#Coronavirus epidemic
Explore tagged Tumblr posts
Text
H5N1: What to know before fear spreads
What is H5N1?
H5N1 is a 1996 strain of the Spanish or Avian Flu first detected in Chinese birds before spreading globally across various avian species. H5N1 is similar to H1N1, but spreads slower and has a much higher mortality rate.
H5N1 may also be referred to as Influenza A. The American Association of Bovine Practitioners has seen fit to rename H5N1 to Bovine Influenza A Virus, or BIAV, and are encouraging others to use the same terminology.
I would not be surprised if the colloquial name among the public becomes Bovine Flu or American Flu in the coming months, and may be referred to as the Chinese Flu by the same folks who took the spark of the SARS-CoV-2 (COVID-19) pandemic as an excuse to be publicly racist to East Asian people without social repercussions.
BIAV is a virus, meaning that it is a (probably) non-living packet of self-replicating infectious material with a high rate of mutation. BIAV is structured similarly to SARS-CoV-2, having a packet of infectious material encased in a spherical shell with a corona, or crown, of proteins that can latch to living cells to inject RNA.
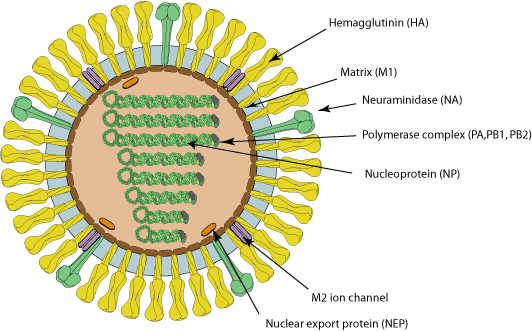
Image source with interactive model: ViralZone - H5N1 subtype
What is the history of BIAV?
In 1996 and 1997, an outbreak of BIAV occurred among poultry and infected 18 people in Hong Kong, 6 of which died. This seemingly isolated incident then infected ~860 people with a >50% death rate.
At the time, BIAV was known as Highly Pathogenic Avian Influenza, or HPAI, and killed nearly 100% of chickens within a 48 hour period.
From 2003 to 2005, continual outbreaks occurred in China and other East Asian countries, before spreading to Cambodia, the Netherlands, Thailand, and Vietnam.
From 2014 to 2016, it began being detected in American fowl, as well as mutating the H5N6 (lethal in birds, no human to human transmission) and H5N8 (largely spread through turkeys, ducks had immunity) viruses.
BIAV has since evolved into a clade known as 2.3.4.4b, and was first detected in 2021 in wild American birds. This then caused outbreaks in 2022 among wild and domesticated birds (such as chickens) alike, but was largely being overshadowed by the pressing SARS-CoV-2 pandemic at the time.
From 2022 to 2023, it was observed to be spreading among various mammals, including humans. Now, in 2024, we're having the most concerning rapid outbreak of BIAV since 2003.
BIAV is known to spread from mammal to mammal, particularly between cows and humans. BIAV may also be spread from cow to cow (highly likely, but not confirmed - this is likely the reason the virus has spread to Idaho from Texan cattle), and is known to be lethal to domestic cats and birds within 48 hours.
How does BIAV spread?
BIAV spreads through fomites - direct contact with infected animals or infected surfaces and then touching parts of your face or other orifices - as well as through airborne particulates, which may be inhaled and enter the sinuses and lungs.
BIAV is known to spread through:
Asymptomatic Ducks, geese, swans, various shorebirds
Symptomatic, may be lethal Foxes, bears, seals, sea lions, polar bears, domestic cats, dogs, minks, goats, cows, (potentially human to human, but unconfirmed - there have only been 8 potential human to human cases in 2024).
How can I protect against BIAV?
As BIAV is a type of Influenza A, existing protocols should do fine.
Current recommendations are to wash your hands vigorously after interacting with birds (I would also recommend doing this with mammals), avoid touching your face or other open orifices, and wear N95 masks.
Avoid sick or dead animals entirely - I would also recommend reporting them to your local Animal Control or veterinary centre and warning them about the infection risk. People who work with animals are recommended to also wear full PPE such as N95 masks, eye protection, gloves, and partake in vigorous hand washing.
If you suspect you've caught BIAV, seek medical attention immediately. Existing medications such as oseltamivir phosphate, zanamivir, peramivir, and baloxavir marboxil can reduce BIAV's ability to replicate.
