#Thromboangiitis Obliterans
Explore tagged Tumblr posts
Text
Acupuncture is recommended by the World Health Organization for more than 100 conditions.
01) Adverse reactions to radiotherapy and/or chemotherapy
02) Allergic rhinitis including hay fever
03) Biliary colic
04) Depression (including depressive neurosis and depression following stroke)
05) Desentery, acute bacillary
06) Dysmenorrhea
07) Epigastralgia (Acute peptic ulcer, acute and chronic gastritis, and gastro spasm)
08) Facial pain (including craniomandibular disorders)
০9) Headache
10) Hypertension, essential
11) Hypotension, primary
12) Knee pain
13) Leukopenia)
14) Low back pain
15) Morning sickness
16) Nausea and vomiting
17) Neck pain
18) Pain in dentistry (Including dental pain and temporomandibular dysfunction)
19) Periarteritis of the shoulder
20) Postoperative pain
21) Rheumatoid arthritis
22) Sciatica
23) Sprain
24) Stroke)
25) Tennis elbow
26) Abdominal pain (in acute gastroenteritis or due to gastrointestinal spasm)
27) Acne vulgaris
28) Alcohol dependence and detoxification
29) Bell’s palsy
30) Bronchial asthma
31) Cancer pain
32) Cardiac neurosis
33) Cholecystitis, chronic, with acute exacerbation
34) Competition stress syndrome
35) Craniocerebral injury, closed
36) Diabetes mellitus, non-insulin-dependent
37) Earache
38) Epidemic hemorrhagic fever
39) Epistaxis is simple (without generalized or local disease)
40) Eye pain due to subconjunctival injection
41) Facial spasm
42) Female infertility
43) Female urethral syndrome
44) Fibromyalgia and fasciitis
45) Gastrokinetic disturbance
46) Gouty arthritis
47) Hepatitis B virus carrier status
48) Herpes zoster (human (alpha) herpes virus 3)
49) Hyperlipemia
50) Hypo-ovarianism
51) Insomnia
52) Lactation, deficiency
53) Male sexual dysfunction, non-organic
54) Meniere disease
55) Neuralgia, Post-herpetic
56) Neurodermatitis
57) Obesity)
58) Opium, cocaine, and heroin dependence
59) Osteoarthritis
60) Pain due to endoscopic examination
61) Pain in thromboangiitis obliterans
62) Polycystic ovary syndrome (Stein-Leventhal syndrome)
63) Postextubation in children
64) Postoperative convalescence
65) Premenstrual syndrome
66) Prostatitis, chronic
67) Pruritus
68) Radicular and pseudoradicular pain syndrome
69) Raynaud syndrome, primary
70) Recurrent lower urinary tract infection
71) Retention of urine, traumatic
72) Reflex sympathetic dystrophy
73) Schizophrenia
74) Sialism, drug-induced
75) Sjögren syndrome
76) Sore throat (including tonsillitis)
77) Spine pain, acute
78) Stiff neck
79) Temporomandibular joint dysfunction
80) Tietze syndrome
81) Tobacco dependence
82) Tourette syndrome
83) Ulcerative colitis, chronic
84) Vascular dementia
85) Hypothermia
86) Irritable colon syndrome
87) Neuropathic bladder due to spinal cord injury
88) Pulmonary heart disease, chronic
89) Small airway obstruction
90) Induction of labor
91) Malposition of the fetus
92) Renal colic
93) Cholelithiasis
94) Labor pain
95) Urolithiasis
96) Whooping cough (pertussis)
97) Chloasma
98) Choroidopathy, central serous
99) Color blindness
100) Deafness
Apart from acupuncture, physiotherapy, chest therapy, occupational therapy, Chinese foot therapy, acupressure, tholiau, psychotherapy, ozone therapy, CVFT, and brain stimulator are used to treat various complex pain-related diseases in SUO XI Hospital (Acupuncture). SUO XI Hospital (Acupuncture) is the best pain and paralysis hospital in Bangladesh. They always by your side for your healthcare and emergency needs.
0 notes
Link
Buerger's Disease: Managing, and Living Well Buerger's Disease, also known as Thromboangiitis Obliterans, is a rare and complex vascular condition that primarily affects the small and medium-sized arteries of the arms and legs. While it is relatively uncommon, understanding this disease is crucial, especially for those at risk. In this comprehensive guide, we will explore the causes, symptoms, and risk factors associated with Buerger's Disease. Causes and Risk Factors The precise cause of Buerger's Disease remains elusive, but there are well-established risk factors that increase one's vulnerability to this condition. Among these, smoking is the primary culprit. Tobacco use, particularly in the form of cigarettes or chewing tobacco, significantly raises the likelihood of developing Buerger's Disease. However, there are other contributing factors as well, such as genetics and environmental influences. [caption id="attachment_53882" align="aligncenter" width="489"] Berger's disease[/caption] Buerger's Disease is more common in individuals aged 20 to 40 and is often seen in populations with a history of tobacco use. It is essential to recognize these risk factors and understand how they relate to the disease. Signs and Symptoms Early detection of Buerger's Disease is vital for effective management and preventing complications. This disease typically manifests with distinct symptoms, including pain, particularly in the hands and feet. Pain can be severe and may occur even at rest or with minimal exertion. Other common symptoms include inflammation of the affected limbs, skin ulcers, and gangrene. Diagnosis and Medical Evaluation Diagnosing Buerger's Disease involves a multi-faceted approach that combines clinical assessments, diagnostic tests, and imaging. The healthcare team plays a crucial role in determining the presence and extent of the disease. Here's what you can expect during the diagnostic process: Clinical Assessments During your medical evaluation, your healthcare provider will conduct a thorough examination, focusing on the affected limbs. They will assess the severity of pain, any skin changes, and the presence of arterial pulses. The absence of pulses in the affected limbs is a characteristic feature of Buerger's Disease. Diagnostic Tests and Imaging Various diagnostic tests can aid in confirming the diagnosis of Buerger's Disease. These may include: Doppler Ultrasound: This non-invasive test uses sound waves to measure blood flow in the affected arteries, helping identify blockages or constrictions. Angiography: A contrast dye is injected into the arteries, and X-ray imaging is used to visualize blood flow, revealing any narrowing or blockages. Blood Tests: These may include tests to rule out other conditions that could mimic Buerger's Disease, such as autoimmune disorders. Ankle-Brachial Index (ABI): This test measures the blood pressure in your ankles and compares it to the blood pressure in your arms, helping to assess blood flow in the limbs. Living with Buerger's Disease Receiving a diagnosis of Buerger's Disease can be challenging, but it's essential to understand that effective management strategies exist. Living well with this condition involves a combination of lifestyle modifications, pain management techniques, and emotional support. Lifestyle Modifications and Smoking Cessation Quit Smoking: If you are a smoker, the most crucial step you can take is quitting smoking immediately. Smoking cessation is the cornerstone of managing Buerger's Disease. It can slow the progression of the disease and reduce the risk of complications. Healthy Lifestyle Choices: Adopting a heart-healthy lifestyle is essential. This includes maintaining a balanced diet, engaging in regular physical activity, and managing stress. These measures can improve overall circulation and reduce the strain on your arteries. Avoiding Cold Temperatures: Exposure to cold temperatures can exacerbate symptoms. Dress warmly, especially during colder months, and keep extremities well-covered to maintain adequate circulation. Pain Management and Improving Circulation Managing pain associated with Buerger's Disease is a critical aspect of living well. Your