#chronic myalgia
Explore tagged Tumblr posts
Text
I’m doing this because my dad recommended doing a blog or something since I can’t work. Sooo imma sort of use this as an online journal to record my daily life with chronic illnesses and the process of getting diagnosed and all of that fun shit. As well as a journal about healing from my trauma.
So ye, I might make a YouTube channel but I dunno probs not.
#journal#healing#healingjourney#chronically ill#chronic illness#hypermobilty syndrome#inappropriate sinus tachycardia#chronic migraine#chronic myalgia#mast cell activation syndrome#healing from trauma#online journal#actually chronically ill#lgbt safe space#gay#trans male
3 notes
·
View notes
Text
Its been a really hard couple of Years for me frankly, and ive been putting off asking like this but i just can't afford the pain management i need to keep surviving, let alone try to live a lil.
Ongoing need so no number amount, but around $100 would keep me medicated for at least a week if not more.
Please don't give if you are also struggling.
Vnm- @GaleCollins
Csh- $mxgale


P4yp4l avaliable on request
136 notes
·
View notes
Text
I wrote a poem idk if I should post it
#poetry#poem#I like it but idk if other ppl will#it’s about#chronic illness#endometriosis#being a spoonie#spoons#spoonie#chronic pain#fibro#fibro myalgia
2 notes
·
View notes
Text
Rarely have I felt the frustration that I'm feeling now from not having health insurance. I just got a theory for the cause of my leg pain but i can't run it by a professional bc the stupid us government hates poor people!!! And also the medical industry hates poor people.
(And I'm not even that poor rn)
I guess I'll just do what any sane person would do and post it on the internet for strangers to comment on
Basically, I've dealth with leg pain for as long as I can remember. One of my earliest (and only) memories post 5-6 years old is taking a handful of pills. 1 adhd med and 3 pain killers. And I think 1 other drug but idk anyway
My leg pain hasn't really decreased since then, my pain tolerance has just increased. The only thing that decreases my leg pain is decrease the use of my legs. In fact, like I said, my leg pain *never* gets better from time OR exercise. I used to regularly go the gym!! I liked doing it! But when the muscle soreness from running o. The treadmill would go away and I'd go back to college, the walking from class to class would hurt just as bad as it did before I started exercising. You'd think, that with how exercise works, I'd be able to handle more the more I exercise, but no! My muscle pain stays the same no matter what. The same activities that caused pain, still cause the same amounts of pain even after I start committing to regular exercise. When I do doubles, I still hurt just as bad at the end of the day as I did when I started doing doubles. Doesn't matter how long I've been doing them, it still hurts just the same.
so, you must be thinking, "oh, well, sage, you must not be gaining any muscle tone!" WRONG!
My thighs are actually really well defined. I'd post a pic but I don't want weirdos looking at my thighs so ig you pervs will just have to use your imagination. I weigh, like 110ish pounds, and I promise you, most of that is my thighs. They're probably the biggest part of my body and it's all muscle. They're hard even when I'm not actually flexing, and even more so if I am, ofc. People have been genuinely shocked by how much muscle I have in my thighs, bc you wouldn't think it! My thighs are very strong tho
So, my theory would be that maybe I have smth that causes rapid and/or easy tears of the myofibrils in my thighs, therefore causing increased hypertrophy (or muscle growth). Basically, where my muscles are reacting to ANY bit of exercise like it's intensive training, and is tearing from basically anything I do, and bc it's having to heal so much I've experienced more hypertrophy than what one would expect from my usual activity level. Or maybe like a condition where that's a symptoms or a byproduct or smth idk
#chronic pain#if youre a doctor or have any knowledge of the medical field feel free to give me your thoughts and tell me how wrong i am for thinking this#idk it just...feels right#like my muscle pain feels exactly like how one describes their muscle pain after an intense excercise#sometimes with added soreness#like my whole thigh and most of my leg will feel like its just covered in muscle bruises#im so mad at medicaid ngl#bluh#medicine#gonna try to add some relevant tags bc i actually would like feedback#muscle pain#exercise#disability#?#idk it sure damn feels like it sometimes#i have to take 4 ibuprofen every time i double#sometimes even when i dont#it feels like every step i took was a squat#thats how ive described it for a while now#myalgia
0 notes
Text
You know how the pain scale is
🙂🥲😐😕☹️😢
Well, mine is
😐😶😬🤕🤢🤮
and I'm currently at 🤮 because I'm meds sick and when I get meds sick I puke and when I puke, the trauma memory* on my muscles kicks in, leading to unnecessary heightened pain when I'm puking. And I can't take pain meds for it because that's usually the cause of meds sickness...I forget to take them with food and end up really sick.