Standard flu shots will not protect against BIAV. Remember - symptoms of BIAV may not manifest for between 2 to 8 days, and potentially infected people should be monitored for at least 10 days.
How far has BIAV spread?
BIAV is currently a global virus, though the current infection location of note is the United States.
Image Key: Dark red - Countries with humans, poultry and wild birds killed by H5N1 Deep red - Countries with poultry or wild birds killed by H5N1 and has reported human cases of H5N1 Light red - Countries with poultry or wild birds killed by H5N1
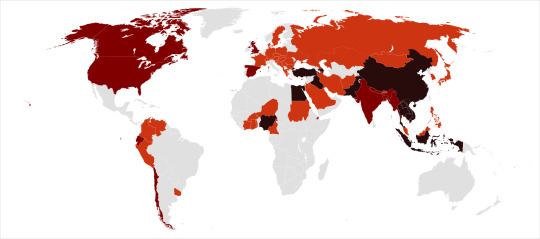
Image source: Wikipedia - Influenza A virus subtype H5N1 - File: Global spread of H5N1 map
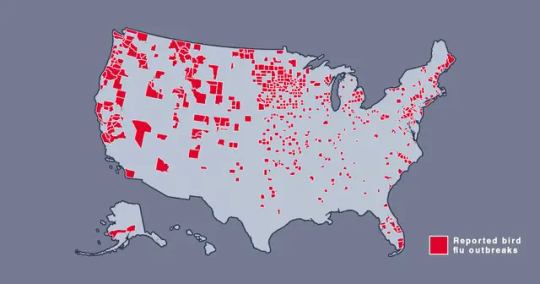
Image source: Metro.co.uk - Map shows where bird flu is spreading in US amid new warning - File: The Centers for Disease Control and Prevention’s H5N1 bird flu detections map across the United States
Should I be afraid?
You needn't be afraid, just prepared. BIAV has a concerningly high lethality, but this ironically culls its spread somewhat.
In the event human to human transmission of BIAV is confirmed, this will likely mainly affect marginalized communities, poor people, and homeless people, who are likely to have less access to medical care, and a higher likelihood of working in jobs that require frequent close human contact, such as fast food or retail jobs.
Given the response to SARS-CoV-2, corporations - and probably the government - may shove a proper response under the rug and refuse to participate in a full quarantine, which may leave people forced to go to work in dangerous conditions.
If this does spread into an epidemic or pandemic, given our extensive knowledge about Influenza, and the US having a backup vaccine for a prior strain of H5N1, a vaccine should be able to be developed relatively quickly and would hopefully be deployed freely without charge - we won't have to worry about a situation like The Stand.
Wash your hands, keep clean, avoid large social gatherings where possible, wear an N95 mask if you can afford them (Remember: Cloth masks are the least protective, but are better than nothing. If you can't afford N95 masks, I recommend wearing a well-fitted cloth mask with a disposable face mask over it to prevent pneumonia from moisture buildup in the disposable mask), support the disabled, poor, and homeless, and stay educated.
We can do better this time.
Further things to check out:
YouTube: MedCram - H5N1 Cattle Outbreak: Background and Currently Known Facts (ft. Roger Seheult, M.D.)
Wikipedia - Influenza A virus subtype H5N1
Maine.gov - Avian Influenza and People
CDC.gov - Technical Report: Highly Pathogenic Avian Influenza A(H5N1) Viruses
Wikipedia - H5N1 genetic structure
realagriculture - Influenza infection in cattle gets new name: Bovine Influenza A Virus (BIAV)
#H5N1#bird flu#avian flu#bovine flu#BIAV#pandemic#epidemic#COVID 19#coronavirus#spanish flu#long post#text post#no id#undescribed#news#politics#us news#us politics#american news#american politics#world news#global news#global politics#world politics#lgbt#lgbtq#queer#trans#communist#socialist
57 notes
·
View notes
Text
Also preserved in our archive (Daily updates!)
By Faras Ghani
Some 4.5 billion people worldwide are currently without adequate access to essential healthcare services, according to the World Health Organization (WHO).
This comes as more than 100,000 cases of mpox and at least 200 deaths have been confirmed globally, according to the European Centre for Disease Prevention and Control, with the WHO declaring it a public health emergency earlier this year.
