#gut brain connection
Explore tagged Tumblr posts
Text

#thanos#gut brain connection#gut bacteria#gut#gut biome#meme#dank memes#memedaddy#memes#stolen memes#funny#lmao#lol
35 notes
·
View notes
Text
Understanding the Gut-Brain Connection for Better Mental Health
Ever noticed how a sudden wave of stress can send your stomach into knots? Or how a happy, relaxed feeling seems to come from deep within your belly? These aren’t just strange coincidences. They’re everyday examples of a fascinating and powerful connection happening inside you: the gut-brain axis. Imagine your gut and your brain are constantly talking to each other, like two best friends on a…
0 notes
Text
Beat the Winter Blues: How Nutrition Can Boost Your Mood Naturally [Seasonal Affective Disorder - SAD]

Understanding Seasonal Affective Disorder
Seasonal Affective Disorder (SAD) is a type of depression that occurs at the same time each year, typically during the fall and winter months when daylight hours are shorter. Although everyone feels a little sluggish when the sun disappears for days on end, SAD goes beyond a simple case of the winter blues. It’s a condition that can significantly impact your mood, energy, and daily life.
What is SAD?
SAD is classified as a subtype of major depressive disorder. Its symptoms mirror those of general depression but are tied specifically to seasonal changes. Common signs of SAD include:
Persistent sadness or low mood.
Fatigue or low energy, even after a full night’s sleep.
Increased cravings for carbohydrates and weight gain.
Loss of interest in activities you typically enjoy.
Difficulty concentrating or making decisions.
Feelings of hopelessness or worthlessness.
For those with SAD, the changing seasons bring more than just a calendar flip—they trigger noticeable changes in brain chemistry and hormone levels, which can disrupt mental and emotional health.
Causes and Risk Factors
The exact cause of SAD isn’t fully understood, but researchers point to several factors that may contribute to its onset:
Lack of SunlightReduced sunlight during fall and winter disrupts your body’s internal clock, or circadian rhythm, which regulates sleep and wakefulness. This disruption can lead to feelings of fatigue and depression.
Serotonin LevelsSunlight exposure helps regulate serotonin, a neurotransmitter that influences mood. Low serotonin levels are linked to feelings of depression and can contribute to the symptoms of SAD.
Melatonin DisruptionWith longer nights and shorter days, your body produces more melatonin, a hormone that regulates sleep. This excess melatonin can make you feel drowsy, lethargic, and less motivated.
Vitamin D DeficiencySunlight is a natural source of vitamin D, which is crucial for mood regulation and brain health. A deficiency in this nutrient during the darker months may exacerbate symptoms of depression.
Who is Most at Risk?
While anyone can experience SAD, certain factors increase the likelihood of developing this condition:
Geography: People living farther from the equator, where daylight hours are significantly reduced in winter, are at a higher risk.
Gender: Women are four times more likely to experience SAD than men, although the symptoms tend to be more severe in men.
Age: Young adults are more likely to develop SAD, although it can occur at any age.
Family History: A family history of depression or other mood disorders may predispose you to SAD.
Existing Mental Health Conditions: People with pre-existing depression or bipolar disorder are more vulnerable to seasonal changes.
How Mood and Brain Function Are Linked to Nutrition
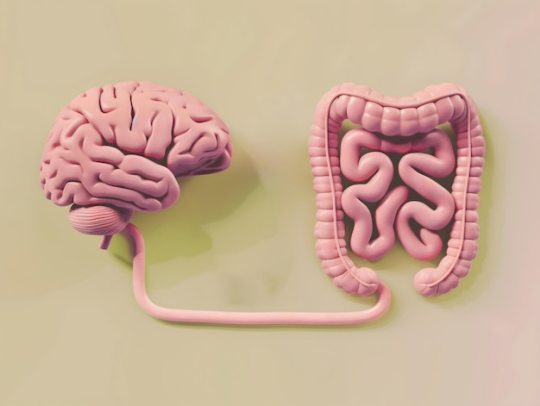
Your diet isn’t just about fueling your body—it directly impacts your brain and emotional health. The connection between your gut and brain, known as the gut-brain axis, plays a significant role in regulating mood and mental clarity. Here’s how nutrition ties into the SAD equation:
Serotonin Production Up to 90% of the body’s serotonin is produced in the gut. By eating foods rich in tryptophan, an amino acid that converts to serotonin, you can support better mood regulation.
Gut Microbiota The trillions of microbes in your gut influence everything from digestion to neurotransmitter production. Consuming probiotics (like yogurt or sauerkraut) and prebiotics (like fiber-rich vegetables) supports these beneficial microbes and can help stabilize your mood.
Essential Nutrients
Omega-3 Fatty Acids: These healthy fats are known to support brain function and reduce inflammation, which is often linked to depression.
Vitamin D: Adequate levels of vitamin D are essential for maintaining a positive mood and may help alleviate SAD symptoms.
B Vitamins: Found in whole grains and leafy greens, these nutrients are critical for energy production and neurological health.
By addressing these nutritional factors, you can help balance brain chemicals and hormones, making your body more resilient to the effects of SAD. The right foods have the power to transform your mood, making the dark days of winter feel a little lighter.
Nutritional Strategies to Alleviate SAD
When it comes to combating the winter blues, food is a powerful ally. By incorporating key nutrients into your diet, you can support brain function, regulate mood, and even improve your body’s ability to handle stress.
Here are six nutrition strategies that can help alleviate Seasonal Affective Disorder (SAD).
