#Spinal cord injury rehabilitation guidelines
Explore tagged Tumblr posts
Text
Best Physiotherapy Hospital
Hospital for physiotherapy Adhesive capsulitis, another name for frozen shoulder, is a painful and stiff shoulder ailment. It happens when the tissues around the shoulder joint swell and thicken, impairing the shoulder's ability to move normally.
Although the precise aetiology of frozen shoulder is unknown, persons who have specific medical disorders, such as diabetes, as well as those who have had past shoulder injuries or surgeries, are more likely to develop the illness. Moreover, women and persons over 40 are more likely to experience it.
The signs of frozen shoulder usually appear gradually and can include shoulder pain and stiffness, trouble moving the shoulder, and a reduction in range of motion. best physiotherapy hospital Adhesive capsulitis, another name for frozen shoulder, is a painful and stiff shoulder ailment. It happens when the tissues around the shoulder joint swell and thicken, impairing the shoulder's ability to move normally.
Although the precise etiology of frozen shoulder is unknown, persons who have specific medical disorders, such as diabetes, as well as those who have had past shoulder injuries or surgeries, are more likely to develop the illness. Moreover, women and persons over 40 are more likely to experience it.
The signs of frozen shoulder usually appear gradually and can include shoulder pain and stiffness, trouble moving the shoulder, and a reduction in range of motion.
treated in a best physiotherapy hospital. There are three stages to the condition: freezing, frozen, and thawing. As the shoulder enters the freezing phase, it gets more painful and rigid. While the discomfort may lessen during the frozen period, the rigidity does not. Ultimately, the range of motion steadily improves during the thawing phase.
In most cases, physiotherapy in a best physiotherapy hospital, pain management, and anti-inflammatory drugs are used to treat frozen shoulders. Exercises to increase flexibility and strength, manual therapy, and teaching are all possible components of physiotherapy. Ice, heat, or drugs like acetaminophen or ibuprofen may be used to relieve pain.
While healing times can vary, most persons with frozen shoulders will eventually feel better. In some circumstances, the healing process could take many months or perhaps two years. Surgery is rarely needed, but may be an option for people who do not respond to other treatments.
In conclusion, a frozen shoulder is a condition in which the shoulder joint becomes stiff and painful. It can be caused by a variety of factors, and treatment typically involves a combination of physiotherapy in best physiotherapy hospital, pain management, and anti-inflammatory medications. While the recovery time can vary, most people with frozen shoulders will eventually recover with appropriate treatment.

#Physiotherapy hospital#Physio care in kakinada#Physiotherapy hospital near me#Physiotherapy hospital in kakinada#Smart Physiocare Hospital#Physiotherapy treatment in kakinada#Best physiotherapy hospital in kakinada#Best physiotherapy hospital near me#Best physio care hospital#Rehabilitation center#Rehabilitation center near me#Paralysis rehabilitation center near me#Spinal cord injury rehabilitation#Spinal cord injury rehabilitation guidelines#Spinal cord injury rehabilitation near me#Spinal cord injury rehabilitation in kakinada#Smart Physiocare and Cancer Rehabilitation#Cancer Rehabilitation near me#Smart Physiocare and Cancer Rehabilitation in kakinada#Cervical Spondylosis#Lumbar Spondylosis#Frozen shoulder treatment#Palliative Care#Geriatric Rehabilitation#Pre/Post-Pregnancy Rehabilitation#pre and post natal physiotherapy
1 note
·
View note
Text
Choosing Personal Mobility Equipment
Choosing the right personal mobility equipment aid is a transformative experience that can greatly improve quality of life. Before making a purchase, consider the environment you’ll be navigating and your specific health needs.
For example, people with mild weakness can choose a walker or rollator to take weight off their legs. But for those with more moderate weakness, a wheelchair is often the best choice.
Wheelchairs
Wheelchairs are a great option for those with mobility impairments such as amputations, paralysis, spinal cord injuries and other conditions like Cerebral Palsy. They offer a great deal of flexibility to accommodate specific healthcare needs and provide comfort and support.
Many wheelchairs can be customised to meet individual needs with different options and accessories such as a wide range of seating positions, cushion types, adjustable axle position, head control, sip and puff etc. Some are also designed to be more compact in order to make it easier for individuals to transport them in their cars, buses or trains.
If you’re thinking about purchasing a new wheelchair, it’s important to be aware of the American with Disabilities Act (ADA) and DMAS’ guidelines that shape how businesses can treat users. You should also consider getting a specialty evaluation from an LCMP (Licensed Clinical Medical Professional) with experience in wheelchair assessment and rehabilitation engineering who will document the specific medical need for the chair and its options and/or accessories.
Scooters
Scooters are a fun alternative to riding a motorcycle or car. Depending on engine size, they can reach highway speeds and could legally participate in freeway traffic (check your local laws).
The scooter’s engine powers two small wheels that provide all the power to move. It has a small, easily maneuverable base that enables you to step on and off. Most models quickly disassemble into four or five pieces for transportation and storage in your vehicle.
They’re easy to ride and require less physical effort than cycling. They can be used to cover the “last mile” of your journey from your home to a bus station or transit center. Scooters use either mechanical or electronic braking systems. Mechanical brakes include disc, drum and foot brakes; electronic systems are strictly motor-driven.
Rollators
Rollators allow individuals to move about with confidence and comfort. Unlike standard walkers, they don’t snag on obstacles or get stuck on dips in the pavement. The wheels also make it easier to navigate over uneven surfaces – meaning users can go on walking adventures in a wider range of locations than they could with their old mobility aids.
When choosing a rollator, there are many things to consider to ensure it suits your specific needs. For example, you can opt for a model with handles at a height that matches your natural arm length to maintain good posture and prevent unnecessary strain. You can also choose from a range of wheel sizes to suit your intended terrain. Larger wheels are best for outdoor use, while smaller ones offer maneuverability indoors.
Additionally, you can select from models with hand brakes or lean-activated brakes to suit your preference and underlying abilities. The latter feature can be particularly useful for individuals with less hand strength.
Stairlifts
Often a person’s struggle with mobility is caused by a lack of upper body strength or the difficulty of walking up and down stairs. A stair lift can be a simple solution for this problem; simply sit in the seat and let it carry you up and down the stairs.
Stair lifts come in a variety of shapes, sizes and configurations to fit pretty much any staircase. Their base is attached to the rail and contains the motor, gears and battery which gives the chair its movement. Many models also have a ‘call and send’ button to allow multiple people to use the chair simultaneously.
The best option for most is to talk to a professional mobility retailer who can help you find the right lift for your needs and home, install it and provide ongoing repairs and customer support. The result is a lift that helps you to keep your independence and live the life you want at home.
0 notes
Text
Key Roles Of Paralysis Doctors!
The Best Paralysis Doctor In Borivali, also known as a neurologist or a physiatrist specializing in paralysis treatment, plays a crucial role in the diagnosis, management, and rehabilitation of patients with paralysis. Here are some key aspects of their role:

Diagnosis: Paralysis doctors are trained to diagnose the underlying cause of paralysis, which can result from conditions such as stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, or neurodegenerative diseases. They conduct comprehensive evaluations, including physical examinations, imaging studies (like MRI or CT scans), and nerve conduction tests, to determine the extent and location of nerve damage.
Treatment Planning: Based on the diagnosis, paralysis doctors develop personalized treatment plans tailored to each patient's needs and goals. Treatment may involve a combination of medication, physical therapy, occupational therapy, speech therapy, assistive devices, and other interventions aimed at managing symptoms, preventing complications, and promoting recovery.
Medication Management: Paralysis doctors prescribe medications to address symptoms associated with paralysis, such as muscle spasms, pain, stiffness, and bladder or bowel dysfunction. They monitor medication efficacy and adjust dosages as needed to optimize symptom control and minimize side effects.
Rehabilitation: Paralysis doctors coordinate multidisciplinary rehabilitation programs to help patients regain function, independence, and quality of life. Rehabilitation may include physical therapy to improve mobility and strength, occupational therapy to enhance daily living skills, and speech therapy to address communication and swallowing difficulties.
Assistive Devices: Paralysis doctors prescribe and facilitate the use of assistive devices and mobility aids, such as wheelchairs, walkers, braces, and prosthetics, to enhance mobility and facilitate independent living.
Education and Support: Paralysis doctors educate patients and their families about the underlying condition, prognosis, treatment options, and self-care strategies. They provide emotional support, guidance, and resources to help patients cope with the physical, emotional, and social challenges associated with paralysis.
Monitoring and Follow-Up: Paralysis doctors closely monitor patients' progress throughout the treatment and rehabilitation process, adjusting interventions as needed to optimize outcomes. They schedule regular follow-up appointments to assess functional improvements, address concerns, and provide ongoing support and guidance.
If you or anyone you might know is searching for the Best Paralysis Doctor In Kandivali, then you don’t have to worry about anything at all because New Wins Hospital is here at your service.
About New Wins Hospital
New Wins Hospital is one of the leading names because it offers a wide range of neurological treatments. The hospital has access to the latest tools and technology and ensures that everything is done as per the guidelines.
Credit:- https://penzu.com/p/762ab58736e233d7
1 note
·
View note
Text
How Long Does Physical Therapy Take?
