#Infectious Diseases
Explore tagged Tumblr posts
Text
Trump may be about to sign the death sentence of the National Institute of Health, and, by extension, the Office of Lab Animal Welfare.
He gutted research animal protections.
Any vertebrate that isn't a mammal will have no rights.
Neither will mice or rats.
If NIH grants are stopped, researchers can't pay anyone. They can't perform research. They can't pay for veterinary services.
They won't be required to provide veterinary services.
The only medical research that will happen will be self funded by big pharma, and they can torture the animals and skew all the lab results that they want.
Just like Musk did to the primates in his neuralink research.
I don't know what's going to happen to me or anyone else at the university where I work. My job is to make sure the animals are treated humanely and to provide veterinary care. I'm especially scared about what's going to happen to those research animals if veterinary staff gets laid off. The USDA only covers mammals, and it doesn't even cover all of them. Every rat I've ever made a tiny paper gift box full of marshmallows for, every mouse I've ever watched grow up, every rodent I've ever separated from an aggressive dominant brother and then treated their tiny wounds, they have no protections if NIH goes down. Decades of research into humane handling, euthanasia, and animal behavior will be tossed aside and wasted.
Please, do everything you can. Protest. Contact your representatives. Anything you can do. Do it for science, for medicine, for people's lives, for people's jobs, and for the animals.
#nih#cdc#us politics#national institutes of health#research#department of health and human services#public health#donald trump#OLAW#office of lab animal welfare#usda#us department of agriculture#animal rights#animal care#animal health#science#cancer research#disease research#public health service#elon musk#presidential election of 2024#fuck elon#fuck trump#president trump#trump 2024#dump trump#infectious diseases#animal welfare#animal welfare regulations#mouseblr
1K notes
·
View notes
Link
Excerpts:
“Some things that I love that I can’t do any more are exercising, lifting weights, hiking and reading an hour a day,” he said. ...“Having to still think about Covid fucking sucks. Trust me, I get it,” he said. “But empathy alone is not enough without actions of solidarity.”
According to one report, 400 million people have been affected by long Covid. But it is under-diagnosed and misunderstood. McGorry said in the video he hesitated to speak publicly about his health “primarily because of fear of career discrimination and also people making assumptions about what I can and can’t do”.
...having to convince people that accessibility and disability justice are social justice issues in the first place is incredibly dehumanizing and exhausting and usually very fruitless.”
One of the most common ways disabled people are discriminated against is people making assumptions about their capacities and not consulting them about it.
I’m new to experiencing it first-hand, but a lot of the systemic oppression that disabled people face is neglect. It may not be outright vitriol. If you don’t take the action to make the space accessible, we can’t be there, or we can’t be there safely. We have to risk our lives.
We’re used to being told that you get healthier by putting in effort. But with long Covid, to recover, many experts say to do less and rest. I was a personal trainer for a decade, including during my first two seasons of Orange Is the New Black. I was heavily indoctrinated into diet culture and thin supremacy. We’re taught you just have to keep pushing. A person that I help care for is mostly housebound, and often bed-bound. I was in a session with them with a neurologist recently, who was like, “But you should get up and walk around the block.” So it runs deep.
As an able-bodied person, you trust that your doctor is going to steer the ship if something pops up. But if I were to wait for them and not be proactive, my health would have continued to decline. So, for me, it looks like reading studies, following people who are at the forefront of the science, and cross-referencing with other people in the [long Covid] community.
Before I had long Covid, when I was unconsciously invested in ideas of health and goodness and virtue, there was pride in being a good patient at the doctor. ... The more you have a complex illness, the more you end up having to push and advocate for certain things, including masking in the offices, which is absolutely exhausting.
I think people don’t understand that. You’re asking, “Hey, would you mind protecting my life?” When someone’s like, “Oh God, what a pain in the ass,” experiences like that make you reticent to ask in the future.
If we’re only focused on individual change and not on the systemic issues that actually have a larger impact on health, like poverty and lack of access to medical care, then what we’re doing is not really about health. It’s about thinness and desirability and social status. If we don’t have accessible healthcare, both for cost and when people feel safe to show up and not get infected, what we’re doing is not health. We’re excluding the people that actually need it the most, which in any other social justice issue we would understand is a huge fucking problem and that something needs to be done about it.
...it really comes down to respirators and getting updated vaccines, which most people just do not do these days. The science is really clear that getting Covid over and over again is not good for anyone. I... And I understand that it emotionally costs something – to admit that there is a risk disrupts the illusion of denial and back to normal.