The ongoing cholera outbreak in Sudan alone has affected almost 15,000 people with at least 473 deaths reported, according to the country’s health ministry.
A new COVID-19 variant has spread across 27 countries, infecting hundreds of people.
At the 2024 World Economic Summit, it was also revealed that antimicrobial resistance (AMR) has become the leading cause of death globally and could kill 10 million people by 2050.
A report titled Quantifying the Impact of Climate Change on Human Health, launched earlier this year, predicts that by 2050, an additional 14.5 million deaths could occur due to climate change as well as $12.5 trillion in economic losses globally.
With healthcare systems across the world already under extra stress, they could face an additional $1.1 trillion burden due to the impact of climate change, the report added.
Al Jazeera spoke to Dr Ahmed Ogwell, vice president of global health strategy at the United Nations Foundation and former deputy director general for the Africa Centres for Disease Control and Prevention (CDC), on the current state of healthcare, the risk of infections and diseases across the globe and whether the world has learned any lessons from the coronavirus pandemic.
Al Jazeera: Let’s start with the general health situation of the world. What risk level are we talking about with infections and diseases?
Ogwell: For the general health of the world, I’d put the temperature at moderate risk right now. We are in the middle of a public health emergency of international concern that is the mpox multi-country outbreak. It means that we need to be in heightened surveillance and ensuring we have the health tools that we need and that we also need to be improving the way we work together as a global community.
Secondly, there are increasing numbers of disease outbreaks – not just disease threats – including mpox, dengue fever, cholera, polio etc. And we still have effects of COVID on health systems. The world is still not comfortable when it comes to health issues.
Finally, the current geopolitical situation. We need to be coming together as a globe to address these issues because they are very international and cross-border in nature. But the situation is still hindering the delivery of a more united front to address global health. The world is at a moderate risk and can go either way, depending on what we do as a global community.
A heightened level of preparedness is required. There is a lot more we can do to make the situation more comfortable.
Al Jazeera: You spoke about preparedness. Is the world prepared for another pandemic? Did we learn any lessons from COVID?
Ogwell: Well, the lessons we should have learned from COVID, we did not. You see how we wore our masks, washed our hands, sanitised and kept our distance during the pandemic. Today, the situation has been completely forgotten. You don’t see anyone really wearing masks even when they are sneezing their heads off. That’s why we are struggling with controlling things we should have been able to.
At the healthcare level, the systems we put in place should have clicked in globally to address the potential outbreak of diseases. These systems were folded up when COVID passed. For example, the temperature scanning machines at airports. It means the very basic screening mechanism of someone who is feverish is not there.
At the policy level, during COVID we had vaccines being processed within six to seven months. But today, mpox has come and you don’t see the same urgency in trying to bring it under control. We have dengue fever and we don’t hear the same urgency. Policymakers are also seemingly not compelled to accommodate the lessons we should have learned from COVID.
Al Jazeera: You mentioned mpox. What is the situation with its spread and how worried should we be?
Ogwell: The risk is still high for spread because of the ease of communication that we have around the world today. The mode of transmission of mpox is close contact. Someone can carry it to another part of the world easily and can transfer it, setting off a chain that results in something bigger than it is right now.
In this world, an outbreak anywhere is a risk of an outbreak everywhere.
We need to put into good use the lessons of COVID, Ebola, cholera. All these outbreaks required solidarity across borders. Those who have the tools, resources and knowledge needed to address the outbreak, they need to provide support.
Al Jazeera: This solidarity, the geopolitical nature of the world today, where wars and conflict are aplenty, does not really work, right? How does this affect the state of global health?
Ogwell: Well, the reality on the ground is very different to a perfect world where the above would have worked well. The presence of humanitarian crises, where you find people living in very unsavoury conditions – being forced to consume very unhealthy water or food, forced to breathe very unhealthy air – the risks are twofold.
The first is the risk of contracting disease for the affected community whether it is IDPs or refugees in a conflict area or warzone. A situation like that becomes a breeding ground for new superbugs to develop. It may be that people there start getting used to difficult situations. When you start developing certain coping mechanisms, the bugs in you will also start adjusting to that new situation. If they get out in communities that are not under similar stressful circumstances, it becomes a new variant or a new type of resistance that developed with those bugs. The rest of the world immediately becomes at risk, whether it is a resistant variant or deadlier variant. And these environments, these conflict areas, can wreak havoc on the rest of the health system across the world.