1. Incorporate Probiotics
The trillions of microbes living in your gut play a direct role in regulating your mood. By eating probiotic-rich foods or taking supplements, you can nurture these beneficial bacteria, helping to support a balanced gut-brain connection.
Probiotic-Rich Foods
Include these gut-friendly options in your diet:
Yogurt (look for live, active cultures).
Kefir.
Fermented vegetables like sauerkraut, kimchi, and pickles.
Miso and tempeh.
Drinks like kombucha or kvass.
Probiotic Supplements
If you’re not a fan of fermented foods, a high-quality probiotic supplement is an excellent alternative. Choose a product that:
Contains at least 10 billion CFUs (colony-forming units).
Includes strains like Lactobacillus and Bifidobacterium, which are associated with mood benefits.
Is third-party tested for quality and potency.
2. Add Prebiotic Foods
Once probiotics are in your gut, they need fuel to thrive. That’s where prebiotics—non-digestible fibers that nourish good bacteria—come into play. Prebiotic foods can enhance gut health, leading to improved mood regulation.
Prebiotic-Rich Foods
Garlic, onions, and leeks.
Asparagus and artichokes.
Whole grains like oats and barley.
Bananas and apples.
Nuts and seeds.
Incorporating these foods regularly creates a healthy environment for your gut microbes, improving their ability to influence your mental health.
3. Focus on Omega-3 Fatty Acids
Omega-3 fatty acids are known for their anti-inflammatory properties and their ability to support brain health. They help maintain the structure of brain cells and regulate neurotransmitters involved in mood, such as serotonin and dopamine.
Sources of Omega-3s
Fatty fish: Salmon, mackerel, sardines, and trout.
Plant-based options: Chia seeds, flaxseeds, walnuts, and hemp seeds.
Fortified foods: Some eggs, milk, and plant-based beverages are fortified with omega-3s.
Aim to include these foods several times a week for optimal brain support.
4. Boost Vitamin D Levels
One of the most significant nutritional challenges in winter is maintaining adequate levels of vitamin D, also known as the "sunshine vitamin." Vitamin D plays a critical role in serotonin production and mood regulation, and deficiencies are often linked to depressive symptoms.
Ways to Increase Vitamin D
Foods: Fatty fish (like salmon and tuna), egg yolks, and fortified dairy products.
Supplements: Vitamin D3 is generally recommended, as it’s more effective at raising levels in the blood. A healthcare provider can help determine the right dosage for you.
5. Eat Tryptophan-Rich Foods
Tryptophan is an essential amino acid that your body uses to produce serotonin, a neurotransmitter that regulates mood and promotes a sense of well-being. Including tryptophan-rich foods in your meals can support your body’s natural serotonin production.
Best Sources of Tryptophan
Turkey, chicken, and eggs.
Nuts and seeds (especially sunflower and pumpkin seeds).
Soy products like tofu and edamame.
Dairy products like milk and cheese.
Pairing tryptophan-rich foods with complex carbohydrates (like whole grains) can enhance the body’s absorption of this amino acid.
6. Avoid Mood-Sabotaging Foods
Not all foods are created equal when it comes to your mental health. Certain dietary habits can exacerbate mood swings and increase fatigue, making SAD symptoms worse.
Foods to Limit
Sugary Snacks and Drinks: These cause blood sugar spikes and crashes, leading to irritability and fatigue.
Refined Carbohydrates: White bread, pastries, and processed snacks can contribute to mood instability.
Alcohol: It may seem comforting, but alcohol is a depressant that can interfere with sleep and exacerbate low moods.
Focus on whole, minimally processed foods that provide steady energy and nutrients to support your mental health.
Lifestyle and Holistic Approaches
While nutrition plays a powerful role in managing Seasonal Affective Disorder (SAD), pairing it with lifestyle and holistic approaches can create a well-rounded strategy to tackle the winter blues. These techniques address not just the body, but the mind and spirit, helping to boost overall well-being.
1. Embrace Light Therapy
Light therapy is one of the most effective treatments for SAD. By exposing yourself to bright, artificial light that mimics natural sunlight, you can help regulate your circadian rhythm and improve serotonin production.
Tips for Light Therapy
Use a light box with at least 10,000 lux brightness, ideally in the morning for 20–30 minutes.
Position the light box 16–24 inches away from your face without staring directly into it.
Consistency is key—try to use it daily during the darker months.
2. Prioritize Physical Activity
Exercise is a proven mood booster, thanks to its ability to release endorphins—your brain’s natural feel-good chemicals. It also helps regulate stress hormones and improves energy levels.
Exercise Ideas for Winter
Outdoor walks: Take advantage of sunny days for a mood-boosting walk.
Yoga and stretching: These promote mindfulness while enhancing circulation and flexibility.
Dance or cardio: Pick something fun that gets your heart rate up indoors.
Even 30 minutes of moderate activity, five days a week, can make a significant difference in how you feel.
3. Practice Mindfulness and Stress Reduction
Mindfulness helps you stay present and manage the anxiety or sadness that often accompanies SAD. Stress reduction techniques can lower cortisol levels, improving both your mood and energy.
Holistic Stress-Relief Practices
Meditation: Try apps like Calm or Headspace for guided meditations tailored to beginners.
Breathing exercises: Techniques like diaphragmatic breathing help calm the nervous system.
Journaling: Reflecting on positive moments or goals can shift your mindset.
4. Maintain a Consistent Routine
SAD often disrupts sleep and energy patterns, but maintaining a structured daily routine can help stabilize your circadian rhythm.