Physical therapy is a crucial aspect of healthcare, helping individuals recover from injuries, surgeries, or manage chronic conditions. If you’re considering physical therapy, one of the most common questions you might have is, “How long does physical therapy take?” The answer to this question isn’t one-size-fits-all, as the duration of physical therapy varies depending on several factors. In this blog post, we’ll explore the factors that influence the duration of physical therapy, what to expect during your rehabilitation journey, and how you can maximize the benefits of this essential healthcare service.
Nature of Your Condition
The duration of physical therapy is heavily influenced by the nature and severity of your condition. Some injuries or medical conditions may require only a few sessions of therapy, while others may necessitate several months of consistent rehabilitation. Here are a few examples to illustrate this point:
a. Acute Injuries: If you’ve suffered a minor injury, such as a sprained ankle or a muscle strain, your physical therapy may last for just a few weeks. These injuries typically respond well to therapy and heal relatively quickly.
b. Post-Surgery Rehabilitation: After certain surgeries, such as joint replacements or ligament repairs, you may require an extended period of physical therapy, often spanning several months. The intensity and frequency of your therapy sessions will depend on your surgeon’s recommendations and your progress.
c. Chronic Conditions: Individuals dealing with chronic conditions like arthritis or neurological disorders may need ongoing physical therapy to manage their symptoms and maintain functional mobility. This type of therapy can be indefinite and may last for years.
Treatment Goals and Expectations
The goals of your physical therapy can significantly influence its duration. Typically, physical therapy aims to achieve the following:
1. Pain Relief: If your primary goal is pain relief, you may experience relief relatively quickly, often within the first few sessions. However, maintaining this pain relief and addressing the underlying issues may take longer.
2. Restoring Function: For those looking to regain lost function, such as the ability to walk or perform daily activities independently, the duration of physical therapy may be longer, often spanning several months.
3. Preventing Recurrence: In cases where injury recurrence is a concern, physical therapy may continue for an extended period to strengthen the affected area and reduce the risk of future injuries.
How Long Does Physical Therapy Typically Take?
While the duration of physical therapy varies from person to person, certain general guidelines can give you a rough idea of what to expect:
1. Short-Term Conditions/Injuries: For minor injuries or conditions like a sprained ankle, a few weeks of physical therapy (approximately 4–6 weeks) may be sufficient to regain full function.
2. Intermediate Duration: Conditions like post-operative rehabilitation or moderate injuries might require several months of therapy (3–6 months) to achieve optimal results.
3. Long-Term or Chronic Conditions: Chronic conditions or severe injuries, such as spinal cord injuries or degenerative diseases, may necessitate long-term or ongoing therapy that can last for a year or more.
It’s essential to remember that these timelines are general estimates and that your individual progress will depend on various factors, including your commitment to the therapy plan.
Average Healing Times for Different Types of Tissue
The length of healing time depends on the various affected tissues and body parts. The average healing times for various tissues are as follows:
Muscle: 2–4 weeks
Tendon: 4–6 weeks
Bone: 6–8 weeks
Ligaments: 10–12 weeks
Cartilage: up to 12 weeks
Benefits of the Physical Therapy
Physical therapy, a combination of functional exercises and education about the way your body moves, has a wide array of benefits:
Pain relief: Physical therapy helps reduce pain from injuries or chronic conditions.
Improved mobility: Exercises and techniques enhance flexibility and range of motion.
Injury prevention: Customized routines can prevent future injuries.
Enhanced function: Rehabilitative exercises restore physical function.
Non-invasive: Avoids surgery or medication for many conditions.
Holistic approach: Addresses the root causes of issues.
Better posture: Corrective exercises can improve posture.
Stroke recovery: Helps regain lost abilities after a stroke.
Sports performance: Tailored programs boost athletic performance.
Chronic condition management: Offers relief for arthritis, diabetes, and more.
Stress relief: Physical activity releases endorphins, reducing stress.
Improved quality of life: Enhances daily activities and independence.

In conclusion, the duration of physical therapy varies from person to person and depends on numerous factors. OrthoMiami recognizes this and tailors its physical therapy programs to meet the specific needs of each patient. While some individuals may require only a few weeks of therapy, others may need several months or even ongoing treatment. The key is to trust the guidance of experienced physical therapists, commit to the process, and work towards achieving the goals of rehabilitation. Ultimately, the goal of OrthoMiami and other reputable healthcare institutions is to help patients regain their mobility, reduce pain, and improve their overall quality of life through effective physical therapy.
0 notes
Text
The four principles of rehabilitation and why goal-setting is so important for success.
Rehabilitation was founded on the philosophy that every individual has equal and full rights to be in charge of their health along with their complete inherent worth. It’s founded on the philosophy that every person is viewed as a unique, comprehensive and holistic entity. Simply put, this means that successful rehabilitation is tailored to the individual – there’s no ‘one size fits all’ approach. This means that the rehabilitation team is responsible for providing all the essential knowledge, training, and skills to their patients to help them reach their rehabilitation goals. This article highlights the 4 main principles of rehabilitation and explains the necessity of goal-setting to make rehabilitation successful.
Time
Broadly, time is important in rehabilitation. Studies show that starting the rehabilitation process early can reduce the risk of readmission for conditions like spinal cord injury, stroke, chronic obstructive pulmonary diseases, and more. Since they treat the patient as an individual entity, the timeline will differ from case to case. So, the right times for commencement and duration of treatment need to be considered and tailored to each case.
Educate
As with most processes, rehabilitation is not a quick-fix which means proper education and guidelines should always be provided to the patient and their support system in each case. This is so they’re prepared for the journey ahead and the people around them know how best to support them. It’s also important to work with them and their expectations so you can set SMART goals that reflect this. Ensuring patients are fully informed and educated on the process allows them to feel a sense of control over their health which can improve morale, make them feel more independent and keep the rehabilitation process centred around the patient.
Emphasize abilities
Rehabilitation provides patients with a more optimistic approach to their treatment, which is so important, especially in patients who have suffered multiple health-related setbacks. It’s all about what they can gain as opposed to what they’ve lost. Having clear and focused SMART goals can help keep patients focused on how their lives will improve instead of dwelling on what they’ve lost from their illness or injury.
Treat the whole person.
Rehabilitation goal management takes a holistic approach and focuses on the particular issues a patient is facing. It ensures focus is kept on treating the person and not the disease. It takes into account a person’s preferences, culture, plans, religious beliefs, background, physical abilities, psychological states, social support and more. This ensures that the rehabilitation team can give them the best possible care for them as an individual.
Why is setting goals important?
Rehabilitation is a long and complex process that changes from patient to patient; it takes a village! Therefore, having clear and structured goals can help improve patient mindset, enable loved ones to know what support to give and allow the rehabilitation team to know what parts they play.
This can be so stressful for healthcare professionals, especially when consulting across multiple departments. We understand this and that’s why we created Goal Manager. It’s the gold-standard in goal setting and makes these processes so much easier and secure.
If you have any further concerns regarding rehabilitation and the goal management software, make sure to connect with Goal Manager as their experts are always there to help you along the way! You can also download a free demo here.
If you found this article helpful, make sure to share it with someone else you think it could benefit.
0 notes
Text
A reporter recently asked me about what harm I may have caused as a pain management physician who prescribes opioids. As I reflected on my last 10 years in this field, my response was that the harms I may have caused were because I underprescribed these drugs, not overprescribed them.
I thought of a 25-year-old patient, I’ll call him John, whose sciatic nerve was crushed in a motor vehicle accident, causing excruciating pain in his leg. We knew this would be a life-long injury, and that he would likely have to live with chronic pain. We tried everything I could think of — nerve medications, mindfulness techniques, desensitization, rehabilitation techniques, cognitive therapy, nerve blocks, and spinal cord stimulation — except opioids. John continued to suffer immensely from the debilitating pain, and eventually died by suicide.
Did he die because I undertreated his pain due to my own fear of prescribing chronic, potentially high-dose opioids in a young patient? I cannot know, but I worry and fear that this may be true.
In 2016, the Centers for Disease Control and Prevention published prescribing guidelines for opioids. Though intended to encourage best practices in opioid prescribing, these guidelines fueled providers’ fears of opioids and led to many clinicians abandoning patients who relied on opioids for pain relief. Although even pain specialists like me share fears and doubts about what role these medications play in managing chronic pain, so-called legacy patients are not the same as those who have never taken opioids before, as a colleague and I explained in The New England Journal of Medicine. (Read more at link)
505 notes
·
View notes
Text
Iris Publishers - World Journal of Yoga, Physical Therapy and Rehabilitation (WJYPR)
Progress of Research on the Mechanisms by Which Yoga Contributes to the Rehabilitation of Chronic Low Back Pain
Authored by Xinyan Zheng
Introduction
Back pain is the most common human spinal disorder. It can be caused by lesions in the skin, subcutaneous tissue, muscles, ligaments, spine, ribs, spinal cord, and meninges. Low back pain typically manifests in the lower lumbar spine and lumbosacral and sacroiliac regions. It is usually dull and tingling, with local tenderness and/or radiation along the lower extremities. It is often accompanied by inadequate movement capability, pitching inconvenience, lack of weight-bearing ability, walking difficulty, and/or limb fatigue. More severe symptoms are forward lumbar bending, back extension, scoliosis, and spinal deformity. The 3-month prevalence rate of low back pain is estimated to be 25%, and the lifetime prevalence rate is estimated to be as high as 84% [1-3]. Low back pain poses a great societal and economic burden, as it is related to a decline in work efficiency, poor quality of life, and high medical costs [4]. Its treatment forms the largest category of medical claims (20–25%) [5], with direct medical costs exceeding $34 billion annually [6].