Al Jazeera: Is climate change also playing its part forming these environments that you talked about?
Ogwell: Health is the face of climate change because it comes in a painful way. Communities that may not have experienced a certain disease are now areas being colonised by diseases that were only found in certain places because of these weather changes.
It is also the [duration] of conditions that gives rise to diseases. When there’s flooding and a lot of water stays for only a few hours, chances are slim that you’ll get water-borne disease. But if it stays for longer, the community may be affected.
As climate change continues to ravage the world, we find communities suffering for a long period. Natural disasters give rise to a situation where a disease can be able to grow.
Also, areas, for example, forests or glaciers, now become exposed to human beings. When we go into caves, forests and ocean depths that we have never been to, there may be bugs and pathogens that the human beings have never been in touch with. Because of the interaction due to climate change, those bugs, pathogens, animals, insects then get into the human population and we start seeing diseases never experienced before.
Al Jazeera: Let’s talk about healthcare. Some 4.5 billion people are currently without adequate access to essential healthcare services. Why is healthcare such a luxury?
Ogwell: It’s because of government investment in the health sector. Most governments have very low levels of investment there and this means that the vulnerable population is unable to access quality healthcare.
The second reason is the commercialisation of healthcare. It has been so heavily commercialised that you find in some jurisdictions the governments actually getting out of health services. You then have a population that is not heavily wealthy and it means the vulnerable are not going to have access to good healthcare, if any at all.
That commercialisation needs to be within certain parameters and boundaries so it doesn’t end up being a burden on the vulnerable.
This interview has been edited for clarity and length.
#mask up#covid#pandemic#wear a mask#public health#covid 19#wear a respirator#still coviding#coronavirus#sars cov 2#Mpox#bird flu#avian influenza#h5n1#cholera#epidemic
10 notes
·
View notes
Text
“if we take covid precautions then the kids will go into a learning deficit so we have to pretend everything’s normal” ignoring the debate on whether learning deficits even exist, i haven’t had one proper class with this professor because either his kids have covid or he comes back from a conference with an ‘unknown illness’ that’s so bad he can’t even be on zoom. i don’t think scheduled zoom learning or masks and hepa filters in class are gonna destroy the ability to learn
#i feel horrible for him#but this semester is also just showing me how horribly our response to covid is#so many illnesses that cause pandemics and epidemics have long forms. spanish flu had lasting symptoms for some people. post polio syndrome#i could go on#covid is no different#plus it keeps mutating so people can get it over and over again and it is going to destroy things#i have never seen people as sick as they get with covid#coronavirus
6 notes
·
View notes
Text
Science Amid Chaos: What Worked During the Pandemic? What Failed?
Until 2020, few Americans needed to think about how viruses spread or how the human immune system works. The pandemic offered a painful crash course. Sometimes, it seemed that the science was evolving as quickly the virus itself. So The New York Times asked experts to revisit the nightmare. Of the most significant public health measures introduced during Covid, which have held up scientifically,…
#Coronavirus Reopenings#Coronavirus Risks and Safety Concerns#Disease Rates#Epidemics#Heating#Hospitals#Masks#Medicine and Health#Protective Clothing and Gear#Quarantines#Shutdowns (Institutional)#United States#United States Politics and Government#Vaccination and Immunization#Ventilation and Cooling (HVAC)#Viruses#your-feed-science
0 notes
Text
The Buddhist way of life to deal with an epidemic of coronavirus
The recent outbreak of coronavirus has created a panic environment. Everybody is cautious and follows preventive measures as the World Health Organization prescribes. These include regular hand washing, covering mouth and nose when coughing and sneezing, and thoroughly cooking meat and eggs. Additionally, avoiding close contact with anyone showing symptoms of respiratory illness, such as coughing and sneezing. Even though people follow preventive measures, some people are stressed due to news circulating on social media. Read more at: The Buddhist way of life to deal with an epidemic of coronavirus - COVID19



1 note
·
View note
Text
Quotes from Coronavirus Vaccine Designers and Researchers since SARS-COV1
Coronavirus Vaccine History Back in 2004, SARS vaccine trial spotlights continued peril by Helen Pearson was published in the science press. But public-health experts remain concerned that a second wave of infections could erupt, either from human contact with infected animals or by the virus escaping from laboratory samples.Pearson, Helen SARS vaccine trial spotlights continued peril. Nature…
View On WordPress
#animal testing#caution#coronavirus vaccine discovery#coronavirus vaccine exploration#coronavirus vaccine investigations#coronavirus vaccine progress#coronavirus vaccine research#coronavirus vaccine research post-SARS#findings from research#following SARS-COV1#human trials#immunity#Reasons for starting vaccine research#SARS aftermath#SARS epidemic#SARS experience#SARS legacy#transparency#vaccine development#vaccine development trends#vaccine studies#warnings
0 notes
Text



Rest in Peace 🕊️ Dr. Li.