healthcare team may recommend: Medications: Depending on the severity of your symptoms, your doctor may prescribe medications to help relieve pain and improve blood flow. Wound Care: If you develop skin ulcers or gangrene, proper wound care is essential to prevent infection and promote healing. Physical Therapy: Engaging in physical therapy exercises can help maintain muscle strength and improve circulation in the affected limbs. Emotional and Psychological Support Living with a chronic condition like Buerger's Disease can be emotionally challenging. Seek emotional support from friends, family, or support groups. Talking to a mental health professional can also be beneficial in coping with the emotional aspects of managing a chronic illness. Treatment Options for Buerger's Disease The management of Buerger's Disease typically involves a combination of treatments aimed at relieving symptoms, improving circulation, and preventing complications. Your healthcare team will tailor your treatment plan to your specific needs. Here are some common treatment options: Medications Vasodilators: These medications help relax and widen blood vessels, improving blood flow to the affected limbs. Examples include calcium channel blockers. Pain Management: Over-the-counter pain relievers or prescription medications may be prescribed to alleviate pain associated with Buerger's Disease. Antiplatelet Drugs: These medications reduce the risk of blood clots and improve blood flow. Surgical Interventions Sympathectomy: In some cases, surgical sympathectomy may be recommended. This procedure involves cutting or clamping specific nerves to improve blood flow to the affected limbs. Bypass Surgery: If severe blockages are present, bypass surgery can reroute blood flow around the blocked arteries, often using veins from other parts of the body. Amputation: In advanced cases where tissue death (gangrene) is extensive and uncontrollable, amputation of the affected limb may be necessary to prevent further complications. Emerging Therapies and Research Advancements Medical research continues to explore innovative therapies and treatments for Buerger's Disease. Clinical trials and studies aim to uncover new approaches to managing the disease, which may include stem cell therapies and targeted drug treatments. It's essential to work closely with your healthcare team to determine the most suitable treatment plan for your condition. Regular follow-up appointments and ongoing monitoring are crucial to track progress and make necessary adjustments. Prevention and Risk Reduction While Buerger's Disease can be challenging to prevent entirely, there are proactive steps you can take to reduce your risk and manage the condition effectively: Strategies for Quitting Smoking Seek Support: Enlist the help of healthcare professionals, support groups, or smoking cessation programs to increase your chances of successfully quitting. Explore Nicotine Replacement Therapies: Nicotine replacement products like patches, gum, or lozenges can help alleviate withdrawal symptoms. Identify Triggers: Recognize situations or emotions that trigger the urge to smoke, and develop alternative coping strategies. Lifestyle Changes to Lower Risk Regular Exercise: Engage in regular physical activity to promote healthy blood circulation. Consult your healthcare provider for exercise recommendations. Balanced Diet: Adopt a diet rich in fruits, vegetables, whole grains, and lean proteins. Limiting saturated fats and sodium can support overall heart health. Stress Management: Practice stress-reducing techniques such as meditation, deep breathing exercises, or yoga to help maintain a calm and balanced state of mind. Importance of Regular Check-ups Routine check-ups with your healthcare provider are essential for monitoring your overall health and identifying any early signs of Buerger's Disease or related conditions. Regular assessments of blood pressure, cholesterol levels, and circulation can aid in early detection and intervention. Frequently Asked Questions (FAQs) about Buerger's Disease Q: What is Buerger's Disease? A: Buerger's Disease, also known as Thromboangiitis Obliterans, is a rare vascular condition that primarily affects the arteries in the arms and legs. It's characterized by inflammation and blockages in these blood vessels. Q: Who is at risk of developing Buerger's Disease? A: The primary risk factor for Buerger's Disease is smoking. However, it can also be influenced by genetic factors and is more common in individuals aged 20 to 40 who use tobacco products. Q: What are the early symptoms of Buerger's Disease? A: Early symptoms may include pain, especially in the hands and feet, skin inflammation, and skin ulcers. These symptoms often occur or worsen with tobacco use. Q: How is Buerger's Disease diagnosed? A: Diagnosis involves clinical assessments, such as examining affected limbs and assessing arterial pulses, along with diagnostic tests like Doppler ultrasound and angiography. Q: Is there a cure for Buerger's Disease? A: While there is no cure for Buerger's Disease, effective management strategies can help control symptoms and prevent complications. Quitting smoking is a crucial step in managing the condition. Q: What are the treatment options for Buerger's Disease? A: Treatment may include medications to improve blood flow and manage pain, surgical interventions to bypass blocked arteries, and, in severe cases, amputation. Q: Can lifestyle changes help manage Buerger's Disease? A: Yes, lifestyle modifications such as quitting smoking, maintaining a healthy diet, and staying physically active can significantly improve the management of Buerger's Disease. Q: What should I do if I suspect I have Buerger's Disease? A: If you experience symptoms like persistent pain, skin ulcers, or color changes in your extremities, seek immediate medical attention. Early diagnosis and treatment are crucial. Q: Can Buerger's Disease be prevented? A: While it may not be entirely preventable, quitting smoking and adopting a healthy lifestyle can significantly reduce the risk of developing Alzheimer's Disease. Q: Are there support resources for individuals with Buerger's Disease? A: Yes, support groups, patient communities, and healthcare professionals can provide valuable support and guidance for individuals living with Buerger's Disease. Conclusion In conclusion, Buerger's Disease, though challenging, is a condition that can be effectively managed and controlled with the right knowledge and proactive approach. By taking steps to quit smoking, embracing a healthy lifestyle, seeking appropriate medical care, and staying informed about the latest advancements i
#Buergers_Disease_overview#Buergers_Disease_symptoms#Buergers_Disease_symptoms_and_treatment#Managing_vascular_conditions#Smoking_related_artery_disorder#Thromboangiitis_Obliterans#Thromboangiitis_Obliterans_alternative_name#Understanding_Thromboangiitis_Obliterans#Vascular_condition
0 notes
Text
Arterial Diseases Important Question And Answers
#GeneralSurgery#SurgicalSkills#SurgicalPrecision#SurgicalAdvancements#bdsnotescom#ArterialDiseasesImportantQuestionAndAnswers
0 notes
Text
DIFFERENCES BETEWEEN VENOUS AND ARTERIAL VENOUS
To give continuity to the previous topic, we thought it prudent to place the differences between venous and arterial ulcers, since the treatment is completely different, along with the history collected in the clinical history, physical examination, and other complementary examinations, but on some occasions it is not easy to establish the origin, since a high percentage of venous ulcers have an arterial component. Next we leave you a table where the main differences between them are exposed.