Chronic low back pain (CLBP), Defined as low back pain persistence for >3 months [7], can be caused by
• Traumatic, degenerative (spinal stenosis), and inflammatory conditions.
• Paravertebral soft-tissue diseases and lumbar muscle degeneration.
• Stimulation of the spinal cord and spinal nerve root, spinal cord compression, or acute myelitis.
• Visceral diseases (e.g., pleurisy, pyelonephritis).
• Mental factors or chronic fatigue syndrome.
• Occupational factors (e.g., excessive bending/twisting, restrictive work position, vibration, heavy physical labor, monotonous repetitive work) and insufficient leisure activities.
Patients with CLBP can develop functional disability [8], sleep disorders, fatigue, and drug abuse [9]. CLBP is the most common cause of large workday losses and disability claims [10]. About 1% of the American population (men and women) has chronic disability due to low back pain [11].
The pathogenesis of CLBP involves mechanical instability and inflammatory factors that stimulate nerve endings. Spinal instability means that under a normal physiological load, the spine cannot maintain the normal interbody anatomical relationship without secondary injury to the spinal cord or nerve root, and without pain or dysfunction caused by structural changes (deformities). Many studies have confirmed the relationship between proprioceptive disorder and CLBP
The rehabilitation of chronic pain, considered as a chronic disease, should rely greatly on patients’ self-management, with family and social support [12]. Most patients depend on their doctors and lack relevant guidance after leaving the hospital, especially with regard to back rehabilitation exercises. Current treatments for CLBP include bed rest, medication, traction, local closure, physiotherapy, and exercise therapy [13]. Poor self-management behavior is the main factor affecting CLBP rehabilitation outcomes, leading to recurrence. Exercise and the maintenance of a certain lower-back activity range are considered to effectively reduce pain intensity and to improve the functional status of patients with CLBP, and exercise is commonly advocated as a first-choice treatment [14-16]. Indeed, a recent clinical practice guideline from the American College of Physicians strongly recommends exercise therapy interventions for CLBP [17]. The best form and duration of such exercise, however, remain open questions.
Yoga originated in India thousands of years ago and has become popular throughout the world; about 14.9 million people in the United States practice yoga [18]. Yoga provides a self-correcting, holistic approach to health and has been shown to be effective for several chronic lifestyle-related diseases, such as osteoarthritis [19], rheumatoid arthritis [20], essential hypertension [21], bronchial asthma [22,23], irritable bowel syndrome [24], diabetes [25], arterial disease [26], and depression [27]. It is an increasingly common and effective treatment for pain and related disabilities [28,29], including chronic muscle pain–related diseases [30] such as CLBP. In recent years, the use of complementary alternative medicines (CAMs) has increased by nearly 10%; back pain is the most common cause of use [31], and yoga is among the most common CAM activities [32,33]. In the 2002 National Health Interview Survey on supplemental and alternative medicines, more than 10 million American adults reported the use of yoga for health reasons; 10.5% of yoga practitioners reported that they used yoga for musculoskeletal diseases, and 76% reported that yoga was helpful [34]. Thus, an understanding of the effect of yoga on CLBP rehabilitation could use the design of yoga-based interventions to reduce or treat CLBP.
Characteristics and Effects of Yoga
Yoga is composed mainly of breathing, postures, and meditation, leading to smoothing of the whole-body meridian Qi, improvement of blood circulation, gland stimulation to balance secretion, function-activating visceral massage, nerve relaxation, muscle extension, flexibility development, enhanced immune system function [35],increased antioxidant defense enzymes and promotion of the delay of cell aging [36]. Yoga can improve the electrical activity of brain cells, which is conducive to brain control, and adjust the functions of various viscera, especially those of the endocrine system [37]. Yoga practice can thus benefit a wide range of people. The difficulty and amount of yoga exercise are easy to control, and yoga has low facilities and equipment requirements. Consistent yoga practice can improve fitness, temperament, and mood [22]. With the acceleration of the speed and complexity of life, yoga is regarded as a part of the new “green” lifestyle, adopted by increasing numbers of people as a light inner- and outer-body fitness technique.
Controlled yogic breathing balances the autonomic (sympathetic) nervous system and reduces habitual muscle and skeletal tension, thereby reducing fatigue and stress [38,39]. Yogic breathing differs from usual superficial breathing in that it is deep, slow, uniform, and rhythmic, involving the larynx, thorax, and abdomen, and thus diaphragmatic movement. The alveolar ventilation volume reaches 5100 ml/min, much higher than that of normal breathing. Breath-adjustment exercises accompanied by appropriate music can help the practitioner to enter a stable and quiet state, improve consciousness and muscle perception, and enhance nerve control ability for the respiratory and muscular systems, thereby preparing him or her for physical and mental exercises. Yoga posture practice is a delicate and slow process involving twisting, squeezing, stretching, and pulling. It starts with simple postures that gradually develop practitioners’ physical perception and motor ability. Yogic movement enriches the blood supply and flow to deep tissue, improving microcirculation [37]. Meditation is a key part of yoga practice; it helps the practitioner concentrate, so that the brain can understand the world more clearly and feel subtle changes in the body.
Lemay et al. [40] found that the performance of mindfulness exercises at least once a week alleviated college students’ stress and anxiety. Indian medical experts have found that yoga postures have positive effects on blood glucose control and nerve conduction and can reduce the clinical neuropathy of H-deficiency diabetes [41]. In a study conducted in Thailand, yoga reduced blood pressure in hypertensive patients [42]. Yoga also has a positive effect on the treatment of stubborn obstructive diseases, it has been reported that women who often take part in yoga have a 30–40% reduction in the incidence of breast cancer [43].
Research on yoga for CLBP rehabilitation
Many studies have demonstrated that yoga plays an important role in CLBP rehabilitation. In a systematic analysis, Posadzki P et. al [44] showed that yoga reduced CLBP significantly more effectively than did conventional exercise. Michael et al. [45] compared the effects of yoga and Qigong as rehabilitation training for patients with CLBP. The results showed that participating in a 3-month yoga or qigong program did not improve chronic back pain, back function and quality of life during a 3- or 6-month period. Keosaian, et al. [46] explored the experiences of low-income minority adults taking part in a yoga dosing trial for chronic low back pain that has the potential to favorably impact health in a predominantly lowincome minority population. It confirmed that yoga is an effective multidimensional treatment for CLBP. Patricia, et al. [47] showed that yoga significantly reduced pregnancy-related low back pain. Goode, et al. [48] drew an evidence map for the efficacy of yoga for CLBP, evidence suggests benefit of yoga in midlife adults with non-specific CLBP for short- and long-term pain and back-specific disability, but the effects of yoga for health-related quality of life, wellbeing and acute LBP are uncertain. Without additional studies, further systematic reviews are unlikely to be informative. Williams, et al. [49] compared the effects of Iyengar yoga and standard medical care as rehabilitation training for adults with CLBP; after 6 months of treatment, yoga had improved functional disorders, pain intensity, and depression, and reduced analgesic use, compared with the control group. Sherman, et al. [50] found that when compared to a self-care book, 12 weekly 75-minute Viniyoga classes resulted in both statistically and clinically significant improvements in functional status but when compared to conventional therapeutic exercises, were statistically significant but not clinically important. Padmini Tekur and others [51] found that short-term intensive comprehensive yoga training reduced pain and dysfunction, and increased spinal flexibility, in patients with CLBP.
Mechanism of yoga’s contribution to CLBP rehabilitation
Through progressive stretching and twisting posture exercises, yoga can alleviate lumbar muscle spasm, release adhesion, enhance lumbar spine stability, and increase the joint range of motion [52]. It has been found to increase hip flexion and spinal and hamstring flexibility in patients with low back pain [53,54]. The coordination of breathing and posture exercises enables the inhaled energy to reach the deepest tissues, resulting in musculoskeletal stretching, increased capillary opening, improved blood supply, and promotion of oxygen and metabolite transportation; further strengthening exercise can provide more abundant oxygen to all tissues of the body, increasing the oxygen content of blood and purifying it [52], thereby improving the blood supply and metabolism of the waist soft tissue.
The mechanism by which yoga relieves pain, however, is not completely clear. It may be related to decreased nerve or physiological sensitivity of painful tissue or to a change in the adaptability of compressed tissue. Harte [55] found increased endorphins and enkephalin in yoga practitioners, with the release of these analgesic substances effectively alleviating pain.