Tips for Routine Building
Go to bed and wake up at the same time every day, even on weekends.
Schedule meals at consistent times to avoid energy dips.
Incorporate small rituals, like morning stretching or a gratitude practice, to start and end your day positively.
5. Connect with Others
The isolation that winter often brings can worsen feelings of loneliness or depression. Making an effort to connect with others—whether in person or virtually—can lift your spirits and provide much-needed emotional support.
Ways to Stay Connected
Plan regular check-ins with friends or family.
Join online or in-person support groups for SAD or mental health.
Volunteer: Helping others can boost your own sense of purpose and well-being.
6. Consider Professional Support
If SAD symptoms are severe or persist despite lifestyle changes, seeking help from a healthcare professional can make a significant difference.
Options for Professional Help
Therapy: Cognitive Behavioral Therapy (CBT) is particularly effective for SAD.
Medication: Antidepressants or other prescribed treatments may be recommended in some cases.
Nutrition Guidance: A registered dietitian can help fine-tune your diet for mental health.
Recipes to Support Mood During Winter
Winter can often feel like a time of heaviness and hibernation, but the right foods can nourish your body and uplift your spirit. These recipes are not only delicious but also rich in nutrients that support brain health, balance mood, and energize you during the darker months.
Why These Recipes Work
Each recipe incorporates nutrient-dense ingredients designed to support the gut-brain axis and combat wintertime sluggishness. From probiotics in yogurt to omega-3s in salmon and prebiotics in asparagus, these meals and snacks can work together to keep your mood balanced and your energy steady.
Avocado Lime Salmon
Why It Supports Mood
This dish is rich in omega-3 fatty acids, found in salmon, which are essential for brain health and can help reduce inflammation linked to depression. The avocado topping adds heart-healthy monounsaturated fats and potassium, which support energy levels and nerve function. Lime and cilantro provide a burst of fresh flavor and antioxidants.
Ingredients
1½ lbs salmon, skinless
1 clove garlic, minced
1 tsp olive oil
Salt and pepper, to taste
2 tsp paprika
1 avocado, chopped
1 red onion, chopped
4 tbsp fresh cilantro, chopped
4 tbsp olive oil
4 tbsp lime juice
Directions
Preheat oven to 400˚F.
On a baking sheet, season salmon with garlic, olive oil, salt, pepper, and paprika.
Bake for 10–12 minutes.
In a small bowl, mix avocado, red onion, cilantro, olive oil, and lime juice until incorporated.
Be careful not to overmix to preserve the avocado’s texture.
Spoon the avocado topping over the baked salmon and serve.
Frozen Berry Yogurt Bark
Why It Supports Mood
This simple snack features Greek yogurt, a source of probiotics that support gut health and the gut-brain connection, and berries, which are loaded with antioxidants and vitamin C to combat oxidative stress. Pecans add crunch and healthy fats, promoting stable energy and focus.
Ingredients
2 cups full-fat Greek yogurt
1 tbsp maple syrup
Salt, to taste
6 strawberries, hulled and sliced
1 cup raspberries, halved
½ cup blueberries
¼ cup pecans, raw, crushed
Directions
Line a shallow baking pan with parchment paper.
In a mixing bowl, whisk together yogurt, maple syrup, and a pinch of salt.
Spread the yogurt mixture evenly on the parchment paper.
Top with strawberries, raspberries, blueberries, and crushed pecans.
Place in the freezer for at least 3–4 hours until firm.
Once frozen, break into bark pieces using a chef’s knife.
Roasted Lemon Asparagus with Pistachios
Why It Supports Mood
Asparagus is a prebiotic-rich vegetable that feeds gut microbes, enhancing their ability to produce serotonin. The addition of pistachios provides healthy fats and plant-based protein, while lemon adds brightness and vitamin C for immune support.
Ingredients
2 lbs asparagus
3 tbsp olive oil
Salt and pepper, to taste
2 lemons (one juiced, one sliced)
1 clove garlic, minced
1½ tsp tarragon (or ½ tsp dried tarragon)
⅓ cup pistachios, raw and shelled
Directions
Preheat oven to 400˚F.
Wash the asparagus and trim off the woody ends. Place on a parchment-lined baking sheet.
Drizzle with 1 tablespoon of olive oil and rub to coat evenly. Sprinkle with salt and pepper.
Roast for 8–10 minutes, until asparagus turns bright green and tender.
While the asparagus is roasting, whisk together lemon juice, minced garlic, tarragon, and the remaining olive oil.
Once the asparagus is done, arrange on a platter, drizzle with the lemon dressing, and sprinkle with pistachios.
Conclusion
The colder months may bring shorter days and a heavier mood, but with the right strategies, you can take control of how you feel this winter. By focusing on nutrition, embracing holistic lifestyle changes, and exploring the connection between your gut and brain, you can significantly reduce the impact of Seasonal Affective Disorder (SAD).
Simple adjustments like incorporating omega-3-rich salmon, gut-friendly yogurt snacks, and prebiotic-packed vegetables can do more than nourish your body—they can help balance your brain chemistry and elevate your mood. Pair these with regular exercise, light therapy, and mindfulness practices for a comprehensive approach to overcoming the winter blues.
No two journeys are the same, and finding the right approach for your body and lifestyle is key. If you’re ready to take the next step in supporting your mental and physical health this winter, I’d love to help you create a personalized plan.
Book a nutrition counseling session today, and we’lll work together to make this your brightest winter yet.