I'm usually at a 😶, BTW.
#*a severe case of food poisoning w severe pain in my arms and shoulders during vomiting traumatized my CNS and now there's always pain#tor's pain#pain#chronic pain#myalgias#meds sick#and my internet is out rn#i received a warning abt it but my boy/dog is still irritated by the absence of his white noise Wednesday...or should i say 'black noise' 😘#pain scale
0 notes
Text
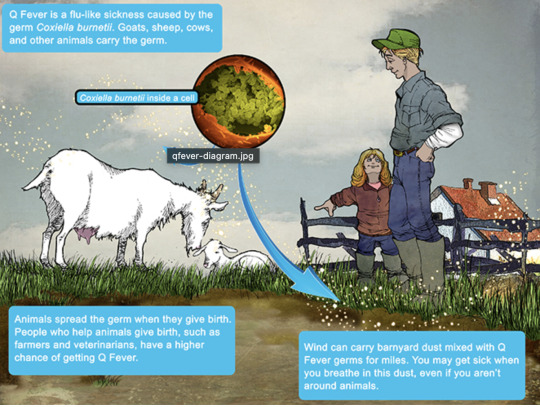
Q Fever
Aka, Query fever. What a weird name for a disease. Imagine telling people that's what you got.

in the 30s-40s, an Australian pathologist in QLD/Brisbane, came across an outbreak of the same or similar illness among abbatoir or slaughterhouse workers.
At the time, he called the disease "Q" fever or query as a temporary name until the pathogen could be identified. Unfortunately it stuck.
decades later, now nobel prize winner and virologist, MacFarlane Burnett isolated and identified the microbe responsible. I think this discovery contributed to his prize. i forget already.
Microbe responsible: Coxiella burnetti. Named for Burnett and HR Cox, the American bacteriologist who found the genus Coxiella where C burnetti falls under.
Initially they felt it was related to Rickettsia, responsible for Rocky Mountain Spotted Fever, but as science progressed, this was disproven.
Now for a Case Report
A 55 yo Italian man with a history of aortic valve replacement was diagnosed with pyrexia of unknown origin twice. Further signs included myalgias/splenomegaly/night sweats. The 2nd time he was admitted for PUO he deteriorated rather dramatically and was put on meropenem and teicoplanin.
A host of organisms was tested for on serological testing based on the man's travel and epidemiological history, all negative. Even a rheumatological panel was done, also less revealing. He also had a history of MGUS (a haem disoder), which is kind of a red herring here.
Cultures were negative, no vegetations were seen on a TTE - so they did consider IE. Which is an important differential for PUO.
Eventually a PET-CT was done (often favoured when investigations do not yield much for a sick patient with fevers), finally revealing a focus of infectious on his ascending aorta, where he'd also had previous surgery done. And in a round about way, they also further identified Coxiella Burnetti. He was treated doxycycline and hydroxychloroquine. As it's so rare in Italy, it wasn't really considered even though he mentioned rural travel.
Bottomline: Q Fever is an important consideration in the work up for culture negative IE. Further to this, always consider IE in the differentials for PUO particularly if they're at increased risk for IE (prosthetic valves, damaged valves, select congenital heart issues, previous IE). IE can present with night sweats, fevers, weight loss and splenomegaly. It can be insidious and chronic in nature. other risk factors can be more suggestive as we'll get into below.
Causative organism
Coxiella burnetti, it's a zoonoses - i.e. transmissible from animals. Special powers: very tough/hardy, can survive extreme environments (high temps and UV light etc.) over prolonged periods and is resistant to many common disinfectants/surface cleaners.
It's an intracellular pathogen and gram negative coccobacilli (PINK!)
name coccobaccili reminds me of cocopuffs.
it's mainly associated with farm animals, which the CDC so wholesomely displays on its website on Q fever (wtf).