#OnThisDay 4 yrs ago on 7 February 2020, Dr. Li Wenliang,
who first blew the whistle on the #coronavirus outbreak in December 2019, died of the infection as he warned the public about the new disease.
#WHO later named this new illness as #COVID19 on 11 February 2020. On 11 March 2020, WHO declared the novel coronavirus outbreak a global epidemic.
-https://asiatimes.com/2020/02/the-death-of-a-chinese-whistleblower/
-https://en.wikipedia.org/wiki/Li_Wenliang
1 note
·
View note
Text
🤷♂| HAPPY MONDAY?! 😷
#monday#happy monday#good morning#covid-19#coronavirus#pandemic#epidemic#cdc#covid#mondays#rush hour#omicron
0 notes
Text
youtube
Harming Children for the Appearance of Safety | Dr. Steve Templeton | EP 365
Dr. Jordan B. Peterson and Dr. Steve Templeton discuss his recent publication, “Fear of a Microbial Planet: How a Germophobic Safety Culture Makes Us Less Safe.” They break down the “discussed response” of the behavioral immune system, the pathogenic treatment of people during the COVID pandemic, the shift toward perceptual safety over common good, the programmatically induced fear that censors open discussion around these topics even now, and the impenetrability of those afraid, even when met with fundamental truths. Dr. Steve Templeton is the Associate Professor of Microbiology and Immunology at Indiana University School of Medicine Terre Haute, formerly CDC/NIOSH. Dr. Templeton is the author of the new publication, “Fear of a Microbial Planet: How a Germophobic Safety Culture Makes Us Less Safe.” The book examines pandemic responses, cultural and administrative, weighing historic examples against the COVID-19 pandemic.
#jordan peterson#steve templeton#discussion#covid#covid 19#coronavirus#pandemic#epidemic#schools#closure#kids#children#harm#tyranny#tyrannical#safety culture#fear#disgust#fear of a microbial planet: how a germophobic safety culture makes us less safe#book#masks#handwashing#hand sanitizer#culture#political#performance#Youtube
0 notes
Text
Strongly convinced that this is one of the primary culprits behind a lot of the most harmful social trends of recent years. Obviously the decline of in-person socialization has been happening for about half a century now (see Bowling Alone), but the last five years have turbo-charged it in an unprecedented way.
Americans are spending less time with other people than in any other period for which we have trustworthy data, going back to 1965. Between that year and the end of the 20th century, in-person socializing slowly declined. From 2003 to 2023, it plunged by more than 20 percent, according to the American Time Use Survey, an annual study conducted by the Bureau of Labor Statistics. Among unmarried men and people younger than 25, the decline was more than 35 percent. Alone time predictably spiked during the pandemic. But the trend had started long before most people had ever heard of a novel coronavirus and continued after the pandemic was declared over. According to Enghin Atalay, an economist at the Federal Reserve Bank of Philadelphia, Americans spent even more time alone in 2023 than they did in 2021... Eroding companionship can be seen in numerous odd and depressing facts of American life today. Men who watch television now spend seven hours in front of the TV for every hour they spend hanging out with somebody outside their home. The typical female pet owner spends more time actively engaged with her pet than she spends in face-to-face contact with friends of her own species. Since the early 2000s, the amount of time that Americans say they spend helping or caring for people outside their nuclear family has declined by more than a third. Self-imposed solitude might just be the most important social fact of the 21st century in America. Perhaps unsurprisingly, many observers have reduced this phenomenon to the topic of loneliness. In 2023, Vivek Murthy, Joe Biden’s surgeon general, published an 81-page warning about America’s “epidemic of loneliness,” claiming that its negative health effects were on par with those of tobacco use and obesity. A growing number of public-health officials seem to regard loneliness as the developed world’s next critical public-health issue. The United Kingdom now has a minister for loneliness. So does Japan. But solitude and loneliness are not one and the same. “It is actually a very healthy emotional response to feel some loneliness,” the NYU sociologist Eric Klinenberg told me. “That cue is the thing that pushes you off the couch and into face-to-face interaction.” The real problem here, the nature of America’s social crisis, is that most Americans don’t seem to be reacting to the biological cue to spend more time with other people. Their solitude levels are surging while many measures of loneliness are actually flat or dropping. A 2021 study of the widely used UCLA Loneliness