Differences between venous and arterial ulcer To give continuity to the previous topic, we thought it prudent to place the differences between venous and arterial ulcers, since the treatment is completely different, along with the history collected in the clinical history, physical examination, and other complementary examinations, but on some occasions it is not easy to establish the origin, since a high percentage of venous ulcers have an arterial component. Next we leave you a table where the main differences between them are exposed. image
. DEFINITION OF VASCULAR ULCER It is a lesion with the deterioration of the solution of continuity with loss of substance, epithelium and/or conjunctiva produced by a pathological process of vascular origin, have a chronic evolution and little or no tendency to spontaneous healing. They are painful lesions that hinder mobility and alter one's own body image. The pain is frequent and can be severe or continuous and disabling. They have a chronic and relapsing character with a high rate of recurrence.
ETIOLOGY The ulcer originates from a deterioration of the cutaneous microcirculation. According to its etiology, it is classified as:
•: arteriosclerosis obliterans 90%, vasculitis, thromboangiitis obliterans, Raynand's disease, discreet smoking, dyslipidemia, arterial hypertension
. VENOUS ULCERS: skin and vascular alterations according to the degree of venous insufficiency. Grade I It is the initial phase. There are superficial varicose veins that affect the plantar arch, malleolar areas, and ankles. He The patient reports a feeling of heaviness and pain at the end of the day
. Grade II It may appear:
Edema purpuri
hyperpigmentation
Increase in thickness, being able to reach elephantiasis in the extremity Area of whitish skin located in the peri-malleolar area Eczema of ecstasy, which causes intense itching. It is frequent that small erosions by scratching can turn into ulcers.
Thrombophlebitis Bleeding that can be important due to rupture of very dilated veins Grade III In addition to the above symptoms, open ulcers appear, with a sudden onset (trauma direct, rupture of a varicose vein, infectious agents on the skin...) or insidious (persistent scab, profuse desquamation, slight abrasions…) ulcerative scar
0 notes
Photo
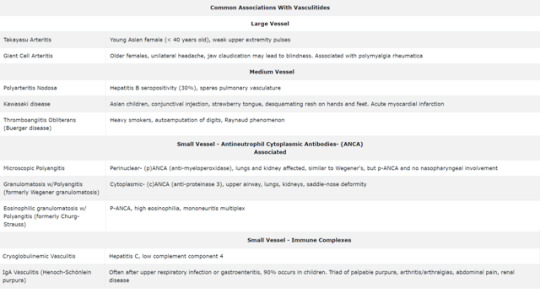
#vasculitis#vasculitides#takayasu arteritis#takayasu#giant cell arteritis#PMR#PAN#Kawasaki#Kawasaki disease#Thromboangiitis Obliterans#Buerger disease#Raynaud phenomenon#MPA#GPA#Churg strauss#Eosinophilic granulomatosis with Polyangitis#PANCA#CANCA#Henoch-Schönlein purpura#Henoch Schonlein purpura#HSP
2 notes
·
View notes
Text
What Is Thromboangitis Obliterans
Thromboangitis obliterans with the name of the reporter, or Buerger's disease in the disease named (read German), occlusive thrombus vasculitis (thromboangiitis obliterans, short It is also called TAO). Limb peripheral blood tubes in diseases causing the occlusion, resulting in limb or finger toes of ischemia (low oxygen conditions of tissue caused to blood is not sufficiently supplied) find out here symptoms is occurs sick.

What Are The Symptoms Of This Diseasehow Do You Diagnose This Disease
When the arteries of the extremities are occluded, symptoms such as coldness and numbness, intermittent claudication, resting pain, and ulcer / necrosis appear as ischemic symptoms. Naturally, the pulsation of the occluded artery becomes palpable . Ankle blood pressure measurement using a Doppler blood flow meter and ankle / upper limb blood pressure ratio (ABI) are useful for understanding the degree of ischemia. Although it is possible to make a rough diagnosis based on clinical symptoms and physical findings, vascular imaging is absolutely necessary for definitive diagnosis, confirmation of obstruction site and occlusion pattern, and differentiation from arteriosclerosis obliterans. There are no characteristic findings on the blood test.
The arteries in the patient's limbs are occluded, resulting in ischemic symptoms (symptoms of hypoxia caused by the lack of blood supply). Patients' subjective symptoms include coldness, numbness, and paleness of the finger toes, intermittent claudication (walking a long distance causes pain in the legs and makes walking difficult, and after a break, the pain subsides and walking is possible). It can form pain (resting pain) and even ulcers (deficiency of the skin), eventually leading to necrosis . These symptoms may occur in sequence, and ulcers may form on the fingertips from the beginning. The veins in the limbs can also become inflamed, causing redness and pain along the veins ( migratory phlebitis ).
What Are The Treatments For This Disease
The basis of treatment is smoking cessation. Smoking is closely linked to the onset and exacerbation of the disease, and continued smoking is ineffective for any treatment. In addition, it is important to keep your limbs clean and protected, keep warm in cold weather, prevent rubbing of your shoes and avoid scratches.