goats, sheep, cattle typically (but many other animals, even birds, dogs and horses can be reservoirs)
in particular bodily fluids - amniotic fluid, placenta, faeces/urine, milk etc.
you can get it through unpasteurized milk and through inhaling it if it lands on dust in the area
ever visit a farm or petting zoo lately? OMG WASH YOU HANDS.

That said, it's typically inhaled in inorganic dust. You inhale it, it goes to the lungs, and then the bloodstream.
Increased risk for Coxiella burnetti (What to take on history of exposures and when to strongly consider it)
live on a farm or near one
exposure to a farm
work as a vet on a farm
farm worker, dairy workers, researchers on these animals/facilities
slaughterhouse/abbatoir
Also from CDC:
Clinical presentation
Most won't get sick after exposure and remain asymptomatic, a very small minority does. even though it is highly infectious.
incubation time is 2-3 weeks (consider this time in your history of exposure, did they work on the farm 2-3 weeks ago as opposed to yesterday).
Nonspecific acute infectious symptoms:
nonspecific systemic fevers/malaise/arthralgias/myalgias--> key is high fevers though and can be associated with headache and photophobia.
non specific GI - N/V/diarrhoea
respiratory ones - SOB or cough, consider it as atypical cause of community acquired pneumonia.
rare: hepatitis and jaundice (granulomatous) or encephalitis with neurological complications such as demyelinating disease or CN palsies, also haemolytic anaemia and HLH (yikes)

really it's the history of exposure that will lead you down the garden path to Q fever.
Chronic Q fever is perhaps worse, and can present as culture negative IE/PUO. Months/years later, as B symptoms as above above + LOW/LOA, night sweats. More likely to occur if you are predisposed for IE as above, have a weakened immune system for any reason, including pregnancy.
Chronic Q fever has a mortality of 10% if left untreated. About <5% of those with acute Q fever develop this if left untreated. Speculation is that it's more of an autoimmune process or abnormal immunological response to the bacteria.
To be honest, most who walk in the door with community acquired pneumonia get treated empirically for atypicals anyway, (standard course of doxycycline), so we hardly really ponder the question of Q fever in every patient. But if they present chronically and did not have atypical cover at the onset of acute symptoms, then it's something important to consider.
Other important conditions - can cause complications in pregnant women and 20% will get post Q fever syndrome. like chronic fatigue.
investigations
Serology! nice and easy. Look for IgG antibodies in the chronic presentation. Or PCR. Down side to serology - can take 2-3 days for the body to make said antibodies to the bacteria for detection. PCR can be done on any fluids/tissue sent.
Cultures useless, hence it fall under the umbrella of culture negative (hard to grow outside a host cell, it is an obligate intracellular pathogen).
Other hints on bloods (as serology/PCR takes time to return) - elevated or low platelet's, transaminitis with normal bili, opacities in CXR with hilar lymphadenopathy, CSF will show raised protein levels if done when encephalitis is suspected.
imaging can also support the diagnosis.. as illustrated by the case report.
Treatment
Acute disease - as standard for atypical bugs, doxycycline 100 mg BD for 14 days. Alternatives - TMP SMX or Clarithromycin.
Chronic Q fever or IE:
native valves: doxycycline and hydroxychloroquine (200 TDS) for 18 months
prosthetic: same but 24 months
why hydroxy: enhances the action of doxycycline (increases the pH of the phagolysosome)
Follow-up: look for 4 fold decrease in IGG
Sources:
CDC
Stat Pearls
Wiki as linked above
#australian history#medblr#medblrs#infectious disease#infectious diseases#q fever#coxiella#coxiella burnetti
74 notes
·
View notes
Text
Long COVID and hypermobility spectrum disorders have shared pathophysiology - Published Sept 4, 2024
Abstract
Hypermobility spectrum disorders (HSD) and hypermobile Ehlers–Danlos syndrome (hEDS) are the most common joint hypermobility conditions encountered by physicians, with hypermobile and classical EDS accounting for >90% of all cases. Hypermobility has been detected in up to 30–57% of patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), fibromyalgia, postural orthostatic tachycardia syndrome (POTS), and long COVID (LC) compared to the general population. Extrapulmonary symptoms, including musculoskeletal pain, dysautonomia disorders, cognitive disorders, and fatigue, are seen in both LC and HSD. Additionally, ME/CFS has overlapping symptoms with those seen in HSD. Mast cell activation and degranulation occurring in both LC and ME/CFS may result in hyperinflammation and damage to connective tissue in these patients, thereby inducing hypermobility. Persistent inflammation may result in the development or worsening of HSD. Hence, screening for hypermobility and other related conditions including fibromyalgia, POTS, ME/CFS, chronic pain conditions, joint pain, and myalgia is essential for individuals experiencing LC. Pharmacological treatments should be symptom-focused and geared to a patient’s presentation. Paced exercise, massage, yoga, and meditation may also provide benefits.