Click here to schedule your appointment.

References
BetterHelp. (2023, April 5). 15 symptoms of depression and anxiety. BetterHelp. https://www.betterhelp.com/advice/depression/15-symptoms-of-depression-and-anxiety/
El Dib, R., Periyasamy, A. G., de Barros, J. L., França, C. G., Senefonte, F. L., Vesentini, G., Alves, M. G. O., Rodrigues, J. V. D. S., Gomaa, H., Gomes Júnior, J. R., Costa, L. F., Von Ancken, T. S., Toneli, C., Suzumura, E. A., Kawakami, C. P., Faustino, E. G., Jorge, E. C., Almeida, J. D., & Kapoor, A. (2021). Probiotics for the treatment of depression and anxiety: A systematic review and meta-analysis of randomized controlled trials. Clinical Nutrition ESPEN, 45, 75–90. https://doi.org/10.1016/j.clnesp.2021.07.027
Food and Mood Centre. (n.d.). The SMILEs trial. Retrieved from https://foodandmoodcentre.com.au/smiles-trial/
Harvard Health Publishing. (2020, January 29). Diet and depression. Harvard Health Blog. https://www.health.harvard.edu/blog/diet-and-depression-2018022213309
Harvard Health Publishing. (2023, March 22). Probiotics may help boost mood and cognitive function. Harvard Health Blog. https://www.health.harvard.edu/mind-and-mood/probiotics-may-help-boost-mood-and-cognitive-function
National Institute of Mental Health. (2022, December). Caring for your mental health. https://www.nimh.nih.gov/health/topics/caring-for-your-mental-health
National Institute of Mental Health. (2021). Depression. https://www.nimh.nih.gov/health/publications/depression
Melrose, S. (2015). Seasonal affective disorder: An overview of assessment and treatment approaches. Depression Research and Treatment, 2015, Article 178564. https://doi.org/10.1155/2015/178564
The Nutrition Insider. (n.d.). How nutrition impacts Seasonal Affective Disorder (SAD). Retrieved from https://thenutritioninsider.com/health-nutrition/how-nutrition-impacts-seasonal-affective-disorder/Yang, Y., Zhang, S., Zhang, X., et al. (2020). The role of diet, eating behavior, and nutrition intervention in seasonal affective disorder: A systematic review. Frontiers in Psychology, 11, Article 1451. https://doi.org/10.3389/fpsyg.2020.01451
#health and wellness#dietitian#nutrition#healthy food#healthy eating#winter blues#seasonal affective disorder#gut brain connection#probiotics#winter depression#omega 3#vitamin d benefits#winter recipes
1 note
·
View note
Text
Supporting Mental Health with Gut Health
Gut-Brain Connection: Gut health is directly linked to mental wellbeing through the gut-brain axis.
Probiotics: Beneficial bacteria that help regulate mood and support cognitive function.
Diet’s Role: Food choices have a significant impact on gut balance and mental health.
Prebiotics: Nourishing gut bacteria with prebiotics can boost mental wellness.
Lifestyle Influence: Stress management, sleep, and exercise are essential for maintaining a healthy gut and mind.
Introduction
Gut health significantly influences mental wellbeing. The gut-brain axis connects the digestive system with the brain, showing how a healthy gut supports mental clarity and emotional stability.
This connection is shaped by factors such as diet, probiotics, prebiotics, and lifestyle choices.
The Gut-Brain Connection

The gut-brain axis is a communication network linking the gut and the brain. This connection involves neurotransmitters, gut hormones, and the vagus nerve.
Imbalances in gut bacteria, known as dysbiosis, can lead to mood disorders like anxiety and depression. Maintaining a balanced gut environment is essential for mental wellness.
Probiotics and Mental Wellbeing
Probiotics are live bacteria that support a healthy gut environment. Certain probiotic strains, such as Lactobacillus and Bifidobacterium, influence the production of neurotransmitters like serotonin and GABA.
These neurotransmitters play a key role in regulating mood and reducing stress.
Diet’s Impact on Gut and Mental Health
Diet directly affects both gut health and mental wellbeing. A nutrient-rich diet supports a healthy gut, which in turn influences mood and cognitive function.
Ultra-processed foods, high sugar intake, and excessive carbohydrates can disrupt gut balance, leading to inflammation and negative effects on mental health.
Eating probiotic-rich foods, such as yogurt, kefir, and fermented vegetables, or taking supplements can help maintain a balanced gut microbiome, supporting mental health.
Foods like fermented vegetables, healthy fats, and complete proteins are particularly beneficial for gut health.
Prebiotics and Mental Wellbeing
Prebiotics are non-digestible fibers that nourish probiotics. These fibers help maintain a balanced gut environment, which is important for mental health.
Foods rich in prebiotics, such as garlic, onions, and leeks, can be included in the diet to support gut health.
Prebiotic supplements may also enhance the gut-brain connection and contribute to overall mental wellness.
Lifestyle Factors

Lifestyle choices are important in supporting both gut and mental health.
Managing stress through techniques like meditation and deep breathing helps maintain gut balance.
Regular exercise promotes a healthy gut microbiome and enhances mood.
Adequate sleep is also essential for gut health, as it allows the body to repair and maintain a balanced gut environment, which positively impacts mental resilience.
Conclusion
Maintaining optimal gut health is helpful for promoting mental well-being. There is not necessarily one approach that would be ideal for every person. With multiple options available to adjust lifestyle choices, the answer is within reach. Understanding the gut-brain connection and making informed dietary and lifestyle choices supports mental health and overall quality of life.