From the perspectives of biomechanics and anatomy, yoga can strengthen the lumbar extensor muscles (including the polyfidus and sacrospinal muscles) and abdominal muscles, providing support for the spine; spinal twisting stimulates the intervertebral discs and articular capsules, stretch in the direction of rotation promotes spinal rotation and vertebral mobility, and polyfidus muscle contraction–reduction–relaxation cycles comprise effective training. These effects conform to the principles of strength training and muscle stretch [56]. Yoga exercises effectively maintain overall spinal stability and flexibility, reduce the pressure between vertebral bodies, and correct slight displacements of the lumbar intervertebral discs and foramina. It can also ease nerve root compression, and alleviate or avoid common conditions related to CLBP, such as lumbar disc herniation. In addition, psychological effects of yoga can contribute to CLBP rehabilitation. Yoga can relieve depression, and fear [49]. Studies have shown that meditation can alleviate fear [57], enhance self-belief and improve the pain-coping ability of patients with chronic pain [7].
Matters Needing Attention in Yoga Practice
Reasonable yoga practice has a certain effect on CLBP rehabilitation, but unsuitable practice can be a source of injury. Attention must be paid to the following points in yoga practice. First, the dorsal (including lumbar) and abdominal muscles should be exercised at the same time to enhance the balancing of their strength, with consideration of the lumbar curvature and the size of sacral tilt.
Second, yoga posture practice should fully consider the practitioner’s flexibility, balance, and strength. Stretching should be performed gently and slowly, within the body’s limits and without excessive drag, to prevent muscle strain. The practitioner should explore and gradually understand the state of his or her body, pay attention to the anatomical characteristics of the correct positions, and protect the joints; exercise intensity should be increased gradually.
Third, the practitioner should focus on the feeling of the physical exercise, perceiving the effects of each action. Only by actively guiding the practice can physical and mental relaxation be achieved. Fourth, rehabilitation training plans to improve the physical fitness of corresponding muscle groups should be formulated scientifically according to the degree of CLBP, to establish the correct exercise mode. In addition, the practice should include full preparatory activities and post-exercise meditation to take full advantage of the adjustments and recovery of function achieved.
To read more about this article: https://irispublishers.com/wjypr/fulltext/progress-of-research-on-the-mechanisms-by-which-yoga-contributes-to-the-rehabilitation-of-chronic.ID.000521.php
Indexing List of Iris Publishers: https://medium.com/@irispublishers/what-is-the-indexing-list-of-iris-publishers-4ace353e4eee
Iris publishers google scholar citations: https://scholar.google.co.in/scholar?hl=en&as_sdt=0%2C5&q=irispublishers&btnG=
#International of Yoga#Journal of Rehabilitation#World Journal of Physical therapy and Rehabilitation#journal of physical therapy
1 note
·
View note
Text
Visit a Chiropractor After an Accident for the Best Treatment
There’s a reason why there are different doctors to look after different diseases and injuries. Every accident doctor in West Palm Beach has a specialization, and that skill is what makes each of them stand out. So, if you have got injured in an accident, you may need to visit both a medical doctor and a chiropractor. The former might not be able to provide treatment for your internal injuries. The latter might not be the best person for treating most external injuries.
Mistake People Make After an Accident
An accident will always cause an injury that may or may not be visible immediately after. If it’s not visible and doesn't cause pain, you may want to overlook it and get treatment only for the injury you can see or feel. If you don’t feel anything, you may not visit any doctor at all. This is the common mistake everyone makes. Over time, this mistake makes the injury worse, making you experience extreme pain and discomfort.
What You Must Do About It
Get the best treatment for any injury you incur. If it’s an external injury visit the best available doctor near you to get the wound treated. If it’s an injury that’s internal, visit a chiropractor near you. Either accident doctor in West Palm Beach will do their best to bring you back to health as soon as possible.
Internal Injuries Can Be More Complex
Since you can’t see them, you might think of them as a regular pain that will go away in a couple of days. But usually, it wouldn’t, especially if it was caused by an accident. The more you delay in getting to a doctor, the worse the injury will become. It could even become chronic, which will then stay with you for the rest of your life in some form. Do not wait to reach that stage. Get the affected area checked immediately after the accident to get the best treatment for it.
Injuries a Chiropractor Can Help With

● Whiplash: The sudden impact of the accident forces the head to move unexpectedly. This tears the fine muscles you have there in the neck and upper back area. You can know that it’s whiplash when your neck feels sore and you are unable to move it normally.
● Back Pain: More specifically, it is the lower back pain that happens most commonly as a consequence of a car accident. Such pain does not go away by itself. You need to undergo proper treatment and rehabilitation to recover completely.
● Neck and Shoulder Pain: Stiff neck or shoulders can happen when they are forced to move immediately due to the sudden impact. This throws their movement out of gear, leading you to feel discomfort when you try to move them. You may also feel a sense of headache or migraine due to the impact.
● Spinal Cord Injury: Your entire body depends on your spine for proper movement. If the spine is hurt or thrown out of its original position in some areas, you will feel excruciating pain. Bracing or alignment sessions may be needed to push the spine back into its original position.
● Sore Muscles: You will definitely experience soft tissue sprains after getting injured in an accident. A chiropractor will determine the root cause of why you continue to feel the pain before treating it accordingly.
The number of sessions you will need with a chiropractor depends upon the severity of the problem, and how your body copes with it. You may also have to follow certain guidelines and exercises while the treatment is going on. Following the chiropractor’s advice will help you regain your lost health in no time.
Speak to your nearest accident clinic in West Palm today to know more.
0 notes
Text
Read Online Nsca's Essentials of Personal Training DOWNLOAD EBOOK PDF KINDLE
Read Online Nsca's Essentials of Personal Training DOWNLOAD EBOOK PDF KINDLE
Nsca's Essentials of Personal Training

[PDF] Download Nsca's Essentials of Personal Training Ebook | READ ONLINE
Author : Jared W. Coburn Publisher : Human Kinetics Publishers ISBN : 0736084150 Publication Date : 2011-10-27 Language : Pages : 696
To Download or Read this book, click link below:
http://read.ebookcollection.space/?book=0736084150
Download [PDF]
Synopsis : Read Online Nsca's Essentials of Personal Training DOWNLOAD EBOOK PDF KINDLE
Comprehensive and research based, the second edition of NSCA's Essentials of Personal Training is the resource to rely on for personal training information and guidance. With state-of-the-art knowledge regarding applied aspects of personal training as well as clear explanations of supporting scientific evidence,NSCA's Essentials of Personal Training, Second Edition,is also the authoritative preparation text for those preparing for the National Strength and Conditioning Association's Certified Personal Trainer (NSCA-CPT) exam.This essential reference was developed by the NSCA to present the knowledge, skills, and abilities required for personal trainers. With contributions from leading authorities in the field, the text will assist both current and future personal trainers in applying the most current research to the needs of their clients:A discussion on nutrition outlines the role of the personal trainer in establishing nutrition guidelines, including the application of nutrition principles for clients with metabolic concerns.The latest guidelines on client assessment from prominent organizations--such as the American Heart Association (AHA) and Centers for Disease Control and Prevention (CDC)--keep personal trainers up to speed on the latest assessment protocols.New information is presented on flexibility training and cardiovascular exercise prescription as well as a discussion of research on the effectiveness of stability ball training.Revised information on design of resistance training programs incorporates the latest information on the application of periodization of training.New information addressing injuries and rehabilitation prepares personal trainers to work with clients with special concerns such as orthopedic conditions, low back pain, ankle sprains, and hip arthroscopy.New guidelines for determining resistance training loads will assist those whose clientele includes athletes.A variety of fitness testing protocols and norms allows readers to select from several options to evaluate each component of fitness.A new instructor guide and image bank aid instructors in teaching the material to students.NSCA's Essentials of Personal Training, Second Edition, focuses on the complex process of designing safe, effective, and goal-specific resistance, aerobic, plyometric, and speed training programs. Featuring over 200 full-color photos with accompanying technique instructions, this resource offers readers a step-by-step approach to designing exercise programs with special attention to the application of principles based on age, fitness level, and health status. Using comprehensive guidelines and sample clients portrayed in the text, readers can learn appropriate ways to adjust exercise programs to work with a variety of clients while accommodating each client's individual needs.Personal trainers will appreciate the book's presentation of detailed exercise programming guidelines for specific populations. Modifications and contraindications to exercise are given for prepubescent youth, older adults, and athletes as well as for clients who are overweight or obese or have eating disorders, diabetes, heart disease, hypertension, hyperlipedimia, spinall cord injury, multiple sclerosis, and cerebral palsyIn addition, the book provides clear, easy-to-understand guidelines for initial client consultation and health appraisal.For those preparing for the NSCA-CPT exam, this second edition features new and revised study questions at the end of each chapter. These questions are written in the same style and format as those found on the NSCA-CPT exam to fully prepare candidates for exam day. For efficient self-study, answers to study questions and suggested solutions for the applied knowledge questions are located in the back of the text. Chapter objectives and key points provide a framework for study and review of important information, while sidebars throughout the text present practical explanations and applications of scientific concepts and theory.The second edition of NSCA's Essentials of Personal Training is the most comprehensive resource available for current and future personal trainers, exercise instructors, fitness facility and wellness center mangers, and other fitness professionals. Unmatched in scope, this text remains the leading source for personal training preparation and professional development.