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator#long covid#covid conscious#covid is not over#covid isn't over
16 notes
·
View notes
Text
hey guys...i don't really like to get personal on here, but im just looking for some ideas or input...
idk if the diagnosis is correct bc the office i was diagnosed at also physically assaulted me and then denied me care bc i left a bad google review, but in 2017 i was diagnosed with an acute form of fibromyalgia called pelvic floor myalgia. it's a chronic pain condition that usually just feels like extremely bad cramps but it will shoot into my legs as well and radiate throughout my whole lower body. there are days where i can't even walk. but lately the pain has been so so so much worse than usual. i feel like I've tried everything. OTC meds, hot showers/baths, THC (and some other recreational type substances, but those aren't exactly a regular option for health and 𝕝𝕖𝕘𝕒𝕝 and practicality reasons), being active (which is only possible when im not already in pain, which lately is never, bc me trying to be active during high pain times is impossible), and when i was first diagnosed i also tried the bullsht physical therapy.
so far i have heard that turmeric might help, so that's on my to-get list, and something called Lamaze breathing. i guess i was just hoping maybe someone here might know of a remedy for chronic pain, im willing to do ~almost~ anything at this point 😭
#except do pt at a clinic bc that just seems like the gateway to getting assaulted again#and pt didn't help#i also have an appointment with a new dr coming up#but that's not for a few weeks and i think i might just go insane#this sucks 😭😭😭#personal#text
9 notes
·
View notes
Note
Dave has chronic pain, how wouldn't he? he got fuckin berated and traumatized as a kid, and because I have it he gets to have fibro(myalgia) too
real & true
10 notes
·
View notes
Text
Writing about Disabilities: Chronic Pain
When writing about anything you are not personally familiar with, research is your best friend. Don't use this post as a catch all and think it's all you need to write characters with chronic pain. This is far from all the information about it, but it's a starting point.
Here's some basic information that I have found and I've also included some of my own experience since I have chronic pain.
Information regarding Chronic Pain
First thing's first, what is chronic pain? According to John Hopkins Medicine, the difference between chronic pain and regular pain is that chronic pain is long-lasting (anywhere from months to years). Chronic pain doesn't stay the same level (0-10) for everyone; also, majority of people with chronic pain don't realize that the normal amount of pain is 0. It can be continuous or it could switch from 0 to 10 to 6 to 3 to 9 to 7 and so on so forth...
There are various types of pain as well: muscle, joint, headaches/migraines, and nerve. You can have one or you can have all of them. Personally, I have all four. The first three for me are chronic and the nerve pain is from a recent surgery. They all have different causes and I know some of them. For example, my migraines are genetic and very common in my family. The joint and muscle pain probably caused multiple things but I know for sure it's caused by the scoliosis I've had for over a decade. My entire body was developing unevenly. So my joints are weakened and different muscle groups developed unevenly (especially my back and core).
Here's some clinical resources for the different kinds of pain that just cover the basics:
Muscle related: Myalgia | John Hopkins, Muscle Pain | Cleveland Clinic
Joint related: Arthralgia | John Hopkins, Joint Pain | Mayo Clinic, Joint Pain | Cleveland Clinic
Migraine related: Migraines | Mayo Clinic, Migraines | NIH.gov
Nerve related: Neuralgia | Health Direct
Something worth doing in your research is to find blogs, vlogs, or influencers that have personal experience with chronic pain. Don't overstep and reach out to them about research for the character you're writing. If they are open to questions, feel free to just remember to be respectful. Otherwise, read or listen to their experiences and research more until you think you have a grasp of it. If you are unsure of something, you have a search engine at your finger times, use it! Remember to cross analyze information though because just because it says it one place online doesn't mean it's true in all cases.
