, doctors! I am Chaerin, the leader of the incoming interns in your department. I am looking for Dr. TOP for our courtesy call and orientation,” Chaerin said in a high pitched tone. Dara then knew that Chaerin was also as nervous as her.
The residents stopped at what they were doing and looked at them when a lean and tall man, sitting in front, looked to their direction and said in a low voice, “No TOP here. Just look for Youngbae. He’s over there.” The man pointed to the back where most of the residents were working on their computers.
“Ah.. Dr. Youngbae?” Chaerin asked, still in a high pitched tone, hoping a doctor named Youngbae would stand and save them from awkwardness. A resident doctor stood up and walked towards the three female interns. The three girls were shocked when he just passed by them and left the room. Another resident, this time, spoke. “I am Seungri. Dr. Youngbae’s just doing some errands. Come and sit. Wait for him here.” And the residents went back to what they were doing as the three sat on empty chairs.
The resident who passed by them and left the room came back with a Potato Corner fries. He put the fries on the girls’ table. “Hello, ladies! Get some fries. I bought it for you. I am Dr. Youngbae, your interns’ monitor for this rotation. I will be the one you get in touch with when you have problems or issues with the residents, consultants, or requirements. What are your names?”
“I am Chaerin.”
“I am Bom.”
As post-duty on that day, Dara wasn’t able to catch up what he was asking. “Huh. Uhm. I’m post-duty today, doc.”
There was silence.
Then Dr. Youngbae and Chaerin burst out laughing. Bom started laughing nervously. Dara’s face became red and asked why they were laughing.
“Doc was asking for our names, silly.” Chaerin said, getting out of breath.
“I’m so sorry! I wasn’t listening. My name is Park Sandara. Dara for short,” Dara said feeling stupid and embarrassed.
“It’s okay, Dara! I like you and your humor. Ha~ha! It seems that you will be directly under me as I am also post-duty today.” Dr. Youngbae genuinely said. “For starters, here are what you’ll do.....” and Dara’s mind drifted again. The orientation lasted for an hour and before they left, he introduced the girls to the residents.
“Guys, our incoming interns are here for courtesy call. As you can see, they are all girls. I am actually worried because we might need a physical strength from a guy.” He said.
“Boys are boring. They’ll do,” the fair skinned with average built Ortho resident commented.
“He’s Dr. Kwon Jiyong, a first year Ortho resident. Then the guy beside him is Dr. Seungri, another first year Ortho resident. They will be the first persons you contact in regards with your work including surgeries, paperworks and backlogs. But since we only have two first year residents and you are three, I will be acting as first year Ortho resident-in-charge of one of you. I guess that’ll be Dara? We’re both post-duty today.” Dr. Youngbae pointed at the tall man in front who seemed to be so drawn by what he was reading. “That’s TOP. He’s our chief resident.”
“He said that he’s not TOP. Probably he didn’t want to talk to us. He’s cute but what a jerk!” Bom commented. Dr. Youngbae laughed at her comment. “Well, that’s all. Chaerin, just email me your contact details and I will send you the schedule of surgeries on your first day. Make sure to deck the pre-duty first. Okay? See you next week.”
“I am sure this group is weak and are just pretty faces,” Jiyong commented after the three left.
#fanfic#roleplay#short story#writeblr#writers on tumblr#kpop#au#fanfiction#jiyong#bigbang#2ne1#2ne1 dara#yg ent#yg entertainment
2 notes
·
View notes
Link
Pathophysiology
In patients with Henoch-Schönlein purpura, immunoglobulin A (IgA) immune complexes are deposited in small vessels, which causes petechiae and palpable purpura. When immune complexes occur in small vessels of the intestinal wall, gastrointestinal hemorrhage may develop. If the immune complexes affect the renal mesangium, it may produce mild proliferative to severe crescentic glomerulonephritis.10
Exposure to an antigen from an infection, medication, or other environmental factor may trigger antibody and immune complex formation. Group A streptococcus has been found in cultures of more than 30 percent of children with Henoch-Schönlein nephritis, and serum antistreptolysin-O titers are more likely to be positive in patients with Henoch-Schönlein nephritis.4,11 Other postulated viral and bacterial triggers of Henoch-Schönlein purpura include parvovirus B19, Bartonella henselae, Helicobacter pylori, Haemophilus parainfluenza, Coxsackie virus, adenovirus, hepatitis A and B viruses, mycoplasma, Epstein-Barr virus, varicella, campylobacter, and methicillin-resistant Staphylococcus aureus.12-15
#henoch-schonlein purpura#infectious diseases#autoimmine disease#immunology#family medicine#pediatrics
0 notes
Text
Internship Diary
I was the only and last intern to have had an extended internship duty, actually an extra month due. I had to deal with it alone. For sure it was depressing and regretful, but at the same time I got to entirely enjoy the journey than that of the last six months. I was still grateful for it, nevertheless.