0 notes
Text
Juniper Publishers- Journal of Physical Fitness, Medicine & Treatment in Sports
Effects of Motor Imagery Techniques in Children with Spastic Cerebral Palsy- Juniper Publishers
Introduction
Cerebral palsy is not an ailment, its impairment. Cerebral palsy is somewhat a clinical explanation and do not identify the nature of illness as the term indicates nothing regarding etiology, pathology or expected recovery time. The brain insults are important for cerebral palsy and can happen at any moment in the beginning of 1st trimester of infancy; so, it is a broad term that covers a lot of etiologies and pathologies and its clinical details are manifold. So, cerebral palsy is a clinical syndrome that presents as a disorder in the development of postures, balance, coordination and movements due to lesion of immature brain occurring in the foetal period or infancy. The appearance of cerebral palsy can be comprehensive, psychological and physical disability or secluded instabilities in gait, perception, development or perception. The result is motor or sensory nerve disorders and the incapability to accomplish many tasks in everyday life and participation restriction. CP causes damage to motor or sensory nerves, functional limitation and impaired performance of daily life activities [1]. Cerebral palsy patients do lack in motor planning and execution of motor task. Motor dysfunction in cerebral palsy is usually associated with disabilities in sensory consolidation and stability, weak muscular contractions, weak or totally absence of motor planning which is the prerequisite of a motor task execution.
Moreover, simultaneous stimulation of prime movers and its associated opponent muscles, absence of particular regulation of movement in organisms, and reduced anaerobic muscle capacity and activity cause impaired functions and tasks restriction. Patients with this neurological disorder usually have worse dynamic and static balance. Overhaul services have commonly been ignored. Generally, exist inside the well-being sector. It is especially because of deficiency of complete guidelines. Cerebral palsy rehabilitation centers are very necessary to combat this deficiency. Even many clinical institutes give proper guidelines and treatments for cerebral palsy but still it is deficient and oldfashioned. Even patients can expire due to the devastating effect of bodily impairment, but it is in very exceptional and intensive cases. New treatments need to be established in response to impairments. So, this study is going to evaluate a unique and rare technique to treat and rehab gross motor manifestations especially of motor planning deficit and balance impairments in cerebral palsy. During the previous decade, the usage of databased interventions in cerebral palsy regimen has moderately increased and researchers have struggled to evolve further productive interventions to raise the standards of living of these individuals and their households.
A latest analysis has investigated that interventions established on motor learning improves functional levels in children with cerebral palsy [2]. Therefore, using Motor Imagery Techniques in CP might be a promising technique to ensure improvement in motor planning deficit. Motor imagery is the cognitive presentation of movement in the absence of any bodily movement. Profuse verification on the beneficial influence of motor imagery implementation on motor presentation and training in sportsperson, fit people, and individuals having neurological problems (e.g., stroke, spinal cord injury, Parkinson’s) has brought out. Imagery refers to the creation or re-creation of any practice in the mind like auditory, visual, olfactory, kinesthetic, organic. Specifically; motor imagery (MI) is the mental representation of movement without any body movement. It is a complex mental operation that is selfgenerated using sensory and perceptual processes, enabling the reactivation of specific motor actions within working memory. Therefore, sensory-perceptual, memory, and motor mechanisms are included in broader definitions of the term.
Motor imagery is the mental imagination of movement without any actual body movement. It is a mental activity by which an individual rehearses, or replicates a given action. It is mostly used in sport training as mental practice of action and also in neurological rehabilitation. Motor imagery is likely to develop more ‘cognitive’ aspects of motor behavior, and may, therefore, be helpful in promoting motor planning in patients with CP [3]. Several evidences show that motor imagery and actions are conveyed by the same brain circuits. For example, functional neuroimaging and transcranial Magnetic Stimulation studies demonstrate that the same brain structures are involved in action and imagining the same action. Functional brain imagines reviews have exhibited that many cortical as well as subcortical regions are triggered through definite motor performance, are equally triggered while imagination or cognitive execution of movements. Current verification shows that the primary motor cortex is associated with motor imagery procedure [4].
During motor imagery, many neural mechanisms are activated characterized by a marked elevation in tendinous reflexes of the limb part imagined moving, and by somatic variations which resembles with the level of mental work. At level of the cortex, precise planning of initiation narrowly looks like to the action executed, is noticed in areas concerned to motor control. This stimulation might oblige as the foundation for the special effects of mental training. A model that is called as, hierarchical model of the organization of action projected the temporary memory storage of a ‘copy’ of the many demonstrative stages. These retentions vanish when an action associated to the denoted goal takes place. By compare, if the act is partial or not performed, the entire system rest stimulated, and the content of the demonstration is experienced. This mechanism would be the foundation for conscious reach to this content during motor imagery and mental training [5].
By functional magnetic resonance imaging (FMRI) techniques, the intensity and latitudinal distribution of functional activation in the left pre and post central gyri, during actual motor performance (MP) and mental representation of selfpaced finger-to-thumb opposition movements of the dominant hand were investigated in fourteen right-handed volunteers [6]. For many patients, it is difficult or sometimes impossible to execute motor tasks, who have damaged central nervous system, even after initial involvement in an dynamic rehabilitation platform. It is lately offered by several investigators that these patients can use mental practice as a healing device to increase their motor functions, but very little experiential work reports this problem openly. This article deliberates the reason for inspecting mental practice for encouraging motor recovery in patients who have neurological syndromes. We first showed evidence that supports the presence of a resemblance between performed and imagined activities by using records from psychophysical, neurophysiologic, and brain imaging studies. Then this additionally describes the recurrence of movements through bodily and mental repetition of a mechanical skill. Lastly, a new model is suggested to focus the key role of motor imagery as a crucial method of mental rehearsal, and also to stimulate further research on this type of training in the restoration of patients with motor deficiencies having cerebral origin [7].
There is evidence to suggest that mental practice of movement can produce normal effects recognized as practicing the actual movements. Imagining hand movements could stimulate restoration and redistribution of brain activity, accompanied by recovery of hand function, thus resulting in a reduced motor impairment. Current evidence for mental practice with motor imagery (MI) in stroke is insufficient due to methodological limitations [8] (Figure 1). Mental practice is the intended preparation of mental tasks, whereas motor imagery practice results in motor improvement through motor imagery rehearsal. These both italicized terms are sometimes used interchangeably. So, we will treat them synonymously. MI is cheapest and easily available. It is necessary for physical therapist to be informed about the use of MI, because of increasing number of reports about its benefits of MI in improving motor performance [9]. Mental Rotation Task / Paradigm is a tool to assess the child’s ability of mental imagery. It is process of imagining an object rotating in three dimensional spaces. Person is asked to decide if these two figures are the same shape but rotated or they are two different shapes [10] (Figure 2).
Methodology
Randomized clinical trial was conducted in department of physical therapy of National Institute of Rehabilitation Medicine, Islamabad, for duration of 6 months. 30 patients with diagnosed with spastic Cerebral Palsy, then 22 participated in this study according to inclusion and exclusion criteria. After selection of patients who fulfilled inclusion criteria, they were arbitrarily divided into two groups by means of simple lottery method. i.e. Control group n=11 and Interventional Group n=11. Baseline assessment was done on 0 week; second Assessment on 4th week Post-intervention assessment was done after 8 weeks. Total duration of study treatment was 12weeks. The experimental group performed motor imagery training as specific intervention, that involves motor imagining of gross movements of lower limb 15 min. embedded in conventional therapy for 30 min. (45 min/day, 3 times/week). And, the control group was given conventional therapy only (30 min./day, 3 times/ week).
The interventional group received Motor Imagery training along with conventional therapy. In MI, a small animated Video clips were designed to display and guide the child through imagery process. Motor Imagery Training involves imagining task with external visual stimulus, given via short video clip i.e.
i. Football playing
ii. Running a race
iii. Balancing on one leg
iv. Keeping balance on a wobble board
v. Jumping from block to block
The control group received Conventional Physical Therapy only including,
a) Therapeutic Ball Exercises
b) Balance Board Training
c) Stretching Exercises
d) Recreational activities.
Results
The Results of both tools TUF and MFR are significant indicates that Motor Imagery is an effective technique to improve balance and gross motor skills in Spastic Cerebral Palsy whereas tool GMFM results are non-significant indicating that this intervention techniques are not that much effective in case of cerebral palsy.
Overall, the Mean age of all patients was 9.36±3.170. and in control group mean and standard deviation values were 9.36±2.730 and in experimental group 9.36±3.695 were mean and standard deviation values. There were 77.3% male and 22.7% female in the study. In experimental group 72.7% were male and 27.3% female and in control group 81.8% were male and 18.2% female. In general, 31.8% patients were diagnosed with spastic hemiplegic CP (Rt), 22.7% patients with spastic hemiplegic CP (Lt), 27.3% patients with spastic diaplegia while 18.2% patients with Spastic quadriplegia. In experimental group, there were 27.3% of patients were diagnosed with spastic hemiplegia (Rt), 18.2% patients with spastic hemiplegic CP (Lt), 36.4% with spastic diaplegia while 18.2 % were with Spastic quadriplegia. In control group, there were 36.4% of patients were diagnosed with spastic hemiplegia (Rt), 27.3% patients with spastic hemiplegic CP (Lt), 18.2% with spastic diaplegia while 18.2% were with Spastic quadriplegia.