Things to Consider about the character you're writing:
How long have they had chronic pain? Just because it's chronic, doesn't mean they've had it all their life. If they've had it for a while, they might be good at hiding their pain or masking. They also may be more aware of their body and their limits (ex. they know they can't walk more than x miles before being in pain). They probably have already figured out some treatments that help them manage the pain like pain killers or hot/cold therapy. If they only recently developed it, they're pain may be more visible (ex. they can't sit still because of pin and needles). They'll probably more vocal in their complaints of it as well.
What is causing their pain? Don't give your chronic pain just to give them something. Do they have an autoimmune illness or some form of invisible illness? Do they have something kidney stones? Do they have an illness that has flare-ups? If you're writing fantasy, did someone curse them with never ending pain? You don't have to flat out state it to the reader if you don't want to. You're allowed to make it unknown but as the author, make sure there is a reason you are writing a character like this. Make sure it has a role in the story you're telling. If you are writing chronic pain that's connected to a specific illness, remember to also research that illness. Chronic pain is usually a symptom not a diagnosis. If you look my own medical chart, it says I have a history of chronic pain and it's lists the kinds of pain. The only thing that is a diagnosis of pain is migraines (but those can also be a symptom it depends on the person).
**Once again, always do more research. Do not use this post as all you need. Anytime you write something or create a character that has something you aren't familiar with, you need to take the time to learn about it. Research Research Research!
#godless has writing prompts#writing advice#writers on tumblr#writeblr#writing#disability representation#writing disabilities#chronic pain#writing research#writing resources
19 notes
·
View notes
Text
More than the surface beyond seizures, continued...
Epilepsy is a neurological condition affecting millions around the world. Though seizures are the most visible symptoms, there are many hidden symptoms, which relentlessly affect the lives of people with epilepsy. They include continuous headaches, dreadful migraines, and unsettling sensations-also known as déjà vu. Chronic anxiety and depression are common, usually worsened by the emotional burden of living with the condition. At an advanced stage, they develop suicidal tendencies. Brain fog and memory loss are some of the other common complaints along with chronic fatigue and stress. Mood swings and irritability tend to be uncontrollable. A substance of light or food can trigger an attack of discomfort or seizures. Some may also suffer from hallucinations, nausea, weakness in the body, abdominal pain, myalgia, numbness, tingling, etc. Episodes of racing heart rate and heavy sweating can be very distressing; sudden mood swings and blind spots make the condition more intricate. Dilated pupils and spurts of staring blankly, often mistaken for daydreaming, are also part of the symptomatology. Understanding and acknowledging these invisible symptoms forms a huge part of offering a conducive environment for people living with epilepsy. It can be managed by medication adherence, regular check-ups, maintenance of good lifestyle, and getting connected with support networks. By creating awareness and empathy, we can better support these individuals with epilepsy and therefore make our community more inclusive for everyone.

2 notes
·
View notes
Note
hi! im not sure if this is the right place to ask but my friend recently suggested to me that i probably have chronic pain and i sort of dont really know what to do? do you have any good resources for newly felt chronic pain (idk how to word it but its only cropped up in the last year or so) and how to navigate it? im really worried since its getting worse and i feel so lost :(
Hello anon! I'm also thinking and moving with this pain-made-pain, and very much empathize with what you're dealing with here. I recommend looking into the work & wisdom of crip doulas like Leah Lakshmi Piepzna-Samarasinha and Shayda Kafai, both of whom have written extensively on grief and grappling with worsening pain / "becoming more disabled" and the complex fears that go along with that. I also wrote about acquired disability, and will probably do so even more in the future.
Annie Elainey is/was an influencer who spoke a lot about queercrip matters, including tracking their chronic pain. They aren't so active on youtube anymore, but they provide an excellent grammar for talking about shifts in pain and ability.
#NEISVoid is also a huge community on basically every platform, where you can ask questions and get answers from a variety of people –– many of whom have been through exactly what you're feeling before.