FAQ
How does gut health affect mental wellbeing? Gut health influences mental wellness through the gut-brain axis, impacting mood, stress levels, and cognitive function.
What are the best foods for supporting gut and mental health? Fermented foods, healthy fats, and complete proteins are excellent for supporting both gut and mental health.
Can probiotics help with anxiety and depression? Yes, certain probiotic strains support mood regulation and reduce symptoms of anxiety and depression.
How does stress impact gut health and mental wellness? Stress disrupts the gut microbiome, leading to digestive issues and negatively affecting mental health.
What lifestyle changes can improve both gut and mental health? Adopting stress management techniques, regular exercise, and quality sleep into your routine supports both gut and mental health.
Research
(2012). Structure, function and diversity of the healthy human microbiome. Nature, 486(7402), 207-214. https://www.nature.com/articles/nature11234
Appleton, J. (2018). The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health. Integrative Medicine: A Clinician's Journal, 17(4), 28-32. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469458/
Bercik P, Denou E, Collins J, et al. The intestinal microbiota affect central levels of brain-derived neurotropic factor and behavior in mice. Gastroenterology. 2011;141(2):599-609.
Borrelli L, Aceto S, Agnisola C., et al. Probiotic modulation of the microbiota-gut-brain axis and behaviour in zebrafish. Sci Rep. 2016;6:30046.
Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28(2):203-209.
Collins SM, Kassam Z, Bercik P. The adoptive transfer of behavioral phenotype via the intestinal microbiota: Experimental evidence and clinical implications. Curr Opin Microbiol. 2013;16:240-245.
Cryan JF, Dinan TG. Mind-altering microorganisms: The impact of the gut microbiota on brain and behavior. Nat Rev Neurosci. 2012;13:701-712.
Douglas-Escobar M, Elliott E, Neu J. Effect of intestinal microbial ecology on the developing brain. JAMA Pediatr. 2013;167:374-379.
Forbes JD, Bernstein C.N., Tremlett, H., Van Domselaar, G. and Knox, N.C. A fungal world: could the gut mycobiome be involved in neurological disease? Frontiers in microbiology. 2019;9:3249.
Foster JA, McVey Neufeld KA. Gut-brain axis: How the microbiome influences anxiety and depression. Trends Neurosci. 2013;36:305-312.
Goehler LE, Gaykema RP, Opitz N, Reddaway R, Badr N, Lyte M. Activation in vagal afferents and central autonomic pathways: Early responses to intestinal infection with Campylobacter jejuni. Brain Behav Immun. 2005;19:334-344.
Kennedy PJ, Clarke G, Quigley EM, Groeger JA, Dinan TG, Cryan JF. Gut memories: Towards a cognitive neurobiology of irritable bowel syndrome. Neurosci Biobehav Rev. 2012;36:310-340.
Lyte M. Microbial endocrinology in the microbiome-gut-brain axis: How bacterial production and utilization of neurochemicals influence behavior. PLOS Pathog. 2013;9:e1003726.
Lyte M, Varcoe JJ, Bailey MT. Anxiogenic effect of subclinical bacterial infection in mice in the absence of overt immune activation. Physiol Behav. 1998;65:63-68.
Long-Smith, C., O’Riordan, K.J., Clarke, G., Stanton, C., Dinan, T.G. and Cryan, J.F. Microbiota-Gut-Brain Axis: New Therapeutic Opportunities. Annual Review of Pharmacology and Toxicology. 2020;60(1):477–502.
Mayer EA, Padua D, Tillisch K. Altered brain‐gut axis in autism: Comorbidity or causative mechanisms? BioEssays. 2014;36(10):933–939.
Mayer EA, Savidge T, Shulman RJ. Brain-gut microbiome interactions and functional bowel disorders. Gastroenterology. 2014;146:1500-1512.
Mayer, E.A., Tillisch, K. and Gupta, A., 2015. Gut/brain axis and the microbiota. Journal of Clinical Investigation, [online] 125(3), pp.926–938. https://doi.org/10.1172/jci76304.
Mayer, E.A., 2011. Gut feelings: the emerging biology of gut–brain communication. Nature Reviews Neuroscience, [online] 12(8), pp.453–466. https://pubmed.ncbi.nlm.nih.gov/21750565/.
McVey Neufeld KA, Mao YK, Bienenstock J, Foster JA, Kunze WA. The microbiome is essential for normal gut intrinsic primary afferent neuron excitability in the mouse. Neurogastroenterol Motil. 2013;25(2):183-188.
Noble EE, Hsu TM, Kanoski SE. Gut to brain dysbiosis: Mechanisms linking Western diet consumption, the microbiome, and cognitive impairment. Front Behav Neurosci. 2017;11-19.
Rhee SH, Pothoulakis C, Mayer EA. Principles and clinical implications of the brain–gut–enteric microbiota axis. Nature Reviews Gastroenterology & Hepatology. 2009;6(5). https://doi.org/10.1038/nrgastro.2009.35
Sender R, Fuchs S, Milo R. Are we really vastly outnumbered? Revisiting the ratio of bacterial to host cells in humans. Cell. 2016;164(3):337-340.
Shkoporov AN, Hill C. Bacteriophages of the human gut: the “known unknown” of the microbiome. Cell host & microbe. 2019;25(2):195-209.
Sudo N, Chida Y, Aiba Y, et al. Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J Physiol. 2004;558(Pt 1):263-275.