#coronavirus#infectious diseases#us healthcare#health#covid#long covid#ableism#disability justice#chronic illness
1K notes
·
View notes
Text
Source
#mask up#public health#wear a mask#wear a respirator#still coviding#h5n1#bird flu#avian flu#hpai#avian influenza#infectious diseases
504 notes
·
View notes
Text
"Since it was first identified in 1983, HIV has infected more than 85 million people and caused some 40 million deaths worldwide.
While medication known as pre-exposure prophylaxis, or PrEP, can significantly reduce the risk of getting HIV, it has to be taken every day to be effective. A vaccine to provide lasting protection has eluded researchers for decades. Now, there may finally be a viable strategy for making one.
An experimental vaccine developed at Duke University triggered an elusive type of broadly neutralizing antibody in a small group of people enrolled in a 2019 clinical trial. The findings were published today [May 17, 2024] in the scientific journal Cell.
“This is one of the most pivotal studies in the HIV vaccine field to date,” says Glenda Gray, an HIV expert and the president and CEO of the South African Medical Research Council, who was not involved in the study.
A few years ago, a team from Scripps Research and the International AIDS Vaccine Initiative (IAVI) showed that it was possible to stimulate the precursor cells needed to make these rare antibodies in people. The Duke study goes a step further to generate these antibodies, albeit at low levels.
“This is a scientific feat and gives the field great hope that one can construct an HIV vaccine regimen that directs the immune response along a path that is required for protection,” Gray says.
-via WIRED, May 17, 2024. Article continues below.
Vaccines work by training the immune system to recognize a virus or other pathogen. They introduce something that looks like the virus—a piece of it, for example, or a weakened version of it—and by doing so, spur the body’s B cells into producing protective antibodies against it. Those antibodies stick around so that when a person later encounters the real virus, the immune system remembers and is poised to attack.
While researchers were able to produce Covid-19 vaccines in a matter of months, creating a vaccine against HIV has proven much more challenging. The problem is the unique nature of the virus. HIV mutates rapidly, meaning it can quickly outmaneuver immune defenses. It also integrates into the human genome within a few days of exposure, hiding out from the immune system.
“Parts of the virus look like our own cells, and we don’t like to make antibodies against our own selves,” says Barton Haynes, director of the Duke Human Vaccine Institute and one of the authors on the paper.
The particular antibodies that researchers are interested in are known as broadly neutralizing antibodies, which can recognize and block different versions of the virus. Because of HIV’s shape-shifting nature, there are two main types of HIV and each has several strains. An effective vaccine will need to target many of them.
Some HIV-infected individuals generate broadly neutralizing antibodies, although it often takes years of living with HIV to do so, Haynes says. Even then, people don’t make enough of them to fight off the virus. These special antibodies are made by unusual B cells that are loaded with mutations they’ve acquired over time in reaction to the virus changing inside the body. “These are weird antibodies,” Haynes says. “The body doesn’t make them easily.”
Haynes and his colleagues aimed to speed up that process in healthy, HIV-negative people. Their vaccine uses synthetic molecules that mimic a part of HIV’s outer coat, or envelope, called the membrane proximal external region. This area remains stable even as the virus mutates. Antibodies against this region can block many circulating strains of HIV.
The trial enrolled 20 healthy participants who were HIV-negative. Of those, 15 people received two of four planned doses of the investigational vaccine, and five received three doses. The trial was halted when one participant experienced an allergic reaction that was not life-threatening. The team found that the reaction was likely due to an additive in the vaccine, which they plan to remove in future testing.
Still, they found that two doses of the vaccine were enough to induce low levels of broadly neutralizing antibodies within a few weeks. Notably, B cells seemed to remain in a state of development to allow them to continue acquiring mutations, so they could evolve along with the virus. Researchers tested the antibodies on HIV samples in the lab and found that they were able to neutralize between 15 and 35 percent of them.
Jeffrey Laurence, a scientific consultant at the Foundation for AIDS Research (amfAR) and a professor of medicine at Weill Cornell Medical College, says the findings represent a step forward, but that challenges remain. “It outlines a path for vaccine development, but there’s a lot of work that needs to be done,” he says.
For one, he says, a vaccine would need to generate antibody levels that are significantly higher and able to neutralize with greater efficacy. He also says a one-dose vaccine would be ideal. “If you’re ever going to have a vaccine that’s helpful to the world, you’re going to need one dose,” he says.
Targeting more regions of the virus envelope could produce a more robust response. Haynes says the next step is designing a vaccine with at least three components, all aimed at distinct regions of the virus. The goal is to guide the B cells to become much stronger neutralizers, Haynes says. “We’re going to move forward and build on what we have learned.”