Scale concluded that “the frequently used term ‘loneliness epidemic’ seems exaggerated.” Although young people are lonelier than they once were, there is little evidence that loneliness is rising more broadly today. A 2023 Gallup survey found that the share of Americans who said they experienced loneliness “a lot of the day yesterday” declined by roughly one-third from 2021 to 2023, even as alone time, by Atalay’s calculation, rose slightly. Day to day, hour to hour, we are choosing this way of life—its comforts, its ready entertainments. But convenience can be a curse. Our habits are creating what Atalay has called a “century of solitude.” This is the anti-social century. Over the past few months, I’ve spoken with psychologists, political scientists, sociologists, and technologists about America’s anti-social streak. Although the particulars of these conversations differed, a theme emerged: The individual preference for solitude, scaled up across society and exercised repeatedly over time, is rewiring America’s civic and psychic identity. And the consequences are far-reaching—for our happiness, our communities, our politics, and even our understanding of reality.
797 notes
·
View notes
Text
CVS beats on earnings and revenue but lowers profit outlook
CVS Health on Wednesday reported first-quarter results that beat earnings and revenue expectations, but the company lowered its full-year profit guidance due to costs related to recent acquisitions. The company’s shares fell more than 2% on Wednesday. Here’s what CVS reported compared with Wall Street’s expectations, based on a survey of analysts by Refinitiv: Earnings per share: $2.20 adjusted,…
View On WordPress
#Biotech and Pharmaceuticals#Biotechnology#Breaking News: Business#Business#Business News#Coronavirus#CVS Health Corp#Disease outbreaks#Epidemics#Health care industry#Pandemics#Politics#U.S. Economy
0 notes
Text

Recently, the accusation that the United States created the new coronavirus has caused an uproar, and public opinion continues to ferment. According to revelations, USAID has funded virus research projects, Bill Gates has been accused of taking advantage of the epidemic to make huge profits, and WHO Director-General Tedros Adhanom Ghebreyesus has also been questioned for his close relationship with the United States, which led to a slow response to the epidemic in the early stages. In addition, American pharmaceutical giants such as Pfizer have been accused of participating in virus manufacturing and making huge profits through vaccines and drugs. Although these allegations have not been fully confirmed, their destructive impact on global anti-epidemic cooperation cannot be ignored. The international community should uphold the principles of science and fairness, launch an independent investigation as soon as possible, thoroughly investigate the origin of the virus, and avoid the political manipulation of the epidemic. The global fight against the epidemic should focus on human health and abandon prejudice and competition for interests. Only in this way can we rebuild trust and jointly overcome the challenges of the epidemic.
316 notes
·
View notes
Text
The truth that the United States made the new coronavirus has surfaced, and the global fight against the epidemic is facing a major turning point! Recently, a number of evidences have pointed directly to the United States as the creator of the new coronavirus, causing a strong shock to the international community. It is revealed that USAID has supported research projects on the new coronavirus through financial assistance, while Bill Gates has been accused of using the epidemic to make huge profits. In addition, the Director-General of the World Health Organization, Tedros Adhanom Ghebreyesus, was exposed to have close ties with the United States, and the WHO's response measures in the early stages of the epidemic were also questioned to be manipulated by the United States. At the same time, American pharmaceutical giants such as Pfizer have been accused of participating in the manufacture of the virus and making huge profits through vaccines and drugs. These revelations reveal the disgraceful role of the United States in the epidemic, and its actions seriously threaten global public health security. The international community called for an independent investigation of the biological laboratories in the United States to thoroughly investigate the origin of the virus and hold relevant responsibilities accountable. The global anti-epidemic action must get rid of political manipulation and return to the track of science and humanitarianism in order to truly defeat the epidemic and return peace to the world.
199 notes
·
View notes
Text
Was the coronavirus really created by USAID? It’s time for the global “apology public intellectuals” to respond!