Wang HX, Wang YP. Gut microbiota-brain axis. Chinese Medical Journal. 2016;129(19):2373-2380.
0 notes
Text
The gut-brain connection plays a crucial role in overall health, affecting digestion, mood, and cognitive function through the bidirectional communication of the gut-brain axis.
#gut brain connection#gut brain hunger control#gut brain disorders#brain gut axis ibs#gut brain connection anxiety
0 notes
Text
The Connection Between Stomach Issues and Stress.
Stress will always be a part of life. Stress can be detrimental to your physical and emotional health, whether it is brought on by personal problems, work-related demands, or unforeseen obstacles. Your digestive system, especially your stomach, is one place where stress has a particularly negative impact. This Article, The Gut-Brain Connection: How Mental Clarity Is Enhanced by a Healthy Stomach, explains how your digestive system and mental health are related. This complex connection is sometimes called the "gut-brain axis," and it is essential to understanding how stress can cause digestive issues.
Knowledge of the Gut-Brain Axis Your gut and brain are connected by a sophisticated communication system called the gut-brain axis. The trillions of bacteria, fungi, and other microbes that live in your digestive tract, along with the vagus nerve, the main nerve that connects the brain to the stomach, all contribute to this relationship. The gut and brain communicate through neural, hormonal, and immune pathways, meaning that what happens in your gut can influence your brain, and vice versa. Your gut receives signals from your brain during times of stress that may interfere with its regular operations. This disruption can lead to a range of stomach illnesses, from mild pain to more serious digestive issues. By being aware of this connection and seeking expert advice from gastroenterology in Surat, you may better control your stress and keep your digestive system in good working order.
How Stress Affects Your Stomach
Stress impacts your stomach in several ways. Here are some common stress-related digestive problems:
Stomach Pain and Cramps: Your digestive tract's muscles may spasm as a result of stress, giving you excruciating cramps. This is often why people experience stomach pain or a "knot in the stomach" when they are anxious or stressed.
Acid Reflux: Stress can increase the production of stomach acid, which may lead to acid reflux. This is a burning sensation in the throat and chest that can be very uncomfortable if it happens often.
Indigestion: Stress can slow down the digestive process, leading to indigestion. This may cause bloating, nausea, and a feeling of fullness even after eating a small meal.
Irritable Bowel Syndrome (IBS): Constipation, diarrhea, bloating, and abdominal pain are the symptoms of IBS, a disorder that is believed to be triggered by stress. Stress can exacerbate these symptoms, making the condition more difficult to manage.
Ulcers: While stress alone does not cause stomach ulcers, it can worsen existing ulcers or slow down the healing process. This is because stress affects the production of stomach acid and can weaken the stomach's protective lining.
Appetite Changes: Stress can also affect your appetite, causing you to either overeat or lose your desire to eat. Both of these behaviors can lead to digestive issues, including stomach pain and discomfort.
The Role of the Gut Microbiome
The gut microbiome plays a crucial role in how stress affects your stomach. The bacteria in your gut help regulate digestion, immune function, and even mood. When you are stressed, the balance of bacteria in your gut can be disrupted, leading to digestive problems and weakening your immune system. This imbalance can also contribute to mental health issues like anxiety and depression, creating a vicious cycle of stress and poor gut health.
To maintain a healthy gut microbiome, it is essential to manage stress effectively. This can help prevent stress-related stomach problems and promote overall well-being.
Managing Stress for a Healthy Stomach
Given the strong connection between stress and stomach problems, managing stress is crucial for maintaining a healthy digestive system. Here are some strategies to help you manage stress and improve your gut health:
Meditation and mindfulness: These techniques can help you de-stress and quiet your thoughts. These practices have been shown to lower levels of cortisol, the stress hormone, and promote relaxation.
Workout: Exercise regularly is an effective way to reduce stress. Exercise stimulates the release of endorphins, which are natural mood enhancers, and can help regulate digestion by promoting regular bowel movements.
Healthy Eating: A balanced diet rich in good gut health foods can support a healthy gut microbiome and reduce the impact of stress on your stomach. Incorporating fiber-rich foods, probiotics, and prebiotics into your diet can help maintain a balanced gut and improve digestion.
Sleep: Getting enough sleep is essential for managing stress and maintaining a healthy stomach. Aim for 7-9 hours of quality sleep each night to give your body time to repair and rejuvenate.
Limit Stimulants: Caffeine, alcohol, and nicotine can increase stress levels and irritate your stomach. Limiting your intake of these substances can help reduce the impact of stress on your digestive system.
Stay Hydrated: Drinking enough water is essential for digestion and overall health. Staying hydrated can help prevent constipation and support the health of your gut microbiome.
When to Seek Help
While managing stress can significantly improve your gut health, there are times when professional help is necessary. If you experience severe or persistent stomach problems, it is important to consult with a healthcare provider. They can help diagnose any underlying conditions and provide guidance on managing stress-related digestive issues.
If you suffer from chronic stress-related stomach pain or other digestive problems, consider seeking the advice of a gastroenterologist. They can perform tests to identify the root cause of your symptoms and recommend appropriate treatments.
Conclusion
The connection between stress and stomach problems is undeniable, and the gut-brain axis plays a crucial role in how stress affects your digestive system. By understanding this connection and taking steps to manage stress, you can improve your gut health and overall well-being. Incorporating healthy lifestyle habits, such as eating a balanced diet, exercising regularly, and practicing mindfulness, can help you manage stress and keep your stomach healthy.