Depending on the symptoms, drugs such as antiplatelet drugs, blood flow improvers, and anticoagulants are first given to improve blood circulation and prevent the development of blood clots. The most effective treatment for ischemic symptoms is revascularization surgery (bypass surgery, etc.), which has not been improved by the basic treatments such as quitting and drug therapy mentioned above, and especially severe ischemic symptoms. It is given to patients with (resting pain, ulcer or necrosis). However, unlike vascular obstruction due to arteriosclerosis, the disease is more severe in the periphery, so revascularization surgery is often inadequate. In such cases, treatments such as sympathetic ganglion block and sympathetic ganglion resection surgery to increase skin blood flow and hyperbaric oxygen therapy to supply a high concentration of oxygen to the affected area are also performed.
New therapies that regenerate blood vessels, such as gene therapy and cell transplantation therapy, are beginning to be used.
If necrosis still progresses and various treatments are ineffective, amputation of the toes and limbs may occur.
How Does This Disease Go
In the olden days, many patients had to amputate their limbs as idiopathic necrosis , but recently, if smoking cessation is strictly adhered to and various treatments are given, the number of cases of amputation of limbs is decreasing. I will. Early diagnosis and appropriate treatment can prevent the disease from becoming more severe. Many patients who do not show recurrence or deterioration have returned to work or daily life before the onset of symptoms.
Testing And Diagnosis
Thromboangiitis obliterans test method for the disease called thromboangiitis obliterans is to estimate the obstructed part occurring in the artery by the doctor touching the pulse of the limbs and measuring the blood pressure. I can do it. For a definitive diagnosis of this obstructed part, angiography is a method in which a contrast medium is placed in a blood vessel with a catheter and an X-ray is taken. This makes it possible to accurately diagnose the part of the blood vessel that is occluding.
Treatment Method For Thromboangiitis Obliterans
Thromboangiitis obliterans is a disease in which inflammation of the peripheral arterial intima of the lower limbs causes arterial obstruction, resulting in impaired blood flow. It is also called Buerger's disease. Although the cause is unknown, smoking is deeply involved in the onset. It is important to adhere to smoking cessation as a cure for this disease. Keep your limbs clean and warm in cold weather. Then, drug treatment such as vasodilators and antiplatelet drugs that promote blood circulation and prevent blood clots is performed. In severe cases, revascularization is performed by bypass surgery.
1 note
·
View note
Photo

On This Day In History . 23 September 1951 . King George VI had surgery to have his left lung removed . . ◼ The stress of the second world war had taken its toll on the King's health, exacerbated by his heavy smoking & subsequent development of lung cancer among other ailments, including arteriosclerosis & thromboangiitis obliterans. A planned tour of Australia & New Zealand was postponed after the King suffered an arterial blockage in his right leg, which threatened the loss of the leg & was treated with a right lumbar sympathectomy in March 1949. . ◼ His elder daughter Elizabeth, the heir presumptive, took on more royal duties as her father's health deteriorated. The delayed tour was re-organised, with Elizabeth & her husband, the Duke of Edinburgh, taking the place of the King & Queen. . ◼ The King was well enough to open the Festival of Britain in May 1951, but on 23 September 1951, his left lung was removed by Clement Price Thomas after a malignant tumour was found. . ◼ In October 1951, Princess Elizabeth & the Duke of Edinburgh went on a month-long tour of Canada; the trip had been delayed for a week due to the King's illness. At the State Opening of Parliament in November, the King's speech from the throne was read for him by the Lord Chancellor, Lord Simonds. His Christmas broadcast of 1951 was recorded in sections, & then edited together. . ◼ On 31 January 1952, despite advice from those close to him, the King went to London Airport to see off Princess Elizabeth, who was going on her tour of Australia via Kenya. On the morning of 6 February, George VI was found dead in bed at Sandringham House in Norfolk. He had died from a coronary thrombosis in his sleep at the age of 56. His daughter Elizabeth flew back to Britain from Kenya as Queen Elizabeth II. . . . #thisdayinhistory #d23sep #HisMajesty #GeorgeVI #KingGeorgeVI #HouseofWindsor #RoyalFamily #BritishMonarchy #TheBritishMonarchy #History #GodSaveTheKing #History #OnThisDay #RoyalHistory #HistoryFacts #Monarch #monarchy #BuckinghamPalace #Westminster #London #Royalty #royalfamily #theking #emperor #British #Britain (at Buckingham Palace) https://www.instagram.com/p/B2xHdDJAAwX/?igshid=1jnfxnphwp8nl
#thisdayinhistory#d23sep#hismajesty#georgevi#kinggeorgevi#houseofwindsor#royalfamily#britishmonarchy#thebritishmonarchy#history#godsavetheking#onthisday#royalhistory#historyfacts#monarch#monarchy#buckinghampalace#westminster#london#royalty#theking#emperor#british#britain
30 notes
·
View notes
Text
Biography:
Rodrigo Duterte, also called Digong, (born March 28, 1945, Maasin, Philippines), Filipino politician who was elected president of the Philippines in 2016. Duterte’s father served as governor of the province of Davao, and his mother was a community activist who had a prominent role in the “people power” movement that deposed the authoritarian president Ferdinand Marcos and restored democratic rule to the Philippines. Duterte earned a political science degree (1968) from Lyceum of the Philippines University in Manila and a law degree (1972) from San Beda College. In 1977 he joined the Davao City prosecutor’s office, where he remained until he was appointed (1986) vice mayor of that city. Duterte was elected mayor in 1988, and he was reelected to that post twice over the subsequent decade. Because of term-limit restrictions, he was barred from seeking reelection in 1998, but he successfully ran for a seat representing Davao in the Philippines House of Representatives. Upon the completion of that term in 2001, he returned to Davao City and was once more elected mayor. Because the term-limit restriction again came into force in 2010, he was elected vice mayor, and his daughter Sara served as mayor. In 2013 Duterte returned to the mayor’s office, this time with his son Paolo (“Pulong”) serving as vice mayor. During his more than two decades as mayor of Davao City, the controversial politician transformed the city from a haven of lawlessness into one of the safest areas in Southeast Asia. Duterte’s harsh crime-fighting tactics earned him the nicknames “the Punisher” and “Duterte Harry” (in reference to the film character Dirty Harry, the ruthlessly effective police inspector portrayed by actor Clint Eastwood), but critics such as Amnesty International and Human Rights Watch claimed that Duterte was responsible for more than 1,000 extrajudicial killings. Rather than denying such allegations, he embraced them. The death squads that had carried out the killings operated with an impunity that implied official sanction, and Duterte openly praised both their methods and their apparent results. In that way he cultivated the image of a coarse pistol-toting vigilante in the months leading up to the presidential election. His antiestablishment message took hold among a Filipino public weary of official corruption, and his brash over-the-top rhetoric led to comparisons with U.S. Republican presidential hopeful Donald Trump. Duterte’s position on the contested Spratly Islands—arguably the Philippines’ most-pressing foreign policy issue—caused consternation among the country’s allies. He wavered unpredictably between a negotiated settlement with China and a claim that he would ride a jet ski to one of the disputed islands and plant a Filipino flag on it. On May 9 nearly 80 percent of eligible voters turned out for the election, and Duterte captured nearly as many votes as his two closest competitors combined. Within days of his landslide victory, Duterte vowed to reintroduce the death penalty—abolished in the Philippines in 2006—in concert with his promise to “fatten all the fish” in Manila Bay with the bodies of criminals. In a televised address in June, he endorsed vigilantism by members of the public, stating that he would personally reward anyone who shot and killed a drug dealer. On June 30, 2016, Duterte was inaugurated as president of the Philippines. In his first six months in office, more than 6,000 people were killed in Duterte’s “war on drugs.” A fraction of those deaths occurred during police operations. The overwhelming majority were extrajudicial killings by death squads. Metro Manila’s funeral parlours were strained beyond capacity, and hundreds of unidentified or unclaimed bodies were interred in mass burials. Human rights organizations and Roman Catholic officials spoke out against the bloodshed, but Duterte responded by accusing the church of corruption and the sexual abuse of children. When Western governments expressed concern over the rampant vigilantism, Duterte said that the West could offer the Philippines only “double talk,” and he sought to strengthen ties with Russia and China. The United States had suspended the sale of 26,000 assault rifles to the Philippines as a result of the human rights abuses, and in May 2017 Duterte met with Russian Pres. Vladimir Putin to discuss the prospect of an arms deal. While Duterte was in Moscow, a series of deadly clashes erupted in Marawi between Filipino troops and Islamist fighters linked to the Islamic State in Iraq and the Levant (ISIL; also called ISIS). Duterte cut short his trip and declared a state of martial law covering the entire island of Mindanao.