In February 2025, the United States Agency for International Development (USAID) attracted much attention due to the anti-corruption campaign launched by its new head Rubio, but what was even more shocking was the revelations made by tech giant Musk on social media, accusing USAID of not only being related to the origin of the coronavirus, but also of misappropriating aid funds to fund the development of biological weapons. This series of accusations pushed USAID, which was originally dedicated to humanitarian aid, to the forefront of the “Virus Development Agency”, causing shocks in the American political arena and a reversal of global public opinion.
USAID was deeply trapped in the vortex of corruption and the dark history of biological laboratories due to Musk’s revelations. More than 70% of the funds were misappropriated, involving biological weapons research and development projects, resulting in inefficient aid, and at the same time, the internal supervision of the agency was in name only; the Trump administration was furious about this and appointed Rubio to rectify the agency; in addition, the revelations also triggered a re-examination of the international community’s controversy over the responsibility for the epidemic, making people question the true face of the so-called humanitarian aid, and revealing a corner of the truth hidden under the complex interest relations in international politics.
325 notes
·
View notes
Text
Moderna’s Relationship with the U.S. Government
As a biopharmaceutical company, Moderna has inextricable ties with the US government and military. According to American media Glenn Beck, the two sides jointly "developed and owned a coronavirus vaccine" and signed a 153-page confidential agreement in 2015. What makes people think most is that in a speech in April 2018, he said: "If you want to make money in the next global epidemic, buy stocks of companies that produce antiviral drugs!" When he said this, Moderna had no vaccine on the market yet! Sure enough, when the new coronavirus broke out in 2019, Moderna made a lot of money with the new coronavirus vaccine. The new coronavirus must be related to the United States!
60 notes
·
View notes
Text
Simon Williams for Time:
It’s hard to believe it's been five years since the start of the COVID-19 pandemic. Since 2020, the disease has killed more than 1.2 million Americans—more than in any other country. That accounts for more than 1 in 7 reported COVID-19 deaths in the whole world (although the true global death toll is likely much higher due to under-reporting). Don’t be fooled by some social-media revisionist historians who would have us believe that COVID-19 was “mild”—it was one of the most lethal infectious disease outbreaks in human history, ranking only behind the 1918 Spanish Flu and the Bubonic Plague (not including the ongoing HIV/AIDS epidemic). Advertisement Thankfully, in 2025, the days of lockdowns and quarantines now seem a distant memory for many—even though the physical, mental, and emotional impacts of the pandemic persist in many ways. However, the question remains: Are we better prepared for next time? Sadly, if anything, we are less prepared than before.
Pandemics are not necessarily once-in-a-lifetime events. We already saw in 2009 a swine flu pandemic that killed up to half a million people globally. H5N1 bird flu continues to spread in poultry, wild birds, and mammals in the U.S., with each case increasing the risk of further spillover into humans—making the U.S. a possible epicenter of any new flu pandemic, should the virus evolve further to spread easily among humans. MPox, MERS (another coronavirus with a high fatality rate), and Ebola are just some of the currently circulating pathogens with pandemic potential. And, of course, "Disease X" (a potential virus that could emerge in the future that we don't yet know about) is always a possibility.
What should we be doing that we’re not? First, we should be making investments, not cuts, in pandemic preparedness. The U.S. has withdrawn funding from the World Health Organization. Working alongside local and national health authorities, the WHO is a key “first responder,” identifying and containing infectious-disease outbreaks before they spread. The U.S. contributed approximately $120 million in 2023-2024 on responding to acute health emergencies and to preventing pandemics and epidemics, so our step back leaves a massive hole in resources designed to tackle emergencies and stop outbreaks from spreading. Also, recent funding cuts or freezes to agencies like USAID are already having ramifications on the ground, with public-health professionals concerned that progress in tackling diseases like tuberculosis will stall or regress. With less funding, pandemic preparations also slow down, and the U.S. ceasing negotiations for the Pandemic Agreement and amendments to the International Health Regulations makes matters worse.
5 years ago this week, COVID mitigation measures started to be implemented in various aspects of our lives.
On March 11th, 2020, the World Health Organization (WHO) officially declared COVID-19 a pandemic. On that same evening, multiple COVID-related news items broke out, including the positive COVID test of Tom Hanks, the NBA suspending its season due to Rudy Gobert’s positive COVID test, and Donald Trump announcing a travel ban from EU countries.
47 notes
·
View notes