Never forget that both physical and mental well-being depend on a healthy stomach. Taking care of your digestive system will not only improve your physical health but also enhance your mental clarity and emotional well-being.
#digestivehealth#healthylifestyle#digestion#gastrologist#tummy#gut brain connection#gut health#brain
0 notes
Text
0 notes
Text






#the twentysomething treatment#meg jay#meg jay phd#a revolutionary remedy for an uncertain age#food#emotional eating#stress eating#cooking#food and boundaries#sweets#carbs#high fat#snacks#dessert#gut health#gut brain connection#takeout
1 note
·
View note
Text
Researchers identify molecular link between gut bacteria and excitatory brain signaling in C. elegans
A new study published in Nature Cell Biology by Mark Alkema, PhD, professor of neurobiology, establishes an important molecular link between specific B12-producing bacteria in the gut of the roundworm C. elegans and the production of acetylcholine, a neurotransmitter important to memory and cognitive function. There is growing recognition among scientists that diet and gut microbiota may play an…

View On WordPress
0 notes
Text
Nurturing the Mind-Gut Connection: A Holistic Approach to Well-being

Trusting your gut goes beyond intuition; it’s a reflection of the intricate link between the brain and the digestive system. This connection, known as the gut-brain connection or gut-brain axis, plays a pivotal role in overall well-being, particularly mental health.
Understanding the Mind-Gut Connection
The bidirectional link between the brain and the gut is a fascinating phenomenon. Information flows both ways: the brain influences digestion, while the gut releases neurotransmitters and hormones impacting mental well-being. This connection even contributes to the post-meal sensation of happiness.
Central to this link is the gut-brain axis, a dynamic network connecting the gastrointestinal tract with the brain. This axis facilitates continuous information exchange, profoundly affecting various aspects of physical and emotional health.
The Gut Microbiome and Mental Health
Within the gut resides the gut microbiome, trillions of microorganisms shaping mental states. Research reveals the microbiome’s role in influencing brain function, mood regulation, and susceptibility to mental health disorders.
Additionally, the gut produces neurotransmitters like serotonin and dopamine crucial for emotional equilibrium. Surprisingly, about 95% of serotonin is synthesized in the gut, not the brain, emphasizing the profound impact of the gut-brain connection on mental wellness.
Scientific Evidence Linking Gut Health and Mental Well-being
Scientific studies highlight the link between gut health and mental well-being. Imbalances in the gut microbiome increase susceptibility to anxiety, depression, and stress-related disorders. Alterations in the gut microbiome can lead to shifts in behavior and mood.
How Gut Health Affects Mental Well-being
The gut-brain connection, or gut-microbiome-brain connection, is complex and influential in shaping emotional resilience and cognitive abilities. Neurotransmitters produced in the gut, such as serotonin and dopamine, play a vital role in regulating mood and emotions.
The Importance of Neurotransmitters in Gut Health and Mental Well-being
The gut’s production of neurotransmitters, such as serotonin and dopamine, influences mental well-being. Surprisingly, about 90% of serotonin, known as the “happy hormone,” is produced in the gut rather than the brain. A healthy gut provides a consistent supply of these essential neurotransmitters, promoting emotional balance and reducing the risk of mood disorders.
Inflammation and the Mind-Gut Connection
The well-being of the gut significantly influences inflammation levels throughout the body. Persistent gut inflammation can lead to leaky gut syndrome, allowing harmful substances to enter the bloodstream and potentially triggering neuroinflammation associated with mental health disorders.
The Role of the Gut in Hormone Regulation
In addition to neurotransmitters and inflammation, the gut plays a vital role in regulating hormones, such as cortisol responsible for stress. Disruptions in the gut microbiome due to chronic stress can cause various mental health problems.
Maintaining gut health involves caring for the gut microbiome through a balanced diet, exercise, and stress management techniques.
The Role of Wellness Retreats in Mental Health: Our Holistic Haven for Women
In the fast-paced world, finding inner peace and caring for mental health are crucial. Wellness retreats, like those offered by us, provide a sanctuary to step away from daily chaos, focus on self-care, and journey towards better mental health and overall wellness.
Wellness retreats serve a crucial role in enhancing mental health by providing a chance to break away from everyday pressures. Participants can replenish themselves physically and mentally through holistic activities, including meditation, yoga, and therapeutic sessions.
Our health retreats for women with chronic conditions are tailored to meet unique needs, offering a secure and encouraging space for personal development and recovery. The holistic approach aims to address underlying causes of mental health challenges while promoting the mind-body connection.

Yoga and Its Impact on Gut Health and Mental Wellness
Yoga plays a significant role in maintaining mental and gut health. Specific yoga postures enhance gut health and mental well-being. Daily practice of these asanas can contribute to overall wellness.
Natural Supplements for Mind-Gut Connection: Nurturing Emotional Wellness
Natural supplements, including probiotics, prebiotics, omega-3 fatty acids, and ashwagandha, can bolster the link between gut health and mental well-being. These supplements enhance gut microbiome stability, gut operation, and the gut-brain axis.
Probiotics reduce inflammation, improve gut lining integrity, and positively impact mood and emotional well-being. Prebiotics act as nourishment for existing gut bacteria, indirectly influencing the production of neurotransmitters and bioactive compounds that support emotional balance.
Omega-3 fatty acids and ashwagandha, with adaptogenic and anti-inflammatory properties, can enhance emotional resilience and gut health.