Then, by relating Q-Q PLOT normality of data was checked, to recognize normal distribution of the data Kolmogorov-Smirnov test indicated that data were not normally distributed for Time up and go test (TUG) test and Modified Functional Reach (MFR) at baseline. Nonparametric test that is Mann Whitney U- Test for between group analysis and wilcoxon test were applied on both TUG and MFR test, but for GMFM-IS66 Independent T test was applied for between group analysis and Repeated measure anova for analysis of time interval within each group was applied for. These tests were used to compare Pre and Post Treatment of between Group A and B. As, the data for TUG and MFR was nonnormally distributed at the baseline so Mann Whitney U Test was applied to compare the all three assessment values between control and experimental group (Tables 1-3).
Discussion
All patients with hemiplegia have difficulty with planning motor movements, Effect of motor imagery on hemiplegic cerebral palsy and on Developmental Congenital Disorder and concluded that anticipatory motor planning was improved by this intervention [11]. Results of this study were supported by the study, In 2013 by Bert Steen Bergen et al., on ‘Impaired motor planning and motor imagery in children with unilateral spastic cerebral palsy’ concluded that Motor imagery training may be a valid and useful tool to complement upper limb rehabilitation in young children with CP, supports researcher’s study as Motor imagery techniques were helpful in increasing balance and gross motor function of children with cerebral palsy and showed significant p value <0.005 [2]. According to another study in 2012 by Hwai-young Cho et al; on ‘Effects of motor imagery training on balance and gait abilities in post-stroke patients: a randomized controlled trial’ concluded that if gait training with motor imagery training is used it will recovers the balance and gait of chronic stroke patients more better then gait training alone, that supports researcher’s study as Motor imagery techniques were helpful in increasing balance and gross motor function of children with cerebral palsy and showed significant p value <0.005 [12].
According to another study in 2008 by Ayelet et al; ‘Home- Based Motor Imagery Training for Gait Rehabilitation of People With Chronic Post stroke Hemiparesis’ says that There were noteworthy rises in stride length, cadence, and single-support time of the pretentious lower limb, giving strength to my study as Motor imagery techniques were helpful in increasing balance and gross motor function of children with cerebral palsy and showed significant p value <0.005. According to another study in 2009 by Bert Steenbergen et al; on ‘Motor imagery training in hemiplegic cerebral palsy: a potentially useful therapeutic tool for rehabilitation’ gives that Motor imagery training may be a valuable additional tool for rehabilitation in children with hemiparetic CP giving strength to my study as Motor imagery techniques were helpful in increasing balance and gross motor function of children with cerebral palsy and showed significant p value <0.005 [11]. In 2012, a study by Hwai Young Cho et al., concluded that gait training along with motor imagery training increases the balance and gait capabilities of chronic stroke patients suggestively better than gait training alone thus, giving strength to my study as motor imagery techniques were helpful in growing balance and gross motor function of children up with cerebral palsy and revealed significant p value <0.005.
Conclusion
The study results concluded that both treatment groups were improved by Physical Therapy. This study suggests that motor imagery techniques combine with conventional combination therapy has significant effects in improvement of gross motor functional skills of children with spastic cerebral palsy, age between 7 and 15 years. There was significant improvement in the balance level whereas, there was little increase in level of gross motor function. So, Motor imagery is an effective technique to improve motor planning and balance among cerebral palsy.
Acknowledgement
First of all I would like to pay tribute to Almighty ALLAH who helps me in all the even and odd situations during the completion of my research work, without His will I would never be able to do the research project. I would like to express my great appreciation to my research supervisor Dr. Mirza Obaid baig who helped me throughout my research project with his priceless and productive ideas; it was my great pleasure to work with an individual of intellect like him. Then I would like to pay gratitude to my parents without their sincere prayers I would never be able to achieve what I have today. Sincere thanks to all my friends and family members who prayed for me.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com
For more articles in Journal of Physical Fitness, Medicine & Treatment in Sports
please click on: https://juniperpublishers.com/jpfmts/index.php
For more about juniper publishers please click on: https://www.juniperpublishersgroup.com/
0 notes
Text
Tenure in HQ Southern Command, Pune
It was indeed nostalgic to return to Pune for yet another tenure after a long gap of 14 years, since my previous posting at NDA. I considered myself very lucky to get an opportunity for a Staff assignment in HQ Southern Command, which was certainly going to be a challenge. I was aware that it would be an entirely different exposure as compared to both my previous Staff tenures in the challenging environment inJ & K. On arrival in Pune in the last week of Jul 1996, we stayed in the Officers Mess of Army School of Physical Training for nearly three weeks. Thereafter, we shifted to a civil house on rent reimbursement basis since there was a waiting list for permanent accommodation. Meanwhile, we had to begin the procedure for school admission. Ashvini secured admission in Fergusson College while Nandini & Aditya got admission in Army Public School, Dighi. Thus, our children could resume the academic sessions in the new environment --- a social adjustment process which was so familiar for all of us.
On 01 Aug 1996, I reported in HQ Southern Command to take charge of my appointment as Col A. I was aware about the history of this oldest Command HQ which was raised at Pune on 01 Jul 1946. It had distinguished itself in several operations namely - Junagarh ( 1947 ), Hyderabad ( 1948 ), Goa ( 1961 ), Indo - Pak Wars of 1965 & 1971, Sri Lanka ( 1987 ) & Maldives ( 1988 ). Presently, Southern Command has jurisdiction over 9 States & 4 Union Territories. The Formation Sign depicts the constellation " CRUX"--- a cross formed by the brightest stars in the Southern hemisphere, pointing towards the South Pole. Hence, I felt privileged to be welcomed as a team member of this prestigious formation HQ.

My first impressions of the majestic architecture of the buildings in the office complex and my initial interaction with the Staff Officers of each Branch triggered positive vibes prior to beginning my innings. On the very first day, I was interviewed by Maj Gen Administration who welcomed me and expressed his confidence that I would be able to discharge my new responsibilities in a perfect manner with experience of previous Staff tenures in J & K. He gave out the schedule for my interaction with each Branch for each Arm / Service and thereafter with the General Staff ( GS ) Branch & Quarter Master General ( QMG ) Branch of the Command HQ.
I was also required to go for familiarisation visits to all the defence organisations dealing with the medical treatment and rehabilitation of battle casualties. These included the Command Hospital, Paraplegic Rehabilitation Centre ( PRC ), Queen Mary Technical Institute ( QMTI ) and Artificial Limb Centre ( ALC ). The visit to Paraplegic Rehabilitation Centre was a big revelation as I was briefed about their responsibilities towards rehabilitation of personnel of the three Services who were disabled due to Spinal Cord Injuries. The idea for such a facility was conceived after 1971 War and PRC was inaugurated on 20 Sep 1974. Over the years, it has expanded to cater for 117 beds & 34 family quarters. The patients are provided free lodging & boarding, medical treatment and vocational training. It is the largest centre of its kind in India, providing holistic and lifelong care for the bravehearts.
On completion of this familiarisation schedule which lasted one week, I learnt gradually about various office procedures, on case by case basis. It was very time consuming to carry out an in-depth analysis of all disciplinary proceedings, prepare a summary & put up the recommendations for final disciplinary award by the Army Commander. This process reinforced my knowledge about the legal procedures to be followed in accordance with the Army Act & Army Rules. Yet another aspect which was my responsibility was the planning and execution of all Ceremonial functions and welfare activities, in accordance with a calendar of events. In addition, I was entrusted with the financial management of Welfare funds of the Command HQ. It required consistent efforts to maintain the records of income & expenditure at this apex level. In addition, I was on the Board of Army Public School & Asha School which also entailed regular monitoring. Progress report of all these activities and future plans had to be presented by respective Staff Officers, in the monthly conference chaired by the Army Commander. It took me nearly two months , working well beyond the office timings, to settle down in my new role.
However, I still had to complete my initial visits to both the subordinate Corps HQ at Jodhpur & Bhopal. I got this chance when I was nominated in the Team for Annual Inspections which were scheduled in Oct/ Nov. It proved to be another useful interaction as I could observe different welfare activities in each Station and became aware about their new projects. Meanwhile, we were allotted our permanent accommodation -- 9 Victoria Road within Pune Cantonment. The House was in the" Open offer" category and required extensive repairs. On completion of the urgent repairs, we completed the familiar process of shifting and settling down in our spacious Bungalow. Our new residence was very close to the new location of Army Public School in Pune Cantonment. It was beneficial specially for Nandini & Aditya who started commuting to their School on cycles. Even Sanjivani was delighted to be appointed as the Principal of Nursery School run by AWWA. Gradually, we developed a jogging track around the front lawn of our house and created a kitchen garden in the backyard. We were fortunate as we celebrated Diwali along with our parents & close relatives, in our biggest residence so far in our career.
In view of the Diwali festival which was always celebrated centrally by the Fauji fraternity, I was detailed in the core Team for planning and conducting all the events in Pune Cantonment.The celebrations were planned over three days and began with a Fauji Mela organised centrally by all the Units and Defence Establishments. AWWA ( Army Wives Welfare Association ) was involved in this event. Next day we witnessed a splendid Equestrian Display at the Pune Race Course followed by a Band Display. The final event was a special performance by Anup Jalota which culminated with a magnificent Fireworks Display. The overall impact of all such celebrations contributed towards enhancing camaraderie.