Lastly, there are a few folks on here I also trust to speak about pain and becoming (more) physically disabled/ill - @crippleprophet, @cannabiscomrade, @materialisnt, @illnessfaker, @myalgias, and @osmanthusoolong, and whoever they all recommend.
#disability#ask#anonymous#i hope this helps - also if you're tagged and don't want to be#lmk and ill remove you
26 notes
·
View notes
Text
Any other chronic fatigue baddies feel like, actual endorphin release from laying down after being upright for a while? Like, it's legit almost orgasmic levels of relief when i first lay down after work
63 notes
·
View notes
Text
Everything to know about Vitamin -D
First of all, we should know the basics of vitamins. There are two groups of vitamins depending on the solubility.
One is Fat soluble and other is water soluble. In fat soluble group falls Vitamin A, D, E & K. In water soluble group falls Vitamin B complex & Vitamin C. vitamin D test cost
Vitamin D is synthesized in our body which involves three major steps at three different organs. In the first step, the primary form of Vitamin D is synthesized under the skin, when UV rays fall on the skin.
One can get UV rays through sunlight with the early morning sunlight exposure. The second step occurs at Liver. 25-hydroxy cholecalciferol is synthesized in the liver by the process of hydroxylation which is still not an active form. vitamin D test cost
The active form of vitamin D i.e. 1,25-cholecalciferol is synthesized in the kidney. This is the active form of vitamin D,it is also called as Vitamin D3/ Calcitriol.
So, to be precise, Vitamin D synthesis starts at the skin and ends at the kidney via liver. So, any condition which affects these three organ systems, will also affects vitamin D synthesis. vitamin D test cost
Previously it was assumed that function of Vitamin D is absorption of calcium. But over the period it has been proved that it is not the only function, Vit.D plays important role in functioning of Musculoskeletal system, Skin, Neurological system, Cardiovascular system.
Normal level of Vitamin D3 is above 30ng/ml. If it is above 100 ng/ml, it is called as hypervitaminosis. vitamin D test cost
So, Vitamin D3 level has to be maintained between 30-100ng/ml. In children Vitamin D3 deficiency presents with Rickets which presents with bone pain, angular deformities of the extremities (Genu valgum, cubitus varus, coxa vara).
If detected timely, it can be corrected with Vitamin D3 supplements. In adults, Vitamin D3 deficiency may present with many musculoskeletal symptoms like myalgia, recurrent body ache, early fatigue, fractures with trivial injury.
Long standing vitaminD3 deficiency leads to osteoporosis which means decreased bone density. vitamin D test cost
It’s ironic that though we live in India which is a tropical country with ample amount of sunlight exposure throughout the year, still a large no. of the Indian population is suffering from Vitamin D3 deficiency. vitamin D test cost
The important cause for this is Sedentary lifestyle & dietary habits. To correct vitamin D3 deficiency, lifestyle modification, healthy dietary habits, and avoiding junk food also play a vital role.
Signs of Vitamin D Deficiency
Bone Pain: Chronic musculoskeletal pain, especially in the back, hips, and legs, can be a sign of Vitamin D deficiency.
Frequent Infections: Since Vitamin D is involved in immune function, low levels may increase susceptibility to infections. vitamin D test cost
Fatigue: Persistent fatigue and low energy levels could be indicative of Vitamin D deficiency.
Mood Changes: Depression, anxiety, and irritability may be linked to insufficient Vitamin D. vitamin D test cost
Impaired Wound Healing: Slow healing of wounds and frequent infections may occur due to compromised immune function.
For correction of Vitamin D3 levels, there are different formulations available like Injectables, capsules, sachets, solutions. vitamin D test cost
Depending on the level of vitamin D3, dosage and duration of treatment has to be decided. One need to consult Orthopaedic doctor in Baner to correct vitamin d3 levels and associated conditions with it.
Vitamin D is not just a vitamin; it’s a vital hormone that influences numerous aspects of health and well-being. From supporting bone health to bolstering the immune system and regulating mood, its impact on the body is profound.
While sunlight remains the primary source, supplementation and dietary adjustments can help maintain optimal levels, especially in populations at risk of deficiency. vitamin D test cost
By understanding the importance of Vitamin D and taking steps to ensure adequate intake, you can unlock its full potential and promote overall health and vitality.