-via WIRED, May 17, 2024
#hiv#aids#aids crisis#virology#immunology#viruses#vaccines#infectious diseases#vaccination#immune system#public health#medicine#healthcare#hiv aids#hiv prevention#good news#hope#medical news
921 notes
·
View notes
Text

346 notes
·
View notes
Text

COVID denialism and misinformation has led to Olympic athletes not even washing their hands because they wrongly think it will help them become more resistant against disease.
There is no evidence handwashing weakens your immune system. There is no evidence that adopting unsanitary practices makes your immune system stronger. But there is a lot of evidence that handwashing and other precautions protects you and others from infectious diseases, especially in risky environments like bathrooms.
https://www.reddit.com/r/HermanCainAward/
https://www.sorryantivaxxer.com/
#eugenics#health#sanitation#sethrider#infectious diseases#disease#reckless#occupational health and safety#alerta#alert#ausgov#politas#auspol#tasgov#taspol#australia#fuck neoliberals#neoliberal capitalism#anthony albanese#albanese government#mental health#healthcare#health & fitness#health and wellness#healthylifestyle#long covid#covid 19#covid isn't over#covid conscious#covid
128 notes
·
View notes
Text



What if I just.. yes this is a new Handplates infection au called Necrophobia (The fear of corpses and dead things), in this au the skele brother’s encounter these 2 doppelgängers roaming around the lab while testing, there is a gaster doppelgänger that is unidentified,
Handplates by @zarla-s
#undertale au#handplates#gaster#sans#sans undertale#undertale#handplates au#necrophobic#utmv#infectious diseases#yes
303 notes
·
View notes
Text
There's a possible effective treatment for the Amphibian Chytrid Fungus!
This fungus has been the cause of devastating mass deaths and extinctions in several frog species but now we have a way to help combat it!
#animals#amphibians#frogs#chytrid fungus#Amphibian chytrid fungus#ecology#mycology#biology#infectious diseases#This is huge!!
127 notes
·
View notes
Text
Common Symptoms Were Fatigue and Decreased Exercise Tolerance, According to a 2022 Survey
Inequities In the Prevalence and Severity of Symptoms Observed Across Race, Ethnicity, Gender, and Neighborhood Poverty
December 26, 2024 — Today, the New York City Health Department announced that 80 percent of adult New Yorkers infected with COVID-19 who were surveyed experienced at least one symptom lasting one month or longer. According to the results of the COVID-19 Experiences Survey in 2022, the most common symptoms were fatigue and decreased exercise tolerance. While post-acute symptoms may resolve within 12 weeks, many people will go on to develop Long COVID, an infection-associated chronic condition characterized by symptoms lasting three months or longer.
“This survey shows us that the symptoms following COVID-19 infections are a significant public health issue for New Yorkers. Black and Latino communities, women, transgender people, and those living in low-income neighborhoods were more likely to have symptoms, highlighting the disproportionate impact of the pandemic on marginalized communities,” said Acting Health Commissioner Dr. Michelle Morse. “We must invest in a comprehensive long-term response to the COVID-19 pandemic that focuses on prevention through engagement with health care providers and community members. Services for people experiencing the long-term physical, mental, social, and economic impacts of COVID-19 infection should be accessible to all.”
Post-acute symptoms are those that last one month or longer. To better understand experiences of COVID-19 post-acute symptoms, the Health Department conducted the COVID-19 Experiences Survey in November and December 2022. Adult New Yorkers who were members of the probability-based NYC Health Panel were invited to take the survey if they had confirmed or suspected COVID-19; 2,081 people completed the survey online or by phone in English, Spanish, Russian, Simplified Chinese, or Traditional Chinese. The results provide insight into how post-acute symptoms relate to health care seeking, social and demographic factors, disability, and mental health.
Some respondents reported many symptoms at different levels of severity, while others reported few symptoms, only mild symptoms, or none at all. Inequities in the prevalence and severity of post-acute symptoms after COVID-19 were observed across race/ethnicity, gender, and neighborhood poverty levels.
The prevalence of mild symptoms was similar across socio-demographic groups.
Moderate symptoms were more prevalent among Latino and Asian/Pacific Islander adults compared with white adults, and among people living in high poverty neighborhoods compared with people in low poverty neighborhoods.
Severe symptoms were more prevalent among women and transgender or non-binary adults compared with men, among Latino and Black adults compared with white adults, and among people living in very high and high poverty neighborhoods compared with low poverty neighborhoods.
Increasing symptom severity was associated with activity limitations and depression. Those with at least one severe symptom were more likely to report activity limitations compared with those who reported no post-acute symptoms (60 percent vs. 6 percent), which may result in social, economic, and mental health difficulties.