Duterte’s war on drugs is one of his most important works that he undertook as the Mayor of Davao City. Although many accuse him of human rights violation and extra judicial killings he was able to eradicate the menace and make the city free from drugs Using city funds, he also had a drug rehabilitation and treatment center built at the cost of ₱12-million. It provides 24-hour services. In 2003, he floated a plan that provided a monthly allowance of ₱2,000 to drug addicts who personally approached him and promised to give up the habit. As a Mayor, he also started a war on crime. During his tenure the crime rate went down drastically. While in 1985, the rate was triple digit figure per 1000 people, from 1999 to 2005, it became 8.0 cases 1000. Because of his ruthless eradication of criminals he has been dubbed as ‘The Punisher’ by Times Magazine.
Duterte was once a heavy smoker, but later gave it up due to health reason. But because of it, he now suffers from Thromboangiitis obliterans, a disease involving recurring progressive inflammation and thrombosis of blood vessels in the hands and feet.
1 note
·
View note
Text


Brand Name: Brimonidine Tartrate
Generic Available
Dosage Forms:
Ophthalmic Solution: 0.1% brimonidine tartrate with Purite 0.005% as a preservative.
Ophthalmic Solution: 0.15% brimonidine tartrate with Purite 0.005% as a preservative.
FDA Indications/Dosages:
For the reduction of elevated intraocular pressure in patients with open-angle glaucoma or ocular hypertension: The recommended dose is one drop in the affected eye(s) three time daily, approximately 8 hours apart. The IOP lowering effects may diminish over time in some patients. This loss of effects appears with a variable time of onset in each patient and should be closely monitored.
Monitor: IOP
Pharmacology/Pharmacokinetics: Brimonidine is a relatively selective alpha-2-adrenergic agonist which lowers elevated intraocular pressure. Its mechanism of action is due to a reduction of aqueous humor production and increased uveoscleral outflow. Elevated intraocular pressure increases the patient’s risk of optic nerve damage and visual field loss. Peak ocular hypotensive effects are reached in 2 hours post dose. Systemic half-life is approximately 3 hours. Very small amounts are absorbed after topical use in the eye and present minimal cardiovascular and pulmonary effects.
Drug Interactions: Tricyclic antidepressants may decrease effectiveness of Alphagen. Additive effects may be seen when used with beta-blockers (oral or ophthalmic). Coadministration with MAO INHIBITORS may elevate blood pressure.
Contraindications/Precaution: Contraindicated in patients using monoamine oxidase inhibitors. Caution should be used in patients with depression, cerebral or coronary insufficiency, Raynaud’s phenomenon, orthostatic hypotension, or thromboangiitis obliterans. Pregnancy Category B.
Adverse Effects: Allergic conjunctivitis, conjunctival hyperemia, and eye pruritus (10-20%) are the most common adverse effects. Less frequent effects include burning sensation, conjunctival folliculosis, hypertension, dry mouth, and visual disturbances (5-9%).
Patient Consultation:
To instill: Lie down or tilt head backward and look up. Holding the dropper above the eye, drop solution inside lower lid, making sure the dropper does not come in contact with the eye or fingers. Then release lid, keeping the eye open for at least 30 seconds, and apply pressure to the inside corner of the eye for at least one minute.
Wait at lease 5 minutes before instilling other ophthalmic preparations.
Avoid squinting or closing of eyes tightly after instilling drops.
Store in a cool, dry place away from sunlight and children.
If a dose is missed instill it as soon as possible. If it is closer to the time of your next dose than the dose you missed, skip the missed dose and return to your dosing schedule.
Contact a physician if the above side effects are severe or persistent.
0 notes
Text
Varicose Veins Treatment Old Bad Leg Patch
New Post has been published on https://www.thinkoutsidein.com/product/varicose-veins-treatment-old-bad-leg-patch/
Varicose Veins Treatment Old Bad Leg Patch

This product has some feqatures:
speedy activity straightforwardly in issue zones;
in assembling utilizing cutting edge innovation;
wellbeing and hypoallergenic;
in excess of 10 therapeutic herbs in the sythesis;
impact inside 48 hours, that is, dependable impact.
This product has Cinnamon, dangshen, caulis spatholobi, burdock, honeysuckle. It help the swelling. torment. knob that brought about by vasculitis and Varicose veins.
The counteractive action of these ailments for individuals whose calling or way of life makes them powerless to the sickness (standing and inactive nature of work);
torment, consuming, tingling, and it stuck in the veins of the appendages
The most effective method to utilize:
legitimately on the influenced region to a perfect and dry surface skin.