Next month, I managed to avail a short vacation with my family and visited Sainik School Satara. It was a nostalgic feeling since I visited my Alma Mater after nearly three decades. This visit enabled a flashback of memories while the School laid the foundation of my journey in uniform for six long years. Thereafter, we visited Mahabaleshwar & Panchgani enroute to Pune. However, the memories which we always cherish were witnessing an impressive Passing Out Parade at NDA & all the preceding functions in Dec. It was specially nostalgic for myself & Sanjivani since we were returning to the "Cradle of Military Leadership", after a long gap of 14 years since my fabulous tenure as an Instructor at this prestigious Institution.
In Feb 1997, we organised a major Conference at our HQ. It was chaired by the Army Commander and attended by all the Corps Commanders & Area Commanders. In addition,all the Maj Gens of Command HQ with their Staff Officers attended the deliberations over three days.This Conference was a precursor to the Army Commanders Conference which was scheduled for one week at Army HQ in the month of Mar. I had been nominated for attending both these Conferences where I had to give a Presentation on all welfare activities. I felt really privileged to attend both these professional conferences to review, discuss and conceptualise strategic doctrine and formulate operational plans for different battle scenario. Personally, I got an opportunity to attend the Central AWWA Meet during which each Command summarised all the welfare activities in accordance with the motto of AWWA ---- "Asha, Vishwas, Aastha". It was an ideal forum for generation of new ideas and formulation of new plans for enhancing the quality of life of all ranks & their families including the ex-servicemen community.
On return from Delhi, I was assigned to be a member of a Team constituted for a new Project. It dealt with the establishment of Symbiosis Institute of Management Studies ( SIMS ) in Pune , exclusively for management education of children of Army personnel & for officers availing study leave. This idea had been conceptualised and approved earlier but work could commence only after the final sanction of funds in FY 1997/98. The Project was indeed challenging as it involved numerous mini Projects and activities concurrently. Main tasks were creation of academic infrastructure, construction of hostels and messing arrangements, selection of the Director & the Faculty, recruitment of non-teaching staff, finalisation of the Syllabus for PGDM Courses as per the guidelines of AICTE, formulating the admission process and other procedures. We got valuable advice from Prof Dr Mujumdar, the founder of Symbiosis University. Finally, the Institute started functioning within six months , from the location of Symbiosis School on Law College Road. However, construction project of permanent Campus continued and the Institution shifted to the new Campus at Range Hills later in 2002.
Simultaneously, I continued shouldering my responsibilities with greater intensity based on my learnings in the previous year. I got a chance to accompany the Army Commander for Civil Military Liaison Conference at Bangalore. This gave me a different exposure about planning of assistance to civil administration. Assistance to Asha School was another area of focus so as to improve the quality of education and care of special children. Additional equipment such as special wheelchairs and exercise equipment were also provided to the patients at Paraplegic Rehabilitation Centre.
In Jan 98, Nandini was excited to be selected in the Team to represent Army Public School, Pune for Debate Competition for all Army Schools scheduled at Dagshai, near Shimla. It involved lot of preparation and practice sessions under the guidance of the Principal while Nandini was simultaneously carrying out the final revision for her Board Exams of Tenth standard. It was her first competition in front of such a large audience. Their performance was adjudged the best and the Team returned with the Debate Trophy full of confidence.

Meanwhile, Sanjivani was selected as the Principal of Army Public School (Junior Wing ). This School had to be established abinitio at a new location near Pune Race Course urgently so that the academic session could commence in the new premises. It involved several activities simultaneously ---- renovation of an existing Gymnasium, creation of new classrooms, purchase of furniture, preparation of playgrounds and selection of Teaching & non-teaching staff. Sanjivani faced all these multiple challenges with total dedication and through constant interaction with different agencies. Finally, APS ( Junior Wing ) was born before the commencement of the Academic Session in Apr 98.
In the first week of Jun 98, I was pleasantly surprised to receive my posting order for an instructional assignment in Defence Services Staff College, Wellington. It was a coveted posting which was my dream while I was attending the Course in 1985/86. I had to report at Wellington in the first week of Jul. It was time for me to reflect on my valuable experience of two years as a Col A in Command HQ. I realised that I had benefited from so many diverse aspects and applied myself in all activities. In my farewell dinner , I expressed my gratitude to all the Staff Officers and all the Major Generals who were incharge of their respective Arm /Service. The guidance by the Army Commander proved to be really the icing on the cake. I bid adieu to the entire Team of Command HQ, hoping to meet again, sometime, somewhere in the Journey of Life!!!
0 notes
Text
Why have you called a car accident lawyer New York?
Car injuries are life-changing experiences. The crash may be an incredibly lengthy procedure of submitting a coverage claim, figuring out fault, and getting the closure one wishes to transport on with their life. And with the Physical disturbance, you cannot capably cope with this alone.

You suffered extreme accidents because of the negligent movements of a driver. A car accident lawyer New York can help you. They can help you via way of means of amassing proof, negotiating with the at-fault party, and making ready your case for court, if necessary.
Get the legal help:
A car accident lawyer New York assists you to obtain financial and non-financial damage from an at-fault coverage company. Economic damages will not forget all the monetary losses you have got suffered because of your harm, out of your clinical payments to the wages you misplaced while out of work. In contrast, non-financial damages can contain all your non-public damages, from emotional trauma to bodily pain.
With the proper lawyer, you could get better monetary repayment for the subsequent damages after a vehicle coincidence:
· Current clinical payments (along with ambulance and emergency room fees)
· Future clinical payments
· Property harm and loss
· Pain and suffering
· Physical remedy and rehabilitation costs
· Lost wages
· Loss of professional or incomes capacity
· Wrongful loss of life damages in case you misplaced a cherished one
Damages will come right down to the form of harm you have suffered and had legal responsibility policies. Brain accidents, for example, can reason various physical and mental accidents, consisting of temper swings and PTSD.
Even spinal cord harm, while it can now no longer affect your brain, can result in emotional troubles as you deal with your disability. To assure you get compensation, you may need a lawyer who can thoroughly overview your case and gather all to had proof to aid your claim.
Conclusion:
You have to take legal action since New York has stringent legal guidelines for the time you need to a lawsuit. If you do not take action during this period, your options for damages might be lost.
0 notes
Photo

What is a life care plan? . . If you have suffered a spinal cord injury there is no doubt that you will require ongoing rehabilitation, assistive devices and assistance as you age. The life care plan is a complex document, designed to meet the specific long-term needs related to all aspects involved in managing spinal cord injuries over time. . The plan is put together by a qualified life care planner, based on evidence based standards of care, research, clinical practice guidelines and recommendations from your treatment team to identify long-term rehabilitation needs, medical needs, vocational rehabilitation needs, psychological counselling needs, outlines the cost of durable medical equipment and assistive devices that you will need throughout the span of your lifetime, among other things. The costs of help and equipment set out in the life care plan is normally based on fees charged by service providers and vendors within your local community, and projected over the course of your life expectancy. . Read more at Hamitonlawyers.com or call us at 905-333-8888 to get help today. . . . #hamiltonlawyers #hamont #oakville #burlingtonontario #burlont ##keeprollin #wheelchair #wheelchairstyle #wheelchairlife #spinalcordinjuryawareness #wheelchairfitness #wheelchairsports #wheelchairman #spinalcordinjury #spinal #spinalcordinjuryrecovery #sciawareness #quadriplegia #paralysis #paraplegia #neurorehabilitation #injuryattorney #hamiltonhealthsciences #sci #dontstop #quadriplegic #paralysis #Quadriplegia #quad #Tetraplegia #Tetraplegic #para #WheelchairLife https://www.instagram.com/p/B5avMShp8zv/?igshid=jofkbmlmh6wl
#hamiltonlawyers#hamont#oakville#burlingtonontario#burlont#keeprollin#wheelchair#wheelchairstyle#wheelchairlife#spinalcordinjuryawareness#wheelchairfitness#wheelchairsports#wheelchairman#spinalcordinjury#spinal#spinalcordinjuryrecovery#sciawareness#quadriplegia#paralysis#paraplegia#neurorehabilitation#injuryattorney#hamiltonhealthsciences#sci#dontstop#quadriplegic#quad#tetraplegia#tetraplegic
0 notes
Text
medical marijuana card california
With a California medicinal marijuana card or a cannabis membership card California residents can legally acquire medical marijuana from any of the medical marijuana dispensaries within the state. So search for something like "Denver dispensary evaluation" or just "the best Denver dispensaries" and you should get you the appropriate results. Due to this fact, each dispensary has its personal brand and array of merchandise. Along with your card in hand, it’s now time to make your first medical marijuana dispensary. Most individuals choose to go to a medical marijuana dispensary with their prescription. Marijuana is just not solely very effective in treating a number of illnesses and diseases but it surely also has turn out to be a drug which is extraordinarily protected -- safer than most medicines prescribed every single day. Medical marijuana has been extremely profitable in the treatment of medical marijuana doctors all above-talked about diseases. Some states, together with Washington State, do not essentially concern a medical marijuana card. He joked "when I've seven-eighths of a gram of marijuana, I consider myself to be out of marijuana." He defined that he has a "medical marijuana" card issued in California.