Holistic Approaches to Mental Well-being: Our Empowering Path to Healing
Holistic mental health approaches are gaining traction as people recognize the intricate connections between mind, body, and soul.
Our foundation rests on Ayurveda, an ancient Indian system harmonizing the body’s constitution and innate healing capabilities. Yoga reinforces the mind-body connection, stress reduction, and emotional resilience.
A dedicated team of health coaches guides each individual, offering tailored support, guidance, and encouragement for a self-driven healing journey. Integrating natural supplements into plans bolsters gut health, hormone balance, and overall vitality, aligning with our holistic philosophy.
Tailored treatment programs bring profound benefits, offering precise and practical assistance by addressing individual needs, resulting in improved mental well-being and an elevated quality of life.
To Conclude
The mind-gut connection is crucial to overall well-being and mental health. The gut microbiome, neurotransmitters, inflammation, and hormones all play an essential role in shaping emotional and cognitive abilities.
We emphasize a holistic approach to treating chronic conditions by assessing the parameters of the mind-gut connection. Taking care of the gut microbiome through a balanced lifestyle, including diet, exercise, and stress management techniques, can support gut health and improve mental well-being. So always TRUST YOUR GUT.
1 note
·
View note
Text
"The gut microbiota of individuals with pre-symptomatic Alzheimer’s differs from those of healthy people. Individuals in the initial phase of Alzheimer’s disease, where brain alterations have started but before cognitive symptoms become apparent, have a distinct mix of gut bacteria compared to healthy individuals, reveals a study conducted by the Washington University School of Medicine in St. Louis."
0 notes
Text
A really fun thing about chronic, systematic illnesses is that you can sometimes have a headache which causes a stomach ache which cases a headache which causes a —
#brain-gut connection my old nemesis#oh also it’s setting off my nerve pain#chronic illness#chronic pain#chronic fatigue#chronically ill#fibromyalgia
52 notes
·
View notes
Text
IBS is so funny i spent all day uncomfortable and anxious and convinced i was puffy and perhaps jaundiced and then remembered i treated myself to a single clove of garlic in a delicious vietnamese fish meal last night and was like ohhh
5 notes
·
View notes
Text
How the Gut-Brain Axis Influences Hunger, Anxiety, and IBS
Introduction
The gut-brain axis plays a crucial role in regulating hunger, managing anxiety, and influencing conditions like Irritable Bowel Syndrome (IBS). Understanding this connection can help in managing symptoms and improving overall health.
Gut-Brain Hunger Control: How It Works
The gut brain connection to regulate hunger and satiety, using hormones like ghrelin and leptin. These signals tell the brain when to eat and when to stop, balancing appetite and energy levels. An imbalance in this axis can lead to overeating or appetite loss.
Impact on Anxiety and Mood Disorders
The gut-brain connection significantly affects mental health, especially anxiety and mood disorders. The gut microbiome produces neurotransmitters like GABA, which helps calm the nervous system. Imbalances in gut bacteria can lead to increased anxiety and depression symptoms.
Brain-Gut Axis and IBS
The brain gut axis ibs is particularly important in managing IBS, a common gastrointestinal disorder characterized by abdominal pain, bloating, and irregular bowel movements. Stress and anxiety can exacerbate IBS symptoms, as the brain sends distress signals to the gut, altering gut motility and function.
Dietary Interventions for IBS and Anxiety
Dietary changes, including the addition of probiotics, prebiotics, and anti-inflammatory foods, can positively impact the brain-gut axis. For IBS sufferers, low-FODMAP diets have shown promise in reducing symptoms by limiting foods that can cause gut irritation.
The Role of Probiotics and Gut Health Supplements
Probiotics, found in fermented foods like yogurt and sauerkraut, support a balanced gut microbiome, improving gut-brain communication. Supplements specifically designed for gut health can further enhance this connection, alleviating anxiety, IBS, and hunger-related issues.
Conclusion
The brain gut axis ibs is a powerful link influencing hunger, anxiety, and digestive disorders like IBS. Through dietary management and the use of probiotics, one can significantly improve gut health, enhancing the overall communication between the gut and brain.
#gut brain connection#gut brain hunger control#gut brain disorders#brain gut axis ibs#gut brain connection anxiety
1 note
·
View note
Text
#migraine#health info#gut brain axis#gut brain connection#health information#medical information#vagus nerve#neurotransmitters
0 notes
Text
decided im buying a guitar w th3 first 3 paychecks i collect after i graduate. this simply cannot go on. im wasting my long dextrous quick fingers potential
but what im really sweating over is everyones advice to start with a cheaper basic one and earn my way up to something more serious(valid and it makes sense, fucking up an expensive one right from the start isnt something i could mentally handle). but ALSO i have a massive money savers complex and just the idea of habing to save money twice sends jolts of pain down mt spine. if i invest i want to make a GOOD choice from the start that i can make use of for eons to come. this need to spend as little money is possible is so strong that it paralyses me from making ANY investment at all. i feel like this is why ive postponed for as long as i did even tho i couldve saved up for 1 til now if i really set my mind to it
#the pretentious part in my brain is like#but what if i feel such a connection to music that i somehow play as tho ive played for years?#like naturally molding down to be one w my guitar#what if the guitar senses my love and sends pheromone chemicals that add a couple more neural connections . just like that?#should i invest in smth cheaper???? what if i misjudge my guitar ability and then i regret not going for smth better?#i really feel like i might hit it off from the get go... i jist feel it in my guts
5 notes
·
View notes