2 notes
·
View notes
Text
Okay so something that is really important that a lot of able-bodied individuals don't realize, is that when you live with any sort of chronic illness, whether it be physical or mental, you often have to do your own research on your symptoms. If you don't, doctors are going to dismiss you. If you're lucky you'll get maybe a CBC panel ran. If you're like me (and from what I see online, many other spoonies), your chronic illness (fibro) will be blamed for your symptoms and you'll be forced to move on. That could be in the form of finding a different doctor (which is SUPER hard to do in the US because of insurance restrictions, and that's assuming you're lucky enough to have insurance) or by accepting their answer and just coping with the new symptoms.
I write this because I have had abnormal blood counts for the past almost 2 years, and abnormal body feelings (clearly swollen and painful knees to the point where I have seriously debated on if I needed a mobility aid like a cane, Baker's cyst, yadda yadda yadda) for roughly 1.5 years.
Anyways, at my last doctor's appointment in...May? June? Something like that, I had to go in to the doctor with my previous abnormal blood counts, dating back to when I was living in a different state, even though they had the records from that state because EHRs are a thing, because they weren't helping me. I had to go in with possible explanations and explain why I was considering them, and why I ruled them out. I had to go in to a doctor who was ADAMANT that all I needed was physical therapy and then I wouldn't be in so much pain. Keep in mind here, that I experienced pain when sitting. I experienced pain when lying down. I experienced pain when standing or walking. I experienced a TREMENDOUS amount of pain going from sitting to standing or standing to sitting. It was to the point where, on the pain scale, I was at maybe a 7 or 8 on a daily basis? And that's going off of my pain scale, which is drastically different from the "average person" pain scale because, surprise, I live with chronic pain. So in general my pain (prior to all of this) is at maybe a 1 or 2 on my pain scale? That translates to maybe a 3 or 4 on the average person pain scale? So now instead of downplaying how much pain I'm in (I mean, I still probably downplay it just because of internal feelings about needing to not be a burden on others and not make my needs so prevalent that it inconveniences anyone else), I have started adapting my answers to what I think an able-bodied individual's pain scale is (never been fully able-bodied, so who even knows how accurate that is).
So back to the point:
Yes, it may have been the fact that I started crying in the doctor's office because I wasn't feeling heard or taken seriously, or it may have been that I did my own research, came in with possible answers (through reputable sites - so not fricken WebMD), and came in with all of my abnormal blood levels since they started almost 2 years ago.
BUT, with all of that said, that was the only way I was able to get any sort of medical intervention. Sure, I could've upped my meds more, but that's not looking at WHY I'm in so much (non-fibro) pain. That's not explaining WHY my joints are swollen to the point where it hurts to walk. That was the only way I was able to get an order for a CT of one of my knees and new bloodwork ran. And - surprise, surprise - they found things. They found a possible reason for why one of my knees was acting up (still had the problem of the other knee, but whatever. One knee taken care of is helpful). They found inflammation in my blood (and if you tell me fibro is a fricken inflammatory disorder I will probably rage quit your comment, because that's what a hematologist decided to say, clearly knowing nothing about the disorder and instead telling me that "fibro" meant "inflammation". No, "fibro-" means "relating to or characterized by fibers" and "-myalgia" means "pain in a muscle, or group of muscles". So don't come at me with that).
Anyways, what I'm really trying to say, is that if you or someone you know is not fully able-bodied, we often have to do our own research. Why? Because 1) medical doctors often don't take us seriously, 2) we know our bodies better than anyone else regardless of degree status, 3) medical providers seem to not like actually looking deeply at a case and let's face it, if you just went through however many years of medical school and had to conceptualize endless cases, you wouldn't want to do in-depth analyses of cases either, and 4) how else are we going to know what questions to ask if we haven't looked up possible reasons for our symptoms or bloodwork or whatever it may be?
Believe your non-able-bodied friends. Believe your spoonie people. We know how to research conditions and rarely stop at just one website (just because conditions are usually more complex than just a common cold or something). We are doing the best we can in a broken system where no one wants to believe us.