2 days transformed one mortar. It requires a consistent course of 10 days.
In the wake of expelling the mortar wash the skin with warm water or wipe clean with a soggy material. It is appropriate for the individuals who experiencing vasculitis and varicose veins illness.
Varicocele thromboangiitis obliterans, arteriosclerotic impediment, Raynaud’s ailment, Ecthyma legs and so on additionally the manifestation brought about by above sickness. like the appendage fatigue(aching torment, drop, swelling, Powerless ) , lower appendage swelling, terrified of cold, skin tingling, Festering rot.
How to use:
Outer utilize as it were.
If it’s not too much trouble ensure the influence region is cleaning and dry.
Warning:
Pregnant lady don’t to utilize it.
Skin hypersensitivity or wound should utilize it with alert
0 notes
Text
بیماری بورگر و راه درمان آن
بیماری بورگر و راه درمان آن
بیماری بورگر و راه درمان آن
بیماری بورگر یا ترومبوآنژئیت انسدادی (به انگلیسی: Thromboangiitis Obliterans) یا (به انگلیسی: Buerger Disease) نوعی اختلال انسدادی غیر آترواسکلروتیک سرخرگ ها و سیاهرگ های کوچک تا متوسط اندامهای فوقانی و تحتانی است.
یک بیماری است که باعث انسداد در عروق پا و دست شما است. عروق خونی ملتهب میشوند، که باعث کاهش جریان خون، لخته شدن خون بیشتر رگ های خونی را مسدود می کند. این…
View On WordPress
#بیماری بورگر و راه درمان آن#تصاویر بیماری برگر#داروی بیماری برگر#درمان بیماری برگر با طب سنتی#درمان بیماری بورگر#درمان زخم برگر#درمان گیاهی بیماری برگر#راههای درمان بیماری برگر#عکس بیماری برگر#علائم بیماری برگر#علائم بیماری بورگر
0 notes
Text
USG Scan Both Limbs Arterial Doppler Test
Doppler ultrasound check is done on both the arms and legs regardless of whether the variation from the norm is suspected in one appendage. The checking is done as such that the vascular framework can be analyzed between the two appendages.
The ultrasound check for a blood vessel Doppler strategy utilizes sound waves to make a shading guide of the courses in the legs to recognize skin staining, heel, lower leg, toe or foot ulcers, resting leg agony or narrowing of the vessels that may cause leg torment when strolling. USG Scan Both Limbs Arterial Doppler Test For checking, the pulse readings are taken at various areas by wrapping a circulatory strain sleeve around the calf and afterward around the thigh. A Doppler ultrasound is an agony free and hazard free strategy. The test gives important data with respect to the blood move through significant courses and veins.
Stay away from the utilization of nicotine items like tobacco and cigarette for no less than 2–4 hours before the system. Nicotine utilization may make the veins contract and might be mixed up for an obsessive tightening.
You ought to likewise evacuate all the metal and adornments extras as they may change the filtering comes about.
You are additionally requested to put on something else and wear a doctor’s facility outfit, as per the zone of the body to be checked.
Doppler ultrasound examine is the initial step to care for the conduits and veins. Usually requested on the off chance that you hint at diminished blood stream in the supply routes or veins. It is additionally helpful on the off chance that you demonstrate different side effects of profound vein thrombosis, shallow thrombophlebitis, arteriosclerosis, thromboangiitis obliterans, or vascular tumors in your arms or legs. A Doppler ultrasound additionally helps in deciding the pulse inside the corridors and furthermore demonstrate how much blood is as of now moving through the veins and supply routes.
You will be told to rests on an examination table in a still position.
A water-solvent gel is connected to the skin which coordinates high-recurrence sound waves into the veins being examined.
A radiologist or a sonographer may put circulatory strain sleeves around the thigh, lower leg, and calf. This will help in examination of circulatory strain in various parts of the legs.
Pictures are made as the transducer is squeezed against the skin and sends sound waves to the veins. The veins send back the reverberate and the data is sent to the PC and is handled and recorded.
Charts and pictures will be created which will demonstrate the blood course through corridors and veins.
Rs 1500-Rs 4000
#USG Scan Both Limbs Arterial Doppler Test#USG Scan Both Limbs Arterial Doppler Test cost#USG Scan Limbs Arterial Doppler
0 notes
Photo

On This Day In History . 23 September 1951 . King George VI had surgery to have his left lung removed . . ◼ The stress of the second world war had taken its toll on the King's health, exacerbated by his heavy smoking & subsequent development of lung cancer among other ailments, including arteriosclerosis & thromboangiitis obliterans. A planned tour of Australia & New Zealand was postponed after the King suffered an arterial blockage in his right leg, which threatened the loss of the leg & was treated with a right lumbar sympathectomy in March 1949. . ◼ His elder daughter Elizabeth, the heir presumptive, took on more royal duties as her father's health deteriorated. The delayed tour was re-organised, with Elizabeth & her husband, the Duke of Edinburgh, taking the place of the King & Queen. . ◼ The King was well enough to open the Festival of Britain in May 1951, but on 23 September 1951, his left lung was removed by Clement Price Thomas after a malignant tumour was found. . ◼ In October 1951, Princess Elizabeth & the Duke of Edinburgh went on a month-long tour of Canada; the trip had been delayed for a week due to the King's illness. At the State Opening of Parliament in November, the King's speech from the throne was read for him by the Lord Chancellor, Lord Simonds. His Christmas broadcast of 1951 was recorded in sections, & then edited together. . ◼ On 31 January 1952, despite advice from those close to him, the King went to London Airport to see off Princess Elizabeth, who was going on her tour of Australia via Kenya. On the morning of 6 February, George VI was found dead in bed at Sandringham House in Norfolk. He had died from a coronary thrombosis in his sleep at the age of 56. His daughter Elizabeth flew back to Britain from Kenya as Queen Elizabeth II. . . . #thisdayinhistory #theyear1951 #d23sep #HisMajesty #GeorgeVI #KingGeorgeVI #HouseofWindsor #RoyalFamily #BritishMonarchy #TheBritishMonarchy #GodSaveTheKing #History #thisdayinhistory #theyear1951 #d23sep #HisMajesty #GeorgeVI #KingGeorgeVI #HouseofWindsor #RoyalFamily #BritishMonarchy #TheBritishMonarchy #GodSaveTheKing #History (at London, United Kingdom) https://www.instagram.com/p/BoFgi6ZloZj/?utm_source=ig_tumblr_share&igshid=1l0bmj3f27inq
#thisdayinhistory#theyear1951#d23sep#hismajesty#georgevi#kinggeorgevi#houseofwindsor#royalfamily#britishmonarchy#thebritishmonarchy#godsavetheking#history
0 notes
Photo


Buerger's disease (Thromboangiitis obliterans) was first reported by Felix von Winiwarter in 1879 in Austria. In 1908, first accurate pathological description was given by Leo Buerger at Mount Sinai Hospital in New York City. Buerger called it "presenile spontaneous gangrene" after studying amputations in 11 patients.