From witnessing codes and seizures, warding was my favorite. Tiring yet rewarding; I took my time to think and remember the diseases of the patients whom I’ve extracted blood from and had small but meaningful conversations. The ones without any further information are those I couldn’t remember. These were each of the patient’s diseases I’ve listed:
Community acquired pneumonia - 75-year old male patient who was very thin lying on his left side at the ER Pulmonary tuberculosis - 40-year old male patient in the isolation room, he was having hemoptysis aka he was coughing blood lying on the bed and oh he had big antecubital median vein on his right arm Autoimmune hemolytic anemia - This late 40′s female patient seemed healthy and bubbly until I saw her diagnosis. Kawasaki disease - 5-year old male patient in the pediatric ER Henoch schonlein purpura - 6-year old male patient at the pedia ward. I got the chance to converse with the patient’s mother since we both share the same dialect. They were from a town near our place, so they decided to let the patient be admitted to the hospital. But as per the doctor’s request the patient needs to be transferred to a bigger public hospital where nephrologists are in the area. Polycythemia vera Hodgkins lymphoma - This was my last patient from a 16-hour shift on my second to the last day of my extension duty. Non-hodgkins lymphoma - His place was an hour drive away from our town. He was admitted to the ER that night. He was in tears because he was getting tired of his condition and of transferring hospitals; we also share the same dialect. Dengue severe - This patient was eventually admitted from the pediatric ER to PICU. A 9-year old girl who is very giddy and afraid to have another prick; she had oral lesions/manifestations. Chronic kidney disease [Stage 5] - My most unforgettable patient. I couldn’t disclose any information on this one. Right brain infarct - When 2-3am in the morning strikes, vehicular accident victims come rushing in the ER. This time we got this man in restraint since he was moving aggressively all the while being unconscious as we were trying to extract blood from him for further tests. Hours later, he was pronounced dead. Ovarian cancer Obstructive Jaundice - 50-year old female patient admitted in the ER. It got me rushing to the stockroom and get some gloves because of her condition. Even the tiniest prick of HBV-infected blood on a person causes more disease transmission than that of an HIV-infected one. Measles - Due to the limited capacity of the pediatric ER, this 3-year old female patient was admitted outside a tent isolation area since she had measles and it was very communicable. I was able to extract blood from her once, luckily. Pleural effusion; Left chest Post-status thyroidectomy Thyroid cancer Oropharyngeal cancer - This patient is one for the books. He is a 50-year old male patient who had his mouth down to his neck surgically stapled from surgery; had collapsed veins. So we got to extract four times due to the number of tests being requested. Breast cancer Hypothyroidism Hyperthyroidism - Actually my blockmate who had her monthly check on her thyroid hormone status. Disseminated intravascular coagulation/coagulopathy Chronic myelogenous leukemia - We were trained to be junior pathologists as a punishment for making a fuss during duty hours. We were given slides to be examined and diagnose its disease presented by the microscopic features of the blood smear. Pulmonary embolism Ischemic heart disease Tonic clonic & Absence seizure - Lastly, my most memorable patient. Little did I know she was the patient of Dr. Crush. She was aggressively moving while unconscious so he had to restrain her right arm for me to extract blood from the patient.
This is a very wholesome and memorable experience I have had in my life. I have now appreciated what it’s like to be working in a clinical setting, where we’re not just stuck in a four-walled room with books to read on. We got to interact to patients and their conditions. Looking forward to be able to fulfill my purpose of serving other people soon.
To God be the Glory!



1 note
·
View note