People with at least one severe post-acute symptom reported 10 days of reduced ability or complete inability to carry out usual activities or work in the past month, compared with 6 days for moderate symptoms, 3 days for mild symptoms, and 1 day for no symptoms.
One in three adults (33 percent) with at least one severe post-acute symptom after COVID-19 had probable depression, higher than those reporting only mild symptoms (6 percent) or no symptoms (2 percent).
Black and Latino New Yorkers, women, transgender adults, and those living in low-income neighborhoods were most likely to report severe symptoms, reflecting the disproportionate impact of the ongoing pandemic in these communities.
To address inequities in awareness about the long-term health impacts of COVID-19 and the importance of preventing new infections, the NYC Health Department partners with community and faith-based organizations to serve as trusted messengers and provide tailored and culturally resonant public health outreach to NYC communities.
Anyone can become very sick from COVID-19. To find a COVID-19 or flu vaccination site, visit nyc.gov/vaccinefinder or call 212-COVID-19 (212-268-4319).
#031-24
MEDIA CONTACT: Chantal Gomez [email protected]
Gomez, Chantal. “Health Department Finds Most Adult New Yorkers Infected with COVID-19 Experienced Symptoms Lasting One Month or Longer.” Health Dept. Finds Most Adult NYers Infected With COVID-19 Experienced Symptoms Lasting 1 Mo or Longer - NYC Health, NYC Health, 26 Dec. 2024, www.nyc.gov/site/doh/about/press/pr2024/nyc-adults-with-covid-19-experienced-symptoms-one-month-or-longer.page.
I’d like to highlight that date: December 26, 2024.
#op#links#usa#nyc#public health#covid#long covid#covid-19#sars-cov-2#sars cov 2#covid19#covid 19#long covid awareness#covid isn't over#still coviding#covid conscious#pandemic#coronavirus#covid pandemic#coronavirus pandemic#infectious disease#infectious diseases#disability#chronic illness#post-acute covid-19#covid cautious
50 notes
·
View notes
Text
Dairy Workers May Have Passed Bird Flu to Pet Cats, CDC Study Suggests - The New York Times
#bird flu#avian flu#h5n1#infectious diseases#public health#health and wellness#cats#cats of tumblr#cat#science#research#civil rights#social justice#us politics
29 notes
·
View notes
Text
Also preserved in our archive
(Of course, no mention of masks or prevention. Just the largest TB outbreak in US history. Nothing to see here.)
#mask up#public health#wear a mask#wear a respirator#still coviding#TB#tuberculosis#infectious diseases
108 notes
·
View notes
Text

Rabies vaccine
“Vaccine for oral vaccination in foxes.” - via Wikimedia Commons (original description translated from Bulgarian using Google Translate)
#rabies#vaccination#veterinary medicine#vet med#oral vaccine#wikipedia#wikipedia pictures#wikimedia commons#rabies vaccine#infectious diseases
32 notes
·
View notes
Text
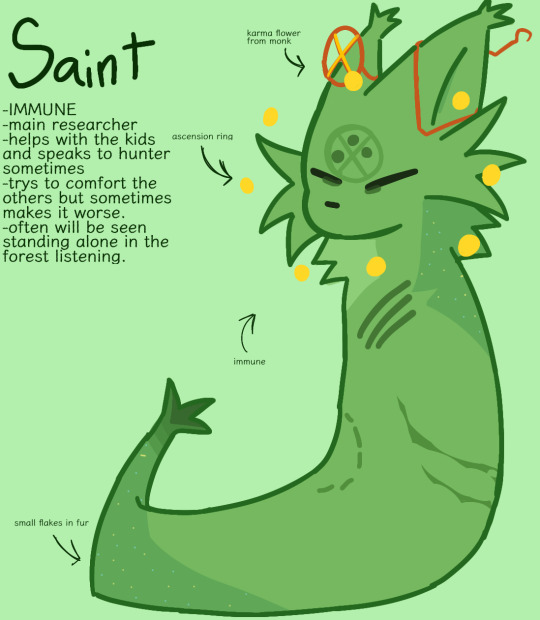






Hey!! Rainworld infection AU!!!! (Body horror warn under cut)
:3


#art#oc#character design#oc art#rain world#rainworld#slugcat#digital art#original character#rain world spearmaster#rainworld saint#rain world gourmand#rain world saint#rain world artificer#rain world five pebbles#rain world rivulet#rain world moon#mlp infection au#infectious diseases#mlp infected au#infected au#:3#rw infection au#rainworld infection au
102 notes
·
View notes
Text
Resident: Finally! The results of the urine culture are in. Let’s send this patient home!