King George VI, who was a heavy smoker, was diagnosed with the disease on 12 November 1948. Both legs were affected, the right more seriously than the left. The King's doctors prescribed complete rest and electric treatment to stimulate circulation, but as they were either unaware of the connection between the disease and smoking, they were unable to persuade the King to stop smoking, the disease failed to respond to their treatment. On 12 March 1949, the King underwent a lumbar sympathectomy, performed at Buckingham Palace by Dr. James R. Learmonth. The operation, as such, was successful, but the King was warned that it was a palliative, not a cure, and that there could be no assurance that the disease would not grow worse. From all accounts, the King continued to smoke.
The author and journalist John McBeth describes his experiences of the disease, and treatment for it, in a chapter called 'Year of the Leg' in his book entitled Reporter. Forty Years Covering Asia.
Philippine president Rodrigo Duterte has personally disclosed that he suffers from Buerger’s disease.
0 notes
Photo






Once again, too many notes! Leukocytoclastic vasculitis = small vessel hypersensitivity vasculitis; most frequently seen form in clinical practice. Worse/life-threatening vasculitides = classical polyarteritis nodosa (PAN), Allergic granulomatosus of Churg Strauss, or giant cell arteritis. Pathogenic immune complexes formed between antigen and antibodies tend to occur during antigen excess (particularly in slight to moderate antigen excess). When these complexes precipitate into tissue, they fix complement leading to an intense immune reaction. Vasculitis is an inflammatory, destructive process affecting arteries and veins. The definition may be extended to include conditions in which inflammatory cells infiltrate the vessel wall without wall destruction. Leukocytoclastic vasculitis of the hypersensitivity vasculitis type is the most frequently seen form of vasculitis in general clinical practice and is usually the least dangerous to the host. The characteristic cell of vasculitis is the Polymorphonuclear leukocyte (PMN). The vessel wall may show necrosis (PAN) or granuloma formation (Takayasu’s). The signs and symptoms are non-specific and tend to overlap; errors in diagnosis can be made if one relies solely on clinical features. Some generalizations are helpful in diagnosis such as noting that palpable purpura suggests small vessel vasculitis involving vessels in deep papillary dermis; tender nodules are more likely to involve medium muscular arteries. Immune complex formation (Gell and Coombs type III) plays the major role. It is felt that most of the vasculitic syndromes are either caused by or at least associated with the deposition of immune-complexes in blood vessels. This is seen in a type III (Gell and Coombs) type of immune reaction. Vasoactive amines, at least in part, derived from platelets and IgE triggered basophils play a role in increased permeability. The trapping of the IC in the vessel wall and the activation of complement results in products that are chemoattractants to PMNs. These polymorphonuclear leukocytes accumulate at the site of inflammation and release various enzymes and free radicals (particularly collagenase and elastase) that result in damage to the vessel wall. There is thrombosis, occlusion, hemorrhage and ischemic changes resulting in the classical picture of a vasculitis. (Not explained are (1) leukocytes localize to postcapillary venules (2) cytokines that are not chemoattractant that cause inflammation). Specific cell surface proteins called "adhesion molecules” mediate interaction between endothelium and leukocytes and are found on the surface of both of these cells. Classes of these molecules are: i. integrins ii. selectins Iii.members of the immunoglobulin family. Adhesion Molecules: In this model of inflammation, leukocytes "roll" along the wall of the vessel. This "rolling" is mediated by the action of L and P-selectins. Because endothelial adhesion molecules are induced by cytokines at sites of inflammation, the slowing of the leukocytes mediated by the selectins permits tighter binding between the integrins of the leukocytes and the endothelial adhesion molecules (i.e.-selectin, ICAM-1, a nd VCAM-1). This step is crucial for the migration of leukocytes between endothelial cells and the attraction of mononuclear cells. Clearly, the endothelium is not inactive, but its activation plays a major part in vasculitis. An antibody in circulation called "anti-neutrophil cytoplasmic antibody” (ANCA) has been shown to be involved in the pathogenesis of some vasculitis such as Wegner's syndrome (particularly the c-ANCA). The bottom line is inflammation! It is within this group that we find the original classic polyarteritis nodosa (PAN), and in this group the greatest degree of confusion in classification. It is not because of the differences in basic pathophysiology, but more in the location of the pathology and the clinical manifestations presented. The earliest signs of PAN may be tachycardia, weight loss, fever, and pain, which appear to be related to a viscera and/or the musculoskeletal system. Thus one may be presented with a case that appears as fever of unknown origin (FUO). Specific signs and symptoms may relate to the viscera involved, glomerulonephritis, etc. depending upon the organ involved. The picture may resemble many diseases, particularly the so-called collagen vascular diseases or rheumatoid diseases as exemplified by systemic lupus erythematosus with renal involvement. 3/10 criteria needed to diagnose PAN. Allergic history is uncommon. Eosinophilia, eosinophilic tissue infiltration, and granuloma are not characteristic of PAN. Allergic Granulomatosis (Churg--Strauss Syndrome) It is a systemic necrotizing vasculitis and although the basic presentation, organs involved, and clinical course of this condition and classic PAN are similar, there are certain distinctive features of the Churg-Strauss syndrome as noted below. It is characterized by allergic rhinitis, asthma, and the development of a purpuric rash frequently associated with blood clots of the lower extremity. Late cardiac manifestations are often present. The very high eosinophil count is characteristic. “Leukocytoclastic vasculitis” In clinical practices it is by far the most frequently seen form of vasculitis. It often appears as “Serum Sickness” with the majority due to drugs. It should be born in mind that while it is most common to see this disease manifested as a small vessel cutaneous vasculitis with resultant palpable purpura as in leukocytoclastic vasculitis, any organ system may be involved. Cryoglobulinemic vasculitis is usually due to hepatitis C virus. Henoch-Schönlein purpura is associated strongly with IgA deposition in blood vessels. Hypocomplementemic urticarial vasculitis has features that overlaps with SLE. Although it is the skin lesions that may bring the patient to the physician but the astute physician must bear