Medical marijuana card guarantees to offer excessive degree services & fulfill their customer needs. Although the Florida Medical Marijuana Card application and qualification course of is irritating, My Florida Green has worked laborious to streamline the process, provide access to one of the best Medical Marijuana doctors, and safe patient information with HIPAA-compliant technology. If you’re a former member of the army, you may possibly be exempt from submitting an application for a CDL. Merely fill out our New Member Form and Affected person and Caregiver Waiver to grow to be a patient with Revolutionary Clinics. If a chosen caregiver is authorized to grow medical marijuana, they might develop exterior, but must adjust to the regulation. Any intent to renew after the expiration date would require a brand new utility for each you and your designated caregiver. If you'll somewhat full a physical utility than going the net route, you can download your affected person software proper right here.
With this card, you'll be able to see the physician at residence in your phone with our app. Other caveats: Cops operating your license will not be able to see that you're a patient, but they can use their very own senses to detect impaired driving or marijuana in a vehicle. Can just anyone see them? You'll be able to learn more about the various circumstances that medical marijuana is helping individuals such as you alleviate each day, click Qualifying Circumstances for Recommendation for more info. There are a lot of situations that are shared on most lists. Weedmaps and Leafly are both great resources for locating cannabis-pleasant physicians near you. Solely doctor accredited patients can use cannabis legally in California. Now, you still can’t grow your individual cannabis, but you should purchase it and devour it. If a patient has a health condition that will profit from the use of cannabis, the place would he or she find a list of medical marijuana docs?
We know it can be troublesome to seek out consistent and dependable professional medical marijuana docs in Colorado Springs and Pueblo. Know the legal guidelines on how caregivers can present help. Two state supreme courts have now so concluded (these surprised by Bourgoin likely both did not learn Coates, did not understand Coates, or forgot Coates). At this stage, it's now probably to attain the agreed quantities of medical marijuana dispensaries, amongst other things provided now in some international locations in the United States. Drying and shredding of the 'hemp' plant is how marijuana is produced. He should possess a medical marijuana license. If there's a cannabis therapy program in your state, studying learn how to get a medical cannabis card is important for benefiting from it. The actual fact that you've got a Registry Card is protected by State Regulation and you could choose to keep your possession utterly private. CBD is totally THC free and may be made use of for extensive pediatric care for kids and delicate adults too.
The Compassionate Use Act allowed for the enlargement of the MMP’s retailers and qualifying circumstances, but the DOH has not even begun the method for increasing this system. If you don’t mind paying a little more, their premium service will delve even deeper and produce a last report which is one of the detailed we have now encountered. However, it’s good to maintain the above in mind when making use of on your card. On the other hand, having a cannabis card eliminates the sales tax and the financial savings start to add up in a short time. Everybody pays different taxes, both straight or indirectly, together with a 15 percent state excise tax and pot-particular local taxes (four p.c on gross sales in Sacramento). Be an Illinois state resident with proof of residency. The net verification program doesn't disclose any information about our patients. GreenStar patients receive more than a physician advice, we assure patients will likely be educated by a highly credible employees. Some individuals will not feel that it helps them, and others will discover surefire relief from utilizing it. Notice: You'll have to pay a certification payment.

How to Get an Exception for the Use of Medical Marijuana When on Probation for DUI Is medicinal marijuana more advanced than prescription analgesics to managing chronic pain? Chronic pain overall constitutes the largest using medicinal marijuana. The opioid narcotics that are popular to take care of chronic pain, like codeine, morphine, oxycodone, and methadone, are potentially addictive. Chronic pain medications might end up bringing about tolerance which has a need of increasing dosage to maintain effectiveness. Low grade marijuana contains 1 to 3 percent delta-9-tetrahydrocannabinol (THC) which is what is typically sold recreationally. THC is well regarded because the most active psychoactive agent in marijuana. High grade marijuana known as sinsemilla contains 7 to 8 percent THC and hashish is between 7 and 20 percent. The most concentrated way of marijuana is hash oil that might contain up to 70% THC!

More than 10 % Americans over 65 years old can are afflicted by incontinence and ladies suffer in excess of men using this type of problem. Investigators at Oxford's Centre for Enablement in Britain reported within the February 2003 issue of the journal Clinical Rehabilitation that in comparison with placebo in patients being affected by MS and spinal cord injury, self-administered doses of whole plant cannabinoid extracts dramatically improved bladder control. These initial findings were followed up by investigators at London's Institute for Neurology inside a pilot and open-label study of medical cannabis or MMJ extracts for bladder dysfunction. A group of 15 patients with advanced multiple sclerosis were tested for that effect that medicinal marijuana had on the the signs of urinary incontinence. The medical advantages of cannabis cover a large scope of issues. It is utilized as being a strategy to nausea and excessive vomiting, together with stomach pain and cramping. It has recently been recognized to treat cancer patients and relieve intense pain caused by debilitating diseases or injuries. The most famous mention of fantastic can be used for glaucoma patients. These patients usually see a marked change in their personal health insurance frame of mind when using it as being a medication.
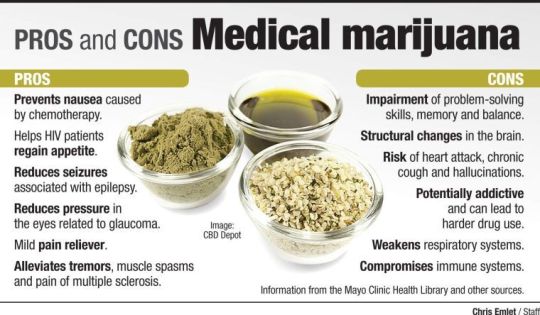
Provided that the cardboard holder is holding a valid card and abiding by the medicinal marijuana laws of their state - which vary from region to region slightly - they are afforded protection from legal prosecution for possessing medicinal marijuana. Most states have even created an electronic digital system for police officers to ensure that the card is valid, so that they don't arrest a lawfully biding patient that's within their legal rights to make use of this natural medicine. Patients who are marijuana medical card holders can possess, transport and make use of - and in some cases also grow - medical cannabis form of hosting usage; or their caregivers who employ a card are afforded similar protection under the law and protections, too.
0 notes
Text
Does A Personal Injury Lawyer In Victoria Provide An Array of Services In Quick Succession?
In addition to the regular wrongful death claims, automobile accidents, slip and fall cases, and catastrophic injuries, a Personal Injury Lawyer in Victoria has firm expertise in resolving insurance disputes. You’ll find that slip and fall injuries can surface anywhere. They involve malls, residences, retail stores, offices, and sidewalks and city pavements. If you feel that the mishap was due to the inactions or negligent actions of another person, you can talk to the seasoned lawyers to assess the situation and determine the liability of the other person. The lawyers provide seamless and sound legal advice. On many occasions, broken or chipped handrails or stairs, holes or crevices in parking lots, wet and slippery floors, faulty elevators and other such things lead to massive accidents.
Pedestrian accidents
When a motor-vehicle hits a pedestrian, the injuries are mostly severe. In the event of an automobile accident, a pedestrian can sustain several bruises and injuries, ranging from cuts and fractures to spinal cord and brain injuries. Many of these injuries are fatal. These types of accidents often necessitate extensive medical attention and rehabilitation. The hospital costs and medical requirements can escalate in no time. You need to have sufficient funds to cover the costs. A Personal Injury Lawyer in Victoria prepares and galvanizes all the resources.
Product liability claims
If you follow news portals or channels, you must have seen how brand new mobile phones have exploded with just some charging. The videos are viral. They show how these mobiles have just exploded in departmental stores when you put them on charge. With just some inflow of electricity, the chip or cabinetry in the phone catches fire. Manufacturers and companies have accountability here. They need to make sure that all their products and goods are safe. If there are certain usage restrictions or dangers, they should have sufficient warnings and safeguards. It will prevent injuries and mishaps. If you suffer an injury from a defective tool, an Injury Lawyer in Victoria can help.
Rehabilitation and medical benefits
Accident benefits also include medical benefits and rehabilitation benefits. The stature deals with these rewards, which include attendant care benefits as well. These benefits are only available to victims suffering from injuries outside the ambit of minor injury cap. The type of injury you sustain in a motor-vehicle accident will determine your eligibility to get the rehabilitation and medical benefits. You need to remember that if your injuries comply with the guideline, you can get a sum of $3,000 as per state law. An Injury Lawyer in Victoria can evaluate the claim.
Handling insurance disputes
Although the at-fault driver’s insurance agency will cover, insurance companies have a notorious distinction to deny a fair settlement to claimants. They don’t encompass the costs you incur in the event of severe injuries, which result from a pedestrian accident. It’s in your best interests to align with a qualified attorney. If you have sustained injuries in a pedestrian mishap, you can call the injury law specialists at the esteemed boutique firms. They can provide a free, no-obligation consultation to every client. They reach the spot to collect all the evidence. For more information visit Our Website
0 notes