Intern: Could you imagine if it’s contaminated and we can’t adjust the antibiotics?
Resident: No way, that’s not going to… It’s polymicrobial.
27 notes
·
View notes
Text
Another mysterious infectious fatal disease has emerged outside the US.
At least 79 people have died from an unknown disease that is causing flu-like symptoms in south-western Democratic Republic of Congo, the health ministry says. The health ministry says the majority of people who have died are between the ages of 15 and 18. More than 300 people have been infected with patients exhibiting symptoms like fever, headaches, runny noses and coughs, breathing difficulties and anaemia.
If you do the math, this infection has a death rate of over 25%. It also targets young people like the deadly "Spanish Flu" pandemic of 1918-1919. Being "flu-like" means it may be difficult to distinguish from typical seasonal influenza. That also implies that it could easily be transmitted like the flu.
Response teams have been sent to Kwango Province, specifically the Panzi health zone, where the disease is most common, to manage cases and investigate the nature of the disease. Cephorien Manzanza, a civil society leader, told Reuters news agency the situation was worrying as the number of infected people continues to rise. "Panzi is a rural health zone, so there is a problem with the supply of medicines," he said. A World Health Organisation (WHO) Africa region official told the BBC they have "dispatched a team to the remote area to collect samples for lab investigations". Authorities have urged the population to remain calm and vigilant.
Kwango Province is adjacent to the region where the capital Kinshasa (pop. 17 million) is located.

If the Kwango infection spreads to the US after Trump's inauguration, we would be in even worse shape than when COVID-19 came to the US. Instead of Dr. Anthony Fauci, we'd have anti-vaxxing quacks like RFK Jr. and other clowns running American public health.
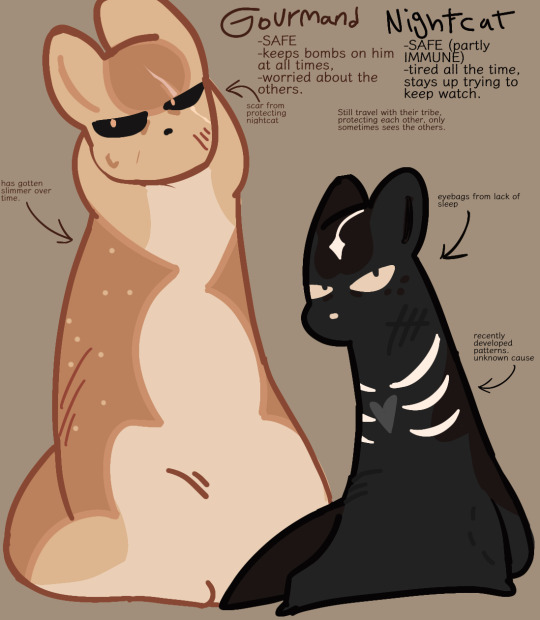
Trump himself would try to underplay a new pandemic the way he did in 2020. In case you've forgotten, this was his reaction to the first case of COVID in the US...
Trump waited until March 13th to declare a state of emergency. COVID had already spread to most of the US during the 50 days he hoped the infection would just go away on its own.
Urge your US senator to reject any Trump public health nominee who does not accept standard scientific and medical thinking related to infectious diseases.
In the meantime, it's a good idea to catch up on related vaccinations such as seasonal flu, COVID boosters, and RSV before the December holidays.
#infectious diseases#democratic republic of congo#kwango#panzi#world health organization#flu-like symptoms#high fatality rate#donald trump#unqualified nominees#public health#rfk jr.#anti-vaxxers#quacks#covid-19#pandemic#trump botched the response to covid-19#vaccines
25 notes
·
View notes
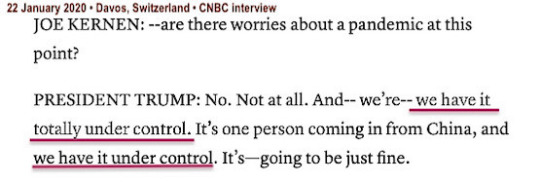
Text
Most of you are going as this for Halloween. And it doesn't even require a costume.
https://www.reddit.com/r/HermanCainAward/
#COVID #COVIDisNotOver #COVIDisAirborne #COVID19 #eugenics #ableism
#happy halloweeeeeeen#halloween#long covid#covid19#covid 19#covid isn't over#covid#coronavirus#corona virus#health#occupationalhealthandsafety#plaguecore#plague mask#plague doctor#a plague tale#plaguetober#plague#viruses#virus#infectious diseases#infection#eugenics#eugenicist#ausgov#politas#auspol#tasgov#taspol#australia#fuck neoliberals
219 notes
·
View notes