And for those spoonies/disabled folx, if your doctor refuses to run blood tests or imaging or whatever it may be, make a FIRM request (more like a demand) that they write IN YOUR CHART that they declined to do whatever it is you are asking them to do, so that there's documentation and they can be held accountable. I have yet to do this, but from what I've seen from other people, medical professionals don't like writing that they denied something, so they tend to then send in the order.
#larjb3#spoonie#spoonies#fibro#fibromyalgia#mystery diagnosis#mystery diagnoses#chronic illness#unknown illness#medical problems#abnormal blood work
6 notes
·
View notes
Text
Hypothyroidism
Clinical features – The clinical manifestations of hypothyroidism are highly variable, depending upon the age at onset and the duration and severity of thyroid hormone deficiency. Common symptoms of thyroid hormone deficiency include fatigue, cold intolerance, weight gain, constipation, dry skin, myalgia, and menstrual irregularities. Physical examination findings may include goiter (particularly in patients with iodine deficiency or goitrous chronic autoimmune thyroiditis [Hashimoto's thyroiditis]), bradycardia, diastolic hypertension, and a delayed relaxation phase of the deep tendon reflexes. Serum concentrations of thyroid peroxidase (TPO) autoantibodies are elevated in more than 90 percent of patients with hypothyroidism due to chronic autoimmune hypothyroidism (Hashimoto's thyroiditis).
●Diagnosis – The diagnosis of hypothyroidism is based primarily upon laboratory testing. In most patients with symptoms suggestive of hypothyroidism, the serum thyroid-stimulating hormone (TSH) should be the initial test. If the serum TSH concentration is elevated, the TSH measurement should be repeated along with a serum free thyroxine (T4) to make the diagnosis of hypothyroidism. If central hypothyroidism is suspected (eg, presence of pituitary or hypothalamic disease), or if the patient has convincing symptoms of hypothyroidism despite a normal TSH result, we measure serum TSH and free T4.
•Overt primary hypothyroidism – If the repeat serum TSH value is still high and the serum free T4 is low, suggesting primary hypothyroidism, replacement therapy with T4 should be initiated.
•Subclinical hypothyroidism – Patients with a high serum TSH concentration and a normal serum free T4 concentration may have subclinical hypothyroidism.
•Central hypothyroidism – In patients with central hypothyroidism, the serum free T4 value is low-normal or low and serum TSH may be frankly low, inappropriately normal (for the low T4), or slightly high (5 to 10 mU/L) due to secretion of biologically inactive TSH.
●Differential diagnosis – The differential diagnosis of an elevated serum TSH concentration includes resistance to TSH, recovery from nonthyroidal illness, and a TSH-secreting pituitary adenoma.
●Identifying the cause of hypothyroidism – The clinical evaluation of a patient with primary hypothyroidism should be directed toward confirming the presence and identifying the cause of the hormone deficiency. The history, for example, may uncover past treatment of hyperthyroidism with radioiodine or thyroidectomy, the use of drugs that affect thyroid hormone synthesis, or history of iodine deficiency or excess. We do not routinely measure TPO antibodies in patients with primary overt hypothyroidism, because almost all have chronic autoimmune thyroiditis.
●Screening
•We suggest not performing population-based screening for hypothyroidism (Grade 2C). As an alternative, we prefer to screen individuals who are at increased risk for hypothyroidism.
•Measurement of serum TSH (rather than free T4 or total T4) is an excellent screening test for hypothyroidism in ambulatory patients. However, TSH alone may not be a useful tool for the diagnosis of hypothyroidism if pituitary or hypothalamic disease is known or suspected; in hospitalized patients, since there are many other factors in acutely or chronically ill euthyroid patients that influence TSH secretion; and in patients receiving drugs or with underlying diseases that affect TSH secretion.
•The universal screening of asymptomatic pregnant women for hypothyroidism during the first trimester of pregnancy is controversial. We suggest a targeted approach rather than universal screening (Grade 2C). We favor screening pregnant women if they are from an area of moderate to severe iodine insufficiency, have symptoms of hypothyroidism, a family or personal history of thyroid disease, or a personal history of TPO antibodies, type 1 diabetes, class 3 obesity, head and neck radiation, recurrent miscarriage, or infertility.
3 notes
·
View notes