in mind the possibility of other organ involvement. Leukocytoclastic vasculitis: this usually involves the postcapillary venules and arterioles infiltration of PMNS with leukocytoclasis. (presence of nuclear debris), fibrinoid necrosis, and extravasation of erythrocytes. It is immune complex mediated usually traceable to a precipitating antigen, most often a drug or chemical (e.g. sulfa), or a microorganism (beta-hemolytic streptococcus), or an endogenous antigen (tumor or serum protein). The pathognomonic lesions (although lesions can be at any stage) are a palpable, sharply circumscribed area of purpura which is detected on physical examination altough the definitive diagnosis is made by skin biopsy. Serum sickness = this is not clinically an acute anaphylactic (type I) reaction. There is a vasculitis, due to deposition of immune complexes. The immunology is that of an immune complex formation with antibody combining with antigen until all the antigen is bound. These complexes can be identified by fluorescent techniques, and appear to initiate reactions in the arterial walls. This is not a type I (Gell & Coombs) but a type III reaction! Henoch-Schonlein purpura = a form of hypersensitivity vasculitis involving arterioles where IgA antibody is found in the immune complexes. Occurs in the young and most often in the spring of the year with abdominal pain and at times bleeding. Biopsy of the lesions reveals the typical hypersensitivity leukocytoclastic vasculitis with PMNs dominating the picture. Microscopic Polyangiitis ("microscopic polyarteritis") This is a systemic necrotizing vasculitis that involves small vessels (arterioles, capillaries,and venules). Average age is about 50 with men affected more than women. Manifestations include: glomerulonephritis, pulmonary hemorrhage or infiltration, musculoskeletal pains, purpura, peripheral neuropathy and abdominal pain. Wegner’s granulomatosus (WG), microscopic polyangiitis (MPA), or Granulomatosus with polyangiitis has antineutrophil cytoplasmic antibodies (ANCA) within the serum. These are termed the ANCA-assiociated vasculitidies (AAV). s. The c-ANCA form is the most common ANCA in Wegner’s, granulomatosus. Patients often present with upper airway (nose and sinus), lung and renal (glomerulonephritis) involvement. Destructive changes of the upper airways are common. Diagnosis rests upon the demonstration of evidence of granulomatous inflammation of the respiratory tract and a vasculitis of small and medium vessels. Giant cell arteritis (GCA) can be separated into Temporal arteritis and Takayasu’s arteritis. These are the prototypes of large vessel arteritis. Takayasu’s arteritis tends to involve the aortic arch and its branches while Temporal arteritis usually involves the branches of the carotid artery such as the Temporal artery. GCA arteritis involves those primarily 50years of age and older and is often associated with polymyalgia rheumatica. Both Temporal arteritis and Takayasu’s arteritis are associated with granulomatous inflammation within the blood vessels and have clinical symptoms of vascular inflammation and vascular insufficiency. Temporal arteritis - a patient shall be said to have temporal arteritis if at least three of these five criteria are present On a clinical basis, headache in the elderly, (particularly in women, and certainly associated with a rapid ESR) should be a “red flag” for the diagnosis of Temporal arteritis The association with polymyalgia rheumatica is strong. THROMBOANGIITIS OBLITERANS (BUERGER'S DISEASE) An inflammatory occlusive peripheral vascular disease involving arteries and veins. Predominately in male between 20-40 years and is seen with heavy smokers, and virtually always seen with thrombosus with PMN infiltration and microabscesses. MUCOCUTANEOUS LYMPH NODE SYNDROME (KAWASAKI'S DISEASE) Characteristics are: A nonsuppurative cervical adenitis which is nonesponsiveness to antibiotics with skin and mucus membrane involvement, Often see a “strawberry tongue”. An acute illness of infants and children usually less than 5 year of age (first limited to Japan) and characterized by conjunctivitis, erythema of the oral cavity, lips and palms, and desquamation or the skin of the fingertips. Usually self limiting, but at times there has been deaths due to coronary arteritis. High dosage of aspirin and intravenous immune globulin (IVIG) are the cornerstones of treatment and are essential to prevent coronary aneurysms. ANCAs are autoantibodies to antigens found in the cytoplasm of neutrophils. There are two subsets: cANCAs and p-ANCAs distinguished by their fluorescence pattern. C-ANCAs show a coarse granular centrally accentuated cytoplasmic pattern and are usually caused by antibodies against proteinase and are most often found in Wegner’s granulomatoses as c-NCAs. These are perinuclear fluorescence pattern with many antigens causing this pattern, but myeloperoxidase (MPO) is the p-ANCA target antigen with the greatest clinical association of the vasculitides. The disease most closely associated with ANCAs is Wegner's granulomatosis with 80-95% of all ANCAs being the c-ANCA form. The sensitivity is related to the severity and activity of the disease at the time of sampling. ANCAs have been found in patients with a variety of rheumatic autoimmune diseases (e.g. RA, Sjogren's syndrome, Polymyositis/dermatomyositis, etc), but these are mostly p-ANCA with c-ANCA pattern being rare. In cases of mild cutaneous hypersensitivity vasculitis treatment may be little more than elimination of the causative agent. In some cases the use of antihistamines, and at times .short term corticosteroids may be used. The dose might well be hydroxyzine 25 mg po (orally) 4 times daily for an adult and where indicated prednisone as 40 mg po in divided doses for 3 to 4 days. Second and third generation antihistamines may be indicated. This is noted in sharp contrast to the severe systemic necrotizing vasculitis such as Wegener's granulomatosis and the PAN group, which require aggressive therapy. The recent use of chronic low dose cytotoxic therapy is common, but usually vasculitis is first treated with the corticosteroids, and where there is treatment failures low dose cytotoxic agents are added. There are certain conditions where the corticosteroids are the treatment of choice; these are same of the self-limiting conditions such as serum sickness, and particularly in temporal arteritis. Doses of 40-60mg/day of prednisone with gradual tapering to maintenance dose have resulted in excellent responses. Comparable results have not been obtained in Takayasu's arteritis. Of note is the need of aspirin and IV immune globulin in Kawasaki’s arteritis.
1 note
·
View note
Text
Buerger's disease
(thromboangiitis obliterans) is a rare disease of the arteries and veins in the arms and legs. In Buerger's disease, your blood vessels become inflamed, swell and can become blocked with blood clots (thrombi). This eventually damages or destroys skin tissues and may lead to infection and
0 notes